The American Journal of Sports Medicine
advertisement

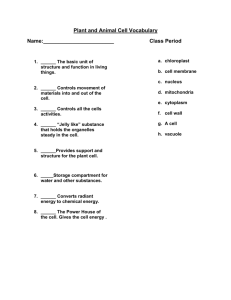
The American Journal of Sports Medicine http://ajs.sagepub.com/ Intramuscular Pressure Before and After Botulinum Toxin in Chronic Exertional Compartment Syndrome of the Leg: A Preliminary Study Marie-Eve Isner-Horobeti, Stéphane Pascal Dufour, Cyril Blaes and Jehan Lecocq Am J Sports Med 2013 41: 2558 originally published online August 22, 2013 DOI: 10.1177/0363546513499183 The online version of this article can be found at: http://ajs.sagepub.com/content/41/11/2558 Published by: http://www.sagepublications.com On behalf of: American Orthopaedic Society for Sports Medicine Additional services and information for The American Journal of Sports Medicine can be found at: Email Alerts: http://ajs.sagepub.com/cgi/alerts Subscriptions: http://ajs.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav >> Version of Record - Nov 1, 2013 OnlineFirst Version of Record - Aug 22, 2013 What is This? Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on November 11, 2013 Intramuscular Pressure Before and After Botulinum Toxin in Chronic Exertional Compartment Syndrome of the Leg A Preliminary Study Marie-Eve Isner-Horobeti,*yz§ MD, PhD, Stéphane Pascal Dufour,§ll PhD, Cyril Blaes,y MD, and Jehan Lecocq,z§ MD Investigation performed at Strasbourg University, Department of Physical Medicine and Rehabilitation, Strasbourg, France Background: Botulinum toxin A (BoNT-A) is used in the treatment of muscle hypertrophy but has never been used in chronic exertional compartment syndrome (CECS). The objective diagnostic criterion in this condition is an abnormally elevated intramuscular pressure (IMP) in the compartment. In this study, the IMP was measured 1 minute (P1) and 5 minutes (P5) after the exercise was stopped before and after BoNT-A injection. Hypothesis: Botulinum toxin A reduces the IMP (P1 and P5) and eliminates the pain associated with CECS. Study Design: Case series; Level of evidence, 4. Methods: Botulinum toxin A was injected into the muscles of moderately trained patients with an anterior or anterolateral exertional compartment syndrome of the leg. The BoNT-A dose (mean 6 SD) ranged from 76 6 7 to 108 6 10 U per muscle, depending on which of the 5 muscles in the 2 compartments were injected. The primary end point was IMP (P1, P5). Secondary end points were exertional pain, muscle strength, and safety. Follow-up was conducted up to 9 months. Results: A total of 25 anterior compartments and 17 lateral compartments were injected in 16 patients. The time interval (mean 6 SD) between the BoNT-A injection and after BoNT-A injection IMP measurement was 4.4 6 1.6 months (range, 3-9 months). In the anterior compartment, P1 and P5 fell by 63% 6 17% (P \ .00001) and 59% 6 24% (P \ .0001), respectively; in the lateral compartment, P1 and P5 fell by 68% 6 21% (P \ .001) and 63% 6 21% (P \ .01), respectively. Exertional pain and muscle strength were monitored, based on the Medical Research Council score. The exertional pain was completely eliminated in 15 patients (94%). In 5 patients (31%), the strength of the injected muscles remained normal. In 11 patients (69%), strength decreased from 4.5 (out of 5) to 3.5 (P \ .01), although without functional consequences. In the conditions of this study, BoNT-A showed a good safety profile in patients with CECS. Conclusion: In this case series, BoNT-A reduced the IMP and eliminated exertional pain in anterior or anterolateral CECS of the leg for up to 9 months after the intervention. The mode of action of BoNT-A is still unclear. A randomized controlled study should be carried out to determine whether BoNT-A can be used as a medical alternative to surgical treatment. Keywords: exertional compartment syndrome; botulinum toxin; leg pain; intramuscular pressure objective diagnostic criterion: an abnormally high intramuscular pressure (IMP) after exercise within the affected compartment.50,55 The pathophysiological process of CECS is poorly understood and probably multifactorial. One of the hypotheses is a discrepancy between the tissue delimiting the compartment and its muscle content, resulting in an excessive IMP. This discrepancy may be due to a hypertrophy of the muscles within the compartment.28,47 However, other plausible pathophysiological mechanisms are also suggested for CECS, including a decreased compartment syndrome size due to a thickened, unelastic fascia,4,31 a supernumerary muscle, or a vascular anatomic or functional abnormality.13,14 The pain could be explained by A muscle compartment is a closed space bound by fascia and bone. The leg includes 4 compartments: the anterior compartment, the lateral compartment, the superficial posterior compartment, and the deep posterior compartment. Chronic exertional compartment syndrome (CECS) is characterized by 2 criteria. The first one is a subjective clinical criterion: pain in the involved compartment triggered by a specific exercise and disappearing when the exercise is stopped. The second one is a paraclinical criterion and the only The American Journal of Sports Medicine, Vol. 41, No. 11 DOI: 10.1177/0363546513499183 Ó 2013 The Author(s) 2558 Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on November 11, 2013 Vol. 41, No. 11, 2013 Compartment Syndrome and Botulinum Toxin muscle ischemia33 or by the stimulation of nociceptors located in the muscles as well as in the fascia. The only curative treatment available for CECS, and considered the gold standard, is a surgical fasciotomy or fasciectomy12,23 to release the tension on the compartment’s boundary. However, the postoperative recurrence rate varies from around 3% to 17% and may reach 35% in partial fasciectomy.19,37,48,56 Therefore, a less invasive alternative may be of interest. Given the proposed role of muscle hypertrophy within the compartment, botulinum toxin A (BoNT-A) could help in the management of CECS by reducing the volume of the compartment content. BoNT-A showed favorable and promising results in the treatment of masseter hypertrophy1,25 and gastrocnemius hypertrophy.21,29 Likewise, its use for analgesic purposes in painful hypertrophy of the calf muscles8 and painful muscle contractures associated with myofascial syndromes has been described.49 The similarity between the symptoms of these conditions led us to examine the effects of BoNT-A in CECS. Although any muscle compartment can be affected, CECS most commonly involves the anterior and lateral compartments of the leg. These 2 compartments are subcutaneous and are more readily accessible and safe for exploration. Consequently, our study focused on CECS involving the anterior and anterolateral compartments of the leg. A first case series conducted in 2008 in 7 patients with anterior or anterolateral CECS of the leg showed that BoNT-A injections helped reduce muscle pain in the affected compartments.27 However, the effects of BoNT-A on IMP have never been investigated in CECS. Therefore, we hypothesized that intramuscular injections of BoNT-A may reduce IMP and relieve pain. Our objective was to test the effect of BoNT-A injection on the only objective criteria able to confirm the diagnosis of CECS, that is, the IMP and associated pain. MATERIALS AND METHODS Population Clinical files from a population of patients seen between January 2010 and June 2012 at a physical and rehabilitation medicine department were retrospectively analyzed. During this period, 148 patients were seen in consultation for leg pain. We retained complete clinical and paraclinical data in patients’ files according to 3 criteria. First, CECS had to be suggested clinically in the anterior or anterolateral compartment by the presence of leg pain, triggered by physical or sport activity, irrespective of the patients’ age or sex. Second, patients had to be injected by BoNT-A in the involved compartment. These patients had to be BoNT-A naı̈ve and to have given their written 2559 TABLE 1 Population Characteristics (N = 16)a Age, y Sex, male/female, No. Height, cm Weight, kg Body mass index, kg/m2 Time to diagnosis, mo Anterior compartment Anterolateral compartment Unilateral involvement Bilateral involvement 23 6 5 (18-36) 13/3 173 6 8 (156-185) 77 6 14 (48-105) 25 6 3 (20-31) 40 6 60 (4-240) 31% (n = 5) 69% (n = 11) 37% (n = 6) 63% (n = 10) a Data given as mean 6 standard deviation (range) unless otherwise noted. consent to receive the proposed intramuscular injection. The third criterion was the assessment of IMP before and after BoNT-A injection. In these patients, the CECS could be unilateral or bilateral. The definitive diagnosis was based on an elevated IMP measured in the involved compartments after running, based on the criteria suggested by Pedowitz et al38: IMP at the first minute after exercise (P1) greater than 30 mm Hg and/or IMP at the fifth minute (P5) greater than 20 mm Hg. Other exertional leg pain causes were ruled out by a clinical examination (general, orthopaedic, neurological, and functional) and paraclinical examination (full blood examination, leg radiographs, bone scintigraphy, lumbar scan, and dynamic echo-Doppler of the lower limbs). Those with abnormal findings in the abovementioned examinations (periostitis, stress fracture, herniated disk, vascular compression) were excluded from the analysis. Using these inclusion criteria, we identified 16 patients, consisting of 11 recreational runners and 5 military runners. These runners had all been running regularly for more than 1 year and had a training volume of at least 5 hours per week. Patients had undergone treatment (eg, rest, stretching, ice, nonsteroidal anti-inflammatory drugs, analgesics) that proved unsuccessful for their persistent muscle leg pain and forced them to reduce or stop their usual physical activity. All members of this group were examined by the same physician. The following data were collected: age, sex, weight, height, body mass index, and time to diagnosis (Table 1). Evaluation and Follow-up Clinical data and IMP were obtained just after the initial running test and before BoNT-A injection. After BoNT-A injection, IMP measurement was assessed only once after ~4.4 6 1.6 months (range, 3-9 *Address correspondence to Marie-Eve Isner-Horobeti, MD, PhD, Institut Universitaire de Réadaptation Clémenceau (IURC)–Strasbourg, 45 boulevard Clémenceau, F-67000 Strasbourg, France (e-mail: marieeve.isner@gmail.com). y Physical and Rehabilitation Medicine Department, Strasbourg University, University Institute of Rehabilitation Clémenceau, Strasbourg, France. z Physiology Institute, Strasbourg University, Medicine Faculty and Hospital, University Hospital, Strasbourg, France. § Fédération de Médecine Translationnelle de Strasbourg (FMTS), Strasbourg University, Strasbourg, France. ll Faculty of Sports Science, Strasbourg University, Strasbourg, France. The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on November 11, 2013 2560 Isner-Horobeti et al Duration of symptoms preinjection: 40±60 mo The American Journal of Sports Medicine 1-month recovery 3- to 9-month recovery: 4.4±1.6 mo Time Running test IMP at 1 and 5 min after running test BoNT-A injection Clinical data Figure 1. Study design: All patients had chronic exertional compartment syndrome (CECS) for a mean (6SD) duration of 40 6 60 months before the first visit to the medical department. During this time, all other exertional leg pain causes were discarded. At the first visit, all patients were asked to run on a treadmill to demonstrate the effects of the usual pain in their lower leg muscles. Intramuscular pressure (IMP) was measured 1 and 5 minutes after running to confirm CECS, and lower leg muscle strength and pain were evaluated. The intramuscular botulinum toxin A (BoNT-A) injection was given 15 minutes after the running test. Patients returned to the department after 1 month of recovery from the BoNT-A injection for evaluation of lower leg muscle strength, pain, and side effects. All patients had their last visit between 3 and 9 months after BoNT-A injection; at this visit, the running test was repeated, IMP was measured, and lower leg muscle strength, pain, and side effects were evaluated. months). For clinical data (ie, exertional pain, muscle strength, and safety), a first evaluation was performed 1 month after the injection of BoNT-A and a second evaluation was performed when the IMP was assessed at ~4.4 6 1.6 months (range, 3-9 months) (Figure 1). Running Test To trigger their usual leg pain, all patients performed a treadmill running test (Medical Development S2500, Andrezieux Boutheon, France) before and 4.4 6 1.6 months after BoNT-A injection. The running speed was increased progressively until the patient complained of leg pain. The exercise was then stopped and the patient was placed lying supine for immediate IMP measurements. The running protocol after BoNT-A injection was identical to the protocol used before the injection. Thus, each patient was asked to run at the same speed and for the same duration in both tests. Special Procedures and Measurements IMP in the Lower Leg Compartments. Before the exercise test, local skin anesthesia was given (1.5 mL, 1% xylocaine) at the point where the IMP needle would be inserted. The needle, connected to a pressure transducer (Stryker Instruments, Mahwah, New Jersey), was inserted immediately into the anterior or lateral compartment.22 The pressures in the compartment and in the transducer were evened out by use of a syringe filled with 0.2 mL of Figure 2. Intramuscular injection of botulinum toxin in the tibialis anterior muscle under electrical stimulation guidance. saline solution. The pressure was displayed on the transducer in mm Hg and was read about 10 seconds after saline injection, as previously described in clinical settings.10,45 The IMP was measured continuously, but we recorded only the values at 1 minute (P1) and 5 minutes (P5) after the exercise. After BoNT-A injection, the IMP was measured in the same conditions and with the same procedures as used for the initial measurements. Clinical Data. Clinical data (ie, exertional pain, muscle strength, and safety) were obtained before as well as 1 month and 4.4 6 1.6 months (range, 3-9 months) after the injection of BoNT-A. Exertional Pain. Pain was assessed as binary data (ie, present or absent) irrespective of its intensity, and therefore a quantified visual analog scale was not necessary. The analgesic effect of BoNT-A was thus considered as positive only if the pain had disappeared after the injection of BoNT-A. Muscle Strength. Muscular strength was assessed with the semiquantitative Medical Research Council score32 (0 to 5). To aid statistical calculations, intermediate values typically represented with the plus (1) symbol were replaced by the decimal 0.5. The duration of muscular strength loss was quantified in months. The functional consequences of any muscle impairment were evaluated during the interview as a feeling of ankle instability when walking or running, as well as the ability to walk on heels. Safety. The potential side effects of BoNT-A (general muscle weakness, muscular atrophy,3,17,18,30 flulike symptoms,34 breathing and swallowing difficulties, and death9,26) were exhaustively explained to study participants before they gave their written consent to receive the proposed intramuscular injection. After the injection, all patients were given the option to call the examiners at any time during the follow-up for any concerns, including occurrence of a potential side effect. Intramuscular Injection of BoNT-A. At 15 minutes after the initial running test, the BoNT-A injection was performed under electrical stimulation guidance, which was used to position the needle as close as possible to the motor endplate35 of all the muscles in the involved compartment Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on November 11, 2013 Vol. 41, No. 11, 2013 Compartment Syndrome and Botulinum Toxin 2561 TABLE 2 Doses of BoNT-A per Compartment and per Musclea Anterior Compartment Tibialis Anterior Extensor Digitorum Longus Extensor Hallucis Longus Lateral Compartment Peroneus Brevis Peroneus Longus 16 288 6 25 (230-330) 3.8 6 0.6 (3.0-5.2) 16 108 6 10 (90-120) 1.4 6 0.3 (0.3-1.9) 16 103 6 13 (70-120) 1.4 6 0.3 (0.3-1.9) 16 76 6 10 (50-100) 1.0 6 0.2 (0.7-1.5) 12 180 6 14 (150-200) 2.4 6 0.4 (1.9-3.0) 12 76 6 7 (70-90) 1.0 6 0.1 (0.7-1.3) 12 104 6 10 (80-120) 1.4 6 0.2 (0.7-1.3) No. BoNT-A, U BoNT-A, U/kg a Data are given as mean 6 standard deviation (range). There was 1 injection site per muscle. BoNT-A, botulinum toxin A; No., number of compartments or muscles. TABLE 3 Intramuscular Injection of Botulinum Toxin A in 42 Compartments Anterior Compartment Patient No. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Lateral Compartment Right Left Right Left X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X and to avoid injecting a muscle more than once (Figure 2). To identify the injection site, a needle electrode 0.46 mm in diameter and 50 mm long (Bioject, Alpine Biomed Aps, Skovlunde, Denmark) was connected to a muscle electrical stimulation device (Cefar Rehab, Mouguerre, France) to detect the point that produced a maximum contraction with the minimum stimulation intensity for each muscle in the compartment. In patients with an anterior CECS, BoNT-A was injected into each of the 3 muscles in the anterior compartment (tibialis anterior, extensor hallucis longus, extensor digitorum longus). In patients with an anterolateral CECS, BoNT-A was injected into the 3 muscles mentioned above and into the 2 muscles of the lateral compartment (peroneus brevis and peroneus longus). The BoNT-A (Dysport, Ipsen, Boulogne-Billancourt, France) was reconstituted with 2.5 mL of saline solution for 500 U. Because of the lack of previous studies, the selection of the dose of BoNT-A was based on the literature and on the authors’ experience and knowledge of spasticity7,40 and musculoskeletal disorders.41,49,54 The objective was to use the minimum effective dose that would not lead to muscle paralysis. This dose was one-third of the maximum recommended dose used for the treatment of lower limb spasticity,7,40 adjusted to the volume of the muscle and the patient’s body weight. BoNT-A was injected into each muscle in a single injection site. The doses of BoNT-A administered in each muscle (measured in units) as well as the dose per muscle based on the patient’s body weight (units per kilogram) were recorded. The total dose of BoNT-A injected into each compartment was also recorded in units and units per kilogram (Table 2). Statistical Analysis To specifically test the effects of BoNT-A injection on the anterior or anterolateral compartments, IMP values were assessed per muscle compartment. For clinical data (ie, pain and muscle strength), the statistical analysis was performed per patient. The Student t test was used to compare the parameters before and after BoNT-A. The results were expressed in terms of mean, standard deviation, and range. The significance level was P \ .05. Correlation tests were based on the Pearson correlation coefficient. RESULTS Effect of BoNT-A Injection on Intramuscular Pressure The IMP was measured before and after the intramuscular injection of BoNT-A in 42 compartments (25 anterior and 17 anterolateral compartments in 16 patients). Of note, some patients presented mono/bilateral and/or anterior/ anterolateral CECS (Tables 1 and 3). The mean interval between BoNT-A injection and postinjection IMP measurement was 4.4 6 1.6 months (range, 3-9 months). After the BoNT-A injection, in the anterior compartment, P1 and P5 decreased by 63% 6 17% (P \ .00001) and 59% 6 24% (P \ .0001), respectively (Figure 3). Specifically, P1 dropped to 30 mm Hg and P5 to 20 mm Hg in 14 patients, whereas these values remained greater than normal in 2 patients. The first of these patients became Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on November 11, 2013 2562 Isner-Horobeti et al The American Journal of Sports Medicine 100 ** 100 $ 80 80 * 70 mmHg 70 mmHg $$ 90 90 60 50 60 50 40 40 30 30 20 20 10 10 0 0 P1 before P1 after P5 before P5 after Figure 3. Intramuscular pressure in the anterior compartment before and after botulinum toxin injection. P1, intramuscular pressure 1 minute after the exercise. P5, intramuscular pressure 5 minutes after the exercise. Statistically significant results compared with preinjection values: *P \ .0001. **P \ .00001. asymptomatic, but IMP values remained high (P1 = 35 mm Hg, P5 = 24 mm Hg). Of note, preinjection values were high (P1 = 75 mm Hg, P5 = 62 mm Hg). For the second patient, postinjection IMP values remained high (P1 = 46 mm Hg, P5 = 21 mm Hg) and pain persisted. This patient was directed to successful fasciotomy. After the BoNT-A injection, in the lateral compartment, P1 and P5 decreased by 68% 6 21% (P \ .001) and 63% 6 21% (P \ .01), respectively (Figure 4). Specifically, P1 dropped to 30 mm Hg and P5 to 20 mm Hg in 15 patients, whereas they remained greater than normal in 1 patient, in whom P1 was 34 mm Hg (vs 57 mm Hg before BoNT-A injection) and P5 was normalized (10 mm Hg vs 36 mm Hg before BoNTA injection). This patient became asymptomatic. The extent of the reductions in P1 and P5 in the anterior and lateral compartments was similar. No correlation was found between the reduction in IMP in the anterior and/or lateral compartment and the total dose of BoNT-A injected into the compartment (Table 4). Effect of BoNT-A Injection on Clinical Data Clinical data were evaluated after 1 month and between 3 to 9 months (mean 6 SD, 4.4 6 1.6 months). Exertional Pain. The exertional pain disappeared completely during the follow-up period in 15 patients (94%). The pain disappeared in less than 1 month in 10 patients (67%), in 1 to 3 months in 2 patients (13%), and in 3 to 5 months in 3 patients (20%). The 15 patients without pain after BoNT-A injection could exercise more at follow-up as they did not report any pain. Only 1 patient reported no pain reduction. This patient had persistently high IMP values after injection (cf IMP results) despite receiving a similar dose of BoNT-A (total dose of 300 U: 110 U in tibialis anterior, 110 U in extensor digitorum longus, and 80 U in extensor hallucis longus). At 5 months, a fasciotomy was recommended, and the patient completely recovered. Muscle Strength. Muscle strength was rated as normal (5 on a scale from 0 to 5) for all muscles before BoNT-A injection. P1 before P1 after P5 before P5 after Figure 4. Intramuscular pressure in the lateral compartment before and after botulinum toxin injection. P1, intramuscular pressure 1 minute after the exercise. P5, intramuscular pres$ $$ sure 5 minutes after the exercise. P \ .01. P\ .001. The strength values per muscle 1 month after BoNT-A injection produced the following results: The mean (6SD) strength of the tibialis anterior was 4.6 6 0.4 (4-5, P = .001) (values were normal [5/5] in 5 patients [31%], 4.5 in 8 patients [50%], and 4 in 3 patients [19%]). The mean strength of the extensor digitorum longus was 4.7 6 0.4 (4-5, P = .001) (normal in 9 patients [56%], 4.5 in 5 patients [31%], and 4 in 2 patients [13%]). The mean strength of the extensor hallucis longus was 4.5 6 0.6 (3.5-5, P = .001) (normal in 8 patients [50%], 4.5 in 3 patients [19%], 4 in 3 patients [19%], and 3.5 in 2 patients [12%]). The mean strength of the peroneus longus was 4.9 6 0.3 (4-5, P = .19) (normal in 10 patients [84%], 4.5 in 1 patient [8%], and 4 in 1 patient [8%]); and the mean strength of the peroneus brevis was 4.9 6 0.3 (4-5, P = .19) (normal in 10 patients [84%], 4.5 in 1 patient [8%], and 4 in 1 patient [8%]). Muscle strength rated normal for all muscles at 4.4 6 1.6 months after BoNT-A injection. The evaluation per study subject provided the following results: The strength of all muscles was normal (5/5) in 5 patients (31%), whereas it was reduced in 11 patients (69%). In these 11 individuals, the average muscle strength 1 month after BoNT-A injection was 4.5 in 6 patients and 4 in 5 patients without functional consequences. No correlation was found between the evaluation of strength of each of the 5 muscles and the dose of BoNT-A injected per muscle expressed in units or in units per kilogram of body weight (Table 5). Safety. In 15 patients, no adverse effects were observed. Only 1 patient reported pain in the posterior compartment of her legs that was different from the anterolateral pain described previously. For this individual, BoNT-A was injected into the 3 muscles of the anterior compartment (total dose of 250 U: 90 U in tibialis anterior, 90 U in extensor digitorum longus, and 70 U in extensor hallucis longus). The BoNT-A dose was similar to the one used for the other 15 patients; the mean value was 288 6 25 U. The IMP measured in the right deep posterior compartment and the muscle strength were both normal. There was no evidence suggesting that the pain reported might have been caused by the BoNT-A injection. Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on November 11, 2013 Vol. 41, No. 11, 2013 Compartment Syndrome and Botulinum Toxin 2563 TABLE 4 Correlation Between the Reduction in IMP and Doses of BoNT-Aa BoNT-A, U BoNT-A, U/kg P1, Anterior Compartment P5, Anterior Compartment P1, Lateral Compartment P5, Lateral Compartment r = 0.12 (P = .61) r = –0.37 (P = .11) r = 0.17 (P = .46) r = –0.23 (P = .33) r = 0.24 (P = .24) r = –0.35 (P = .39) r = 0.43 (P = .43) r = –0.01 (P = .99) a BoNT-A, botulinum toxin A; IMP, intramuscular pressure; P1, IMP at 1 minute after cessation of exercise. P5, IMP at 5 minutes after cessation of exercise. TABLE 5 Correlation Between the Tested Muscle Strength and Dose of BoNT-Aa BoNT-A, U BoNT-A, U/kg Tibialis Anterior Extensor Digitorum Longus Extensor Hallucis Longus Peroneus Brevis Peroneus Longus r = 0.21 (P = .43) r = –0.01 (P = .97) r = 0.12 (P = .636) r = 0.25 (P = .33) r = –0.25 (P = .33) r = 0.22 (P = .39) r = –0.18 (P = .55) r = –0.22 (P = .47) r = –0.23 (P = .45) r = –0.16 (P = .60) a BoNT-A, botulinum toxin A. Moreover, after BoNT-A injection the patients did not complain about ankle instability during walking or running, and all were able to walk on their heels without pain. DISCUSSION The results of this case series show that an intramuscular injection of BoNT-A reduces intramuscular pressure in the compartments involved and eliminates exertional pain. These findings support our initial results in 2008 in a series of 7 patients who reported pain reduction after a BoNT-A injection in the muscles of the compartments affected by a CECS.27 This new case series is the first to examine the effects of BoNT-A on IMP, muscle pain, and muscle strength score in CECS patients. Effect of Intramuscular BoNT-A Injection on Intramuscular Pressure Our sample is representative of the population with CECS, as its characteristics are similar to those of other studies on anterior or anterolateral CECS of the leg.11,44,46,48,52 The patients’ average age was 23 years, and there was a marked male predominance (13 of 16 patients). The CECS was bilateral in almost two-thirds of the cases. The time to diagnosis, an average of 40 months, was close to that reported by Turnipseed et al52: 60 months. The IMP in the painful compartments was abnormal in all patients based on the criteria of Pedowitz et al.38 The choice of a cutoff value of 30 mm Hg at 1 minute after exercise was confirmed a posteriori by a 2012 systematic review,2 which showed that at 1 minute after exercise there was no overlap between IMP values in CECS patients and healthy controls and that in healthy controls, the IMP was never greater than 27.5 mm Hg at 1 minute after exercise. To date, surgical decompression52,24 is the only treatment for CECS recognized as curative. All other treatment alternatives are preventive or treat only the symptom. The medical approaches include reducing sports activities below the level that triggers pain or changing sports.46 Various physiotherapy techniques have been suggested to treat the pain, but none have had any lasting or proven efficacy.20,46 All these treatments were evaluated in studies using only posttreatment pain as the end point, not the IMP. However, because IMP is the only objective diagnostic parameter of CECS, it seemed logical to use it as the primary efficacy end point. Moreover, unlike the present study, most previous studies looked at pain reduction only, not complete elimination of pain. In the present study, IMP measured ~4.4 months after BoNT-A injection in the 42 compartments was 59% to 69% lower than the preinjection values, with a significance level of .01 to .00001 depending on the compartment. The IMP values returned to normal in the majority of patients (87.5%, n = 14). To date, only 2 studies comparing IMP before and after treatment have been reported in the literature. Blackman et al5 studied 7 athletes with anterior CECS of the leg; no changes in IMP (63 vs 68 mm Hg; P = .15) were found, but athletes reported some pain reduction after 5 weeks of treatment with massage and stretching. Biedert and Marti,4 in a study of 15 patients 8 to 72 months after a fasciotomy of the deep posterior compartment of the leg, reported a 91% reduction in the average IMP (18.5 mm Hg vs 1.6 mm Hg; P = .0001) as well as a reduction in pain. These results do not allow us to determine the time when IMP reduction starts or the duration of the effect of BoNT-A in lowering IMP. Further studies on the kinetics of BoNT-A are necessary to define the onset of action and total duration of efficacy of BoNT-A in lowering IMP. Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on November 11, 2013 2564 Isner-Horobeti et al The American Journal of Sports Medicine Effect of Intramuscular BoNT-A Injection on Clinical Parameters Exertional pain in CECS was considered an accessory criterion as it is a subjective functional parameter. The pain was followed up 1 month after the injection of BoNT-A, and a second evaluation was performed between 3 and 9 months (mean 6 SD, 4.4 6 1.6 months). The duration of action of BoNT-A on exertional pain beyond this period has yet to be examined. The efficacy of BoNT-A on exertional pain, measured as binary data (present or absent), may be considered positive since 15 of the 16 patients reported no exertional pain at 9 months after BoNT-A injection. The only participant who reported no pain relief had the highest IMP after the injection (P1 = 46 mm Hg and P5 = 21 mm Hg). Of note, the dose of BoNT-A used for this patient in the anterior compartment (300 U) was similar to the one used for the other 15 patients and was close to the mean value (288 6 25 U). The lack of previous studies using BoNT-A in this indication led us to choose the dose of BoNT-A according to our clinical experience and based on the literature. Our goal was to use the smallest dose possible in order to avoid muscle paralysis and functional impairment. This dose was onethird of the maximum recommended dose used for the treatment of lower limb spasticity,7,40 which is adjusted to the volume of the muscle to be injected and the patient’s body weight. Therefore, these initial results raise a question about the optimum dose of BoNT-A per muscle. Motor impairment was observed in 11 of the participants, but this effect had no functional consequences and was fully reversed after 3 months in 7 patients and after 4 months in the remaining 4 patients. Therefore, BoNT-A doses should be adjusted to maintain an optimum effect on IMP and pain while causing minimal motor deficit or side effects. The safety profile was excellent; only 1 patient reported a side effect, not serious and unexplained, involving pain in the treated leg but not in the territory injected. The BoNT-A dose injected into the anterior compartment of this patient was similar to the one used for the other study participants. The causality with respect to BoNT-A is unlikely. Regarding muscle strength, no correlation was found between the BoNT-A dose per muscle and muscle strength, but the doses injected were almost identical in all patients. The BoNT-A doses were chosen arbitrarily, based on doses used for other conditions, but this case series will help determine the doses for a future randomized, controlled study. Additionally, this study found no relation between the dose of BoNT-A injected and the reduction in IMP, probably because the doses were almost identical in all patients. We did not look for a correlation between exertional pain and the BoNT-A dose, as the total dose per patient was based on the number of affected compartments (anterior or anterolateral, unilateral or bilateral). Plausible Pathophysiological Mechanisms of BoNT-A in CECS The mechanism by which BoNT-A affects IMP and pain associated with CECS has yet to be determined, and several hypotheses have been suggested. Muscle fiber atrophy might be an indirect effect of BoNT-A given the reduced release of acetylcholine. The number of fibers remains unchanged, but their diameter is reduced.18,42 The first hypothesis is based on the known action of BoNT-A resulting in muscle hypotonia, which may cause moderate amyotrophy16,51,53 in muscles injected over a long period. This mode of action has been used for the treatment of unsightly hypertrophy of the masseter1,25 or triceps surae muscles.8,21,29 Therefore, a reduction of the hypertrophy of the lower leg muscles, even if only minimal, should help reduce CECS. This action of BoNT-A was targeted in our study, and further studies using medical imaging are necessary to support this pathophysiological hypothesis. The second hypothesis is based on the muscle relaxation induced by BoNT-A. The muscle hypotonia obtained may prolong the duration of the relaxation phase and reduce IMP,6 thereby improving blood flow to the muscles. One of the pathophysiological hypotheses formulated to explain CECS is the presence of muscle ischemia resulting in edema inside the compartment, which in turn explains the increases in IMP and in pain. Oskarsson et al,36 in a study of patients suffering from epicondylitis, showed that intramuscular BoNT-A injection in the extensor of the wrist improved blood flow in this muscle and was accompanied by pain belief. By analogy, muscle BoNT-A injection might improve blood flow in other pathological situations, such as CECS, leading to reduced IMP and pain relief. More recently, Edmundsson et al13 analyzed muscle biopsy specimens from patients during fasciotomy for CECS. The investigators showed a lower capillary supply of the tibialis anterior muscle in CECS, suggesting that local ischemia may be involved in the pathogenesis of CECS. The third hypothesis is related to the possible analgesic action of BoNT-A, as suggested in recent studies.15,39,43 The exertional pain associated with CECS may be related to the stimulation of nociceptors in the muscles and the fascia. This action could explain the elimination of exertional pain in 94% of the patients but cannot explain the posttreatment reduction of IMP. These 3 modes of action of BoNT-A are not necessarily exclusive and could work together. Limitations of the Study The present study is a retrospective analysis of clinical patient files that was performed to deepen our understanding of the possible beneficial effect of BoNT-A injection in painful muscle compartments resulting from CECS. Therefore, the timing of data measurements was not set a priori and it differed between patients, leading to a large variability in the follow-up period, ranging from 3 to 9 months after BoNT-A injection. Such a study design does not allow comparison of all participants at specific time points in the recovery period but provides a view of the recovery process at different time points. Another potential weakness of the study design is that IMP and clinical parameters (ie, muscle strength and pain) were not always assessed simultaneously, which prevents direct comparison of the time course of these variables. Nevertheless, we believe that these potential limitations do not affect the main findings of the study: muscular injection of BoNT-A into painful Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on November 11, 2013 Vol. 41, No. 11, 2013 Compartment Syndrome and Botulinum Toxin compartments of study subjects with CECS characterized by abnormally elevated IMP restored normal IMP in 88% of participants and alleviated the associated muscle pain in 94% of participants. The remaining symptomatic patient was directed to fasciotomy and fully recovered. Therefore, a major outcome of this study is that a therapeutic strategy combining BoNT-A injection and (if injection is not successful) fasciotomy allowed all our patients with CECS to resume their normal level of physical activity. Of note, the present result that BoNT-A injection lowered IMP and muscle pain was observed without dramatic impairment of muscle function, as indicated by significant but moderate reductions of Medical Research Council scores. Although muscle function might be more accurately evaluated in future studies to further ascertain the functional effect of BoNT-A injection, we believe that muscle function was mostly preserved because of the low volume of BoNT-A injected into the painful muscle compartments of our CECS patients. Although the BoNT-A dose was established from previous reports as well as the experience of our clinicians, it might well be further optimized to favor the reduction of IMP while maintaining the most muscle function. In conclusion, the initial results of this case series showed that the intramuscular injection of BoNT-A has a short-term effect in reducing IMP and lowering exertional pain in patients with CECS in the anterior or anterolateral compartment of the leg. These encouraging results need to be confirmed by a randomized controlled study carried out over a longer period. Such a study would help define the onset and duration of action as well as the optimum dose of BoNT-A in this indication. Further studies are also necessary to define the mechanisms of action of BoNT-A on IMP and exertional pain in CECS. ACKNOWLEDGMENT Special thanks goes to Professor Bernard Poulain, deputy scientific director, Neurosciences et Cognition, Institut des Sciences Biologiques du Centre National de la Recherche Scientifique (France), for reading the manuscript and for his advice. REFERENCES 1. Ascher B, Talarico S, Cassuto D, et al. International consensus recommendations on the aesthetic usage of botulinum toxin type A (Speywood Unit)—part II: wrinkles on the middle and lower face, neck and chest. J Eur Acad Dermatol Venereol. 2010;24(11):1285-1295. 2. Aweid O, Del Buono A, Malliaras P, et al. Systematic review and recommendations for intracompartmental pressure monitoring in diagnosing chronic exertional compartment syndrome of the leg. Clin J Sport Med. 2012;22(4):356-370. 3. Bakheit AM, Ward CD, McLellan DL. Generalised botulism-like syndrome after intramuscular injections of botulinum toxin type A: a report of two cases. J Neurol Neurosurg Psychiatry. 1997;62(2):198. 4. Biedert RM, Marti B. Intracompartmental pressure before and after fasciotomy in runners with chronic deep posterior compartment syndrome. Int J Sports Med. 1997;18(5):381-386. 5. Blackman PG, Simmons LR, Crossley KM. Treatment of chronic exertional anterior compartment syndrome with massage: a pilot study. Clin J Sport Med. 1998;8(1):14-17. 2565 6. Bouche RT. Chronic compartment syndrome of the leg. J Am Podiatr Med Assoc. 1990;80(12):633-648. 7. Burbaud P, Wiart L, Dubos JL, et al. A randomised, double blind, placebo controlled trial of botulinum toxin in the treatment of spastic foot in hemiparetic patients. J Neurol Neurosurg Psychiatry. 1996;61(3):265-269. 8. Costa J, Graca P, Evangelista T, de Carvalho M. Pain and calf hypertrophy associated with spontaneous repetitive discharges treated with botulinum toxin. Clin Neurophysiol. 2005;116(12):2847-2852. 9. Cote TR, Mohan AK, Polder JA, Walton MK, Braun MM. Botulinum toxin type A injections: adverse events reported to the US Food and Drug Administration in therapeutic and cosmetic cases. J Am Acad Dermatol. 2005;53(3):407-415. 10. Davey JR, Rorabeck CH, Fowler PJ. The tibialis posterior muscle compartment: an unrecognized cause of exertional compartment syndrome. Am J Sports Med. 1984;12(5):391-397. 11. de Fijter WM, Scheltinga MR, Luiting MG. Minimally invasive fasciotomy in chronic exertional compartment syndrome and fascial hernias of the anterior lower leg: short- and long-term results. Mil Med. 2006;171(5):399-403. 12. Detmer DE, Sharpe K, Sufit RL, Girdley FM. Chronic compartment syndrome: diagnosis, management, and outcomes. Am J Sports Med. 1985;13(3):162-170. 13. Edmundsson D, Toolanen G, Thornell LE, Stal P. Evidence for low muscle capillary supply as a pathogenic factor in chronic compartment syndrome. Scand J Med Sci Sports. 2010;20(6):805-813. 14. Ehsan O, Darwish A, Edmundson C, Mills V, Al-Khaffaf H. Non-traumatic lower limb vascular complications in endurance athletes: review of literature. Eur J Vasc Endovasc Surg. 2004;28(1):1-8. 15. Favre-Guilmard C, Auguet M, Chabrier PE. Different antinociceptive effects of botulinum toxin type A in inflammatory and peripheral polyneuropathic rat models. Eur J Pharmacol. 2009;617(1-3):48-53. 16. Finn S, Ryan P, Sleeman D. The medical management of masseteric hypertrophy with botulinum toxin. J Ir Dent Assoc. 2000;46(3):84-86. 17. Fortuna R, Horisberger M, Vaz MA, Van der Marel R, Herzog W. The effects of electrical stimulation exercise on muscles injected with botulinum toxin type-A (botox). J Biomech. 2013;46(1):36-42. 18. Fortuna R, Vaz MA, Youssef AR, Longino D, Herzog W. Changes in contractile properties of muscles receiving repeat injections of botulinum toxin (Botox). J Biomech. 2011;44(1):39-44. 19. Fraipont MJ, Adamson GJ. Chronic exertional compartment syndrome. J Am Acad Orthop Surg. 2003;11(4):268-276. 20. Gill CS, Halstead ME, Matava MJ. Chronic exertional compartment syndrome of the leg in athletes: evaluation and management. Phys Sportsmed. 2010;38(2):126-132. 21. Han KH, Joo YH, Moon SE, Kim KH. Botulinum toxin A treatment for contouring of the lower leg. J Dermatolog Treat. 2006;17(4):250-254. 22. Hislop M, Tierney P. Intracompartmental pressure testing: results of an international survey of current clinical practice, highlighting the need for standardised protocols. Br J Sports Med. 2011;45(12):956-958. 23. Howard JL, Mohtadi NG, Wiley JP. Evaluation of outcomes in patients following surgical treatment of chronic exertional compartment syndrome in the leg. Clin J Sport Med. 2000;10(3):176-184. 24. Hutchinson MR, Bederka B, Kopplin M. Anatomic structures at risk during minimal-incision endoscopically assisted fascial compartment releases in the leg. Am J Sports Med. 2003;31(5):764-769. 25. Kim NH, Park RH, Park JB. Botulinum toxin type A for the treatment of hypertrophy of the masseter muscle. Plast Reconstr Surg. 2010;125(6):1693-1705. 26. Kuehn BM. FDA requires black box warnings on labeling for botulinum toxin products. JAMA. 2009;301(22):2316. 27. Lecocq J, Isner-Horobeti ME. Treatment of exertional compartment syndrome leg with botulinum toxin A: a first open pilot study. J Rehabil Med. 2008;(suppl 47):111-112. 28. Lecocq J, Isner-Horobeti ME, Dupeyron A, Helmlinger JL, Vautravers P. [Exertional compartment syndrome]. Ann Readapt Med Phys. 2004;47(6):334-345. 29. Lee HJ, Lee DW, Park YH, Cha MK, Kim HS, Ha SJ. Botulinum toxin A for aesthetic contouring of enlarged medial gastrocnemius muscle. Dermatol Surg. 2004;30(6):867-871; discussion 871. Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on November 11, 2013 2566 Isner-Horobeti et al The American Journal of Sports Medicine 30. Longino D, Butterfield TA, Herzog W. Frequency and length-dependent effects of botulinum toxin-induced muscle weakness. J Biomech. 2005;38(3):609-613. 31. Martens MA, Backaert M, Vermaut G, Mulier JC. Chronic leg pain in athletes due to a recurrent compartment syndrome. Am J Sports Med. 1984;12(2):148-151. 32. Medical Research Council. Aids to the Investigation of Peripheral Nerve Injuries. War Memorandum No. 7. 2nd ed. rev. London: His Majesty’s Stationery Office; 1943. 33. Mohler LR, Styf JR, Pedowitz RA, Hargens AR, Gershuni DH. Intramuscular deoxygenation during exercise in patients who have chronic anterior compartment syndrome of the leg. J Bone Joint Surg Am. 1997;79(6):844-849. 34. Naidu K, Smith K, Sheedy M, Adair B, Yu X, Graham HK. Systemic adverse events following botulinum toxin A therapy in children with cerebral palsy. Dev Med Child Neurol. 2010;52(2):139-144. 35. O’Brien C. Injection techniques for botulinum toxin using electromyography and electrical stimulation. Muscle Nerve. 1997;6(suppl):176180. 36. Oskarsson E, Piehl Aulin K, Gustafsson BE, Pettersson K. Improved intramuscular blood flow and normalized metabolism in lateral epicondylitis after botulinum toxin treatment. Scand J Med Sci Sports. 2009;19(3):323-328. 37. Packer JD, Day MS, Nguyen JT, Hobart SJ, Hannafin JA, Metzl JD. Functional outcomes and patient satisfaction after fasciotomy for chronic exertional compartment syndrome. Am J Sports Med. 2013;41(2):430-436. 38. Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni DH. Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med. 1990;18(1):35-40. 39. Pickett A. Re-engineering clostridial neurotoxins for the treatment of chronic pain: current status and future prospects. BioDrugs. 2010;24(3):173-182. 40. Pittock SJ, Moore AP, Hardiman O, et al. A double-blind randomised placebo-controlled evaluation of three doses of botulinum toxin type A (Dysport) in the treatment of spastic equinovarus deformity after stroke. Cerebrovasc Dis. 2003;15(4):289-300. 41. Placzek R, Drescher W, Deuretzbacher G, Hempfing A, Meiss AL. Treatment of chronic radial epicondylitis with botulinum toxin A: a double-blind, placebo-controlled, randomized multicenter study. J Bone Joint Surg Am. 2007;89(2):255-260. 42. Poulain B, Poppof MR. How do the botulinum neurotoxins block neurotransmitter release: from botulism to the molecular mechanism of action. Botulinum J. 2008;1(1):14-87. 43. Ranoux D, Attal N, Morain F, Bouhassira D. Botulinum toxin type A induces direct analgesic effects in chronic neuropathic pain. Ann Neurol. 2008;64(3):274-283. 44. Schepsis AA, Gill SS, Foster TA. Fasciotomy for exertional anterior compartment syndrome: is lateral compartment release necessary? Am J Sports Med. 1999;27(4):430-435. 45. Schepsis AA, Martini D, Corbett M. Surgical management of exertional compartment syndrome of the lower leg: long-term followup. Am J Sports Med. 1993;21(6):811-817; discussion 817. 46. Schissel DJ, Godwin J. Effort-related chronic compartment syndrome of the lower extremity. Mil Med. 1999;164(11):830-832. 47. Schubert AG. Exertional compartment syndrome: review of the literature and proposed rehabilitation guidelines following surgical release. Int J Sports Phys Ther. 2011;6(2):126-141. 48. Slimmon D, Bennell K, Brukner P, Crossley K, Bell SN. Long-term outcome of fasciotomy with partial fasciectomy for chronic exertional compartment syndrome of the lower leg. Am J Sports Med. 2002;30(4):581-588. 49. Soares A, Andriolo RB, Atallah AN, da Silva EM. Botulinum toxin for myofascial pain syndromes in adults. Cochrane Database Syst Rev. 2012;(4):CD007533. 50. Styf J. Definitions and terminology: etiology and pathogenesis of chronic compartment syndrome. In: Compartment Syndromes: Diagnosis, Treatment, and Complications. Styf J Ed. Boca Raton, FL: CRC Press; 2004:1-8. 51. To EW, Ahuja AT, Ho WS, et al. A prospective study of the effect of botulinum toxin A on masseteric muscle hypertrophy with ultrasonographic and electromyographic measurement. Br J Plast Surg. 2001;54(3):197-200. 52. Turnipseed W, Detmer DE, Girdley F. Chronic compartment syndrome: an unusual cause for claudication. Ann Surg. 1989;210(4):557-562; discussion 562-563. 53. von Lindern JJ, Niederhagen B, Appel T, Berge S, Reich RH. Type A botulinum toxin for the treatment of hypertrophy of the masseter and temporal muscles: an alternative treatment. Plast Reconstr Surg. 2001;107(2):327-332. 54. Waseem Z, Boulias C, Gordon A, Ismail F, Sheean G, Furlan AD. Botulinum toxin injections for low-back pain and sciatica. Cochrane Database Syst Rev. 2011;(1):CD008257. 55. Wilder RP, Magrum E. Exertional compartment syndrome. Clin Sports Med. 2010;29(3):429-435. 56. Wittstein J, Moorman CT III, Levin LS. Endoscopic compartment release for chronic exertional compartment syndrome: surgical technique and results. Am J Sports Med. 2010;38(8):1661-1666. For reprints and permission queries, please visit SAGE’s Web site at http://www.sagepub.com/journalsPermissions.nav Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on November 11, 2013