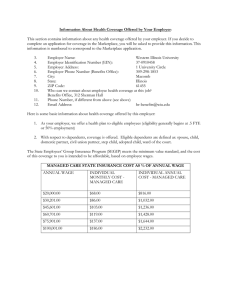
YOUR BENEFIT PLAN
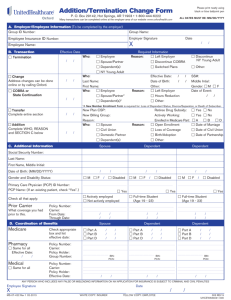
advertisement

YOUR BENEFIT PLAN Long Term Disability, Basic Term Life, Supplemental Dependent Life, Supplemental Term Life, Basic Accidental Death and Dismemberment Questions about Your Coverage In the event You have questions regarding any aspect of Your coverage, You should contact Your Employee Benefits Manager or You may write to us at: The Hartford Group Benefits Division, Customer Service P.O. Box 2999 Hartford, CT 06104-2999 Or call Us at: 1-800-523-2233 When calling, please give Us the following information: 1) the policy number; and 2) the name of the policyholder (employer or organization), as shown in Your Certificate of Insurance. Or You may contact Our Sales Office: Hartford Life and Accident Insurance Company Group Sales Department 2 Bala Plaza Suite 400 Bala Cynwyd, PA 19004 TOLL FREE: 866-610-6640 FAX: 610-538-1859 If you have a complaint, and contacts between you and the insurer or an agent or other representative of the insurer have failed to produce a satisfactory solution to the problem, the following states require we provide you with additional contact information: For Residents of: Arkansas Write Arkansas Insurance Department Consumer Services Division 1200 West Third Street Little Rock, AR 72201-1904 Telephone 1(800) 852-5494 California State of California Insurance Department Consumer Communications Bureau 300 South Spring Street, South Tower Los Angeles, CA 90013 1(800) 927-HELP Illinois Illinois Department of Insurance Consumer Services Station Springfield, Illinois 62767 Consumer Assistance: 1(866) 445-5364 Officer of Consumer Health Insurance: 1(877) 527-9431 Indiana Public Information/Market Conduct Indiana Department of Insurance 311 W. Washington St. Suite 300 Indianapolis, IN 46204-2787 Consumer Hotline: 1(800) 622-4461 1(317) 232-2395 (in the Indianapolis Area) Virginia Life and Health Division Bureau of Insurance P.O. Box 1157 Richmond, VA 23209 1(804) 371-9741 (inside Virginia) 1(800) 552-7945 (outside Virginia) Wisconsin Office of the Commissioner of Insurance Complaints Department P.O. Box 7873 Madison, WI 53707-7873 1(800) 236-8517 (outside of Madison) 1(608) 266-0103 (in Madison) to request a complaint form. The following states require that We provide these notices to You about Your coverage: For residents of: Arizona Florida Maryland Montana This certificate of insurance may not provide all benefits and protections provided by law in Arizona. Please read This certificate carefully. The benefits of the policy providing you coverage are governed primarily by the law of a state other than Florida. The group insurance policy providing coverage under this certificate was issued in a jurisdiction other than Maryland and may not provide all the benefits required by Maryland law. The benefits of the policy providing your coverage are governed primarily by the law of a state other than Montana. Georgia The laws of the state of Georgia prohibit insurers from unfairly discriminating against any person based upon his or her status as a victim of family abuse. Maine The benefits under this policy are subject to reduction due to other sources of income. This means that your benefits will be reduced by the amount of any other benefits for loss of time provided to you or for which you are eligible as a result of the same period of disability for which you claim benefits under this policy. Other sources of income are plans or arrangements of coverage that provide disability-related benefits such as Worker’s Compensation or other similar governmental programs or laws, or disability-related benefits received from your employer or as the result of your employment, membership or association with any group, union, association or other organization. Other sources of income include disability-related benefits under the United States Social Security Act or an alternate governmental plan, the Railroad Retirement Act, and other similar plans or acts. Other sources of income may also include certain disability-related or retirement benefits that you receive because of your retirement unless you were receiving them prior to becoming disabled. What comprises other sources of income under this policy is determined by the nature of the policyholder. Therefore, we strongly urge you to Read Your Certificate Carefully. A full description of the plans and types of plans considered to be other sources of income under this policy will be found in the definition of “Other Income Benefits” located in the Definitions section of your certificate. North Carolina UNDER NORTH CAROLINA GENERAL STATUTE SECTION 58-50-40, NO PERSON, EMPLOYER, FINANCIAL AGENT, TRUSTEE, OR THIRD PARTY ADMINISTRATOR, WHO IS RESPONSIBLE FOR THE PAYMENT OF GROUP LIFE INSURANCE, GROUP HEALTH OR GROUP HEALTH PLAN PREMIUMS, SHALL: 1) CAUSE THE CANCELLATION OR NONRENEWAL OF GROUP LIFE INSURANCE, GROUP HEALTH INSURANCE, HOSPITAL, MEDICAL, OR DENTAL SERVICE CORPORATION PLAN, MULTIPLE EMPLOYER WELFARE ARRANGEMENT, OR GROUP HEALTH PLAN COVERAGES AND THE CONSEQUENTIAL LOSS OF THE COVERAGES OF THE PERSON INSURED, BY WILLFULLY FAILING TO PAY THOSE PREMIUMS IN ACCORDANCE WITH THE TERMS OF THE INSURANCE OR PLAN CONTRACT; AND 2) WILLFULLY FAIL TO DELIVER, AT LEAST 45 DAYS BEFORE THE TERMINATION OF THOSE COVERAGES, TO ALL PERSONS COVERED BY THE GROUP POLICY WRITTEN NOTICE OF THE PERSON'S INTENTION TO STOP PAYMENT OF PREMIUMS. VIOLATION OF THIS LAW IS A FELONY. ANY PERSON VIOLATING THIS LAW IS ALSO SUBJECT TO A COURT ORDER REQUIRING THE PERSON TO COMPENSATE PERSONS INSURED FOR EXPENSES OR LOSSES INCURRED AS A RESULT OF THE TERMINATION OF THE INSURANCE. IMPORTANT TERMINATION INFORMATION YOUR INSURANCE MAY BE CANCELLED BY THE COMPANY. PLEASE READ THE TERMINATION PROVISION IN THIS CERTIFICATE. THIS CERTIFICATE OF INSURANCE PROVIDES COVERAGE UNDER A GROUP MASTER POLICY. THIS CERTIFICATE PROVIDES ALL OF THE BENEFITS MANDATED BY THE NORTH CAROLINA INSURANCE CODE, BUT YOU MAY NOT RECEIVE ALL OF THE PROTECTIONS PROVIDED BY A POLICY ISSUED IN NORTH CAROLINA AND GOVERNED BY ALL OF THE LAWS OF NORTH CAROLINA. PRE-EXISTING LIMITATION READ CAREFULLY NO BENEFITS WILL BE PAYABLE UNDER THIS PLAN FOR PRE-EXISTING CONDITIONS WHICH ARE NOT COVERED UNDER THE PRIOR PLAN. PLEASE READ THE LIMITATIONS IN THIS CERTIFICATE. READ YOUR CERTIFICATE CAREFULLY. IMPORTANT NOTICE Texas AVISO IMPORTANTE To obtain information or make a complaint: Para obtener informacion o para someter una queja: You may call The Hartford's toll-free telephone number for information or to make a complaint at: Usted puede llamar al numero de telefono gratis de The Hartford para informacion o para someter una queja al: 1-800-523-2233 1-800-523-2233 You may also write to The Hartford at: P.O. Box 2999 Hartford, CT 06104-2999 Usted tambien puede escribir a The Hartford: P.O. Box 2999 Hartford, CT 06104-2999 You may contact the Texas Department of Insurance to obtain information on companies, coverages, rights or complaints at: Puede comunicarse con el Departamento de Seguros de Texas para obtener informacion acerca de companias, coberturas, derechos o quejas al: 1-800-252-3439 1-800-252-3439 You may write the Texas Department of Insurance at: P.O. Box 149104 Austin, TX 78714-9410 Fax # (512) 475-1771 Web: http://www.tdi.state.tx.us E-mail: ConsumerProtection@tdi.state.tx.us Puede escribir al Departamento de Seguros de Texas: P.O. Box 149104 Austin, TX 78714-9410 Fax # (512) 475-1771 Web: http://www.tdi.state.tx.us E-mail: ConsumerProtection@tdi.state.tx.us PREMIUM OR CLAIM DISPUTES: Should you have a dispute concerning your premium or about a claim you should contact the agent or The Hartford first. If the dispute is not resolved, you may contact the Texas Department of Insurance. DISPUTAS SOBRE PRIMAS O RECLAMOS: Si tiene una disputa concerniente a su prima o a un reclamo, debe comunicarse con el agente o The Hartford primero. Si no se resuelve la disputa, puede entonces comunicarse con el departamento (TDI). THIS IS NOT A POLICY OF WORKERS' COMPENSATION INSURANCE. THE EMPLOYER DOES NOT BECOME A SUBSCRIBER TO THE WORKERS' COMPENSATION SYSTEM BY PURCHASING THIS POLICY, AND IF THE EMPLOYER IS A NON-SUBSCRIBER, THE EMPLOYER LOSES THOSE BENEFITS WHICH WOULD OTHERWISE ACCRUE UNDER THE WORKERS' COMPENSATION LAWS. THE EMPLOYER MUST COMPLY WITH THE WORKERS' COMPENSATION LAW AS IT PERTAINS TO NON-SUBSCRIBERS AND THE REQUIRED NOTIFICATIONS THAT MUST BE FILED AND POSTED. CERTIFICATE OF INSURANCE HARTFORD LIFE AND ACCIDENT INSURANCE COMPANY Simsbury, Connecticut (A stock insurance company) Policyholder: DREXEL UNIVERSITY Policy Number: GLT-395241 Policy Effective Date: January 1, 2010 Policy Anniversary Date: January 1, 2011 We have issued The Policy to the Policyholder. Our name, the Policyholder's name and The Policy Number are shown above. The provisions of The Policy, which are important to You, are summarized in this certificate consisting of this form and any additional forms which have been made a part of this certificate. This certificate replaces any other certificate We may have given to You earlier under The Policy. The Policy alone is the only contract under which payment will be made. Any difference between The Policy and this certificate will be settled according to the provisions of The Policy on file with Us at Our home office. The Policy may be inspected at the office of the Policyholder. Signed for the Company Richard G. Costello, Secretary John C. Walters, President A note on capitalization in this certificate: Capitalization of a term, not normally capitalized according to the rules of standard punctuation, indicates a word or phrase that is a defined term in The Policy or refers to a specific provision contained herein. GBD-1200 A.1 (395241) GLT 2.10 TABLE OF CONTENTS SCHEDULE OF INSURANCE...........................................................................................................................................8 Cost of Coverage ..........................................................................................................................................................8 Eligible Class(es) for Coverage......................................................................................................................................8 Eligibility Waiting Period for Coverage ...........................................................................................................................8 Benefit Amounts............................................................................................................................................................8 ELIGIBILITY AND ENROLLMENT ....................................................................................................................................9 Eligible Persons ............................................................................................................................................................9 Eligibility for Coverage...................................................................................................................................................9 Enrollment.....................................................................................................................................................................9 Evidence of Insurability................................................................................................................................................10 PERIOD OF COVERAGE ...............................................................................................................................................10 Effective Date..............................................................................................................................................................10 Deferred Effective Date ...............................................................................................................................................10 Changes in Coverage..................................................................................................................................................10 Termination .................................................................................................................................................................11 Continuation Provisions...............................................................................................................................................11 Conversion Right.........................................................................................................................................................12 BENEFITS......................................................................................................................................................................13 Disability Benefit..........................................................................................................................................................13 Mental Illness and Substance Abuse Benefits..............................................................................................................13 Family Care Credit Benefit...........................................................................................................................................15 Survivor Income Benefit...............................................................................................................................................15 Workplace Modification Benefit....................................................................................................................................16 Pension Contribution Benefit .......................................................................................................................................16 EXCLUSIONS AND LIMITATIONS .................................................................................................................................17 Pre-Existing Condition Limitation .................................................................................................................................17 GENERAL PROVISIONS................................................................................................................................................17 DEFINITIONS.................................................................................................................................................................21 AMENDATORY RIDER...................................................................................................................................................25 ERISA ............................................................................................................................................................................82 SCHEDULE OF INSURANCE The Policy of long term Disability insurance provides You with long term income protection if You become Disabled from a covered injury, Sickness or pregnancy. Cost of Coverage: You must contribute toward the cost of coverage. Eligible Class(es) for Coverage: All Full-time Active Employees and Faculty Members who are citizens or legal residents of the United States, its territories and protectorates, excluding Stationary Engineers, temporary, leased or seasonal Employees. With respect to Faculty Members: Full-time Employment: at least 12 credit hours per term or 36 credit hours per academic year With respect to all other Employees: Full-time Employment: at least 40 hours weekly Annual Enrollment Period: as determined by Your Employer on a yearly basis. Eligibility Waiting Period for Coverage: None Elimination Period: 90 day(s) Maximum Monthly Benefit: $20,000 Minimum Monthly Benefit: the greater of: 1) $100; or 2) 10% of the benefit based on Monthly Income Loss before the deduction of Other Income Benefits. Benefit Percentage: 60% Maximum Duration of Benefits Maximum Duration of Benefits Table Age When Disabled Benefits Payable Prior to Age 63 To Normal Retirement Age or 48 months, if greater To Normal Retirement Age or 42 months, if greater 36 months 30 months 27 months 24 months 21 months 18 months Age 63 Age 64 Age 65 Age 66 Age 67 Age 68 Age 69 and over Normal Retirement Age means the Social Security Normal Retirement Age as stated in the 1983 revision of the United States Social Security Act. It is determined by Your date of birth as follows: 8 Year of Birth Normal Retirement Age 1937 or before 1938 1939 1940 1941 1942 1943 thru 1954 1955 1956 1957 1958 1959 1960 or after 65 65 + 2 months 65 + 4 months 65 + 6 months 65 + 8 months 65 + 10 months 66 66 + 2 months 66 + 4 months 66 + 6 months 66 + 8 months 66 + 10 months 67 Additional Benefit Family Care Credit Benefit see Benefit Survivor Income Benefit see Benefit Workplace Modification Benefit see Benefit Pension Contribution Benefit see Benefit ELIGIBILITY AND ENROLLMENT Eligible Persons: Who is eligible for coverage? All persons in the class or classes shown in the Schedule of Insurance will be considered Eligible Persons. Eligibility for Coverage: When will I become eligible? You will become eligible for coverage on the later of: 1) the Policy Effective Date; or 2) the date You complete the Eligibility Waiting Period for Coverage shown in the Schedule of Insurance, if applicable. Enrollment: How do I enroll for coverage? To enroll for coverage you must: 1) complete and sign a group insurance enrollment form which is satisfactory to Us; and 2) deliver it to Your Employer. You have the option to enroll electronically. Your Employer will provide instructions. If You do not enroll within 31 days after becoming eligible under The Policy, or if You were eligible to enroll under the Prior Policy and did not do so, and later choose to enroll: 1) You must give Us Evidence of Insurability satisfactory to Us; and 2) You may only enroll: a) during an Annual Enrollment Period designated by the Policyholder; or b) within 31 days of the date You have a Change in Family Status. The dates of the Annual Enrollment Period are shown in the Schedule of Insurance. 9 Evidence of Insurability: What is Evidence of Insurability? Evidence of Insurability must be satisfactory to Us and may include, but will not be limited to: 1) a completed and signed application approved by Us; 2) a medical examination; 3) attending Physician’s statement; and 4) any additional information We may require. All Evidence of Insurability will be furnished at Your expense. We will then determine if You are insurable under The Policy. Change in Family Status: What constitutes a Change in Family Status? A Change in Family Status occurs when: 1) You get married or You execute a domestic partner affidavit; 2) You and Your spouse divorce or You terminate a domestic partnership; 3) Your child is born or You adopt or become the legal guardian of a child; 4) Your spouse or domestic partner dies; 5) Your child is no longer financially dependent on You or dies; 6) Your spouse is no longer employed, which results in a loss of group insurance; or 7) You have a change in classification from part-time to full-time or from full-time to part-time. PERIOD OF COVERAGE Effective Date: When does my coverage start? Your coverage will start on the earliest of: 1) the date You become eligible, if You enroll or have enrolled by then; or 2) the date on which You enroll, if You do so within 31 days after the date You are eligible; or 3) the date We approve Your Evidence of Insurability, for benefit amounts requiring Evidence of Insurability; or 4) the January 1st following the Annual Enrollment Period if You enroll, during an Annual Enrollment Period. Deferred Effective Date: When will my effective date for coverage or a change in my coverage be deferred? If You are absent from work due to: 1) accidental bodily injury; 2) sickness; 3) Mental Illness; 4) Substance Abuse; or 5) pregnancy; on the date Your insurance, or increase in coverage, would otherwise have become effective, Your insurance, or increase in coverage will not become effective until You are Actively at Work one full day. Changes in Coverage: Can I change my benefit options? You may change Your benefit option only: 1) during an Annual Enrollment Period; or 2) within 31 days of a Change in Family Status. At such time You may decrease coverage, or increase coverage to a higher option. An increase in coverage will be subject to Your submission of an application that meets Our approval. When will a requested change in benefit option take effect? If You enroll for a change in benefit option during an Annual Enrollment Period, the change will take effect on the later of: 1) January 1st following the Annual Enrollment Period; or 2) the date We approve Your Evidence of Insurability if You are required to submit Evidence of Insurability. If You enroll for a change in benefit option within 31 days following a Change in Family Status, the change will take effect on the later of: 1) the first of the month following the date You enroll for the change; or 2) the date We approve Your Evidence of Insurability if You are required to submit Evidence of Insurability. Any such increase in coverage is subject to the following provisions: 10 1) Deferred Effective Date; and 2) Pre existing Conditions Limitations. Do coverage amounts change if there is a change in my class or my rate of pay? Your coverage may increase or decrease on the date there is a change in Your class or Pre-disability Earnings. However, no increase in coverage will be effective unless on that date You: 1) are an Active Employee; and 2) are not absent from work due to being Disabled. If You were so absent from work, the effective date of such increase will be deferred until You are Actively at Work for one full day. No change in Your Pre-disability Earnings will become effective until the date We receive notice of the change. What happens if the Employer changes The Policy? Any increase or decrease in coverage because of a change in The Policy will become effective on the date of the change, subject to the following provisions: 1) Deferred Effective Date; and 2) Pre existing Conditions Limitations. Continuity From A Prior Policy: Is there continuity of coverage from a Prior Policy? If You were: 1) insured under the Prior Policy; and 2) not eligible to receive benefits under the Prior Policy; on the day before the Policy Effective Date, the Deferred Effective Date provision will not apply. Is my coverage under The Policy subject to the Pre-existing Condition Limitation? If You become insured under The Policy on the Policy Effective Date and were covered under the Prior Policy on the day before the Policy Effective Date, the Pre-existing Conditions Limitation will end on the earliest of: 1) the Policy Effective Date, if Your coverage for the Disability was not limited by a pre-existing condition restriction under the Prior Policy; or 2) the date the restriction would have ceased to apply had the Prior Policy remained in force, if Your coverage was limited by a pre-existing condition limitation under the Prior Policy. The amount of the Monthly Benefit payable for a Pre-existing Condition in accordance with the above paragraph will be the lesser of: 1) the Monthly Benefit which was paid by the Prior Policy; or 2) the Monthly Benefit provided by The Policy. The Pre-existing Conditions Limitation will apply after the Policy Effective Date to the amount of a benefit increase which results from a change from the Prior Policy to The Policy, a change in benefit options, a change of class or a change in The Policy. Do I have to satisfy an Elimination Period under The Policy if I was Disabled under the Prior Policy? If You received Monthly benefits for disability under the Prior Policy, and You returned to work as a Full-time Active Employee before The Policy Effective Date, then, if within 6 months of Your return to work: 1) You have a recurrence of the same disability while covered under The Policy; and 2) there are no benefits available for the recurrence under the Prior Policy; the Elimination Period, which would otherwise apply, will be waived if the recurrence would have been covered without any further elimination period under the Prior Policy. Termination: When will my coverage end? Your coverage will end on the earliest of the following: 1) the date The Policy terminates; 2) the date The Policy no longer insures Your class; 3) the date the premium payment is due but not paid; 4) the last day of the period for which You make any required premium contribution; 5) the date Your Employer terminates Your employment; or 6) the date You cease to be a Full time Active Employee in an eligible class for any reason; unless continued in accordance with any of the Continuation Provisions. Continuation Provisions: Can my coverage be continued beyond the date it would otherwise terminate? 11 Coverage can be continued by Your Employer beyond a date shown in the Termination provision, if Your Employer provides a plan of continuation which applies to all employees the same way. Continued coverage: 1) is subject to any reductions in The Policy; 2) is subject to payment of premium by the Employer; and 3) terminates if: a) The Policy terminates; or b) coverage for Your class terminates. In any event, Your benefit level, or the amount of earnings upon which Your benefits may be based, will be that in effect on the day before Your coverage was continued. Coverage may be continued in accordance with the above restrictions and as described below: Leave of Absence: If You are on a documented leave of absence, other than Family or Medical Leave, that is on file with the Employer, all of Your coverage may be continued for a period of time, not to exceed 36 months. If the leave terminates prior to the agreed upon date, this continuation will cease immediately. Lay-off: If You are temporarily laid off by the Employer due to lack of work, Your coverage may be continued for 60 day(s) after the lay-off commenced. If the lay-off becomes permanent, this continuation will cease immediately. Family Medical Leave: If You are granted a leave of absence, in writing, according to the Family and Medical Leave Act of 1993, or other applicable state or local law, Your coverage may be continued for up to 12 weeks, or 26 weeks if You qualify for Family Military Leave, or longer if required by other applicable law, following the date Your leave commenced. If the leave terminates prior to the agreed upon date, this continuation will cease immediately. Sabbatical: If You are on a documented paid sabbatical, that is on file with the Employer, Your coverage may be continued for a period of time, not to exceed 36 month(s) after the sabbatical commenced. If the sabbatical terminates prior to the agreed upon date, this continuation will cease immediately. Coverage while Disabled: Does my insurance continue while I am Disabled and no longer an Active Employee? If You are Disabled and You cease to be an Active Employee, Your insurance will be continued: 1) during the Elimination Period while You remain Disabled by the same Disability; and 2) after the Elimination Period for as long as You are entitled to benefits under The Policy. Waiver of Premium: Am I required to pay Premiums while I am Disabled? No premium will be due for You: 1) after the Elimination Period; and 2) for as long as benefits are payable. Extension of Benefits for Total Disability: Do my benefits continue if The Policy terminates? If You are entitled to benefits while Disabled and The Policy terminates, benefits: 1) will continue as long as You remain Disabled by the same Disability; but 2) will not be provided beyond the date We would have ceased to pay benefits had the insurance remained in force. Termination of The Policy for any reason will have no effect on Our liability under this provision. Conversion Right: If my coverage under The Policy ends, do I have a right to conversion? If Your insurance terminates because: 1) Your employment ends for a reason other than Your retirement; or 2) You are no longer in an eligible class; and if: 1) You have been continuously insured for at least 12 consecutive month(s) under The Policy or under both The Policy and the Prior Policy; 2) a Disability is not preventing You from performing duties of Your Occupation; 3) The Policy has not terminated; and 4) You are not eligible or covered for similar benefits under another group Policy or an individual policy; then You are eligible to enroll for personal insurance under another group policy called the group long term disability conversion policy. How do I convert my Coverage? To obtain coverage under the group long term disability conversion Policy, You must: 1) send Us a written enrollment request; and 12 2) pay the required premium and enrollment fee for the conversion Policy; within 31 days of the termination of Your insurance. If You meet the preceding conditions, We will issue You a certificate of insurance under the group long term disability conversion Policy. Such coverage will: 1) be issued without Evidence of Insurability; 2) be on one of the forms then being issued by Us for conversion purposes; and 3) be effective on the day following the date Your insurance under The Policy terminates. The coverage available under the conversion Policy may differ from The Policy. We will determine the terms of the group long term disability conversion Policy, including: 1) the type and amount of coverage provided; and 2) the premium payable; based on the kinds of insurance provided by the group long term disability conversion Policy at the time such enrollment request is made. BENEFITS Disability Benefit: What are my Disability Benefits under The Policy? We will pay You a Monthly Benefit if You: 1) become Disabled while insured under The Policy; 2) are Disabled throughout the Elimination Period; 3) remain Disabled beyond the Elimination Period; and 4) submit Proof of Loss to Us. Benefits accrue as of the first day after the Elimination Period and are paid monthly. However, benefits will not exceed the Maximum Duration of Benefits. Mental Illness Benefits: Are benefits limited for Mental Illness? If You are Disabled because of: 1) Mental Illness that results from any cause; 2) any condition that may result from Mental Illness; then, subject to all other provisions of The Policy, We will limit the Maximum Duration of Benefits. Benefits will be payable: 1) for as long as you are confined in a hospital or other place licensed to provide medical care for the disabling condition; or 2) if not confined, or after you are discharged and still Disabled, for a total of 24 month(s) for all such disabilities during your lifetime. Recurrent Disability: What happens if I Recover but become Disabled again? Periods of Recovery during the Elimination Period will not interrupt the Elimination Period, if the number of days You return to work as an Active Employee are equal to 14 days. Any day within such period of Recovery, will not count toward the Elimination Period. After the Elimination Period, if You return to work as an Active Employee and then become Disabled and such Disability is: 1) due to the same cause; or 2) due to a related cause; and 3) within 12 months of the return to work; the Period of Disability prior to Your return to work and the recurrent Disability will be considered one Period of Disability, provided The Policy remains in force. If You return to work as an Active Employee for 12 months or more, any recurrence of a Disability will be treated as a new Disability. The new Disability is subject to a new Elimination Period and a new Maximum Duration of Benefits. Period of Disability means a continuous length of time during which You are Disabled under The Policy. Recover or Recovery means that You are no longer Disabled and have returned to work with the Employer and premiums are being paid for You. 13 Calculation of Monthly Benefit: Return to Work Incentive: How are my Disability benefits calculated? If You remain Disabled after the Elimination Period, but work while You are Disabled, We will determine Your Monthly Benefit for a period of up to 12 consecutive months as follows: 1) multiply Your Pre-disability Earnings by the Benefit Percentage; 2) compare the result with the Maximum Benefit; and 3) from the lesser amount, deduct Other Income Benefits. The result is Your Monthly Benefit. Current Monthly Earnings will not be used to reduce Your Monthly Benefit. However, if the sum of Your Monthly Benefit and Your Current Monthly Earnings exceeds 100% of Your Pre-disability Earnings, We will reduce Your Monthly Benefit by the amount of excess. The 12 consecutive month period will start on the last to occur of: 1) the day You first start work; or 2) the end of the Elimination Period. If You are Disabled and not receiving benefits under the Return to Work Incentive, We will calculate Your Monthly Benefit as follows: 1) multiply Your Monthly Income Loss by the Benefit Percentage; 2) compare the result with the Maximum Benefit; and 3) from the lesser amount, deduct Other Income Benefits. The result is Your Monthly Benefit. Calculation of Monthly Benefit: What happens if the sum of my Monthly Benefit, Current Monthly Earnings and Other Income Benefits exceeds 100% of my Pre-disability Earnings? If the sum of Your Monthly Benefit, Current Monthly Earnings and Other Income Benefits exceeds 100% of Your Predisability Earnings, We will reduce Your Monthly Benefit by the amount of the excess. However, Your Monthly Benefit will not be less than the Minimum Monthly Benefit. If an overpayment occurs, We may recover all or any portion of the overpayment, in accordance with the Overpayment Recovery provision. Minimum Monthly Benefit: Is there a Minimum Monthly Benefit? Your Monthly Benefit will not be less than the Minimum Monthly Benefit shown in the Schedule of Insurance. Partial Month Payment: How is the benefit calculated for a period of less than a month? If a Monthly Benefit is payable for a period of less than a month, we will pay 1/30 of the Monthly Benefit for each day You were Disabled. Termination of Payment: When will my benefit payments end? Benefit payments will stop on the earliest of: 1) the date You are no longer Disabled; 2) the date You fail to furnish Proof of Loss; 3) the date You are no longer under the Regular Care of a Physician; 4) the date You refuse Our request that You submit to an examination by a Physician or other qualified medical professional; 5) the date of Your death; 6) the date You refuse to receive recommended treatment that is generally acknowledged by Physicians to cure, correct or limit the disabling condition; 7) the last day benefits are payable according to the Maximum Duration of Benefits Table; or 8) the date Your Current Monthly Earnings exceed: a) 80% of Your Indexed Pre-disability Earnings if You are receiving benefits for being Disabled from Your Occupation; or b) the product of Your Indexed Pre-disability Earnings and the Benefit percentage if You are receiving benefits for being Disabled from Any Occupation; 9) the date no further benefits are payable under any provision in The Policy that limits benefit duration; 10) the date You refuse to participate in a Rehabilitation program, or refuse to cooperate with or try: a) modifications made to the work site or job process to accommodate Your identified medical limitations to enable You to perform the Essential Duties of Your Occupation; b) adaptive equipment or devices designed to accommodate Your identified medical limitations to enable You to perform the Essential Duties of Your Occupation; 14 c) modifications made to the work site or job process to accommodate Your identified medical limitations to enable You to perform the Essential Duties of Any Occupation, if You were receiving benefits for being disabled from Any Occupation; or d) adaptive equipment or devices designed to accommodate Your identified medical limitations to enable You to perform the Essential Duties of Any Occupation, if You were receiving benefits for being disabled from Any Occupation; provided a qualified Physician or other qualified medical professional agrees that such modifications, Rehabilitation program or adaptive equipment accommodate Your medical limitation. Family Care Credit Benefit: What if I must incur expenses for Family Care Services in order to participate in a Rehabilitation program? If You are working as part of a program of Rehabilitation, We will, for the purpose of calculating Your benefit, deduct the cost of Family Care from earnings received from work as a part of a program of Rehabilitation, subject to the following limitations: 1) Family Care means the care or supervision of: a) Your children under age 13; or b) a member of Your household who is mentally or physically handicapped and dependent upon You for support and maintenance; 2) the maximum monthly deduction allowed for each qualifying child or family member is: a) $350 during the first 12 months of Rehabilitation; and b) $175 thereafter; but in no event may the deduction exceed the amount of Your monthly earnings; 3) Family Care Credits may not exceed a total of $2,500 during a calendar year; 4) the deduction will be reduced proportionally for periods of less than a month; 5) the charges for Family Care must be documented by a receipt from the caregiver; 6) the credit will cease on the first to occur of the following: a) You are no longer in a Rehabilitation program; or b) Family Care Credits for 24 months have been deducted during Your Disability; and 7) no Family Care provided by someone Related to the family member receiving the care will be eligible as a deduction under this provision. Your Current Monthly Earnings after the deduction of Your Family Care Credit will be used to determine Your Monthly Income Loss. In no event will You be eligible to receive a Monthly Benefit under The Policy if Your Current Monthly Earnings before the deduction of the Family Care Credit exceed 80% of Your Indexed Pre-disability Earnings. Survivor Income Benefit: Will my survivors receive a benefit if I die while receiving Disability Benefits? If You were receiving a Monthly Disability Benefit at the time of Your death, We will pay a Survivor Income Benefit, when We receive proof satisfactory to Us: 1) of Your death; and 2) that the person claiming the benefit is entitled to it. We must receive the satisfactory proof for Survivor Income Benefits within 1 year of the date of Your death. The Survivor Income Benefit will only be paid: 1) to Your Surviving Spouse; or 2) if no Surviving Spouse, in equal shares to Your Surviving Children. If there is no Surviving Spouse or Surviving Children, then no benefit will be paid. However, We will first apply the Survivor Income Benefit to any overpayment which may exist on Your claim. The Survivor Income Benefit is calculated as 3 times the lesser of: 1) Your Monthly Income Loss multiplied by the Benefit Percentage in effect on the date of Your death; or 2) The Maximum Monthly Benefit. Surviving Spouse means Your wife or husband who was not legally separated or divorced from You when You died. “Spouse” will include Your domestic partner, provided You have executed a domestic partner affidavit acceptable to us, establishing that You and Your partner are domestic partners for purposes of The Policy. You will continue to be considered domestic partners provided You continue to meet the requirements described in the domestic partner affidavit. Surviving Children means Your unmarried children, step children, legally adopted children who, on the date You die, are primarily dependent on You for support and maintenance and who are under age 23. 15 The term Surviving Children will also include any other children related to You by blood or marriage or domestic partnership and who: 1) lived with You in a regular parent-child relationship; and 2) were eligible to be claimed as dependents on Your federal income tax return for the last tax year prior to Your death. If a minor child is entitled to benefits, We may, at Our option, make benefit payments to the person caring for and supporting the child until a legal guardian is appointed. Workplace Modification Benefit: Will the Rehabilitation program provide for modifications to my workplace to accommodate my return to work? We will reimburse Your Employer for the expense of reasonable Workplace Modifications to accommodate Your Disability and enable You to return to work as an Active Employee. You qualify for this benefit if: 1) Your Disability is covered by The Policy; 2) the Employer agrees to make modifications to the workplace in order to reasonably accommodate Your return to work and the performance of the Essential Duties of Your job; and 3) We approve, in writing, any proposed Workplace Modifications. Benefits paid for such workplace modification shall not exceed the amount equal to the amount of the Maximum Monthly Benefit. We have the right, at Our expense, to have You examined or evaluated by: 1) a Physician or other health care professional; or 2) a vocational expert or rehabilitation specialist; of Our choice so that We may evaluate the appropriateness of any proposed modification. We will reimburse the Employer's costs for approved Workplace Modifications after: 1) the proposed modifications made on Your behalf are complete; 2) We have been provided written proof of the expenses incurred to provide such modification; and 3) You have returned to work as an Active Employee. Workplace Modification means change in Your work environment, or in the way a job is performed, to allow You to perform, while Disabled, the Essential Duties of Your job. Payment of this benefit will not reduce or deny any benefit You are eligible to receive under the terms of The Policy. Pension Contribution Benefit: Does this Policy also cover contributions to a Pension Plan? If You: 1) become Disabled while You are covered under this Pension Contribution Benefit; 2) remain Disabled for 365 day(s) of one continuous period of Disability; and 3) are receiving a Monthly Benefit under The Policy; We will pay a monthly Pension Contribution Benefit to the trustee or administrator of Your Pension Plan for deposit to Your pension account. The Pension Contribution Benefit will be the least of: 1) Age 39 & under = 9%; Age 40 - 49 = 11%; Age 50 & over = 13% of Your monthly Pre-disability Earnings; 2) $1,950; 3) the amount of the average monthly tax deferred contributions the Employer made to Your Pension Plan during the 12 calendar months prior to becoming Disabled. We will make payments under this benefit according to the rules and regulations of the Internal Revenue Service and the provisions of Your Pension Plan. We will make any such payment that cannot be paid to the trustee or administrator of Your Pension Plan to a deferred annuity account designated by You. No Pension Contribution Benefit will be payable after Your Monthly Benefit terminates. Pension Plan means, for the purpose of this Pension Contribution Benefit, a qualified defined contribution pension Plan, profit sharing Plan, or other Plan approved by Us, in which You are participating as a result of Your employment with the Employer. 16 EXCLUSIONS AND LIMITATIONS Exclusions: What Disabilities are not covered? The Policy does not cover, and We will not pay a benefit for any Disability: 1) unless You are under the Regular Care of a Physician; 2) that is caused or contributed to by war or act of war (declared or not); 3) caused by Your commission of or attempt to commit a felony; 4) caused or contributed to by Your being engaged in an illegal occupation; or 5) caused or contributed to by an intentionally self inflicted injury. If You are receiving or are eligible for benefits for a Disability under a prior disability plan that: 1) was sponsored by Your Employer; and 2) was terminated before the Effective Date of The Policy; no benefits will be payable for the Disability under The Policy. Pre-Existing Conditions Limitation: Are benefits limited for Pre-existing Conditions? We will not pay any benefit, or any increase in benefits, under The Policy for any Disability that results from, or is caused or contributed to by, a Pre-existing Condition, unless, at the time You become Disabled You have been continuously insured under The Policy for 365 consecutive day(s). Pre existing Condition means: 1) any accidental bodily injury, sickness, Mental Illness, pregnancy, or episode of Substance Abuse; or 2) any manifestations, symptoms, findings, or aggravations related to or resulting from such accidental bodily injury, sickness, Mental Illness, pregnancy, or Substance Abuse; for which You received Medical Care during the 90 day(s) period that ends the day before: 1) Your effective date of coverage; or 2) the effective date of a Change in Coverage. Medical Care is received when a physician or other health care provider: 1) is consulted or gives medical advice; or 2) recommends, prescribes or provides Treatment. Treatment includes, but is not limited to: 1) medical examinations, tests, attendance, or observation; and 2) use of drugs, medicines, medical services, supplies or equipment. GENERAL PROVISIONS Notice of Claim: When should I notify the Company of a claim? You must give Us, written notice of a claim within 30 days after Disability or loss occurs. If notice cannot be given within that time, it must be given as soon as reasonably possible after that. Such notice must include Your name, Your address and the Policy Number. Claim Forms: Are special forms required to file a claim? We will send forms to You to provide Proof of Loss, within 15 days of receiving a Notice of Claim. If We do not send the forms within 15 days, You may submit any other written proof which fully describes the nature and extent of Your claim. Proof of Loss: What is Proof of Loss? Proof of Loss may include but is not limited to the following: 1) documentation of: a) the date Your Disability began; b) the cause of Your Disability; c) the prognosis of Your Disability; d) Your Pre-disability Earnings, Current Monthly Earnings or any income, including but not limited to copies of Your filed and signed federal and state tax returns; and e) evidence that You are under the Regular Care of a Physician; 2) any and all medical information, including x-ray films and photocopies of medical records, including histories, physical, mental or diagnostic examinations and treatment notes; 17 3) the names and addresses of all: a) Physicians or other qualified medical professionals You have consulted; b) hospitals or other medical facilities in which You have been treated; and c) pharmacies which have filled Your prescriptions within the past three years; 4) Your signed authorization for Us to obtain and release: a) medical, employment and financial information; and b) any other information We may reasonably require; 5) Your signed statement identifying all Other Income Benefits; and 6) proof that You and Your dependents have applied for all Other Income Benefits which are available. You will not be required to claim any retirement benefits which You may only get on a reduced basis. All proof submitted must be satisfactory to Us. Additional Proof of Loss: What additional proof of loss is the Company entitled to? To assist Us in determining if You are Disabled, or to determine if You meet any other term or condition of The Policy, We have the right to require You to: 1) meet and interview with our representative; and 2) be examined by a Physician, vocational expert, functional expert, or other medical or vocational professional of Our choice. Any such interview, meeting or examination will be: 1) at Our expense; and 2) as reasonably required by Us. Your Additional Proof of Loss must be satisfactory to Us. Unless We determine You have a valid reason for refusal, We may deny, suspend or terminate Your benefits if You refuse to be examined or meet to be interviewed by Our representative. Sending Proof of Loss: When must proof of Loss be given? Written Proof of Loss must be sent to Us within 90 days after the start of the period for which We are liable for payment. If proof is not given by the time it is due, it will not affect the claim if: 1) it was not possible to give proof within the required time; and 2) proof is given as soon as possible; but 3) not later than 1 year after it is due, unless You are not legally competent. We may request Proof of Loss throughout Your Disability. In such cases, We must receive the proof within 30 day(s) of the request. Claim Payment: When are benefit payments issued? When We determine that You; 1) are Disabled; and 2) eligible to receive benefits; We will pay accrued benefits at the end of each month that You are Disabled. We may, at Our option, make an advance benefit payment based on Our estimated duration of Your Disability. If any payment is due after a claim is terminated, it will be paid as soon as Proof of Loss satisfactory to Us is received. Claims to be Paid: To whom will benefits for my claim be paid? All payments are payable to You. Any payments owed at Your death may be paid to Your estate. If any payment is owed to: 1) Your estate; 2) a person who is a minor; or 3) a person who is not legally competent; then We may pay up to $1,000 to a person who is Related to You and who, at Our sole discretion, is entitled to it. Any such payment shall fulfill Our responsibility for the amount paid. Claim Denial: What notification will I receive if my claim is denied? If a claim for benefits is wholly or partly denied, You will be furnished with written notification of the decision. This written notification will: 1) give the specific reason(s) for the denial; 2) make specific reference to The Policy provisions on which the denial is based; 3) provide a description of any additional information necessary to perfect a claim and an explanation of why it is necessary; and 4) provide an explanation of the review procedure. 18 Claim Appeal: What recourse do I have if my claim is denied? On any claim, You or Your representative may appeal to Us for a full and fair review. To do so You: 1) must request a review upon written application within: a) 180 days of receipt of claim denial if the claim requires Us to make a determination of disability; or b) 60 days of receipt of claim denial if the claim does not require Us to make a determination of disability; and 2) may request copies of all documents, records, and other information relevant to Your claim; and 3) may submit written comments, documents, records and other information relating to Your claim. We will respond to You in writing with Our final decision on the claim. Social Security: When must I apply for Social Security Benefits? You must apply for Social Security disability benefits when the length of Your Disability meets the minimum duration required to apply for such benefits. You must apply within 45 days from the date of Our request. If the Social Security Administration denies Your eligibility for benefits, You will be required: 1) to follow the process established by the Social Security Administration to reconsider the denial; and 2) if denied again, to request a hearing before an Administrative Law Judge of the Office of Hearing and Appeals. Benefit Estimates: How does the Company estimate Disability benefits under the United States Social Security Act? We reserve the right to reduce Your Monthly Benefit by estimating the Social Security disability benefits You or Your spouse and children may be eligible to receive. When We determine that You or Your Dependent may be eligible for benefits, We may estimate the amount of these benefits. We may reduce Your Monthly Benefit by the estimated amount. Your Monthly Benefit will not be reduced by estimated Social Security disability benefits if: 1) You apply for Social Security disability benefits and pursue all required appeals in accordance with the Social Security provision; and 2) You have signed a form authorizing the Social Security Administration to release information about awards directly to Us; and 3) You have signed and returned Our reimbursement agreement, which confirms that You agree to repay all overpayments. If We have reduced Your Monthly Benefit by an estimated amount and: 1) You or Your Dependent are later awarded Social Security disability benefits, We will adjust Your Monthly Benefit when We receive proof of the amount awarded, and determine if it was higher or lower than Our estimate; or 2) Your application for disability benefits has been denied, We will adjust Your Monthly Benefit when You provide Us proof of final denial from which You cannot appeal from an Administrative Law Judge of the Office of Hearing and Appeals. If Your Social Security Benefits were lower than we estimated, and We owe You a refund, We will make such refund in a lump sum. If Your Social Security Benefits were higher than we estimated, and If Your Monthly Benefit has been overpaid, You must make a lump sum refund to Us equal to all overpayments, in accordance with the Overpayment Recovery provision Overpayment: When does an overpayment occur? An overpayment occurs: 1) when We determine that the total amount We have paid in benefits is more than the amount that was due to You under The Policy; or 2) when payment is made by Us that should have been made under another group policy. This includes, but is not limited to, overpayments resulting from: 1) retroactive awards received from sources listed in the Other Income Benefits definition; 2) failure to report, or late notification to Us of any Other Income Benefit(s) or earned income; 3) misstatement; 4) fraud; or 5) any error We may make. Overpayment Recovery: How does the Company exercise the right to recover overpayments? We have the right to recover from You any amount that We determine to be an overpayment. You have the obligation to refund to Us any such amount. Our rights and Your obligations in this regard may also be set forth in the reimbursement agreement You will be required to sign when You become eligible for benefits under The Policy. 19 If benefits are overpaid on any claim, You must reimburse Us within 30 days. If reimbursement is not made in a timely manner, We have the right to: 1) recover such overpayments from: a) You; b) any other organization; c) any other insurance company; d) any other person to or for whom payment was made; and e) Your estate; 2) reduce or offset against any future benefits payable to You or Your survivors, including the Minimum Monthly Benefit, until full reimbursement is made. Payments may continue when the overpayment has been recovered; 3) refer Your unpaid balance to a collection agency; and 4) pursue and enforce all legal and equitable rights in court. Subrogation: What are the Company’s subrogation rights? If You: 1) suffer a Disability because of the act or omission of a Third Party; 2) become entitled to and are paid benefits under The Policy in compensation for lost wages; and 3) do not initiate legal action for the recovery of such benefits from the Third Party in a reasonable period of time; then We will be subrogated to any rights You may have against the Third Party and may, at Our option, bring legal action against the Third Party to recover any payments made by Us in connection with the Disability. Reimbursement: What are the Company’s Reimbursement Rights? We have the right to request to be reimbursed for any benefit payments made or required to be made under The Policy for a Disability for which You recover payment from a Third Party. If You recover payment from a Third Party as: 1) a legal judgment; 2) an arbitration award; or 3) a settlement or otherwise; You must reimburse Us for the lesser of: 1) the amount of payment made or required to be made by Us; or 2) the amount recovered from the Third Party less any reasonable legal fees associated with the recovery. Third Party means any person or legal entity whose act or omission, in full or in part, causes You to suffer a Disability for which benefits are paid or payable under The Policy. Legal Actions: When can legal action be taken against Us? Legal action cannot be taken against Us: 1) sooner than 60 days after the date proof of loss is given; or 2) more than 3 years after the date Proof of Loss is required to be given according to the terms of The Policy. Insurance Fraud: How does the Company deal with fraud? Insurance Fraud occurs when You and/or Your Employer provide Us with false information or file a claim for benefits that contains any false, incomplete or misleading information with the intent to injure, defraud or deceive Us. It is a crime if You and/or Your Employer commit Insurance Fraud. We will use all means available to Us to detect, investigate, deter and prosecute those who commit Insurance Fraud. We will pursue all available legal remedies if You and/or Your Employer perpetrate Insurance Fraud. Misstatements: What happens if facts are misstated? If material facts about You were not stated accurately: 1) Your premium may be adjusted; and 2) the true facts will be used to determine if, and for what amount, coverage should have been in force. No statement, except fraudulent misstatements, made by You relating to Your insurability will be used to contest the insurance for which the statement was made after the insurance has been in force for two years during Your lifetime. In order to be used, the statement must be in writing and signed by You. Policy Interpretation: Who interprets the terms and conditions of The Policy? 20 We have full discretion and authority to determine eligibility for benefits and to construe and interpret all terms and provisions of The Policy. This provision applies where the interpretation of The Policy is governed by the Employee Retirement Income Security Act of 1974, as amended (ERISA). DEFINITIONS Actively at Work means at work with the Employer on a day that is one of the Employer's scheduled workdays. On that day, You must be performing for wage or profit all of the regular duties of Your Occupation: 1) in the usual way; and 2) for Your usual number of hours. If school is not in session due to normal vacation or school break(s), Actively at Work shall mean You are able to report for work with the Employer, performing all the regular duties of Your Occupation in the usual way for Your usual number of hours as if school was in session. Active Employee means an Employee who works for the Employer on a regular basis in the usual course of the Employer's business. This must be at least the number of hours shown in the Schedule of Insurance. Any Occupation means any occupation for which You are qualified by education, training or experience, and that has an earnings potential greater than the lesser of: 1) the product of Your Indexed Pre-disability Earnings and the Benefit Percentage; or 2) the Maximum Monthly Benefit. Current Monthly Earnings means monthly earnings You receive from: 1) Your Employer; and 2) other employment; while You are Disabled. Disability or Disabled means You are prevented from performing one or more of the Essential Duties of: 1) Your Occupation during the Elimination Period; 2) Your Occupation, for the 24 month(s) following the Elimination Period, and as a result Your Current Monthly Earnings are less than 80% of Your Indexed Pre-disability Earnings; and 3) after that, Any Occupation. If at the end of the Elimination Period, You are prevented from performing one or more of the Essential Duties of Your Occupation, but Your Current Monthly Earnings are greater than 80% of Your Pre-disability Earnings, Your Elimination Period will be extended for a total period of 12 months from the original date of Disability, or until such time as Your Current Monthly Earnings are less than 80% of Your Pre-disability Earnings, whichever occurs first. Your Disability must result from: 1) accidental bodily injury; 2) sickness; 3) Mental Illness; 4) Substance Abuse; or 5) pregnancy. Your failure to pass a physical examination required to maintain a license to perform the duties of Your Occupation, alone, does not mean that You are Disabled. Elimination Period means the longer of the number of consecutive days at the beginning of any one period of Disability which must elapse before benefits are payable or the expiration of any Employer sponsored short term Disability benefits or salary continuation program, excluding benefits required by state law. Employer means the Policyholder. Indexed Pre-disability Earnings means Your Pre-disability Earnings adjusted annually by adding the lesser of: 1) 10%; or 2) the percentage change in the Consumer Price Index (CPI-W). 21 The percentage change in the CPI-W means the difference between the current year's CPI-W as of July 31, and the prior year's CPI-W as of July 31, divided by the prior year's CPI-W. The adjustment is made January 1st each year after You have been Disabled for 12 consecutive month(s), provided You are receiving benefits at the time the adjustment is made. The term Consumer Price Index (CPI-W) means the index for Urban Wage Earners and Clerical Workers published by the United States Department of Labor. It measures on a periodic (usually monthly) basis the change in the cost of typical urban wage earners' and clerical workers' purchase of certain goods and services. If the index is discontinued or changed, We may use another nationally published index that is comparable to the CPI-W. Mental Illness means a mental disorder as listed in the current version of the Diagnostic and Statistical Manual of Mental Disorders, published by the American Psychiatric Association. A Mental Illness may be caused by biological factors or result in physical symptoms or manifestations. For the purpose of The Policy, Mental Illness does not include the following mental disorders outlined in the Diagnostic and Statistical Manual of Mental Disorders: 1) Mental Retardation; 2) Pervasive Developmental Disorders; 3) Motor Skills Disorder; 4) Substance-Related Disorders; 5) Delirium, Dementia, and Amnesic and Other Cognitive Disorders; or 6) Narcolepsy and Sleep Disorders related to a General Medical Condition. Monthly Benefit means a monthly sum payable to You while You are Disabled, subject to the terms of The Policy. Monthly Income Loss means Your Pre-disability Earnings minus Your Current Monthly Earnings. Other Income Benefits means the amount of any benefit for loss of income, provided to You or Your family, as a result of the period of Disability for which You are claiming benefits under The Policy. This includes any such benefits for which You or Your family are eligible or that are paid to You, or Your family or to a third party on Your behalf, pursuant to any: 1) temporary, permanent disability, or impairment benefits under a Workers' Compensation Law, the Jones Act, occupational disease law, similar law or substitutes or exchanges for such benefits; 2) governmental law or program that provides disability or unemployment benefits as a result of Your job with Your Employer; 3) plan or arrangement of coverage, whether insured or not, which is received from Your Employer as a result of employment by or association with Your Employer or which is the result of membership in or association with any group, association, union or other organization; 4) disability benefits under: a) the United States Social Security Act or alternative plan offered by a state or municipal government; b) the Railroad Retirement Act; c) the Canada Pension Plan, the Canada Old Age Security Act, the Quebec Pension Plan or any provincial pension or disability plan; or d) similar plan or act; that You, Your spouse and/or children, are eligible to receive because of Your Disability; or 5) disability benefit from the Department of Veterans Affairs, or any other foreign or domestic governmental agency: a) that begins after You become Disabled; or b) that You were receiving before becoming Disabled, but only as to the amount of any increase in the benefit attributed to Your Disability. Other Income Benefits also means any payments that are made to You or to Your family, or to a third party on Your behalf, pursuant to any: 1) disability benefit under Your Employer's Retirement plan; 2) temporary, permanent disability or impairment benefits under a Workers’ Compensation Law, the Jones Act, occupational disease law, similar law or substitutes or exchanges for such benefits; 3) portion of a settlement or judgment, minus associated costs, of a lawsuit that represents or compensates for Your loss of earnings; or 4) retirement benefit from a Retirement Plan that is wholly or partially funded by employer contributions, unless: a) You were receiving it prior to becoming Disabled; or b) You immediately transfer the payment to another plan qualified by the United States Internal Revenue Service for the funding of a future retirement; 22 (Other Income Benefits will not include the portion, if any, of such retirement benefit that was funded by Your after-tax contributions.); or 5) retirement benefits under: a) the United States Social Security Act or alternative plan offered by a state or municipal government; b) the Railroad Retirement Act; c) the Canada Pension Plan, the Canada Old Age Security Act, the Quebec Pension Plan or any provincial pension or disability plan; d) similar plan or act; that You, Your spouse and/or children receive because of Your retirement, unless You were receiving them prior to becoming Disabled. If You are paid Other Income Benefits in a lump sum or settlement, You must provide proof satisfactory to Us of: 1) the amount attributed to loss of income; and 2) the period of time covered by the lump sum or settlement. We will pro rate the lump sum or settlement over this period of time. If You cannot or do not provide this information, We will assume the entire sum to be for loss of income, and the time period to be 60 month(s). We may make a retroactive allocation of any retroactive Other Income Benefit. A retroactive allocation may result in an overpayment of Your claim. The amount of any increase in Other Income Benefits will not be included as Other Income Benefits if such increase: 1) takes effect after the date benefits become payable under The Policy; and 2) is a general increase which applies to all persons who are entitled to such benefits. Physician means a person who is: 1) a doctor of medicine, osteopathy, psychology or other legally qualified practitioner of a healing art that We recognize or are required by law to recognize; 2) licensed to practice in the jurisdiction where care is being given; 3) practicing within the scope of that license; and 4) not Related to You by blood or marriage. Pre-disability Earnings means Your contracted annual rate of pay from Your Employer divided by the number of pay periods occurring in the pay cycle established by You and Your Employer prior to Your date of Disability. However, if You are an hourly paid Employee, Pre-Disability Earnings means the product of: 1) the average number of hours You worked per month, not including overtime pay, over the most recent 12 month period immediately prior to the last day You were Actively at Work before You became Disabled, multiplied by: 2) Your hourly wage in effect on the last day You were Actively at Work before You became Disabled. If we determine your earnings vary substantially from month to month, we may determine Your rate of pay by averaging Your earnings over the most recent 3 months. Prior Policy means the long term disability insurance carried by the Employer on the day before the Policy Effective Date. Regular Care of a Physician means that You are being treated by a Physician: 1) whose medical training and clinical experience are suitable to treat Your disabling condition; and 2) whose treatment is: a) consistent with the diagnosis of the disabling condition; b) according to guidelines established by medical, research, and rehabilitative organizations; and c) administered as often as needed; to achieve the maximum medical improvement. Rehabilitation means a process of Our working together with You in order for Us to plan, adapt, and put into use options and services to meet Your return to work needs. A Rehabilitation program may include, when We consider it to be appropriate, any necessary and feasible: 1) vocational testing; 2) vocational training; 3) alternative treatment plans such as: a) support groups; b) physical therapy; c) occupational therapy; or d) speech therapy; 23 4) 5) 6) 7) work-place modification to the extent not otherwise provided; job placement; transitional work; and similar services. Related means Your spouse or other adult living with You, sibling, parent, step-parent, grandparent, aunt, uncle, niece, nephew, son, daughter, or grandchild or similar relationship in law. Retirement Plan means a defined benefit or defined contribution plan that provides benefits for Your retirement and which is not funded wholly by Your contributions. It does not include: 1) a profit sharing plan; 2) thrift, savings or stock ownership plans; 3) a non-qualified deferred compensation plan; or 4) an individual retirement account (IRA), a tax sheltered annuity (TSA), Keogh Plan, 401(k) plan, 403(b) plan or 457 deferred compensation arrangement. Substance Abuse means the pattern of pathological use of alcohol or other psychoactive drugs and substances characterized by: 1) impairments in social and/or occupational functioning; 2) debilitating physical condition; 3) inability to abstain from or reduce consumption of the substance; or 4) the need for daily substance use to maintain adequate functioning. Substance includes alcohol and drugs but excludes tobacco and caffeine. The Policy means the Policy which We issued to the Policyholder under the Policy Number shown on the face page. We, Our, or Us means the insurance company named on the face page of The Policy. Your Occupation means Your Occupation as it is recognized in the general workplace. Your Occupation does not mean the specific job You are performing for a specific employer or at a specific location. You or Your means the person to whom this certificate is issued. 24 AMENDATORY RIDER This rider is attached to all certificates given in connection with The Policy and is effective on The Policy Effective Date. This rider is intended to amend Your certificate, as indicated below, to comply with the laws of Your state of residence. Only those references to benefits, provisions or terms actually included in Your certificate will affect Your coverage. For California residents: 1) The following is added to the definition of Surviving Spouse in the Survivor Income Benefit: “Spouse” will also include an individual who is in a registered domestic partnership with You in accordance with California law. References to Your marriage or divorce will include Your registered domestic partnership or dissolution of Your registered domestic partnership. 2) The following is added to the definition of Surviving Children in the Survivor Income Benefit: Surviving Children will also include children of Your California registered domestic partner. For Connecticut residents, the following is added to the definition of Spouse: Spouse will include Your domestic partner, provided You have executed a domestic partner affidavit satisfactory to Us, establishing that You and Your partner are domestic partners for the purposes of The Policy. You will continue to be considered domestic partners provided You continue to meet the requirements described in the domestic partner affidavit. For Indiana residents: The last sentence in the Policy Interpretation provision is deleted and replaced by the following: This provision applies only where the interpretation of The Policy is governed by the Employee Retirement Income Security Act of 1974, as amended (ERISA), 29 U.S.C. 1001 et seq. For Louisiana residents, the following provision is added: Reinstatement after Military Service: Can my coverage be reinstated after return from active military service? If: 1) Your coverage terminates because You enter active military service; and 2) You are rehired within 12 months of the date You return from active military service; then coverage may be reinstated, provided You request such reinstatement within 31 days of the date you return to work. The reinstated coverage will: 1) be the same coverage amounts in force on the date coverage terminated; and 2) not be subject to any Waiting Period for Coverage, Evidence of Insurability or Pre-existing Conditions Limitations; and 3) be subject to all the terms and provisions of The Policy. For Massachusetts residents, the following is added to the Continuation Provisions: In accordance with Massachusetts state law, if Your insurance terminates because Your employment terminates or You cease to be a member of an eligible class, Your insurance will automatically be continued until the end of a 31 day period from the date Your insurance terminates or the date You become eligible for similar benefits under another group plan, whichever occurs first. Additionally, if Your insurance terminates because Your employment is terminated as a result of a plant closing or covered partial closing, Your insurance may be continued. You must elect in writing to continue insurance and pay the required premium for continued coverage. Coverage will cease on the earliest to occur of the following dates: 1) 90 days from the date You were no longer eligible for coverage as a Full-time Active Employee; 2) the date You become eligible for similar benefits under another group plan; 3) the last day of the period for which required premium is made; 4) the date the group insurance policy terminates; or 5) the date Your Employer ceases to be a Participant Employer, if applicable. Continued coverage is subject to all other applicable terms and conditions of The Policy. 25 For Minnesota residents: 1) the definition of Any Occupation is amended by the addition of the phrase “or may reasonably become qualified” to the first line; 2) The first two paragraphs of the Pre-Existing Conditions Limitation provision are deleted and replaced by the following: No benefit will be payable under The Policy for any Disability that is due to, contributed to by, or results from a Pre-Existing Condition, unless such Disability or loss is incurred: 1) After the lesser of the last day of: a) the number of days stated in Your certificate; or b) 730 consecutive days; while insured, during which you receive no medical care for the Pre-Existing Condition; or 2) After the lesser of the last day of: a) the number of days stated in Your certificate; or b) 730 consecutive days; during which you have been continuously insured under The Policy. The amount of a benefit increase, which results from a change in benefit options, a change of class or a change in The Policy, will not be paid for any disability that is due to, contributed to by, or results from a Pre-Existing Condition, unless such Disability begins: 1) After the lesser of the last day of : a) the number of days stated in Your certificate; or b) 730 consecutive days; while insured for the increased benefit amount during which you receive no medical care for the PreExisting Condition; or 2) After the lesser of the last day of : a) the number of days stated in Your certificate; or b) 730 consecutive days; during which you have been continuously insured for the increased benefit amount. 3) The definition of Pre-existing Condition in the Pre-Existing Conditions Limitation provision is deleted and is replaced by the following: Pre-existing Condition means any accidental bodily injury, sickness, Mental Illness, pregnancy, or episode of Substance Abuse for which You received Medical Care during the lesser of: 1) the period of time stated in Your certificate; or 2) the 730 day period; that ends the day before: 1) Your effective date of coverage; or 2) the effective date of a Change in Coverage. For Missouri residents, the Exclusion related to intentionally self-inflicted Injury is replaced by the following: intentionally self-inflicted Injury, suicide or attempted suicide, while sane; or For Montana residents, pregnancy will be covered, the same as any other Sickness, anything in the Policy to the contrary notwithstanding. For New Hampshire residents: 1) The definition of Other Income Benefits is amended by the deletion of 'mandatory "no-fault" automobile insurance plan'; 2) LTD The time period, stated in the Recurrent Disability provision, within which a Disability must recur in order to be considered the same Period of Disability is changed to 6 months, if less than 6 months. 3) The Policy Interpretation provision is deleted and replaced by the following: Under ERISA, the Company is hereby designated by the plan sponsor as a claim fiduciary with discretionary authority to determine eligibility for benefits and to interpret and construe the terms and provisions of the policy. As claim fiduciary, the Company has a duty to administer claims solely in the interest of the participants and beneficiaries of the employee benefit plan and in accordance with the documents and instruments governing the plan. This assignment of discretionary authority does not prohibit a participant or beneficiary from seeking judicial review of the Company's benefit eligibility determination after exhausting administrative remedies. The assignment of discretionary authority made under this provision may affect the standard of review that a court will use in reviewing the appropriateness of the Company's determination. In order to prevail, a plan participant or beneficiary may be required to prove that the Company's determination was arbitrary and capricious or an abuse of discretion. 26 4) The time periods stated in the Claim Appeal provision are changed to 180 days, if less than 180 days. For North Carolina residents: 1) The definition of Other Income Benefits is amended by the deletion of 'mandatory "no-fault" automobile insurance plan'; 2) The last sentence of the first paragraph of the Disability Benefit is amended by the addition of the following clause: "unless qualified medical professionals have determined that further medical care and treatment would be of no benefit to you." 3) The exclusion regarding Workers' Compensation benefits is replaced by the following in the Exclusions provision: for which the final adjudication or a Workers' Compensation claim determines that benefits are paid, or may be paid, if duly claimed; 4) The Subrogation provision is deleted. For Oregon residents: 1) The following is added to the definition of Surviving Spouse in the Survivor Income Benefit: "Spouse" will also include an individual who is in a registered domestic partnership with You in accordance with Oregon law. References to Your marriage or divorce will include Your registered domestic partnership or dissolution of Your registered domestic partnership. 2) The following is added to the definition of Surviving Children in the Survivor Income Benefit: Surviving Children will also include children of Your Oregon registered domestic partner. For South Carolina residents: 1) The first paragraph of the Continuity from a Prior Policy provision is replaced by the following: If You become insured under The Policy on the Policy Effective Date and within 30 days of being covered under the Prior Policy, the Pre-existing Conditions Limitation will end on the earliest of: 1) the Policy Effective Date, if Your coverage for the Disability was not limited by a pre-existing condition restriction under the Prior Policy; or 2) the date the restriction would have ceased to apply had the Prior Policy remained in force, if Your coverage was limited by a pre-existing condition limitation under the Prior Policy. 2) The time period in the Notice of Claim provision is changed to 20 days, if not already 20 days. 3) The following is added to the Physical Examinations and Autopsy provision: "Such autopsy must be performed during the period of contestability and must take place in the state of South Carolina." For South Dakota residents: 1) The definition of Physician is deleted and replaced by the following: Physician means a legally qualified physician or surgeon other than a physician or surgeon who is related to You by blood or marriage or a physician or surgeon who is a partner of S-Corp Shareholder working with You in the same business. This does not apply in areas in which the immediate family member is the only physician in the area and acting within the scope of their normal employment. 2) The definition of Other Income Benefits is amended by the deletion of all references to Your family, Your spouse and/or children. 3) The provision titled Policy Interpretation is deleted in its entirety. For Utah residents: 1) The time period during which You must be continuously insured in order to exercise the Conversion Right is changed to 6 consecutive months, if not already 6 consecutive months. 2) The time period in the Sending Proof of Loss provision is changed to 90 days, if not already 90 days. 3) The Policy Interpretation provision is deleted and replaced by the following: Benefits under this plan will be paid only if We, the plan administrator, decides in Our discretion that you are entitled to them. We also have discretion to determine eligibility for benefits and to interpret the terms of conditions of the benefit plan. Determinations made by Us, the plan administrator, pursuant to this reservation of discretion does not prohibit or prevent a claimant from seeking judicial review in federal court or Our determinations. The reservation of discretion made under this provision only establishes the scope of review that a federal court will apply when you seek judicial review of our determination of eligibility for benefits, the payment of benefits, or interpretation of the terms and conditions applicable to the plan. 27 We are an insurance company that provides insurance of this plan and the federal court will determine the level of discretion that it will accord Our determination. For Vermont residents: Purpose: Vermont law requires that health insurers offer coverage to parties to a civil union that is equivalent to coverage provided to married persons. Definitions, Terms, Conditions and Provisions: The definitions, terms, conditions or any other provisions of the policy, contract, certificate and/or riders and endorsements to which this mandatory endorsement is attached are hereby amended and superseded as follows: 1) Terms that mean or refer to a marital relationship, or that may be construed to mean or refer to a marital relationship, such as "marriage", "spouse", "husband", "wife", "dependent", "next of kin", "relative", "beneficiary", "survivor", "immediate family" and any other such terms, include the relationship created by a civil union established according to Vermont law. 2) Terms that mean or refer to the inception or dissolution of a marriage, such as "date of marriage", "divorce decree", "termination of marriage" and any other such terms include the inception or dissolution of a civil union established according to Vermont law. 3) Terms that mean or refer to family relationships arising from a marriage, such as “family”, “immediate family”, “dependent”, “children”, “next of kin”, “relative”, “beneficiary”, “survivor” and any other such terms include family relationships created by a civil union established according to Vermont law. 4) "Dependent" means a spouse, a party to a civil union established according to Vermont law, and a child or children (natural, stepchild, legally adopted or a minor or disabled child who is dependent on the insured for support and maintenance) who is born to or brought to a marriage or to a civil union established according to Vermont law. 5) "Child or covered child" means a child (natural, step-child, legally adopted or a minor or disabled child who is dependent on the insured for support and maintenance) who is born to or brought to a marriage or to a civil union established according to Vermont law. CAUTION: FEDERAL LAW RIGHTS MAY OR MAY NOT BE AVAILABLE Vermont law grants parties to a civil union the same benefits, protections and responsibilities that flow from marriage under state law. However, some or all of the benefits, protections and responsibilities related to health insurance that are available to married persons under federal law may not be available to parties to a civil union. For example, federal law, the Employee Income Retirement Security Act of 1974 known as “ERISA”, controls the employer/employee relationship with regard to determining eligibility for enrollment in private employer health benefit plans. Because of ERISA, Act 91 does not state requirements pertaining to a private employer’s enrollment of a party to a civil union in an ERISA employee welfare benefit plan. However, governmental employers (not federal government) are required to provide health benefits to the dependents of a party to a civil union if the public employer provides health benefits to the dependents of married persons. Federal law also controls group health insurance continuation rights under COBRA for employers with 20 or more employees as well as the Internal Revenue Code treatment of health insurance premiums. As a result, parties to a civil union and their families may or may not have access to certain benefits under this policy, contract, certificate, rider or endorsement that derive from federal law. You are advised to seek expert advice to determine your rights under this contract. For Virginia residents, any and all references to Domestic Partners are hereby deleted. For Washington residents: 1) The term “hyperemesis gravidarum” is deleted from the third paragraph of the definition of Complications of Pregnancy and is added to the second paragraph; 2) The General Work Stoppage continuation provision is replaced with the following: General Work Stoppage (including a strike or lockout): If Your employment terminates due to a cessation of active work as the result of a general work stoppage (including a strike or lockout), Your coverage shall be continued during the work stoppage until the last day of the month in which the coverage terminated, but in no event for a period exceeding six months. If the work stoppage ends, this continuation will cease immediately. 3) The provision titled Policy Interpretation is deleted in its entirety. 4) The following is added to the definition of Spouse: Spouse will include Your domestic partner, provided You have executed a domestic partner affidavit satisfactory to Us, establishing that You and Your partner are domestic partners for the purposes of The Policy. You will continue to be considered domestic partners provided You continue to meet the requirements described in the domestic partner affidavit. For Wisconsin residents, the time periods stated in the Claim Appeal provision are removed. 28 In all other respects, the Policy and certificates remain the same. Signed for Hartford Life and Accident Insurance Company Richard G. Costello, Secretary John C. Walters, President 29 CERTIFICATE OF INSURANCE HARTFORD LIFE AND ACCIDENT INSURANCE COMPANY Simsbury, Connecticut (A stock insurance company) Policyholder: DREXEL UNIVERSITY Policy Number: GL-395241 Policy Effective Date: January 1, 2010 Policy Anniversary Date: January 1, 2011 We have issued The Policy to the Policyholder. Our name, the Policyholder's name and The Policy Number are shown above. The provisions of The Policy, which are important to You, are summarized in this certificate consisting of this form and any additional forms which have been made a part of this certificate. This certificate replaces any other certificate We may have given to You earlier under The Policy. The Policy alone is the only contract under which payment will be made. Any difference between The Policy and this certificate will be settled according to the provisions of The Policy on file with Us at Our home office. The Policy may be inspected at the office of the Policyholder. Signed for the Company Richard G. Costello, Secretary John C. Walters, President A note on capitalization in this Certificate: Capitalization of a term, not normally capitalized according to the rules of standard punctuation, indicates a word or phrase that is a defined term in The Policy or refers to a specific provision contained herein. GBD-1100 A.1 (395241) GL 2.10 TABLE OF CONTENTS SCHEDULE OF INSURANCE.........................................................................................................................................32 Cost of Coverage ........................................................................................................................................................32 Eligible Class(es) for Coverage....................................................................................................................................32 Eligibility Waiting Period for Coverage .........................................................................................................................32 Benefit Amounts..........................................................................................................................................................33 ELIGIBILITY AND ENROLLMENT ..................................................................................................................................34 Eligible Persons ..........................................................................................................................................................34 Eligibility for Coverage.................................................................................................................................................34 Enrollment...................................................................................................................................................................34 Evidence of Insurability................................................................................................................................................35 PERIOD OF COVERAGE ...............................................................................................................................................36 Effective Date..............................................................................................................................................................36 Deferred Effective Date ...............................................................................................................................................36 Continuity From a Prior Policy .....................................................................................................................................36 Dependent Effective Date............................................................................................................................................37 Dependent Deferred Effective Date .............................................................................................................................37 Dependent Continuity From a Prior Policy....................................................................................................................37 Change in Coverage....................................................................................................................................................37 Termination .................................................................................................................................................................38 Continuation Provisions...............................................................................................................................................38 Waiver of Premium......................................................................................................................................................40 BENEFITS......................................................................................................................................................................41 Life Insurance Benefit..................................................................................................................................................41 Suicide Exclusion.....................................................................................................................................................41 Accelerated Benefit..................................................................................................................................................41 Conversion Right.........................................................................................................................................................42 Portability ....................................................................................................................................................................43 Accidental Death and Dismemberment Benefits ..........................................................................................................45 Definitions................................................................................................................................................................45 Benefits ...................................................................................................................................................................45 Exclusions ...............................................................................................................................................................45 EXCLUSIONS ................................................................................................................................................................46 GENERAL PROVISIONS................................................................................................................................................47 DEFINITIONS.................................................................................................................................................................50 AMENDATORY RIDER...................................................................................................................................................53 Change in Coverage....................................................................................................................................................66 ERISA ............................................................................................................................................................................82 SCHEDULE OF INSURANCE Cost of Coverage: Non-Contributory Coverage: Contributory Coverage: Basic Life Insurance Accidental Death and Dismemberment Supplemental Life Insurance Supplemental Dependent Life Insurance With respect to Basic Life Insurance, Accidental Death and Dismemberment, and Supplemental Dependent Life Insurance: Eligible Class(es) For Coverage: All Full-Time Active Employees and Faculty Members who are citizens or legal residents of the United States, its territories and protectorates, excluding Stationary Engineers, temporary, leased or seasonal Employees. With respect to Faculty Members: Full-time Employment: at least 12 credit hours per term or 36 credit hours per academic year With respect to all other Employees: Full-time Employment: at least 40 hours weekly With respect to Supplemental Life Insurance: Eligible Class(es) For Coverage: All Full-Time and Part-Time Active Employees and Faculty Members who are citizens or legal residents of the United States, its territories and protectorates, excluding Stationary Engineers, temporary, leased or seasonal Employees. With respect to Faculty Members: Full-time Employment: at least 12 credit hours per term or 36 credit hours per academic year Part-time Employment: at least 20 hours weekly With respect to all other Employees: Full-time Employment: at least 40 hours weekly Part-time Employment: at least 20 hours weekly Annual Enrollment Period: as determined by Your Employer on a yearly basis. Eligibility Waiting Period for Coverage: None 32 Life Insurance Benefit Amount of Life Insurance Option 1: Basic Amount of Life Insurance Maximum Amount 2 times Your annual Earnings, subject to a maximum of $500,000 rounded to the next higher $1,000 if not already a multiple of $1,000. Option 2: Basic Amount of Life Insurance Maximum Amount $50,000 Supplemental Amount of Life Insurance Guaranteed Issue Amount 2 times Your annual Earnings, subject to a maximum of $500,000 rounded to the next higher $1,000 if not already a multiple of $1,000. Maximum Amount 1, 2, 3, or 4 times Your annual Earnings, subject to a maximum of $2,500,000 rounded to the next higher $1,000 if not already a multiple of $1,000. Dependent Life Insurance Benefit Supplemental Amount of Dependent Life Insurance Spouse Guaranteed Issue Amount The amount You elect in increments of $10,000, subject to a maximum of $30,000. Maximum Amount The amount You elect in increments of $10,000, subject to a maximum of $150,000. Maximum Amount $500 Dependent Children: Age 14 day(s) but under age 6 month(s) Dependent Children: Age 6 month(s) but under age 19 year(s) The amount You elect in increments of $5,000, subject to a maximum of $10,000. Accidental Death and Dismemberment Benefit Option 1: Basic Principal Sum Maximum Amount 2 times Your annual Earnings, subject to a maximum of $500,000 rounded to the next higher $1,000 if not already a multiple of $1,000. 33 Option 2: Basic Principal Sum Maximum Amount $50,000 Additional Accidental Death and Dismemberment Benefits: Seat Belt and Air Bag Coverage Seat Belt Benefit Amount: Percentage of AD&D Principal Sum: 10% Maximum Amount: $10,000 Minimum Amount: $1,000 Air Bag Benefit Amount: Percentage of AD&D Principal Sum: 5% Maximum Amount: $5,000 Repatriation Benefit Percentage of AD&D Principal Sum: 5% Maximum Amount: $5,000 Reduction in Amount of Life Insurance We will reduce the Amount of Life Insurance for You and Your Dependents by any Amount of Life Insurance in force, paid or payable: 1) in accordance with the Conversion Right; 2) under the Portability provision; or 3) under the Prior Policy. Reduction in Coverage Due to Age We will terminate the Life Insurance Benefit for Your Spouse on the date You attain age 70. ELIGIBILITY AND ENROLLMENT Eligible Persons: Who is eligible for coverage? All persons in the class or classes shown in the Schedule of Insurance will be considered Eligible Persons. Eligibility for Coverage: When will I become eligible? You will become eligible for coverage on the latest of: 1) the Policy Effective Date; 2) the date You become a member of an Eligible Class; or 3) the date You complete the Eligibility Waiting Period for Coverage shown in the Schedule of Insurance, if applicable. Eligibility for Dependent Coverage: When will I become eligible for Dependent Coverage? You will become eligible for Dependent coverage on the later of: 1) the date You become eligible for Employee coverage; or 2) the date You acquire Your first Dependent. No person may be covered: 1) as a Dependent and an Employee; or 2) as a Dependent of more than one Employee; under The Policy. Enrollment: How do I enroll for coverage? For Non-Contributory Coverage, Your Employer will automatically enroll You for coverage. However, You will be required to complete a beneficiary designation form. 34 To enroll for Contributory Coverage, You must: 1) complete and sign a group insurance enrollment form which is satisfactory to Us, for Your coverage and Your Dependent's coverage; and 2) deliver it to Your Employer. You have the option to enroll electronically. Your Employer will provide instructions. If You do not enroll for Your coverage and/or Your Dependent's coverage within 31 days after becoming eligible under The Policy, or if You were eligible to enroll under the Prior Policy and did not do so, and later choose to enroll, You may enroll for Your coverage and/or Your Dependent's coverage only: 1) during an Annual Enrollment Period designated by the Policyholder; or 2) within 31 days of the date You have a Change in Family Status. Any Enrollment may be subject to the Evidence of Insurability Requirements provision. Evidence of Insurability Requirements: When will I first be required to provide Evidence of Insurability? We require Evidence of Insurability for initial coverage, if You: 1) enroll more than 31 days after the date You are first eligible to enroll including electing initial coverage after a Change in Family Status; 2) enroll for an Amount of Life Insurance greater than the Supplemental Guaranteed Issue Amount, regardless of when You enroll for coverage; or 3) were eligible for any coverage under the Prior Policy, but did not enroll and later choose to enroll for that coverage under The Policy. If Your Evidence of Insurability is not satisfactory to Us: 1) Your Amount of Life Insurance will equal the amount for which You were eligible without providing Evidence of Insurability, provided You enrolled within 31 days of the date You were first eligible to enroll; and 2) You will not be covered under The Policy if You enrolled more than 31 days after the date You were first eligible to enroll. Dependent Evidence of Insurability Requirements: When will my Dependents first be required to provide Evidence of Insurability? We require Evidence of Insurability, for initial coverage, if You: 1) enroll for Your Dependents’ coverage more than 31 days after the date You are first eligible to enroll, including electing initial coverage after a Change in Family Status; 2) enroll for an Amount of Dependent Life Insurance greater than the Dependent Guaranteed Issue Amount, regardless of when You enroll for coverage; or 3) were eligible for any coverage under the Prior Policy, but did not enroll and later choose to enroll for that coverage under The Policy. However, no Evidence of Insurability will be required if the Amount of Life Insurance for Your Dependent Child is $15,000 or less. If Your Dependents' Evidence of Insurability is not satisfactory to Us: 1) Your Dependents' Amount of Life Insurance will equal the amount for which Your Dependents were eligible without providing Evidence of Insurability, provided You enrolled within 31 days of the date You were first eligible to enroll; or 2) Your Dependents will not be covered under The Policy if You enrolled more than 31 days after the date You were first eligible to enroll. Evidence of Insurability: What is Evidence of Insurability? Evidence of Insurability must be satisfactory to Us and may include, but will not be limited to: 1) a completed and signed application approved by Us; 2) a medical examination; 3) attending Physician's statement; and 4) any additional information We may require. Evidence of Insurability will be furnished at Our expense except for Evidence of Insurability due to late enrollment. We will then determine if You or Your Dependents are insurable for initial coverage or an increase in coverage under The Policy, as described in the Increase in Amount of Life Insurance provision. 35 You will be notified in writing of Our determination of any Evidence of Insurability submission. Change in Family Status: What constitutes a Change in Family Status? 1) You get married or You execute a domestic partner affidavit; 2) You and Your spouse divorce or You terminate a domestic partnership; 3) Your child is born or You adopt or become the legal guardian of a child; 4) Your spouse or domestic partner dies; 5) Your child is no longer financially dependent on You or dies; 6) Your spouse is no longer employed, which results in a loss of group insurance; or 7) You have a change in classification from part-time to full-time or from full-time to part-time. PERIOD OF COVERAGE Effective Date: When does my coverage start? Non-Contributory Coverage, for which Evidence of Insurability is not required, will start on the date You become eligible. Contributory Coverage, for which Evidence of Insurability is not required, will start on the latest to occur of: 1) the date You become eligible, if You enroll on or before that date; 2) the January 1st on or next following the last day of the Annual Enrollment Period, if You enroll during an Annual Enrollment Period; or 3) the date You enroll, if You do so within 31 days from the date You are eligible. Any coverage for which Evidence of Insurability is required, will become effective on the later of: 1) the first of the month following the date You become eligible; or 2) the first of the month following the date We approve Your Evidence of Insurability. All Effective Dates of coverage are subject to the Deferred Effective Date provision. Deferred Effective Date: When will my effective date for coverage or a change in my coverage be deferred? If, on the date You are to become covered: 1) under The Policy; 2) for increased benefits; or 3) for a new benefit; You are not Actively at Work due to a physical or mental condition, such coverage will not start until the date You are Actively at Work. Continuity from a Prior Policy: Is there Continuity of Coverage from a Prior Policy? Your initial coverage under The Policy will begin, and will not be deferred if on the day before the Policy Effective Date, You were insured under the Prior Policy, but on the Policy Effective Date, You were not Actively at Work, and would otherwise meet the Eligibility requirements of The Policy. However, Your Amount of Insurance will be the lesser of the amount of life insurance and Accidental Death and Dismemberment Principal Sum: 1) You had under the Prior Policy; or 2) shown in the Schedule of Insurance; reduced by any coverage amount: 1) that is in force, paid or payable under the Prior Policy; or 2) that would have been so payable under the Prior Policy had timely election been made. Such amount of insurance under this provision is subject to any reductions in The Policy and will not increase. Coverage provided through this provision ends on the first to occur of: 1) the last day of a period of 12 consecutive months after the Policy Effective Date; 2) the date Your insurance terminates for any reason shown under the Termination provision; 3) the last day You would have been covered under the Prior Policy, had the Prior Policy not terminated; or 4) the date You are Actively at Work. However, if the coverage provided through this provision ends because You are Actively at Work, You may be covered as an Active Employee under The Policy. 36 Dependent Effective Date: When does Dependent coverage start? Coverage will start on the later to occur of: 1) The date You become eligible for Dependent coverage, if You have enrolled on or before that date; or 2) the January 1st on or next following the last day of the Annual Enrollment Period, if You enroll during an Annual Enrollment Period; or 3) the date You enroll, if You do so within 31 days from the date You are eligible for Dependent coverage. Coverage for which Evidence of Insurability is required, will become effective on the later of: 1) the date You become eligible for Dependent coverage; or 2) the date We approve Your Dependents’ Evidence of Insurability. In no event will Dependent coverage become effective before You become insured, with respect to the Basic Dependent Life Insurance and eligible, with respect to the Supplemental Dependent Life Insurance. Dependent Deferred Effective Date: When will the effective date for Dependent coverage or a change in coverage be deferred? If, on the date Your Dependent, is to become covered: 1) under The Policy; 2) for increased benefits; or 3) for a new benefit; he or she is: 1) confined in a hospital; or 2) Confined Elsewhere; such coverage will not start until he or she: 1) is discharged from the hospital; or 2) is no longer Confined Elsewhere; and has engaged in all the normal and customary activities of a person of like age and gender, in good health, for at least 15 consecutive days. This Deferred Effective Date provision will not apply to disabled children who qualify under the definition of Dependent Children. Confined Elsewhere means Your Dependent is unable to perform, unaided, the normal functions of daily living, or leave home or other place of residence without assistance. Dependent Continuity from a Prior Policy: Is there Continuity of Coverage from a Prior Policy for my Dependents? If on the day before the Policy Effective Date, You were covered with respect to Your Dependents under the Prior Policy, the Deferred Effective Date provision will not apply to initial coverage under The Policy for such Dependents. However, the Dependent Amount of Insurance will be the lesser of the Amount of Life Insurance: 1) they had under the Prior Policy; or 2) shown in the Schedule of Insurance; reduced by any coverage amount: 1) that is in force, paid or payable under the Prior Policy; or 2) that would have been so payable under the Prior Policy had timely election been made. Change in Coverage: When may I change my coverage or coverage for my Dependents? After Your initial enrollment You may increase or decrease coverage for You or Your Dependents, or add a new Dependent to Your existing Dependent coverage: 1) during any Annual Enrollment Period designated by the Policyholder; or 2) within 31 days of the date of a Change in Family Status. Effective Date for Changes in Coverage: When will changes in coverage become effective? Any decrease in coverage will take effect on the date of the change. Any increase in coverage will take effect on the latest of: 1) the date of the change; 2) the date requirements of the Deferred Effective Date provision are met; 3) the date Evidence of Insurability is approved, if required; or 4) the January 1st next following the last day of the Annual Enrollment Period, except for an increase as a result of a Change in Family Status. 37 Increase in Amount of Life Insurance: If I request an increase in the Amount of Life Insurance for myself or my Dependents, must we provide Evidence of Insurability? If You or Your Dependents are: 1) already enrolled for an Amount of Supplemental Life Insurance under The Policy, then You and Your Dependents must provide Evidence of Insurability for an increase of more than one level; or 2) not already enrolled for Supplemental Life Insurance under The Policy, You and Your Dependents must provide Evidence of Insurability for any amount of Supplemental Life Insurance; including an initial amount. In any event, if the Amount of Life Insurance You request is greater than the Guaranteed Issue Amount, You or Your Dependents, as applicable, must provide Evidence of Insurability. If Your Evidence of Insurability is not satisfactory to Us, the Amount of Life Insurance You had in effect on the date immediately prior to the date You requested the increase will not change. If Your Dependents' Evidence of Insurability is not satisfactory to Us, the Amount of Life Insurance they had in effect on the date immediately prior to the date You requested the increase will not change. Increase in Amount of Life Insurance: If my Amount of Life Insurance increases because my Earnings increase, must I provide Evidence of Insurability? If Your Amount of Life Insurance is based on a multiple of Your Earnings, You must provide Evidence of Insurability if Your Earnings increase such that Your Amount of Life Insurance is greater than the Guaranteed Issue Amount. Once approved, We will not require Evidence of Insurability again if Your Amount of Life Insurance increases solely because Your Earnings increased. However, if: 1) You do not submit Evidence of Insurability; or 2) Your Evidence of Insurability is not satisfactory to Us; Your Amount of Life Insurance: 1) will increase, but only up to the amount for which You were eligible without having to provide Evidence of Insurability; and 2) will not increase again, or beyond that amount, until Your Evidence of Insurability is approved. Termination: When will my coverage end? Your coverage will end on the earliest of the following: 1) the date The Policy terminates; 2) the date You are no longer in a class eligible for coverage, or The Policy no longer insures Your class; 3) the date the premium payment is due but not paid; 4) the date Your Employer terminates Your employment; or 5) the date You are no longer Actively at Work; unless continued in accordance with any of the Continuation Provisions. Dependent Termination: When does coverage for my Dependent end? Coverage for Your Dependent will end on the earliest to occur of: 1) the date Your coverage ends; 2) the date the required premium is due but not paid; 3) the date You are no longer eligible for Dependent coverage; 4) the date We or the Employer terminate Dependent coverage; or 5) the date the Dependent no longer meets the definition of Dependent; unless continued in accordance with the continuation provisions. Continuation Provisions: Can my coverage and coverage for my Dependents be continued beyond the date it would otherwise terminate? Coverage can be continued by Your Employer beyond a date shown in the Termination provision, if Your Employer provides a plan of continuation which applies to all employees the same way. Coverage may not be continued under more than one Continuation Provision. 38 The amount of continued coverage applicable to You or Your Dependents will be the amount of coverage in effect on the date immediately before coverage would otherwise have ended. Continued coverage: 1) is subject to any reductions in The Policy; 2) is subject to payment of premium; 3) may be continued up to the maximum time shown in the provisions; and 4) terminates if The Policy terminates. In no event will the amount of insurance increase while coverage is continued in accordance with the following provisions. In all other respects, the terms of Your coverage and coverage for Your Dependents remain unchanged. Leave of Absence: If You are on a documented leave of absence, other than Family and Medical Leave or Military Leave of Absence, that is on file with the Employer, all of Your coverage (including Dependent Life coverage) may be continued for a period of time, not to exceed 36 month(s). If the leave terminates prior to the agreed upon date, this continuation will cease immediately. Military Leave of Absence: If You enter active military service and are granted a military leave of absence in writing, Your coverage (including Dependent Life coverage) may be continued for up to 36 month(s). If the leave ends prior to the agreed upon date, this continuation will cease immediately. Status Change: If You are: 1) employed by the Policyholder; and 2) due to a reduction in the number of scheduled hours You work; Your coverage (including Dependent Life coverage) may be continued as long as You remain in an eligible Class Code after the date Your scheduled hours were reduced. Disability Insurance: If You are working for the Policyholder and: 1) are covered by; and 2) meet the definition of disabled under; a Group Disability Insurance Policy, issued by Us to Your Employer, Your coverage (including Dependent Life coverage) may be continued until the last day of the 12th month after the month in which You became disabled, as defined in the Group Disability Insurance Policy. Sickness or Injury: If You are not Actively at Work due to sickness or injury, all of Your coverages (including Dependent Life coverage) may be continued: 1) for a period of 9 consecutive month(s) from the date You were last Actively at Work; or 2) if such absence results in a leave of absence in accordance with state and/or federal family and medical leave laws, then the combined continuation period will not exceed 9 consecutive month(s). Family Medical Leave: If You are granted a leave of absence, in writing, according to the Family and Medical Leave Act of 1993, or other applicable state or local law, Your coverage(s) (including Dependent Life coverage) may be continued for up to 12 weeks, or 26 weeks if You qualify for Family Military Leave, or longer if required by other applicable law, following the date Your leave commenced. If the leave of absence terminates prior to the agreed upon date, this continuation will cease immediately. Sabbatical: If You are on a documented paid sabbatical, that is on file with the Employer, Your coverage (including Dependent Life coverage) may be continued for a period of time, not to exceed 36 month(s) after the sabbatical commenced. If the sabbatical terminates prior to the agreed upon date, this continuation will cease immediately. Continuation for Dependent Child(ren) with Disabilities: Will coverage for Dependent Children with disabilities be continued? If Your Dependent Child(ren) reach the age at which they would otherwise cease to be a Dependent as defined, and they are: 1) age 19 or older; and 2) disabled; and 3) primarily dependent upon You for financial support; then Dependent Child(ren) coverage will not terminate solely due to age. However: 1) You must submit proof satisfactory to Us of such Dependent Child(ren)'s disability within 31 days of the date he or she reaches such age; and 2) such Dependent Child(ren) must have become disabled before attaining age 19. 39 Coverage under The Policy will continue as long as: 1) You remain insured; 2) the child continues to meet the required conditions; and 3) any required premium is paid when due. However, no increase in the Amount of Life Insurance for such Dependent Children will be available. We have the right to require proof, satisfactory to Us, as often as necessary during the first two years of continuation, that the child continues to meet these conditions. We will not require proof more often than once a year after that. Waiver of Premium: Does coverage continue if I am Disabled? Waiver of Premium is a provision which allows You to continue Your and Your Dependent’s Life Insurance coverage without paying premium, while You are Disabled and qualify for Waiver of Premium. If You qualify for Waiver of Premium, the amount of continued coverage: 1) will be the amount in force on the date You cease to be an Active Employee; 2) will be subject to any reductions provided by The Policy; and 3) will not increase. Eligible Coverages: What coverages are eligible under this provision? This provision applies only to: 1) Your Basic Life Insurance; 2) Your Supplemental Life Insurance; and 3) Dependent Life Insurance. You are not eligible to apply for both the Portability Benefit and Waiver of Premium for the same coverage amount. Disabled: What does Disabled mean? Disabled means You are prevented by injury or sickness from doing any work for which You are, or could become, qualified by: 1) education; 2) training; or 3) experience. In addition, You will be considered Disabled if You have been diagnosed with a life expectancy of 12 months or less. Conditions for Qualification: What conditions must I satisfy before I qualify for this provision? To qualify for Waiver of Premium You must: 1) be covered under The Policy and be under age 60 when You become Disabled; 2) be Disabled and provide Proof of Loss that You have been Disabled for 6 consecutive month(s), starting on the date You were last Actively at Work; and 3) provide such proof within one year of Your last day of work as an Active Employee. In any event, You must have been Actively at Work under The Policy to qualify for Waiver of Premium. When Premiums are Waived: When will premiums be waived? If We approve Waiver of Premium, We will notify You of the date We will begin to waive premium. In any case, We will not waive premiums for the first 6 month(s) You are Disabled. We have the right to: 1) require Proof of Loss that You are Disabled; and 2) have You examined at reasonable intervals during the first 2 years after receiving initial Proof of Loss, but not more than once a year after that. If You fail to submit any required Proof of Loss or refuse to be examined as required by Us, then Waiver of Premium ceases. However, if We deny Your application for Waiver of Premium, You may be eligible to: 1) continue coverage under the Portability Benefit; or 2) convert coverage in accordance with the Conversion Right; for You and Your Dependents. If You cease to be Disabled and return to work for a total of 5 days or less during the first 6 month(s) that You are Disabled, the 6 month(s) waiting period will not be interrupted. Except for the 5 days or less that You worked, You must be 40 Disabled by the same condition for the total 6 month(s) period. If You return to work for more than 5 days, You must satisfy a new waiting period. Benefit Payable before Approval of Waiver of Premium: What if I die or my Dependent dies before I qualify for Waiver of Premium? If You or Your Dependent die within one year of Your last day of work as an Active Employee, but before You qualify for Waiver of Premium, We will pay the Amount of Life Insurance which is in force for the deceased person provided: 1) You were continuously Disabled; 2) the Disability lasted or would have lasted 6 month(s) or more; and 3) premiums had been paid for coverage. Waiver Ceases: When will Waiver of Premium cease? We will waive premium payments and continue Your coverage, while You remain Disabled, until the date You attain age 70 if Disabled prior to age 60. We will waive premium payments for Your Dependent Life Insurance and continue such coverage, while You remain Disabled, until the earliest of the date: 1) You die; 2) You no longer qualify for Waiver of Premium; 3) The Policy terminates; 4) Your Dependents are no longer in an Eligible Class, or Dependent coverage is no longer offered; or 5) Your Dependent no longer meets the definition of Dependent. What happens when Waiver of Premium ceases? When the Waiver of Premium ceases: 1) if You return to work in an Eligible Class, as an Active Employee, then You may again be eligible for coverage for Yourself and Your Dependents as long as premiums are paid when due; or 2) if You do not return to work in an Eligible Class, coverage will end and You may be eligible to exercise the Conversion Right for You and Your Dependents if You do so within the time limits described in such provision. The Amount of Life Insurance that may be converted will be subject to the terms and conditions of the Conversion Right. Portability will not be available. Effect of Policy Termination: What happens to the Waiver of Premium if The Policy terminates? If The Policy terminates before You qualify for Waiver of Premium: 1) You may be eligible to exercise the Conversion Right, provided You do so within the time limits described in such provision; and 2) You may still be approved for Waiver of Premium if You qualify. If The Policy terminates after You qualify for Waiver of Premium: 1) Your Dependent coverage will terminate; and 2) Your coverage under the terms of this provision will not be affected. BENEFITS Life Insurance Benefit: When is the Life Insurance Benefit payable? If You or Your Dependents die while covered under The Policy, We will pay the deceased person’s Life Insurance Benefit after We receive Proof of Loss, in accordance with the Proof of Loss provision. The Life Insurance Benefit will be paid according to the General Provisions of The Policy. Suicide: What benefit is payable if death is a result of suicide? If You or Your Dependent commit suicide while sane or insane, We will not pay any Supplemental Amount of Life Insurance or Supplemental Amount of Dependent Life Insurance for the deceased person which was elected within the 2 year period immediately prior to the date of death. This applies to initial coverage and elected increases in coverage. It does not apply to benefit increases that resulted solely due to an increase in Earnings. This 2 year period includes the time group life insurance coverage was in force under the Prior Policy. Accelerated Benefit: What is the benefit? 41 In the event that You or Your Dependent are diagnosed as Terminally Ill while the Terminally Ill person is covered under The Policy for an Amount of Life Insurance of at least $10,000, We will pay the Accelerated Benefit amount as shown below, provided We receive proof of such Terminal Illness. You must request in writing that a portion of the Terminally Ill person’s Amount of Life Insurance be paid as an Accelerated Benefit. The Amount of Life Insurance payable upon the Terminally Ill person’s death will be reduced by any Accelerated Benefit Amount paid under this benefit. You may request a minimum Accelerated Benefit amount of $3,000, and a maximum of $500,000. However, in no event will the Accelerated Benefit Amount exceed 80% of the Terminally Ill person’s Amount of Life Insurance. This option may be exercised only once for You and only once for each of Your Dependents. For example, if You are covered for a Life Insurance Benefit Amount under The Policy of $20,000 and are Terminally Ill, You can request any portion of the Amount of Life Insurance Benefits from $3,000 to $16,000 to be paid now instead of to Your beneficiary upon death. However, if You decide to request only $3,000 now, You cannot request the additional $13,000 in the future. A person who submits proof satisfactory to Us of his or her Terminal Illness will also meet the definition of Disabled for Waiver of Premium. In the event: 1) You are required by law to accelerate benefits to meet the claims of creditors; or 2) if a government agency requires You to apply for benefits to qualify for a government benefit or entitlement; You will still be required to satisfy all the terms and conditions herein in order to receive an Accelerated Benefit. If You have executed an Assignment of rights and interest with respect to Your or Your Dependent’s Amount of Life Insurance, in order to receive the Accelerated Benefit, We must receive a release from the assignee before any benefits are payable. Terminal Illness or Terminally Ill means a life expectancy of 12 months or less. Proof of Terminal Illness and Examinations: Must proof of Terminal Illness be submitted? We reserve the right to require satisfactory Proof of Terminal Illness on an ongoing basis. Any diagnosis submitted must be provided by a Physician. If You or Your Dependents do not submit proof of Terminal Illness satisfactory to Us, or if You or Your Dependents refuse to be examined by a Physician, as We may require, then We will not pay an Accelerated Benefit. No Longer Terminally Ill: What happens to my coverage if I am no longer Terminally Ill or my Dependent is no longer Terminally Ill? If You or Your Dependents are diagnosed by a Physician as no longer Terminally Ill and: 1) return to an Eligible Class, coverage will remain in force, provided premium is paid; 2) do not return to an Eligible Class, but You continue to meet the definition of Disabled, coverage will remain in force, subject to the Waiver of Premium provision; or 3) are not in an Eligible Class, but You do not continue to meet the definition of Disabled, coverage will end and You may be eligible to exercise the Conversion Right, if You do so within the time limits described in such provision. In any event, the amount of coverage will be reduced by the Accelerated Benefit paid. Conversion Right: If coverage under The Policy ends, do I have a right to convert? If Life Insurance coverage or any portion of it under The Policy ends for any reason, You and Your Dependents may have the right to convert the coverage that terminated to an individual conversion policy without providing Evidence of Insurability. Conversion is not available for: 1) the Accidental Death and Dismemberment Benefits; or 2) any Amount of Life Insurance for which You or Your Dependents were not eligible and covered; under The Policy. If coverage under The Policy ends because: 1) The Policy is terminated; or 42 2) Coverage for an Eligible Class is terminated; then You or Your Dependent must have been insured under The Policy for 5 years or more, in order to be eligible to convert coverage. The amount which may be converted under these circumstances is limited to the lesser of: 1) $2,000; or 2) the Life Insurance Benefit under The Policy less any Amount of Life Insurance for which You or Your Dependent may become eligible under any group life insurance policy issued or reinstated within 31 days of termination of group life coverage. If coverage under The Policy ends for any other reason, the full amount of coverage which ended may be converted. Insurer, as used in this provision, means Us or another insurance company which has agreed to issue conversion policies according to this Conversion Right. Conversion: How do I convert my coverage or coverage for my Dependents? To convert Your coverage or coverage for Your Dependents, You must: 1) complete a Notice of Conversion Right form; and 2) have your Employer sign the form. The Insurer must receive this within: 1) 31 days after Life Insurance terminates; or 2) 15 days from the date Your Employer signs the form; whichever is later. However, We will not accept requests for Conversion if they are received more than 91 days after Life Insurance terminates. After the Insurer verifies eligibility for coverage, the Insurer will send You a Conversion Policy proposal. You must: 1) complete and return the request form in the proposal; and 2) pay the required premium for coverage; within the time period specified in the proposal. Any individual policy issued to You or Your Dependents under the Conversion Right: 1) will be effective as of the 32nd day after the date coverage ends; and 2) will be in lieu of coverage for this amount under The Policy. Conversion Policy Provisions: What are the Conversion Policy provisions? The Conversion Policy will: 1) be issued on one of the Life Insurance policy forms the Insurer is issuing for this purpose at the time of conversion; and 2) base premiums on the Insurer's rates in effect for new applicants of Your class and age at the time of conversion. The Conversion Policy will not provide: 1) the same terms and conditions of coverage as The Policy; 2) any benefit other than the Life Insurance Benefit; and 3) term insurance. However, Conversion is not available for any Amount of Life Insurance which was, or is being, continued: 1) in accordance with the Waiver of Premium provision; 2) under a certificate of insurance issued in accordance with the Portability provision; or 3) in accordance with the Continuation Provisions; until such coverage ends. Death within the Conversion Period: What if I or my Dependents die before coverage is converted? We will pay the deceased person’s Amount of Life Insurance You would have had the right to apply for under this provision if: 1) coverage under The Policy terminates; 2) You or Your Dependent die within 31 days of date coverage terminates; and 3) We receive Proof of Loss. If the Conversion Policy has already taken effect, no Life Insurance Benefit will be payable under The Policy for the amount converted. Portability Benefits: What is Portability? 43 Portability is a provision which allows You and Your Dependents to continue coverage under a Group Portability policy when coverage would otherwise end due to certain Qualifying Events. Portability applies to Life Insurance only. Qualifying Events: What are Qualifying Events? Qualifying Events for You are: 1) Your employment terminates for any reason prior to Normal Retirement Age; or 2) Your membership in an Eligible Class under The Policy ends. Qualifying Events for Your Dependents are: 1) Your employment terminates, for any reason prior to Normal Retirement Age; or 2) Your death; 3) Your membership in a class eligible for Dependent coverage ends; 4) He or she no longer meets the definition of Dependent. However a Dependent Child who reaches the limiting age under The Policy is not eligible for Portability. Electing Portability: How do I elect Portability? You may elect Portability for Your coverage after Your coverage ends because You had a Qualifying Event. You may also elect Portability for Your Dependent coverage if Your Dependent has a Qualifying Event. The Policy must still be in force in order for Portability to be available. In order for Dependent Child coverage to be continued under this provision, You or Your Spouse must elect to continue coverage. To elect Portability for You or Your Dependents, You must: 1) complete and have Your Employer sign a Portability application; and 2) submit the application to Us, with the required premium. This must be received within: 1) 31 days after Life Insurance terminates; or 2) 15 days from the date Your Employer signs the application; whichever is later. However, Portability requests will not be accepted if they are received more than 91 days after Life Insurance terminates. After We verify eligibility for coverage, We will issue a certificate of insurance under a Portability policy. The Portability coverage will be: 1) issued without Evidence of Insurability; 2) issued on one of the forms then being issued by Us for Portability purposes; and 3) effective on the day following the date Your or Your Dependent’s coverage ends. The terms and conditions of coverage under the Portability policy will not be the same terms and conditions that are applicable to coverage under The Policy. Limitations: What limitations apply to this benefit? You may elect to continue 50%, 75%, or 100% of the Amount of Life Insurance which is ending for You or Your Dependent. This amount will be rounded to the next higher multiple of $1,000, if not already a multiple of $1,000. However, the Amount of Life Insurance that may be continued will not exceed: 1) $250,000 for You; 2) $50,000 for Your Spouse ; or 3) $10,000 for Your Dependent Child(ren). If You elect to continue 50% or 75% now, You may not continue any portion of the remaining amount under this Portability provision at a later date. In no event will You or Your Spouse be able to continue an Amount of Life Insurance which is less than $5,000. Portability is not available for any Amount of Life Insurance for which You or Your Dependents were not eligible and covered. In addition Portability is not available if You or Your Dependents are entering active military service. Effect of Portability on other Provisions: How does Portability affect other Provisions? Portability is not available for any Amount of Life Insurance which was, or is being, continued in accordance with the: 1) Conversion Right; 2) Waiver of Premium Provision; or 44 3) Continuation provisions; under The Policy. However, If: 1) You elect to continue only a portion of terminated coverage under this Portability provision; or 2) the Amount of Life Insurance exceeds the maximum Portability amount; then the Conversion Right may be available for the remaining amount. The Waiver of Premium provision will not be available if You elect to continue coverage under this Portability provision. Accidental Death and Dismemberment Benefit: When is the Accidental Death and Dismemberment Benefit payable? If You sustain an Injury which results in any of the following Losses within 365 days of the date of accident, We will pay Your amount of Principal Sum, or a portion of such Principal Sum, as shown opposite the Loss after We receive Proof of Loss, in accordance with the Proof of Loss provision. The loss period does not apply to loss of Life. This Benefit will be paid according to the General Provisions of The Policy. We will not pay more than the Principal Sum to any one person, for all Losses due to the same accident. Your amount of Principal Sum is shown in the Schedule of Insurance. For Loss of: Benefit: Life…………………………………………………….………….…………………….Principal Sum Both Hands or Both Feet or Sight of Both Eyes………….………………………..Principal Sum One Hand and One Foot……………………..…………………….………..………Principal Sum Speech and Hearing in Both Ears…………….………………….…………………Principal Sum Either Hand or Foot and Sight of One Eye…….……………….………………….Principal Sum Movement of Both Upper and Lower Limbs (Quadriplegia)….….……………….Principal Sum Movement of Both Lower Limbs (Paraplegia)…….………....Three-Quarters of Principal Sum Movement of Three Limbs (Triplegia)…………….…………..Three-Quarters of Principal Sum Movement of the Upper and Lower Limbs of One Side of the Body (Hemiplegia)……………...............................................One-Half of Principal Sum Either Hand or Foot………………………………………………….....One-Half of Principal Sum Sight of One Eye………………………………………………………..One-Half of Principal Sum Speech or Hearing in Both Ears………………………………………One-Half of Principal Sum Movement of One Limb (Uniplegia)……………………………...One-Quarter of Principal Sum Thumb and Index Finger of Either Hand………………………...One-Quarter of Principal Sum Loss means with regard to: 1) hands and feet, actual severance through or above wrist or ankle joints; 2) sight, speech and hearing, entire and irrecoverable loss thereof; 3) thumb and index finger, actual severance through or above the metacarpophalangeal joints; or 4) movement, complete and irreversible paralysis of such limbs. Seat Belt and Air Bag Benefit: When is the Seat Belt and Air Bag Benefit payable? If You sustain an Injury which results in a Loss payable under the Accidental Death and Dismemberment Benefit, We will pay an additional Seat Belt and Air Bag Benefit if the Injury occurred while You were: 1) a passenger riding in; or 2) the licensed operator of; a properly registered Motor Vehicle and was wearing a Seat Belt at the time of the Accident as verified on the police accident report. This Benefit will be paid: 1) after We receive Proof of Loss, in accordance with the Proof of Loss provision; and 2) according to the General Provisions of The Policy. If a Seat Belt Benefit is payable, We will also pay an Air Bag Benefit if You were: 1) positioned in a seat equipped with a factory-installed Air Bag; and 2) properly strapped in the Seat Belt when the Air Bag inflated. The Seat Belt Benefit is the lesser of: 1) an amount resulting from multiplying Your amount of Principal Sum by the Seat Belt Benefit Percentage; or 2) the Maximum Amount for this Benefit. 45 The Air Bag Benefit is the lesser of: 1) an amount resulting from multiplying Your amount of Principal Sum by the Air Bag Benefit Percentage; or 2) the Maximum Amount for this Benefit. If it cannot be determined that You were wearing a Seat Belt at the time of Accident, a Minimum Benefit will be payable under the Seat Belt Benefit. Accident, for the purpose of this Benefit only, means the unintentional collision of a Motor Vehicle during which You were wearing a Seat Belt. Air Bag means an inflatable supplemental passive restraint system installed by the manufacturer of the Motor Vehicle or its proper replacement parts installed as required by the Motor Vehicle’s manufacturer's specifications that inflates upon collision to protect an individual from Injury and death. An Air Bag is not considered a Seat Belt. Seat Belt means: 1) an unaltered belt, lap restraint, or lap and shoulder restraint installed by the manufacturer of the Motor Vehicle, or proper replacement parts installed as required by the Motor Vehicle’s manufacturer’s specifications; or 2) a child restraint device that meets the standards of the National Safety Council and is properly secured and used in accordance with applicable state law and installed according to the recommendations of its manufacturer for children of like age and weight. The Seat Belt and Air Bag Benefit will not be payable if You are operating the Motor Vehicle at the time of Injury while: 1) Intoxicated; or 2) taking drugs, including but not limited to sedatives, narcotics, barbiturates, amphetamines, or hallucinogens, unless as prescribed by or administered by a Physician. Intoxicated means: 1) the blood alcohol content; 2) the results of other means of testing blood alcohol level; or 3) the results of other means of testing other substances; that meet or exceed the legal presumption of intoxication, or under the influence, under the law of the state where the accident occurred. The specific amounts for this Benefit are shown in the Schedule of Insurance. Repatriation Benefit: When is the Repatriation Benefit payable? If You sustain an Injury that results in Loss of life payable under the Accidental Death and Dismemberment Benefit, We will pay an additional Repatriation Benefit, if the death occurs outside the territorial limits of the state or country of Your place of permanent residence. This Benefit will be paid: 1) after We receive Proof of Loss, in accordance with the Proof of Loss provision; and 2) according to the General Provisions of The Policy. The Repatriation Benefit will pay the least of: 1) the actual expenses incurred for: a) preparation of the body for burial or cremation; and b) transportation of the body to the place of burial or cremation; 2) the amount resulting from multiplying Your amount of Principal Sum by the Repatriation Benefit Percentage; or 3) the Maximum Amount for this Benefit. The specific amounts for this Benefit are shown in the Schedule of Insurance. EXCLUSIONS 46 Exclusions: (applicable to all benefits except the Life Insurance, Accelerated Benefit): What losses are not covered? The Policy does not cover any loss caused or contributed to by: 1) intentionally self-inflicted Injury; 2) suicide or attempted suicide, whether sane or insane; 3) war or act of war, whether declared or not; 4) Injury sustained while on full-time active duty as a member of the armed forces (land, water, air) of any country or international authority; 5) Injury sustained while taking drugs, including but not limited to sedatives, narcotics, barbiturates, amphetamines, or hallucinogens, unless as prescribed by or administered by a Physician; 6) Injury sustained while committing or attempting to commit a felony; or 7) Injury sustained while Intoxicated. Intoxicated means: 1) the blood alcohol content; 2) the results of other means of testing blood alcohol level; or 3) the results of other means of testing other substances; that meet or exceed the legal presumption of intoxication, or under the influence, under the law of the state where the accident occurred. GENERAL PROVISIONS Notice of Claim: When should I notify the Company of a claim? You, or the person who has the right to claim benefits, must give Us, written notice of a claim within 30 days after: 1) the date of death; or 2) the date of loss. If notice cannot be given within that time, it must be given as soon as reasonably possible after that. Such notice must include the claimant’s name, address and the Policy Number. Claim Forms: Are special forms required to file a claim? We will send forms to the claimant to provide Proof of Loss, within 15 days of receiving a Notice of Claim. If We do not send the forms within 15 days, the claimant may submit any other written proof which fully describes the nature and extent of the claim. Proof of Loss: What is Proof of Loss? Proof of Loss may include, but is not limited to, the following: 1) a completed claim form; 2) a certified copy of the death certificate (if applicable); 3) Your Enrollment form; 4) Your Beneficiary Designation (if applicable); 5) documentation of: a) the date Your Disability began; b) the cause of Your Disability; and c) the prognosis of Your Disability; 6) any and all medical information, including x-ray films and photocopies of medical records, including histories, physical, mental or diagnostic examinations and treatment notes; 7) the names and addresses of all: a) Physicians or other qualified medical professionals You have consulted; b) hospitals or other medical facilities in which You have been treated; and c) pharmacies which have filled Your prescriptions within the past three years; 8) Your signed authorization for Us to obtain and release medical, employment and financial information (if applicable); or 9) Any additional information required by Us to adjudicate the claim. All proof submitted must be satisfactory to Us. Sending Proof of Loss: When must Proof of Loss be given? Written Proof of Loss: 1) with respect to the Life Insurance Benefits, should be sent within 90 day(s); and 47 2) with respect to the Accidental Death and Dismemberment Benefits, must be sent within 90 day(s); after the loss. All Proof of Loss should be sent to Us. However, all claims should be submitted to Us within 90 day(s) of the date coverage ends. If proof is not given by the time it is due, it will not affect the claim if: 1) it was not possible to give proof within the required time; and 2) proof is given as soon as possible; but 3) not later than 1 year after it is due unless You, or the person who has the right to claim benefits, are not legally competent. Physical Examination and Autopsy: Can We have a claimant examined or request an autopsy? While a claim is pending We have the right at Our expense: 1) to have the person who has a loss examined by a Physician when and as often as We reasonably require; and 2) to have an autopsy performed in case of death where it is not forbidden by law. Claim Payment: When are benefit payments issued? When We determine that benefits are payable, We will pay the benefits in accordance with the Claims to be Paid provision, but not more than 30 day(s) after such Proof of Loss is received. Claims to be Paid: To whom will benefits for my claim be paid? Life Insurance Benefits and benefits for loss of life under the Accidental Death and Dismemberment Benefits will be paid in accordance with the life insurance Beneficiary Designation. If no beneficiary is named, or if no named beneficiary survives You, We may, at Our option, pay: 1) the executors or administrators of Your estate; or 2) all to Your surviving Spouse; or 3) if Your Spouse does not survive You, in equal shares to Your surviving Children; or 4) if no child survives You, in equal shares to Your surviving parents. In addition, We may, at Our option, pay a portion of Your Life Insurance Benefit up to $500 to any person equitably entitled to payment because of expenses from Your burial. Payment to any person, as shown above, will release Us from liability for the amount paid. If any beneficiary is a minor, We may pay his or her share, until a legal guardian of the minor’s estate is appointed, to a person who at Our option and in Our opinion is providing financial support and maintenance for the minor. We will pay: 1) $200 at Your death; and 2) monthly installments of not more than $200. Payment to any person as shown above will release Us from all further liability for the amount paid. We will pay the Life Insurance Benefit at Your Dependents' death to You, if living. Otherwise, it will be paid, at Our option, to Your surviving Spouse or the executor or administrator of Your estate. If benefits are payable and meet Our guidelines, then We may pay benefits into a draft book account (checking account) which will be owned by: 1) You, if living; or 2) Your beneficiary, in the event of Your death. The account owner may elect a lump sum payment by writing a check for the full amount in the account. However, an account will not be established for a benefit payable to Your estate. We will make any payments, other than for loss of life, to You. We may make any such payments owed at Your death to Your estate. If any payment is owed to: 1) Your estate; 2) a person who is a minor; or 3) a person who is not legally competent, then We may pay up to $1,000 to a person who is related to You and who, at Our sole discretion, is entitled to it. Any such payment shall fulfill Our responsibility for the amount paid. Beneficiary Designation: How do I designate or change my beneficiary? 48 You may designate or change a beneficiary by doing so in writing on a form satisfactory to Us and filing the form with the Employer. Only satisfactory forms sent to the Employer prior to Your death will be accepted. Beneficiary designations will become effective as of the date You signed and dated the form, even if You have since died. We will not be liable for any amounts paid before receiving notice of a beneficiary change from the Employer. In no event may a beneficiary be changed by a Power of Attorney. Claim Denial: What notification will my Beneficiary or I receive if a claim is denied? If a claim for benefits is wholly or partly denied, You or Your Beneficiary will be furnished with written notification of the decision. This written notification will: 1) give the specific reason(s) for the denial; 2) make specific reference to the provisions on which the denial is based; 3) provide a description of any additional information necessary to perfect a claim and an explanation of why it is necessary; and 4) provide an explanation of the review procedure. Claim Appeal: What recourse do my Beneficiary or I have if a claim is denied? On any claim, the claimant or his or her representative may appeal to Us for a full and fair review. To do so, he or she: 1) must request a review upon written application within: a) 180 days of receipt of claim denial if the claim requires Us to make a determination of disability; or b) 60 days of receipt of claim denial if the claim does not require Us to make a determination of disability; and 2) may request copies of all documents, records, and other information relevant to the claim; and 3) may submit written comments, documents, records and other information relating to the claim. We will respond in writing with Our final decision on the claim. Policy Interpretation: Who interprets the terms and conditions of The Policy? We have full discretion and authority to determine eligibility for benefits and to construe and interpret all terms and provisions of The Policy. This provision applies where the interpretation of The Policy is governed by the Employee Retirement Income Security Act of 1974, as amended (ERISA). Incontestability: When can the Life Insurance Benefit of The Policy be contested? Except for non-payment of premiums, Your or Your Dependent's Life Insurance Benefit cannot be contested after two years from its effective date. This provision does not apply to the Accidental Death and Dismemberment benefit(s). In the absence of Fraud, no statement made by You relating to Your insurability will be used to contest Your insurance for which the statement was made after Your insurance has been in force for two years. In order to be used, the statement must be in writing and signed by You. No statement made relating to Your Dependents being insurable will be used to contest their insurance for which the statement was made after their insurance has been in force for two years. In order to be used, the statement must be in writing and signed by You or Your representative. Assignment: Are there any rights of assignment? Except for the dismemberment benefits under the Accidental Death and Dismemberment Benefit, You have the right to absolutely assign Your rights and interest under The Policy including, but not limited to the following: 1) the right to make any contributions required to keep the insurance in force; 2) the right to convert; and 3) the right to name and change a beneficiary. We will recognize any absolute assignment made by You under The Policy, provided: 1) it is duly executed; and 2) a copy is acknowledged and on file with Us. We and the Policyholder assume no responsibility: 1) for the validity or effect of any assignment; or 2) to provide any assignee with notices which We may be obligated to provide to You. You do not have the right to collaterally assign Your rights and interest under The Policy. 49 Legal Actions: When can legal action be taken against Us? Legal action cannot be taken against Us: 1) sooner than 60 days after the date Proof of Loss is furnished; or 2) 3 years after the date Proof of Loss is required to be furnished according to the terms of The Policy. Workers' Compensation: How does The Policy affect Workers' Compensation coverage? The Policy does not replace Workers' Compensation or affect any requirement for Workers' Compensation coverage. Insurance Fraud: How does the Company deal with fraud? Insurance fraud occurs when You, Your Dependents and/or Your Employer provide Us with false information or file a claim for benefits that contains any false, incomplete or misleading information with the intent to injure, defraud or deceive Us. It is a crime if You, Your Dependents and/or Your Employer commit insurance fraud. We will use all means available to Us to detect, investigate, deter and prosecute those who commit insurance fraud. We will pursue all available legal remedies if You, Your Dependents and/or Your Employer perpetrate insurance fraud. Misstatements: What happens if facts are misstated? If material facts about You or Your Dependents were not stated accurately: 1) the premium may be adjusted; and 2) the true facts will be used to determine if, and for what amount, coverage should have been in force. DEFINITIONS Active Employee means an employee who works for the Employer on a regular basis in the usual course of the Employer's business. This must be at least the number of hours shown in the Schedule of Insurance. Actively at Work means at work with Your Employer on a day that is one of Your Employer's scheduled workdays. On that day, You must be performing for wage or profit all of the regular duties of Your job: 1) in the usual way; and 2) for Your usual number of hours. We will also consider You to be Actively At Work on any regularly scheduled vacation day or holiday, only if You were Actively At Work on the preceding scheduled work day. Common Carrier means a conveyance operated by a concern, other than the Policyholder, organized and licensed for the transportation of passengers for hire and operated by that concern. Contributory Coverage means coverage for which You are required to contribute toward the cost. Contributory Coverage is shown in the Schedule of Insurance. Dependent Child(ren) means: 1) Your unmarried children, stepchildren, legally adopted children; or 2) any other children related to You by blood or marriage or domestic partnership who: a) live with You in a regular parent-child relationship; and/or b) You claimed as a dependent on Your last filed federal income tax return; provided such children are primarily dependent upon You for financial support and maintenance and are: 1) at least 14 day(s) old but under age 19; 2) age 19, but under age 23 and in full-time attendance (at least 12 course credit hours per semester) at an accredited institution of learning. If the institution establishes full-time status in any other manner, We reserve the right to determine whether the student continues to qualify as a Dependent; or 3) age 19 or older and disabled. Such children must have become disabled before attaining age 19. You must submit proof, satisfactory to Us, of such children’s disability. Dependents means Your Spouse and Your Dependent Child(ren). A dependent must be a citizen or legal resident of the United States, its territories and protectorates. Any person who is in full-time military service cannot be a dependent. Earnings means Your regular annual rate of pay, not counting bonuses, commissions and tips and tokens, overtime pay or any other fringe benefits or extra compensation, in effect on the date You were last Actively at Work. 50 However, if You are an hourly paid Employee, Earnings means the product of: 1) the average number of hours You worked per year, not including overtime, over the most recent 1 year period immediately prior to the date You were last Actively at Work, multiplied by: 2) Your hourly wage in effect on the date immediately prior to the date You were last Actively at Work. Employer means the Policyholder. Guaranteed Issue Amount means the Amount of Life Insurance for which We do not require Evidence of Insurability. The Guaranteed Issue Amount is shown in the Schedule of Insurance. Injury means bodily injury resulting: 1) directly from an accident; and 2) independently of all other causes; which occurs while You are covered under The Policy. Loss resulting from: 1) sickness or disease, except a pus-forming infection which occurs through an accidental wound; or 2) medical or surgical treatment of a sickness or disease; is not considered as resulting from Injury. Motor Vehicle means a self-propelled, four (4) or more wheeled: 1) private passenger: car, station wagon, van or sport utility vehicle; 2) motor home or camper; or 3) pick-up truck; not being used as a Common Carrier. A Motor Vehicle does not include farm equipment, snowmobiles, all-terrain vehicles, lawnmowers or any other type of equipment vehicles. Non-Contributory Coverage means coverage for which You are not required to contribute toward the cost. NonContributory Coverage is shown in the Schedule of Insurance. Normal Retirement Age means the Social Security Normal Retirement Age under the most recent amendments to the United States Social Security Act. It is determined by Your date of birth, as follows: Year of Birth Normal Retirement Age Year of Birth Normal Retirement Age 1937 or before 65 1955 66 + 2 months 1938 65 + 2 months 1956 66 + 4 months 1939 65 + 4 months 1957 66 + 6 months 1940 65 + 6 months 1958 66 + 8 months 1941 65 + 8 months 1959 66 + 10 months 1942 65 + 10 months 1960 or after 67 1943 through 1954 66 Physician means a person who is: 1) a doctor of medicine, osteopathy, psychology or other legally qualified practitioner of a healing art that We recognize or are required by law to recognize; 2) licensed to practice in the jurisdiction where care is being given; 3) practicing within the scope of that license; and 4) not Related to You by blood or marriage. Prior Policy means the group life insurance Policy carried by Your Policyholder on the day before the Policy Effective Date and will only include the coverage which is transferred to Us. Related means Your Spouse, or someone in a similar relationship in law to You, or other adult living with You, or Your sibling, parent, step-parent, grandparent, aunt, uncle, niece, nephew, son, daughter, or grandchild. Spouse means Your spouse who is not legally separated or divorced from You. 51 Spouse will include Your domestic partner, provided You have executed a domestic partner affidavit satisfactory to Us, establishing that You and Your partner are domestic partners for purposes of The Policy. You will continue to be considered domestic partners provided You continue to meet the requirements described in the domestic partner affidavit. The Policy means the policy which We issued to the Policyholder under the Policy Number shown on the face page. We, Us or Our means the insurance company named on the face page of The Policy. You or Your means the person to whom this certificate is issued. 52 AMENDATORY RIDER This rider is attached to all certificates given in connection with The Policy and is effective on The Policy Effective Date. This rider is intended to amend Your certificate, as indicated below, to comply with the laws of Your state of residence. Only those references to benefits, provisions or terms actually included in Your certificate will affect Your coverage. In addition, any reference made herein to Dependent coverage will only apply if Dependent coverage is provided in Your certificate. For California residents: 1) The following is added to the definition of Spouse: Spouse will also include an individual who is in a registered domestic partnership with You in accordance with California law. References to Your marriage or divorce will include Your registered domestic partnership or dissolution of Your registered domestic partnership. 2) The following is added to the definition of Dependent Child(ren): Dependent Child(ren) will also include child(ren) of Your California registered domestic partner. For Colorado residents, the Suicide provision will only exclude amounts of life insurance in effect within the first year of coverage or within the first year following an increase in coverage. For Connecticut residents: 1) The definition of Dependent Child(ren) is amended to include relationships due to domestic partnership. 2) The following is added to the definition of Spouse: Spouse will include Your domestic partner, provided You have executed a domestic partner affidavit satisfactory to Us, establishing that You and Your partner are domestic partners for the purposes of The Policy. You will continue to be considered domestic partners provided You continue to meet the requirements described in the domestic partner affidavit. For Louisiana residents: 1) The definition of Dependent Child(ren) is replaced by the following: Dependent Child(ren) means: 1) Your unmarried children, stepchildren, legally adopted children; 2) unmarried child who is placed in your home pursuant to an adoption placement agreement; executed with a licensed adoption agency (from the date of placement in your home); 3) an unmarried child who is placed in your home following execution of an act of voluntary surrender (as of the date on which the act of voluntary surrender becomes irrevocable); 4) Your unmarried grandchildren who are in Your legal custody and live with You; or 5) any other children related to You by blood or marriage who live with You in a regular parent-child relationship; provided such children are primarily dependent upon You for financial support and maintenance and are: 1) from live birth to age 21 years; 2) age 21, but under age 24, and in full-time attendance at an accredited institution of learning. If a student is attending a Louisiana vocational, technical, vocational-technical, or trade school or institute on a fulltime basis, as defined by the institution, then we will consider the student to have satisfied the requirements of full-time attendance for The Policy; 3) Coverage will be continued for a child up to age 24 who is deemed to be unable to attend school full-time due to a mental or nervous condition, problem or disorder; or 4) age 21 or older and disabled. Such children must have become disabled before attaining age 21. You must submit proof, satisfactory to Us, of such children’s disability. 2) The definition of Dependent is replaced by the following: Dependent means Your Spouse and Your Dependent Child(ren). A dependent must be a citizen or legal resident of the United States, its territories and protectorates. Any person who is in full-time military service cannot be a dependent, unless that person is subsequently called to military service and any required premium is paid. 3) Any and all references to Domestic Partners are hereby deleted. 53 4) The age limit stated in the Continuation for Dependent Children with Disabilities provision is increased to 21, if less than 21. 5) The following provision is added to the Period of Coverage provisions: Reinstatement after Military Service: If: 1) Your coverage terminates because You enter active military service; and 2) You are rehired within 12 months of the date Your coverage terminated/within 12 months of the date You return from active military service; then coverage for You and Your previously covered Dependent Spouse/Dependents may be reinstated, provided You request such reinstatement within 31 days of the date You return to work. The reinstated coverage will: 1) be the same coverage amounts in force on the date coverage terminated; and 2) not be subject to any Waiting Period for Coverage, Evidence of Insurability or Pre-existing Conditions Limitations; and 3) be subject to all the terms and provisions of The Policy. 6) The last paragraph of the Claims to be Paid provision is replaced by the following: In addition, We may, at Our option, pay a portion of Your Life Insurance Benefit up to $500 to any person equitably entitled to payment because of expenses from Your funeral or other expenses incident to Your last illness or death. Payment to any person, as shown above, will release Us from liability for the amount paid. 7) The exclusion for the Seatbelt and Air Bag benefit is replace by the following: The Seat Belt and Air Bag Benefit will not be payable if the injured person is operating the Motor Vehicle at the time of Injury while: 1) Intoxicated; or 2) under the influence of narcotics, unless administered on the advice of a physician. 8) The drug exclusion in the Accidental Death and Dismemberment Exclusions is replaced by the following: Injury sustained while under the influence of narcotics, unless administered on the advice of a Physician; For Maryland residents: 1) The definition of Dependent Child(ren) is amended to include relationships due to domestic partnership. 2) The following is added to the definition of Spouse: Spouse will include Your domestic partner, provided You have executed a domestic partner affidavit satisfactory to Us, establishing that You and Your partner are domestic partners for the purposes of The Policy. You will continue to be considered domestic partners provided You continue to meet the requirements described in the domestic partner affidavit. For Minnesota residents: 1) The term "granted military leave of absence" in the Military Leave of Absence portion of the Continuation Provisions section, is amended to "documented military leave of absence." 2) The following applies to You if there are more than 25 residents of Minnesota who are covered under The Policy and those 25 residents constitute 25% or more of the total number of people covered under The Policy: The provision titled "Lay Off" is deleted from the Continuation Provisions and is replaced by the following: Lay Off: If You are voluntarily or involuntarily terminated or Laid Off, You may elect to continue Your coverage by making monthly premium payments to the Employer for the cost of continued coverage. You must elect this continued coverage within 60 days from: 1) the date Your coverage would otherwise terminate; or 2) the date You receive a written notice of Your right to continue coverage; whichever is later. The amount of premium charged may not exceed 102% of the premium paid, either by You or the Employer, for life insurance coverage for an Active Employee. The Employer will inform You of: 1) Your right to continue coverage; 2) the amount of monthly premium; and 3) how, where and by when payment must be made. Upon request, the Employer will provide You Our written verification of the cost of coverage. Coverage will continue until the first to occur of: 1) the date You are covered under another group policy; or 2) the last day of the 18th month following the date of termination or layoff. At the end of such 18 month period, You may exercise the Conversion Right if You do so within the time limits described in such provision. However, in lieu of conversion coverage You may accept a policy providing reduced benefits at a reduced premium rate. Minnesota law requires that if Your coverage ends because the Employer fails: 1) to notify You of Your right to continue coverage; or 2) to pay the premium after timely receipt; 54 the Employer will be liable for benefit payments to the extent We would have been liable had You still been covered. Laid Off means that there is a reduction in the number of hours You work for the Employer so that You are no longer eligible for coverage. The term termination does not include discharge for gross misconduct but does include retirement. 3) the 7th paragraph of the Accelerated Benefit provision is deleted. 4) the 2nd, 3rd and 4th paragraphs of the Conversion Right provision are deleted. 5) The first sentence of the 5th paragraph of the Claims to be Paid provision is amended as follows: If benefits are payable and are greater than $15,000, then You or Your beneficiary may request that We pay benefits into a draft book account (checking account) which will be owned by: 1) You, if living; or 2) Your beneficiary, in the event of Your death. For Missouri residents: 1) The time periods stated in the Conditions for Qualification and the Benefit Payable before Approval of Waiver of Premium provisions are changed to 180 days, if greater than180 days. 2) The following language is added to the When Premiums are Waived provision: If Waiver of Premium is approved, it will be retroactive to the date the disability began. Premiums will be waived retrospectively once You have completed the 180 day waiting period. 3) The Suicide provision is replaced by the following: Suicide: What benefit is payable if death is a result of suicide? If You or Your Dependent commit suicide, whether sane or insane, We will not pay any Supplemental Amount of Life Insurance or Supplemental Amount of Dependent Life Insurance for the deceased person which was elected within the 1 year period immediately prior to the date of death. This applies to initial coverage and elected increases in coverage. It does not apply to benefit increases that resulted solely due to an increase in Earnings. If You or Your Dependent die as a result of suicide, whether sane or insane, within 1 year of the Policy effective date, all premiums paid for coverage will be refunded. This 1 year period includes the time group life insurance coverage was in force under the Prior Policy. For Montana residents: 1) The time period stated in the Conversion Right provision is changed to 3 years, if greater than 3 years. 2) The dollar amount stated in the Conversion Right provision is changed to $10,000, if less than $10,000. 3) The 2nd paragraph of the Conversion Policy Provisions is deleted. 4) The dollar amount stated in the second paragraph of the Claims to be Paid provision is changed to $500, if not $500. 5) The following provision is added to the Claims to be Paid provision. Payable Interest: Is interest payable on death claims? Claims payable for loss of life will be paid within 60 days of the date due proof is received. If the claim is paid more than 30 days after the date due proof is received, the amount payable will include interest. Interest will be paid at the discount rate, on 90-day commercial paper, in effect at the Federal Reserve Bank in the Ninth Federal Reserve District on the date due proof is received. For New Hampshire residents: 1) The Waiver of Premium and Disability Extension provision or the Disability Extension provision is deleted 2) The following is added to the end of the first paragraph of the Conversion provision: The Notice of Conversion Right form will be mailed to You within 15 days after the Policy ceases. If notice is given more than 15 days after the Policy ceases, the time You have to convert will be extended for 15 days from the date notice was given. 3) The last sentence of the second paragraph of the Conversion provision is replaced by the following: However, unless you did not have notice, We will not accept requests for Conversion if they are received more than 91 days after Life Insurance terminates. 4) Item #3 in the second paragraph of the Sending Proof of Loss provision is deleted. 5) The dollar amount stated in the second paragraph of the Claims to be Paid provision is changed to $250, if not $250. 6) The following is added to the Period of Coverage if Spouse Accidental Death and Dismemberment is included in the contract: Spouse Continuation: Can coverage be continued for a divorced Spouse? If You are legally separated or divorced from Your Spouse, coverage for Your former Spouse may continue under The Policy until the earliest of: 1) the last day of the third year following the anniversary of a final divorce or legal separation; 55 2) 3) 4) 5) 6) the date You remarry; the date Your former Spouse remarries; a date specified in the final divorce decree; the date Your former Spouse fails to pay any premiums that may be due; or the date You die. For North Dakota residents, the Suicide provision will only exclude amounts of life insurance in effect within the first year of coverage or within the first year following an increase in coverage. For Oregon residents: 1) The following is added to the definition of Spouse: Spouse will also include an individual who is in a registered domestic partnership with You in accordance with Oregon law. References to Your marriage or divorce will include Your registered domestic partnership or dissolution of Your registered domestic partnership. 2) The following is added to the definition of Dependent Child(ren): Dependent Child(ren) will also include child(ren) of Your Oregon registered domestic partner. For South Carolina residents: 1) The following is added to the Physical Examinations and Autopsy provision: "Such autopsy must take place in the state of South Carolina." 2) The dollar amount stated in the second paragraph of the Claims to be Paid provision is changed to $2,000, if not $2,000. For South Dakota residents: 1) The suicide, felony, speed or endurance contest exclusions are replaced by the following: suicide, whether sane or insane, within two years of the individual’s coverage under the policy; Injury caused directly or indirectly by riding or driving on land, air, or water if participating in a speed or endurance contest; Injury sustained while committing a felony. 2) The self-inflicted Injury, drug, Intoxicated and Driving while Intoxicated exclusions are deleted. 3) The definition of “Intoxicated” is deleted from the Exclusion section. 4) The exclusions set forth in the Seat Belt and Air Bag benefit are deleted. 5) The definition of Felonious Assault set forth in the Felonious Assault Benefit is replaced by the following: Felonious Assault means a violent or criminal act directed at You or Your Dependents during the course of a robbery, kidnapping or criminal assault, which constitutes a felony under the law. For Utah residents: 1) The time period stated in the Suicide provision is changed to 2 years if not already 2 years. 2) Item 1 of the first paragraph in the Conversion Policy Provisions is replaced by the following: 1) be issued on one of the Life Insurance policy forms the Insurer is customarily issuing at the age and for the amount applied for at the time of conversion except for term insurance; and 3) The following sentence is added to the Effect of Waiver of Premium on Conversion provision, if not already added: The Insurer will refund the premium paid for such Conversion Policy. 4) The time period stated in the Claim Forms provision is changed to 15 days if not already 15 days. 5) Item 3 of the second paragraph of the Sending Proof of Loss provision is deleted. 6) The time period stated in the Claim Payment provision is changed to 15 days if not already 15 days. 7) The provision titled Policy Interpretation is deleted in its entirety. 8) The words "In the absence of fraud" are deleted from the Incontestability provision. 9) The following provision is added to the Continuation provisions: Disability: If You are not Actively at Work due a Disability, all of Your coverage (including Dependent Life coverage) may be continued beyond a date shown in the Termination provision. Coverage may not be continued under more than one Continuation Provision. The amount of continued coverage applicable to You or Your Dependents will be the amount of coverage in effect on the date immediately before coverage would otherwise have ended. Coverage will continue until the earliest of: 1) six months from the date of Disability; 2) approval by Us of continuation of the coverage under any disability provision The Policy may contain; 3) the date premium payment is due but not paid; 4) The Policy terminates; or 5) if the Policyholder is a trust, Your Employer ceases to be a Participating Employer. 56 In no event will the amount of insurance increase while coverage is continued in accordance with this provision. The Continuation Provisions shown above may not be applied consecutively. If such absence results in a leave of absence in accordance with state and/or federal family and medical leave laws, then the combined continuation period will not exceed twelve consecutive months. For Vermont residents: The following Endorsement applies: Purpose: This endorsement is intended to provide benefits for parties to a civil union. Vermont law requires that insurance contracts and policies offered to married persons and their families be made available to parties to a civil union and their families. In order to receive benefits in accordance with this endorsement, the civil union must have been established in the state of Vermont according to Vermont law. General Definitions, Terms, Conditions and Provisions: The general definitions, terms, conditions or any other provisions of the policy, contract, certificate and/or riders and endorsements to which this mandatory endorsement is attached are hereby amended and superseded as follows: 1) Terms that mean or refer to a marital relationship or that may be construed to mean or refer to a marital relationship: such as "marriage", "spouse", "husband", "wife", "dependent", "next of kin", "relative", "beneficiary", "survivor", "immediate family" and any other such terms include the relationship created by a civil union. 2) Terms that mean or refer to a family relationship arising from a marriage such as "family", "immediate family", "dependent", "children", "next of kin", "relative", "beneficiary", "survivor" and any other such terms include the family relationship created by a civil union. 3) Terms that mean or refer to the inception or dissolution of a marriage, such as "date of marriage", "divorce decree", "termination of marriage" and any other such terms include the inception or dissolution of a civil union. 4) "Dependent" means a spouse, a party to a civil union, and/or a child or children (natural, stepchild, legally adopted or a minor who is dependent on the insured for support and maintenance) who is born to or brought to a marriage or to a civil union. 5) "Child or covered child" means a child (natural, step-child, legally adopted or a minor who is dependent on the insured for support and maintenance) who is born to or brought to a marriage or to a civil union. Cautionary Disclosure: THIS RIDER IS ISSUED TO MEET THE REQUIREMENTS OF VERMONT LAW AS EXPLAINED IN THE "PURPOSE" PARAGRAPH OF THE RIDER. THE FEDERAL GOVERNMENT OR ANOTHER STATE GOVERNMENT MAY NOT RECOGNIZE THE BENEFITS GRANTED UNDER THIS RIDER. YOU ARE ADVISED TO SEEK EXPERT ADVICE TO DETERMINE YOUR RIGHTS UNDER THIS CONTRACT. For Virginia residents, any and all references to Domestic Partners are hereby deleted. For Washington residents: 1) The Suicide provision is deleted in its entirety. 2) The following is added to the No Longer Terminally Ill provision: Dispute about Diagnosis: If Your attending physician, and a physician appointed by Us, disagree on whether You are Terminally Ill, Our physician’s opinion will not be binding upon You. The two parties shall attempt to resolve the matter promptly and amicably. In case the disagreement is not resolved, You have the right to mediation or binding arbitration conducted by a disinterested third party who has no ongoing relationship with either. Any such arbitration shall be conducted in accordance with the laws of the State of Washington. As part of the final decision, the arbitrator or mediator shall award the costs of the arbitrator to one party or the other, or may divide the costs equally or otherwise. 3) The Labor Dispute continuation provision is replaced with the following: Labor Dispute: If You are not Actively at Work as the result of a labor dispute, all of Your coverages (including Dependent Life coverage) may be continued during such dispute until the last day of the month in which the coverage terminated, but in no event for a period exceeding six months. If the labor dispute ends, this continuation will cease immediately. 4) The provision titled Policy Interpretation is deleted in its entirety. 5) The definition of Dependent Child(ren) is amended to include relationships due to domestic partnership. 6) The following is added to the definition of Spouse: Spouse will include Your domestic partner, provided You have executed a domestic partner affidavit satisfactory to Us, establishing that You and Your partner are domestic partners for the purposes of The Policy. You will continue to be considered domestic partners provided You continue to meet the requirements described in the domestic partner affidavit. For Wisconsin residents: 57 1) The dollar amount stated in the Conversion Right provision is changed to $5,000, if not $5,000. 2) The dollar amounts stated in the second paragraph and the last paragraph of the Claims to be Paid provision are changed to $1,000, if not $1,000. In all other respects, the Policy and certificates remain the same. Signed for Hartford Life and Accident Insurance Company. Richard G. Costello, Secretary John C. Walters, President 58 Questions about Your Coverage In the event You have questions regarding any aspect of Your coverage, You should contact Your Employee Benefits Manager or You may write to us at: The Hartford Group Benefits Division, Customer Service P.O. Box 2999 Hartford, CT 06104-2999 Or call Us at: 1-800-523-2233 When calling, please give Us the following information: 1) the policy number; and 2) the name of the policyholder (employer or organization), as shown in Your Certificate of Insurance. Or You may contact Our Sales Office: Hartford Life and Accident Insurance Company Group Sales Department 2 Bala Plaza Suite 400 Bala Cynwyd, PA 19004 TOLL FREE: 866-610-6640 FAX: 610-538-1859 If you have a complaint, and contacts between you and the insurer or an agent or other representative of the insurer have failed to produce a satisfactory solution to the problem, the following states require we provide you with additional contact information: For Residents of: Arkansas Write Arkansas Insurance Department Consumer Services Division 1200 West Third Street Little Rock, AR 72201-1904 Telephone 1(800) 852-5494 California State of California Insurance Department Consumer Communications Bureau 300 South Spring Street, South Tower Los Angeles, CA 90013 1(800) 927-HELP Illinois Illinois Department of Insurance Consumer Services Station Springfield, Illinois 62767 Consumer Assistance: 1(866) 445-5364 Officer of Consumer Health Insurance: 1(877) 527-9431 Indiana Public Information/Market Conduct Indiana Department of Insurance 311 W. Washington St. Suite 300 Indianapolis, IN 46204-2787 Consumer Hotline: 1(800) 622-4461 1(317) 232-2395 (in the Indianapolis Area) Virginia Life and Health Division Bureau of Insurance P.O. Box 1157 Richmond, VA 23209 1(804) 371-9741 (inside Virginia) 1(800) 552-7945 (outside Virginia) Wisconsin Office of the Commissioner of Insurance Complaints Department P.O. Box 7873 Madison, WI 53707-7873 1(800) 236-8517 (outside of Madison) 1(608) 266-0103 (in Madison) to request a complaint form. The following states require that We provide these notices to You about Your coverage: For residents of: Arizona This certificate of insurance may not provide all benefits and protections provided by law in Arizona. Please read This certificate carefully. The benefits of the policy providing you coverage are governed primarily by the law of a state other than Florida. The group insurance policy providing coverage under this certificate was issued in a jurisdiction other than Maryland and may not provide all the benefits required by Maryland law. The benefits of the policy providing your coverage are governed primarily by the law of a state other than Montana. Florida Maryland Montana Georgia The laws of the state of Georgia prohibit insurers from unfairly discriminating against any person based upon his or her status as a victim of family abuse. North Carolina UNDER NORTH CAROLINA GENERAL STATUTE SECTION 58-50-40, NO PERSON, EMPLOYER, FINANCIAL AGENT, TRUSTEE, OR THIRD PARTY ADMINISTRATOR, WHO IS RESPONSIBLE FOR THE PAYMENT OF GROUP LIFE INSURANCE, GROUP HEALTH OR GROUP HEALTH PLAN PREMIUMS, SHALL: 1) CAUSE THE CANCELLATION OR NONRENEWAL OF GROUP LIFE INSURANCE, GROUP HEALTH INSURANCE, HOSPITAL, MEDICAL, OR DENTAL SERVICE CORPORATION PLAN, MULTIPLE EMPLOYER WELFARE ARRANGEMENT, OR GROUP HEALTH PLAN COVERAGES AND THE CONSEQUENTIAL LOSS OF THE COVERAGES OF THE PERSON INSURED, BY WILLFULLY FAILING TO PAY THOSE PREMIUMS IN ACCORDANCE WITH THE TERMS OF THE INSURANCE OR PLAN CONTRACT; AND 2) WILLFULLY FAIL TO DELIVER, AT LEAST 45 DAYS BEFORE THE TERMINATION OF THOSE COVERAGES, TO ALL PERSONS COVERED BY THE GROUP POLICY WRITTEN NOTICE OF THE PERSON'S INTENTION TO STOP PAYMENT OF PREMIUMS. VIOLATION OF THIS LAW IS A FELONY. ANY PERSON VIOLATING THIS LAW IS ALSO SUBJECT TO A COURT ORDER REQUIRING THE PERSON TO COMPENSATE PERSONS INSURED FOR EXPENSES OR LOSSES INCURRED AS A RESULT OF THE TERMINATION OF THE INSURANCE. IMPORTANT TERMINATION INFORMATION YOUR INSURANCE MAY BE CANCELLED BY THE COMPANY. PLEASE READ THE TERMINATION PROVISION IN THIS CERTIFICATE. THIS CERTIFICATE OF INSURANCE PROVIDES COVERAGE UNDER A GROUP MASTER POLICY. THIS CERTIFICATE PROVIDES ALL OF THE BENEFITS MANDATED BY THE NORTH CAROLINA INSURANCE CODE, BUT YOU MAY NOT RECEIVE ALL OF THE PROTECTIONS PROVIDED BY A POLICY ISSUED IN NORTH CAROLINA AND GOVERNED BY ALL OF THE LAWS OF NORTH CAROLINA. IMPORTANT NOTICE Texas AVISO IMPORTANTE To obtain information or make a complaint: Para obtener informacion o para someter una queja: You may call The Hartford's toll-free telephone number for information or to make a complaint at: Usted puede llamar al numero de telefono gratis de The Hartford para informacion o para someter una queja al: 1-800-523-2233 1-800-523-2233 You may also write to The Hartford at: P.O. Box 2999 Hartford, CT 06104-2999 Usted tambien puede escribir a The Hartford: P.O. Box 2999 Hartford, CT 06104-2999 You may contact the Texas Department of Insurance to obtain information on companies, coverages, rights or complaints at: Puede comunicarse con el Departamento de Seguros de Texas para obtener informacion acerca de companias, coberturas, derechos o quejas al: 1-800-252-3439 1-800-252-3439 You may write the Texas Department of Insurance at: P.O. Box 149104 Austin, TX 78714-9410 Fax # (512) 475-1771 Web: http://www.tdi.state.tx.us E-mail: ConsumerProtection@tdi.state.tx.us Puede escribir al Departamento de Seguros de Texas: P.O. Box 149104 Austin, TX 78714-9410 Fax # (512) 475-1771 Web: http://www.tdi.state.tx.us E-mail: ConsumerProtection@tdi.state.tx.us PREMIUM OR CLAIM DISPUTES: Should you have a dispute concerning your premium or about a claim you should contact the agent or The Hartford first. If the dispute is not resolved, you may contact the Texas Department of Insurance. DISPUTAS SOBRE PRIMAS O RECLAMOS: Si tiene una disputa concerniente a su prima o a un reclamo, debe comunicarse con el agente o The Hartford primero. Si no se resuelve la disputa, puede entonces comunicarse con el departamento (TDI). THIS IS NOT A POLICY OF WORKERS' COMPENSATION INSURANCE. THE EMPLOYER DOES NOT BECOME A SUBSCRIBER TO THE WORKERS' COMPENSATION SYSTEM BY PURCHASING THIS POLICY, AND IF THE EMPLOYER IS A NON-SUBSCRIBER, THE EMPLOYER LOSES THOSE BENEFITS WHICH WOULD OTHERWISE ACCRUE UNDER THE WORKERS' COMPENSATION LAWS. THE EMPLOYER MUST COMPLY WITH THE WORKERS' COMPENSATION LAW AS IT PERTAINS TO NON-SUBSCRIBERS AND THE REQUIRED NOTIFICATIONS THAT MUST BE FILED AND POSTED. CERTIFICATE OF INSURANCE HARTFORD LIFE AND ACCIDENT INSURANCE COMPANY Simsbury, Connecticut (A stock insurance company) Policyholder: DREXEL UNIVERSITY Policy Number: ADD-S07332 Policy Effective Date: January 1, 2010 Policy Anniversary Date: January 1, 2011 We have issued The Policy to the Policyholder. Our name, the Policyholder's name and The Policy Number are shown above. The provisions of The Policy, which are important to You, are summarized in this certificate consisting of this form and any additional forms which have been made a part of this certificate. This certificate replaces any other certificate We may have given to You earlier under The Policy. The Policy alone is the only contract under which payment will be made. Any difference between The Policy and this certificate will be settled according to the provisions of The Policy on file with Us at Our home office. The Policy may be inspected at the office of the Policyholder. Signed for the Company Richard G. Costello, Secretary John C. Walters, President A note on capitalization in this Certificate: Capitalization of a term, not normally capitalized according to the rules of standard punctuation, indicates a word or phrase that is a defined term in The Policy or refers to a specific provision contained herein. Table of Contents Schedule of Insurance Period of Coverage Benefits Exclusions General Provisions Definitions Amendatory Rider GBD-1300 A.1 (ADD-S07332) 1.05 SCHEDULE OF INSURANCE Cost of Coverage: Contributory Coverage: Supplemental Accidental Death and Dismemberment Insurance Supplemental Dependents' Accidental Death and Dismemberment Insurance Eligible Class(es) For Coverage: All Full-Time and Part-Time Active Employees and Faculty Members who are citizens or legal residents of the United States, its territories and protectorates, excluding Stationary Engineers, President(s) of the University, temporary, leased or seasonal employees. With respect to Faculty Members: Full-time Employees: at least 12 credit hours per term or 36 credit hours per academic year. Part-time Employees: at least 20 hours weekly. With respect to all other Employees: Full-time Employees: at least 40 hours weekly. Part-time Employees: at least 20 hours weekly. Annual Enrollment Period: as determined by Your Employer on a yearly basis. Eligibility Waiting Period for Coverage: None Accidental Death and Dismemberment Benefit (AD&D) Supplemental AD&D Principal Sum Principal Sum The Principal Sum applicable to You is the amount for which: a) You are eligible to request as determined below; b) You have given us a Written Request; and c) the required premium is paid. Principal Sum Amount: 1, 2, 3, or 4 times Earnings, subject to a Maximum Amount of $1,000,000 rounded to the next higher $1,000 if not already a multiple of $1,000. Principal Sum for each of Your Eligible Dependents Principal Sum for Your Eligible Spouse: Option 1: Principal Sum Amount: $25,000 Option 2: Principal Sum Amount: $50,000 Option 3: Principal Sum Amount: $100,000 63 Principal Sum for Your Eligible Children: Principal Sum Amount: $10,000 Additional Benefits Seat Belt and Air Bag Coverage: Seat Belt Benefit Amount: 10% of Principal Sum to a maximum amount of $5,000 Air Bag Benefit Amount: 10% of Principal Sum to a maximum amount of $5,000 Day Care Benefit: Maximum Amount: $5,000 Day Care Benefit Percentage: 3% Coma Benefit: Waiting Period: 30 day(s) Continuation of Medical Coverage (COBRA) Benefit: Maximum Benefit Amount: $3,000 Percentage for the Continuation of Medical Coverage Benefit: 2% Conversion Right Conversion Limit: $250,000 ELIGIBILITY AND ENROLLMENT Eligible Persons: Who is eligible for coverage? All persons in the class or classes shown in the Schedule of Insurance will be considered Eligible Persons. Eligibility for Coverage: When will I become eligible? You will become eligible for coverage on the latest of: 1) the Policy Effective Date; 2) the date You become a member of an Eligible Class; or 3) the date You complete the Eligibility Waiting Period for coverage shown in the Schedule of Insurance, if applicable. Eligibility for Dependent Coverage: When will I become eligible for Dependent Coverage? You will become eligible for Dependent coverage on the later of: 1) the date You become eligible for employee coverage; or 2) the date You acquire Your first Dependent. You may not cover Your Dependent if such Dependent is covered as an Employee under The Policy. No person can be insured as a Dependent of more than one Employee under The Policy. Enrollment: How do I enroll for coverage? To enroll You must: 1) complete and sign a group insurance enrollment form which is satisfactory to Us, for Your coverage and Your Dependent's coverage; and 2) deliver it to Your Employer. You have the option to enroll electronically. Your Employer will provide instructions. If You do not enroll for Your coverage and/or Your Dependent's coverage within 31 days after becoming eligible under The Policy, or if You were eligible to enroll under the Prior Policy and did not do so, and later choose to enroll, You may enroll for Your coverage and/or Your Dependent's coverage only: 1) during an Annual Enrollment Period designated by the Policyholder; or 64 2) within 31 days of the date You have a Change in Family Status. Change in Family Status: What constitutes a Change in Family Status? A Change in Family Status occurs when: 1) You get married or You execute a domestic partner affidavit; 2) You and Your spouse divorce or terminate a domestic partnership; 3) Your child is born or You adopt or become the legal guardian of a child; 4) Your spouse or domestic partner dies; 5) Your child is no longer financially dependent on You or dies; 6) Your spouse is no longer employed, which results in a loss of group insurance; or 7) You have a change in classification from part-time to full-time or from full-time to part-time. PERIOD OF COVERAGE Effective Date: When does my coverage start? Coverage will start on the latest to occur of: 1) The date You become eligible, if You enroll on or before that date; or 2) the first day of January on or next following the last day of the Annual Enrollment Period, if You enroll during an Annual Enrollment Period; or 3) the date You enroll if You do so within 31 days of the date You are eligible. Any coverage for which Evidence of Insurability is required, will become effective on the later of: 1) the first of the month following the date You become eligible; or 2) the first of the month following the date We approve Your Evidence of Insurability. All Effective Dates of coverage are subject to the Deferred Effective Date provision. Deferred Effective Date: When will my effective date for coverage or a change in my coverage be deferred? If, on the date You are to become covered: 1) under The Policy; 2) for increased benefits; or 3) for a new benefit; You are not Actively at Work due to a physical or mental condition, such coverage will not start until the date You are Actively at Work. Continuity from a Prior Policy: Is there Continuity of Coverage from a Prior Policy? Your initial coverage under The Policy will begin, and will not be deferred if on the day before the Effective Date, You were insured under the Prior Policy, but on the Effective Date, You were not Actively at Work, but would otherwise meet the Eligibility requirements of The Policy. However, Your Amount of Insurance will be the amount of accidental death and dismemberment principal sum: 1) You had under the Prior Policy; or 2) shown in the Schedule of Insurance; reduced by any coverage amount: 1) that is in force, paid or payable under the Prior Policy; or 2) that would have been so payable under the Prior Policy had timely election been made. Such amount of insurance under this provision is subject to any reductions in The Policy and will not increase. Coverage provided through this provision ends on the first to occur of: 1) the last day of a period of 12 consecutive months after the Effective Date; 2) the date Your insurance terminates for any reason shown under the Termination provision; 3) the last day You would have been covered under the Prior Policy, had the Prior Policy not terminated; or 4) the date You are Actively at Work. However, if the coverage provided through this provision ends because You are Actively at Work, You may be covered as an Active Employee under The Policy. Dependent Effective Date: When does Dependent coverage start? Contributory Coverage will start on the latest to occur of: 65 1) The date You become eligible for Dependent coverage, if You have enrolled on or before that date; or 2) the first day of January on or next following the last day of the Annual Enrollment Period, if You enroll during an Annual Enrollment Period; or 3) the date You enroll, if You do so within 31 days from the date You are eligible for Dependent coverage. In no event will Dependent coverage become effective before You become eligible. Dependent Deferred Effective Date: When will the effective date for Dependent coverage or a change in coverage be deferred? If, on the date Your Dependent, other than a newborn, is to become covered: 1) under The Policy; 2) for increased benefits; or 3) for a new benefit; he or she is: 1) confined in a hospital; or 2) Confined Elsewhere; such coverage will not start until he or she: 1) is discharged from the hospital; or 2) is no longer Confined Elsewhere; and has engaged in all the normal and customary activities of a person of like age and gender, in good health, for at least 15 consecutive days. This Deferred Effective Date provision will not apply to disabled children who qualify under the definition of Dependent Children. Confined Elsewhere means Your Dependent is unable to perform, unaided, the normal functions of daily living, or leave home or other place of residence without assistance. Dependent Continuity from a Prior Policy: Is there Continuity of Coverage from a Prior Policy for my Dependents? If on the day before the Effective Date, You were covered with respect to Your Dependents under the Prior Policy, the Deferred Effective Date provision will not apply to initial coverage under The Policy for such Dependents. However, the Dependent Amount of Insurance will be the amount of accidental death and dismemberment insurance: 1) they had under the Prior Policy; or 2) shown in the Schedule of Insurance; reduced by any coverage amount: 1) that is in force, paid or payable under the Prior Policy; or 2) that would have been so payable under the Prior Policy had timely election been made. Change in Coverage: When may I change my coverage or coverage for my Dependents? After Your initial enrollment You may increase or decrease coverage for You or Your Dependents, or add a new Dependent to Your existing Dependent coverage: 1) during any Annual Enrollment Period designated by the Policyholder; or 2) within 31 days of the date of a Change in Family Status. Effective Date for Changes in Coverage: When will changes in coverage become effective? Any decrease in coverage will take effect on the date of the change. Any increase in coverage will take effect on the latest of: 1) the date of the change; and 2) the date requirements of the Deferred Effective Date provision are met. Termination: When will my coverage end? Your coverage will end on the earliest of the following: 1) the date The Policy terminates; 2) the date You are no longer in a class eligible for coverage, or the Policy no longer covers Your class; 3) the date the required premium is due but not paid; 4) the date Your Employer terminates Your employment; 5) the date You are no longer Actively at Work; unless continued in accordance with one of the Continuation Provisions. 66 Dependent Termination: When does coverage for my Dependent end? Coverage for Your Dependent will end on the earliest to occur of: 1) the date Your coverage ends; 2) the date the required premium is due but not paid; 3) the date You are no longer eligible for Dependent coverage; 4) the date We or the Employer terminate Dependent coverage; or 5) the date the Dependent no longer meets the definition of Dependent; unless continued in accordance with the continuation provisions. Continuation Provisions: Can my coverage and coverage for my Dependents be continued beyond the date it would otherwise terminate? Coverage can be continued by Your Employer beyond a date shown in the Termination provision, if Your Employer provides a plan of continuation which applies to all employees the same way. Coverage may not be continued under more than one Continuation Provision. The amount of continued coverage applicable to You or Your Dependents will be the amount of coverage in effect on the date immediately before coverage would otherwise have ended. Continued coverage: 1) is subject to any reductions in The Policy; 2) is subject to payment of premium; 3) may be continued up to the maximum time shown in the provisions; and 4) terminates if The Policy terminates. In no event will the amount of insurance increase while coverage is continued in accordance with the following provisions. In all other respects, the terms of Your coverage and coverage for Your Dependents remain unchanged. Leave of Absence: If You are on a documented leave of absence, other than Family and Medical Leave or Military Leave of Absence, Your coverage (including Dependent Accidental Death and Dismemberment coverage) may be continued for 12 week(s). If the leave terminates prior to the agreed upon date, this continuation will cease immediately. Military Leave of Absence: If You or Your Dependent enter active military service and are granted a military leave of absence in writing, Your coverage (including Dependent Accidental Death and Dismemberment coverage) may be continued for up to 1 month(s). If the leave ends prior to the agreed upon date, this continuation will cease immediately. Lay Off: If You are temporarily laid off by the Employer due to lack of work, Your coverage (including Dependent Accidental Death and Dismemberment coverage) may be continued for 60 days if You qualify for the Workers Assistance Retraining Act and for 12 months if You do not. If the lay-off becomes permanent, this continuation will cease immediately. Status Change: If You are: 1) employed by the Policyholder; and 2) no longer in an Eligible Class due to a reduction in the number of scheduled hours You work; Your coverage (including Dependent Accidental Death and Dismemberment coverage) may be continued until the end of the month from the date Your scheduled hours were reduced. Disability Insurance: If You are working for the Policyholder and: 1) are covered by; and 2) meet the definition of disabled under; a Group Disability Insurance Policy, issued by Us to Your Employer, Your coverage (including Dependent Accidental Death and Dismemberment coverage) may be continued as long as You continue to be Disabled as defined in the Group Disability Insurance Policy. Sickness or Injury: If You are not Actively at Work due to sickness or injury, all of Your coverages (including Dependent Accidental Death and Dismemberment coverage) may be continued as long as You continue to be Disabled as defined in the Group Disability Insurance Policy. Family and Medical Leave: If You are granted a leave of absence, in writing, in accordance with state and/or federal family and medical leave laws, all of Your coverages (including Dependent Accidental Death and Dismemberment coverage) may be continued for up to 12 weeks, or 26 weeks if You qualify for Family Military Leave, or longer if required by state law, following the date Your insurance would have terminated. If the leave of absence ends prior to the agreed upon date, this continuation will cease immediately. 67 Spouse Continuation: Can coverage for my Spouse be continued in the event of my death? If You die while Your Spouse is covered under The Policy, Your surviving Spouse may continue: 1) his or her coverage; and 2) coverage of Your Dependent Child(ren) who were covered by The Policy on the date of Your death. We must receive Your Spouse’s written request and the required premium to continue the coverage within 31 days of the Premium Due Date next following the date of Your death. Solely for the purpose of continuing the coverage, Your Spouse will be considered the insured person. However, Your Spouse's or any of the Dependent Child(ren)'s coverage will not continue beyond: 1) a date the coverage would otherwise have ended under the Dependent Termination provision; or 2) the Premium Due Date next following the date Your Spouse remarries. Dependent Continuation: Can coverage for my Dependents be continued if I die? If You die while insured under The Policy, the Accidental Death and Dismemberment Insurance coverage for Your Dependents in force at the time of Your death may be continued, until the earliest of: 1) the date the coverage would otherwise have ended under the Dependent Termination provision; 2) the date Your Spouse remarries, dies, or obtains coverage under another group plan; or 3) 5 years from Your date of death. Coverage continued under this provision will be Contributory Coverage and may not be increased. Continuation for Dependent Child(ren) with Disabilities: Will coverage for Dependent Children with Disabilities be continued? If Your Dependent Child(ren) reach the age at which they would otherwise cease to be a Dependent as defined, and they are: 1) age 19 or older; and 2) disabled; and 3) primarily dependent upon You for financial support; then Dependent Child(ren) coverage will not terminate solely due to age. However: 1) You must submit proof satisfactory to Us of such Dependent Child(ren)'s disability within 31 days of the date he or she reaches such age; and 2) such Dependent Child(ren) must have become disabled before attaining age 19. Coverage under The Policy will continue as long as: 1) You remain insured; 2) the child continues to meet the required conditions; and 3) any required premium is paid when due. However, no increase in the Amount of Dependent Accidental Death and Dismemberment Insurance for such Dependent Children will be available. We have the right to require proof, satisfactory to Us, as often as necessary during the first two years of continuation, that the child continues to meet these conditions. We will not require proof more often than once a year after that. Conversion Right: If my coverage under The Policy ends, do I have a right to conversion? If You or Your Dependents cease to be covered under The Policy because You cease to be eligible for coverage and: 1) The Policy has not terminated; and 2) You have paid any required premium; You have a Conversion Right as provided below. The Conversion Right allows You to request coverage under a conversion policy from the Insurer, without giving medical evidence of insurability, to cover Yourself and Your Dependents who are covered under The Policy on the date Your coverage ceases. Dependents who continue to be covered under The Policy in the same or a different class cannot be covered under Your converted policy. Insurer, as used for this Conversion Right, means Us or another insurance company which has agreed with Us to issue converted policies according to this conversion right. You must: 1) give the Insurer a written request for the converted policy; and 2) pay the Insurer the initial premium; 68 within 31 days after You cease to be covered under The Policy. The Conversion Right will provide a converted policy that: 1) will have the provisions, limitations and exclusions on the form the Insurer is issuing for this purpose at conversion; 2) will provide coverage on a twenty four hour a day basis; 3) will provide benefits for Accidental Death and Dismemberment alone; 4) will take effect on the date You cease to be covered under The Policy; 5) may exclude any condition excluded by The Policy; 6) will not pay for any loss covered by The Policy; 7) will provide a Principal Sum for You which will be: a) the amount of Your Principal Sum under The Policy on the date of conversion, rounded to the nearest $1,000, subject to a minimum of $25,000.00 and a maximum of $250,000, if You are under age 70; b) $25,000.00, if You are age 70 or older but less than age 75; or c) $12,500.00, if You are age 75 or older; 8) will have premiums based on the Insurer’s rates in effect for new applicants of Your class and age at conversion. The Principal Sum amounts for Your Dependents who become covered under the converted policy will be the amounts We are offering for this purpose at conversion. Reinstatement after Military Service: Can my coverage be reinstated after return from active military service? If: 1) Your coverage terminates because You enter active military service; and 2) You are rehired within 12 months of the date Your coverage terminated; then coverage for You and Your previously covered Spouse/Dependents may be reinstated, provided You request such reinstatement within 31 days of the date You return to work. The reinstated coverage will be the same coverage amounts in force on the date coverage terminated and will be subject to all the terms and provisions of The Policy. BENEFITS Exposure and Disappearance: What if Loss is due to exposure or disappearance? Exposure to the elements will be presumed to be Injury if: 1) it results from the forced landing, stranding, sinking or wrecking of a conveyance in which You or Your Dependents were an occupant at the time of the accident; and 2) The Policy would have covered an Injury resulting from the accident. We will presume that You or Your Dependents suffered Loss of life if: 1) the person’s body has not been found within one year after the disappearance of a conveyance in which he or she was an occupant at the time of its disappearance; 2) the disappearance of the conveyance was due to its accidental forced landing, stranding, sinking or wrecking; and 3) The Policy would have covered an Injury resulting from the accident. Seat Belt and Air Bag Benefit: When is the Seat Belt and Air Bag Benefit payable? If You or Your Dependents sustain an Injury that results in a Loss payable under the Accidental Death and Dismemberment Benefit, We will pay an additional Seat Belt and Air Bag Benefit if the Injury occurred while the injured person was: 1) a passenger riding in; or 2) the licensed operator of; a properly registered Motor Vehicle and was wearing a Seat Belt at the time of the Accident as verified on the police accident report. This Benefit will be paid: 1) after We receive Proof of Loss, in accordance with the Proof of Loss provision; and 2) according to the General Provisions of The Policy. If a Seat Belt Benefit is payable, We will also pay an Air Bag Benefit if the injured person was: 69 1) positioned in a seat equipped with a factory-installed Air Bag; and 2) properly strapped in the Seat Belt when the Air Bag inflated. The Seat Belt Benefit is the lesser of: 1) an amount resulting from multiplying the injured person’s amount of Principal Sum by the Seat Belt Benefit Percentage; or 2) the Maximum Amount for this Benefit. The Air Bag Benefit is the lesser of: 1) an amount resulting from multiplying the injured person’s amount of Principal Sum by the Air Bag Benefit Percentage; or 2) the Maximum Amount for this Benefit. If it cannot be determined that the injured person was wearing a Seat Belt at the time of Accident, a Minimum Benefit will be payable under the Seat Belt Benefit. Accident, for the purpose of this Benefit only, means the unintentional collision of a Motor Vehicle during which the injured person was wearing a Seat Belt. Air Bag means an inflatable supplemental passive restraint system installed by the manufacturer of the Motor Vehicle or its proper replacement parts installed as required by the Motor Vehicle’s manufacturer's specifications that inflates upon collision to protect an individual from Injury and death. An Air Bag is not considered a Seat Belt. Seat Belt means: 1) an unaltered belt, lap restraint, or lap and shoulder restraint installed by the manufacturer of the Motor Vehicle, or proper replacement parts installed as required by the Motor Vehicle’s manufacturer’s specifications; or 2) a child restraint device that meets the standards of the National Safety Council and is properly secured and used in accordance with applicable state law and installed according to the recommendations of its manufacturer for children of like age and weight. The specific amounts for this Benefit are shown in the Schedule of Insurance. Day Care Benefit: When is the Day Care Benefit payable? If You or Your Spouse sustains an Injury that results in Loss of life payable under the Accidental Death and Dismemberment Benefit, We will pay an additional Day Care Benefit for each of your Dependent Children who are covered if such Dependent Child is under age 13 at the time of Your or Your Spouse’s death. This Benefit will be paid: 1) after We receive proof of enrollment in a Day Care Program as described in this Benefit; and 2) according to the General Provisions of The Policy. We will make one Day Care Benefit payment each year, for a maximum of 4 Day Care Benefit payments, for each Dependent Child. The Benefit will be paid to the person who has primary responsibility for the Dependent Child's Day Care expenses. Proof of enrollment satisfactory to Us for each Dependent Child in a Day Care Program includes, but will not be limited to, the following: 1) a copy of the Dependent Child's approved enrollment application in a Day Care Program; 2) cancelled check(s) evidencing payment to a Day Care facility or Day Care provider; 3) a letter from the Day Care facility or Day Care provider stating that the Dependent Child: a) is attending a Day Care Program; or b) has been enrolled in a Day Care Program and will be attending within 365 days of the date of the death. th Proof of enrollment must be sent to Us prior to the last day of the 12 month following the date of death. If you die, the Day Care Benefit pays an amount equal to the lesser of: 1) the amount resulting from multiplying Your Principal sum by the Day Care Benefit Percentage; or 2) the Maximum Amount for this Benefit. If Your Spouse dies, the Day Care Benefit pays an amount equal to the lesser of: 1) the amount resulting from multiplying Your Spouse’s amount of Principal sum by the Day Care Benefit Percentage; or 70 2) the Maximum Amount for this Benefit. We will pay the Minimum Amount for this Benefit in accordance with the Claims to be Paid provision for payment of benefits for Loss of life if: 1) a Principal Sum is payable because of the deceased person’s death; and 2) no person qualifies as a Child eligible for the Day Care Benefit. Day Care or Day Care Program means a program of child care which: 1) is operated in a private home, school or other facility; 2) provides, and makes a charge for, the care of children; and 3) is licensed as a day care center or is operated by a licensed day care provider, if such licensing is required by the state or jurisdiction in which it is located; or 4) licensing is not required, provides childcare on a daily basis for 12 months a year. The specific amounts for this Benefit are shown in the Schedule of Insurance. Coma Benefit: When is the Coma Benefit payable? If, as the result of an Injury, You or Your Dependents: 1) are in a Coma within 31 days from the date of accident; and 2) remain continuously in a Coma for at least the number of days shown as the Waiting Period; We will pay 1% of the Coma Maximum Benefit Amount for each month after the Waiting Period that the injured person remains in a Coma. This Benefit will be paid: 1) after We receive Proof of Loss, in accordance with the Proof of Loss provision; and 2) according to the General Provisions of The Policy. We will pay the benefit until the earliest to occur of: 1) the end of the month in which the injured person dies; 2) the end of the month in which the injured person recovers from the Coma; or 3) when the total payment equals the Coma Maximum Benefit Amount. The Coma Maximum Benefit equals the injured person’s amount of Principal Sum less all other payments under The Policy for the Injury. Coma means complete and continuous: 1) unconsciousness; and 2) inability to respond to external or internal stimuli, as verified by a Physician. The specific amounts for this Benefit are shown in the Schedule of Insurance. Continuation of Medical Coverage (COBRA) Benefit: When is the Continuation of Medical Coverage (COBRA) Benefit payable? If You sustain an Injury that results in a Loss of life payable under the Accidental Death and Dismemberment Benefit, and Your Dependents: 1) are covered under The Policy; and 2) elect to continue medical coverage in accordance with the Consolidated Omnibus Reconciliation Act of 1988 (COBRA); We will pay a Continuation of Medical Coverage Benefit. This Benefit will be paid: 1) after We receive Proof of Loss, in accordance with the Proof of Loss provision; and 2) according to the General Provisions of The Policy. We will pay the COBRA Benefit in three annual installment amounts each equal to the lesser of: 1) the amount resulting from multiplying Your Principal Sum by the Percentage for the Continuation of Medical Coverage Benefit; or 2) the Maximum Amount for this Benefit. 71 The COBRA Benefit is payable to Your Dependents’ insurance carrier on the date We receive the bill for such continuation of coverage. If the Principal Sum is payable because of Your death; and 1) no person qualifies as a Dependent; or 2) Your Dependents do not elect to continue coverage pursuant to COBRA; We will pay the Minimum Amount for this Benefit in accordance with the Claims to be Paid provision of The Policy. The specific amounts for this Benefit are shown in the Schedule of Insurance. EXCLUSIONS Exclusions: What losses are not covered? The Policy does not cover any loss caused or contributed to by: 1) intentionally self-inflicted Injury; 2) suicide or attempted suicide, whether sane or insane; 3) war or act of war, whether declared or not; 4) Injury sustained while on full-time active duty as a member of the armed forces (land, water, air) of any country or international authority except Reserve National Guard Service; 5) 6) 7) 8) (We will refund the pro rata portion of any premium paid for You or Your Dependents while You or Your Dependents are in the armed forces on full-time active duty, for a period of two months or more. Written notice must be given to Us within 12 months of the date You or Your Dependents enter the armed forces); Injury sustained while On any aircraft except a Civil or Public Aircraft, or Military Transport Aircraft; Injury sustained while On any aircraft: a) as a pilot, crewmember or student pilot; b) as a flight instructor or examiner; c) if it is owned, operated or leased by or on behalf of the Policyholder, or any Employer or organization whose eligible persons are covered under The Policy; d) being used for tests, experimental purposes, stunt flying, racing or endurance tests; or Injury sustained while committing or attempting to commit a felony; or Injury sustained or contracted in consequence while driving. Intoxicated means: 1) the blood alcohol content; 2) the results of other means of testing blood alcohol level; or 3) the results of other means of testing other substances; that meet or exceed the legal presumption of intoxication, or under the influence, under the law of the state where the accident occurred. Reserve National Guard Service means: You or Your Dependents are: 1) attending or en route to or from any active duty training of less than sixty (60) days; 2) attending or en route to or from a service school of any duration; 3) taking part in any authorized inactive duty training; or 4) taking part as a unit member in a parade or exhibition authorized by official orders. GENERAL PROVISIONS Notice of Claim: When should I notify the Company of a claim? You, or the person who has the right to claim benefits, must give Us, written notice of a claim within 30 days after: 1) the date of death; or 2) the date of loss. If notice cannot be given within that time, it must be given as soon as reasonably possible after that. Such notice must include the claimant’s name, address and the Policy Number. Claim Forms: Are special forms required to file a claim? 72 We will send forms to the claimant to provide Proof of Loss, within 15 days of receiving a Notice of Claim. If We do not send the forms within 15 days, the claimant may submit any other written proof which fully describes the nature and extent of the claim. Proof of Loss: What is Proof of Loss? Proof of Loss may include, but is not limited to, the following: 1) a completed claim form; 2) a certified copy of the death certificate (if applicable); 3) Your Enrollment form; 4) Your Beneficiary Designation (if applicable); 5) any and all medical information, including x-ray films and photocopies of medical records, including histories, physical, mental or diagnostic examinations and treatment notes; 6) the names and addresses of all: a) Physicians or other qualified medical professionals You have consulted; b) hospitals or other medical facilities in which You have been treated; and c) pharmacies which have filled Your prescriptions within the past three years; 7) Your signed authorization for Us to obtain and release medical, employment and financial information (if applicable); or 8) Any additional information required by Us to adjudicate the claim. All proof submitted must be satisfactory to Us. Sending Proof of Loss: When must Proof of Loss be given? Written Proof of Loss must be sent within 90 day(s) after the loss. All Proof of Loss should be sent to Us. However, all claims should be submitted to Us within 90 day(s) of the date coverage ends. If proof is not given by the time it is due, it will not affect the claim if: 1) it was not possible to give proof within the required time; and 2) proof is given as soon as possible; but 3) not later than 1 year after it is due unless You, or the person who has the right to claim benefits, are not legally competent. Physical Examination and Autopsy: Can We have a claimant examined or request an autopsy? While a claim is pending We have the right at Our expense: 1) to have the person who has a loss examined by a Physician when and as often as We reasonably require; and 2) to have an autopsy performed in case of death where it is not forbidden by law. Claim Payment: When are benefit payments issued? When We determine that benefits are payable, We will pay the benefits in accordance with the Claims to be Paid provision, but not more than 30 day(s) after such Proof of Loss is received. Claims to be Paid: To whom will benefits for my claim be paid? Benefits for Loss of Life will be paid in accordance with the Beneficiary Designation. If no beneficiary is named, payment will be made according to the beneficiary designation under the group life policy issued to the Policyholder and in effect at the time of death. If no beneficiary is named, or if no named beneficiary survives You, We may, at Our option, pay: 1) the executors or administrators of Your estate; or 2) all to Your surviving Spouse; or 3) if Your Spouse does not survive You, in equal shares to Your surviving Child(ren); or 4) if no Child survives You, in equal shares to Your surviving parents. In addition, We may, at Our option, pay a portion of Your Accidental Death Benefit up to $500 to any person equitably entitled to payment because of expenses from Your burial. Payment to any person, as shown above, will release Us from liability for the amount paid. If any beneficiary is a minor, We may pay his or her share, until a legal guardian of the minor's estate is appointed, to a person who at Our option and in Our opinion is providing financial support and maintenance for the minor. We will pay: 1) $200 at Your death; and 2) monthly installments of not more than $200. Payment to any person as shown above will release Us from all further liability for the amount paid. 73 We will pay the Accidental Death and Dismemberment Insurance Benefit at Your Dependents' death to You, if living. Otherwise, it will be paid, at Our option, to Your surviving Spouse or the executors or administrators of Your estate. We will make any payments, other than for loss of life, to You. We may make any such payments owed at Your death to Your estate. If any payment is owed to: 1) Your estate; 2) a person who is a minor; or 3) a person who is not legally competent, then We may pay up to $1,000 to a person who is related to You and who, at Our sole discretion, is entitled to it. Any such payment shall fulfill Our responsibility for the amount paid. Beneficiary Designation: How do I designate or change my beneficiary? You may designate or change a beneficiary by doing so in writing on a form satisfactory to Us and filing the form with the Employer. Only satisfactory forms sent to the Employer prior to Your death will be accepted. Beneficiary designations will become effective as of the date You signed and dated the form, even if You have since died. We will not be liable for any amounts paid before receiving notice of a beneficiary change from the Employer. In no event may a beneficiary be changed by a Power of Attorney. Claim Denial: What notification will my Beneficiary or I receive if a claim is denied? If a claim for benefits is wholly or partly denied, You or Your beneficiary will be furnished with written notification of the decision. This written notification will: 1) give the specific reason(s) for the denial; 2) make specific reference to the provisions on which the denial is based; 3) provide a description of any additional information necessary to perfect a claim and an explanation of why it is necessary; and 4) provide an explanation of the review procedure. Claim Appeal: What recourse do my Beneficiary or I have if a claim is denied? On any claim, the claimant or his or her representative may appeal to Us for a full and fair review. To do so, he or she: 1) must request a review upon written application within: a) 180 days of receipt of claim denial if the claim requires Us to make a determination of disability; or b) 60 days of receipt of claim denial if the claim does not require Us to make a determination of disability; and 2) may request copies of all documents, records, and other information relevant to the claim; and 3) may submit written comments, documents, records and other information relating to the claim. We will respond in writing with Our final decision on the claim. Policy Interpretation: Who interprets the terms and conditions of The Policy? We have full discretion and authority to determine eligibility for benefits and to construe and interpret all terms and provisions of The Policy. Assignment: Are there any rights of assignment? You have the right to absolutely assign Your rights and interest under The Policy including, but not limited, to the following: 1) the right to make any contributions required to keep the insurance in force; 2) the right to convert; and 3) the right to name and change a beneficiary. We will recognize any absolute assignment made by You under The Policy, provided: 1) it is duly executed; and 2) a copy is acknowledged and on file with Us. We and the Policyholder assume no responsibility: 1) for the validity or effect of any assignment; or 2) to provide any assignee with notices which We may be obligated to provide to You. 74 You do not have the right to collaterally assign Your rights and interest under The Policy. Legal Actions: When can legal action be taken against Us? Legal action cannot be taken against Us: 1) sooner than 60 days after the date Proof of Loss is furnished; or 2) more than 3 years after the date Proof of Loss is required to be furnished according to the terms of The Policy. Workers' Compensation: How does The Policy affect Workers' Compensation coverage? The Policy does not replace Workers' Compensation or affect any requirement for Workers' Compensation coverage. Insurance Fraud: How does the Company deal with fraud? Insurance Fraud occurs when You, Your Dependents and/or Your Employer provide Us with false information or file a claim for benefits that contains any false, incomplete or misleading information with the intent to injure, defraud or deceive Us. It is a crime if You, Your Dependents and/or Your Employer commit Insurance Fraud. We will use all means available to Us to detect, investigate, deter and prosecute those who commit Insurance Fraud. We will pursue all available legal remedies if You, Your Dependents and/or Your Employer perpetrate Insurance Fraud. Misstatements: What happens if facts are misstated? In the absence of Insurance Fraud, if material facts about You or Your Dependents were not stated accurately: 1) the premium may be adjusted; and 2) the true facts will be used to determine if, and for what amount, coverage should have been in force. DEFINITIONS Active Employee means an employee who works for the Employer on a regular basis in the usual course of the Employer's business. This must be at least the number of hours shown in the Schedule of Insurance. Actively at Work means at work with Your Employer on a day that is one of Your Employer's scheduled workdays. On that day, You must be performing for wage or profit all of the regular duties of Your job: 1) in the usual way; and 2) for Your usual number of hours. We will also consider You to be Actively At Work on any regularly scheduled vacation day or holiday, only if You were Actively At Work on the preceding scheduled work day. Actively at Work does not include everyday travel to and from work. Airworthiness Certificate means: 1) the “Standard” Airworthiness Certificate issued by the United States Federal Aviation Administration (FAA); or 2) a foreign equivalent issued by the governmental authority with jurisdiction over civil aviation in the country of its registry. Civil or Public Aircraft means a civil or public aircraft which: 1) has a current and valid Airworthiness Certificate; 2) is piloted by a person who has a valid and current certificate of competency of a rating which authorizes him or her to pilot the aircraft; and 3) is not operated by the militia, or armed forces of any state, national government or international authority. Common Carrier means a conveyance operated by a concern, other than the Policyholder, organized and licensed for the transportation of passengers for hire and operated by that concern. Common Carrier will not mean any such conveyance which is hired or used for a sport, gamesmanship, contest, sightseeing, observatory and/or recreational activity, regardless of whether such conveyance is licensed. Contributory Coverage means coverage for which You are required to contribute toward the cost. Contributory Coverage is shown in the Schedule of Insurance. Dependent Child(ren) means: 75 1) Your unmarried children, stepchildren, legally adopted children, child in the process of adoption, foster child; or 2) any other children related to You by blood or marriage or domestic partnership who: a) live with You in a regular parent-child relationship; and/or b) You claimed as a dependent on Your last filed federal income tax return; provided such children are primarily dependent upon You for financial support and maintenance and are: 1) at least 14 days old but under age 19; 2) age 19, but under age 23, and in full-time attendance (at least 12 course credit hours per semester) at an accredited institution of learning. If the institution establishes full-time status in any other manner, We reserve the right to determine whether the student continues to qualify as a Dependent; or 3) age 19 or older and disabled. Such children must have become disabled before attaining age 19. You must submit proof, satisfactory to Us, of such children’s disability. Dependents means Your Spouse and Your Dependent Child(ren). A dependent must be a citizen or legal resident of the United States, its territories and protectorates. Any person who is in full-time military service cannot be a Dependent. Earnings means Your regular annual rate of pay, not counting bonuses, commissions, tips and tokens, overtime pay or any other fringe benefits or extra compensation, in effect on the last Policy Anniversary Date. However, if You are an hourly paid Employee, Earnings means the product of: 1) the average number of hours You worked per year, not including overtime, over the most recent 2 year period, immediately prior to the last Policy Anniversary Date, multiplied by: 2) Your hourly wage in effect on the last Policy Anniversary Date. Employer means the Policyholder. FAA means: 1) the Federal Aviation Administration of the United States; or 2) the equivalent aviation authority for the country of the aircraft's registry, if the governmental authority is recognized by the United States. Injury means bodily injury resulting: 1) directly from an accident; and 2) independently of all other causes; which occurs while You or Your Dependents are covered under The Policy. Loss resulting from: 1) sickness or disease, except a pus-forming infection which occurs through an accidental wound; or 2) medical or surgical treatment of a sickness or disease; is not considered as resulting from Injury. Military Transport Aircraft means a transport aircraft operated by: 1) the United States Air Mobility Command (AMC); or 2) a national military air transport service of a governmental authority recognized by the United States. Motor Vehicle means a self-propelled, four (4) or more wheeled: 1) private passenger: car, station wagon, van or sport utility vehicle; 2) motor home or camper; or 3) pick-up truck; not being used as a Common Carrier. A Motor Vehicle does not include farm equipment, snowmobiles, all-terrain vehicles, lawnmowers or any other type of equipment vehicles. Physician means a person who is: 1) a doctor of medicine, osteopathy, psychology or other legally qualified practitioner of a healing art that We recognize or are required by law to recognize; 2) licensed to practice in the jurisdiction where care is being given; 3) practicing within the scope of that license; and 4) not Related to You by blood or marriage. 76 Prior Policy means the group accidental death and dismemberment insurance Policy carried by the Policyholder on the day before the Policy Effective Date and will only include the coverage which is transferred to Us. Related means Your Spouse or other adult living with You, sibling, parent, step-parent, grandparent, aunt, uncle, niece, nephew, son, daughter, grandchild, or step-child or similar relationship in law. Spouse means Your spouse who is not legally separated or divorced from You. Spouse will include Your domestic partner provided you have executed a domestic partner affidavit acceptable to Us, establishing that You and Your partner are domestic partners for purposes of The Policy. You will continue to be considered domestic partners provided You continue to meet the requirements described in the domestic partner affidavit. The Policy means the policy which We issued to the Policyholder under the Policy Number shown on the face page. We, Us, or Our means the insurance company named on the face page of The Policy. You or Your means the person to whom this certificate is issued. 77 AMENDATORY RIDER This rider is attached to all certificates given in connection with The Policy and is effective on The Policy Effective Date. This rider is intended to amend Your certificate, as indicated below, to comply with the laws of Your state of residence. Only those references to benefits, provisions or terms actually included in Your certificate will affect Your coverage. In addition, any reference made herein to Dependent coverage will only apply if Dependent coverage is provided in Your certificate. For California residents: 1) The following is added to the definition of Spouse: Spouse will also include an individual who is in a registered domestic partnership with You in accordance with California law. References to Your marriage or divorce will include Your registered domestic partnership or dissolution of Your registered domestic partnership. 2) The following is added to the definition of Dependent Child(ren): Dependent Child(ren) will also include child(ren) of Your California registered domestic partner. For Indiana residents: The first paragraph of the Traumatic Brain Injury Benefit is deleted and is replaced by the following: If You or Your Dependents sustain an Injury that results in a Traumatic Brain Injury within 60 days of the date of accident which: 2) requires that the injured person be Hospitalized for at least 7 days during the first 60 days following the accident; and 3) the Traumatic Brain Injury continues for 12 consecutive months; We will pay a Traumatic Brain Injury Benefit. For Louisiana residents: 1) the following will be considered Dependent Child(ren) and are added to the definition of Dependent Child(ren): a) unmarried Child who is placed in your home pursuant to an adoption placement agreement; executed with a licensed adoption agency (from the date of placement in your home); b) an unmarried Child who is placed in your home following execution of an act of voluntary surrender (as of the date on which the act of voluntary surrender becomes irrevocable); c) your unmarried grandchild who is in your legal custody. 2) The child limiting age is changed to 21 years, or 24 years if a student, if less than such ages. 3) The following is added to the definition of Dependent Child(ren): "Coverage will be continued for a Child up to age 24 who is deemed to be unable to attend school full-time due to a mental or nervous condition, problem or disorder." 4) The following replaces the last sentence of the Dependents definition: "Any person who is in full-time military service cannot be a dependent, unless that person is subsequently called to military service and any required premium is paid." 5) The following provision is added: Reinstatement after Military Service: Can my coverage be reinstated after return from active military service? If: 1) Your coverage terminates because You enter active military service; and 2) You are rehired within 12 months of the date You return from active military service; then coverage may be reinstated, provided You request such reinstatement within 31 days of the date you return to work. The reinstated coverage will: 1) be the same coverage amounts in force on the date coverage terminated; and 2) not be subject to any Waiting Period for Coverage, Evidence of Insurability or Pre-existing Conditions Limitations; and 3) be subject to all the terms and provisions of The Policy. 78 For Maine residents: 1) The time period stated in the Notice of Claim provision is changed to 30 days if not already 30 days. 2) The time period stated in the Claim Forms provision is changed to 15 days if not already 15 days. 3) The time periods stated in the Sending Proof of Loss provision are changed to 90 days and 1 year if not already 90 days and 1 year, respectively. 4) The time period stated in the Claim Payment provision is changed to 30 days if not already 30 days. 5) The dollar amount stated in the Claims to be Paid provision is changed to $2,000 if not already $2,000. 6) The phrase "In the absence of Insurance Fraud" is deleted from the Misstatements provision. For Minnesota residents, the definition of Disabled or Total Disability in the Permanent Total Disability Benefit is replaced by the following: Disabled or Total Disability, for the purpose of this Benefit, means Your or Your Spouse's: 3) inability during the first two years of disability to perform the Essential Duties of Your or Your Spouse's Occupation; and 4) after that, Your or Your Spouse's inability to engage in Any Occupation for which you are suited by education, training and experience; or 5) with respect to a Spouse who is unemployed, his or her inability to engage in the normal and customary activities of a person of like age and gender in good health. You unemployed Spouse must be: 1) regularly attended by Physician; and 2) continuously confined within his or her house or Hospital, provided such house or Hospital confinement will not preclude transportation of Your Spouse to or from a Hospital or Physician's office for necessary treatment at the direction of his or her Physician. For Missouri residents, the suicide Exclusion is replaced by the following: "suicide or attempted suicide, while sane". For New Hampshire residents: 1) Item 1 of the definitions of Disabled and Disabled or Disability is replaced by the following: 1) perfoming any work or occupation for wage or profit for which You are, or become, reasonably qualified by reason of education, training or experience. 2) Item 3 of the last paragraph of the Sending Proof of Loss provision is deleted. 3) Item 3 of the Conditions for Qualification provision is replaced by the following: 1) provide such proof in accordance with the Sending Proof of Loss provision. 4) The Policy Interpretation provision is deleted. 5) The time period stated in the definition of Period of Confinement in the Accident Hospital Income Benefit, is changed to 180 days, if less than 180 days. 6) Item 1 of the definition of Extended Care Facility in the Extended Care Facility Benefit is replaced by the following: 1) Operates pursuant to law; 7) The following is added to the Period of Coverage: Spouse Continuation: Can coverage be continued for a divorced Spouse? If You are legally separated or divorced from Your Spouse, coverage for Your former Spouse may continue under The Policy until the earliest of: 1) the last day of the third year following the anniversary of a final divorce or legal separation; 2) the date You remarry; 3) the date Your former Spouse remarries; 4) a date specified in the final divorce decree; 5) the date Your former Spouse fails to pay any premiums that may be due; or 6) the date You die. For Oregon residents: 1) The following is added to the definition of Spouse: Spouse will also include an individual who is in a registered domestic partnership with You in accordance with Oregon law. References to Your marriage or divorce will include Your registered domestic partnership or dissolution of Your registered domestic partnership. 2) The following is added to the definition of Dependent Child(ren): Dependent Child(ren) will also include child(ren) of Your Oregon registered domestic partner. For South Carolina residents: 79 1) The time period in the Notice of Claim provision is changed to 20 days, if not already 20 days. 2) The following is added to the Physical Examinations and Autopsy provision: "Such autopsy must be performed during the period of contestability and must take place in the state of South Carolina." 3) Item 2 of the Legal Actions provision is replaced by the following: 2) 6 years of the date Proof of Loss is required to be furnished according to the terms of The Policy. For South Dakota residents, the provision titled Policy Interpretation is deleted in its entirety. For Utah residents: 1) The following benefits are not available: o Anti-Inflation Benefit o Therapeutic Counseling Benefit o Accidental Death Benefit with Double Indemnity while On a Common Carrier o Accidental Death Motor Vehicle Benefit o Accidental Death Benefit while in a Covered Accident o Accidental Death and Dismemberment: while Actively at Work o Double Indemnity while On A Common Carrier 2) The maximum age for a student, stated in the Child Education Benefit is changed to 26 if not already 26. 3) The definition of Dependent Child(ren) is amended as follows: 1) items a and b of item 2 are deleted 2) the second item 2 is deleted 3) the maximum age for a child is changed to 26 if not already 26. 4) The following is added to the first sentence of the Change in Family Status provision:or from the date of placement for adoption with You. 5) Item 3 of the Sending Proof of Loss provision is deleted in its entirety. 6) The age references in the Continuation for Dependent Child(ren) with Disabilities provision are changed to 26 if not already 26. For Vermont residents: Purpose: Vermont law requires that health insurers offer coverage to parties to a civil union that is equivalent to coverage provided to married persons. Definitions, Terms, Conditions and Provisions: The definitions, terms, conditions or any other provisions of the policy, contract, certificate and/or riders and endorsements to which this mandatory endorsement is attached are hereby amended and superseded as follows: 1) Terms that mean or refer to a marital relationship, or that may be construed to mean or refer to a marital relationship, such as "marriage", "spouse", "husband", "wife", "dependent", "next of kin", "relative", "beneficiary", "survivor", "immediate family" and any other such terms, include the relationship created by a civil union established according to Vermont law. 2) Terms that mean or refer to the inception or dissolution of a marriage, such as "date of marriage", "divorce decree", "termination of marriage" and any other such terms include the inception or dissolution of a civil union established according to Vermont law. 3) Terms that mean or refer to family relationships arising from a marriage, such as “family”, “immediate family”, “dependent”, “children”, “next of kin”, “relative”, “beneficiary”, “survivor” and any other such terms include family relationships created by a civil union established according to Vermont law. 4) "Dependent" means a spouse, a party to a civil union established according to Vermont law, and a child or children (natural, stepchild, legally adopted or a minor or disabled child who is dependent on the insured for support and maintenance) who is born to or brought to a marriage or to a civil union established according to Vermont law. 5) "Child or covered child" means a child (natural, step-child, legally adopted or a minor or disabled child who is dependent on the insured for support and maintenance) who is born to or brought to a marriage or to a civil union established according to Vermont law. CAUTION: FEDERAL LAW RIGHTS MAY OR MAY NOT BE AVAILABLE Vermont law grants parties to a civil union the same benefits, protections and responsibilities that flow from marriage under state law. However, some or all of the benefits, protections and responsibilities related to health insurance that are available to married persons under federal law may not be available to parties to a civil union. For example, federal law, the Employee Income Retirement Security Act of 1974 known as “ERISA”, controls the employer/employee relationship with regard to determining eligibility for enrollment in private employer health benefit plans. Because of ERISA, Act 91 does not state requirements pertaining to a private employer’s enrollment of a party 80 to a civil union in an ERISA employee welfare benefit plan. However, governmental employers (not federal government) are required to provide health benefits to the dependents of a party to a civil union if the public employer provides health benefits to the dependents of married persons. Federal law also controls group health insurance continuation rights under COBRA for employers with 20 or more employees as well as the Internal Revenue Code treatment of health insurance premiums. As a result, parties to a civil union and their families may or may not have access to certain benefits under this policy, contract, certificate, rider or endorsement that derive from federal law. You are advised to seek expert advice to determine your rights under this contract. For Virginia residents, any and all references to Domestic Partners are hereby deleted. For Washington residents: 1) The Accelerated Benefit is not available. 2) The provision titled Policy Interpretation is deleted in its entirety. For Wisconsin residents, the time periods stated in the Claim Appeal provision are removed. In all other respects, the Policy and certificates remain the same. Signed for Hartford Life and Accident Insurance Company. Richard G. Costello, Secretary John C. Walters, President 81 ERISA INFORMATION THE FOLLOWING NOTICE CONTAINS IMPORTANT INFORMATION This employee welfare benefit plan (Plan) is subject to certain requirements of the Employee Retirement Income Security Act of 1974 (ERISA), as amended. ERISA requires that you receive a Statement of ERISA Rights, a description of Claim Procedures, and other specific information about the Plan. This document serves to meet ERISA requirements and provides important information about the Plan. The benefits described in your booklet-certificate (Booklet) are provided under a group insurance policy (Policy) issued by the Hartford Life and Accident Insurance Company (Insurance Company) and are subject to the Policy’s terms and conditions. The Policy is incorporated into, and forms a part of, the Plan. The Plan has designated and named the Insurance Company as the claims fiduciary for benefits provided under the Policy. The Plan has granted the Insurance Company full discretion and authority to determine eligibility for benefits and to construe and interpret all terms and provisions of the Policy. A copy of the Plan is available for your review during normal working hours in the office of the Plan Administrator. 1. Plan Name Group Long Term Disability, Basic Term Life, Supplemental Dependent Life, Supplemental Term Life, Basic Accidental Death and Dismemberment Plan for Employees of DREXEL UNIVERSITY. 2. Plan Number LTD - 501 LIFE - 501 ADD - 501 3. Employer/Plan Sponsor DREXEL UNIVERSITY 3141 Chestnut Street Philadelphia, PA 19104 4. Employer Identification Number 23-1352630 5. Type of Plan Welfare Benefit Plan providing Group Long Term Disability, Basic Term Life, Supplemental Dependent Life, Supplemental Term Life, Basic Accidental Death and Dismemberment. 6. Plan Administrator DREXEL UNIVERSITY 3141 Chestnut Street Philadelphia, PA 19104 82 7. Agent for Service of Legal Process For the Plan DREXEL UNIVERSITY 3141 Chestnut Street Philadelphia, PA 19104 For the Policy: Hartford Life and Accident Insurance Company 200 Hopmeadow St. Simsbury, CT 06089 In addition to the above, Service of Legal Process may be made on a plan trustee or the plan administrator. 8. Sources of Contributions The Employer pays the premium for the insurance, but may allocate part of the cost to the employee. The Employer determines the portion of the cost to be paid by the employee. 9. Type of Administration The plan is administered by the Plan Administrator with benefits provided in accordance with the provisions of the applicable group plan. 10. The Plan and its records are kept on a Policy Year basis. 11. Labor Organizations None 12. Names and Addresses of Trustees None 13. Plan Amendment Procedure The Plan Administrator reserves full authority, at its sole discretion, to terminate, suspend, withdraw, reduce, amend or modify the Plan, in whole or in part, at any time, without prior notice. The Employer also reserves the right to adjust your share of the cost to continue coverage by the same procedures. 83 STATEMENT OF ERISA RIGHTS As a participant in the Plan you are entitled to certain rights and protections under the Employee Retirement Income Security Act of 1974 (ERISA), as amended. ERISA provides that all Plan participants shall be entitled to: 1. Receive Information About Your Plan and Benefits a) Examine, without charge, at the Plan Administrator's office and at other specified locations, such as worksites and union halls, all documents governing the Plan, including insurance contracts and collective bargaining agreements, and a copy of the latest annual report (Form 5500 Series) filed by the Plan with the U.S. Department of Labor and available at the Public Disclosure Room of the Employee Benefits Security Administration. b) Obtain, upon written request to the Plan Administrator, copies of documents governing the operation of the Plan, including insurance contracts and collective bargaining agreements, and copies of the latest annual report (Form 5500 Series) and updated summary Plan description. The administrator may make a reasonable charge for the copies. c) Receive a summary of the Plan's annual financial report. The Plan Administrator is required by law to furnish each participant with a copy of this summary annual report. 2. Prudent Actions by Plan Fiduciaries In addition to creating rights for Plan participants ERISA imposes duties upon the people who are responsible for the operation of the employee benefit Plan. The people who operate your Plan, called “fiduciaries” of the Plan, have a duty to do so prudently and in the interest of you and other Plan participants and beneficiaries. No one, including your employer, your union, or any other person, may fire you or otherwise discriminate against you in any way to prevent you from obtaining a welfare benefit or exercising your rights under ERISA. 3. Enforce Your Rights If your claim for a welfare benefit is denied or ignored, in whole or in part, you have a right to know why this was done, to obtain copies of documents relating to the decision without charge, and to appeal any denial, all within certain time schedules. Under ERISA, there are steps you can take to enforce the above rights. For instance, if you request a copy of Plan documents or the latest annual report from the Plan and do not receive them within 30 days, you may file suit in a Federal court. In such a case, the court may require the Plan Administrator to provide the materials and pay you up to $110 a day until you receive the materials, unless the materials were not sent because of reasons beyond the control of the administrator. If you have a claim for benefits which is denied or ignored, in whole or in part, you may file suit in a state or Federal court. If the Plan requires you to complete administrative appeals prior to filing in court, your right to file suit in state or Federal court may be affected if you do not complete the required appeals. If it should happen that Plan fiduciaries misuse the Plan’s money, or if you are discriminated against for asserting your rights, you may seek assistance from the U.S. Department of Labor, or you may file suit in a Federal court. The court will decide who should pay court costs and legal fees. If you are successful the court may order the person you have sued to pay these costs and fees. If you lose, the court may order you to pay these costs and fees, for example, if it finds your claim is frivolous. 4. Assistance with Your Questions If you have any questions about your Plan, you should contact the Plan Administrator. If you have any questions about this statement or about your rights under ERISA, or if you need assistance in obtaining documents from the Plan Administrator, you should contact the nearest office of the Employee Benefits Security Administration (formerly known as the Pension and Welfare Benefits Administration), U.S. Department of Labor, listed in your telephone directory or the Division of Technical Assistance and Inquiries, Employee Benefits Security Administration, U.S. Department of Labor, 200 Constitution Avenue N.W., Washington, D.C. 20210. You may also obtain certain publications about your rights and responsibilities under ERISA by calling the publications hotline of the Employee Benefits Security Administration. CLAIM PROCEDURES The Plan has designated and named the Insurance Company as the claims fiduciary for benefits provided under the Policy. The Plan has granted the Insurance Company full discretion and authority to determine eligibility for benefits and to construe and interpret all terms and provisions of the Policy. Claim Procedures for Claims Requiring a Determination of Disability 84 Claims for Benefits If you or your authorized representative would like to file a claim for benefits for yourself or your insured dependents, you or your authorized representative should obtain a claim form(s) from your Employer or Plan Administrator. The applicable section of such form(s) must be completed by (1) you, (2) the Employer or Plan Administrator and (3) the attending physician or hospital. Following completion, the claim form(s) must be forwarded to the Insurance Company’s claim representative. The Insurance Company will evaluate your claim and determine if benefits are payable. The Insurance Company will make a decision no more than 45 days after receipt of your properly filed claim. The time for decision may be extended for two additional 30 day periods provided that, prior to any extension period, the Insurance Company notifies you in writing that an extension is necessary due to matters beyond the control of the Plan, identifies those matters and gives the date by which it expects to render its decision. If your claim is extended due to your failure to submit information necessary to decide your claim, the time for decision may be tolled from the date on which the notification of the extension is sent to you until the date we receive your response to our request. If the Insurance Company approves your claim, the decision will contain information sufficient to reasonably inform you of that decision. Any adverse benefit determination will be in writing and include: 1) specific reasons for the decision, 2) specific references to the Policy provisions on which the decision is based, 3) a description of any additional material or information necessary for you to perfect the claim and an explanation of why such material or information is necessary, 4) a description of the review procedures and time limits applicable to such procedures, 5) a statement that you have the right to bring a civil action under section 502(a) of ERISA after you appeal our decision and after you receive a written denial on appeal, and 6) (A) if an internal rule, guideline, protocol, or other similar criterion was relied upon in making the denial, either (i) the specific rule, guideline, protocol or other similar criterion, or (ii) a statement that such a rule, guideline, protocol or other similar criterion was relied upon in making the denial and that a copy will be provided free of charge to you upon request, or (B) if denial is based on medical judgment, either (i) an explanation of the scientific or clinical judgment for the determination, applying the terms of the Policy to your medical circumstances, or (ii) a statement that such explanation will be provided to you free of charge upon request. Appealing Denials of Claims for Benefits On any wholly or partially denied claim, you or your representative must appeal once to the Insurance Company for a full and fair review. You must complete this claim appeal process before you file an action in court. Your appeal request must be in writing and be received by the Insurance Company no later than the expiration of 180 days from the date you received your claim denial. As part of your appeal: 1. you may request, free of charge, copies of all documents, records, and other information relevant to your claim; and 2. you may submit written comments, documents, records and other information relating to your claim. The Insurance Company’s review on appeal shall take into account all comments, documents, records and other information submitted by you relating to the claim, without regard to whether such information was submitted or considered in the initial benefit determination. The Insurance Company will make a final decision no more than 45 days after it receives your timely appeal. The time for final decision may be extended for one additional 45 day period provided that, prior to the extension, the Insurance Company notifies you in writing that an extension is necessary due to special circumstances, identifies those circumstances and gives the date by which it expects to render its decision. If your claim is extended due to your failure to submit information necessary to decide your claim on appeal, the time for decision shall be tolled from the date on which the notification of the extension is sent to you until the date we receive your response to the request. The individual reviewing your appeal shall give no deference to the initial benefit decision and shall be an individual who is neither the individual who made the initial benefit decision, nor the subordinate of such individual. The review process provides for the identification of the medical or vocational experts whose advice was obtained in connection with an initial adverse decision, without regard to whether that advice was relied upon in making that decision. When deciding an appeal that is based in whole or part on medical judgment, we will consult with a medical professional having the appropriate training and experience in the field of medicine involved in the medical judgment and who is neither an individual consulted in connection with the initial benefit decision, nor a subordinate of such individual. If the Insurance Company grants your claim appeal, the decision will contain information sufficient to reasonably inform you of that decision. 85 However, any final adverse benefit determination on review will be in writing and include: 1) specific reasons for the decision, 2) specific references to the Policy provisions on which the decision is based, 3) a statement that you have the right to bring a civil action under section 502(a) of ERISA, 4) a statement that you may request, free of charge, copies of all documents, records, and other information relevant to your claim; 5) (A) if an internal rule, guideline, protocol, or other similar criterion was relied upon in making the decision on appeal, either (i) the specific rule, guideline, protocol or other similar criterion, or (ii) a statement that such a rule, guideline, protocol or other similar criterion was relied upon in making the decision on appeal and that a copy will be provided free of charge to you upon request, or (B) if the decision on appeal is based on medical judgment, either (i) an explanation of the scientific or clinical judgment for the decision on appeal, applying the terms of the Policy to your medical circumstances, or (ii) a statement that such explanation will be provided to you free of charge upon request, and 6) any other notice(s), statement(s) or information required by applicable law. Claim Procedures for Claims Not Requiring a Determination of Disability Claims for Benefits If you or your authorized representative would like to file a claim for benefits for yourself or your insured dependents, you or your authorized representative should obtain a claim form(s) from your Employer or Plan Administrator. The applicable section of such form(s) must be completed by (1) you, (2) the Employer or Plan Administrator and (3) the attending physician or hospital. Following completion, the claim form(s) must be forwarded to the Insurance Company’s claim representative. The Insurance Company will evaluate your claim and determine if benefits are payable. The Insurance Company will make a decision no more than 90 days after receipt of your properly filed claim. However, if the Insurance Company determines that special circumstances require an extension, the time for its decision will be extended for an additional 90 days, provided that, prior to the beginning of the extension period, the Insurance Company notifies you in writing of the special circumstances and gives the date by which it expects to render its decision. If extended, a decision shall be made no more than 180 days after your claim was received. If the Insurance Company approves your claim, the decision will contain information sufficient to reasonably inform you of that decision. However, any adverse benefit determination will be in writing and include: 1) specific reasons for the decision; 2) specific references to Policy provisions on which the decision is based; 3) a description of any additional material or information necessary for you to perfect the claim and an explanation of why such material or information is necessary; 4) a description of the review procedures and time limits applicable to such, and 5) a statement that you have the right to bring a civil action under section 502(a) of ERISA after you appeal our decision and after you receive a written denial on appeal. Appealing Denials of Claims for Benefits On any wholly or partially denied claim, you or your representative must appeal once to the Insurance Company for a full and fair review. You must complete this claim appeal process before you file an action in court. Your appeal request must be in writing and be received by the Insurance Company no later than the expiration of 60 days from the date you received your claim denial. As part of your appeal: 1. you may request, free of charge, copies of all documents, records, and other information relevant to your claim; and 2. you may submit written comments, documents, records and other information relating to your claim. The Insurance Company’s review on appeal shall take into account all comments, documents, records and other information submitted by you relating to the claim, without regard to whether such information was submitted or considered in the initial benefit determination. The Insurance Company will make a final decision no more than 60 days after it receives your timely appeal. However, if the Insurance Company determines that special circumstances require an extension, the time for its decision will be extended for an additional 60 days, provided that, prior to the beginning of the extension period, the Insurance Company notifies you in writing of the special circumstances and gives the date by which it expects to render its decision. If extended, a decision shall be made no more than 120 days after your appeal was received. If the Insurance Company grants your claim appeal, the decision will contain information sufficient to reasonably inform you of that decision. However, any final adverse benefit determination on review will be in writing and include: 1) specific reasons for the decision and specific references to the Policy provisions on which the decision is based, 2) a statement that you are entitled to receive, upon request and free of charge, reasonable access to, and copies of, all documents, records and 86 other information relevant to the claim, 3) a statement of your right to bring a civil action under section 502(a) of ERISA, and 4) any other notice(s), statement(s) or information required by applicable law. 87 The Plan Described in this Booklet is Insured by the Hartford Life and Accident Insurance Company Simsbury, Connecticut Member of The Hartford Insurance Group