The American Journal of Sports Medicine
advertisement

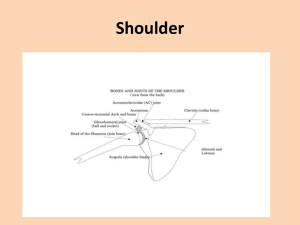
The American Journal of Sports Medicine http://ajs.sagepub.com/ A Prospective Analysis of 179 Type 2 Superior Labrum Anterior and Posterior Repairs: Outcomes and Factors Associated With Success and Failure Matthew T. Provencher, Frank McCormick, Christopher Dewing, Sean McIntire and Daniel Solomon Am J Sports Med 2013 41: 880 originally published online March 4, 2013 DOI: 10.1177/0363546513477363 The online version of this article can be found at: http://ajs.sagepub.com/content/41/4/880 Published by: http://www.sagepublications.com On behalf of: American Orthopaedic Society for Sports Medicine Additional services and information for The American Journal of Sports Medicine can be found at: Email Alerts: http://ajs.sagepub.com/cgi/alerts Subscriptions: http://ajs.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav >> Version of Record - Apr 2, 2013 OnlineFirst Version of Record - Mar 4, 2013 What is This? Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on December 2, 2014 In-Depth A Prospective Analysis of 179 Type 2 Superior Labrum Anterior and Posterior Repairs Outcomes and Factors Associated With Success and Failure CDR Matthew T. Provencher,*y MD, MC USN, LCDR Frank McCormick,z MD, MC USNR, CDR Christopher Dewing,y MD, MC USN, LT Sean McIntire,y MD, MC USN, and CDR Daniel Solomon,§ MD, MC USNR Investigation performed at the Naval Medical Center San Diego, San Diego, California Background: There is a paucity of type 2 superior labrum anterior and posterior (SLAP) surgical outcomes with prospective data. Purpose: To prospectively analyze the clinical outcomes of the arthroscopic treatment of type 2 SLAP tears in a young, active patient population, and to determine factors associated with treatment success and failure. Study Design: Case-control study; Level of evidence, 3. Methods: Over a 4-year period, 225 patients with a type 2 SLAP tear were prospectively enrolled. Two sports/shoulderfellowship-trained orthopaedic surgeons performed repairs with suture anchors and a vertical suture construct. Patients were excluded if they underwent any additional repairs, including rotator cuff repair, labrum repair outside of the SLAP region, biceps tenodesis or tenotomy, or distal clavicle excision. Dependent variables were preoperative and postoperative assessments with the American Shoulder and Elbow Surgeons (ASES), Single Assessment Numeric Evaluation (SANE), and Western Ontario Shoulder Instability (WOSI) scores and independent physical examinations. A failure analysis was conducted to determine factors associated with failure: age, mechanism of injury, preoperative outcome scores, and smoking. Failure was defined as revision surgery, mean ASES score below 70, or an inability to return to sports and work duties, which was assessed statistically with the Student t test and stepwise logarithmic regression. Results: There were 179 of 225 patients who completed the follow-up for the study (80%) at a mean of 40.4 months (range, 26-62 months). The mean preoperative scores (WOSI, 54%; SANE, 50%; ASES, 65) improved postoperatively (WOSI, 82%; SANE, 85%; ASES, 88) (P \ .01). The mean postoperative range of motion was 159° of flexion, 151° of abduction, and 51° of external rotation at the side, which was less than the mean preoperative range of motion (164° of flexion, 166° of abduction, and 56° of external rotation at the side). Of the 179 patients, 66 patients (36.8%) met failure criteria. Fifty patients elected revision surgery. Advanced age within the cohort (.36 years) was the only factor associated with a statistically significant increase in the incidence of failure. Those who were deemed failed had a mean age of 39.2 years (range, 29-45 years) versus those who were deemed healed with a mean age of 29.7 years (range, 18-36 years) (P \ .001). The relative risk for failure for patients older than 36 years was 3.45 (95% CI, 2.0-4.9). Conclusion: Arthroscopic SLAP repair provides a clinical and statistically significant improvement in shoulder outcomes. However, a reliable return to the previous activity level is limited; 37% of patients had failure, with a 28% revision rate. Age greater than 36 years was associated with a higher chance of failure. Additional work is necessary to determine the optimal diagnosis, indications, and surgical management for those with SLAP injuries. Keywords: superior labrum anterior and posterior; biceps tenotomy; biceps tenodesis; arthroscopy; surgical outcomes acceptable treatment.12 There is an increasing incidence of surgically treated SLAP lesions.21 Snyder et al19 subclassified SLAP tears, with type 2 being the most common and amenable to surgical repair. The patient satisfaction after type 2 SLAP repairs ranges primarily from good to excellent,3,5,6,10,13,16,23 but with an unsatisfactory returnto-play percentage.3,10,13,16 Nonoperative treatment may also be effective and yield comparable results.8 Additionally, diagnosis of a SLAP tear at an older age (usually With the development of shoulder arthroscopic surgery and recognition of superior labrum anterior and posterior (SLAP) tears,20 SLAP tears are recognized as a cause of shoulder pain, and operative stabilization is deemed an The American Journal of Sports Medicine, Vol. 41, No. 4 DOI: 10.1177/0363546513477363 Ó 2013 The Author(s) 880 Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on December 2, 2014 Vol. 41, No. 4, 2013 Prospective Analysis of 179 Type 2 SLAP Repairs .50 years) has been associated with increased failures. In this population, biceps tenodesis or tenotomy has been suggested as an alternative to repair.2 However, there is a paucity of surgical outcomes with prospective data analysis2,3,10 with a sample size large enough to identify failure rates or allow subgroup analysis of factors associated with failures. The active-duty military population has a proportionately high number of SLAP injuries14 attributed to the demands of a military occupation, specifically traction injuries while lifting. While this is not a throwing population, the traction injury has been well described as a SLAP injury mechanism, with ensuing pain and disability attributable to the SLAP traction injury.20 In addition, the military population has unique but very codified, highly physical demands of push-ups, pull-ups, lifting activities, and combat readiness that are difficult to omit from daily routine. This repetition may also produce more of a degenerative SLAP-type injury, but these factors remain difficult to quantify.11 To better understand the outcomes of a SLAP tear in a young, active population, we performed a prospective outcome analysis using validated outcome measures and independent physical examinations of patients surgically treated for isolated type 2 SLAP tears.22 Moreover, we sought to identify factors associated with either successes or failures of surgical treatment. Our null hypothesis was that there would be no statistical difference between preoperative and postoperative outcome scores after surgical repair and that independent variables would be predictive of outcome. MATERIALS AND METHODS After institutional review board approval was obtained, between 2005 and 2008, a total of 225 patients were enrolled in a longitudinal prospective cohort study at a tertiary care center under the care of 2 sports/shoulder fellowship-trained surgeons (M.T.P., D.S.). Inclusion criteria included patients aged 18 to 50 years with both a clinical examination and magnetic resonance arthrogram (MRA) evidence for a type 2 superior labral tear who failed nonoperative measures (activity modification and physical therapy). All patients who underwent surgery for a potential SLAP tear had an MRA before surgery. Exclusion criteria were defined as the presence of any other concomitant lesion, including a full-thickness rotator cuff tear, symptomatic acromioclavicular joint arthrosis, or 881 a labral tear requiring a repair outside the SLAP region (10:30-1:30 clock position of the superior labrum). In addition, patients were also excluded if they underwent any additional repairs at the time of surgery, including rotator cuff repair, labrum repair outside of the SLAP region, biceps tenodesis or tenotomy, or distal clavicle procedures (Figure 1). On initial evaluation and presentation to the clinic, the diagnosis of a type 2 SLAP tear was made upon a comprehensive history assessment, physical examination, and MRA confirmation. Patients were offered enrollment into the prospective study once they were thought to meet clinical preoperative criteria; however, they were instructed that the diagnosis of a type 2 SLAP tear would be confirmed intraoperatively to continue with the prospective study enrollment. If at any time the patients were found not to have a type 2 SLAP tear, they were removed from the study. All patients underwent an initial period of nonoperative care including physical therapy (mean, 10.5 weeks; range, 4-24 weeks) and activity modification. Those with failed results were offered surgical intervention for clinical history, examination, and radiographic findings consistent with a type 2 SLAP tear.19 Surgical Technique After consenting for surgical treatment, the patients underwent a comprehensive examination under anesthesia in the lateral decubitus position. A diagnostic arthroscopic procedure was performed using a posterior viewing portal and a midglenoid portal in the midportion of the rotator interval with a 5-mm smooth plastic cannula. A type 2 SLAP lesion was confirmed if there was separation of the bone-labrum junction, with erythema at the SLAP anchor insertion, and a minimum of 5 mm of excursion utilizing the Snyder et al19 criteria for determination of a type 2 SLAP tear. Additional pathological lesions were fully documented in a comprehensive diagnostic glenohumeral arthroscopic procedure with an arthroscope from both posterior and anterior directions. Once an isolated type 2 SLAP tear was confirmed, an 8-mm cannula was then inserted in the midglenoid portal through the rotator interval. An arthroscopic elevator and a 3.5-mm bone-cutting shaver were utilized to prepare the bony glenoid and supraglenoid tubercle for the superior labral repair. Once a bleeding superior glenoid base was confirmed under arthroscopic surgery, the bone preparation was finalized with an arthroscopic rasp. *Address correspondence to CDR Matthew T. Provencher, MD, MC USN, Department of Orthopaedic Surgery, Naval Medical Center San Diego, 34800 Bob Wilson Dr. Ste 112, San Diego, CA 92134 (e-mail: matthew.provencher@med.navy.mil). y Sports Medicine Division, Department of Orthopedic Surgery, Naval Medical Center San Diego, San Diego, California. z Rush Orthopedic Sports Medicine Fellowship Program, Midwest Orthopedics at Rush, Chicago, Illinois. § Marin Orthopedics and Sports Medicine, Novato, California. Presented at the 37th annual meeting of the AOSSM, San Diego, California, July 2011. The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government. One or more of the authors has declared the following potential conflict of interest or source of funding: Dr Provencher is affiliated with the following: AOSSM (board of directors, research), SOMOS (past president), AAOS (publications), BOS (research), ISAKOS (upper extremity), and AANA (program/ education). He also received the following research support: AOSSM Young Investigators grant (2005), AANA research grant (2008, 2006), and OREF grant (2002, 2004, 2011). Moreover, he is involved with the following: Elsevier (deputy editor, Arthroscopy), JSES, JBJS, JAAOS, Slack (orthopedics, JKS), and SAGE (AJSM). Dr Solomon participates in the following: Arthroscopy (editorial board) and AOSSM (board of directors). He has also received honoraria from Arthrex and Pacific Medical for educational presentations within the past 5 years. Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on December 2, 2014 882 Provencher et al The American Journal of Sports Medicine TABLE 1 Respondent Cohort Demographics of 179 Patients Who Completed Follow-upa Demographics Age, mean (range), y Sex, n (%) Male Female Follow-up, mean (range), mo Injury origin, n (%) Traumatic Atraumatic Injury to dominant extremity, n (%) No. of anchors required for repair, mean (range) 31.6 (18-45) 144 (80) 35 (20) 40.4 (26-62) 85 94 101 1.6 (47) (53) (56.4) (1-2) a Consists of more than 80% of the total operative cohort. Figure 1. Flow diagram of patient identification, enrollment criteria, and study completion requirements. AC, acromioclavicular; PRCT, partial rotator cuff tear; RCT, rotator cuff tear. The first anchor was then inserted at the posterior aspect of the SLAP region near the posterior extent of the tear (11-o’clock position). A 3.0-mm anchor (Bio-SutureTak; Arthrex, Naples, Florida) was inserted in a percutaneous fashion through a small 3-mm skin incision just off the lateral edge of the anterior acromion once the correct trajectory was finalized with an 18-gauge spinal needle. With use of a sharp anchor inserter and drill guide, the guide was passed through the muscle-tendon junction of the rotator cuff and then inserted in the 11-o’clock position (right shoulder; 1-o’clock position for a left shoulder) of the glenoid, just at the posterior base of the SLAP attachment. The anchor was placed, and the suture left out through the percutaneous skin incision. From the anterior portal, an arthroscopic labral repair hook was used (Spectrum II; Linvatec, Largo, Florida), just anterior to the biceps tendon and passed around the biceps-labrum junction just posterior to the biceps. A No. 1 polydioxanone (PDS) suture was brought out the cannula and the No. 2 suture from the anchor shuttled for a simple vertical repair stitch. This was the post suture, and the glenoid side suture was retrieved out of the cannula. The sutures were shuttled on the superior aspect of the biceps between the biceps and the capsule and then tied with a sliding-locking knot (modified Roeder) with 3 alternating half-hitches. In cases with a labral injury and clear superior labral tear that extended anteriorly to the 1o’clock position (n = 49), 1 additional anchor was placed anterior to the biceps-labrum junction in a similar fashion. In patients with subacromial symptoms (n = 22), a bursal debridement was performed with the arthroscope in the posterior portal and a combination of shaver and radiofrequency wand placed from the lateral portal. Only anterior osteophytes of the anterior acromion were removed and only performed in a minority of cases (n = 4); in the remainder (n = 18), a subacromial debridement was performed with a complete anterior and anterolateral bursectomy. All patients underwent the identical printed rehabilitation protocol with supervised physical therapy. Patients used a sling for a total of 4 weeks with scapular mobility and gentle passive range of motion, followed by progressive full range of motion that started at 4 to 6 weeks postoperatively. Scapular exercises were started by 1 week, and rotator cuff strengthening was instituted between 4 to 6 weeks postoperatively. At 3 months, patients were allowed to return to light (nonthrowing/nonlifting) sports and a work-specific strengthening regimen, with resumption of full activities between 4 to 5 months. At 5 months, overhead lifting and sporting activities were allowed. Surgical Outcomes Patients were evaluated in the clinic preoperatively and postoperatively with a comprehensive history evaluation, independent physical examination, and assessment with a battery of outcome scores that included the American Shoulder and Elbow Surgeons (ASES), Single Assessment Numeric Evaluation (SANE),7 and Western Ontario Shoulder Instability (WOSI) scores.17 The physical examination was performed by an unblinded independent examiner and consisted of evaluation of a full range of motion in the supine position with a goniometer, including flexion, abduction, abduction external rotation (ABER), and abduction internal rotation (ABIR). The examiners were not associated with the study, were aware of the procedure but not patient details, and serially evaluated the patients until final follow-up. Subgroup Failure Analysis A subgroup analysis was performed to identify factors associated with surgical failure. Surgical failure was defined as revision surgery or an ASES score of less than 70. In addition, patients were also evaluated to see if Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on December 2, 2014 Vol. 41, No. 4, 2013 Prospective Analysis of 179 Type 2 SLAP Repairs 883 TABLE 2 Preoperative and Postoperative Outcome Scores and ROMa Preoperative, Mean 6 SD Outcome score ASES 64.3 6 4.1 WOSI 980/2100b 6 32.1 SANE 50 6 5.4 ROM, deg Flexion 164 6 7.2 Abduction 166 6 8.1 ER at side 56 6 3.9 ABER 86 6 6.6 ABIR 77 6 8.1 Postoperative, Mean 6 SD P Value 88.2 6 5.3 380/2100c 6 26.4 85 6 6.1 .01d .01d .001d 159 151 51 83 60 6 6 6 6 6 5.5 6.1 4.1 5.9 8.4 .042d .039d .38 .44 .29 a There was a statistically significant improvement across each patient-reported outcome measure. However, there was a statistically significant mean decrease in range of motion in forward flexion and abduction. ROM, range of motion; ASES, American Shoulder and Elbow Surgeons; WOSI, Western Ontario Shoulder Instability; SANE, Single Assessment Numeric Evaluation; ER, external rotation; ABER, abduction external rotation; ABIR, abduction internal rotation. b Converts to 54% of normal. c Converts to 82% of normal. d Statistical significance at P \ .05. Figure 2. At a mean follow-up of 40.4 months (range, 26-62 months) after primary surgery of the 179-patient cohort, there was a statistically significant improvement in overall outcome parameters (P \ .01). The mean preoperative scores (WOSI, 54% 6 32.1%; SANE, 50% 6 5.4%; ASES, 65 6 4.1) improved postoperatively (WOSI, 82% 6 26.4%; SANE, 85% 6 6.1%; ASES, 88 6 5.3). *Statistically significant improvement (P \ .01). ASES, American Shoulder and Elbow Surgeons; SANE, Single Assessment Numeric Evaluation; WOSI, Western Ontario Shoulder Instability. they could return to full military duty as well as their desired sport. Variables that were assessed to be potential predictors of surgical failure were tear origin (traumatic, or a defined day of injury, vs atraumatic), smoker or nonsmoker, preoperative outcome scores, and age. Because all of the patients treated for type 2 SLAP tears and enrolled in the study had to perform overhead-lifting tasks as part of their military duties, overhead athlete subcategorization was not included as a subgroup analysis. Statistical Analysis Statistical analysis included a stepwise linear regression on the aforementioned preoperative variables to determine overall success or failure. In addition, preoperative and postoperative outcome scores and shoulder ranges of motion were compared utilizing Student t tests, with a statistical significance set at P \ .05 utilizing XLSTAT-Pro software package (Addinsoft, New York, New York). We performed a prestudy power analysis based upon finding a difference in a preoperative versus postoperative ASES score of 20 points comparing failure versus success, with a standard deviation of 7.4, which identified that a total of 44 patients needed to be enrolled in the study.4 Figure 3. The mean postoperative range of motion, assessed by an independent observer, was 159° 6 5.5° of flexion (Flex), 151° 6 6.1° of abduction (Abd), and 51° 6 4.1° of external rotation (ER) at the side, which was less than the mean preoperative range of motion. *Statistically significant improvement (P \ .01). ABER, abduction external rotation; ABIR, abduction internal rotation. were 144 men and 35 women, with a mean age of 31.6 years (range, 18-45 years). Approximately half (n = 85, 47.4%) described a traumatic event to their shoulder, of which almost all (97%) were traction injuries due to lifting heavy objects. The remainder (n = 94, 52.6%) could not identify an isolated event for their shoulder injury. There were 101 (56.4%) with the dominant extremity injured, and 130 were right-hand dominant. A mean of 1.6 anchors were utilized for repair (range, 1-2) of the type 2 SLAP injuries (Table 1). RESULTS Demographics Surgical Outcomes At a mean follow-up of 40.4 months (range, 26-62 months), a total of 179 of 225 patients completed the study (mean follow-up of 80%) (Figure 1). Of the 179 patients, there There was a statistically significant improvement in overall outcome parameters and range of motion (P \ .01) (Table 2 and Figures 2 and 3). Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on December 2, 2014 884 Provencher et al The American Journal of Sports Medicine TABLE 3 Stepwise Logistical Regression Results of Independent Factors Associated With Likelihood for Failure Age .36 y at time of surgery Smoking Traumatic origin Relative Risk for Failure (95% CI) P Value 3.45 (2.0-4.9) 1.10 (0.45-1.75) 1.25 (0.42-1.98) .012a .422 .355 a Statistical significance at P \ .05. TABLE 4 Characteristics of Success and Failure Subgroupsa Age, y ASES WOSI SANE Failed Cases, Mean 6 SD Successful Cases, Mean 6 SD P Value 39.2 83.0 6 8.9 672/2100b 6 39 74 6 6.1 27.9 93.4 6 9.2 105/2100c 6 9 96 6 7.4 .01d .021d .01d .001d a Figure 4. Flow diagram of surgical outcome analysis. A total of 66 patients (66/179, 36.8%) met the failure criteria, and 28% underwent revision surgery, with biceps tenodesis being the most common revision procedure. ASES, American Shoulder and Elbow Surgeons. Subgroup Analysis of Surgical Failures A total of 66 patients (66/179, 36.8%) were deemed to have failures based on the aforementioned criteria (Figure 4). In those with failures (n = 66), the mean time to failure was 11.8 months (range, 6-22 months), and mean postoperative outcome scores of those with failures were much less than those with successful outcomes. All patients with failures had ASES outcome scores of less than 70 and a significantly diminished range of motion versus those who were deemed a success. A total of 16 of 66 patients were medically separated from the military, and the remaining 50 patients underwent revision shoulder surgery at a mean time of 12.9 months (range, 8-26 months) after the index procedure. Those with failed results had a mean age of 39.2 years (range, 29-45 years) versus those who were deemed healed with a mean age of 29.7 years (range, 18-36 years) (P \ .001). The group that underwent revision surgery (n = 44) had a biceps tenodesis (n = 42), tenotomy (n = 4), or intra-articular debridement (n = 4). Twenty of these patients also had subacromial debridement (no bony excision was performed). The only factor associated with failure on regression analysis was age (age .36 years; P \ .01) (Table 3). The relative risk for failure for patients older than 36 years was 3.45 (95% confidence interval, 2.0-4.9). A total of 51 patients (51/66, 77%) with failures were over the age of 36 years, and 15 patients (15/66, 23%) were under the age of 36 years. The remainder of the variables in the logistical regression were When the cohort is separated into success and failure subgroups, the above characteristics of each group demonstrate a bimodal distribution, which is clinically and statistically significant between the 2 groups. ASES, American Shoulder and Elbow Surgeons; WOSI, Western Ontario Shoulder Instability; SANE, Single Assessment Numeric Evaluation. b Converts to 68% of normal. c Converts to 95% of normal. d Statistical significance at P \ .05. not associated with either success or failure, and origin of injury (traumatic vs atraumatic), smoking history, and individual preoperative scores were not associated with success or failure (P . .55 for all variables). Outcome scores between successes and failures are listed in Table 4. DISCUSSION In this study, we sought to prospectively determine the shortterm and midterm clinical results in a large, young, and active population with isolated type 2 SLAP tears. The principal findings of our study demonstrate that type 2 SLAP tear repairs have a clinical and statistically significant improvement using validated outcome scores. Thus, we reject our null hypothesis. However, there is a large group (38%) of patients who did not fare well after the surgery, with many in the original primary repair cohort who met failure criteria and eventually had revision surgery (28% of the cohort). The overall outcome scores were improved across all variables, demonstrating that the type 2 SLAP repair does work, likely in the correctly selected patient. Our data demonstrate a statistical and clinical improvement across all validated outcome measures with moderate/ high correlation between outcome scores. This is in accordance with previously published short-term surgical results in athletes and active patients for isolated SLAP lesions: Friel et al10 reported good to excellent results in Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on December 2, 2014 Vol. 41, No. 4, 2013 Prospective Analysis of 179 Type 2 SLAP Repairs 79% of 48 patients, with 89% patient satisfaction and an 8% reoperation rate; Cohen et al5 reported 69% good to excellent results in 39 patients, with 71% patient satisfaction; Ide et al13 investigated overhead athletes and demonstrated 90% good to excellent outcome scores; Enad et al9 showed 88% good to excellent outcome scores; and Yung et al23 reported on 12 young patients with good results. However, our patients demonstrated an unexpectedly high failure rate of 38%, with 28% of patients requiring revision. As previously mentioned, our cohort has a high athletic activity requirement to remain on active duty. Our data are not dissimilar to those of other authors who have published difficulty with returning patients to their previous level of activity after SLAP repair, especially with overhead athletes. Of 2 prospective studies, Friel et al10 reported that 62% of patients returned to play, 59% of overhead athletes, comparable with Brockmeier et al,3 who described that 74% returned to play, with 71% returning to play as overhead athletes. A previous retrospective analysis by Ide et al13 showed that 75% returned to play as overhead athletes; Kim et al16 showed that 63% returned to play but only 20% returned to play as overhead athletes. Our findings are in contrast to those of Enad et al,9 who demonstrated that 90% returned to active military duty. Our failure rate is likely a comparable measure of return-to-play rates. Boileau et al2 suggested that biceps tenodesis is superior to the repair of type 2 SLAP tears, especially in the older, overhead-throwing athletic population. In a prospective randomized study of 20 older overhead athletes, all patients improved, with an equivocal outcome score between the 2 groups; 87% returned to play after tenodesis, whereas only 20% returned to play after repair. Our study results are in agreement. Based on our subgroup analysis, those failing surgery were significantly older than those with good outcomes. Although the terminal end point we defined as ‘‘failure’’ may be debatable, it was decided to use rigorous, yet realistic patient-derived criteria to provide meaningful information regarding SLAP treatment. The age at which we found one’s risk for failure with type 2 SLAP repair is over 36 years. This is in contrast to the findings of Alpert el al,1 who concluded that age was not a predictor of surgical failure using outcome measurements based on a retrospective analysis of 52 patients divided into 2 groups (age \40 years and .40 years). However, this study was likely underpowered to find a difference, and it demonstrated a trend toward worse outcomes in those over 40 years. Thus, in older athletes with type 2 SLAP tears, the surgeon should discuss the risks of type 2 SLAP repair versus biceps tenodesis at the initial surgery.15 Yet, with a young patient, our study demonstrates a clear benefit to arthroscopically repairing the SLAP tear. The young cohort had excellent outcomes and a desirable and reasonable return-to-duty percentage. The younger group (\36 years) had higher outcome scores and higher level of function throughout versus those who were over the age of 36 years. There may be some protective function of the biceps, especially as it relates to overhead activity and a secondary shoulder stabilizer.18 Thus, given our excellent outcome scores in the younger subgroup, it may be wise to repair the biceps lesion while leaving tenodesis as an option for revision. 885 The major strength of our study is its methodology. We performed a prospective study with 80% follow-up at a mean follow-up of 3.5 years and assessed patients with multiple validated outcome measurements and an independent physical examination. Moreover, strict inclusion and exclusion criteria were used, notably excluding concomitant pathological abnormalities. Finally, with our large cohort, we were able to perform subgroup analysis and identify factors associated with failures supported by clinically meaningful statistical findings. Our study of only an active military population creates some external validity concerns that our results may not be generalizable to other patient cohorts. However, this study does encompass a working and lifting population with documented isolated SLAP lesions and is certainly generalizable to some degree. Despite a limited overheadthrowing population, all patients are required to meet minimum standards of fitness, including push-ups and pull-ups, and suitability for combat operations. The need for all military members to meet this minimum may be reflected in our high failure rate despite a mean improvement in the shoulder outcome measurements. In addition, our failure definition parallels the return to athletic activity rate previously published in the literature. Another concern is that all surgical repairs were performed by 2 surgeons who used an identical repair technique. Repair security may have been an issue with 1.6 anchors used per case and a simple suture pattern. Also, as a response to the high failure rate and the resultant diminished range of motion in those failures, our rehabilitation protocols have since been modified. We now are more aggressive in regaining range of motion. There is also an element of selection bias by those who chose to enroll in the study. Finally, there is a potential for response bias from the 20% of patients who did not complete the study and were not available for final evaluation. CONCLUSION Arthroscopic SLAP repair provides a clinical and statistically significant improvement in shoulder outcomes. However, a reliable return to the previous activity level is limited, and within this population, 37% of patients failed, with a 28% revision rate. Age greater than 36 years was associated with a higher chance of failure. Additional work is necessary to determine the optimal diagnosis, indications, and surgical management for those with SLAP injuries. Scan the QR code with your smartphone to view the InDepth podcast associated with this article or visit http:// ajsm.sagepub.com/site//misc/Index/Podcasts.xhtml. REFERENCES 1. Alpert JM, Wuerz TH, O’Donnell TF, Carroll KM, Brucker NN, Gill TJ. The effect of age on the outcomes of arthroscopic repair of type II superior labral anterior and posterior lesions. Am J Sports Med. 2010;38(11):2299-2303. Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on December 2, 2014 886 Provencher et al The American Journal of Sports Medicine 2. Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, Bicknell R. Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37(5):929-936. 3. Brockmeier SF, Voos JE, Williams RJ 3rd, Altchek DW, Cordasco FA, Allen AA. Outcomes after arthroscopic repair of type-II SLAP lesions. J Bone Joint Surg Am. 2009;91(7):1595-1603. 4. Buford D Jr, Mologne T, McGrath S, Heinen G, Snyder S. Midterm results of arthroscopic co-planing of the acromioclavicular joint. J Shoulder Elbow Surg. 2000;9(6):498-501. 5. Cohen DB, Coleman S, Drakos MC, et al. Outcomes of isolated type II SLAP lesions treated with arthroscopic fixation using a bioabsorbable tack. Arthroscopy. 2006;22(2):136-142. 6. Coleman SH, Cohen DB, Drakos MC, et al. Arthroscopic repair of type II superior labral anterior posterior lesions with and without acromioplasty: a clinical analysis of 50 patients. Am J Sports Med. 2007;35(5):749-753. 7. DeBerardino TM, Arciero RA, Taylor DC, Uhorchak JM. Prospective evaluation of arthroscopic stabilization of acute, initial anterior shoulder dislocations in young athletes: two- to five-year follow-up. Am J Sports Med. 2001;29(5):586-592. 8. Edwards SL, Lee JA, Bell JE, et al. Nonoperative treatment of superior labrum anterior posterior tears: improvements in pain, function, and quality of life. Am J Sports Med. 2010;38(7):1456-1461. 9. Enad JG, Gaines RJ, White SM, Kurtz CA. Arthroscopic superior labrum anterior-posterior repair in military patients. J Shoulder Elbow Surg. 2007;16(3):300-305. 10. Friel NA, Karas V, Slabaugh MA, Cole BJ. Outcomes of type II superior labrum, anterior to posterior (SLAP) repair: prospective evaluation at a minimum two-year follow-up. J Shoulder Elbow Surg. 2010;19(6):859-867. 11. Gobezie R, Zurakowski D, Lavery K, Millett PJ, Cole BJ, Warner JJ. Analysis of interobserver and intraobserver variability in the diagnosis 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. and treatment of SLAP tears using the Snyder classification. Am J Sports Med. 2008;36(7):1373-1379. Gorantla K, Gill C, Wright RW. The outcome of type II SLAP repair: a systematic review. Arthroscopy. 2010;26(4):537-545. Ide J, Maeda S, Takagi K. Sports activity after arthroscopic superior labral repair using suture anchors in overhead-throwing athletes. Am J Sports Med. 2005;33(4):507-514. Kampa RJ, Clasper J. Incidence of SLAP lesions in a military population. J R Army Med Corps. 2005;151(3):171-175. Katz LM, Hsu S, Miller SL, et al. Poor outcomes after SLAP repair: descriptive analysis and prognosis. Arthroscopy. 2009;25(8):849-855. Kim SH, Ha KI, Kim SH, Choi HJ. Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg Am. 2002;84(6):981-985. Kirkley A, Griffin S, McLintock H, Ng L. The development and evaluation of a disease-specific quality of life measurement tool for shoulder instability: the Western Ontario Shoulder Instability Index (WOSI). Am J Sports Med. 1998;26(6):764-772. Rodosky MW, Harner CD, Fu FH. The role of the long head of the biceps muscle and superior glenoid labrum in anterior stability of the shoulder. Am J Sports Med. 1994;22(1):121-130. Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4(4):243-248. Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy. 1990;6(4):274-279. Weber SC, Martin DF, Seiler JG 3rd, Harrast JJ. Superior labrum anterior and posterior lesions of the shoulder: incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery. Part II candidates. Am J Sports Med. 2012;40(7):1538-1543. Wright RW, Baumgarten KM. Shoulder outcomes measures. J Am Acad Orthop Surg. 2010;18(7):436-444. Yung PS, Fong DT, Kong MF, et al. Arthroscopic repair of isolated type II superior labrum anterior-posterior lesion. Knee Surg Sports Traumatol Arthrosc. 2008;16(12):1151-1157. For reprints and permission queries, please visit SAGE’s Web site at http://www.sagepub.com/journalsPermissions.nav Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on December 2, 2014