International Comparisons of Health Care Output and Productivity May 18, 2004
advertisement

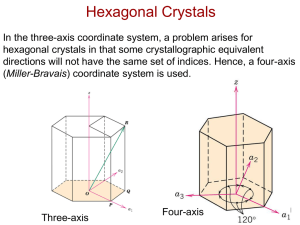
International Comparisons of Health Care Output and Productivity Hui Duan and Kam Yu∗ May 18, 2004 Abstract Measuring the output and productivity of the health care sector is important but difficult, and it has been a long-standing policy concern. Statistical agencies in some countries such as U.K., Eurostat, Australia, and the U.S. have done substantial research to investigate various approaches to measure the output. This paper reviews recent developments in the economic measurement of health care output and compares the results by applying different methods to the health care sector in Canada. Our initial results show that different approaches result in significant different output measurement. Health care analysts and policy makers should be aware of these differences in comparing output and productivity across countries. JEL: C43, H51 1 Introduction The definition of health care sector adopted by the Bureau of Labour Statistics (BLS) in the U.S. is “to focus on the treatments of diseases or the relief of pain and the suffering” (Cutler and Berndt, 2001). Thus, its major function is to improve the health conditions of the general population. Obviously, the health care industry is largely based on services. Measuring the output of the service industries has long been regarded difficult. Because we do not know exactly what is being transacted and what services correspond to the payments made to their providers, conceptual problems arise. Among the hard-to-measure services, the health care sector has been perceived as one of the most difficult. However, measuring health care output is an important component in health and welfare economics. For example, in order to evaluate the productivity of the health care sector, we usually conduct cost-effective analysis. In such an analysis, we need ∗ Department of Economics, Lakehead University, Thunder Bay, Ontario, Canada, P7B 5E1. Phone: 807-343-8229, Fax: 807-346-7936, E-mail: Kam.Yu@lakeheadu.ca. 1 to compare what we can get out of the health care sector with its expenditures. To accurately answer the question, we require measuring health care output. This is the problem faced by both health care analysts and national income accountants. In national income accounts, we divide nominal spending growth into changes in prices and changes in quantities. But without an accurate measure of health care industry output, we can estimate neither prices nor quantities. There are two major difficulties in implementation: First, “Measuring health status is difficult, and attributing changes in health status to a particular factor such as health care is even more challenging” (Cutler and Berndt, 2001). Second, another difficulty rests on the measurement of real output. For most industries in most countries, real output measurement is accomplished by deflation, that is, dividing data on revenues (values) by a price index to obtain a measure of real output. Such an approach requires reliable revenue data and a price index. In a country where the market prices are available, this method can be implemented, although other measuring problems still exist. However, for countries such as Canada where health care goods and services are provided by the government without direct charge or with only nominal direct charges, the revenue data may not be available or may be irrelevant. In such cases the problem of measuring health care output is combined with the problem of measuring the output of the government sector (Berndt et al., 2001). In this paper, we mainly focus on the issues of measurement in public health care systems. Section 2 below reviews the basic concept in output measurement and the difficulties encountered in measuring government services. The traditional cost approach is described in section 3. Various newly developed direct measurement techniques are reviewed in section 4. In section 5 we apply the various techniques to the Canadian health sector for the case of health disease treatment and show that different methods gives significant different GDP measurement. Section 6 concludes and recommends further studies. 2 The Index Number Problem Consider one of the most important identities in index number theory: P (p1 , p2 , q 1 , q 2 )Q(p1 , p2 , q 1 , q 2 ) = p2T q 2 . p1T q 1 (1) P is the price index function of four vectors, namely, p1 is the price vector of N goods and services in period 1 (base period), p2 is the prices in period 2 (comparison period), q 1 and q 2 are the corresponding quantityP vectors. Superscript T denotes the transpose of a matrix or vector. Thus pT q = N i=1 pi qi is the inner product of the vectors p and q. Q is the quantity index function. The right hand side of (1) is the ratio of the total values of the N products in the two period. This identity 2 is sometimes called the product test. It requires the product of the price index and the quantity index to be equal to the total value ratio. If there is only one product, that is, N = 1, then the price index P is simply p21 /p11 and quantity index Q = q12 /q11 . Identity (1) is trivially satisfied and there is no index number problem. For N > 1, we have to find a way to sum up the prices and quantities of different goods so that the resulting indices will satisfy (1). In other words, we try to compare apples with oranges, and then add them up together. Mathematically speaking we decompose the value ratio into two factors P and Q. In the economic approach to index numbers literature, P is interpreted as a cost of living index. It compares the cost of consuming the N goods and services to achieve the same standard of living in both period (Konüs, 1939). Q, on the other hand, measures the change in the standard of living. Recently there has been a lot of discussion about adapting the economic approach in the construction of the consumer price index (CPI).1 Some countries such as the U.S. have adopted the concept as the objective of the CPI. Although the objectives and goals of the CPI may be different from those of the SNA, the economic approach can provide a theoretical foundation for both. The goal of the SNA is to measure the quantities of goods and services produced and consumed in the economy, which then serves as a partial social welfare indicator. In principle this objective is compatible with the conceptual framework of a cost-ofliving price index. For example, if Q in (1) is the constant dollar GDP per capita, then it can be interpreted as the SNA-economic welfare indicator. Consequently, identity (1) stipulates that the implicit GDP deflator P is indeed a cost-of-living index. In addition, the economic approach does not conflict the other purposes of the SNA in economic analysis, decision-taking, and policy-making. In practice we often deflate the current dollar value of a product (or a product group) with a proper price index to obtain a constant dollar volume index.2 That is, on a subindex level, we implicitly defined the Konüs quantity index as 1 p2T q 2 QK = PK p1T q 1 where PK = and C(p, u) = min q (2) C(u, p2 ) C(u, p1 ) ( X ) pi qi : U (q) ≥ u i PK is the Konüs cost-of-living (sub)index. It is defined as the ratio of the cost functions in periods 2 and 1 when a consumer faces prices p2 and p1 . The consumer 1 A detailed discussion justifying the economic approach is given by Triplett (2001). The name volume index is used interchangeably with the term quantity index. See SNA93, p. 381. 2 3 is supposed to maximize her utility U (q) in both periods. The cost function C is the minimum amount of money the consumer needs to achieve the same reference standard of living or utility u in both periods. The choice of u is of course very important because PK and consequently QK depend on it. It can be shown, however, that there exists a utility level u∗ between the utility levels of the consumer in periods 1 and 2 such that PK lies between the values of the Laspeyres price index PL and the Paasche price index PP . That is, there is a u∗ = λu1 + (1 − λ)u2 for 0 ≤ λ ≤ 1 such that3 PP ≤ PK ≤ PL or (3) PL ≤ P K ≤ PP . In fact the implicit Konüs quantity index is a special case of a more general index, known as the Allen index: QA (q 1 , q 2 , p) = C(U (q 2 ), p) . C(U (q 1 ), p) (4) Here we directly compare the cost function of the utility or standard of living in periods 2 and 1, using a reference price vector p. In the literature of cost benefit analysis, C(U (q), p) is called a money metric measure of quantity vector q. Another commonly used theoretical index is the Malmquist quantity index: QM (q 1 , q 2 , q) = D(U (q), q 2 ) D(U (q), q 1 ) (5) where D(u, q t ) = max k : U (q t /k) ≥ u, k > 0 k is called a distance or deflation function. D measures the maximum value that can deflate the quantity q t such that the resulting utility level is at least as high as u. In (5) q is a reference quantity vector that defines the reference utility level u = U (q). And QM is the ratio of the deflators for q 2 and q 1 with respect to U (q). So far we have defined three theoretical quantity indices. In principle if the consumer’s utility function is known or can be estimated, all three indices can be computed using duality theory. In practice, of course, this is seldom done. These indices are used to derive simple non-parametric index formulae. A natural question is which one should be used to develop our quantity index in practice. It turns out that if we make further assumptions about the utility function, the three indices become the same. In particular, if we assume that consumers’ preferences are homothetic, then QK = QA = QM = U (q 2 )/U (q 1 ). Technically, a homothetic preference structure means that the utility function is an increasing transform of a linearly homogeneous function. That is, U (q) = f (Û (q)) 3 For a proof and other discussions on economic approach to index number see Diewert (1981). 4 where f is a single-variable increasing function, i.e., f 0 > 0, and Û (αq) = αÛ (q) for all α > 0. It implies that a consumer has constant expenditure share for each commodity even when total expenditure varies. Although this assumption is very restrictive, it provides us with a guideline for the search of the index formulae. For example, a frequently used utility function in economic analysis is the Cobb-Douglas function N Y U (q) = qiαi i=1 where PN i=1 αi = 1. It is easy to show that for this utility function QK = QA = QM = N 2 α i Y q i i=1 qi1 . That is, the three theoretical indices all equal to the weighted geometric mean of the quantity ratios, which is often called the weighted geometric index. In this case we say that the weighted geometric index is exact for the Cobb-Douglas utility function. This example shows that different assumptions on the utility function give rise to different index number formulae. In applied economic analysis a group of functions called flexible functional forms is often used for empirical estimation of demand and supply functions. The advantage is that they approximate an arbitrary utility function to the second degree in a Taylor expansion. For example, the square root quadratic utility function defined as U (q) = (q T Aq)1/2 , (6) where A is a symmetric N × N square matrix of coefficients, is a commonly used flexible functional form. It can be shown that the Fisher quantity index, which is the geometric mean of the Laspeyres index and the Paasche index, is exact for the square root quadratic function. An index which is exact to a flexible functional form is called a superlative index. Critics of superlative indices often argue that the homotheticity assumption is too restrictive and unrealistic.4 This argument is misleading in light of (3) because the result does not invoke the homotheticity assumption. Being a geometric mean of PL and PP , the Fisher price index is good approximation for PK . Based on the above concept, international comparisons of output and productivity can be studied using the economic approach (Diewert 1996). In measuring government outputs, however, there are no prices, quantities are difficult to define, and some products and services undergo constant quality change. Nevertheless, the value of government services has to be estimated and then added to the value of marketed goods to get the GDP. How we add apples to oranges when oranges have no price tag has long been a vexing problem for economic statisticians. 4 See, for example, Hillinger (2002). 5 3 The Cost Approach Because of the service orientation of the health care sector, some statistical agencies in countries with public health care systems think of health care as a kind of government services to be included into the System of National Accounts (SNA). They simply take the sum of factor costs (inputs) as the outputs.5 This implies that productivity growth for this sector is always zero. Generally, we can divide an economic process into four phases: factor inputs, activities, outputs and outcomes. Factor inputs include labour, capital as well as other intermediate products consumed in the production process. The intermediate steps that contribute to a final product are activities. Outputs are the products and services that the consumer purchase from the producers. The effects of the final products on the consumers are considered as outcomes. In the case of health care, physicians, nurses and medical investments are input factors. Activities can be the number of admitted or discharged patients, number of days in hospital, or number of operations performed for different diseases. Output may be the number of cured heart attacks or strokes, or cases of diabetes treated. The physical well-being or the welfare of the patients can be treated as outcome. If we assume the whole health care sector as a large producer in a market economy and take the factor inputs as outputs, then there is no productivity change or growth reflected in the national accounts since any added-value is neglected. Despite some criticisms, taking inputs as outputs in the health care sector is justifiable for some reasons. First, it is the most convenient way to include non-market output in the SNA. Second, intermediate transactions and products generated in the sector are difficult to be included in the SNA. Actually, if we consider the problem from microeconomic perspective, we may consider the output prices p to be the marginal costs ∇q C(w, q). The inner product of quantities and marginal costs q T ∇q C(w, q) should equal total cost C(w, q).6 Therefore, cost can be the “correct” value for health care output. And we may split the value of volume into price and quantity components using the vector of marginal costs. Although the cost approach is justifiable, there are still some problems with it, as mentioned before. Therefore, we still need to find alternative methods to evaluate health care output more accurately for policymaking reasons. 4 Direct Output Measurement Approaches Due to the inherit drawbacks of input method, some health economists and statisticians have recommended the improvements of output measurement in public health 5 In fact, Statistics Canada follows the exact method to calculate the output of Canadian health care sector. 6 We wish to thank Erwin Diewert for this point. 6 care systems. In recent years, a lot of research has been done to investigate the feasibility of direct output measurement. In particular, statistical agencies in some countries and regions have examined output measurement methods. Among them are the Office for National Statistics (ONS) in the U.K., European Statistics (Eurostat), and the Australian Bureau of Statistics (ABS). 4.1 The U.K. Methods From 1998 to 2001, the ONS in the U.K. allocated resources to develop approaches of measuring government output and non-market services. The researchers at ONS made some suggestions to improve the current SNA system and applied the direct measurement approaches to some public services. As mentioned earlier, for non-market production it is impossible to measure the output by looking at the prices paid by final consumers, as there may be no price information available, and a convention is needed to value the output. British national accountants previously used the costs of production as a measure of the value of output. These costs include the compensation of the employees, the value of goods and services purchased to produce the output (the intermediate consumption), and the depreciation of capital items (capital consumption). Historically, in the U.K., the measure of volume is done by adding the volumes of labour, intermediate consumption and capital consumption to get the total volume. As Caplan (1998) indicated, “there is a serious deficiency in this approach as there is an implicit assumption that there is no change in labour productivity”. He used an example to illustrate the underlying deficiency. In the example, there is a clerical process of writing cheques. As printing technology improves, this process becomes automated so the cheques are printed by a computer rather than hand written. As a result, fewer clerks will be employed. However, if we look at the the national accounts, the volume of output would be recorded as having fallen because the decline in the volume of labour used will not be offset by the increases in capital consumption. In fact, we can see that the output remains at the same level as the same number of cheques are being written. This is actually a problem of measuring the productivity of the public sector and technology in general. For example, Baumol (1967) examined the relationship between “unbalanced growth”7 and the urban crisis. The corresponding cost increase and limited source of tax funds, which are associated with “unbalanced growth”, might lead to financial problems of a large city. 7 The growth of activities with technological progress and those with sporadic productivity increase. 7 4.1.1 Concerns and Concepts In recent years, there has been growing concern for the ONS that the implicit assumption of no change in productivity was unreasonable, and such productivity improvements should be recorded in the national accounts. The ONS was committed to producing national accounts compatible with the 1995 European System of Accounts (ESA). The ESA recommended that “direct measures of the output of non-market services should be used in preference to input measures”. Additionally, at the European level, there is a coordinated attempt to improve estimates of GDP at constant prices (Caplan, 1998). ONS developed the approach based on the idea that “it is better to measure the right thing approximately than the wrong thing precisely” (Caplan, 1998). This idea implies that any new indicators would not necessarily be perfect or beyond criticism, but at least, would be more appropriate than the existing input approach. Output “proxies” for market output was considered by the ONS. A proxy itself cannot necessarily measure the output but it measures something reasonably thought to move in a similar way to output.8 To carry out the approach, the ONS defined the output and how it could be measured. The four definitions (inputs, activities, output and outcome) are the same as those mentioned in Section 3. However, the measures of output should be used rather than outcome, which is recommended by the ESA: “. . . , it is of prime importance to adopt the principle that the production and consumption of non-market services, like the production and consumption of goods and market services, must be defined in terms of the actual flows of these goods and services and not in terms of final results obtained from their use. As these results depend on several other factors as well, . . . ” (Caplan, 1998). But it is sometimes difficult to distinguish between an outcome and an output, and in practice, output is impossible to be measured in some cases, so activities would be more can reasonably be taken as proxies for output. Therefore, the measurement of economic activity has an important distinction. 4.1.2 Approaches In the U.K., health services are broken down into two categories: Family Health Services (FHS, or primary care) and Hospital and Community Health Services (HCHS, or secondary care). For HCHS, there has been a long established indicator of activities called the Cost Weighted Activity Index (CWAI). The general procedure for this technique are as follows (Ashaye, 2001): 1. Identify an area of services where activities are to be measured 8 For example, the output of the banking sector may be measured by counting the number of transactions. This figure is regarded to reflect changes in output although it does not measure the results directly. 8 2. List all activities of the area 3. Find a volume measure for each activity (number of incidents or cases, etc.) 4. Form a volume ratio for each activity between the comparison period and the base period 5. Aggregate the volume ratios using cost shares as weights to produce a subindex for the area The FHS covers services provided by family doctors, opticians, etc. Each activity indicator is identified for each category of services (e.g, the number of consultations with general practitioners, the number of NHS sight tests). After counting the numbers, they are aggregated using each service’s expenditure or cost as weights (like the CWAI method for HCHS). The methods described above is in fact a measurement of activities instead of output. However, they are regarded as an improvement on the input or cost method. Such methods can also be applied to measure the output of health services in countries with public health care systems, as there are similarities between these services and services provided by the government. 4.2 The Eurostat Methods From 1998 to 2000, the European Statistics established two task forces to investigate the “embryonic” output methods used in the volume measurement of Section N of NACE.9 According to the definition of ESA, non-market output is “output that is provided free, or at prices that are not economically significant, to other units”. Further, “economically significant” is defined as “any sums recovered through sales cover less than 50% of the production costs” (Eurostat, 1998, p.7). 4.2.1 Classifications of Health Services In Europe, there are two classifications of health services to serve different objectives: the NACE and the COICOP.10 NACE classifies the production of health services by activity, while COICOP classifies the expenditure of individual consumption. “Nonmarket output at current prices is defined as the sum of its production costs, and the expenditure on non-market output is defined as the output of their producers, that is NPISHs11 and general government, less receipts from sales” (Eurostat, 1998, p.7). Accordingly, Section N of NACE Group includes the following main activities: 9 The “Nomenclature générale des Activités économiques dans les Communautés Européennes” (NACE - General Industrial Classification of Economic Activities within the European Communities) 10 Classification of individual consumption by purpose 11 Non-profit institutions serving households 9 • Hospital activities. • Medical practice activities. • Dental practice activities. • Other human health activities. In COICOP, the individual health expenditures are classified as follows: • Hospital services. • Outpatient medical services. • Outpatient dental services. • Outpatient paramedical services. • Public health services. • Other health services. However, it is not a one-to-one correspondence between the two classifications, so it is necessary to ensure consistent coverage and treatments of individual health services on both sides of the accounts (Eurostat, 1998, p.6). 4.2.2 Recommendation Criteria Like the ONS in the U.K., the task forces made the following definition of output: The health output is the quantity of health care received by patients, adjusted to allow for the qualities of service provided, for each type of health care. The quantities should be weighted together using data on the costs or prices of the health care provided. (Eurostat, 1998, p.9) More importantly, the task forces suggested: “the quantity of health care received by patients should be measured in terms of treatments.” As we may notice, this is a different measure from the one used by the ONS of U.K., and it is an “output” measure in strict sense. A treatment should also be measured in entirety, taking into account the whole bundle of complementary services (e.g., the medical services, laboratory and radiological services, and non-medical services in hospitalization). But in practice, the degree of fragmentation of the services in a treatment can affect the feasibility of measuring complete treatments. For example, there is not a strong linkage between the inpatient services and outpatient services for a transferred patient before and after hospitalization. 10 The task forces also indicated the output measure should reflect the quality changes. Generally, the quality of treatments may depend on the amount of resources used for each patient (including the number and mix of medical and paramedical staff, the sophistication of the equipment and the availability of the drugs and medicines) (Eurostat, 1998, p.9). But sometimes quality changes are complicated and difficult to measure because there are combined effects (both positive and negative).12 In order to ensure the consistency between the constant price estimates of market output and non-market output, the task forces suggested an output price method for market output and an output indicator method used for either market output or non-market output. The best output price method should use the ideal price index, which can produce the ideal volume index when used to deflate the output at current prices. And the best output indicator method would be the one which uses the ideal volume index. To be considered “ideal”, the prices/quantities used to construct indices should meet the following six practical requirements (Eurostat, 1998, p.10): 1. Direct relation to output: They should relate directly to complete treatments and not to contributory activities or any primary inputs. 2. Sufficient stratification: Different prices/quantities should be available for all different product groups comprising output. 3. Sufficient homogeneity: If there is more than one product within a product group, the composition of the product group does not change over time. 4. Sufficient representation: It is ideal if every item of the product group has observations of prices/quantities. However, in many cases, there is not enough available information for the prices/quantities of all products but only those for a sample group of products. In these circumstances, changes in the observed prices/quantities should represent changes in the prices/quantities that are not observed. 5. Changes in the quality: The prices/quantities for a product group should account for changes in the quality. Moreover, changes in values from quality changes should be included in the volume index rather than the price index (i.e., the volume index = quantity index × quality index). 6. Different weights: The value of output in time period t should be used as weights to aggregate prices, while the value (output for market production and 12 For example, a reduction in the length of stay in hospital can imply a gain in quality due to technological advances in drugs and surgeries; but it is also possible that the patient now receive post-operative services from family and visiting paramedics rather than hospitals, then it indicates a quality loss. 11 total costs for non-market production) at period t − 1 be used as weights to aggregate quantities. The above requirements apply to both prices and quantities. However, there are two exceptions: 1. Quantities may have less strict sufficient representation requirement than prices because price changes in a sample can represent the whole population more often than quantity changes in the same sample. 2. The price indices should be Paasche indices (using weights of the current period) and the volume indices should be Laspeyres indices (using weights of the base period). Based on the extent to which a method satisfies the six requirements, the task forces divided different methods into three classifications: A method (recommended), B method (reasonable) and C method (avoided). Obviously, the volume index constructed using an A method is the most approximate to the ideal volume index, and the volume index of a C method differs most from the ideal volume index.13 Therefore, the A, B and C methods should have the following properties: • A method: It takes account both quantity and quality changes in output. Quantity measures number of complete treatments. The quality indicator covers both changes in the physical characteristics of products and in the product mix. It is possible to analyze productivity changes using an A method. • B method: It may be used when we cannot apply an A method. It has similar properties of an A method except that it can only reflect the quality changes resulting from changes in the product mix. • C method: It is neither an A method nor a B method. The volume index obtained by this method is an unacceptable approximation of the ideal volume index. 4.2.3 Recommendations Considering the proposed criteria, the task forces made recommendations on the measurement of the output of health services. An A method or B method was suggested according to these requirements. First, the indicators and weights should both relate directly to output in order to satisfy the requirement for an A method. Hospital output is expected to be the total number of discharged patients by kind of complete treatments, using the 13 However, the actual ideal volume index is unknown, so in practice, the method choice should be determined by statistical analysts. 12 corresponding cost in period t − 1 as weight. Output indicators for consultations and dental services may adopt similar methods. However, in cases where the information on prices or costs for weights is unknown, allocating costs of nursing days (or surgical operations etc.) to complete treatments by cross-tabulation. Then the cost of each treatment can be used as approximate weight. This method is considered to meet the B method requirement since there is no direct data and assumptions are needed.14 Second, to be considered an A method for the output of hospitals, a detailed classification of complete treatments (or treated patients), which accounts for the differences between diseases and treatment methods, should be used. Generally, the use of DRG 15 or ICD 16 systems can meet the requirements of sufficient stratification and homogeneity for A and B methods (if the product group is homogeneous, the number of patient days or activities can be used). Third, regarding sufficient representation, generally, we need large samples for output indicators to be sufficiently representative of the whole population, if we apply both A and B methods. However, when the volume index can only represent part of the group, we may use the implicit-price index to represent the remaining based on the assumption that price indicators from incomplete observations have more representative ability than the associated volume indicators (Eurostat, 1998, p.15). The above work was done by the first task force (TF I). To further investigate the key issues of direct output measurement for health, the Eurostat formed another task force (TF II) in November 2000. The task force II distinguished the inpatient and outpatient treatments. “Inpatient treatment is by definition provided by hospitals only, whereas outpatient treatments are provided both by hospitals and by general practitioners and specialists outside hospitals.” A detailed overview on inpatient and outpatient treatments was provided on the basis of a cross-classification. It also examined the issue of re-admissions in both hospital and other medical and dental practice services. It showed that for hospitals, the percentage of readmissions in the total number of discharges is relatively low, and do not affect the output indicators significantly. Therefore, this indicator may be thought of to qualify for an A method even without the correction for re-admissions (Eurostat, 2000, p10). For medical and dental services, some countries (such as the Netherlands) use the number of “first visits” as an indicator. But the task force II only recommended “first visits” as an ideal indicator for dental practice services because there are differences between specialist services and those services provided by a general practitioner. 14 But the task forces still had opinion that a volume index based on numbers of contributory activities could not fulfil the A or B method requirements because of the mixed effects of those activities on output and quality. 15 Diagnosis Related Groups, a classification system for hospital stays in general and specialized hospitals, used in the U.S. and some European countries. 16 World Health Organisation’s (WHO) International Statistical Classification of Diseases and Health Related Problems. 13 Regarding the weights, the task force II recommended four possible solutions: 1. Best solution: proper output values or cost weights based on full (exhaustive) coverage. 2. Second best: proper cost weights based on representative samples. In France and Norway, the costs in a sample of hospitals are used as weights for DRG groups. 3. Third best: indirect cost weights (e.g., cross-classifying the expenditure by sub-sectors and diagnosis groups). 4. Fourth best: expert guesses if the requirement of precision for weights is not “100% correct”. Both the best and second best solutions can be acceptable for an A method. Finally, due to lack of enough time, the task force II recommended the ratio of qualified staff (man year)/occupant days as a quality indicator in hospital services be further investigated (Eurostat, 2000, p.17). The methods recommended by the European Statistics improved those used by the ONS of U.K. and contained useful details about the output measurement in the health care sector (rather than general government and non-market sectors). 4.3 The ABS Methods In 1997, the Australian Bureau of Statistics (ABS) undertook a major project to improve the measurement of output and productivity for the government sector and other service industries in Australia. As part of the project, the Methodology Division of ABS proposed a research program with the aim of trying to improve the measures for the health services industry. Researchers in the program presented their report of “measuring the outputs and productivity for Australian public acute care hospitals” at the 19th Australian Conference of Health Economists. 4.3.1 Issues and Requirements The researchers realized that the output of health services is more difficult to measure than the medical goods producers because of intangibility and heterogeneity. Problems exist when measuring the output both in a given year and across years. If we try to measure the output in a given year, it is not straightforward to distinguish the difference between two treatments involving the “same” service; and we also have to construct a composite output measure by aggregating the numbers of different types of services. 14 Because of the heterogeneity of health services, the quality changes cannot be easily identified in the measures across several years, and “the change in productivity may be under-estimated or over-estimated” (Daniel et al., 1997). Like the ONS and the Eurostat, ABS also recognizes that it should focus on the measure of “output” rather than “outcome” to conform to the standards of U.N. SNA, i.e., measure the services provided (consumption) rather than their effects on people’s health conditions and life expectancy (utility or welfare).17 It is also because the goal of the project is to enhance and improve the measurement of health services in the Australian national accounts. Viewing outputs as the final products rather than the component processes or intermediate parts, the ABS developed a similar classification system called “casemix”, which classifies the patient care episodes. A casemix should have the following characteristics: 1. Clinical meaning: that is, patients in the same category should have similarities in terms of clinics. 2. Resource homogeneity: the costs of treating patients in the same class should be almost the same. 3. Right number of classes: it should correspond to the number of service types. The acute care hospitals (both public and private) in Australia adopt a DRG-like casemix classification: Australian National Diagnosis Related Groups (AN-DRG). 4.3.2 Indicators and Indices Based on the activity data from the National Hospital Morbidity Database, the ABS has the following activity indicators for inpatient care available in the version 3.0 of the AN-DRG casemix (Daniel et al., 1997, p.7): • Separations: including the cases when a patient is discharged, transferred to another institution, dies while in care, changes status or leaves hospital for a period of seven days or more • Occupied bed days • Same day separations • Average length of stay • Average cost, Relative cost weight and Cost by volume 17 “The objective is to measure the quantities of services actually delivered to households. This should not be confused with the benefits or utility derived from those services.” SNA93 (para. 16.135) 15 The researchers in the project program adopted the number of separations as the primary indicator of activity.18 In Australia, non-inpatients refer to patients who are treated on the hospital site (including emergency patients, outpatients and day program patients). The researchers took the total number of occasions of service as the activity measure for non-inpatient care in public acute hospitals. But there are only limited activity indicators and the information is available only from HUCS.19 The HUCS historically counted treatments as occasions of service. Each attendance at a non-inpatient clinic is counted by HUCS as a treatment and a patient may have more than one treatment in hospital.20 Different from the other two agencies, the ABS takes into account the research and education activities that hospitals engage in. Although some argued that research and education activities should be treated as part of the output since it “will improve procedures and health outcomes or reduce costs and increase efficiencies”, the researchers do not recommend this. First, it is impossible to isolate expenditure on non-patient-care products given the available data.” Moreover, in the national accounts, in-house research and education services are not treated as an output of hospitals, but as an intermediate input. For non-market production, two “quality change” measurement approaches are identified by the ABS. The first approach is to assess the consequences or effects of the service variations on people’s utility. The other focuses on the degree to which the providers conform with the the existing “good practice” procedures, while ignoring whether these standards or criteria are correct or not. The second approach suggests that the ABS assumes desirable results from the procedures. In the Australian health services industry, there is a tendency to incorporate the two approaches to adjust quality change. For example, the Department of Health and Family Services identifies quality-of-care as a measure of “the extent to which the resources allocated to a patient”, and “the processes by which those resources were applied to a patient”. The First National Report on Health Sector Performance Indicators suggests to combine both the quality-of-care and the patient satisfaction Indicators in future development (Daniel et al., 1997). When it comes to the aggregation needed to produce a composite output measure, the ABS puts forward a problem of consistency. Because there is significant proportion of non-market output in the public acute care hospitals, no “current price” value is available. If we treat the cost of production as “current price”, there is “a zero net operating surplus”. An alternative to this approach is to use pseudo 18 However, we note that, according to the definition of “separation” by ABS, it is neither an “activity” nor a “complete treatment” from the perspective of ONS and Eurostat. 19 The Hospital Utilization and Costs Surveys, a comprehensive Australian national dataset containing information on activity and other data for health care institutions. 20 We may also notice that, this is different from the “first visits” indicator recommended by the Eurostat. 16 market price (e.g., imputing the data from similar services in the market sector). However, the aggregated volume measure using the pseudo price is inconsistent with the SNA convention, although there is a non-zero net operating surplus. The researchers finally suggested to use the cost data as weights for aggregation due to the imputing difficulties and the aim of the research project (for the use in national accounts). Using the data from the National Hospital Morbidity Database and the National Costing Study developed by the Department of Health and Family Services of Australia, the researchers developed the following weighting system: Si0 × Average Total Costi0 wi0 = P , i Si0 × Average Total Costi0 ) where wi0 and Si0 are respectively the cost share and the number of separations of group i in the AN-DRG and t = 0 refers to the base period. The output index Qt is based on cost shares as the fixed weights: X Sit . Qt = wi0 Si0 i As we may notice that, the output (volume) index proposed by ABS is consistent with Eurostat’s recommendation: “volume indices should be Laspeyres indices (using weights of the base period)”. For the purpose of compiling a composite output index involving both inpatient and non-inpatient services, the researchers used another set of fix weights called inpatient fraction of costs (IFRAC).21 A composite output index can be constructed by aggregating the subindices for inpatient and non-inpatient services using the IFRACs. 5 An Empirical Study Using Canadian Data We now compare the different approaches to measure the output of treating heart attacks from 1994 to 1999 in Canada. The results can be used as references for measuring other types of diseases, and the whole health care sector. A heart attack (myocardial infarction) is an acute event which results from a blockage of arteries supplying blood to the heart. It will become life-threatening if not diagnosed and treated early and effectively. Because of the high mortality (30%) among elderly people, nearly everyone who suffers from a heart attack will receive medical treatment (Cutler, 2002). 21 A ratio reflecting the relative cost of non-inpatient to inpatient care episodes (usually in terms of occupied bed days (OBD)), with the assumption that “inpatient services account for a fixed share (77.6%) of input costs”. 17 A diagnostic procedure called “cardiac catheterization” is usually used to detect the extent of arterial blockage. Then physicians may decide to perform either of the following two revascularization procedures: bypass surgery (creating a blood flow around occluded arteries) or angioplasty (inserting a balloon catheter into the arteries to remove the blockage and restore blood flow). We use the number of procedures for the treatment of heart attack as an output indicator. The data source is mainly from Canadian Institute for Health Information (CIHI). We obtained the number of cases and number of patient days for each province from CIHI’s Hospital Morbidity Database (HMDB). These data can be freely downloaded from CIHI’s official web site. Based on the numbers, simple output indices can be constructed by applying the following formula (1994 is treated as the base year): Case Indext = Number of Casest , Number of Cases1994 and similarly, Patient Day Indext = Number of Patient Dayst , Number of Patient Days1994 where t stands for the year (1994-1999). Table 1 illustrates the number of heart attack cases, number of patient days and their corresponding indices for Canada. We see a generally increasing trend in the number of cases. While the number of patient days increased during 1995 and 1996, it declined afterwards to a number that is close to the base year (1994) level. The appendix includes output indices using “direct output measurement” for each province/territory. However, for some provinces/territories (e.g., Newfoundland and Northwest Territories), these indices have large fluctuations probably due to small sample sizes. The “number of cases” indicator is based on “complete treatments”, and can be considered “output measure”, while the “number of patient days”, which is an “activity” indicator, does not reflect output in strict sense. However, if it has direct relation to output, we may regard it as a proper “proxy” to an output indicator, given its sufficient representation and homogeneity.22 For comparison, Table 2 shows the indices constructed using the cost approach, which is adopted by Statistics Canada. Due to the unavailability of specific data for heart attacks, it is the hospitals GDP. However, it may reflect the general trend of heath services output to some extent and 1994 is still regarded as the base year. As we may notice, contrary to the “patient days” indices, the “cost” indices declines around 4% during 1996 and 1997, and increases after that period. An activity-based method is to calculate the number of procedures (operations). To construct this type of indices, four major CMG codes, which correspond to the 22 If each patient has to stay nearly the same number of days while receiving heart attack treatment, then it has direct relation to output. 18 Table 1: Number of Heart Attack Cases, Cases Year No. Index 1994 53685 1.00 1995 57146 1.06 1996 59622 1.11 1997 59250 1.10 1998 59003 1.10 1999 61015 1.14 Patient Days and Indices; Canada Patient Days No. Index 500433 1.00 513942 1.03 518060 1.04 500236 1.00 491959 0.98 504652 1.01 Table 2: Hospitals GDP; Canada; 1997 Constant Dollars (Millions) Year Cost (GDP) Index 1994 $20,939 1.00 1995 $20,444 0.98 1996 $20,101 0.96 1997 $20,002 0.96 1998 $20,301 0.97 1999 $20,599 0.98 above-mentioned treatments for heart attacks are identified.23 They are: • CMG 178: coronary bypass with heart pump with cardiac catheterization • CMG 179: coronary bypass with heart pump without cardiac catheterization • CMG 188: percutaneous transluminal coronary angioplasty with complicating cardiac conditions • CMG 189: percutaneous transluminal coronary angioplasty without complicating cardiac conditions. Because the medical records on some provinces such as Quebec and Manitoba are not included in CIHI’s DAD database, we are unable to construct indices for those provinces. As for weights, “Resource Intensity Weights” (RIW) in 2003 from CIHI are used to aggregate the number of each CMG procedure.24 A procedure-based indicator 23 CMG is a classification system designed to aggregate acute care inpatients with similar clinical and resource utilization characteristics. It assigns acute care inpatients to groups based on clinical and administrative data collected via CIHI’s Discharge Abstract Database (DAD). 24 The RIW system is a relative resource allocation methodology for estimating a hospital’s inpatient-specific costs for both acute and day procedure care. In this case, averaged expected length of stay (ELOS) across all age groups and complexity levels is the RIW for each CMG code. 19 Table 3: Cost Per Case and RIW For Each CMG Code CMG Cost Per Case RIW 178 $22,858.75 16.31 179 $14,031.53 8.42 188 $9,447.85 8.39 189 $4,921.61 5.23 Table 4: Number of Procedures and Indices; Canada (provinces in DAD database) Year CMG178 CMG179 CMG188 CMG189 CPC Index RIW Index 1994 642 8096 7257 927 1.00 1.00 1995 643 8308 7707 935 1.04 1.04 1996 3098 7579 3634 6510 1.21 1.24 1997 2949 9776 4323 10773 1.48 1.54 1998 3183 10078 5473 11615 1.60 1.69 1999 3100 9971 6471 12443 1.65 1.76 can be calculated using a method that is similar to the CWAI proposed by ONS in the U.K.: P Number of Proceduresit × RIWi , RIW Indext = P i i Number of Proceduresi1994 × RIW i where i stands for each of the CMG code. The RIW indices (for provinces that have medical records in CIHI’s DAD) are also included in the appendix. Although the weights used to construct RIW indices are not “costs”, we can still treat them as proxies if “expected length of stay” is proportional to the cost of each procedure. Fortunately, “cost per case” (CPC) in 2002 for each of the specified CMG code can be requested from Ontario Case Costing Initiative (OCCI).25 Table 3 shows the weights (both RIW and “cost per case”) used to aggregate the numbers of procedures. Then we may apply the CWAI method directly to measure the output of heart attack treatments in Ontario. Accordingly, P Number of Proceduresit × CPCi CPC Indext = P i . i Number of Proceduresi1994 × CPCi Together with the cost(GDP) index (see tables 4–6), five different kinds of output indices for Ontario can be constructed based on the data from CIHI and OCCI. The results for the 1994–1999 period are illustrated in table 8 and figure 1. To look at the trend at national level, table 9 and figure 2 show these indices for Canada. These tables and figures show that, generally for each year, RIW Index > CPC Index > 25 OCCI is an under-taking of the Ontario Ministry of Health and Long-Term Care. It was created to continue the work started by the Ontario Case Costing Project (OCCP). 20 Year 1994 1995 1996 1997 1998 1999 Table 5: Number of Procedures and Indices; Ontario CMG178 CMG179 CMG188 CMG189 CPC Index RIW Index 371 4638 3651 497 1.00 1.00 365 4851 3821 481 1.04 1.04 1630 4558 1710 2625 1.18 1.19 1620 5933 2307 3868 1.46 1.48 1509 6037 2820 4442 1.52 1.56 1523 5940 3213 4978 1.57 1.63 Table 6: Number of Heart Attack Cases, Cases Year No. Index 1994 21457 1.00 1995 22427 1.05 1996 23999 1.12 1997 23996 1.12 1998 24176 1.13 1999 25036 1.17 Patient Days and Indices; Ontario Patient Days No. Index 187544 1.00 190112 1.01 196622 1.05 193343 1.03 192151 1.02 201687 1.08 Table 7: Hospitals GDP; Ontario; 1997 Constant Dollars Year Cost (GDP) Index 1994 $7,837.80 1.00 1995 $7,555.20 0.96 1996 $7,343.70 0.94 1997 $7,162.50 0.91 1998 $7,368.30 0.94 1999 $7,506.00 0.96 Year Case Index 1994 1.00 1995 1.05 1996 1.12 1997 1.12 1998 1.13 1999 1.17 Table 8: Output Indices for Ontario Patient Day Index CPC Index RIW Index 1.00 1.00 1.00 1.01 1.04 1.04 1.05 1.18 1.19 1.03 1.46 1.48 1.02 1.52 1.56 1.08 1.57 1.63 21 Cost Index 1.00 0.96 0.94 0.91 0.94 0.96 Figure 1: Output Indices for Ontario Year 1994 1995 1996 1997 1998 1999 Table 9: Output Indices for Canada Case Index Patient Day Index CPC Index RIW Index 1.00 1.00 1.00 1.00 1.06 1.03 1.04 1.04 1.11 1.04 1.21 1.24 1.10 1.00 1.48 1.54 1.10 0.98 1.60 1.69 1.14 1.01 1.65 1.76 22 Cost Index 1.00 0.98 0.96 0.96 0.97 0.98 Figure 2: Output Indices for Canada Case Index > Patient Day Index > Cost Index. We may notice that the cost index is always less than 1, which reflects the fact that both federal and provincial cut budget for health care during the 1994–1999 period, since Statistics Canada simply takes the health care budget as output (GDP). When the case index is compared with patient day index, we can see an obvious difference: patient day index remains almost constant (less than 1.10) in the period, while the case index increases slightly. The gap between the two indices becomes bigger after the base year (1994). Such difference shows decreasing average days of stay in hospital for a single complete heart attack treatment, which may be regarded as an indicator of “quality change” or“productivity improvement” in the treatment. As for the “procedure-based” indices (CPC and RIW), they increase much more than other indices after 1996. The underlying reason for the “dramatic increase” is the “big sudden jump” of the numbers of some CMG procedures. Figure 3 and figure 4 illustrate the changes graphically for both Ontario and Canada. From 1995 to 1996, the procedure numbers of CMG 178 and CMG 189 increased more than five times, while those figures of CMG 179 and CMG 188 moved in the opposite direction, which may imply substitutions in these procedures. However, this effect cannot offset the increasing effect from CMG 178 and CMG 189, thus leading to a small upward change in both CPC and RIW indices in the period. But from 1996 to 23 Figure 3: Number of CMG procedures for Ontario 1997, nearly all the numbers of four CMG procedures increased substantially, which generated an even bigger “jump”. One possible explanation for these big movements is that the diagnostic procedure “cardiac catheterization” showed significant technological improvement in 1996 and could detect the extent of arterial blockage more accurately. Therefore, patients tended to rely more on such procedure before undergoing coronary bypass surgeries. Furthermore, using the “RIW” weights leads to higher output indices than using “CPC” to aggregate the procedure numbers. It is probably because “CPC” system places less weight on CMG 189 than “RIW”, and as we can see from figure 3 and figure 4, the number of CMG 189 procedures had the largest increasing rate in the period. As a result, the more increase in the number of CMG 189 procedures by percentage, the bigger difference between these two indices. The “output” (case) index might be misleading if we look at the measure from the perspective of “activity” (procedure). Although the case index has a slightly upward trend, both the “CPC” and “RIW” indices increased far more significantly in the same period. That is, in each case, the patient had much more procedures than before while receiving the treatment. Therefore, the simple number of cases is unable to account for the quality change or improvement in the treatment of heart attacks. However, on the other hand, one can speculate: is there indeed any quality improvement? Some evidence gave a negative answer. Health researchers have investigated the outcomes of utilizing such procedures to treat acute myocardial infarction (heart attack). They compared the use of invasive cardiac procedures and the mor24 Figure 4: Number of CMG procedures for Canada (provinces in DAD database) tality rates among 224,258 elderly Medicare beneficiaries in the United States and 9444 elderly patients in Ontario, each of whom had a new acute myocardial infarction in 1991. What they found is that the U.S. patients were significantly more likely than those in Canada to undergo percutaneous transluminal coronary angioplasty (11.7 percent vs. 1.5 percent), and coronary-artery bypass surgery (10.6 percent vs. 1.4 percent) during the first 30 days after the infarction. In the following 180 days these differences still persisted although narrowed. U.S. patients had slightly but significantly lower 30-day mortality rates than Canadian (Ontario) patients (21.4 percent vs. 22.3 percent). But the one-year mortality rates were almost identical with 34.3 percent in the U.S. vs. 34.4 percent in Ontario (Tu et al., 1997). Therefore, they concluded that the much higher cardiac procedures usage rates do not bring better long-term survival rates to elderly U.S. patients with heart attacks. As mentioned earlier, it is sometimes difficult to distinguish “output” from “outcome”. However, as a general rule, quality improvement should be reflected in better outcomes to some extent. Therefore, how to measure the output with quality being adjusted becomes a crucial problem. Since it involves outcome measurement and is out of this paper topic, future research can be carried out to explore possible solutions. 25 6 Conclusion and Further Studies In this paper, we choose heart attack as a typical acute clinical disease to compare the direct output indices constructed on different bases. Theoretically, statistical agencies can use direct output “proxies” (indicators) to measure the output (GDP) for the whole health care sector on a disease-based classification system (e.g., stroke, diabetes). However, as far as Ontario is concerned, it turns out that the choice of “proxy” has large influence on final output (GDP) results. Different “activity” proxies (such as patient days and procedures) may result in largely different output indices. Even for the procedure-based approach, using different weights (shares) can lead to somewhat slightly different figures. When it comes to the national level, as mentioned earlier, both the CPC index and RIW index for Canada do not account for the records of some provinces like Quebec and Manitoba, and the cost index is based on the GDP for all hospitals rather than heart attack treatments. Moreover, the CPC index is based on Ontario’s “costs per case” as weights, and it is assumed that such costs remain the same for all other provinces, which might not be the case in reality. Furthermore, the “costs” data may not be from all Ontario hospitals, which can cause an insufficient representation problem. As a result, strictly speaking, these indices for Canada are not comparable.26 Therefore, important problems need to be addressed before these approaches can be implemented. Which method should be used by statistical agencies in practice requires further investigation. Research may also be necessary to evaluate the properties of different direct approaches or even different weights for the same approach. The large difference between directly measured output and health care GDP has interesting implications for cross-country (e.g. U.S. and Canada) comparison. Lastly, direct output-based cost-effectiveness study on a disease treatment across different ages/provinces, or on the CMG procedures can be innovative future research topics in this field. Further studies can extend our results in heart disease treatments to other major categories. The trends of different measurement methods should be compared and analyzed to obtain a deeper understanding of the impact on health care output and productivity measurement. 26 However, for reference purpose, they do reflect the general output trend to some extent. 26 References Ashaye, Timi (2001) “Recent Developments in the Measurement of General Government Output”, Economic Trends, No. 576, November 2001, 41-44. Baumol, William J. (1967) “Macroeconomics of Unbalanced Growth: The Anatomy of Urban Crisis”, American Economic Review, Vol. 57, Issue 3 (June, 1967), 415-426. Berndt, Ernst R. et al. (2001) “Price Indices for Medical Care Goods and Services”, Medical Care Output and Productivity, Chicago and London, The University of Chicago Press 141-200. Caplan, David (1998) “Measuring the Output of Non-market Services”, Economic Trends, No. 539, October 1998, 45-49. CIHI (2003) “DAD Resource Intensity Weights and Expected Length of Stay 2003”, CIHI publication, Canadian Institute for Health Information. Cutler, David M. (2002) “Equality, Efficiency, and Market Fundamentals: The Dynamics of International Medical-Care Reform”, Journal of Economic Literature, Vol. XL, 881-906. Cutler, David M. and Berndt, Ernst R. (2001) “Introduction”, Medical Care Output and Productivity, Chicago and London, The University of Chicago Press 1-11. Cutler, David M. and Richardson, Elizabeth (1998) “The Value of Health: 1970– 1990”, American Economic Review, Papers and Proceedings, Vol. 88, No. 2, 97-100. Cutler, David M. and Richardson, Elizabeth (1997) “Measuring the Health of the United Sates Population”, Brookings Papers on Economic Activity, Microeconomics, 217-271. Daniel, Judy et al. (1997) “Measuring Outputs, Inputs and Productivity For Australian Public Acute Care Hospitals”, Economics and Health ’97, Working Paper, 19th Australian Conference of Health Economists, Melbourne University. Diewert, W.E., (1981) ‘The Economic theory of Index Numbers: A Survey,’ in Deaton, Angus ed., Essays in the Theory and Measurement of Consumer Behavior in honour of Sir Richard Stone, Cambridge University Press, 163-208. Diewert, W. Erwin (1996) ‘Axiomatic and Economic Approaches to International Comparisons,’ Working Paper 5559, National Bureau of Economic Research. 27 Eurostat (1998) “Report of The Task Force: Prices and Volumes For Health—NACE N ”, Working Paper, European Statistics. Eurostat (2000) “Report of The Task Force Health II: Volume Measures For Health”, Working Paper, European Statistics. Grossman, Michael (1972) “The Demand For Health: A Theoretical and Empirical Investigation”, New York, Columbia University Press. Hillinger, Claude (2002) ‘Consistent Aggregation and Chaining of Price and Quantity Measures,’ Journal of Economic and Social Measurement, 28, 120. Inter-Secretariat Working Group on National Accounts, 1993, System of National Accounts 1993, Commission of the European Communities, IMF, OECD, UN, World Bank. Konüs, A.A., (1939) ‘The Problem of the True Index of the Cost of Living’, Econometrica, 7:1, 10-29. Pritchard, Alwyn and Powell, Matthew (2001) “Direct Measures of Government Output: A Few Conceptual and Practical Issues”, Working Paper, OECD Meeting of National Accounts Experts, STD/NA(2001)28. Triplett, Jack E., (2001) ‘Should the Cost-of-Living Index Provide the Conceptual Framework for a Consumer Price Index?’ The Economic Journal, 111 (June), F321-F335. Tu, Jack V. et al. (1997) “Use of Cardiac Procedures and Outcomes in Elderly Patients With Myocardial Infarction in The United States and Canada”, The New England Journal of Medicine, Vol. 336, No. 21, 1500-1505. 28 Table 10: Number of Heart Attack Cases, Patient Days and Indices; Alberta Cases Patient Days Year No. Index No. Index 1994 4162 1.00 35842 1.00 1995 4362 1.05 35572 0.99 1996 4548 1.09 36721 1.02 1997 4410 1.06 34803 0.97 1998 4544 1.09 35809 1.00 1999 4787 1.15 37372 1.04 Table 11: Number of Heart Attack Cases, Patient Days and Indices; B.C. Cases Patient Days Year No. Index No. Index 1994 6284 1.00 46066 1.00 1995 6487 1.03 47427 1.03 1996 6730 1.07 47950 1.04 1997 6362 1.01 42591 0.92 1998 6504 1.04 43762 0.95 1999 6806 1.08 45801 0.99 Table 12: Number of Heart Attack Cases, Cases Year No. Index 1994 2019 1.00 1995 2062 1.02 1996 2192 1.09 1997 2025 1.00 1998 2026 1.00 1999 2201 1.09 Patient Days and Indices; Manitoba Patient Days No. Index 17790 1.00 18626 1.05 19501 1.10 16687 0.94 17190 0.97 20599 1.16 Table 13: Number of Heart Attack Cases, Patient Days and Indices; New Brunswick Cases Patient Days Year No. Index No. Index 1994 1730 1.00 16330 1.00 1995 1790 1.03 16466 1.01 1996 1668 0.96 14187 0.87 1997 1807 1.04 15160 0.93 1998 1744 1.01 17772 1.09 1999 1876 1.08 15121 0.93 29 Table 14: Number of Heart Attack Cases, Patient Days and Indices; Nova Scotia Cases Patient Days Year No. Index No. Index 1994 1951 1.00 20238 1.00 1995 2100 1.08 19812 0.98 1996 2087 1.07 20182 1.00 1997 2212 1.13 20986 1.04 1998 2041 1.05 17768 0.88 1999 2288 1.17 18836 0.93 Table 15: Number of Heart Attack Cases, Patient Days and Indices; NT Cases Patient Days Year No. Index No. Index 1994 17 1.00 94 1.00 1995 37 2.18 232 2.47 1996 25 1.47 152 1.62 1997 42 2.47 346 3.68 1998 52 3.06 352 3.74 1999 36 2.12 216 2.30 Table 16: Number of Heart Attack Cases, Patient Days and Indices; PEI Cases Patient Days Year No. Index No. Index 1994 289 1.00 2613 1.00 1995 286 0.99 2455 0.94 1996 276 0.96 2540 0.97 1997 295 1.02 2364 0.90 1998 395 1.37 3066 1.17 1999 367 1.27 3372 1.29 Table 17: Number of Heart Attack Cases, Patient Days and Indices; Quebec Cases Patient Days Year No. Index No. Index 1994 13743 1.00 156612 1.00 1995 14186 1.03 154116 0.98 1996 14510 1.06 150113 0.96 1997 14561 1.06 144839 0.92 1998 14265 1.04 136912 0.87 1999 14293 1.04 135813 0.87 30 Table 18: Number of Heart Attack Cases, Patient Days and Indices; Saskatchewan Cases Patient Days Year No. Index No. Index 1994 2001 1.00 17074 1.00 1995 2133 1.07 16840 0.99 1996 2305 1.15 18327 1.07 1997 2278 1.14 17024 1.00 1998 2060 1.03 15688 0.92 1999 2122 1.06 14720 0.86 Table 19: Number of Heart Attack Cases, Patient Days and Indices; Yukon Territory Cases Patient Days Year No. Index No. Index 1994 23 1.00 181 1.00 1995 27 1.17 161 0.89 1996 21 0.91 100 0.55 1997 37 1.61 215 1.19 1998 26 1.13 104 0.57 1999 35 1.52 208 1.15 Table 20: Number of Procedures and Indices; Alberta Year CMG178 CMG179 CMG188 CMG189 RIW Index 1994 57 928 775 100 1.00 1995 40 887 866 109 1.01 1996 252 1116 948 1117 1.73 1997 234 1200 871 1496 1.84 1998 336 1145 1138 1518 2.07 1999 313 1264 1166 1530 2.13 Table 21: Number of Procedures and Indices; British Columbia Year CMG178 CMG179 CMG188 CMG189 RIW Index 1994 89 1304 1619 192 1.00 1995 106 1286 1560 175 0.98 1996 403 1174 522 1717 1.10 1997 439 1476 620 2725 1.44 1998 476 1527 791 2890 1.57 1999 505 1528 1169 3205 1.76 31 Table 22: Number of Procedures and Indices; New Brunswick Year CMG178 CMG179 CMG188 CMG189 RIW Index 1994 36 214 295 43 1.00 1995 37 216 306 27 1.01 1996 268 53 131 148 1.31 1997 58 38 148 559 1.07 1998 268 173 205 647 2.15 1999 273 165 242 609 2.17 Table 23: Number of Procedures and Indices; Newfoundland Year CMG178 CMG179 CMG188 CMG189 RIW Index 1994 23 182 214 17 1.00 1995 27 184 165 17 0.91 1996 148 169 24 268 1.43 1997 141 236 21 722 2.17 1998 178 228 35 786 2.43 1999 100 81 20 650 1.55 Table 24: Number of Procedures and Indices; Nova Scotia Year CMG178 CMG179 CMG188 CMG189 RIW Index 1994 46 505 228 28 1.00 1995 29 559 491 66 1.37 1996 232 307 52 376 1.24 1997 247 540 117 764 1.92 1998 239 547 183 714 1.95 1999 213 560 230 727 1.97 Table 25: Number of Procedures and Indices; Saskatchewan Year CMG178 CMG179 CMG188 CMG189 RIW Index 1994 20 325 475 50 1.00 1995 39 325 498 60 1.08 1996 165 202 247 259 1.07 1997 210 353 239 639 1.61 1998 177 421 301 618 1.67 1999 173 433 431 744 1.91 32
![[#EXASOL-1429] Possible error when inserting data into large tables](http://s3.studylib.net/store/data/005854961_1-9d34d5b0b79b862c601023238967ddff-300x300.png)