Deformation Imaging
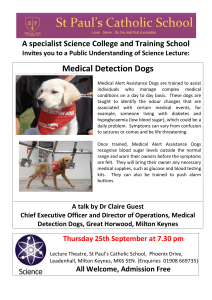
advertisement

Deformation Imaging AN ABSTRACT OF THE THESIS OF Marco L. Margiocco for the degree of Master of Science in Veterinary Science presented on December 17, 2007. Title: Deformation Imaging. Abstract approved: D. David Sisson Recent developments in the field of clinical echocardiography allow the ultrasonographer to objectively quantify both regional and global myocardial function. Regional deformation (Strain) and deformation rate (Strain Rate) are novel indices of ventricular function that can be estimated non-invasively by ultrasonographic interrogation of the heart. Deformation Imaging (DI) represents a family of echocardiographic techniques that can be employed to detect, quantify and display the characteristics of physical deformation of the myocardium. The objective of the studies described in this thesis was to investigate Doppler-derived deformation imaging in dogs. This Master’s Degree thesis is structured in two separate studies. The initial study compared Doppler-derived DI measures of ventricular function with more traditional invasive indices of cardiovascular function in healthy adult anesthetized dogs over a range of hemodynamic conditions created by serial pharmacologic manipulations. Five adult healthy dogs underwent simultaneous cardiac catheterization and transthoracic echocardiography under general anesthesia. The following invasive indices were monitored during the study: cardiac output (CO), femoral arterial (FA) and left ventricular (LV) pressures, +dP/dtmax, -dP/dtmax, right atrial (RA) and pulmonary arterial (PA) pressures, and pulmonary capillary wedge pressure (PCWP). Sequential manipulations of systolic function, afterload and preload were performed, respectively, by means of dobutamine, nitroprusside, and hetastarch infusions. Significant changes were induced in the following invasive hemodynamic parameters: cardiac output (p<0.0001, range 2.600 - 9.340 L/min), +dP/dtmax (p=0.0152, range 953.7 - 3822 mmHg/s), left ventricular end-diastolic pressure (LVEDP) (p<0.0001, range 0.210 -16.43 mmHg), mean right atrial pressure (p<0.0004, range -2.490 - 9.920 mmHg), systemic vascular resistance (SVR) (p<0.0001, range 510.0 - 2652 dyne*sec/cm5), and pulmonary vascular resistance (PVR) (p<0.05, range 256.4 -1635 dyne*sec/cm5). All dogs underwent a complete echocardiographic exam before anesthesia, after induction of general anesthesia and after each hemodynamic manipulation. A total of 750 regions of interest (ROIs) were included in the final analysis. Measurable plots were obtained in 741 (98.67%) out of 750 ROIs. Peak systolic strain rate (SSR) values obtained at the 6 ROIs did not differ significantly from each other and the avSSR (average of the 6 ROIs) negatively correlated with +dP/dtmax (r=0.9792, p=0.0208). Individual values of SSR from the different ROIs also negatively correlated with +dP/dtmax, with the exception of ROI 4 (basal portion of the interventricular septum). The lack of correlation was attributed to high variability in the measurements obtained from this specific ROI. The avSSR was significantly reduced, i.e. systolic function was increased, by the dobutamine infusion, but was not significantly changed during nitroprusside and hetastarch infusions. The LVEDP was significantly reduced during infusion of nitroprusside, apparently not influencing avSSR, and suggesting the possible preload independence of this parameter in the hemodynamic range generated in the study. Nitroprusside infusion effected a significant reduction of systemic vascular resistance without alteration of avSSR, suggesting a possible afterload independence of this parameter, at least in the hemodynamic range obtained in this study. Study 2 was conducted on healthy adult non-sedated dogs divided into four groups (group 1: Body weight (BW) < 15 kg, group 2: BW 15 - 30 kg, group 3: BW > 30 kg, and group 4: Doberman pinscher dogs). The aim of the study was to collect information on the feasibility, repeatability and reproducibility of Doppler-derived DI performed in a clinical setting. Of the initial 56 dogs from which echocardiographic data were collected, 7 dogs (12.5%) were excluded because of poor image quality, and data from 49 (87.5%) dogs were included in the final analysis. Of a total of 1470 ROIs analyzed, 4.65% yielded good quality curves, 88.3% were characterized by a significant amount of noise but retained a discernible pattern, and 7.14% were considered non-interpretable. Some pair-wise comparisons of the SSR values obtained from the 6 ROIs reached statistically significant difference. DI values in the Doberman pinscher group did not differ significantly compared to values obtained from a BWmatched group. DI values in group 1 dogs, but not the traditional indices FS and EF, were significantly higher compared to groups 2 and 3. Results from a Bland-Altman analysis revealed overall poor clinical repeatability and reproducibility, as a result of the wide variability of the data. Based on the results of study 1 we conclude that Doppler-derived SSR represents a useful load-independent index of global systolic function, as demonstrated in anesthetized dogs. However study 2 suggests that, in a population of non-sedated dogs, with a relatively wide range of breeds and BW, Doppler-derived DI measurements are characterized by less than optimal intra-operator and inter-operator variability which may limit its value as a tool to evaluate myocardial function in a clinical setting. Comparison to other newly developed non-invasive techniques to estimate regional myocardial deformation is needed to determine the eventual clinical utility of the method. ©Copyright by Marco L. Margiocco December 17, 2007 All Rights Reserved Deformation Imaging by Marco L. Margiocco A THESIS submitted to Oregon State University in partial fulfillment of the requirements for the degree of Master of Science Presented December 17, 2007 Commencement June 2008 Master of Science thesis of Marco L. Margiocco presented on December 17, 2007. APPROVED: Major Professor, representing Veterinary Science Head of the Department of Clinical Sciences Dean of the Graduate School I understand that my thesis will become part of the permanent collection of Oregon State University libraries. My signature below authorizes release of my thesis to any reader upon request. Marco L. Margiocco, Author ACKNOWLEDGEMENTS I wish to express sincere appreciation to the many individuals who have offered support, inspiration, and encouragement throughout this research effort. I like to thank Dr. Michele Borgarelli, who first introduced me to the world of veterinary cardiology, and still teaches me a lot about cardiology and friendship. A special thank goes to the Students, Staff, Faculty, breeders and owners who volunteered their dogs to the study. Immense gratitude goes to Ms. Robyn Panico, who devoted innumerable hours of technical support and who helped me throughout my whole residency: thank you Robyn for being a good and sincere friend to me. Dr. Craig Mosley and Dr. Rolando Quesada provided anesthesia support during the long hours of the invasive study, and without their assistance the study would have been much more challenging. The author would also like to thank the senior students, too numerous to be listed, who helped with data collection. Dr. Paul Rist and Dr. Chris Cebra also participated in my thesis committee and provided constructive criticism during the course of the study. Dr. Donna Champeau kindly accepted to serve as Graduate Council Representative. Dr. Randolph P. Martin and Dr. Andreas Kalogeropoulos at Emory University Hospital shared with me their experience and perplexities with the technique object of this investigation. Statistical assistance was provided by Dr. Roby Joehanes, Department of Statistics, and Dr. Ronette Gehring, Department of Clinical Sciences, both at Kansas State University. Dr. Barret Bulmer was instrumental in planning and conducting the study and was always willing to provide help and assistance. I feel particularly fortunate for the opportunity of working with him. My deepest expression of appreciation goes to my mentor Dr. David Sisson, who accepted me (twice) into his program, helped me find my way in the “New World”, continuously offered encouragement and advice, and shared with me his knowledge and love for science, decorated with pearls of surfer wisdom. And, above all, the final thank-you goes to my wife Patrizia, who always supported my dreams and contributed making them come true. TABLE OF CONTENTS Page Introduction ...................................................................................................... 1 Literature review............................................................................................... 3 Motion versus deformation imaging .............................................................. 3 Review of M-mode and 2D-based echocardiographic techniques used to evaluate ventricular function ......................................................................... 3 Tissue Velocity Imaging (Motion Imaging) and its natural evolution: Deformation Imaging .................................................................................... 6 The physical concepts of Strain and Strain Rate ........................................ 10 Strain and Strain Rate by ultrasonography: Strain Rate Imaging (SRI) ...... 13 Technical limitations of SRI ........................................................................ 15 Technical strengths of SRI.......................................................................... 17 Current and future clinical applications of SRI ............................................ 18 Normal SRI tracings.................................................................................... 24 Doppler-derived DI in dogs ......................................................................... 24 Aims of the Project ......................................................................................... 33 Materials and methods ................................................................................... 34 Study 1 - Invasive indirect validation of Doppler-derived Strain Rate imaging in anesthetized healthy adult dogs.............................................................. 34 Hypothesis .............................................................................................. 34 Inclusion criteria and study protocol ........................................................ 34 Statistical methods .................................................................................. 39 Study 2 – Deformation Imaging in normal adult dogs ................................. 39 Hypotheses ............................................................................................. 40 Inclusion criteria and study protocol ........................................................ 41 Estimation of the intra-operator variability ............................................... 42 Estimation of the inter-operator variability ............................................... 42 Statistical methods .................................................................................. 42 TABLE OF CONTENTS (Continued) Page Results ........................................................................................................... 46 Study 1 ....................................................................................................... 46 Study 2 ....................................................................................................... 62 Discussion...................................................................................................... 98 Study 1 ....................................................................................................... 98 Study 2 ..................................................................................................... 103 Conclusion ................................................................................................... 112 Bibliography ................................................................................................. 114 LIST OF FIGURES Figure Page 1: Comparison between single- and bi-plane methods for the estimation of left ventricular volumes ................................................................................. 25 2: The Doppler principle: stationary target...................................................... 26 3: The Doppler principle: target in relative motion .......................................... 26 4: Velocity/amplitude relationship of backscatters from blood and tissues ..... 27 5: Example of one-dimensional S................................................................... 27 6: The four components of bidimensional S ................................................... 28 7: Relationships between Cartesian axes and cardiac longitudinal (L), radial (R) and circumferential (C) axes ............................................................. 28 8: Schematic of Doppler-derived Strain Rate Imaging.................................... 29 9: Short axis view showing radial (R) and circumferential (C) axes................ 29 10: Long axis view showing the longitudinal (L) axis ...................................... 30 11: The cosine function .................................................................................. 30 12: Comparison between TVI and SRI with respect to the effects of translation of the whole heart.................................................................................... 31 13: Schematic representation of the reciprocating pump principle, with emphasis on the systolic phase .............................................................. 31 14: Normal longitudinal S (solid line) and reduced S (dashed line) as a typical example of pathologic S.......................................................................... 32 15: Normal SR (solid line) and pathologic SR (dashed line) as commonly found with ischemia................................................................................. 32 16: Schematic representation of the apical 4-chamber view .......................... 45 LIST OF FIGURES (Continued) Figure Page 17: Results of a repeated measure ANOVA on the variable RR between the 5 stages of the study .................................................................................. 49 18: Results of a repeated measure ANOVA on the variable FS between the 5 stages of the study .................................................................................. 50 19: Results of a repeated measure ANOVA on the variable CO during the 3 pharmacologic manipulations.................................................................. 50 20: Results of a repeated measure ANOVA on the variable SV during the 3 pharmacologic manipulations.................................................................. 51 21: Results of a repeated measure ANOVA on the variable +dP/dtmax during the 3 pharmacologic manipulations......................................................... 51 22: Results of a repeated measure ANOVA on the variable LVEDP during the 3 pharmacologic manipulations............................................................... 52 23: Results of a repeated measure ANOVA on the variable mean RAP during the 3 pharmacologic manipulations......................................................... 52 24: Results of a repeated measure ANOVA on the variable SVR during the 3 pharmacologic manipulations.................................................................. 53 25: Multiple comparison test on the variable PVR between the 3 pharmacologic manipulations.................................................................. 53 26: Multiple comparison test on the variable -dP/dtmax between the 3 pharmacologic manipulations.................................................................. 54 27: Multiple comparison test on the variable mean FA pressure between the 3 pharmacologic manipulation ................................................................... 54 28: Multiple comparison test on the variable PCWP between the 3 pharmacologic manipulations.................................................................. 55 29: Result of a linear regression analysis with Pearson correlation test, between LiDCO® and Thermodilution techniques ................................... 55 LIST OF FIGURES (Continued) Figure Page 30: Result of a linear regression analysis with Pearson correlation test, between 2D-FS and +dP/dtmax ................................................................ 56 31: Results of a repeated measure ANOVA comparing the SSR values between the 6 ROIs ................................................................................ 56 32: Results of a repeated measure ANOVA comparing the avSSR during the five phases of the study .......................................................................... 57 33: Result of a linear regression analysis with Pearson correlation test, between 2D-FS and avSSR .................................................................... 57 34: Result of a linear regression analysis with Pearson correlation test, between SSR and +dP/dtmax ................................................................... 58 35: Result of a linear regression analysis with Pearson correlation test, between SSR measured at ROI 1 and +dP/dtmax .................................... 58 36: Result of a linear regression analysis with Pearson correlation test, between SSR measured at ROI 2 and +dP/dtmax .................................... 59 37: Result of a linear regression analysis with Pearson correlation test, between SSR measured at ROI 3 and +dP/dtmax .................................... 59 38: Result of a linear regression analysis with Pearson correlation test, between SSR measured at ROI 5 and +dP/dtmax .................................... 60 39: Result of a linear regression analysis with Pearson correlation test, between SSR measured at ROI 6 and +dP/dtmax .................................... 60 40: Result of a linear regression analysis with Pearson correlation test, between SSR measured at ROI 4 and +dP/dtmax .................................... 61 41: Sex distribution in the four study groups .................................................. 71 42: Age distribution in the four study groups .................................................. 71 43: BW distribution in the four study groups................................................... 72 LIST OF FIGURES (Continued) Figure Page 44: Distribution of plot quality scores in the four study groups ....................... 72 45: Distribution of the DI variable SSR in the six ROIs................................... 73 46: Distribution of the DI variable S in the six ROIs........................................ 74 47: Distribution of the DI variable SRE in the 6 ROIs ..................................... 75 48: Distribution of the DI variable SRA in the 6 ROIs ..................................... 75 49: Distribution of the DI variable SSR in the 6 ROIs in group 1 .................... 76 50: Distribution of the DI variable SSR in the 6 ROIs in group 2 .................... 76 51: Distribution of the DI variable SSR in the 6 ROIs in group 3 .................... 77 52: Distribution of the DI variable SSR in the 6 ROIs in group 4 .................... 77 53: Distribution of the HR values in the four study groups.............................. 78 54: Distribution of the HR values during the two echocardiographic examinations performed by the same operator ....................................... 78 55: Distribution of the HR values during the two echocardiographic examinations performed by the two different operators .......................... 79 56: Distribution of the BP values in the 4 study groups .................................. 79 57: Comparison between a BW-matched subgroup 3 and group 4................ 80 58: Comparison between the EF values in the BW-matched subgroup 3 and group 4.................................................................................................... 80 59: Comparison between the avSSR values in the BW-matched subgroup 3 and group 4 ............................................................................................. 81 LIST OF FIGURES (Continued) Figure Page 60: Comparison between the avS values in the BW-matched subgroup 3 and group 4.................................................................................................... 81 61: Comparison between the avSSR values in the three BW groups ............ 82 62: Same analysis as in Figure 36, excluding dogs from group 4 .................. 82 63: Comparison between the FS values in the three BW groups ................... 83 64: Comparison between the EF values in the three BW groups ................... 83 65: Simple linear regression analysis between avSSR and BW..................... 84 66: Simple linear regression analysis between avS and BW.......................... 84 67: Simple linear regression analysis between avSSR and FS...................... 85 68: Simple linear regression analysis between avS and FS........................... 85 69: Simple linear regression analysis between avSSR and EF...................... 86 70: Simple linear regression analysis between avS and EF........................... 86 71: Simple linear regression analysis between avSSR and HR ..................... 87 72: Simple linear regression analysis between avS and HR .......................... 87 73: Bland-Altman plots of the repeatability sub-analysis for avSSR............... 88 74: Bland-Altman plots of the repeatability sub-analysis for avSRE............... 89 75: Bland-Altman plots of the repeatability sub-analysis for avSRA............... 90 76: Bland-Altman plots of the repeatability sub-analysis for avS.................... 91 77: Bland-Altman plots of the reproducibility sub-analysis for avSSR ............ 93 78: Bland-Altman plots of the reproducibility sub-analysis for avSRE ............ 94 LIST OF FIGURES (Continued) Figure Page 79: Bland-Altman plots of the reproducibility sub-analysis for avSRA ............ 95 80: Bland-Altman plots of the reproducibility subanalysis for avS .................. 96 LIST OF TABLES Table Page 1: Imaging views and modalities utilized in the echocardiographic acquisition protocol ................................................................................................... 44 2: Imaging views and modalities utilized in the echocardiographic off-line analysis ................................................................................................... 45 3: Summary table indicating the most important hemodynamic changes obtained during the pharmacologic manipulations .................................. 49 4: Descriptive statistics of the 49 dogs included in the final analyses ............ 69 5: DI parameters from the six ROIs (Mean values) ........................................ 70 6: DI parameters as average of the six ROIs ................................................. 70 7: Results of a Dunn’s Multiple Comparison Test for the variable SSR, between the 6 ROIs ................................................................................ 73 8: Results of a Dunn’s Multiple Comparison Test for the variable S, between the 6 ROIs............................................................................................... 74 9: Results of a Bland-Altman analysis of the data from the repeatability subanalysis ............................................................................................. 92 10: Results of a Bland-Altman analysis of the data from the reproducibility subanalysis ............................................................................................. 97 LIST OF ABBREVIATIONS +dP/dtmax: Maximum rate of pressure rise -dP/dtmax: Maximum rate of pressure decay 2D imaging: two-dimensional imaging 2D-SRI: Two-Dimensional Strain Rate Imaging 4CH: Four-chamber view 5CH: Five-Chamber view A wave: Late diastolic filling wave AV plane: Atrio-ventricular plane AVC: Aortic Valve Closure AVO: Aortic Valve Opening avS: Average Strain avSRA: Average SRA avSRE: Average SRE avSSR: Average SSR BSA: Body Surface Area BW: Body Weight C.I.: Confidence Intervals CO: Cardiac Output CP: Constrictive Pericarditis CRI: Constant Rate Infusion LIST OF ABBREVIATIONS (Continued) CRT: Cardiac Resynchronization Therapy CV: Coefficient of Variability CW: Continuous Wave Doppler DCM: Dilated Cardiomyopathy DI: Deformation Imaging DICOM: Digital Imaging and Communications in Medicine DP: Doberman pinscher E wave: Early diastolic filling wave E’: TVI Early diastolic filling wave EDV: End Diastolic Volume EF: Ejection Fraction ESV: End Systolic Volume FA: Femoral Artery fe= Emitted frequency fr= Reflected frequency fps: Frames Per Second FS: Fractional Shortening HCM: Hypertrophic Cardiomyopathy HR: Heart Rate IV: Intravenous injection LIST OF ABBREVIATIONS (Continued) IVC: Isovolumetric Contraction IVR: Isovolumetric Relaxation KS test: Kolmogorov-Smirnov test LA: Left Atrium LiDCO©: Lithium Dilution Cardiac Output LV: Left Ventricle LVDd: Left Ventricular end-diastolic Diameter LVEDP: Left Ventricular end-diastolic Pressure LVDs: Left Ventricular end-systolic Diameter LVOT: Left Ventricular Outflow Tract LVSP: Left Ventricular end-systolic Pressure MRI: Magnetic Resonance Imaging MVC: Mitral Valve Closure MVG: Myocardial Velocity Gradient MVO: Mitral Valve opening NIBP: Non Invasive Blood Pressure PA: Pulmonary Artery PCWP: Pulmonary Capillary Wedge Pressure PSS: Post Systolic Shortening PVR: Pulmonary Vascular Resistance LIST OF ABBREVIATIONS (Continued) PW: Pulsed Wave Doppler RA: Right Atrium RCM: Restrictive Cardiomyopathy R&R analysis: Repeatability and Reproducibility analysis ROI: Region of Interest RR Interval: R wave to R wave Interval RV: Right Ventricle S: Strain SC: Subcutaneous injection SD: Standard Deviation SSR: peak Systolic Strain Rate SR: Strain Rate SRA: Strain Rate late diastolic wave SRE: Strain Rate early diastolic wave SRI: Strain Rate Imaging SV: Stroke Volume SVR: Systemic Vascular Resistance TD: Thermodilution TMF: Trans Mitral Flow TSI: Tissue Synchronization Imaging LIST OF ABBREVIATIONS (Continued) TT: Tissue Tracking TVI: Tissue Velocity Imaging Introduction Assessment of regional and global myocardial function, during both systole and diastole, is essential for the evaluation of patients suspect for heart disease. Such evaluations are important in the diagnosis and management of patients with most forms of heart disease including coronary atherosclerosis, myocardial and valvular heart diseases, and most of the common congenital cardiac disorders. With the introduction of cardiac ultrasonography into routine clinical practice, such evaluations can, for the first time, be accomplished non-invasively and at low cost without the need for sedation or anesthesia. Since the initial introduction of echocardiography to clinical practice, a variety of different imaging techniques, including M-Mode echocardiography, real-time two-dimensional (2D) imaging, and blood velocity (Doppler) imaging has been developed to improve the assessment of cardiac function. While many of these techniques have been extensively studied and embraced by both medical and veterinary cardiologists, other methodologies have not enjoyed such widespread acceptance despite some apparent advantages over traditional imaging. Tissue velocity imaging (TVI), although better established in the human cardiology, is not yet widely available in veterinary practice; and deformation imaging (DI), also referred to as strain rate imaging (SRI), has received even less attention from the veterinary medical community. Deformation imaging was developed to display and 2 quantify the phenomenon of physical deformation of an object, in particular the changes in shape of myocardium. This term is used to differentiate this modality from other motion imaging techniques, such as spectral Doppler, color-Doppler and tissue velocity imaging (TVI). The overall objective of the research undertaken in this thesis was to investigate the accuracy and utility of Doppler-derived deformation imaging to evaluate myocardial function in dogs. 3 Literature review Motion versus deformation imaging Of the various imaging modalities that are currently available for the study of myocardial dynamics, an important distinction exists between motion imaging and deformation imaging. Both techniques can be based on TVI technology, which is able to estimate and display the velocity of a target, relative to the imaging probe. In motion imaging, the relative velocities of the interrogated object are displayed and post-processed without further calculations. With Deformation Imaging, the relative velocities of neighboring areas within the target are compared to each other, allowing detection and quantification of a regional velocity gradient. The presence of a velocity gradient between different areas of an object indicates that a change in shape (i.e. deformation) is taking place. In turn, the term deformation implies that different interrogated areas are characterized by a different velocity relative to a common point. Review of M-mode and 2D-based echocardiographic techniques used to evaluate ventricular function The non-invasive study of left and right ventricular function is based on a series of assumptions that allow the adoption of simplified models, but, of course, decrease the reliability of our estimates. Among the different techniques, the most commonly adopted parameter of systolic performance is 4 Fractional Shortening (FS%). It represents a linear measurement of ventricular systolic function, defined as: (1) FS = LVDd − LVDs % LVDd Where LVDd is the end-diastolic diameter and LVDs is the end-systolic diameter of the left ventricle. The limitations of this functional index are that it only estimates the contraction along the short axis (i.e. radial and circumferential shortening) and only at a specific region of the left ventricle (standard sampling is performed at the level of the chordae tendineae). For example, it does not accurately reflect global chamber function in the presence of dyskinesia or focal hypokinesia. Another commonly used index of left ventricular function is the ejection fraction (EF%). This parameter represents an attempt to investigate simultaneously the behavior of the radial, circumferential and longitudinal components of the left ventricle. It is calculated from estimates of left ventricular volume at endsystole and end-diastole. A variety of different algorithms can be used to estimate the volume of the ventricle from echocardiographic images.(1) Among them, the modified Simpson’s rule, also known as the method of the discs, treats the LV as a stack of discs. In the formula, the LV volume is obtained by summation of the volumes of a number (usually 20) of equal cylinders whose areas are determined from estimated diameters of the LV from two orthogonal long-axis views and whose lengths are 1/20 of the long axis of the LV. Another commonly adopted method is the single plane area-length method. Usually 5 applied from the apical two-chamber view, it can also be applied to a right parasternal long axis four chamber view. When this method is utilized, the area and the length of the long axis of the left ventricle are measured, and the length of the short axis of the left ventricle is calculated (estimated) from these data, on the assumption that the left ventricle is a spheroid. Figure 1 shows a comparison between the two methods. Once the chamber volumes are estimated, the EF% can be calculated as follows: (2) EF = EDV − ESV % EDV Where EDV represents the end-diastolic volume and ESV represents the end-systolic volume of the left ventricle. Among the major limitations of these methods are the already mentioned geometric assumptions that might not be fulfilled in the presence of moderateto-severe cardiac diseases associated with substantial remodeling. Furthermore these 2D-based techniques rely on the accurate detection of the endocardial borders to obtain accurate estimates of the chamber diameters. Alternatively, tissue velocity (TVI) and strain rate imaging (SRI) can provide measurements of ventricular function that are independent of geometric assumptions and which do not require endocardial tracing. 6 Tissue Velocity Imaging (Motion Imaging) and its natural evolution: Deformation Imaging Myocardial velocities can be estimated by ultrasound-based techniques derived from the phenomenon of the Doppler shift as first described in the nineteenth century by Christian Andreas Doppler (1803-1853). The Doppler phenomenon can be simply described as the change in frequency (or wavelength) of a wave that is perceived by an observer in relative motion compared to the interrogated object. Spectral Doppler and tissue Velocity Imaging are techniques based on the concept of Doppler shift. When ultrasound waves are reflected by an object that is not moving compared to the detector (probe), the reflected frequency (fr) equals the emitted frequency (fe) as shown in Figure 2. In contrast, if the object is in relative motion compared to the probe (Figure 3), the reflected frequency differs compared to the emitted frequency and the difference between these two quantities is the Doppler shift (Df), as predicted by the Doppler equation: (3) Df = 2 × f e × v × cos α c Where fe is the transmitted frequency, v is the relative velocity of the object compared to the probe, α is the angle between the ultrasound beam and the trajectory of the object, and c is the speed of sound in the medium (the average speed of sound in body tissues is 1540 m/s). 7 Equation (4) shows the Doppler equation solved for v: (4) V= Df × c 2 × f e × cos α Applying this equation, the velocity of an object, relative to the probe, can be estimated by means of Doppler ultrasonography. The Doppler principle has been extensively applied to detect, quantify and visualize the motion of blood through normal and pathologic cardiovascular structures. Approximately 20 years ago Isaaz et al.(2) published the first report on the use of pulsed and color Doppler for the measurement of velocities of solid structures. By inverting the filter settings for blood flow Doppler, so that the low-velocity, high-amplitude signals from solid structures were now selectively displayed instead of the high-velocity, low-amplitude signals originating from the red blood cells (Figure 4), it was possible to detect and visualize direction and velocity of motion of the myocardium. Over the last decade, tissue velocity imaging modalities have been improved and optimized, so that velocities calculated from a desired region of interest (ROI) of the myocardium can be displayed either as spectral Doppler graphs (velocity versus time) or as colorcoded velocity maps overlaying the real time two dimensional images. As importantly, the validity of TVI has been established in vitro and in vivo, by comparison with sonomicrometry.(3) Moreover, TVI has been shown to provide clinically useful measures of systolic and diastolic function, providing a more 8 complete non-invasive evaluation than can be achieved by the isolated application of more traditional echocardiographic imaging techniques. TVI has certain desirable attributes that make it particularly useful in clinical practice. In contrast to traditional grey-scale imaging, which is reliant on the amplitude of reflected waves to construct an interpretable image, TVI relies on the detection of Doppler-shifts, permitting the acquisition of useful data from areas of the myocardium that may not provide satisfactory grey-scale information.(4) For the study of systolic function, TVI has certain advantages over other techniques, such as two-dimensional imaging, because it is not reliant on boundary detection. For the study of diastolic function, TVI provides functional measures that are less flow-dependent than blood flow-derived Doppler indices.(5,6,7) In addition, the time resolution of myocardial velocity events is superior to blood velocity events providing an important advantage for evaluating diastolic function. In some instances, TVI data may complement blood velocity data, as demonstrated by the calculation of the E/E’ ratio that shows a high correlation with the mean left atrial pressure.(8) This ratio allows a quick and non-invasive estimate of the filling pressures of the left heart that is particularly useful in the diagnosis of left sided congestive heart failure. There are important limitations inherent to TVI techniques, which must be appreciated. Inasmuch as TVI detects relative velocity, that is motion of the ROI with respect to the probe, it is subject to certain unavoidable errors. Tissue velocities measured by TVI can be influenced by translational motion, 9 either the result of the movement of the heart during the cardiac cycle or the result of voluntary or respiratory movements. These translational velocities will add or subtract to the inherent velocity of the myocardium, resulting in falsely elevated or reduced myocardial velocities, or in an exaggerated beat-to-beat variability. Another limitation of TVI is its inability to differentiate between “tethering”, which represents passive motion of a portion of myocardium that is pulled or pushed by adjacent muscle, and active motion. This limitation is particularly significant in the evaluation of focal dyskinesia or hypocontractile states. In order to overcome these limitations, researchers at the Norwegian University of Science and Technology have worked to develop an imaging technique based on a different concept. Instead of detecting and visualizing relative velocities, these investigators endeavored to develop a technology to detect changes in shape, or deformation; hence the term deformation imaging (DI). Soon after the introduction of TVI, Doppler M-mode and color Doppler studies revealed the existence of differences in velocities across the thickness of the left ventricular wall.(9) The systematic evaluation of these myocardial velocity gradients (MVG), eventually led to the idea of studying myocardial deformation by manipulating data obtained from TVI studies. Subsequent technical improvements allowed the quantification of myocardial deformation, at first as an off-line elaboration of raw TVI data with the use of specific software, and more recently in real time as part of the software capabilities of advanced ultrasound units. In this regard, DI represents an evolution of TVI. 10 The DI application does not require specialized hardware but is based on the analysis, by dedicated software, of raw TVI data. The application of this specific software to TVI velocity data permits the nearly instantaneous calculation of estimates of strain (S) and strain rate (SR). Useful DI studies require high frame rate TVI imaging and high computational power. The physical concepts of Strain and Strain Rate In solid-state physics, linear S (one-dimensional S) is defined as the change in length (Δl) of an object relative to its original length (l0), produced by the application of a stress (force per unit cross-sectional area). This corresponds to the so-called Lagrangian S, as defined by the Lagrangian equation (5). (5) ε= l − lo Δl = lo lo Where ε is strain (S), l0 = baseline length, l is the instantaneous length at the time of the measurement (Figure 5). In practice, it is not possible to measure l0 as “unstressed” length, because some degree of “stress” is constantly applied to myocardial fibers during the whole cardiac cycle. Hence the concept of “unstressed-based” S is not applicable to a clinical setting. In the beating heart l0 is approximated by the end-diastolic length, so that deformation is detected from end diastole to end systole. S is a dimensionless ratio, and is most commonly expressed in percent (S%). Importantly, S can be measured in all three spatial dimensions 11 (normal S) and, by definition, positive S is lengthening or stretching. A value of S of 10% implies a lengthening of 10% in relation to baseline length. Negative S is shortening or compression. The Lagrangian formula only describes S in one dimension. In two dimensions, S has four components: two normal strains and two shear strains (Figure 6). Shear strain is defined as relative displacement of one object border with respect to the object’s parallel border. In three dimensions S is composed of nine components: three normal strains and six shear strains. If the object is incompressible, as is the case with the myocardium, all the components of S occur simultaneously. An object is defined incompressible if the mass conserves its volume; hence it is said to follow the law of conservation of volume. Based on this law we would expect to see a balance between the different components of S: strain in one direction has to be balanced by inverse S in other normal directions. In this case the sum of S in the three dimensions is zero under the assumption that no shear S occurs: (6) εx + ε y + ε z = 0 Where ε is strain, and x, y and z are the three orthogonal Cartesian coordinates. The concept of myocardial strain, to study myocardial deformation, was introduced in the early seventies.(11) Instead of adopting the three orthogonal Cartesian coordinate system (x, y, and z) it is more practical to divide the heart into longitudinal (l), radial (r) and circumferential (c) axes as shown in Figure 6. 12 These three coordinates are perpendicular to each other; hence the same geometric relationships apply. It must be recognized that S alone is not able to provide a complete description of the pattern of deformation of an object. Inasmuch as deformation is a dynamic event, two objects may undergo the same extent of deformation at two different rates. By measuring the rate at which S occurs, this time dependent dimension of deformation can be quantified. Thus, strain rate (SR) is a measure of the change of S per time unit: (7) SR = Δε Δt Where Δε indicates change in S, and Δt represents change in time. The unit of SR is cm/s/cm or s-1. SR has the same direction as S, i.e. negative SR is associated with shortening, positive SR with lengthening. As already mentioned, Fleming et al. introduced the concept of Myocardial Velocity Gradient (MVG) in 1994.(9) It is defined as the slope of the linear regression line of myocardial velocities along the M-mode line perpendicular to the ventricular wall: (8) MVG = Vendoc. − Vepic. W = ΔV W Where W = wall thickness, Vendoc. = endocardial velocity, Vepic. = epicardial velocity. Inasmuch as SR represents the rate of change in wall thickness, it follows that: 13 (9) SR = ΔW Wd ΔW Δt ΔV ≈ = Δt W W Hence MVG is an estimate of SR, where strain per time unit is an approximation of velocity per length unit. The reason why it represents an approximation will be described in the next paragraph. Strain and Strain Rate by ultrasonography: Strain Rate Imaging (SRI) Strain and Strain Rate can be estimated non-invasively by the manipulation of TVI data (Figure 8). It is important to note that in TVI myocardial baseline “object” length (l0) is not calculated (it is an undefined entity). Instead S is calculated “by comparing instantaneous length to the length shortly (ideally infinitesimally) earlier”.(12) In fact, for small (<0.1%) instantaneous changes in length, SR can be calculated from the spatial velocity gradient as shown in equations (9) and (10). Using a TVI unit (hardware) able to achieve high frame rates, it is possible to record the velocity of two points (a and b) at a known distance (d) in the direction of the (one) ultrasound beam (Figure 8). (10) SR ~ = Va − Vb d Where Va-Vb represents the difference of instantaneous myocardial velocities of points a and b, and d represents the distance between these two points, the “offset”, often referred to as Strain Length (SL). To obtain an accurate impression of myocardial deformation, SR is routinely calculated along the radial (r), circumferential (c), and longitudinal (l) axes as 14 shown in Figures 9 and 10. By summing the SR of all frames times the sampling interval from each frame, S in each pixel can be calculated (estimated), as shown in equation (11). (11) ⎛ Δε ⎞ ∑ (SR × Δt ) = ∑ ⎜⎝ Δt × Δt ⎟⎠ = ∑ Δε = ε Where ε is S In other words, if we assume that the interval (Δt) between consecutive frames is infinitesimally short then we can obtain S by summing (i.e. integrating) instantaneous SR values, from a starting time point (t0) to an end time point (t). This physical entity is called Eulerian Strain or Natural Strain, and it provides an estimate of instantaneous deformation, as shown, in integral notation, in equation (12). t (12) ε n = ∫ SRdt Where εn represents Natural S or Eulerian S to Current technology allows the extraction of both S and SR from stored color TVI cine-loops. Most units also allow on-line acquisition of real-time S and SR color-coded images. Regional expansion corresponds to positive S and SR, and is coded in blue. It corresponds with the systolic thickening that occurs along the radial axis and the diastolic lengthening visible along the longitudinal axis. Negative S and SR are coded in yellow-red, and denote regional compression. It corresponds with diastolic thinning in the radial axis and systolic shortening in the longitudinal axis. Scanning along the circumferential 15 axis shows systolic shortening and diastolic lengthening. Off-line postprocessing is available that allows the generation of S and SR time-velocity plots, enabling the operator to position several ROIs in the desired myocardial locations. Another imaging modality that is currently available in TVI and SRI is curved M-mode color display. It is a reconstructed color M mode recording along a manually traced line. It provides an easily interpretable visual display of segmental asynchrony between different segments. Technical limitations of SRI Analogous to other Doppler-derived measurements, SRI data are only obtainable along the path of the ultrasound beam. As a result, only deformation in the direction of the ultrasound beam is recorded, while in reality deformation occurs in all directions. It must also be appreciated that errors resulting from angulation of the interrogating beam relative to the motion of the object being interrogated are inherent to the method. The relationship between the Doppler shift and the angle (α) between the ultrasound beam and the direction of motion of the object is shown in equation (3), wherein the estimated velocity is inversely proportional to cos α. Figure 11 shows the behavior of the function y = cos x . When x = π 2 (a 90 degrees angle), cos x = 0 , the detected Doppler shift becomes zero and the movement of the object cannot be studied. Not only is SRI affected by the angle dependency typical of 16 the Doppler technique, but also the problem is accentuated by the spatial components comprising S. Inasmuch as the myocardium is an incompressible material, for every component of S there is a perpendicular component that has opposite direction, due to the law of conservation of volume. Hence, with suboptimal alignment, it is possible to sample both components. In this way, the perpendicular (or transverse) component will subtract to the original component with the reduction of the value of S proportional to the cosine of the transverse angle β. As predicted by the Doppler shift equation (3) TVI velocity becomes zero at an angle of 90 degrees. However SRI is more sensitive to misalignment, giving values of zero at angles close to 45 degrees and negative values for angles wider then 45 degrees. Another important limitation of the Doppler method in general is a consequence of aliasing of the signal. When the velocity of an interrogated object exceeds the Nyquist limit, it appears to be transposed to the other end of the velocity scale (opposite direction). In SRI imaging two velocities are simultaneously sampled. If both velocities exceed the Nyquist limit, the velocity difference remains unchanged and no aliasing of SR occurs. However if only one velocity exceeds the Nyquist limit, the resultant SR will be false. In a practical setting noise is an important cause of aliasing, but in most instances both velocities are affected. SRI is seriously affected by noise because the SR is calculated as the difference between two velocities, and the total error is the sum of the errors in estimating each of these two velocities. Thus, the signal-to-noise ratio is less 17 favorable than in TVI, where velocities are calculated separately. One method of decreasing noise is to increase offset distance between the sampling points. Because noise is a random phenomenon, increasing the offset will increase the velocity difference (Va-Vb) and the distance (d) as expressed in equation (8). This will increase the signal-to-noise ratio, giving “temporal smoothing” of the SR tracings, albeit at the expense of reducing spatial resolution. Spatial resolution describes how closely two reflectors, or scattering regions, can be to one another and remain identifiable as different reflectors. As a general rule, SRI has a lower spatial resolution compared to TVI, because of the need for sampling two velocities instead of one. A 5- to 10-mm Strain Length appears to represent a reasonable trade-off between requirements of spatial resolution and low levels of noise. S appears less prone to noise because integration of SR tends to minimize the influence of noise.(13) The reliability of SRI is also highly dependent on the frame rate adopted to generate the images. High frame rate minimizes noise by increasing the number of points used to generate the time-velocity plot. Thus, the maximal obtainable frame rate should be adopted for image acquisition. Technical strengths of SRI In contrast to TVI, wherein relative velocity is calculated, SRI uses calculations of the difference between two velocities. Hence S and SR measure local myocardial lengthening and shortening rather than myocardial translation with 18 respect to the transducer (Figure 12). As shown by inspection of equations (10) and (13), translational velocities (Vt) annul each other. As a result, SRI is not affected by translational motion created by respiration, motion of the heart, motions of the patient, or involuntary motion of the transducer. (13) SR = Va ± Vt − (Vb ± Vt ) Va − Vb = d d Where: ± Vt − (± Vt ) = 0 Translational movement of the ROI is also important when a portion of myocardium is non-actively contracting. In this scenario the akinetic area is passively dragged by neighboring myocardium. This phenomenon is referred to as “tethering”. For the same reason that SRI is not sensitive to translational motion, it is also resistant to tethering. In fact, the velocity due to tethering can be considered as a translational velocity (Vt). Hence SRI is not affected by tethering and is able to reliably identify areas of myocardium that are not actively participating to the systolic or diastolic function of the heart, but that are being passively dragged by normal neighboring myocardium. Current and future clinical applications of SRI Myocardial S and SR imaging has been validated in vitro using compressed gelatin phantoms(14,15) and in vivo using sonomicrometry(16), pressure-volume loops(17), and MRI(18) as gold standards. It has been shown that S correlates with fiber shortening and SR correlates with the velocity of fiber shortening, which is a measure of intrinsic myocardial contractility. The technical 19 superiority of SRI over TVI for tracking local systolic and diastolic function has been demonstrated by several independent investigators, mainly because SRI is resistant to translation and tethering.(19,20,21,22) Cardiac contraction is the product of the mechanical properties of a complex myocardial fiber architecture in which three major fiber orientations have been identified: longitudinal, radial and spiral. Primitive and inappropriate investigative models suggested that systole is mainly the result of an inward squeezing motion and this false impression has, unfortunately, persisted for decades. In fact, the longitudinal motion of the heart appears to be the dominating mechanical event that drives the cardiac pump function.(23,24) The concept that the heart functions as a double pump, with the atrioventricular (AV) plane acting as a piston, dates back to Leonardo da Vinci (1452-1519). There is a wealth of theoretical and experimental evidence supporting the assertion that an important component of the systolic and diastolic excursion of the heart is in the longitudinal plane. In this model the cardiac apex and the outer ventricular contour remain relatively stationary and the AV plane shows a wide range of motion. If the heart pumped only by inward squeezing, significantly reducing its outer contour, this would be extremely unfavorable from the energetic point of view. In this scenario, the myocardium would have to win the inertia of the surrounding tissues both during systole and during diastole. Experimental studies, performed as early as 1932 suggested that the heart worked mainly by movement of the heart base (AV plane) toward the apex in systole, and 20 away from the apex in diastole, while the apex itself remained almost stationary and the outer contour of the heart relatively constant.(23) This hypothesis is referred to as the principle of the reciprocating pump, and was subsequently confirmed by Hoffman and Ritmann in CT studies in dogs in 1985, in which they demonstrated a stationary apex, relatively constant outer contour and motion of the AV plane.(24) Figure 13 shows the motion of the AV plane towards the apex during systole: minimal reduction of the outer contour associated with substantial translation of the AV plane, accounting for a significant percentage of the generated stroke volume (SV). The opposite occurs during diastole. The important excursion of the AV plane is easily appreciable with real time 2D imaging from the apical view. In 1967, Harvey Feigenbaum first suggested that the estimation of the excursion of the AV plane, performed by M-mode imaging, provided an index of left ventricular systolic function.(25) With modern echocardiographs, the excursion of the mitral valve annulus (located on the AV plane) can be studied by TVI and several independent groups have validated the use of this technique for the assessment of global ventricular function.(26,27) In one notable clinical study, the peak mitral annular descent velocity from the apical 4-chamber view correlated most closely, as an individual index, with the radionuclide ventriculographic LV ejection fraction (r=0.85).(28) Such studies confirm that the longitudinal motion of the myocardium and cardiac structures most closely reflects the pump function of the heart as an organ. 21 Based on its ability to discriminate between passive and active deformation/motion, SRI, is a particularly promising tool for the study of myocardial dynamics. One of the most important differences between myocardial velocities and myocardial velocity gradients (i.e. SR), refers to the pattern of distribution of these physical entities along the ventricular wall. Compared with the apex-to-base gradient of tissue velocities, longitudinal SR is more homogeneously distributed.(29) In fact, the longitudinal velocities decrease from base to apex.(30) However S and SR do not significantly change along the ventricular wall.(31) This proves that the longitudinal tissue velocity gradient is not the result of local differences in tissue velocities, as demonstrated by the absence of a longitudinal SR gradient. Rather, it appears to be a function of the greater motion of the whole heart at the base, compared with the mid and apical regions. This is an example of how SRI might represent a powerful tool to study the mechanical properties of the myocardium, both in normal and abnormal hearts. In 2001 Jamal et al. demonstrated that peak systolic SR, but not S, was linearly related to global measures of LV contractility.(32) One of the most important areas of application of SRI is the diagnosis and management of ischemic heart disease. Such disorders are characterized by variable degrees of systolic and diastolic impairment, which are most often focal in nature and SRI appears particularly well suited to the study of such changes. Progressive delay and reduced amplitude in longitudinal systolic shortening (S and SR) 22 occur early during myocardial ischemia. At the same time the physiologic uniformity of longitudinal distribution of S and SR is lost.(33) Peak systolic S and SR decrease and tend to shift towards end-systole or early diastole, i.e. beyond aortic valve closure (AVC). This finding, called post-systolic shortening (PSS) or post-systolic thickening, appears as a high and abnormal SR during the isovolumetric relaxation period (IVR). It has been suggested that this observation represents a relatively sensitive marker of ischemia.(33) Unfortunately, specificity is reportedly not high because similar changes can be detected in a substantial population of normal patients. To increase the specificity of this finding, Jamal et al. used the ratio of PSS to maximal segmental deformation, and found that it was the best quantitative parameter to identify stress-induced ischemia as an objective marker of ischemia during dobutamine stress echocardiography in a porcine model.(32) Complete transmural infarctions do not exhibit appreciable S or SR, either at rest or during dobutamine stimulation. This aptly demonstrates the superiority of SRI to TVI, as the former is being able to differentiate between passive and active deformation.(34) SRI was also investigated in an experimental model of altered myocardial bioenergetics in which myofibrillar creatine kinase and glyceraldehyde dehydrogenase were inhibited by iodoacetamide.(35) The SRI findings were similar to acute ischemia and infarction. TVI and SRI have also been investigated in patients affected by congenital and acquired nonischemic cardiomyopathies. Several studies showed that SRI has the potential 23 of detecting early changes occurring in the subclinical phase of the disease (the so-called “occult” phase). In a transgenic murine model of human hypertrophic cardiomyopathy (HCM), TVI was able to detect early diastolic and systolic abnormality, before an appreciable hypertrophy was visible.(36) The same author obtained equivalent results in a group of clinical patients.(37) Early evidence of impaired systolic and diastolic function has been demonstrated by means of SRI in patients affected by Friedreich’s ataxia with normal LV volumes and preserved EF.(38) Reduced peak systolic radial SR was observed in patients with normal EF, undergoing anthracycline therapy.(39) Therefore SRI might represent a sensitive tool in the early recognition of myocardial toxicity in veterinary patients treated with doxorubicin. SRI might also prove a valuable aid in differentiating restrictive cardiomyopathy (RCM) versus constrictive pericarditis (CP). Systolic SR during ventricular ejection and rapid (early) diastolic filling were lower in RCM compared with CP.(40) In particular, SR during IVR was positive in RCM patients, and negative in patients affected by CP, while early diastolic SR was low in RCM compared with CP and normal controls. Furthermore, SRI appears able to differentiate between primary and secondary concentric hypertrophy. In fact, systolic myocardial SR values were significantly lower in patients affected by HCM, compared with athletes, hypertensive patients and normal controls.(41) 24 Normal SRI tracings Figure 14 shows a normal longitudinal S tracing (solid line) and an example of reduced S (dashed line). Figure 15 shows a normal longitudinal SR tracing (solid line) and an example of SR associated with ischemia (dashed line) showing reduced amplitude systolic SR and PSS during IVR. E and A waves represent early and late diastolic filling. In normal human patients longitudinal S and SR values are lower in the left ventricle (LV) compared to the right ventricle (RV) or compared to radial deformations. In fact radial SR is approximately twofold higher than longitudinal SR.(42) A transmural gradient exists in normal myocardium, with higher SR occurring in the subendocardium. Doppler-derived DI in dogs Doppler-derived DI has been evaluated by a French study group in 2006.(43) The study consisted in an assessment of the intra-operator variability conducted on 6 healthy Beagle dogs, followed by the assessment of normal values in a population of 30 adult healthy dogs from different breeds. The conclusions of the authors were that Doppler-derived DI provides reasonably acceptable intra-operator variability. G. Wess presented an abstract at the 16th ECVIM-CA Congress (2006) where he evaluated Doppler-derived DI in a population of 42 healthy adult Doberman pinscher dogs.(44) Normal ranges for longitudinal Strain and Strain Rate were reported in this abstract. 25 Figure 1: Comparison between single- and bi-plane methods for the estimation of left ventricular volumes 26 fe V=0 fr=fe Figure 2: The Doppler principle: stationary target fe V°0 fr ° fe Figure 3: The Doppler principle: target in relative motion α 27 Tissue Amplitude Blood Velocity Figure 4: Velocity/amplitude relationship of backscatters from blood and tissues l0 l Figure 5: Example of one-dimensional S 28 y y x x x x y y y y x x Figure 6: The four components of bidimensional S y r c l x z Figure 7: Relationships between Cartesian axes and cardiac longitudinal (L), radial (R) and circumferential (C) axes 29 Va d Vb Figure 8: Schematic of Doppler-derived Strain Rate Imaging c r Figure 9: Short axis view showing radial (R) and circumferential (C) axes 30 l l Figure 10: Long axis view showing the longitudinal (L) axis Figure 11: The cosine function 31 TVI SRI Va Vt d Vb Figure 12: Comparison between TVI and SRI with respect to the effects of translation of the whole heart Figure 13: Schematic representation of the reciprocating pump principle, with emphasis on the systolic phase 32 Strain(%) 0 % Figure 14: Normal longitudinal S (solid line) and reduced S (dashed line) as a typical example of pathologic S Strain Rate E A 0 s-1 AVO S IVR AVC Figure 15: Normal SR (solid line) and pathologic SR (dashed line) as commonly found with ischemia 33 Aims of the Project Deformation Imaging might represent an interesting addition to the currently available techniques for the diagnosis and management of both congenital and acquired cardiovascular diseases in veterinary patients. At the same time it will surely enrich our knowledge on the dynamics of diastolic and systolic function in normal patients. The techniques described in the preceding paragraphs are currently available at our Institution and our group has already gained a decent level of basic practical experience. This Master’s Degree thesis is structured into two studies: Study 1 - Invasive indirect validation of Doppler-derived Strain Rate Imaging in anesthetized healthy adult dogs: will correlate DI with invasive techniques in the assessment of global systolic function in normal anesthetized dogs undergoing pharmacologic manipulations. Study 2 - Deformation Imaging in normal adult dogs: will provide normal DI values in normal non-sedated dogs and will also allow the analysis of the intraoperator (repeatability) and inter-operator (reproducibility) variability (R&R analysis). 34 Materials and methods Study 1 - Invasive indirect validation of Doppler-derived Strain Rate imaging in anesthetized healthy adult dogs There is clinical and experimental evidence in the medical literature that S and SR imaging accurately reflect the changes in ventricular function induced by pharmacologic interventions.(45) The aim of this study was to evaluate, in a canine model, the changes in Doppler-derived DI data during manipulations of the inotropic state and loading conditions. Hypothesis We hypothesized that S and SR imaging accurately reflect, in a loadindependent manner, the changes in the LV systolic function induced by the pharmacologic manipulation of intrinsic contractility, as documented by changes in the maximum rate of pressure rise (+dP/dtmax) obtained by analyzing hi-fidelity LV pressure tracings by means of cardiac catheterization. Inclusion criteria and study protocol Five adult clinically healthy dogs were enrolled in the study. The study protocol was approved by the Institutional Animal Care and Use Committee in compliance with the Public Health Service (PHS) Policy on the Humane Care and Use of Laboratory Animals, the US Department of Agriculture’s (USDA) 35 Animal Welfare Act & Regulations (9CFR Chapter 1, 2.31), and the United States Government Principles for the Utilization and Care of Vertebrate Animals Used in Research, Teaching and Testing. All dogs underwent a complete physical exam, a non-invasive blood pressure measurement, and a ten-lead electrocardiogram. A device based on the oscillometric method was utilized to obtain non-invasive blood pressure measurements (Cardell®, Sharn Veterinary Inc. Tampa, FL). Systemic hypertension was defined as a systolic pressure higher than 170 mmHg.(46,47) A total of five consecutive NIBP measurements were recorded, the readings with the highest and lowest mean blood pressure values were discarded, and the average of the three remaining measurements was used. An echocardiogram was acquired before sedation, based on the following protocol (Tables 1 and 2, Figure 16). A Vivid 7 Dimension Cardiovascular Ultrasound System (GE Healthcare, Milwaukee, WI, USA) with Doppler-derived SRI software was used for the acquisition of the echocardiographic data. A 3Mhz probe with octave strain imaging application was used for image acquisition. For traditional imaging modalities, a set of 7 consecutive beats was digitally stored and measurements were made as the average of 3 good quality beats. For the acquisition of DI data, two sets of 7 consecutive beats were digitally stored and measurements were made as the average of 5 good quality beats. Dedicated left apical long axis views of the left ventricular free wall and interventricular septum were obtained in order to optimize the alignment with the longitudinal myocardial fibers and to 36 reduce the sector width, so to maximize the frame rate. With this technique, a minimum frame rate of 220 fps was obtained in all the cineloops. DI data were collected with the preceding RR interval. Table 1 shows the imaging views and modalities included in the echocardiographic acquisition protocol. Measurements with the traditional echocardiographic modalities were performed as previously described.(48,49) The off-line analysis (post- processing) of the DI data was performed using the software embedded in the ultrasound unit (Vivid 7 Dimension Cardiovascular Ultrasound System, GE Healthcare, Milwaukee, WI, USA) and a dedicated workstation (EchoPAC Dimension ’06, GE Healthcare, Milwaukee, WI, USA). Oval sample volumes of 5 mm x 10 mm with Strain Length of 10 mm were used as ROIs for obtaining SR-time plots and S-time plots (Figure 16). Temporal gaussian smoothing was set at 40 ms. The Cine Compound function was disabled. Off-line analysis of DI data was performed following the protocol indicated in Table 2. Figure 16 shows positions and labeling of the 6 ROIs and displays the two narrow-sector dedicated views of the interventricular septum and left ventricular free wall, used to generate the DI plots. All the dogs were found to be free of evidence of cardiac disease and were defined normal. The dogs were pre-medicated with Diazepam (0.1 mg/kg IV) and Morphine (1 mg/kg SC). General anesthesia was induced with Thiopental (10 mg/kg IV) and maintained with 2% isoflurane in 100% oxygen. Meloxicam (0.2 mg/kg SC) was used to control surgical pain. The dogs were placed in left 37 lateral recumbency on an echocardiographic table. The right jugular vein was accessed percutaneously, using a Seldinger technique, and a 7Fr introducerdilator set (Check-Flo® Performer® Introducer set, Cook Inc. Bloomington, IN) was inserted. A 6 Fr Swan-Ganz catheter (Arrow International, Inc., Reading, PA, USA) was positioned in the main pulmonary artery to record right atrial (RA) pressure, pulmonary artery (PA) pressure, pulmonary capillary wedge pressure (PCWP) and to allow the estimation of cardiac output (CO) by thermodilution technique. The right carotid artery was surgically exposed, using the Sones technique, and a 6 Fr introducer-dilator set inserted. The left ventricle was catheterized with a 5 Fr high-fidelity microtransducer pressure catheter (Mikro-Tip®, Millar Instruments, Inc., Houston, TX, USA) connected with a physiologic monitor (Biopac® MP100WSW, Biopac System Inc., Goleta, CA, USA) to record left ventricular pressure tracings and derive +dP/dtmax and -dP/dtmax. Simultaneous quantification of cardiac output by lithium-dilution technique was also performed using a LiDCO® Plus Hemodynamic Monitor (LiDCO Ltd., Cambridge, UK). Correct positioning of the catheters was confirmed by fluoroscopy. An arterial catheter was inserted in the dorsal pedal artery, to record a peripheral arterial pressure tracing. A baseline set of echocardiographic measurements (standard echocardiography and DI), and invasive measurements were recorded at steady state, defined as stabilization of +dP/dtmax, -dP/dtmax, HR and systemic blood pressure. The invasive parameters acquired or calculated during each phase of the study were the 38 following: cardiac output by thermodilution and Lithium-dilution, stroke volume (SV), left ventricular systolic pressure (LVSP), left ventricular end-diastolic pressure (LVEDP), +dP/dtmax, -dP/dtmax, mean right atrial pressure, pulmonary capillary wedge pressure (PCWP), systemic vascular resistance (SVR), pulmonary vascular resistance (PVR), femoral artery mean pressure, pulmonary artery mean pressure. After the initial set of measurements was obtained, a sequence of three pharmacologic manipulations was performed. At first a constant rate infusion (CRI) of Dobutamine (10 µg/kg/min) was initiated, and a set of invasive and echocardiographic data was collected at steady state.(50) After discontinuation of the infusion, a wash-out period of at least 20 minutes allowed the return of the +dP/dtmax, HR, and mean blood pressure to baseline. The infusion of dobutamine was performed in order to achieve a positive inotropic effect. The second manipulation was performed starting a CRI of Nitroprusside (3.0 µg/kg/min), with the goal of reducing the loading conditions of the left ventricle, by means of inducing balanced vasodilation.(51) At steady state the same set of measurements was repeated. A wash-out period of at least 20 minutes allowed the return to baseline and a final pharmacologic manipulation was performed by means of administering a bolus of the plasma volume expander hetastarch (10 ml/kg/15 min), with the goal of increasing preload.(52) A final set of measurements was obtained at steady state. At the end of the study the right carotid artery was ligated and 39 the soft tissues sutured in the usual fashion. The dogs recovered uneventfully from anesthesia. Statistical methods Most data sets were normally distributed, as confirmed by the result of a Kolmogorov-Smirnov test (KS test) with Dallal-Wilkonson-Lilliefor p value, a D'Agostino & Pearson omnibus normality test, and a Shapiro-Wilk normality test. For the normally distributed data sets, repeated measures ANOVA with Bonferroni corrections was used to compare the hemodynamic parameters recorded at baseline (under anesthesia) with the parameters recorded during the three pharmacologic manipulations. When the assumption of normality was not fulfilled, and data transformations proved ineffective, a non-parametric repeated-measures analysis (Friedman test with Dunn’s comparisons between groups) was performed. Simple linear regression analysis was used to study the correlation between peak systolic SR and several invasive parameters, when the assumptions of normality, equal variance and linearity were met. Statistical significance was set at p<0.05. Study 2 – Deformation Imaging in normal adult dogs The aim of this study was to investigate the feasibility of DI in non-sedated dogs and to provide DI values in normal dogs divided into three groups based on body weight. A fourth group of Doberman Pinchers (DP) was also included. 40 The reason for the segregation of dogs belonging to this specific breed to a separate study group is the high prevalence of dilated cardiomyopathy (DCM), and the high number of DP dogs with borderline echocardiographic indices of systolic function. DCM in DP is characterized by a long period during which echocardiography is unable to definitely diagnose the disease, the so-called “occult phase”. In this phase arrhythmias may be present and a relatively high risk of sudden cardiac death has been documented. The study was also designed to allow the analysis of the intra-operator (repeatability) and interoperator (reproducibility) variability. Hypotheses With Study 2 we aimed at investigating the following hypotheses: 1. DI is an echocardiographic technique that is feasible, reproducible and repeatable, in a veterinary clinical setting. 2. S and SR represent parameters of ventricular function that are independent of body weight. 3. S and SR values are different in Doberman Pinchers compared to weightmatched non-Doberman controls. 4. S and SR values are uniform throughout the left ventricle in healthy adult dogs (absence of a significant apical-basal gradient). 41 Inclusion criteria and study protocol Clinically healthy adult dogs were enrolled on a voluntary basis and were divided into 4 groups. Inclusion in the first three groups was dependent on body weight (BW) (Group 1: BW < 15 kg, Group 2: BW 15 - 30 kg, Group 3: BW > 30 kg). A fourth group enrolled Doberman pinschers. An informed consent form signed by the owner was obtained in all dogs prior to the study. The study protocol was approved by the Institutional Animal Care and Use Committee in compliance with the Public Health Service (PHS) Policy on the Humane Care and Use of Laboratory Animals, the US Department of Agriculture’s (USDA) Animal Welfare Act & Regulations (9CFR Chapter 1, 2.31), and the United States Government Principles for the Utilization and Care of Vertebrate Animals Used in Research, Teaching and Testing. Dogs were considered eligible for the study if their age was between 12 months and 8 years, there was no history of cardiovascular disease, and were not on any treatment that could have affected their cardiovascular function (i.e. thyroid hormone supplementation, phenylpropanolamine, etc). All dogs underwent a complete physical exam, a non-invasive blood pressure (NIBP) measurement, and a ten-lead electrocardiogram. The normal blood pressure values for dogs are breed-specific.(46) Where appropriate, breed-specific data were adopted in the definition of normal systemic blood pressure.(46) In case data were not available for the specific breed, systemic hypertension was defined as a systolic pressure higher than 170 mmHg.(47) In dogs in which the results of 42 these preliminary studies were within normal limits, a complete echocardiographic examination was performed, following the same protocol used in study 1. Estimation of the intra-operator variability Four (about 40%) randomly selected dogs in each group underwent an echocardiographic study twice by the same operator, with an interval of at least 20 minutes between the two studies, in order to collect data on repeatability in the phase of both image acquisition and post-processing. Estimation of the inter-operator variability Four (about 40%) randomly selected dogs in each study group were examined by two operators in order to collect data to estimate an index of inter-operator variability (reproducibility) in the phase of image acquisition and postprocessing of the DI data. Statistical methods Most data were normally distributed, as confirmed by the results of a Kolmogorov-Smirnov test (KS test) with Dallal-Wilkonson-Lilliefor p value, a D'Agostino & Pearson omnibus normality test, and a Shapiro-Wilk normality test. For the normally distributed data sets, paired or unpaired t-Tests or Oneway ANOVA with Bonferroni correction were used to make comparisons 43 between various subsets of data. When the assumption of normality was not fulfilled, and transformation of data proved to be ineffective, non-parametric tests such as Mann-Whitney-Wilcoxon test or Friedman test with Dunn’s comparisons between groups were performed. Simple linear regression analysis was used to study potential correlations between DI data and other parameters, when the assumptions of normality, equal variance and linearity were met. Statistical significance was set at p<0.05. For the repeatability and reproducibility analysis, Bland and Altman plots were utilized to compare the intra- and inter-observer variability, which was quantified by using the bias (average of the differences between the two studies) and its standard deviation, from which the 95% limits of agreement were calculated. 44 Table 1: Imaging views and modalities utilized in the echocardiographic acquisition protocol R. parasternal window Short axis LV apex Papillary muscle Chordae tendineae MV Ao root Long axis 4CH (4 chamber view) LVOT L. parasternal window Apical view 4 CH view 5 CH view 2D cineloop TVI cineloop 2D cineloop TVI cineloop 2D cineloop TVI cineloop M-mode 2D cineloop TVI cineloop M-mode 2D cineloop (Ao and LA) M-mode (Ao and L auricle) Color-Doppler PV PW PV Color-Doppler TV 2D cineloop Color-Doppler MV Color-Doppler TV 2D cineloop Color LVOT 2D cineloop Color-Doppler MV PW of Trans-Mitral Flow (TMF) Flow propagation velocity (FPV) TVI cineloop PW-TVI lateral MV annulus PW-TVI medial MV annulus Color-Doppler TV PW Trans-Tricuspid Flow (TTF) PW-TVI lateral TV annulus PW-TVI medial TV annulus 2D cineloop Color-Doppler LVOT PW Ao 45 Table 2: Imaging views and modalities utilized in the echocardiographic off-line analysis L. parasternal window Apical view 4 CH view Optimized S view free wall S tracings at locations 1-2-3 Optimized SR view free wall SR tracings at locations 1-2-3 Optimized S view IV septum S tracings at locations 4-5-6 Optimized SR view IV septum SR tracings at locations 4-5-6 6 5 4 3 2 1 Figure 16: Schematic representation of the apical 4-chamber view. Numbers 1 through 6 represent the positions of the six ROIs used during the off-line analysis of DI data. The two “optimized” narrow-sector views are shown 46 Results Study 1 The results of study 1 have been previously presented as an oral abstract at the 25th Annual Forum of the American College of Veterinary Internal Medicine.(53) Five dogs were enrolled in the invasive study. There were three females and two males, with ages ranging between 2 and 7 years (mean 3.80, median 2.90). The breeds included mixed breed hound (3 dogs) and mixed breed Labrador retriever (2 dogs). Their BW ranged from 22.60 to 40.20 kilograms, with a mean BW of 28.88 kilograms and a median BW of 27.89 kilograms. Repeated measures ANOVA confirmed that the following parameters were significantly changed during at least some of the pharmacologic manipulations, compared to baseline under anesthesia (Table 3): RR interval (p<0.01, range 333.2 - 898.9 ms) (Figure 17), Fractional shortening (2D-FS) (p<0.001, range 15 - 53%) (Figure 18), cardiac output (P<0.0001, range 2.600 - 9.340 L/min) (Figure 19), stroke volume (p<0.001, range 18.92 - 45.68 ml) (Figure 20), +dP/dtmax (p=0.015, range 953.7 - 3822 mmHg/s) (Figure 21), left ventricular end diastolic pressure (p<0.0001, range 0.210 - 16.43 mmHg) (Figure 22), Mean right atrial pressure (p<0.0004, range -2.490 - 9.920 mmHg) (Figure 23), and Systemic Vascular Resistance (p<0.0001, range 510.0 - 2652 dyne*sec/cm5) (Figure 24). The following parameters did not change significantly during the pharmacologic 47 manipulations, compared to baseline under anesthesia: Pulmonary Vascular Resistance (p>0.05, range 256.4 - 1635 dyne*sec/cm5) (Figure 25), -dP/dtmax (p>00.5, range -1872.0 - -984.20 mmHg/s) (Figure 26), mean femoral artery pressure (p>0.05, range 51.77 - 101.00 mmHg) (Figure 27), and pulmonary capillary wedge pressure (p>0.05, range 0.06 - 13.59 mmHg) (Figure 28). A good correlation between thermodilution and LiDCO® techniques in estimating cardiac output was observed (p=0.0002, Pearson r=0.993) (Figure 29). The results of a repeated measure ANOVA revealed that the fractional shortening (FS) significantly increased (p<0.001, mean difference 24.8%) (Figure 18) during the dobutamine infusion and returned to baseline during nitroprusside and hetastarch administration. FS was positively correlated with +dP/dtmax (p=0.004, r squared=0.991 from a Pearson correlation test) (Figure 30). The analyses of the DI data yielded the following results. A total of 750 ROIs were included in the final analyses, 150 in each of the 5 dogs. Measurable DI curves were obtained in 741 out of 750 ROIs (98.8%). The peak systolic strain rate (SSR) values obtained from the 6 ROIs did not differ significantly from each other (p=0.072 from a Kruskal-Wallis test) (Figure 31). The average SSR (avSSR), calculated as the average value from the 6 ROIs, did not change significantly between the baseline echocardiogram before anesthesia and the steady state after induction of anesthesia (p>0.05 from a one-way analysis of variance) (Figure 32). A good correlation was found between 2D-derived FS% (2D-FS) and avSSR (p=0.040, r squared=0.922) (Figure 33). The avSSR 48 changed significantly during dobutamine infusion versus both baseline preanesthesia and baseline after induction of anesthesia (p<0.001 from a repeated measure ANOVA) (Figure 32). The variable avSSR negatively correlated with +dP/dtmax (p=0.021, r=0.979,) (Figure 34). Individual values of SSR at the level of the basal portion of the free wall (ROI 1; Figure 35) (p=0.011, r=0.989), mid portion of the free wall (ROI 2; Figure 36) (p=0.002, r=0.997), apical portion of the free wall (ROI 3; Figure 37) (p=0.011, r=0.989), mid portion of the septum (ROI 5; Figure 38) (p=0.018, r=0.981), and apical portion of the septum (ROI 6; Figure 39) (p=0.049, r=0.951) were also negatively correlated with +dP/dtmax. However, statistically significant correlation was not reached between SSR obtained at the level of the basal portion of the interventricular septum (ROI 4; Figure 40) and +dP/dtmax (p=0.170, r=0.830). 49 Table 3: Summary table indicating the most important hemodynamic changes obtained during the pharmacologic manipulations Mean±SD CO Anesthesia Dobutamine 3.11±0.40† 7.62±1.09† 29.82±4.66† 8.65±2.67†‡ Nitroprusside Hetastarch P-value 3.67±0.75 P<0.001† 60.24±10.81† 24.85±4.31 36.79±6.61 P<0.001† 1.24±3.63† 10.08±4.89 1754±291.1 P < 0.001† P < 0.01‡ P < 0.001† 1463±167.2 P < 0.001† 3.59±0.37 (L/min) SV (ml) LVEDP 3.44±3.08‡ (mmHg) SVR(dyne* 2191±426.2† 5 927.4±378.2† 1568±285.6† sec/cm ) +dP/dtmax 1546 ±375.5† 3157±464.7† 1675±432.9 (mmHg/s) RR 900 800 P < 0.01 700 P < 0.01 600 500 400 300 Baseline Anesthesia Dobutamine Nitroprusside Hetastarch Manipulations Figure 17: Results of a repeated measure ANOVA on the variable RR between the 5 stages of the study 50 2D-FS 55 50 P < 0.001 45 40 35 30 25 20 15 10 5 0 Baseline Anesthesia Dobutamine Nitroprusside Hetastarch Manipulations Figure 18: Results of a repeated measure ANOVA on the variable FS between the 5 stages of the study CO (TD) 9.5 9.0 8.5 8.0 7.5 7.0 6.5 6.0 5.5 5.0 4.5 4.0 3.5 3.0 2.5 2.0 1.5 1.0 0.5 0.0 P<0.0001 Anesthesia Dobutamine Nitroprusside Hetastarch Figure 19: Results of a repeated measure ANOVA on the variable CO during the 3 pharmacologic manipulations 51 SV 80 70 60 P < 0.001 50 40 30 20 10 0 Anesthesia Dobutamine Nitroprusside Hetastarch Manipulations Figure 20: Results of a repeated measure ANOVA on the variable SV during the 3 pharmacologic manipulations +dP/dtmax 4000 3000 P<0.0001 2000 1000 0 Anesthesia Dobutamine Nitroprusside Hetastarch Manipulations Figure 21: Results of a repeated measure ANOVA on the variable +dP/dtmax during the 3 pharmacologic manipulations 52 LVED Pressure 17 16 15 14 13 12 11 10 9 8 7 6 5 4 3 2 1 0 -1 -2 -3 P < 0.05 P < 0.01 Anesthesia Dobutamine Nitroprusside Hetastarch Manipulations Figure 22: Results of a repeated measure ANOVA on the variable LVEDP during the 3 pharmacologic manipulations Mean RA Pressure 10 9 8 7 P < 0.001 6 5 4 3 2 1 0 Anesthesia Dobutamine Nitroprusside Hetastarch Manipulations Figure 23: Results of a repeated measure ANOVA on the variable mean RAP during the 3 pharmacologic manipulations 53 SVR 2750 P > 0.05 P < 0.01 2500 2250 P < 0.001 2000 1750 1500 1250 1000 750 500 250 0 Anesthesia Dobutamine Nitroprusside Hetastarch Manipulations Figure 24: Results of a repeated measure ANOVA on the variable SVR during the 3 pharmacologic manipulations Pulmonary Vascular Resistance No post tests. P > 0.05 1700 1600 1500 1400 1300 1200 1100 1000 900 800 700 600 500 400 300 200 100 0 Anesthesia Dobutamine Nitroprusside Hetastarch Manipulations Figure 25: Multiple comparison test on the variable PVR between the 3 pharmacologic manipulations 54 -dP/dt max -750 No post tests. P > 0.05 -1000 -1250 -1500 -1750 -2000 -2250 -2500 Anesthesia Dobutamine Nitroprusside Hetastarch Manipulations Figure 26: Multiple comparison test on the variable -dP/dtmax between the 3 pharmacologic manipulations Mean FA pressure No post tests. P > 0.05 105 100 95 90 85 80 75 70 65 60 55 50 Anesthesia Dobutamine Nitroprusside Hetastarch Manipulations Figure 27: Multiple comparison test on the variable mean FA pressure between the 3 pharmacologic manipulation 55 PCWP No post tests. P > 0.05 14 13 12 11 10 9 8 7 6 5 4 3 2 1 0 -1 Baseline Dobutamine Nitroprusside Hetastarch Manipulations Figure 28: Multiple comparison test on the variable PCWP between the 3 pharmacologic manipulations P value 0.0002 Pearson r 0.9929 P value (two-tailed) 0.0071 LiDCO vs Thermodilution 8.5 8.0 7.5 7.0 6.5 6.0 5.5 5.0 4.5 4.0 3.5 3.0 2.5 2.0 1.5 1.0 0.5 0.0 0 1 2 3 4 5 6 7 8 9 10 Thermodilution (L/min) Figure 29: Result of a linear regression analysis with Pearson correlation test, between LiDCO® and Thermodilution techniques 56 FS vs +dP/dT max 3750 R squared 0.9915 Pearson r 0.9957 P value 0.0043 3500 3250 3000 2750 2500 2250 2000 1750 1500 1250 1000 750 500 250 0 0 10 20 30 40 50 60 FS % Figure 30: Result of a linear regression analysis with Pearson correlation test, between 2D-FS and +dP/dtmax SSR No post tests. P > 0.05 -0.50 -0.75 -1.00 -1.25 -1.50 -1.75 -2.00 -2.25 -2.50 -2.75 1 2 3 4 5 6 ROIs Figure 31: Results of a repeated measure ANOVA comparing the SSR values between the 6 ROIs 57 avSSR -0.50 -0.75 P > 0.05 -1.00 -1.25 -1.50 -1.75 P < 0.001 -2.00 -2.25 P < 0.001 -2.50 -2.75 -3.00 -3.25 Baseline Anesthesia Dobutamine Nitroprusside Hetastarch Manipulations Figure 32: Results of a repeated measure ANOVA comparing the avSSR during the five phases of the study FS vs SSR -0.25 R squared 0.9221 Spearman r -0.8000 -0.50 P value 0.0397 -0.75 -1.00 -1.25 -1.50 -1.75 -2.00 -2.25 -2.50 -2.75 -3.00 -3.25 -3.50 0 10 20 30 40 50 60 FS % Figure 33: Result of a linear regression analysis with Pearson correlation test, between 2D-FS and avSSR 58 avSSR vs +dP/dTmax -0.50 -0.75 r squared 0.9588 Pearson r -0.9792 P value 0.0208 -1.00 -1.25 -1.50 -1.75 -2.00 -2.25 -2.50 -2.75 -3.00 -3.25 0 250 500 750 1000 1250 1500 1750 2000 2250 2500 2750 3000 3250 3500 3750 +dP/dTmax (mmHg/s) Figure 34: Result of a linear regression analysis with Pearson correlation test, between SSR and +dP/dtmax ROI 1 -0.50 r squared 0.9778 -0.75 P value 0.0111 -1.00 -1.25 -1.50 -1.75 -2.00 -2.25 -2.50 -2.75 -3.00 -3.25 -3.50 0 500 1000 1500 2000 2500 3000 3500 4000 max +dP/dT Figure 35: Result of a linear regression analysis with Pearson correlation test, between SSR measured at ROI 1 and +dP/dtmax 59 ROI 2 -0.25 -0.50 r squared 0.9950 P value 0.0025 -0.75 -1.00 -1.25 -1.50 -1.75 -2.00 -2.25 0 500 1000 1500 2000 2500 3000 3500 4000 max +dP/dT Figure 36: Result of a linear regression analysis with Pearson correlation test, between SSR measured at ROI 2 and +dP/dtmax ROI 3 -0.25 r squared 0.9788 -0.50 P value 0.0106 -0.75 -1.00 -1.25 -1.50 -1.75 -2.00 -2.25 -2.50 -2.75 -3.00 0 500 1000 1500 2000 2500 3000 3500 4000 max +dP/dT Figure 37: Result of a linear regression analysis with Pearson correlation test, between SSR measured at ROI 3 and +dP/dtmax 60 ROI 5 -0.5 r squared 0.9634 P value 0.0185 -1.0 -1.5 -2.0 -2.5 -3.0 -3.5 -4.0 0 500 1000 1500 2000 2500 3000 3500 4000 max +dP/dT Figure 38: Result of a linear regression analysis with Pearson correlation test, between SSR measured at ROI 5 and +dP/dtmax ROI 6 0.0 -0.5 r squared 0.9051 P value 0.0486 3500 4000 -1.0 -1.5 -2.0 -2.5 -3.0 -3.5 -4.0 -4.5 0 500 1000 1500 2000 2500 3000 max +dP/dT Figure 39: Result of a linear regression analysis with Pearson correlation test, between SSR measured at ROI 6 and +dP/dtmax 61 ROI 4 0.0 r squared 0.6889 P value 0.1700 3500 4000 -0.5 -1.0 -1.5 -2.0 -2.5 -3.0 -3.5 -4.0 0 500 1000 1500 2000 2500 3000 max +dP/dT Figure 40: Result of a linear regression analysis with Pearson correlation test, between SSR measured at ROI 4 and +dP/dtmax 62 Study 2 A total of 65 dogs was initially evaluated. Nine dogs did not completely meet the inclusion criteria because of the presence of a murmur (3 dogs), systemic hypertension (1 dog), ongoing thyroid hormone supplementation (1 dog), ongoing treatment with phenylpropanolamine (1 dog), echocardiographic evidence of mild tricuspid valve dysplasia (1 dog), and echocardiographic evidence of reduced systolic function (2 dogs). The remaining 56 dogs were enrolled in the study. There were a total of 4 intact females, 6 intact males, 18 spayed females, and 21 neutered males, with ages ranging between 1 and 8 years. The breeds included American Staffordshire Terrier (1 dog), Australian shepherd (4), Beagle (1), Border collie (1), Chihuahua (1), Cocker spaniel (1), Doberman pinscher (10), French Bulldog (1), Golden retriever (2), Great Dane (2), Greyhound (1), Heeler mix (1), Italian Greyhound (1), Labrador Retriever (2), Mastiff (1), mixed breed (19), Pitbull (1), Poodle (1), Pug (2), Rhodesian Ridgeback (1), Saint Bernard (1), and Yorkshire Terrier (1). Their body weights (BW) ranged from 2.4 to 63.2 kilograms. Echocardiographic data from seven dogs were not included in the final analysis because of overall poor image quality. Table 4 shows the descriptive statistics of the 49 dogs included in the final analysis, as they were divided into the four study groups. There was a tendency toward a higher number of intact dogs in group 4 (4 intact females and 5 intact males) compared to the other groups, but it did not reach 63 statistical significance (p=0.956 from a Kruskal-Wallis test) (Figure 41). Although a tendency for dogs in group 4 to have a younger age was identified, it did not reach statistical significance either (p=0.162 from a Kruskal-Wallis test) (Figure 42). Figure 43 shows the body weight distribution of the study population. As expected, being part of the inclusion criteria, there was a statistically significant difference between groups 1, 2, and 3 (p<0.001 from an ANOVA test). There was also a significant difference (p<0.05 from an ANOVA test, mean difference -8.11 kg) between group 4 and group 3. As already mentioned, of the initial 56 dogs from which echocardiographic data were available, 7 dogs (12.5%) were excluded because of poor image quality. Reasons included poor patient cooperation (2 dogs), poor acoustic window (2 dogs), sinus tachycardia (1 dog), tachypnea (1 dog), and an operatordependent error in storing the images (1 dog). In fact, DI data can only be post-processed from Hi-Definition DICOM files (HD-DCM files); depending on the media utilized for storage and/or transfer of images, different compression algorithms can be involved, in some instances negating further analysis of DI data. The final analysis included DI data from 49 total dogs. Fourteen randomly selected dogs (28.6% of the 49 total dogs) were included in the repeatability sub-analysis, and underwent two echocardiographic studies performed by the same operator. Seventeen randomly selected dogs (34.7% of the 49 total dogs) underwent two echocardiographic exams performed by two operators, to provide data on reproducibility (interoperator variability in the 64 phase of image acquisition and off-line analysis). The quality of the DI plots was subjectively quantified by a single operator, attributing a score to each curve (i.e. heart beat) analyzed, defined as follows: 0 = non- measurable/interpretable plot; 1 = significant noise is present but the plot is still interpretable; 2 = good noise-to-signal ratio. The seven dogs that were excluded from the final analysis had images from which it was not possible to generate recognizable DI curves. The score “0” was attributed to cases in which it was not possible to generate a minimum of 5 good quality plots from five separate cardiac cycles. A total of 1,470 ROIs were included in the final analysis, excluding the echocardiograms that were repeated as part of the R&R analysis. Only 5 dogs (10.2% of the 49 total dogs) received a score 2 in some of the plots, for a total of 71 plots (4.84% of 1,470 plots). None of them received a score 2 in all of their plots included in the final analysis. The majority of plots (1294, equal to 88.02% of 1,470 curves analyzed) were given a score of 1. The remainder of the curves received a score of 0 (105, equal to 7.14% of 1,470 curves). It means that, of the total number of DI values obtained from the 49 dogs, 7.14% is not the average of five good quality beats, but the result of the average of 4 good quality beats. Figure 44 shows the distribution of scores in the four study groups. There was a tendency towards a higher number of dogs receiving a score 1 in groups 2 and 3, although it did not reach statistical significance (p=0.988 from a Kruskal-Wallis test). Tables 5 and 6 show a summary of the DI parameters in the 49 dogs 65 included in the final analysis. The values are the average of 4-5 heart beats. Table 5 shows values of individual ROIs, while in Table 6 the average of the 6 ROIs, standard deviation (SD), lower and upper 95% confidence interval, and % coefficient of variability are indicated. Figure 45 shows the distribution of the DI variable SSR in the six ROIs. There was a significant difference in the medians from a Kruskal-Wallis test, between some groups, as indicated in Table 7. Similar analyses were performed on the S, SRE, and SRA data, to evaluate the presence of differences between the six ROIs. Figure 46 shows the distributions of DI parameter S. There was a significant difference in the means (p<0.0001 from an ANOVA test) between some ROIs, as indicated in Table 8. Figure 47 and Figure 48 show the distributions of the variables SRE and SRA, between the six ROIs. There were no statistically significant differences in the medians (p<0.05 from Kruskal-Wallis tests) for both SRE and SRA. Figures 49, 50, 51, and 52 show the distributions of the DI parameter SSR in the six ROIs, respectively in groups 1, 2, 3, and 4. There were statistically significant differences between some ROIs in group 1 and 2, but not in group 3 and 4. The instantaneous heart rate was measured from the RR interval, and recorded for each cardiac cycle evaluated in the final analysis. There were no significant differences in HR between the four groups (p<0.05 from an ANOVA test) (Figure 53). The HR was also evaluated in the subset of data utilized in the R&R analysis. Figure 54 shows the distribution of HR during the two echocardiographic examinations performed by the same 66 operator. There were no significant differences (Two-tailed p=0.429 from a paired t Test) in HR between the two echocardiograms. Same results were obtained from the analysis of the HR distribution between the two echocardiographic examinations used in the reproducibility analysis. Figure 55 shows the distribution of HR during the two echocardiographic examinations performed by the two operators. There were no significant differences (Twotailed p=0.431 from a paired t Test) in HR between the two sets of data. To rule out differences in NIBP as a potential confounding variable in the assessment of ventricular performance, the mean NIBP values were compared in the four study groups. There were no differences between the groups (p=0.176 from a Kruskal-Wallis test), as shown in Figure 56. To identify potential differences in the group of Doberman pinschers versus other breeds, controlling for differences in BW, initially a weight-matched subgroup of dogs was identified and compared with group 4. As previously reported dogs in group 3 were significantly different regarding their BW, compared to dogs in group 4. Figure 57 shows a comparison between a BW-matched subgroup 3 and group 4. There was no significant difference between the BW in these two groups (p=0.302 from an unpaired t Test). Initially the EF was compared between these two groups. There was no difference between the two groups (Two-tailed p=0.325 from an unpaired t Test) (Figure 58). The DI variable avSSR was compared between these two groups (Figure 59). There was no significant difference between the two groups (p=0.065 from a Mann Whitney 67 test). Similar analysis was conducted on the variable avS. There was no difference between the two groups (p=0.250 from an unpaired t Test) (Figure 60). The potential effect of BW on DI data was also investigated. For this analysis dogs were initially re-grouped into three BW groups, independently on their breed (i.e. dogs in group 4 were included in other groups based on their BW). Figure 61 shows the effect of BW on avSSR. There was a statistically significant difference between group 1 and 2 (p<0.01 from an ANOVA test) and between group 1 and 3 (p<0.05 from an ANOVA test). There was no significant difference between group 2 and 3 (p>0.05 from an ANOVA test). When the data from the Doberman pinscher group were excluded from the analysis, the results of the comparison did not change (Figure 62). The three BW groups were also compared based on the traditional echocardiographic indices of systolic function, FS and EF (Figures 63 and 64, respectively). Both FS (p=0.069 from an ANOVA test) and EF (p=0.245 from an ANOVA test) did not differ significantly between the three BW groups. To further characterize the potential effects of BW on avSSR, simple linear regression analysis between avSSR and BW was conducted (Figure 65). No significant correlation was documented with this model (r squared=0.011). Same analysis was conducted on avS. The absence of a significant correlation that can be explained with a simple linear regression model (r squared=0.013) was documented as well (Figure 66). A potential correlation between traditional indices of systolic function (FS and EF) and DI indices of systolic function 68 (avSSR and avS) was investigated constructing a simple linear regression model. Figures 67, 68, 69, and 70 show the results of these models. It was not possible to document a significant correlation between avSSR and FS (r squared=0.196), avSSR and EF (r squared=0.047), avS and FS (r squared=0.079), and avS and EF (r squared=0.080), in the set of data from this study. The potential effects of HR on avSSR and avS were investigated using the same regression model. It was not possible to document a significant correlation between avSSR and HR (r squared=0.314) (Figure 71) and between avS and HR (r squared=0.026) (Figure 72). The R&R analysis was conducted using Bland-Altman analysis. This analysis generates plots that display the differences between the two measurements as a function of the average of each sample, which can be considered as the best estimate of the true value. The bias (which corresponds to the average of the differences between the two sets of data), the SD of the differences between the two sets of data, and the 95% limits of agreement are provided in the tables. Figures 73, 74, 75, and 76 show the Bland-Altman plots of the repeatability subanalysis, and Table 9 shows bias, SD and 95% limits of agreement for the variables avSSR, avSRE, avSRA and avS in the repeatability subanalysis. Figures 77, 78, 79, and 80 show the Bland-Altman plots of the reproducibility sub-analysis, and Table 10 reports bias, SD and 95% limits of agreement for the variables avSSR, avSRE, avSRA and avS in the reproducibility subanalysis. 69 Table 4: Descriptive statistics of the 49 dogs included in the final analysis Variable Group 1 Group 2 Group 3 Group 4 Sex Females Males Spayed females Neutered males 0 0 2 8 0 0 9 6 0 1 6 7 4 5 1 0 Mean SD Median Minimum Maximum 9.67 3.52 10.15 2.40 14.50 24.25 3.84 26.00 16.20 29.52 41.69 9.21 41.15 31.00 63.21 33.58 4.97 32.30 28.00 43.60 Mean SD Median Minimum Maximum 4.2 2.73 4.0 1.0 8.0 4.26 2.22 4.0 2.0 8.0 4.21 2.15 3.5 2.0 8.0 2.42 0.84 2.0 1.0 4.0 10 15 14 10 BW Age Total 70 Table 5: DI parameters from the six ROIs (Mean values) SSR SRE SRA S ROI 1 ROI 2 ROI 3 ROI 4 -1.40 -1.21 -1.38 -1.55 1.69 1.45 1.71 1.52 1.27 1.25 1.45 1.19 -12.38 -12.00 -12.92 -14.25 ROI 5 -1.88 1.51 1.30 -16.70 ROI 6 -1.52 1.69 1.45 -14.22 Table 6: DI parameters as average of the six ROIs Mean avSSR -1.49 avSRE 1.60 avSRA 1.32 avS -13.74 SD Lower 95%C.I. Upper 95% C.I. 0.31 -1.58 -1.40 0.43 1.47 1.72 0.35 1.22 1.42 2.09 -14.34 -13.15 CV% 20.79 26.90 26.25 15.18 71 Sex distribution Group 1 Group 2 Group 3 Group 4 P value 9 0.9561 8 7 6 5 4 3 2 1 0 F M SF NM Sex status Figure 41: Sex distribution in the four study groups Age distribution P value 8.5 0.1617 8.0 7.5 7.0 6.5 6.0 5.5 5.0 4.5 4.0 3.5 3.0 2.5 2.0 1.5 1.0 0.5 0.0 Group 1 Group 2 Group 3 Figure 42: Age distribution in the four study groups Group 4 72 BW P value 70 P<0.0001 60 50 40 30 20 10 0 Group 1 Group 2 Group 3 Group 4 Figure 43: BW distribution in the four study groups Plot scores 450 Group 1 Group 2 Group 3 Group 4 400 P value 0.9883 350 300 250 200 150 100 50 0 Score 0 Score 1 Score 2 Figure 44: Distribution of plot quality scores in the four study groups 73 SSR (ROIs 1-6) -0.10 -0.20 -0.30 -0.40 -0.50 -0.60 -0.70 -0.80 -0.90 -1.00 -1.10 -1.20 -1.30 -1.40 -1.50 -1.60 -1.70 -1.80 -1.90 -2.00 -2.10 -2.20 -2.30 -2.40 -2.50 -2.60 -2.70 -2.80 -2.90 -3.00 -3.10 -3.20 -3.30 -3.40 -3.50 -3.60 -3.70 1 2 3 4 5 6 ROIs Figure 45: Distribution of the DI variable SSR in the six ROIs Table 7: Results of a Dunn’s Multiple Comparison Test for the variable SSR, between the 6 ROIs Parameter Dunn's Multiple Comparison Test 1 vs 2 1 vs 3 1 vs 4 1 vs 5 1 vs 6 2 vs 3 2 vs 4 2 vs 5 2 vs 6 3 vs 4 3 vs 5 3 vs 6 4 vs 5 4 vs 6 5 vs 6 Value Difference in rank sum -29.34 2.796 28.59 76.78 15.95 32.13 57.93 106.1 45.29 25.80 73.98 13.15 48.18 -12.64 -60.83 Data Set-B P value P > 0.05 P > 0.05 P > 0.05 P < 0.001 P > 0.05 P > 0.05 P < 0.05 P < 0.001 P > 0.05 P > 0.05 P < 0.001 P > 0.05 P > 0.05 P > 0.05 P < 0.01 Data Set-C Summary ns ns ns *** ns ns * *** ns ns *** ns ns ns ** 74 S (ROIs 1-6) -2.00 -3.00 -4.00 -5.00 -6.00 -7.00 -8.00 -9.00 -10.00 -11.00 -12.00 -13.00 -14.00 -15.00 -16.00 -17.00 -18.00 -19.00 -20.00 -21.00 -22.00 -23.00 -24.00 -25.00 -26.00 -27.00 -28.00 -29.00 -30.00 1 2 3 4 5 6 ROIs Figure 46: Distribution of the DI variable S in the six ROIs Table 8: Results of a Dunn’s Multiple Comparison Test for the variable S, between the 6 ROIs Parameter Bonferroni's Multiple Comparison Test 1 vs 2 1 vs 3 1 vs 4 1 vs 5 1 vs 6 2 vs 3 2 vs 4 2 vs 5 2 vs 6 3 vs 4 3 vs 5 3 vs 6 4 vs 5 4 vs 6 5 vs 6 Value Mean Diff. -0.3745 0.5471 1.872 4.325 1.845 0.9216 2.247 4.699 2.219 1.325 3.778 1.298 2.453 -0.02714 -2.480 Data Set-B t 0.4942 0.7220 2.470 5.707 2.434 1.216 2.964 6.201 2.929 1.748 4.985 1.712 3.237 0.03582 3.272 Data Set-C P value P > 0.05 P > 0.05 P > 0.05 P < 0.001 P > 0.05 P > 0.05 P < 0.05 P < 0.001 P > 0.05 P > 0.05 P < 0.001 P > 0.05 P < 0.05 P > 0.05 P < 0.05 Data Set-D 95% CI of diff -2.618 to 1.869 -1.696 to 2.790 -0.3711 to 4.115 2.082 to 6.568 -0.3982 to 4.088 -1.321 to 3.165 0.003414 to 4.490 2.456 to 6.943 -0.02373 to 4.463 -0.9182 to 3.568 1.535 to 6.021 -0.9454 to 3.541 0.2097 to 4.696 -2.270 to 2.216 -4.723 to -0.2369 75 SR E (ROIs 1-6) 4.50 No post tests. P > 0.05 4.00 3.50 3.00 2.50 2.00 1.50 1.00 0.50 0.00 1 2 3 4 5 6 ROIs Figure 47: Distribution of the DI variable SRE in the 6 ROIs SR A (ROIs 1-6) No post tests. P > 0.05 7.00 6.00 5.00 4.00 3.00 2.00 1.00 0.00 1 2 3 4 5 6 ROIs Figure 48: Distribution of the DI variable SRA in the 6 ROIs 76 SSR (ROIs 1-6) Group 1 -0.50 -0.75 -1.00 -1.25 -1.50 -1.75 -2.00 -2.25 -2.50 P < 0.01 -2.75 P < 0.05 -3.00 -3.25 1 2 3 4 5 6 ROIs Figure 49: Distribution of the DI variable SSR in the 6 ROIs in group 1 SSR (ROIs 1-6) Group 2 -0.25 -0.50 -0.75 -1.00 -1.25 -1.50 -1.75 -2.00 P < 0.01 -2.25 -2.50 P < 0.001 P < 0.01 -2.75 1 2 3 4 5 6 ROIs Figure 50: Distribution of the DI variable SSR in the 6 ROIs in group 2 77 SSR (ROIs 1-6) Group 3 No post tests. P > 0.05 -0.10 -0.20 -0.30 -0.40 -0.50 -0.60 -0.70 -0.80 -0.90 -1.00 -1.10 -1.20 -1.30 -1.40 -1.50 -1.60 -1.70 -1.80 -1.90 -2.00 -2.10 -2.20 -2.30 -2.40 -2.50 -2.60 -2.70 -2.80 -2.90 -3.00 -3.10 -3.20 -3.30 -3.40 -3.50 -3.60 -3.70 1 2 3 4 5 6 ROIs Figure 51: Distribution of the DI variable SSR in the 6 ROIs in group 3 SSR (ROIs 1-6) Group 4 -0.50 No post tests. P > 0.05 -0.60 -0.70 -0.80 -0.90 -1.00 -1.10 -1.20 -1.30 -1.40 -1.50 -1.60 -1.70 -1.80 -1.90 -2.00 -2.10 1 2 3 4 5 6 ROIs Figure 52: Distribution of the DI variable SSR in the 6 ROIs in group 4 78 HR No post tests. P > 0.05 175 170 165 160 155 150 145 140 135 130 125 120 115 110 105 100 95 90 85 80 75 70 65 60 Group 1 Group 2 Group 3 Group 4 Figure 53: Distribution of the HR values in the four study groups HR (Repeatabilty) P value 0.4290 175 170 165 160 155 150 145 140 135 130 125 120 115 110 105 100 95 90 85 80 75 70 65 60 55 50 45 40 35 30 25 20 15 10 5 0 1 2 Echocardiogram Figure 54: Distribution of the HR values during the two echocardiographic examinations performed by the same operator 79 HR (Reproducibility) P value 0.4317 160 150 140 130 120 110 100 90 80 70 60 50 40 30 20 10 0 HR Op1 HR Op2 Figure 55: Distribution of the HR values during the two echocardiographic examinations performed by the two different operators Mean BP No post tests. P > 0.05 155 150 145 140 135 130 125 120 115 110 105 100 95 90 85 80 75 Group 1 Group 2 Group 3 Group 4 Figure 56: Distribution of the BP values in the 4 study groups 80 BW-matched Group 3 vs Group 4 47 46 45 44 43 42 41 40 39 38 37 36 35 34 33 32 31 30 29 28 27 P value BW-matched Group 3 0.3019 Group 4 Figure 57: Comparison between a BW-matched subgroup 3 and group 4 EF BW-matched Group 3 vs Group 4 P value 0.3252 77.5 75.0 72.5 70.0 67.5 65.0 62.5 60.0 57.5 55.0 52.5 50.0 47.5 45.0 42.5 40.0 "BW-matched" Group 3 Group 4 Figure 58: Comparison between the EF values in the BW-matched subgroup 3 and group 4 81 avSSR BW-matched Group 3 vs Group 4 P value 0.0653 -0.6 -0.7 -0.8 -0.9 -1.0 -1.1 -1.2 -1.3 -1.4 -1.5 -1.6 -1.7 -1.8 -1.9 "BW-matched" Group 3 Group 4 Figure 59: Comparison between the avSSR values in the BW-matched subgroup 3 and group 4 avS BW-matched Group 3 vs Group 4 P value -9 0.2515 -10 -11 -12 -13 -14 -15 -16 -17 -18 BW matched Group 3 Group 4 Figure 60: Comparison between the avS values in the BW-matched subgroup 3 and group 4 82 avSSR vs BW groups -0.6 -0.7 -0.8 -0.9 -1.0 -1.1 -1.2 -1.3 -1.4 -1.5 -1.6 -1.7 -1.8 -1.9 -2.0 P < 0.01 -2.1 -2.2 -2.3 P < 0.05 -2.4 Group 1 Group 2 Group 3 Figure 61: Comparison between the avSSR values in the three BW groups (For this analysis groups 4 dogs were redistributed to other groups based on their BW) avSSR vs BW groups (excluding Dobermans) -0.9 -1.0 -1.1 -1.2 -1.3 -1.4 -1.5 -1.6 -1.7 -1.8 -1.9 -2.0 -2.1 P < 0.01 -2.2 P < 0.01 -2.3 -2.4 Group 1 Group 2 Group 3 Figure 62: Same analysis as in Figure 36, excluding dogs from group 4 83 FS vs BW groups No post tests. P > 0.05 37 36 35 34 33 32 31 30 29 28 27 26 25 24 23 22 21 20 19 18 17 16 15 14 13 12 11 10 9 8 7 6 5 4 3 2 1 0 Group 1 Group 2 Group 3 Figure 63: Comparison between the FS values in the three BW groups EF vs BW groups No post tests. P > 0.05 82.5 80.0 77.5 75.0 72.5 70.0 67.5 65.0 62.5 60.0 57.5 55.0 52.5 50.0 47.5 45.0 42.5 40.0 37.5 35.0 32.5 30.0 27.5 Group 1 Group 2 Group 3 Figure 64: Comparison between the EF values in the three BW groups 84 avSSR vs BW avSSR -0.50 r squared 0.01106 -0.75 -1.00 -1.25 -1.50 -1.75 -2.00 -2.25 -2.50 0 10 20 30 40 50 60 70 BW (kg) Figure 65: Simple linear regression analysis between avSSR and BW avS vs BW -8 r squared 0.01300 -9 -10 -11 -12 -13 -14 -15 -16 -17 -18 -19 -20 0 10 20 30 40 50 60 70 BW (kg) Figure 66: Simple linear regression analysis between avS and BW 85 avSSR vs FS -0.7 -0.8 r squared 0.1960 -0.9 -1.0 -1.1 -1.2 -1.3 -1.4 -1.5 -1.6 -1.7 -1.8 -1.9 -2.0 -2.1 -2.2 -2.3 -2.4 -2.5 0.0 2.5 5.0 7.5 10.0 12.5 15.0 17.5 20.0 22.5 25.0 27.5 30.0 32.5 35.0 37.5 40.0 FS% Figure 67: Simple linear regression analysis between avSSR and FS avS vs FS -8 -9 r squared 0.07943 -10 -11 -12 -13 -14 -15 -16 -17 -18 -19 -20 0.0 2.5 5.0 7.5 10.0 12.5 15.0 17.5 20.0 22.5 25.0 27.5 30.0 32.5 35.0 37.5 40.0 FS% Figure 68: Simple linear regression analysis between avS and FS 86 avSSR vs EF r squared -8 0.08088 -9 -10 -11 -12 -13 -14 -15 -16 -17 -18 -19 -20 30 35 40 45 50 55 60 65 70 75 80 85 EF Figure 69: Simple linear regression analysis between avSSR and EF avS vs EF r squared -8 0.08088 -9 -10 -11 -12 -13 -14 -15 -16 -17 -18 -19 -20 30 35 40 45 50 55 60 65 70 75 80 85 EF Figure 70: Simple linear regression analysis between avS and EF 87 avSSR vs HR r squared -0.50 0.3143 avSSR -0.75 -1.00 -1.25 -1.50 -1.75 -2.00 -2.25 -2.50 60 70 80 90 100 110 120 130 140 150 160 170 180 HR (bpm) Figure 71: Simple linear regression analysis between avSSR and HR avS vs HR r squared -8 0.02634 avS -9 -10 -11 -12 -13 -14 -15 -16 -17 -18 -19 -20 60 70 80 90 100 110 120 130 140 150 160 170 180 HR (bpm) Figure 72: Simple linear regression analysis between avS and HR 88 avSSR (Repeatability) -0.9 -1.0 -1.1 -1.2 -1.3 -1.4 -1.5 -1.6 -1.7 -1.8 -1.9 -2.0 -2.1 -2.2 -2.3 -2.4 Echo 1 Echo 2 Bland-Altman (Repeatability): Difference vs average 0.65 0.60 0.55 0.50 0.45 0.40 0.35 0.30 0.25 0.20 0.15 0.10 0.05 -0.00 -0.05 -0.10 -0.15 -0.20 -0.25 -0.30 -0.35 -0.40 -0.45 -0.50 -0.55 -0.60 -0.65 -0.70 -2.2 -2.1 -2.0 -1.9 -1.8 -1.7 -1.6 -1.5 -1.4 -1.3 -1.2 -1.1 -1.0 Average Figure 73: Bland-Altman plots of the repeatability sub-analysis for avSSR 89 avSRE (Repeatability) 2.4 2.3 2.2 2.1 2.0 1.9 1.8 1.7 1.6 1.5 1.4 1.3 1.2 1.1 1.0 0.9 Echo 1 Echo 2 egareva sv ecnereffiD :)ytilibataepeR( namtlA-dnalB 54.0 04.0 53.0 03.0 52.0 02.0 51.0 01.0 50.0 00.050.001.051.002.052.003.053.004.054.005.055.006.056.007.05.2 4.2 3.2 2.2 1.2 0.2 9.1 8.1 7.1 6.1 5.1 4.1 3.1 2.1 1.1 0.1 9.0 egarevA Figure 74: Bland-Altman plots of the repeatability sub-analysis for avSRE 90 avSRA (Repeatability) 2.2 2.1 2.0 1.9 1.8 1.7 1.6 1.5 1.4 1.3 1.2 1.1 1.0 0.9 Echo 1 Echo 2 Bland-Altman (Repeatability): Difference vs average 0.85 0.80 0.75 0.70 0.65 0.60 0.55 0.50 0.45 0.40 0.35 0.30 0.25 0.20 0.15 0.10 0.05 -0.00 -0.05 -0.10 -0.15 -0.20 -0.25 -0.30 -0.35 -0.40 -0.45 -0.50 -0.55 -0.60 -0.65 0.9 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 2.0 2.1 2.2 2.3 Average Figure 75: Bland-Altman plots of the repeatability sub-analysis for avSRA 91 avS (Repeatability) -9 -10 -11 -12 -13 -14 -15 -16 -17 -18 -19 Echo 1 Echo 2 Bland-Altman (Reproducibility) :Difference vs average 4 3 2 1 0 -1 -2 -3 -4 -5 -6 -18 -17 -16 -15 -14 -13 -12 -11 -10 Average Figure 76: Bland-Altman plots of the repeatability sub-analysis for avS 92 Table 9: Results of a Bland-Altman analysis of the data from the repeatability subanalysis Parameter (repeatability) Bias SD 95% Limits of agreement From: To: avSSR 0.076 0.301 avSRE -0.056 0.264 avSRA -0.023 0.395 avS -0.124 2.598 -0.514 0.666 -0.574 0.461 -0.797 0.751 -5.215 4.968 93 avSSR (Reproducibility) -0.75 -1.00 -1.25 -1.50 -1.75 -2.00 -2.25 -2.50 Op. 1 Op. 2 Bland-Altman (Reproducibility): Difference vs average 0.6 0.5 0.4 0.3 0.2 0.1 -0.0 -0.1 -0.2 -0.3 -0.4 -0.5 -2.3 -2.2 -2.1 -2.0 -1.9 -1.8 -1.7 -1.6 -1.5 -1.4 -1.3 -1.2 -1.1 Average Figure 77: Bland-Altman plots of the reproducibility sub-analysis for avSSR 94 avSRE (Reproducibility) 3.50 3.25 3.00 2.75 2.50 2.25 2.00 1.75 1.50 1.25 1.00 0.75 0.50 0.25 0.00 Op. 1 Op. 2 Bland-Altman (Reproducibility): Difference vs average 1.7 1.6 1.5 1.4 1.3 1.2 1.1 1.0 0.9 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 -0.0 -0.1 -0.2 -0.3 -0.4 -0.5 -0.6 -0.7 1.3 1.4 1.5 1.6 1.7 1.8 1.9 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Average Figure 78: Bland-Altman plots of the reproducibility sub-analysis for avSRE 95 avSRA (Reproducibility) 3.50 3.25 3.00 2.75 2.50 2.25 2.00 1.75 1.50 1.25 1.00 0.75 0.50 0.25 0.00 Op. 1 Op. 2 Bland-Altman (Reproducibility): Difference vs average 0.65 0.60 0.55 0.50 0.45 0.40 0.35 0.30 0.25 0.20 0.15 0.10 0.05 -0.00 -0.05 -0.10 -0.15 -0.20 -0.25 -0.30 -0.35 -0.40 -0.45 0.8 0.9 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 2.0 2.1 Average Figure 79: Bland-Altman plots of the reproducibility sub-analysis for avSRA 96 avS (Reproducibility) -9 -10 -11 -12 -13 -14 -15 -16 -17 Op. 1 Op. 2 Bland-Altman (Reproducibility): Difference vs average 2.5 2.0 1.5 1.0 0.5 0.0 -0.5 -1.0 -1.5 -2.0 -2.5 -3.0 -3.5 -17 -16 -15 -14 -13 -12 -11 -10 -9 Average Figure 80: Bland-Altman plots of the reproducibility subanalysis for avS 97 Table 10: Results of a Bland-Altman analysis of the data from the reproducibility subanalysis Parameter (reproducibility) Bias SD 95% Limits of agreement From: To: avSSR 0.043 0.272 avSRE 0.624 0.586 avSRA 0.000 0.254 avS -0.650 1.680 -0.491 0.577 -0.524 1.772 -0.497 0.497 -3.942 2.642 98 Discussion Study 1 The comparisons between the hemodynamic variables obtained at steady state after induction of anesthesia and during the different pharmacologic manipulations suggest that significant changes in the inotropic state, preload and afterload were reached during the study. Hence, the study was able to generate a model in which a relatively wide range of inotropic and loading conditions was created. The significance of these variations was of both statistical and clinical importance, as documented not only by a p-value of less then 0.05, but also by a wide range of variations in many hemodynamic parameters, as shown in Table 3. The dobutamine infusion was able to increase the SV from 29.82 ± 4.66 ml at steady state after induction of anesthesia, to 60.24 ± 10.81 ml. The RR interval was significantly shortened during the dobutamine and nitroprusside infusions, compared to baseline under anesthesia, indicating that the HR was significantly increased. In fact, the RR interval is a parameter linearly and inversely correlated to the HR, as shown by the relationship RR = 60,000/HR, where 60,000 is the number of ms in one minute, and the HR is expressed in beats per minute (BPM). Therefore one could comment that the increase in CO (where CO = HR x SV) could have been merely the result of an increase in HR. Hence, it is important to focus on 99 the SV, because it represents an index of LV systolic function that is relatively independent of the HR. Dobutamine also increased the +dP/dtmax from 1546 ± 375.5 mmHg/s to 3157 ± 464.7 mmHg/s. Both changes indicate that a significant positive inotropic effect was obtained, making this study an adequate model to correlate invasive and non-invasive indices of systolic function. Both CO and SV returned to baseline during nitroprusside and hetastarch administration. Pharmacokinetic data for dobutamine in domestic animals are apparently unavailable.(50) Data from the human literature describe dobutamine as a drug that is metabolized rapidly in the liver and other tissues and has a plasma half-life of approximately 2 minutes. These facts should support the appropriateness of a wash-out period of a minimum of 20 minutes, as it was adopted in the study. Dobutamine is a sympathomimetic drug capable of exerting a positive lusitropic effect (improved relaxation).(50) Nitroprusside, a balanced vasodilator, has the ability of reducing the preload.(51) The LVEDP was significantly reduced during dobutamine and nitroprusside infusions, and returned to baseline after the hetastarch bolus. These findings indicate that significant changes in the preload have been obtained during the study. Systemic vascular resistances were significantly reduced during nitroprusside infusion, documenting that a reduction in the afterload was obtained in the study. Mean RA pressure was significantly increased during the hetastarch infusion, indicating that volume expansion, with secondary increase in the right ventricular preload, was obtained. 100 However, the pulmonary capillary wedge pressure did not change significantly. This may indicate, together with the fact that the left ventricular end-diastolic pressure was not significantly elevated during the hetastarch infusion, that this model was unable of creating a significant increase in the LV preload. An alternative explanation could be that, at the time of the hetastarch infusion, the LV was still somehow benefiting from a residual positive lusitropic effect of dobutamine, enabling it to accommodate the increased venous return, without significant increases in the LVEDP. Against this hypothesis is the fact that the invasive parameter -dP/dtmax did not change significantly throughout the study, indicating that, although the LVEDP (an end-diastolic event) was reduced, the maximum rate of relaxation during the isovolumic relaxation phase (an early diastolic event) was not significantly increased. Although there was a trend toward more negative values of -dP/dtmax during dobutamine infusion, this change did not reach statistical significance. Because of this we cannot document that this study created an adequate model to correlate invasive and non-invasive indices of diastolic function, because what would have been our “gold-standard” for the quantification of the intrinsic diastolic function did not reach statistical significance. This is the most important reason why we focused on indices of systolic function (mainly avSSR and avS). This study also focused on the longitudinal systolic function of the LV, for reasons explained in an earlier chapter; findings from this research cannot be extrapolated to the study of the radial and circumferential LV function. The 101 parameter avSSR was significantly reduced, i.e. systolic function was increased, by the dobutamine infusion, but was not significantly different during nitroprusside and hetastarch infusion. It is worth noting that the LVEDP was significantly reduced during the nitroprusside infusion, apparently not influencing avSSR, and suggesting the possible preload independence of this parameter, in the hemodynamic range generated in the study. Furthermore, SVR remained significantly reduced during nitroprusside administration, but appeared not to influence avSSR, suggesting a possible afterload independence of this parameter, in the hemodynamic range obtained in this study. A significant percentage (98.67%) of ROIs included in the final analysis yielded interpretable Doppler-derived DI curves. In order to correctly interpret the value of this finding it is important to consider that a total of 14 cardiac cycles were available for off-line analysis, providing the operator with an amount of data to choose from, which is significantly greater compared to what is stored in a routine echocardiographic study (usually between 2 and 5 cardiac cycles). The SSR values obtained from the 6 ROIs and analyzed separately over the hemodynamic range generated in the study did not differ significantly from each other. For this reason the results of many analyses focusing on single ROIs are not included. This finding supports the hypothesis that longitudinal SSR is homogeneously distributed along the long axis of the LV, negating the 102 presence of a significant longitudinal gradient for this parameter. Theoretically, this finding by itself suggests that the functional information obtainable with SRI could be independent of the location of the specific ROI along the long axis of the LV, with the only exception being a patient with LV dyskinesia. Both FS% (Figure 18) and avSSR (Figure 32) did not change significantly between the baseline echocardiogram before anesthesia and the steady state after induction of anesthesia. The level of anesthesia was monitored closely by a board-certified anesthesiologist and always maintained as light as possible. The procedures performed on the animals were not particularly invasive, hence surgical pain was limited. The light level of anesthesia definitely played a role in the absence of detectable negative inotropic effects, as documented by the absence of changes in FS and peak systolic SR. These data may be useful in the interpretation of data from echocardiographic examinations conducted under a similar anesthetic protocol. 103 Study 2 The analysis of the population of dogs enrolled in study 2 could not identify significant differences between the four groups, beyond the obvious differences in BW and breed, which were part of our inclusion criteria. Because it was difficult to enroll the minimum number of Doberman pinschers defined in the study protocol, breeders in the area were contacted. This led to the fact that the majority of Doberman pinschers were relatively young, intact dogs; animals for which the breeder had an interest in obtaining a complete cardiovascular work-up. This bias in the phase of recruitment is reflected by the trend for group 4 toward a younger age and a higher number of intact individuals. This trend did not reach statistical significance with the statistical model adopted in this study, but should be considered as a potential limitation of the study. Seven dogs out of the initial 56 (12.5%) were excluded from the off-line analysis because the quality of the DI curves was considered unacceptable. These dogs had acceptable traditional echocardiographic images. Furthermore, of the 1,470 ROIs analyzed, only 10.2% received a score of 2 (good noise-to-signal ratio), and this level of quality was never found in all of the four/five beats included in the final analysis. It was not possible to analyze 7.14% of the ROIs and the majority of the curves were assigned a score 1, indicating that their noise-to-signal ratio was high, but that systolic, early diastolic (E) and late diastolic (A) waves were still discernible. A 104 high level of noise can cause two major problems in terms of off-line analysis. The noise can add to or subtract from the real parameter, causing falsely elevated or falsely reduced values and contributing to the overall variability of these parameters. Noise also causes the appearance of spurious waves, which makes the identification of the real wave pattern challenging, potentially leading to an incorrect interpretation of the tracing. There appeared to be a trend for larger breed dogs toward higher plot quality scores, although it did not reach statistical significance. A higher number of dogs might have yielded a different result. This trend can be explained by the fact that medium size dogs often have a better acoustic window, and frequently are also more willing to cooperate, compared to small breed dogs, hypothetically because of different temperament and/or different training. The hypothesis of the absence of a left ventricular longitudinal gradient for DI parameters could not be confirmed by the results of study 2. The analyses of the systolic phase DI parameters SSR and S identified the presence of a difference between some of the ROIs. The same difference could not be documented for the diastolic phase DI variables SRE and SRA. The finding of a significant difference in SSR and S values between different ROIs in study 2 is in disagreement with the results of study 1, and with the medical literature on the topic. One explanation for this contradictory finding is that the high level of variability in the DI data collected in this group of non-sedated dogs might have confounded the results of the statistical analysis. Other explanations include 105 some systematic sampling error or a true deformation difference that might be body weight or heart size dependent. Why the SRE and SRA waves were apparently not affected by this phenomenon, remains to be explained. It was not possible to document a difference in avSSR between Doberman pinschers and BW-matched non-Doberman dogs. The p value from a Mann Whitney test was 0.060; it can be hypothesized that a higher number of dogs might have yielded a different result. However this moderate lack of significance is in agreement with the convincing lack of significance (p=0.325) obtained comparing the EF values between the same two groups. It can be probably concluded that there was no detectable difference in systolic function between the group of Doberman pinschers enrolled in the study and the BW-matched non-Doberman group. Interestingly the study documented a significant difference (p<0.01) in avSSR in dogs weighting less than 15 kilograms (group 1) compared to group 2. Relatively convincing difference (p<0.05) was also found between group 1 and 3. These findings did not change when Doberman pinscher dogs were excluded from the analysis. The mean difference ranged from -0.45 s-1 (between group 1 and 2) and -0.33 s-1 (between group 1 and 3), showing a tendency for small breed dogs toward higher values of systolic function, when evaluated based on avSSR. This mean difference is not only statistically significant, but it also appears to be clinically significant, when compared to the 95% C.I. for the parameter. No differences were found when FS, EF and S values were compared between the three BW groups. It could 106 be hypothesized that avSSR has a higher sensitivity in detecting subtle changes in systolic performance between normal dogs. Simple linear regression models could not identify any correlation between the DI parameters avSSR and avS and the population parameters BW and HR. At the same time, it was not possible to document a correlation between the DI indices of systolic function avSSR and avS and the traditional indices FS and EF. This finding is in contradiction with the results of study 1, in which relatively convincing evidence supporting the existence of a linear correlation (r squared=0.922, p=0.039) between avSSR and FS was found. The most plausible explanation for this discrepancy is the high level of variability (notice the high coefficient of variability of the DI parameters in Table 6) encountered in study 2 relative to the relatively modest range of contractile states encountered in a population of healthy dogs. This may have confounded most of the linear regression models constructed during the analysis. The results of the R&R analysis based on the Bland-Altman plots allow for an interpretation of the data with a strong clinical emphasis. Many papers in the veterinary literature used various statistical approaches to estimate intra- and interoperator variability and several references in the literature comment on the inappropriateness of some of these statistical approaches.(54,55,56,57,58) In particular, Bland and Altman in the 1980’s criticized the use of these statistical tools for clinical purposes.(58) In this paper, the use of correlation, regression and the difference between means (such as a paired t-Test) are defined 107 inappropriate models to answer the question of interest: what is the level of agreement between two sets of results? To summarize the points made by the authors we can quote them as follows: “The correlation coefficient is not a measure of agreement; it is a measure of association”. Furthermore, criticizing the use of tests that compare the means of two data sets, the authors state that by this criterion: “the greater the measurement error, and hence the less chance of a significant difference, the better”. Finally the authors comment on the use of linear regression, stating that: “this is equivalent to testing the correlation coefficient against zero, and the above remarks apply”. Bland and Altman conclude stating that: “a simple approach to the analysis may be the most revealing way of looking at the data” and emphasize that this is a question of estimating, both error and bias, and that no single statistic can estimate both. The analysis they developed provides estimates of both error and bias. Bland-Altman plots are generally interpreted informally, without further analysis. There are three major questions the clinician should try to answer. The first question pertains to how big the average discrepancy is between the two sets of measurements (i.e. the bias). Is the discrepancy large enough to be important? This question must be interpreted from the clinical, not the statistical standpoint. Second question: Is there a trend? Does the difference between measurements tend to get larger (or smaller) as the average increases? Final question: is the variability consistent across the graph? In other words: does the scatter around the bias line gets larger as the 108 average gets higher? The two last questions can be better assessed if the number of measurements is moderately high, and is not feasible with small samples. Another common statistical parameter used to estimate intra-operator and inter-operator variability is the coefficient of variation (CV), customarily presented as a percentage (CV%). It represents a statistical measure of dispersion of data points, calculated as: (14) cv = σ × 100 Where σ is the standard deviation (SD) and μ is the μ mean of the distribution. The CV% is a useful statistic for comparing the degree of variation from one data series to another, even if the means are drastically different from each other. In fact, specifying the SD alone is more or less useless without the additional specification of the mean value (and of course the type of distribution). An important limitation of this statistic is that, when the mean value is near zero, the coefficient of variation becomes almost entirely dependent to changes in the standard deviation, limiting its usefulness.(59) The mean differences between the two sets of measurements in both the repeatability and reproducibility sub-analyses were, in most instances, numbers close to zero (range from -0.650 to 0.624). This is the reason why the CV% was deemed to be not the ideal statistic in the R&R analysis. In the repeatability analysis (Table 9 from a Bland-Altman analysis) the intra- 109 operator bias ranged from -0.023 for avSRA to 0.076 for avSSR, which by themselves represent relatively small numbers. However, when their SD is taken into account we can appreciate how wide the 95% limits of agreement are compared to the 95% confidence intervals of the corresponding DI parameters, as shown in Table 6. If we consider, for instance, the variable avS, the mean value from the four study groups was -13.74%, with a standard deviation of 2.09, from which we can calculate the lower and upper 95% confidence intervals (respectively -9.77 and -17.71). It means that, with 95% confidence we can predict that, in the population of normal dogs enrolled in the study, the variable will fall within this interval. The results of this study suggest that, when this parameter is measured twice by the same operator, there is 95% confidence that the difference between the two measurements will range from -5.21 to 4.97. Assuming that the 95% C.I. obtained from the four study groups are a good approximation of the normal range (at least in the study population), it can be inferred that there is a high chance that repeating the measurement in a hypothetical, normal animal could “shift” the result out of the “normal” range; that is, that the intra-operator variability is greater then the apparent natural variability of the parameter. This interpretation holds true for the other parameters (avSSR, avSRE, and avSRA), although, from inspection of Table 9, it appears that some parameters performed slightly better than others. The results of study 2 suggest a relatively poor repeatability for the technique, when investigated 110 with a Bland-Altman analysis, which can be explained by the high variability of the measurements. The reproducibility analysis gave similar results (Table 10). Again, the 95% limits of agreement for the four DI parameters are wider then the estimated normal variability of each corresponding variable. Interestingly there appears not to be a significant difference between the intra-operator and inter-operator variability. Given the relatively small number of data points, the visual inspection of the plots does not provide convincing evidence of a pattern, with the exception of the plot on reproducibility of avSRE (Figure 78), which shows a tendency toward a systematic bias. Measurements taken by operator 2 tended to be consistently lower then measurements taken by operator 1. A potential explanation for the poor reproducibility in the assessment of SRE is that these deflections occur in the early diastolic phase and there is not a specific marker that enables their unequivocal identification. This is in contrast to SRA waves, which occur immediately after the P wave on the surface ECG. This reason could somewhat contribute to poor reproducibility, although it does not provide a convincing justification for the systematic bias noticed on the Bland-Altman plot, for which we do not have a good explanation. Theoretically, the adoption of a marker indicating the timing of mitral valve opening (MVO) could help improving the identification of SRE. 111 112 Conclusion Based on the results of study 1, we conclude that Doppler-derived avSSR represents a useful load-independent index of global systolic function as demonstrated in anesthetized dogs, although time-consuming in the phase of post-processing, sensitive to noise and, as described in the medical literature, highly angle-dependent. However study 2 suggests that, in a population of non-sedated dogs, with a relatively wide range of breeds and body weight, Doppler-derived DI is characterized by less than optimal levels of intraoperator and inter-operator agreement which may limit its value as a tool to evaluate myocardial function in a clinical setting. This study reports a wider intra-operator variability compared to the results published by Chetboul et al.(43) A possible explanation is that in our study repeatability was investigated in a population of 49 dogs, characterized by a wide range of breeds and body weight, while the study by Chetboul et al. assessed repeatability in a more homogeneous group of six adult Beagles. Comparisons on reproducibility cannot be made, because Chetboul et al. did not investigate inter-operator variability. The DI values obtained from group 4 (Doberman pinschers) are relatively similar to the results obtained by Wess et al.(44) However, the mean age of the dogs enrolled in the two studies was different (2.4 ± 0.84 years in study 2 and 4.3 ± 2.5 in the study by Wess et al.), potentially representing a 113 confounding variable in comparing the results of the two studies, given that the prevalence of systolic dysfunction secondary to dilated cardiomyopathy increases with age in Doberman pinschers.(60) The dogs enrolled in these studies were not randomly selected from a broader population; hence these results may not necessarily apply to a population of clinical patients. The results of study 2 are in agreement with the limitations inherent with the technique (low signal-to-noise ratio and high angle-dependence) described in the medical literature.(13) The question as to whether experience with the technique would improve its overall reliability cannot be answered by this study. However, by the time the final analysis was conducted, both operators had gained a total exposure to the technique of about two years, which, compared with the learning curve typical of other echocardiographic techniques, appears to be a reasonably appropriate time. The results of these two studies indicate that further research efforts should be finalized toward the evaluation of more sophisticated forms of DI, in particular the recently introduced two-dimensional Strain Rate Imaging (2D-SRI), based on speckletracking technology. This new imaging modality represents a non-Doppler technique, apparently non-angle dependent, more robust to noise, and characterized by better repeatability and reproducibility.(61) 114 Bibliography 1. Folland ED, Parisi AF, Moyniham PF, et al. Assessment of left ventricular ejection fraction and volumes by real-time, two-dimensional echocardiography. A comparison of cineangiographic and radionuclide techniques. Circulation 1979; 4(60): 760-766 2. Isaaz K, Thompson A, Ethevenot G, et al. Doppler echocardiographic measurements of flow velocity motion of left ventricular posterior wall. Am J Cardiol 1989; 64: 66-75 3. Sutherland GR, Stewart MJ, Groundstroem KW, et al. Color Doppler myocardial imaging: a new technique for the assessment of myocardial function. J Am Soc Echcardiogr 1994; 7: 441-45 4. Lange A, Palka P, Caso P, et al. Doppler myocardial imaging vs. B-mode grey-scale imaging: a comparative in vitro and in vivo study into their relative efficacy in endocardial boundary detection. Ultrasound Med Biol 1997; 23: 6975 5. Sohn DW, Chai IH, Lee DJ, et al. Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol 1997; 30: 474-80. 6. Nagueh SF, Mikati I, Kopelen HA, et al. Doppler estimation of left ventricular filling pressure in sinus tachycardia, a new application of tissue Doppler imaging. Circulation 1998; 98: 1644-50. 7. Nagueh S, Middleton K, Kopelen HA, et al. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 1997; 30: 1527-33 8. Oyama MA, Sisson DD, Bulmer BJ, et al. Echocardiographic estimation of mean left atrial pressure in a canine model of acute mitral valve insufficiency. J Vet Intern Med 2004; 18(5): 667-72 9. Fleming AD, McDicken WN, Sutherland GR, et al. Myocardial velocity gradients detected by Doppler imaging. Br J Radiol 1994; 67: 679-88 10. Pan C et al. Tissue tracking allows rapid and accurate visual evaluation of left ventricular function. Europ J Echocardiography 2001; 2(3): 197-202 115 11. Mirsky I, Parmley WW. Assessment of passive elastic stiffness for isolated heart muscle and the intact heart. Circ. res. 1973; 33(2): 233-43 12. Voigt JU, Flachskampf FA. Strain and strain rate. New and clinically relevant echo parameters of regional myocardial function. Z Kardiol 2004; 93: 249-58 13. Urheim S, Edvardsen T, Torp H, et al. Myocardial strain by Doppler echocardiography: validation of a new method to quantify regional myocardial function. Circulation 2000; 102: 1158-165 14. Belohlavek M, Bartleson VB, Zobitz ME. Real-time strain rate imaging:validation of peak compression and expansion rates by a tissue mimicking phantom. Echocardiography 2001; 18: 565-71 15. Heimdal A, D’Hooge J, Bijnens B, et al. In vitro validation of in-plane strain rate imaging. A new ultrasound technique for evaluating regional myocardial deformation based on tissue Doppler imaging. Echocardiography 1998; 15: S40 16. Teske AJ, De Boeck BW, Melman PG et al. Echocardiographic quantification of myocardial function using tissue deformation imaging, a guide to image acquisition and analysis using tissue Doppler and speckle tracking. Cardiovasc Ultrasound 2007; 5: 27-47 17. Greenberg NL, Firstenberg MS, Castro PL, et al. Doppler-derived myocardial systolic strain rate is a strong index of left ventricular contractility. Circulation 2002; 105: 99-105 Edvardsen T, Gerber BL, Garot J, et al. Quantitative assessment of intrinsic regional myocardial deformation by Doppler strain rate echocardiography in humans: validation against three-dimensional tagged magnetic resonance imaging. Circulation 2002; 106: 50-6 18. Tsutsui H, Uematsu M, Shimizu H, et al. Comparative usefulness of myocardial velocity gradient in detecting ischemic myocardium by a dobutamine challenge. J Am Coll Cardiol 1998; 31: 89-93 19. Armstrong G, Pasquet A, Fukamachi K, et al. Use of peak systolic strain as an index of regional left ventricular function: comparison with tissue Doppler velocity during dobutamine stress and myocardial ischemia. J Am Soc Echocardiogr 2000; 13: 731-37 116 20. Greenberg NL, Firstenberg MS, Castro PL, et al. Doppler-derived myocardial systolic strain rate is a strong index of left ventricular contractility. Circulation 2002; 105: 99-105 21. Kukulski T, Jamal F, D’Hooge J, et al.: Acute changes in systolic and diastolic events during clinical coronary angioplasty: a comparison of regional velocity, strain rate, and strain measurement. J Am Soc Echocardiogr 2002; 15: 1-12 22. Hamilton WF, Rompf JH. Movements of the base of the ventricle and relative constancy of the cardiac volume. Am J Physiol 1932; 102: 559-65 23. Hoffman EA, Ritman EL. Invariant total heart volume in the intact thorax. Am J Physiol 1985; 249: 883-90 24. Feigenbaum H, Zaky A, Nasser WK. Use of ultrasound to measure left ventricular stroke volume. Circulation 1967; 38: 1092-99 25. Jones CJH, Raposo L, Gibson DG. Functional importance of the long axis dynamics of the human left ventricle. Br Heart J 1990; 63: 215-20 26. Pai RG, Bodenheimer MM, Pai SM, Koss JH, et al. Usefulness of systolic excursion of the mitral anulus as an index of left ventricular systolic function. Am J Cardiol 1991; 67: 222-4 27. Gulati VK, Katz WE, Follansbee WP, et al. Mitral annular descent velocity by tissue Doppler echocardiography as an index of global left ventricular function. Am J Cardiol 1996; 77: 979-84 28. C Pislaru, T.P. Abraham, M Belohlavek. Strain and strain rate echocardiography. Curr Opin Cardiol 2002; 17: 443-54 29. Galiuto L, Ignone G, DeMaria AN. Contraction and relaxation velocities of the normal left ventricle using pulsed-wave tissue Doppler echocardiography. Am J Cardiol 1998; 81: 609-14 30. Edvardsen T, Gerber BL, Garot J, et al. Quantitative assessment of intrinsic regional myocardial deformation by Doppler strain rate echocardiography in humans: validation against three-dimensional tagged magnetic resonance imaging. Circulation 2002; 106: 50-6 117 31. Jamal F, Kukulski T, Strotmann J, et al. Quantification of the spectrum of changes in regional myocardial function during acute ischemia in closed chest pigs: an ultrasonic strain rate and strain study. J Am Soc Echocardiogr 2001; 4: 874-84 32. Derumeaux G, Ovize M, Loufoua J, t al. Assessment of nonuniformity of transmural myocardial velocities by color-coded tissue Doppler imaging: characterization of normal, ischemic, and stunned myocardium. Circulation 2000; 101: 1390-5 33. Weidemann F, Dommke C, Bijnens B, et al. Defining the transmurality of a chronic myocardial infarction by ultrasonic strain-rate imaging: implications for identifying intramural viability: an experimental study. Circulation 2003; 107: 883-8 34. Anagnostopoulos PC, Belohlavek M, Dzeja P, et al. Strain-rate echocardiography: a new quantitative tool for measurement of regional myocardial function during experimentally altered myocardial energetics. J Am Coll Cardiol 2001; 37(Suppl A): 443A 35. Nagueh SF, Kopelen HA, Lim DS, et al. Tissue Doppler imaging consistently detects myocardial contraction and relaxation abnormalities, irrespective of cardiac hypertrophy, in a transgenic rabbit model of human hypertrophic cardiomyopathy. Circulation 2000; 102: 1346-50 36. Nagueh SF, Bachinski LL, Meyer D, et al. Tissue Doppler imaging consistently detects myocardial abnormalities in patients with hypertrophic cardiomyopathy and provides a novel means for an early diagnosis before and independently of hypertrophy. Circulation 2001; 104: 128-30 37. Dutka DP, Donnelly E, Palka P, et al. Echocardiographic characterization of cardiomyopathy in Friedreich’s ataxia with tissue Doppler echocardiographically derived myocardial velocity gradients. Circulation 2002; 102: 1276-82 38. Takenaka K, Kuwada Y, Sonoda M, et al. Anthracycline-induced cardiomyopathies evaluated by tissue Doppler tracking system and strain rate imaging. J Cardiol 2001; 37(Suppl 1): 129-32 39. Palka P, Lange A, Donnelly JE, et al. Differentiation between restrictive cardiomyopathy and constrictive pericarditis by early diastolic Doppler myocardial velocity gradient at the posterior wall. Circulation 2000; 102: 65562 118 40. Lange A, Fleming AD, et al. Differences in myocardial velocity gradient measured throughout the cardiac cycle in patients with hypertrophic cardiomyopathy, athletes and patients with left ventricular hypertrophy due to hypertension. J Am Coll Cardiol 1997; 30: 760-8 41. Weidemann F, Eyskens B, Jamal F, et al. quantification of regional left and right ventricular radial and longitudinal function in healthy children using ultrasound-based strain rate and strain imaging. J Am Soc Echocardiogr 2002; 15: 20-8 42. Chetboul V, Carlos Semperdano C, Gouni Vassiliki, et al. Ultrasonographic assessment of regional radial and longitudinal systolic function in healthy awake dogs. J Vet Intern Med 2006; 20: 885-93 43. Wess G, Killich M, Butz, Hartmann K. Evaluaiton of the new tissue Doppler imaging methods strain and strain rate in Doberman pinschers. Abstract presented at the 16th ECVIM-CA Congress, Amsterdam, Holland, September 14 – September 16, 2006 44. Weidemann F, Jamal F, Sutherland GR, et al. Myocardial function defined by strain rate and strain during alterations in inotropic states and heart rate. Am J Physiol Heart Circ Physiol 2002; 283: H792-99 45. Egner B, Carr A, Brown S. Canine normal values. In Essential facts of blood pressure in dogs and cats. A reference guide. BE Vet Verlag, Babenhausen, 2003, pg. 12 46. Stepien RL, Rapoport GS, Henik RA, et al. Comparative diagnostic test characteristics of oscillometric and Doppler ultrasonographic methods in the detection of systolic hypertension in dogs. J Vet Intern Med. 2003; 17(1): 6572. 47. Cheitlin MD et al. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation. 2003; 108(9): 1146-62 48. Quinones MA et al. ACC/AHA clinical competence statement on echocardiography: a report of the American College of Cardiology/American Heart Association/American College of Physicians-American Society of 119 Internal Medicine Task Force on Clinical Competence. Circulation 2003; 108(9): 1146-62 49. Plumb DC. Dobutamine. In Plumb’s Veterinary Drug Handbook 5th Ed. 2005; pg. 272 50. Plumb DC. Nitroprusside. In Plumb’s Veterinary Drug Handbook 5th Ed. 2005; pg. 566 51. Plumb DC. Hetastarch. In Plumb’s Veterinary Drug Handbook 5th Ed. 2005; pg. 388 52. Margiocco ML, Bulmer BJ, Mosley CA, Sisson DD. Invasive validation of Doppler-derived strain rate imaging in anesthetized healthy adult dogs. Abstract presented at the 25th Annual ACVIM Forum, Seattle, WA, June 6 June 9, 2007 53. Storaa C. Reproducibility and Interpretation in Tissue Doppler Echocardiography, PhD dissertation. Karolinska Institutet, Division of Medical Engineering. Stockholm, 26th July 2004 54. Altman DG, Bland JM. Measurements in medicine: the analysis of method comparisons studies. The Statistician 1983; 32: 307-31 55. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307-10 56. Bland JM, Altman DG. Applying the right statistics: analyses of measurement studies. Ultrasound Obstet Gynecol 2003; 22: 85-93 57. Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet 1995; 346: 1085-7 58. Livers JJ. Some Limitations to Use of Coefficient of Variation. J of Farm Economics 1942; 24: 892-5 59. Calvert CA, Pickus CW, Jacobs GJ, et al. Signalment, survival, and prognostic factors in Doberman pinschers with end-stage cardiomyopathy. J Vet Intern Med 1997; 11: 323-6 60. Perk G, Tunick PA, Kronzon I. Non-Doppler two-dimensional strain imaging by echocardiography - from technical considerations to clinical applications. J Am Soc Echocardiogr 2007; 20(3): 234-43