Acute Patellar Dislocation in Children and Adolescents: A Randomized Clinical Trial 463

463
C OPYRIGHT
Ó 2008 BY T HE J OURNAL OF B ONE AND J OINT S URGERY , I NCORPORATED
Acute Patellar Dislocation in Children and
Adolescents: A Randomized Clinical Trial
By Sauli Palmu, BM, Pentti E. Kallio, MD, PhD, Simon T. Donell, FRCS(Orth), MD,
Ilkka Helenius, MD, PhD, and Yrj¨an¨a Nietosvaara, MD, PhD
Investigation performed at Aurora Hospital, Helsinki, and Children’s Hospital, Helsinki University Central Hospital, Helsinki, Finland
Background: The treatment of acute patellar dislocation in children is controversial. Some investigators have advocated early repair of the medial structures, whereas others have treated this injury nonoperatively. The present report describes the long-term subjective and functional results of a randomized controlled trial of nonoperative and operative treatment of primary acute patellar dislocation in children less than sixteen years of age.
Methods: The data were gathered prospectively on a cohort of seventy-four acute patellar dislocations in seventy-one patients (fifty-one girls and twenty boys) younger than sixteen years of age. Sixty-two patients (sixty-four knees) without large (>15 mm) intra-articular fragments were randomized to nonoperative treatment (twenty-eight knees) or operative treatment (thirty-six knees). Operative treatment consisted of direct repair of the damaged medial structures if the patella was dislocatable with the patient under anesthesia (twenty-nine knees) or lateral release alone if the patella was not dislocatable with the patient under anesthesia (seven knees). All but four patients who underwent operative treatment had a concomitant lateral release. The rehabilitation protocol was the same for both groups. The patients were seen at two years, and a telephone interview was conducted at a mean of six years and again at a mean of fourteen years. Fifty-eight patients (sixty-four knees; 94%) were reviewed at the time of the most recent follow-up.
Results: At the time of the most recent follow-up, the subjective result was either good or excellent for 75% (twentyone) of twenty-eight nonoperatively treated knees and 66% (twenty-one) of thirty-two operatively treated knees. The rates of recurrent dislocation in the two treatment groups were 71% (twenty of twenty-eight) and 67% (twenty-four of thirty-six), respectively. The first redislocation occurred within two years after the primary injury in twenty-three (52%) of the forty-four knees with recurrent dislocation. Instability of the contralateral patella was noted in thirty (48%) of the sixty-two patients. The only significant predictor for recurrence was a positive family history of patellar instability. The mode of treatment and the existence of osteochondral fractures had no clinical or significant influence on the subjective outcome, recurrent patellofemoral instability, function, or activity scores.
Conclusions: The long-term subjective and functional results after acute patellar dislocation are satisfactory in most patients. Initial operative repair of the medial structures combined with lateral release did not improve the long-term outcome, despite the very high rate of recurrent instability. A positive family history is a risk factor for recurrence and for contralateral patellofemoral instability. Routine repair of the torn medial stabilizing soft tissues is not advocated for the treatment of acute patellar dislocation in children and adolescents.
Level of Evidence: Therapeutic Level II. See Instructions to Authors for a complete description of levels of evidence.
A cu te patellar dislocation is the most common acute knee disorder in children and adolescents, and it may lead to functional disability 1-3 . The peak incidence of acute patellar dislocation occurs at the age of fifteen years 2,4-6 .
The reported incidence in the urban population of Helsinki is forty-three per 100,000 for those under sixteen years of age 2 .
Disclosure: The authors did not receive any outside funding or grants in support of their research for or preparation of this work. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which the authors, or a member of their immediate families, are affiliated or associated.
A commentary is available with the electronic versions of this article, on our web site (www.jbjs.org) and on our quarterly CD-ROM (call our subscription department, at 781-449-9780, to order the CD-ROM).
J Bone Joint Surg Am.
2008;90:463-70 d doi:10.2106/JBJS.G.00072
T H E J O U R N A L O F B O N E & J O I N T S U R G E R Y d
J B J S
.
O R G
V O L U M E 9 0 - A d
N U M B E R 3 d
M
A R C H 2 0 0 8
464
A C U T E P AT E L L A R D I S L O C AT I O N I N C H I L D R E N A N D A D O L E S C E N T S :
A R A N D O M I Z E D C L I N I C A L T R I A L
The proposed etiological predisposing factors for acute patellar dislocation include patellofemoral dysplasia, female gender, and a positive family history 1,7 . The reported risk factors for recurrent patellar dislocation and poor outcome include young age at the time of primary dislocation, female gender, and dysplasia of the patellofemoral joint 2,8,9 .
Nonoperative treatment traditionally has been advocated for acute patellar dislocation unless substantial joint surface damage is found 1,6,7 . Primary operative repair of the medial patella-stabilizing soft tissues became popular during the 1980s because such treatment was thought to reduce the risk of redislocation 10 . Most previous studies on acute patellar dislocation have involved mainly adult patient populations and have demonstrated high redislocation rates following both operative and nonoperative treatment 6-8,11,12 . However, to our knowledge, there has been only one report on acute patellar dislocation in a pediatric population 13 and there have been no reports comparing the results of operative and nonoperative treatment.
Our hypothesis in 1990 was that primary operative repair of the injured medial retinacular structures would reduce the redislocation rate and improve the results of treatment in pediatric patients with an acute patellar dislocation. The aim of the present prospective population-based study was also to examine the long-term results in such patients and to attempt to identify possible risk factors for late poor subjective and functional outcomes.
Materials and Methods
Patient Selection and Demographic Data
A ll children younger than sixteen years of age with an evident or suspected acute patellar dislocation were admitted to the emergency department of our hospital during a two-year prospective study period in 1991 and 1992. Over this time-period, our hospital admitted 90% of the pediatric patients in the city. Clinical examination, imaging studies (anteroposterior and lateral radiographs of the injured knee and tangential radiographs of both patellae with the knees in 20 ° of flexion 14 ), examination with use of anesthesia, and diagnostic arthroscopy were performed for all patients.
Seventy-four knees in seventy-one patients met at least one of three diagnostic criteria of acute patellar dislocation.
These criteria included lateral dislocation of the patella necessitating reduction (thirty knees), the ability to dislocate the patella on examination with the patient under anesthesia (fiftyfive knees), and the presence of findings that are typical of acute patellar dislocation, particularly a synovial tear medial to the patella, on diagnostic arthroscopy (all seventy-four knees).
The initial study population included thirty-nine left knees and thirty-five right knees. The mean age of the seventyone patients was thirteen years (range, nine to fifteen years).
Fifty-one patients were girls, and twenty were boys. Thirtythree patients (46%) had a positive family history of patellar dislocation. The femoral sulcus was abnormally shallow in
71% of the affected knees according to the criterion of
Jacobsen and Bertheussen 15 (a sulcus angle of >148 ° ) and in
53% of the knees according to the criterion of Larsen and
Lauridsen 16 (a sulcus angle of >150 ° ). The frequency of patella alta was 66% according to the criterion of Insall et al.
17,18 (a patellar height ratio in excess of 1.2) and 34% according to the criterion of Jacobsen and Bertheussen 15 (a patellar height ratio in excess of 1.3). An unstable patellar configuration (type II/III,
III, IV, or V) 19,20 was noted in 82% of the knees. Radiographs revealed that the tibial tubercle apophysis was open in 89% of all knees.
A subgroup was selected for a randomized treatment study on the basis of five inclusion criteria: (1) the occurrence of an acute lateral patellar dislocation within two weeks before treatment, (2) no history of previous knee surgery or substantial knee injury, (3) no major coexistent tibiofemoral ligamentous injury requiring repair, (4) no large osteochondral fracture fragments (diameter >15 mm) requiring fixation, and
(5) a willingness of the patient and parents to participate. Two patients (two knees) were excluded because they had sustained an acute patellar dislocation more than two weeks before treatment, two patients (two knees) were excluded because they had been managed operatively by surgeons not involved in the study, four patients (four knees) were excluded because they had osteochondral fracture fragments requiring fixation, and two patients (two knees) were excluded because they were unwilling or unable to participate (including one patient who was mentally handicapped and one patient who refused randomization).
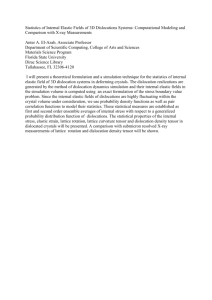
The excluded patients did not differ from the study population with respect to gender, age distribution, or clinical, radiographic, or arthroscopic findings. In all, sixty-four knees in sixty-two patients were recruited into the randomized study
(Fig. 1).
Randomization and Treatment
The hospital ethics committee approved the study. In order to avoid the use of different treatment methods in patients with bilateral involvement, randomization was performed according to the year of birth, with patients who had been born in odd years being randomized to nonoperative treatment (twentyeight knees) and those who had been born in even years being randomized to operative treatment (thirty-six knees). Randomization was performed by the treating surgeon (Y.N.) at the time of admission. The mean age of the patients in both randomized treatment groups was 13 ± 2 years. A positive family history was reported for fifteen of the twenty-seven patients in the nonoperative treatment group and fifteen of the thirty-five patients in the operative treatment group.
Pre-injury Tegner activity scores were estimated by the patients and their parents at the time of admission to the hospital. The mean pre-injury Tegner activity level was 5 in both treatment groups.
In the nonoperative treatment group, the mean sulcus angle 4 was 153 ° (range, 130 ° to 174 ° ) and the mean Insall-
Salvati index 17 was 1.27 (range, 0.93 to 1.65). In the operative treatment group, the mean sulcus angle was 152 ° (range, 139 ° to 165 ° ) and the mean Insall-Salvati index 17 was 1.29 (range,
1.00 to 1.64).
T H E J O U R N A L O F B O N E & J O I N T S U R G E R Y d
J B J S
.
O R G
V O L U M E 9 0 - A d
N U M B E R 3 d
M
A R C H 2 0 0 8
465
A C U T E P AT E L L A R D I S L O C AT I O N I N C H I L D R E N A N D A D O L E S C E N T S :
A R A N D O M I Z E D C L I N I C A L T R I A L
Fig. 1
Flow chart describing the allocation and follow-up of seventy-four acute patellar dislocations in seventy-one patients. MR = medial soft-tissue repair, LR = lateral release, and EUA = examination with the patient under anesthesia. The n values are expressed as the number of knees followed by the number of patients. *Lateral release was performed in all except four knees with medial tissue repair.
In twenty-nine of the thirty-six knees that had been randomized to operative treatment, the patella was dislocatable with the patient under anesthesia. In this subgroup of twentynine knees, surgical exploration revealed simultaneous rupture of the medial patellotibial ligament at the patellar insertion and the medial patellofemoral ligament at the femoral insertion in nine knees, isolated medial patellofemoral ligament rupture in five knees, isolated medial patellotibial ligament rupture in four knees, a midsubstance medial retinacular tear in six knees, and a parapatellar retinacular tear in five knees. Operative repair was performed by means of direct absorbable suture placement at the site of injury without aponeurotic or tendinous augmentations. Lateral release was also performed in all except four knees. In the seven knees that had been randomized to operative treatment in which the patella was not dislocatable when examined with the patient under anesthesia, only a lateral release was performed.
The aftercare was identical for both treatment groups.
Patients in whom the patella was dislocatable under anesthesia were managed with a removable knee extension orthosis (Immobilizer; Camp International, Jackson, Michigan) for three weeks, followed by a patella-stabilizing orthosis (Patella Stabilizer; Camp International) for an additional three weeks.
Patients in whom the patella was not dislocatable under anesthesia were managed with a patella-stabilizing orthosis for six weeks. Thigh muscle exercises and full weight-bearing were
T H E J O U R N A L O F B O N E & J O I N T S U R G E R Y d
J B J S
.
O R G
V O L U M E 9 0 - A d
N U M B E R 3 d
M
A R C H 2 0 0 8
466
A C U T E P AT E L L A R D I S L O C AT I O N I N C H I L D R E N A N D A D O L E S C E N T S :
A R A N D O M I Z E D C L I N I C A L T R I A L
TABLE I Characteristics of the Sixty-two Randomized Patients (Sixty-four Knees)*
Nonoperative Treatment
Group (N = 28)
Demographic characteristics
Age † (yr)
No. of girls
Tegner activity level †
Primary injury (no. of knees)
Indirect
Spontaneous relocation
Joint surface damage
Radiographic findings
Sulcus angle † (deg)
Insall-Salvati ratio †
Results at 6-year follow-up ‡
Percentage of knees with an excellent or good subjective result
Redislocation rate
Kujala score †
Hughston visual analog score †
Tegner activity level †
Results at 14-year follow-up§
Percentage of knees with an excellent or good subjective result
Redislocation rate
Kujala score †
Hughston visual analog score †
Tegner activity level †
13
19
6
27
18
153
1.3
79% (22 of 28)
54% (15 of 28)
88 ± 8
90 ± 9
5.2
± 2.1
75% (21 of 28)
71% (20 of 28)
84
8
±
±
±
±
±
2
2
6
0.2
13
91 ± 10
6.0
± 1.9
Operative Treatment
Group (N
13
27
5
33
17
152
9
1.3
±
±
±
±
2
2
8
=
0.2
58% (21 of 36)
50% (18 of 36)
81 ± 21
83 ± 17
4.7
± 2.0
36)
66% (21 of 32)
67% (24 of 36)
83 ± 18
84 ± 18
4.4
± 1.4
*Significant differences between the groups were not found.
† The values are given as the mean and the standard deviation.
‡ The rate of follow-up was 100% for all outcomes. §The rate of follow-up was 94% for all outcomes except the redislocation rate, for which it was 100%.
started as soon as tolerated by the patient. All patients were encouraged to use the orthosis in the rehabilitation sessions and during athletic activities for the first six months after the injury.
Follow-up
All sixty-two randomized patients (sixty-four knees) were examined two years after acute patellar dislocation and were interviewed by telephone at an average of six years (range, five to eight years) after acute patellar dislocation. A final telephone interview of fifty-eight patients (reporting on 94% of the randomized knees) was conducted by an independent observer (S.P.) at an average of fourteen years (range, eleven to fifteen years). At the time of each follow-up, the subjective result, the history of subluxations, the history of repeat patellar dislocations, the time of recurrence, the history of reoperations, and the change in activity level were noted. The patients were questioned about a family history of patellar dislocation at the six and fourteen-year follow-up evaluations, and the history was regarded as positive if a first or seconddegree relative with patellar dislocation was reported. Routine follow-up radiographs were not made at any of the sampling times.
Outcomes were evaluated with the Hughston visual analog scale knee score 21 (adjusted to give values ranging from
28 to 100), the Kujala score 22 , and a subjective grade (patients were asked to grade their knees as excellent, good, fair, or poor). The activity level was analyzed with use of the Tegner activity scale 23 .
Statistical Analysis
To test the normality of the variances, the Shapiro-Wilk W test and the Kolmogorov-Sminov test were used. The t test was used for parametric variances, and the Mann-Whitney U test and chi-square test were used for nonparametric variances.
The level of significance was set at 5%. Correlations were tested with use of Spearman rho.
The sample-size requirement of sixteen patients per study group was calculated with use of a study power of 80%, a type-I error ( a ) of 0.05, and an estimated effect size of 1.0.
Effect size evaluation was based on an assumption that the mean Kujala symptom score (the primary end point) would be
70 and 85 for the nonoperative and operative treatment groups, respectively.
If the redislocation rate would have been 10% for the operative treatment group and 50% for the nonoperative treat-
T H E J O U R N A L O F B O N E & J O I N T S U R G E R Y d
J B J S
.
O R G
V O L U M E 9 0 - A d
N U M B E R 3 d
M
A R C H 2 0 0 8
467
A C U T E P AT E L L A R D I S L O C AT I O N I N C H I L D R E N A N D A D O L E S C E N T S :
A R A N D O M I Z E D C L I N I C A L T R I A L
Fig. 2
Graph illustrating the occurrence of redislocation of the patella in the sixty-four knees with an acute patellar dislocation that were recruited for the randomized treatment trial.
ment group, seventeen patients in each group would have been required with use of similar study power and type-I error numbers as above.
Results
Subjective Results
A fter a mean duration of follow-up of fourteen years, a good or excellent subjective result was recorded for twentyone (75%) of twenty-eight knees that had been randomized to the nonoperative treatment group and twenty-one (66%) of thirty-two knees that had been randomized to the operative treatment group (Table I). A good or excellent subjective result was recorded for twenty-five (60%) of forty-two knees without joint surface damage, compared with eleven (61%) of eighteen knees with joint surface damage. These differences were not significant (p = 0.479 and 0.961, respectively). With the numbers available, we did not find any significant predictive value between the radiographic indices and the final subjective result. There was a positive correlation between the final subjective result and the Hughston visual analog scale (Spearman rho, 0.595; p < 0.001) and Kujala scores (Spearman rho, 0.671; p < 0.001).
Patellofemoral Instability
The redislocation rates were similar in the two groups of randomized patients, with a rate of 71% (twenty of twentyeight) following nonoperative treatment and of 67% (twentyfour of thirty-six) following operative repair (Table I). More than half of the patients with redislocation (twenty-three
[52%] of forty-four knees) experienced the first recurrent patellar dislocation within two years after the primary injury
(Fig. 2). The mean number of redislocations was two (range, one to ten). Patellofemoral instability, including recurrent patellar dislocation and subjective sensations of subluxation, occurred in 91% (fifty-eight) of the sixty-four randomized knees, with no significant differences between the two treatment groups. Patellofemoral instability of the contralateral knee was found in 44% (twelve) of the twenty-seven patients in the nonoperative treatment group and in 51% (eighteen) of the thirty-five patients in the operative treatment group
(p = 0.539).
Recurrent patellar dislocation was recorded in 83%
(twenty-five) of the thirty knees in patients with a positive family history of patellar instability and in 56% (nineteen) of the thirty-four knees in patients with a negative family history
(p = 0.027). In comparison with patients who had a negative family history of patellar instability, those who had a positive family history showed greater rates of patellofemoral instability of both the affected knee (97% [twenty-nine of thirty] compared with 88% [thirty of thirty-four]; p = 0.201) and the contralateral knee (70% [twenty-one of thirty] compared with
32% [eleven of thirty-four]; p = 0.004).
Age, gender, sulcus angle, and patellar height were similar in patients with or without recurrent patellofemoral instability. The mean patellar height ratio was 1.25 in patients with zero to three recent patellar dislocations and 1.39 in those with more than three dislocations (p = 0.025). The mean sulcus angle was 151 ° and 156 ° , respectively (p = 0.022).
Eight of the ten nonrandomized patients experienced patellofemoral instability during follow-up. The mean number of patellar redislocations in this small group of patients was two. Half of these patients had a positive family history of patellar instability.
Reoperations
Altogether, twenty-seven of the sixty-four knees (including eleven of twenty-eight that initially had been randomized to the nonoperative treatment group and sixteen of the thirty-six
T H E J O U R N A L O F B O N E & J O I N T S U R G E R Y d
J B J S
.
O R G
V O L U M E 9 0 - A d
N U M B E R 3 d
M
A R C H 2 0 0 8
468
A C U T E P AT E L L A R D I S L O C AT I O N I N C H I L D R E N A N D A D O L E S C E N T S :
A R A N D O M I Z E D C L I N I C A L T R I A L
Fig. 3
Bar graph illustrating the estimated Tegner activity score in all sixty-two randomized patients before the acute patellar dislocation and in fifty-eight of sixty-two patients at the time of the most recent follow-up. Tegner activity scores were estimated by the patients and their parents at the time of admission to the hospital (pre-injury activity) and again by the patients at the time of the most recent follow-up.
that initially had been randomized to the operative treatment group) had surgery for the treatment of patellofemoral problems.
The median number of reoperations was one (range, one to seven). Five of the ten nonrandomized knees underwent reoperation.
Functional Results
At the time of the most recent follow-up, the mean Kujala scores for the nonoperative and operative groups were 84 and
83, respectively (p = 0.489) (Table I). The mean Kujala scores for patients with and without joint surface damage were 85 and
83, respectively (p = 0.994). The mean Hughston visual analog scale scores for the nonoperative and operative groups were 91 and 84, respectively (p = 0.195). The mean Hughston visual analog scale scores for patients with and without joint surface damage were 89 and 86, respectively (p = 0.808). The mean
Kujala and Hughston visual analog scale scores in the nonrandomized patients were both 86.
Boys (n = 16) had better results than girls (n = 42) as measured with both Kujala scores (89 compared with 80, p =
0.056) and Hughston visual analog scale scores (93 compared with 83, p = 0.007). There was a positive correlation between the two functional scoring systems used (0.824, p < 0.001). In addition, the Hughston visual analog scale score correlated positively with the Tegner activity score (Spearman rho,
0.413; p < 0.001) and negatively with the number of recurrent patellar dislocations (Spearman rho, 2 0.366; p = 0.004).
The Kujala score correlated negatively with the number of recurrent patellar dislocations (Spearman rho, 2 0.448; p < 0.001).
Tegner Activity Scores
Tegner activity scores were estimated by the patients and their parents at the time of admission to the hospital (on the basis of the level of pre-injury activity) and again by the patients at the time of the most recent follow-up (Fig. 3). The Tegner activity score improved for twenty of fifty-eight patients, remained at the pre-injury level for ten, and decreased for twenty-eight; the median score was unchanged (median, 5; range, 1 to 10). The median Tegner activity score for the nonrandomized patients also remained unchanged. We could not identify a relationship between an improved Tegner activity score and age, gender, the type of treatment, or patellofemoral instability. The mean Tegner activity scores were better for boys than for girls both at the time of admission (6.5 compared with 4.8; p < 0.001) and at the time of the most recent follow-up (6.1 compared with 4.8; p = 0.007).
Discussion
T his population-based cohort probably represented 90% of the patients with an acute patellar dislocation within the catchment area 24 and is, to our knowledge, the largest study of pediatric patients that has been performed to date 13 . The minimum duration of follow-up was eleven years. During the follow-up period, all patients were contacted at least twice and thus the follow-up rate concerning recurrent instability was
100%. The subjective result and the functional and activity scores were recorded at the time of the most recent follow-up for 94% of the randomized knees. Performance measures
(figure-of-eight run, one-leg hop, number of squats per minute) that were registered at the time of the two-year follow-up
T H E J O U R N A L O F B O N E & J O I N T S U R G E R Y d
J B J S
.
O R G
V O L U M E 9 0 - A d
N U M B E R 3 d
M
A R C H 2 0 0 8
469
A C U T E P AT E L L A R D I S L O C AT I O N I N C H I L D R E N A N D A D O L E S C E N T S :
A R A N D O M I Z E D C L I N I C A L T R I A L were similar in the nonoperatively and operatively treated patients 24,25 .
To our knowledge, there have been no previous randomized clinical trials comparing the long-term results of operative and nonoperative treatment of acute patellar dislocation in children and adolescents. Thus, we were compelled to make assumptions when calculating the sample-size requirement with use of the accepted standards for study power
(80%) and type-I error ( a = 0.05). The sample-size requirement was evaluated for both continuous outcomes (e.g., the
Kujala score) and categorical outcomes (e.g., the redislocation rate). This calculation may, however, underestimate the sample size requirement since the redislocation rates were much higher than anticipated. The assumptions were based on previous studies, especially for the operative group 26,27 . However, the study groups were very similar in terms of both Kujala scores and redislocation rates, without any trends, which may indicate that the conclusion would not be different with a considerably larger sample size.
The present study had some weaknesses. We randomized sixty-four of the seventy-four knees in the present study according to the year of birth of the patient. This method of randomization is suboptimal, but it was chosen in order to avoid treating the two limbs differently in patients with bilateral involvement. The surgical methods used in the present study can be criticized as not being current. Repair of the torn medial stabilizing soft-tissue structures by means of direct suturing in a dysplastic patellofemoral joint does not improve patellar stability 24 . Furthermore, lateral release is not advocated for the treatment of patellar instability 28,29 as it was in the early
1990s 3 . Currently, acute patellar dislocation is treated nonoperatively in our hospital, except in patients with an osteochondral fracture requiring surgical repair. Surgical treatment is considered for patients with recurrent patellar dislocation, with reconstruction of the medial patellofemoral and patellotibial ligaments being the most common option. Nevertheless, the present study provides valuable information about the prognosis of an acute patellar dislocation in children and adolescents.
To our knowledge, the subjective results of treatment have not previously been reported in a pediatric population.
However, the subjective results in a mixed-aged population have varied, with 60% to 93% patients reporting satisfaction with the result 26,27,30-32 . Hvass et al.
33 reported that patient dissatisfaction did not correlate with redislocation, although
Harilainen and Sandelin 32 contradicted that opinion. The majority of our patients were satisfied with their knees in early adulthood (after a mean of fourteen years of follow-up). The method of treatment, any associated joint surface damage, and recurrent patellar instability did not affect patient satisfaction in the present study. However, our patients with satisfactory subjective outcomes had better functional scores.
McManus et al.
13 suggested that, after an acute patellar dislocation, every sixth child would have a recurrence. However, other investigators have emphasized that the risk of recurrence seems to be especially high in growing patients, with redislocation rates of as high as 60% having been documented for pediatric patients 1,6,17 . The results of the present study, with a redislocation rate of 69% and a recurrent patellar instability rate of 91%, confirm that recurrent instability is very common in pediatric patients. Of particular interest is that the rate of recurrent patellar dislocation was not reduced by primary surgical repair. Most of the first redislocations occurred within two years after the primary dislocation, and most patients with redislocation had more than one redislocation. This clinical information is useful for advising and managing pediatric patients who have an acute patellar dislocation.
Radiographic measurements at the time of acute patellar dislocation did not have prognostic value for the recurrence of patellar instability, a finding that is logical because the majority of our patients had dysplastic changes affecting the patellofemoral joint as demonstrated by the patellar height and the sulcus angle. Similar radiographic findings have been reported previously in skeletally immature patients 13,17 . We noted that patella alta and a shallow femoral sulcus were more common in patients with more than three episodes of recurrent patellar dislocation as compared with those with three redislocations or fewer. Furthermore, a positive family history was a risk factor for recurrent patellar dislocation in the affected knee and for acute patellar dislocation in the contralateral knee.
Previous studies have demonstrated that female gender is a risk factor for a poor prognosis 2,8,9,34 . The present study supports this finding as the functional scores were clearly better at the time of final follow-up in male patients than in female patients.
The functional outcome in early adulthood following an acute patellar dislocation sustained during the growing period has not been previously reported, to our knowledge. In our study, the Kujala score correlated better with the subjective result and the recurrence of patellar dislocation than the
Hughston visual analog score did. In the original study by
Kujala et al.
22 , the mean Kujala score was 100 in adults without knee symptoms, 83 in patients with anterior knee pain, 68 in patients with patellar subluxation, and 62 in patients with recurrent patellar dislocation. Deie et al.
28 reported a Kujala score of >90 in forty-three surgically treated patients with a mean age of nineteen years (range, six to forty-three years) who had acute patellar dislocation, recurrent patellar dislocation, or an unstable patella. The Kujala scores for our patients were better than those for the surgically managed patients with patellar dislocation or subluxation in the report by Kujala et al.
22 . However, the scores in the present study were worse than those in the report by Deie et al.
28 , which included a mixed-age patient population with a ten-year follow-up. In our study, the functional outcome could not be improved by primary repair of the injured medial retinacular structures, so our original hypothesis was proven to be wrong.
To our knowledge, the activity level of pediatric patients with acute patellar dislocation has not been previously evaluated with use of the Tegner activity score. Half of our patients either improved or stayed at their pre-injury activity level, whereas the other half reported a decrease in their activity. Part of the decrease in Tegner activity scores may be explained by the fact that, in Finland, children and adolescents generally are
T H E J O U R N A L O F B O N E & J O I N T S U R G E R Y d
J B J S
.
O R G
V O L U M E 9 0 - A d
N U M B E R 3 d
M
A R C H 2 0 0 8
470
A C U T E P AT E L L A R D I S L O C AT I O N I N C H I L D R E N A N D A D O L E S C E N T S :
A R A N D O M I Z E D C L I N I C A L T R I A L more active in sports and participate in competitive sports more frequently than adults do 35 . It is clinically helpful to know that an acute patellar dislocation sustained during the growing period may not necessarily affect the activity level in early adulthood.
Despite a very high rate of recurrence, the majority of young adults who sustained an acute patellar dislocation during the growth period were satisfied with their knee function.
Patients with a positive family history had more pronounced dysplasia of the patellofemoral joint, leading to a higher rate of bilateral recurrent instability. The functional outcome in patients with acute patellar dislocation correlated with the subjective result but not with the presence of recurrent patellar instability. Primary repair of the torn medial retinacular structures in patients with acute patellar dislocation did not improve the long-term subjective or functional results. Therefore, this surgical approach cannot be recommended for a pediatric patient with an acute patellar dislocation.
n
Sauli Palmu, BM
Rakuunantie 18 A 21, FIN-00330 Helsinki, Finland.
E-mail: sauli.palmu@helsinki.fi
Pentti E. Kallio, MD, PhD
Ilkka Helenius, MD, PhD
Yrj¨an¨a Nietosvaara, MD, PhD
Children’s Hospital, Helsinki University Central Hospital,
Stenb¨ackinkatu 11, FIN-00290 Helsinki, Finland
Simon T. Donell, FRCS(Orth), MD
Institute of Health, University of East Anglia, Norwich,
NR4 7TJ, United Kingdom
References
1.
Beasley LS, Vidal AF. Traumatic patellar dislocation in children and adolescents: treatment update and literature review. Curr Opin Pediatr. 2004;16:29-36.
2.
Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14:513-5.
3.
V¨ asarja V, Kinnunen P, Lanning P, Serlo W. Operative realignment of patellar malalignment in children. J Pediatr Orthop. 1995;15:281-5.
4.
Brattstr¨ location of patella. A clinical and x-ray-anatomical investigation. Acta Orthop Scand
Suppl. 1964;68:1-148.
5.
R¨ alized joint laxity and anatomy of the patellar articulation. Acta Orthop Scand Suppl.
1983;201:1-53.
6.
Cash JD, Hughston JC. Treatment of acute patellar dislocation. Am J Sports
Med. 1988;16:244-9.
7.
Buchner M, Baudendistel B, Sabo D, Schmitt H. Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment.
Clin J Sport Med. 2005;15:62-6.
8.
Nikku R, Nietosvaara Y, Aalto K, Kallio P. Operative treatment of primary patellar dislocation does not improve medium-term outcome. A 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop. 2005;76:699-704.
9.
Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19-26.
10.
Vainionp¨ a S, Laasonen E, Silvennoinen T, Vasenius J, Rokkanen P. Acute dislocation of the patella. A prospective review of operative treatment. J Bone Joint
Surg Br. 1990;72:366-9.
11.
M¨ operative management in 100 patients. Am J Sports Med. 1997;25:213-7.
12.
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, White LM.
Epidemiology and natural history of acute patellar dislocation. Am J Sports Med.
2004;32:1114-21.
13.
McManus F, Rang M, Heslin DJ. Acute dislocation of the patella in children.
The natural history. Clin Orthop Relat Res. 1979;139:88-91.
14.
Laurin CA, Dussault R, Levesque HP. The tangential x-ray investigation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation.
Clin Orthop Relat Res. 1979;144:16-26.
15.
Jacobsen K, Bertheussen K. The vertical location of the patella. Fundamental views on the concept patella alta, using a normal sample. Acta Orthop Scand.
1974;45:436-45.
16.
Larsen E, Lauridsen F. Conservative treatment of patellar dislocations. Influence of evident factors on the tendency to redislocation and the therapeutic result.
Clin Orthop Relat Res. 1982;171:131-6.
17.
Insall J, Salvati E. Patella position in the normal knee joint. Radiology.
1971;101:101-4.
18.
Insall J, Goldberg V, Salvati E. Recurrent dislocation and the high-riding patella.
Clin Orthop Relat Res. 1972;88:67-9.
19.
Baumgartl F. Fehlentwicklungen der tibialen Patellarfacette. In: Baumgartl F, editor. Das Kniegelenk. Berlin: Springer; 1964. p 276-85. German.
20.
Carson WG Jr, James SL, Larson RL, Singer KM, Winternitz WW. Patellofemoral disorders: physical and radiographic evaluation. Part II: radiographic examination.
Clin Orthop Relat Res. 1984;185:178-86.
21.
Flandry F, Hunt JP, Terry GC, Hughston JC. Analysis of subjective knee complaints using visual analog scales. Am J Sports Med. 1991;19:112-8.
22.
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O.
Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159-63.
23.
Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43-9.
24.
Nietosvaara Y. Acute patellar dislocation in children and adolescents
[dissertation]. Helsinki: University of Helsinki; 1996.
25.
Nikku R, Nietosvaara Y, Kallio PE, Aalto K, Michelsson JE. Operative versus closed treatment of primary dislocation of the patella. Similar 2-year results in 125 randomized patients. Acta Orthop Scand. 1997;68:419-23.
26.
Harilainen A, Myllynen P. Operative treatment in acute patellar dislocation.
Radiological predisposing factors, diagnosis, and results. Am J Knee Surg.
1988;1:178-85.
27.
Vainionp¨ a S, Laasonen E, Silvennoinen T, Vasenius J, Rokkanen P. Acute dislocation of the patella. A prospective review of operative treatment. J Bone Joint
Surg Br. 1990;72:366-9.
28.
Deie M, Ochi M, Sumen Y, Adachi N, Kobayashi K, Yasumoto M. A long-term follow-up study after medial patellofemoral ligament reconstruction using the transferred semitendinosus tendon for patellar dislocation. Knee Surg Sports
Traumatol Arthrosc. 2005;13:522-8.
29.
Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation.
Clin Sports Med. 2002;21:499-519.
30.
Cofield RH, Bryan RS. Acute dislocation of the patella: results of conservative treatment. J Bone Joint Surg Br. 1948;30:153-7.
31.
Boring TH, O’Donoghue DH. Acute patellar dislocation: results of immediate surgical repair. Clin Orthop Relat Res. 1978;136:182-5.
32.
Harilainen A, Sandelin J. Prospective long-term results of operative treatment in primary dislocation of the patella. Knee Surg Sports Traumatol Arthrosc.
1993;1:100-3.
33.
Hvass I, Johnsen F, Frandsen PA. Conservative treatment of patellar dislocation. Acta Orthop Scand. 1988;59:739-47.
34.
Letts RM, Davidson D, Beaule P. Semitendinosus tenodesis for repair of recurrent dislocation of the patella in children. J Pediatr Orthop. 1999;19:742-7.
35.
National Sport Survey 2005-2006. Finnish Sports Federation; 2006.