ARTICLE IN PRESS Journal of Science
advertisement

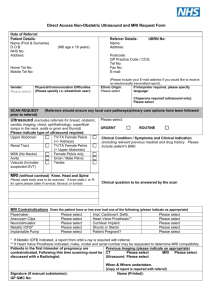
G Model JSAMS-1145; No. of Pages 6 ARTICLE IN PRESS Journal of Science and Medicine in Sport xxx (2015) xxx–xxx Contents lists available at ScienceDirect Journal of Science and Medicine in Sport journal homepage: www.elsevier.com/locate/jsams Original research Normative MRI, ultrasound and muscle functional MRI findings in the forearms of asymptomatic elite rowers Michael K. Drew a,b,c,∗ , Larissa Trease d , J.P. Caneiro e , Ivan Hooper a , Chin-Chin Ooi f,g , Peter Counsel h , David A. Connell h,i , Anthony A. Rice j , Emma Knight k , Gregory Hoy l , Gregory Lovell m a Department of Physical Therapies, Australian Institute of Sport, Australia Department of Physiotherapy, Faculty of Health, University of Canberra, Australia c Australian Centre for Research into Injury in Sport and its Prevention (ACRISP), Federation University, Australia d Department of Sports Medicine, Rowing Australia, Australia e Department of Physiotherapy, Curtin University, Australia f Department of Diagnostic Radiology, Singapore General Hospital, Singapore g Department of Diagnostic Radiology, Monash University, Australia h Imaging at Olympic Park, Australia i Department of Medicine, Nursing and Healthcare, Monash University, Australia j Department of Physiology, Australian Institute of Sport, Australia k Department of Performance Research, Australian Institute of Sport, Australia l Melbourne Orthopaedic Group, Australia m Department of Sports Medicine, Australian Institute of Sport, Australia b a r t i c l e i n f o Article history: Received 26 September 2014 Received in revised form 26 January 2015 Accepted 14 February 2015 Available online xxx Keywords: Rowing Ultrasound imaging Intersection syndrome Magnetic resonance imaging Forearm Athletes a b s t r a c t Objectives: Forearm injuries are common and debilitating to elite rowers. Chronic exertional compartment syndrome, intersection syndrome and proximal radial bone stress injuries have been documented in this population. This paper explores the imaging findings related to these conditions in asymptomatic elite rowers. Design: Observational study. Methods: 19 asymptomatic senior elite and under-23 rowers currently competing at National level or above underwent ultrasound (US), Magnetic Resonance Imaging (MRI) and muscle functional MRI evaluation of their forearms. A comprehensive evaluation sheet identifying characteristics of bone stress, intersection syndrome and chronic exertional compartment syndrome was utilised based on a literature search and review by senior clinicians working with this population. Results: Peritendinous fluid of Extensor Carpi Radialis Longus (n = 10, 53%) or Extensor Carpi Radialis Brevis (n = 6, 32%) was a common finding on US. MRI had a higher rate of identification than US. Extensor Digitorum (Coeff = −1.76, 95%CI −3.04 to −0.49), Flexor Carpi Radialis (Coeff = −2.86, 95%CI −5.35 to −0.38) and Flexor Carpi Ulnaris (Coeff = −3.31, 95%CI −5.30 to −1.32), Pronator Teres (Coeff = −3.94, 95%CI −6.89 to −0.99), and Supinator (Coeff = −168, 95%CI −3.28 to −0.02) showed statistically significant changes immediately post-exercise. Mild proximal radial marrow hyperintensity was present (n = 15, 78.9%) with three participants (15.8%) also having mild periosteal oedema of the radius. Conclusions: Imaging findings commonly seen in symptomatic populations are observed in elite, asymptomatic rowers. Care should be taken when diagnosing bone stress injuries, intersection syndrome and compartment syndrome on imaging findings alone. Data presented can be utilised as a normative dataset for future case studies. © 2015 Published by Elsevier Ltd on behalf of Sports Medicine Australia. 1. Introduction ∗ Corresponding author at: Corresponding author. E-mail addresses: Michael.drew@ausport.gov.au, michaelkdrew@gmail.com (M.K. Drew). Forearm injuries in international rowers are associated with high loss of training days.1 Of these, intersection syndrome, chronic exertional compartment syndrome (CECS), and proximal radius stress reaction have been recorded in an Australian population.1 http://dx.doi.org/10.1016/j.jsams.2015.02.002 1440-2440/© 2015 Published by Elsevier Ltd on behalf of Sports Medicine Australia. Please cite this article in press as: Drew MK, et al. Normative MRI, ultrasound and muscle functional MRI findings in the forearms of asymptomatic elite rowers. J Sci Med Sport (2015), http://dx.doi.org/10.1016/j.jsams.2015.02.002 G Model JSAMS-1145; No. of Pages 6 ARTICLE IN PRESS M.K. Drew et al. / Journal of Science and Medicine in Sport xxx (2015) xxx–xxx 2 A record of normative imaging findings in this population currently does not exist and imaging studies of forearm injuries in this population are devoid of control groups.2–4 Therefore establishing normative imaging results in this population is imperative to allow for better comparisons and eventually improved diagnostic procedures and statistics in this population. This may assist clinicians to understand the pathogenesis of the three conditions. Intersection syndrome (IS) is described as a non-infectious inflammatory condition localised to the area at the intersection of the first and second dorsal extensor compartments. Typical signs and symptoms consist of tenderness on palpation, pain on wrist movements (particularly extension), local swelling, erythema and crepitus with flexion and extension of the wrist.2–5 The aetiology of this condition is still under debate. A recent ultrasound study has found peritendinous oedema and small amounts of synovial fluid within the tendon sheaths at the point of intersection, thickened tendons and hyperechoic nodules within the fluid related to proliferation of the synovial membrane.3 This indicates tendinopathic processes. In a case-series (Level IV evidence), compartmental tearing between the first and second dorsal comparts has been shown surgically with authors proposing early surgical management.6 It is therefore plausible that intersection syndrome may be two separate pathologies that can also be coexistent; tendinopathic changes and inter-compartmental tearing. If these changes can be imaged it could streamline care to either surgical or conservative management. It is currently unknown whether MRI and/or ultrasound can assess the integrity of the compartmental fascia at the intersection and whether tearing is present in asymptomatic, elite rowing populations. Chronic exertional compartment syndrome is a state of intermittent and reversible elevation of intra-compartmental pressure related to exertion. It has been documented in athletes of motorcycle racing,7,8 weight lifting9 and kayaking10 and is under-reported in the rowing literature11 when compared to recent Australian data.12,13 The diagnostic value of MRI scans in chronic exertional compartment syndrome of the lower leg has been shown to be of high value.14,15 However, diagnosing CECS in rowers presents a unique challenge due to the nature of it being a water-based sport. The ergometer is a viable alternative to use in the replacement of on-water rowing however, it neglects the “feathering” action (rotation of the oar to change the angle of the blade) and repetitive gripping tasks (such as rope winding exercises) may over accentuate the feathering action. Muscle functional MRI (mfMRI) studies have been used recently to determine the level to which a muscle is involved in a functional task.16 The purpose of this study was to: (i) establish US imaging results in asymptomatic elite rowers; (ii) establish MRI findings in asymptomatic elite rowers (iii) establish muscle functional MRI changes following a set stationary ergo workload and (iv) to assess the relationship that level of competition and gender has on the imaging findings. 2. Methods Elite asymptomatic rowers (n = 20) competing in senior (n = 7, male: female 4:3) and under-23 levels (n = 13, male: female, 7:6) were recruited through the Victorian Institute of Sport during the domestic season of competition (January, 2013). Inclusion and exclusion criteria are presented in Table 1. This study was approved by the Australian Institute of Sport Ethics Committee and was performed following the Declaration of Helsinki. All patients provided written informed consent. All participants underwent a standard radiological examination procedure. The study design is shown in Supplementary Fig. 1. All Table 1 Inclusion and exclusion criteria. Inclusion criteria Exclusion criteria Currently competing at National level Full training without restrictions or limitations Able to complete the ergometer test >18 years of age Current injury or illness anywhere in the body Previous history of injury to the forearm or wrist region Previous symptoms in the wrist such as tightness and/or pain that required medical or physiotherapy treatment or prevented training Contra-indication to MRI or standard safety procedures in accordance with standard radiology policies images were taken on the inside arm of sweep rowers (ipsilateral side to the oar) and the dominant arm of scullers. All participants underwent a standard ultrasound procedure to evaluate the intersection region. The standard assessment incorporated results from a literature search and the clinical experience of the authors with backgrounds in sports medicine, radiology, surgery and sonography (LT, GH, GL, OC, and DC). All ultrasound examinations were performed using a Philips iU22 (Philips Healthcare, Bothell, WA) that was equipped with a 17.5 MHz high resolution linear transducer. A single sonographer (OC), with greater than 10 years of experience in musculoskeletal ultrasound, performed the scans. Patients were seated facing the sonographer, with their forearm rested comfortably on the examination couch, elbow in mid-flexion and the wrist in pronation. A preprogramed scanning technical protocol (with optimised scanning parameters such as depth, frequency, focal zone and colour Doppler setting for perfusion) was used to ensure consistency of results obtained. Multiple transverse and longitudinal scans were acquired at the dorsal aspect of the distal forearm and wrist, with particular attention paid to the point of the intersection region. The anterior-posterior (AP) thickness and cross-sectional area (CSA) of the tendons in the first and second compartments were measured. The presence of tendinopathic signs (subcutaneous oedema, peritendinous fluid, fluid between the first and second extensor compartments, breaching or tearing of the synovia, hypervascularity of tendons, compartment thickness at the intersection and tendon hypoechogeneity) were observed and documented. In addition, dynamic real-time scanning with flexion–extension of the patient’s wrist was performed and mobility of the tendons at the level of intersection was evaluated for presence of staccato tendon movement. All MRI scans were taken in a single Philips Ingenia 3T scanner (Philips, Veenpluis, Best, Netherlands) using a 32 channel phased array body coil (Invivo, Gainesville, FL, USA) with their arm extended in a true anatomical position. The scans were obtained from the wrist to the elbow in the axial plan at the pre-exercise, immediate post-exercise and delayed post-exercise time points. The scan parameters were as follows. Pre-exercise axial PD spin fast spin echo technique (40 slices at TR 3400 ms, TE 30 ms, 12.0 cm × 12.0 cm Field of View (FOV), 512 × 512 matrix, 3.0 mm slice thickness, 7 to 9 mm gap, ETL of 14 and 1 NSA) extending from the distal radioulnar joint to the proximal. Pre-exercise T2 SPAIR (fat sat) axial fast spin echo technique was the same 40 slices with a constant FOV, slice thickness and slice gap. The matrix size was 432 × 432 and using a TR of 8500 ms, TE 50 ms, ETL of 14 and 2 NSA. The immediate post-exercise and delayed scans used the same parameters as the pre-exercise T2 Axial SPAIR. Muscle functional MRI (mfMRI) techniques were utilised to evaluate the effect of ergometer rowing on the forearm muscles. The participants rested for 30 min prior to the mfMRI. This occurred simultaneously with the ultrasound evaluation. The ergometer protocol consisted of a standardised warm up of 3 min at a selfselected rate and wattage; following this the participant completed Please cite this article in press as: Drew MK, et al. Normative MRI, ultrasound and muscle functional MRI findings in the forearms of asymptomatic elite rowers. J Sci Med Sport (2015), http://dx.doi.org/10.1016/j.jsams.2015.02.002 G Model JSAMS-1145; No. of Pages 6 ARTICLE IN PRESS M.K. Drew et al. / Journal of Science and Medicine in Sport xxx (2015) xxx–xxx 8 min of rowing on a stationary ergometer at 90% wattage of their most recent 6 km ergometer test. All workloads were completed on a Concept II Rowing Ergometer (Concept2, Vermont, USA) and utilised drag factors consistent with the Rowing Australia policies for ergometer testing for the participant’s weight class and gender (lightweight women = 95; lightweight men and heavyweight female = 105; heavyweight men = 115). The participants were instructed to maintain a constant rate for the test (24–26 strokes/min). This protocol was selected to ensure that the participant had to grip the handle to provide a sufficient stimulus to invoke MRI detectable changes. Upon completion of the test, the participants were allowed to regain their breath and proceed immediately into the MRI scanner for post-exercise imaging. All participants began imaging within 2 min of completing the test. All delayed post-exercise MRI images were taken between 60 and 90 min (mean = 73.5 min) following the ergometer test. During the break, participants were instructed to rest quietly in a seated position and avoid any physical activity and tasks which would change their forearm signal such as lifting bags. After scanning, the ultrasound data was analysed by the sonographer (OC). The baseline MRIs were evaluated by two radiologists (DC and PC) using the same standard reporting proforma as the sonographer (Table 2). Calculation of the muscle T2 signal intensities utilised the InteleViewer program (InteleViewer, Intelerad Medical Systems Incorporated). Regions of interest (ROI) were identified on the T2 images at the level where the proximal interosseous membrane became visible. The mean and standard deviations of signal intensities were measured for each muscle. This enabled visualisation and data collection of the m. Extensor Carpi Radialis Brevis (ECRB), m. Extensor Carpi Radialis Longus (ECRL), m. Extensor Carpi Ulnaris (ECU), m. Extensor Digitorum (ED), m. Extensor Digiti Minimi (EDM), m. Flexor Carpi Ulnaris (FCU), m. Flexor Digitorum Profundus (FDP), m. Flexor Digitorum Superficialis (FDS), m. Palmaris Longus (PL) (if present), m. Pronator Teres (PT), m. Brachioradialis (BR), and m. Supinator (S). When defining the ROI, all non-muscular tissue such as fat, fascia, bone and vessels was avoided. This protocol is in accordance with other studies.3 Analysis was performed using Stata 13 (Version 13 IC, StataCorp, USA). To look at the relationship between the presence of fluid in either or both ECRL and ECRB, and the level of competition and gender, univariate logistic regression models were fitted with presence of fluid as the response variable and competition, gender and their interaction as explanatory variables. The mean T2 values of signal intensity were measured in all three scans and utilised for analysis. To look at changes in T2 signal intensity over the three time points (baseline, immediately post-, delayed post-exercise), a linear mixed model for each muscle was fitted with gender, competition, time and their interactions as fixed effects and participant as a random effect to account for within participant correlation. 3 were no interactions between gender and competition and therefore removed from the model. Comparison between under-23 and senior athletes, revealed no association between athlete group and fluid present in ECRL (OR = 0.53, 95%CI 0.09–3.31) or ECRB (OR = 1.17, 95%CI = 0.17–8.09) alone or in both tendons (OR = 0.29, 95%CI 0.02–3.48). Similarly, no association was found between gender and fluid present in ECRL (OR = 2.92, 95%CI 0.44–19.23) or ECRB (OR = 1.71, 95%CI = 0.23–12.89) alone or in both tendons (OR = 2.63, 95%CI 0.22–31.35). Tendon volumes were ECRL (median = 3.2 mm, range 2.5–3.8 mm), ECRB (median = 2.8, range = 2.0–3.3 mm), APL (median 2.5 mm, range 1.9–3.0 mm) and EPB (median = 1.9, range 1.4–2.4 mm). The results of the baseline MRI scans can be found in Table 2. Mild hyperintensity of the pronator quadratus muscle was present in 18 of 19 rowers (94.7%) on pre-exercise imaging (Sup. 3). Peritendinous fluid was observed in at least one tendon of compartment 2 in all but one participant (n = 18, 94.7%; ECRL, n = 10, ECRB, n = 6, both ECRL and ECRB, n = 4) (Sup. 2). Mild bone marrow hyperintensity (Sup. 4) in the proximal radius was present in the majority of the participants (n = 15, 78.9%) with three (15.8%) also having mild periosteal oedema. One participant (5.3%) had foci of marrow hyperintensity in both the ulna and radius. In nine (47.4%) participants, there was no evidence of bicipitoradial bursal effusion with a trace of fluid in seven (36.8%) and mild effusion in three (15.8%) (Sup. 5), respectively. A significant random effect of participant was observed in all linear mixed models (Coeff = 4.43, 95%CI 0.98–20.04 to 160.34, 95%CI 72.68–353.72). A significant effect of gender was observed in ECRB (Coeff = 8.57, 95%CI 1.45 to 15.68), ECU (Coeff = 3.02, 95%CI 0.24 to 5.80), ED (Coeff = 6.19, 95%CI 1.27 to 11.12), and EDM (Coeff = 5.35, 95%CI 1.30 to 9.43) with female participants as the reference. There was no significant interactions in the mixed models and therefore removed. After accounting for gender and competition, a statistically significant decreased signal intensity immediately following exercise was observed in ED (Coeff = −1.76, 95%CI −3.04 to −0.49), FCR (Coeff = −2.86, 95%CI −5.35 to −0.38) and FCU (Coeff = −3.31, 95%CI −5.30 to −1.32), PT (Coeff = −3.94, 95%CI −6.89 to −0.99), and S (Coeff = −168, 95%CI −3.28 to −0.02). FCR (Coeff = −2.65, 95%CI −5.26 to −0.03) and FCU (Coeff = −2.68, 95%CI −4.82 to −0.55) remained significantly decreased in signal intensity in the delayed scan. Non-significant signal intensity increases were observed in FDS (Coeff = 1.44, 95%CI −0.99 to 3.88), FDP (Coeff = 1.08, 95%CI −1.28 to 3.43), RB (Coeff = 1.95, 95%CI −0.26 to 4.17) and ECRB (Coeff = 0.48, 95%CI −0.88 to 1.84) immediately following exercise. The percentage changes from the baseline in the T2 shifts of the exercise-induced MRI changes are presented in Table 3. 4. Discussion 3. Results Seventeen of 19 participants completed all scans. This was the entire eligible population. Two participants withdrew after the immediate post-exercise scan citing work-related commitments. No adverse events were recorded. The results of the ultrasound scan are presented in Table 2. No pathology was found in the first extensor compartment (APL, EPB) of any of the participants. Peritendinous fluid was identified around the tendons of ECRL (n = 10, 53%; male:female, 7:3) and ECRB (n = 6, 32%; male:female, 4:2) with four participants having fluid around both tendons (22%; male:female, 3:1) (Sup. 2). One female participant (5%) had hypervascularity present on Doppler examination of her ECRB, co-existing with peritendinous fluid. No tearing of the synovia of either compartment was identified. There This study has found that ultrasound findings are common in elite, asymptomatic rowers. No tendon pathology was found in the tendons of the thumb muscles. Tendinopathic changes were found in the ECRL and ECRB tendons at the level of the intersection. No tearing of the synovia was identified on either the US or MRI evaluations and it is unclear whether these modalities of investigation can identify this. However, our study supports previous research3 indicating US to be an important part of the diagnostic procedure of rowers with forearm pain. Peritendinous fluid was common on MRI and US, with MRI showing a higher rate. Giovagorio and Miozzi3 found peritendinous oedema and small amounts of synovial fluid within the tendon sheaths at the point of intersection, thickened tendons and hyperechoic nodules within the fluid. Comparatively, in our asymptomatic population we found fluid in and around the Please cite this article in press as: Drew MK, et al. Normative MRI, ultrasound and muscle functional MRI findings in the forearms of asymptomatic elite rowers. J Sci Med Sport (2015), http://dx.doi.org/10.1016/j.jsams.2015.02.002 G Model ARTICLE IN PRESS JSAMS-1145; No. of Pages 6 M.K. Drew et al. / Journal of Science and Medicine in Sport xxx (2015) xxx–xxx 4 Table 2 Imaging findings for ultrasound, MRI and dynamic ultrasound. Compartment 1† Imaging modality Imaging finding Ultrasound Thickness at wrist APL EPB ECRL ECRB Compartment thickness at intersection Hypertrophy Intratendinous alterations Peritendinous fluid Breach or presence of tear or hole in synovium Fluid within compartment Hypervascularity of tendons on Doppler Fluid between 1st and 2nd compartment at crossover Fascial thickness between the muscle/tendons of C1/C2 at intersection Fascial thickening Stenosis of the compartment 2 Subcutaneous oedema Hypertrophy Intratendinous alterations Peritendinous fluid Breach or presence of tear or hole in synovium Fluid within compartment Stenosis of the 2nd dorsal compartment Subcutaneous oedema Movement Free movement Friction between tendons/compartments Staccato movement MRI Dynamic Ultrasound Compartment 2† 2.51 ± 0.40 1.94 ± 0.29 1.30 ± 0.10 19:0 (0%) 19:0 (0%) 19:0 (0%) 19:0 (0%) 19:0 (0%) 19:0 (0%) 18:1 (5.3%) 0.27 ± 0.05 19:0 (0%) 3.23 ± 0.38 2.71 ± 0.38 2.61 ± 0.63 17:2 (10.5%) 19:0 (0%) 7:12* (63.2%) 19:0 (0%) 18:1 (5.3%) 18:1 (5.3%) 19:0 (0%) 19:0 (0%) 19:0 (0%) 19:0 (0%) 13:6 (31.6%)* 19:0 (0%) 16:3 (15.8%)# 19:0 (0%) Extension 0:19 (100%) 19:0 (0%) 19:0 (0%) 19:0 (0%) 19:0 (0%) 1:18 (94.7%)+ 19:0 (0%) 16:3 (15.8%)# 19:0 (0%) Flexion 0:19 (100%) 19:0 (0%) 19:0 (0%) † Continuous data are presented as mean ± standard deviation measured in millimetres (mm). Categorical data, no:yes, Percentages presented represent prevalence of positive finding; APL: Abductor pollicis longus, C1: compartment 1, C2: compartment 2; EPB: extensor pollicis brevis; ECRL: extensor carpi radialis longus, ECRB: extensor carpi radialis brevis. # 2/3 has trace of fluid. * Fluid present in APL (n = 5) and EPB (n = 1). + Fluid present in ECRL (n = 7) and both ECRL and ECRB (n = 11). * Mild peritendinous fluid was identified in at least one tendon in C2 (ECRL n = 10, ECRB n = 6, both ECRL and ECRB n = 4). tendon sheaths which indicates that these may be a normal finding in this population. The results of this study highlight the need to include matched controls in future diagnostic studies. The MRI results in the study indicate that one participant would be considered indicative of having intersection syndrome (Sup. 6) for most radiologists evaluating a symptomatic patient and two further participants could reflect very low grade intersection syndrome (Sup. 7). If taken as false positives, this would give a false positive rate of 5–15% based on imaging alone, although subclinical pathology might also account for these findings. Future studies should explore alternate imaging methodologies such as post-Gadolinium MRI to identify findings of fluid associated with tenosynovitis from physiological fluid. Bone stress injuries of the forearms have been documented in Australian rowers.1 Hyperintensity of the bone marrow was a common finding in this asymptomatic elite rowing population and may be a typical finding in this population. The high rate of mild marrow hyperintensity may be indicative of low grade subclinical stress reaction, although ultimately comparison to a non-rowing population would be needed to test this hypothesis. This study illustrates that the muscles ED, PT, FCR, FCU and S exhibit significant decreases in signal intensity following the row- Table 3 Percentage change of the T2 signal intensities of the muscle functional MRI. Muscle ECRB ECRL ECU ED EDM FCU FCR FDP FDS PL PT RB SUP Baseline versus immediate Baseline versus delayed Mean ± SD 95% CI Mean ± SD 95% CI 1.43 ± 11.78 −1.55 ± 11.98 −2.24 ± 10.50 −5.34 ± 9.58a −3.12 ± 11.61 −7.45 ± 11.40a −8.78 ± 15.56a 4.13 ± 13.39 3.25 ± 18.02 −5.66 ± 18.13 −9.63 ± 15.56a 6.70 ± 17.18 −4.46 ± 11.44a −4.43–7.29 −7.51–4.41 −7.46–2.98 −10.10 to −0.57 −8.89–2.66 −13.12 to −1.78 −17.07 to −0.49 −2.53–10.78 −6.02–12.52 −15.70–4.38 −17.92 to −1.34 −1.84–15.24 −10.15–1.23 −3.78 −2.46 −2.39 −3.02 −1.25 −4.10 1.33 −4.41 0.65 4.07 −6.77 −5.76 −3.86 −10.79–3.22 −10.27–5.36 −7.87–3.09 −8.84–2.79 −8.03–5.52 −14.14–5.94 −17.07–19.74 −10.71–1.88 −16.94–18.24 −17.30–25.45 −15.11–1.57 −11.77–0.26 −7.96–0.24 ± ± ± ± ± ± ± ± ± ± ± ± ± 12.66 14.11 9.89 10.50 12.23 18.13a 31.88a 11.37 31.76 35.37 13.81 10.87 7.40 a Statistically significant fixed effect (P < 0.05); Baseline n = 19, delayed n = 17; CI: confidence interval; SD: standard deviation; ECRB: extensor carpi radialis brevis, ECRL: extensor carpi radialis longus, ECU: extensor carpi ulnaris, ED: extensor digitorum, EDM: extensor digiti minimi, FCR: flexor carpi radialis, FCU: flexor carpi ulnaris, FDP: flexor digitorium profundus, FDS: flexor digitorium superficialis, PL: palmaris longus, PT: pronator teres, RB: radiobrachialis, S: supinator. Please cite this article in press as: Drew MK, et al. Normative MRI, ultrasound and muscle functional MRI findings in the forearms of asymptomatic elite rowers. J Sci Med Sport (2015), http://dx.doi.org/10.1016/j.jsams.2015.02.002 G Model JSAMS-1145; No. of Pages 6 ARTICLE IN PRESS M.K. Drew et al. / Journal of Science and Medicine in Sport xxx (2015) xxx–xxx ing ergometer protocol. This may be related to the aerobic exercise administered rather than the anaerobic exercises used in previous studies16,17 and is a consideration for future mfMRI study designs. Non-significant increases in FDS, FDP, RB and ECRB were observed immediately after exercise. FCR and FCU showed significant decreases in signal intensity in the delayed-MRI images and this should be taken into account clinically when imaging between 60 and 90 min after ergometer rowing. Mild MRI hyperintensity of m. pronator quadratus was seen in most of our patients, and has been previously described as a normal finding.18 CECS is a debilitating condition for elite rowers and usually results in an inability to row. Clinically MRI has been used to diagnose this condition; however, these protocols have not been evaluated in the forearm or in this population. The purpose of this study was to establish some normative data on asymptomatic elite rowers. Pragmatically we investigated what happens to the imaging between 60 and 90 min after exercise. This was chosen based on previous research which has shown that exercise-induced signal intensities changes on T2 images have a half-life of 7 min with a complete resolution between 45 min and 1 h.12 This potentially will allow clinicians to prescribe the workload outlined in this study at the athletes’ rowing club or nearby gymnasium prior to imaging as it would be impractical for a rower with suspected CECS to undertake an ergometer session at the radiology clinic. In the delayed-MRI sequence we observed that FCR and FCU decreased in signal intensity which reached statistical significance. Clinically care should be taken when making clinical judgements based on the immediate scan protocols without comparison to the normative findings. Future studies are warranted to see if this decrease in signal intensity is observed in patients suffering from CECS as an increase would usually be expected. Clinicians should also be aware that FDS, FDP, RB and ECRB have the potential to show increased signal intensity following exercise, although in this study the changes were not statistically significant. This may be due to the small sample size and this is a limitation of the study. However, the magnitude of T2 shifts seen in this study are below those observed in patients with compartment syndrome of the leg.14 A limitation of this study is that it only evaluated asymptomatic, elite rowers who were free of any forearm injury history and therefore may have limited generalisability to sub-elite and recreational rowers. Furthermore, the prevalence of many of the reported findings in this study is unknown among the general population. Future research may benefit from a wider control group containing nonrowers and symptomatic rowers. A further limitation identified before the study was that the ergometer protocol negated the feathering action of the wrist during the rowing stroke. It is unknown what impact this action has on the mfMRI findings and caution should be taken when comparing the current results to post- onwater rowing images. 5. Conclusion In ultrasound and MRI scans of the forearm in asymptomatic athletes peritendinous fluid is often seen in the region of the intersection in asymptomatic rowers. It is important to note that all fluid seen was of a small quantity and florid oedema may still be important clinically. Imaging findings without clinical symptoms may be considered normal in this population. For suspected compartment syndrome of the forearm in rowers pre- and post-exercise comparative MRI imaging may be appropriate. Post-exercise MRI should be obtained between 60 and 90 min after activity where an increase in compartment T2 signal may be diagnostic of CECS pathology. Bone marrow hyperintensity interpreted as mild bone stress was a common finding in this asymptomatic elite rowing population and this can be considered a typical finding. 5 Practical implications • Fluid around the tendons of the intersection region is a common finding. Both MRI and US are able to detect these. MRI showed a higher rate of identification. • Ultrasound allows the visualisation of tendon movements within their sheath and these should be able to freely move without staccato movements or limitations. • Mild marrow and periosteal oedema was a common finding on MRI. • MRI of athletes with suspected compartment syndrome should be imaged between 60 and 90 min after the stationary ergometer protocol. Funding This study was funded by the Clinical Research Fund through the Australian Institute of Sport Grant ID : C2DREW. Acknowledgments The authors would like to acknowledge and thank Rowing Australia and the Victorian Institute of Sport for allowing access to their athletes. The authors would like to acknowledge the contribution Mark Ward for his assistance with the MRI protocol and obtaining the MRI images. The authors would also like to thank Alice McNamara for her assistance in data collection. Appendix A. Supplementary data Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.jsams.2015.02.002. References 1. Hooper I, Drew MK. 2011 Rowing Australia injury statistics report, Canberra, Australia, Australian Institute of Sport/National Rowing Centre of Excelence, 2011. 2. de Lima JE, Kim H, Albertotti F et al. Intersection syndrome: MR imaging with anatomic comparison of the distal forearm. Skeletal Radiol 2004; 33:627–631. 3. Giovagnorio F, Miozzi F, Springer, editors. Ultrasound findings in intersection syndrome. J Med Ultrasonics 2012; 39(4):217–220. 4. Lee RP, Hatem SF, Recht MP. Extended MRI findings of intersection syndrome. Skeletal Radiol 2009; 38:157–163. 5. De Maeseneer MD, Marcells S, Jager T et al. Spectrum of normal and pathologic findings in the region of the first extensor compartment of the wrist: sonographic findings and correlations with dissections. J Ultrasound Med 2009; 28:779–786. 6. Hoy G, Trease L, Braybon W. Intersection syndrome an acute surgical disease in athletes? 2013 (in preparation). 7. Gielen J, Peersman B, Peersman G et al. Chronic exertional compartment syndrome of the forearm in motocross racers: findings on MRI. Skeletal Radiol 2009; 38(12):1153–1161. 8. Winkes MB, Luiten EJT, van Zoest WJF et al. Long-term results of surgical decompression of chronic exertional compartment syndrome of the forearm in motocross racers. Am J Sports Med 2012; 40(2):452–458. 9. Jawed S, Jawed AS, Padhiar N et al. Chronic exertional compartment syndrome of the forearms secondary to weight training. Rheumatology (Oxford) 2001; 40(3):344–345. 10. Piasecki DP, Meyer D, Bach BRJ. Exertional compartment syndrome of the forearm in an elite flatwater sprint kayaker. Am J Sports Med 2008; 36(11):2222–2225. 11. Dickx N, D’Hooge R, Cagnie B et al. Magnetic resonance imaging and electromyography to measure lumbar back muscle activity. Spine 2010; 35(17): E836–E842. 12. Cagnie B, Elliott J, O’Leary S et al. Muscle functional MRI as an imaging tool to evaluate muscle activity. JOSPT 2011; 41(11):896–903. 13. Cagnie B, Dolphens M, Peeters I et al. Use of muscle functional magnetic resonance imaging to compare cervical flexore activity between patients with whiplash-associated disorders and people who are healthy. Phys Ther 2010; 90(8):1157–1164. 14. van den Brand JGH, Nelson T, Verleisdonk EJMM et al. The diagnostic value of intracompartmental pressure measurement, magnetic resonance imaging, and near-infrared spectroscopy in chronic exertional compartment syndrome. Am J Sport Med 2005; 33(5):699–704. Please cite this article in press as: Drew MK, et al. Normative MRI, ultrasound and muscle functional MRI findings in the forearms of asymptomatic elite rowers. J Sci Med Sport (2015), http://dx.doi.org/10.1016/j.jsams.2015.02.002 G Model JSAMS-1145; No. of Pages 6 6 ARTICLE IN PRESS M.K. Drew et al. / Journal of Science and Medicine in Sport xxx (2015) xxx–xxx 15. Verleisdonk EJMM, van Gils A, van der Werken C. The diagnostic value of MRI scans for the diagnosis of chronic exertional compartment syndrome of the lower leg. Skeletal Radiol 2001; 30(6):321–325. 16. Pattyn E, Verdonk P, Steyaert A et al. Muscle functional MRI to evaluate quadriceps dysfunction in patellofemoral pain. Med Sci Sports Exerc 2013; 45(6):1023–1029. 17. Cagnie B, Dolphens M, Peeters I et al. The use of functional MRI to evaluate cervical flexor activity during different cervical flexion exercises. J Appl Physiol 2008; 104:230–235. 18. Gyftopoulos S, Rosenberg ZS, Petchprapa C. Increased MR signal intensity in the pronator quadratus muscle: does it always indicate anterior interosseous neuropathy? Am J Roentgenol 2010; 194(2):490–493. Please cite this article in press as: Drew MK, et al. Normative MRI, ultrasound and muscle functional MRI findings in the forearms of asymptomatic elite rowers. J Sci Med Sport (2015), http://dx.doi.org/10.1016/j.jsams.2015.02.002