Balance Measures for Discriminating between
advertisement

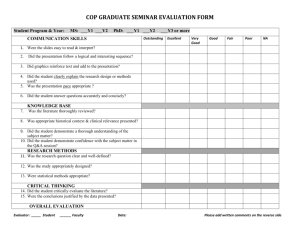
Balance Measures for Discriminating between Functionally Unstable and Stable Ankles 2 2 2 SCOTT E. ROSS', KEVIN M. GUSKIEWICZ , MICHAEL T. GROSS , and BING YU 'Virginia Commonwealth University, Richmond, VA; and 2 Universitv of North Carolina, Chapel Hill, NC ABSTRACT ROSS, S. E., K. M. GUSKIEWICZ, M. T. GROSS, and B. YU. Balance Measures for Discriminating between Functionally Unstable and Stable Ankles. Med. Sci. Sports Exerc., Vol. 41, No. 2, pp. 399-407, 2009. Purpose: To identify force plate measures that discriminate between ankles with functional instability and stable ankles and to determine the most accurate force plate measure for enabling this distinction. Methods: Twenty-two subjects (177 + 10 cm, 77 ± 16 kg, 21 ± 2 yr) without a history of ankle injury and 22 subjects (177 + 10 cm, 77 + 16 kg, 20 ± 2 yr) with functional ankle instability (FAI) performed a single-leg static balance test and a single-leg jump-landing dynamic balance test. Static force plate measures analyzed in both anterior/posterior (A/P) and medial/lateral (M/L) directions included the following: ground reaction force (GRF) SD; center-of-pressure (COP) SD; mean, maximum, and total COP excursion; and mean and maximum COP velocity. COP area was also analyzed for static balance. A/P and M/L time to stabilization quantified dynamic balance. Greater values of force plate measures indicated impaired balance. A stepwise discriminant function analysis examined group differences, group classification, and accuracy of force plate measures for discriminating between ankle groups. Results: The FAI group had greater values than the stable ankle group for A/P GRF SD (P 0.027), M/L GRF SD (P = 0.006), M/L COP SD (P = 0.046), A/P mean COP velocity (P = 0.015), M/L mean COP velocity (P 0.016), A/P maximum COP velocity (P = 0.037), M/L mean COP excursion (P = 0.014), M/L total COP excursion (P = 0.016), A/P time to stabilization (P = 0.011), and M/L time to stabilization (P = 0.040). M/L GRF SD and A/P time to stabilization had the greatest accuracy scores of 0.73 and 0.72, respectively. Conclusion: Although 10 measures identified group differences, M/L GRF SD and A/P time to stabilization were the most accurate in discriminating between ankle groups. These results provide evidence for choosing these GRF measures for evaluating static and dynamic balance deficits associated with FAI. Key Words: CHRONIC INSTABILITY, CENTER OF PRESSURE, FORCE PLATE, FUNCTIONAL INSTABILITY, POSTURE, STABILITY Freeman et al. (10,11) originally proposed ligament deafferentation as a causal factor of FAL. The damaged ankle ligament sensory receptors were thought to disrupt sensorimotor function by diminishing proprioceptive messages related to joint movement and position to afferent pathways. The resulting proprioceptive deficits could also lead to diminished postural reflex responses and consequently contribute to balance deficits. Thus, sensorimotor deficits were one potential contributing factor to recurrent ankle sprains (10,11). Although Freeman et al. (10,11) used single-leg Romberg tests to identify balance impairments, other researchers have used instrumented force plates to identify balance deficits associated with ankle instability (2,6,7,12,14,16,18,20,21, 23-26,35,37,38). Center-of-pressure (COP) force plate measures and ground reaction force (GRF) measures that have been used to quantify balance in the ankle instability literature included the following: COP SD; mean, maximum, and total COP excursion; COP velocity; COP area; and ground reaction force (GRF) SD (2,6,7,12,14,16,18, 20,21,23-26,35,37,38). In our review of literature, we found that 55% of static force plate measures used in research studies detected balance deficits in subjects with ankle instability (2,6,7,12,14,16,18,20,21,23-26,35,37,38). among physically active individuals (13,33). Approxinjuries theoflateral ligaments of the ankle are common mately to 25% all injuries in athletics are ankle sprains, and 85% of these injuries involve lateral ligament sprains (13). A functional instability at the ankle joint might persist after initial injury, and anywhere from 30% to 78% of injured individuals may suffer recurrent sprains (1,3,10,11, 31,34,36). Although the exact casual factor is unknown, functional ankle instability (FAI) is believed to occur from a combination of mechanical instability, ankle strength deficits, and ligament deafferentation (10,11,21). Address for correspondence: Scott E. Ross, Ph.D., ATC, Department of Health and Human Performance, Virginia Commonwealth University, PO Box 842020, 1015 W. Main St., Richmond, VA 23284-2020; E-mail: seross@vcu.edu. Submitted for publication January 2008. Accepted for publication July 2008. 0195-9131/09/4102-0399/0 MEDICINE & SCIENCE IN SPORTS & EXERCISE8 Copyright © 2009 by the American College of Sports Medicine DOI: 10.1249/MSS.0b013e3181872d89 399 Some researchers have reported greater COP excursions and greater GRF SD in ankles with functional instability compared with stable ankles,(14,18,21,23,37,38), and others have reported contrary results (2,14,18,20,24,26). Thus, this discrepancy suggests that selected force plate measures may be more sensitive than others at discriminating between ankles with functional instability and stable ankles. Although balance deficits can exist with single-leg stance, the functionality of this test has been questioned (26). Dynamic single-leg hopping tests that challenge postural control greater than single-leg stance have been recommended as alternative assessment techniques to single-leg static balance tests (26). Anterior/posterior (A/P) and medial/lateral (M/L) time to stabilization force plate measures have been used to evaluate single-leg jump-landing dynamic balance of subjects with FAI (4,26-28,39). Subjects with FAI take longer to stabilize than subjects with stable ankles after a single-leg jump landing (4,26-28,39). This stabilization measure has been theorized to have greater sensitivity than static measures for discriminating between ankles with functional instability and stable ankles (26,27). The sensitivity of static and dynamic force plate measures for discriminating between ankles with functional instability and stable ankles has not been established. Determining force plate measures that accurately discriminate between ankles with functional instability and stable ankles might assist researchers in identifying balance impairments that might otherwise go undetected with less accurate measures. Therefore, the objectives of this study were 1) to identify force plate measures that discriminate between ankles with functional instability and stable ankles and 2) to determine the most accurate force plate measure for enabling this distinction between ankles with functional instability and stable ankles. The identification of these force plate measures might assist researchers in detecting individuals at risk for sprains or help researchers determine the efficacy of an injury prevention program. signs and symptoms of injury included pain, loss of function, mild point tenderness, swelling, and abnormal range of motion. Subjects with stable ankles with a history of ankle sprain injury were excluded from this study. Informed written consent was obtained from all subjects before participation in this study. The Committee for the Protection of the Rights of Human Subjects granted approval for this project. All subjects completed the Ankle Joint Functional Assessment Tool to assess ankle stability (30). Possible scores on this instrument range from 0 to 48, and greater scores indicate greater functional instability. A certified athletic trainer (SER) tested the subjects' ankle laxity by performing the anterior drawer and talar tilt orthopedic tests before balance testing. Single-leg balance test. Subjects were instructed to remain as motionless as possible while standing with their test leg on a force plate. Subjects kept their eyes open, their hands on their hips, and their non-weight-bearing leg slightly flexed at the hip and knee. The weight-bearing leg was slightly flexed at the knee, and the foot was in a neutral toe in/ out position with the tips of their shoes pointed straight ahead. All subjects wore athletic shoes during testing; however, we did not control for the type of athletic shoes. Our rationale for testing subjects while wearing athletic shoes was to keep contact surfaces consistent between static and dynamic tests. Additionally, this single-leg balance protocol has been used in previous ankle instability studies (28,29). Subjects performed one 10-s practice trial, followed by three 20-s testing trials. Subjects rested 20 s between each trial. Trials were repeated TABLE 1. Charateristics of subjects with and without FAI Dominant test limb, n Nondominant test limb, n Height (cm), mean (SD) Weight (kg), mean (SD) Age (yr), mean (SD) Sprains in the past year Stable Ankle Group (10 males, 12 females) FAIGroup (10 males, 12 females) 13 9 177 (10) 77 (16) 21 (2) Number ofSubjects No subjects reported a history of ankle sprain injury. 13 9 177 (10) 77 (16) 21 (2) Number of Number of Sprains Subjects 2 8 3 4 4 3 5 1 6 1 7 2 1 9 10 2 Number of Number of Give Ways Subjects 2 1 3 1 4 4 5 2 7 3 10 2 15 5 20 4 Number of Give Ways Drawer Talar Tilt 11 12 11 10 33.05 (4.02) METHODS Subjects. Subject characteristics are reported in Table 1. Twenty-two control subjects with stable ankles were matched by height, mass, age, sex, and leg tested to 22 subjects with clinically diagnosed FAI. Subjects with stable ankles were tested on the same leg (dominant or nondominant) as their match. Dominance was defined as the preferred leg used to kick a ball. Inclusion criteria for FAI included 1) self-report of a history of one sprain followed by at least 3 d of immobilization and 2) self-report of at least two ankle sprains and at least two episodes of "giving way" sensations during physical activity within the year before the subjects' enrollment in this study. Potential subjects were excluded if they displayed acute signs and symptoms of injury or reported an ankle sprain within 6 wk before their participation in the study. Acute 400 Official Journal of the American College of Sports Medicine Giving way sensalions the past year Special Test Positive Positive AJFAT score, mean (SD) Number of Subjects No subjects reports reported a history of giving way sensations. Number of Subjects Drawer Talar Tilt 4 4 18 18 22.60 (1 22) AJFAT, Ankle Joint Functionsal Assessment Tool, http://www.acsm-msse.org TABLE 2. Definitions of force plate measures. Measure Definition GRF SD Overall SD of the GRF in a given direction in a given time for a given number of trials Overall SD of the COP in a given direction in a given time for a given number of trials The absolute averaged distance between the instantaneous COP and the average COP position in a given direction during a given time The absolute maximum distance between the instantaneous COP position and the average COP position during a given period The absolute length of the path movements over the testing period The absolute mean value of the instantaneous velocity of the COP in a given direction during a given period The absolute maximum value of the instantaneous velocity of the COP in a given direction during a given period A rectangular area defined by the maximum anterior, posterior, medial, and lateral sways during a given time Time needed to reduce the variation of a smoothed GRF to the range of vibration of the corresponding component of the GRF in a stabilized single-leg stance of individuals with stable ankles COP SD Mean COP excursion Maximum COP excursion Total COP excursion Mean COP velocity Maximum COP velocity COP area Time to stabilization GRF, ground reaction force; COP, center of pressure. if subjects hopped on the weight-bearing leg or touched down with the non-weight-bearing leg. Single-leg jump landing. Methods for performing single-leg jump-landing tests have been described in previous reports (26-28). First, subjects performed maximum standing reach while standing flat footed directly underneath a Vertec (Sports Imports, Columbus, OH) by flexing their shoulders to 180' and touching the highest plastic rod that they could reach with the distal end of their fingers. The Vertec has adjustable plastic rods set at different heights that permit maximum reach and jump height assessments. Subjects were then assessed for maximum vertical jump height as they stood on the floor 70 cm away from a Vertec. Three maximum vertical jump heights were assessed while subjects jumped using a bilateral foot takeoff technique. Subjects were allowed to swing their arms while they jumped off of the floor. Then, subjects flexed their shoulders to 180' and fully extended their elbows, touched the highest plastic rod that they could reach with the distal end of their fingers, and then landed on both feet on the floor. The greatest jump height of the three vertical jumps for each subject was recorded and then subtracted from their respective maximum standing reach. Thus, the difference between maximum vertical jump height and maximum standing reach was recorded as the true maximum jump. Next, the plastic rods on the Vertec were placed in line with the center of a force plate, and the plastic rods were then set between 50% and 55% of subjects' true maximum jump. Subjects stood on the floor 70 cm away from the center of the force plate and performed a jump using a bilateral foot takeoff technique. Again, subjects were allowed to swing their arms while they jumped off of the floor. However, subjects were required to reach with their shoulder flexed at 180' and elbow fully extended after take off. The reaching arm was the ipsilateral arm of the ankle with functional instability or the matched testing ankle of subjects with stable ankles. As subjects jumped vertically, they touched the plastic rods between 50% and 55% of their maximum jump with the distal end of their fingers, and then they landed on a single leg (their test leg) on a force plate. Subjects were instructed to stabilize as quickly as possible and remain as motionless as possible in single-leg stance for 20 s. Three practice trials and seven testing trials were performed with 30 s of rest between trials. Trials were repeated if subjects failed to jump within the 50-55% range, hopped on the test leg, or touched down with the non-weight-bearing leg. Data collection and reduction. A Bertec force plate model number 4060-08A (Bertec Corp., Columbus, OH) collected GRF data at a sampling rate of 180 Hz (4,26-28). Analog signals were amplified with a Bertec amplifier (AM6701). Signals were then passed through a BNC adapter chassis that was interfaced with an analog-to-digital board within a personal computer. MotionSoft Balance Assessment TABLE 3. Mean + SO and ES for force plate measure analyses. Force Plate A/P GRF SO M/L GRF SD A/P COP SD (cm) M/L COP SD (cm) A/P mean COP excursion (cm) M/L mean COP excursion (cm) A/P maximum COP excursion (cm) M/L maximum COP excursion (cm) A/P total COP excursion (cm) M/L total COP excursion (cm) A/P mean COP velocity (cm.s-1) M/L mean COP velocity (cm.s-1) A/P maximum COP velocity (cm.s-1) M/L maximum COP velocity (cm.s-1) 2 COP area (cm ) A/P time to stabilization (s) M/L time to stabilization (s) FAl 0.45 0.54 1.01 0.73 0.80 0.60 3.01 2.02 63.61 64.63 3.17 3.23 24.99 21.53 0.21 1.86 2.09 ± ± ± ± ± ± ± ± ± ± ± ± + ± 0.18a 0.22a 0.38 0.19 0.30 0.15 1.32 0.52 20.03 15.89 1.00 0.80 15.81 7.93 ±0.14 ± 0.67 ± 0.80 Stable Ankle ES 0.35 0.39 0.85 0.64 0.67 0.51 2.41 0.72 0.92 0.54 0.60 0.57 0.71 0.60 0.46 0.58 0.75 0.76 0.75 0.65 0.54 0.60 0.80 0.62 + 0.08a ± 0.07' ± 0.18 + 0.10 ± 0.12 + 0.10 ± 0.52 1.82 ± 0.33 54.16 ± 11.00 54.88 ± 9.03 2.59 ± 0.39 2.74 ± 0.45 17.48 ± 4.24 18.07 ± 3.47 0.15 + 0.01 1.44 ± 0.33 1.70 ± 0.38 .A, F(1 , 42), Pvalue A = 0.90, A = 0.84, A = 0.93, A = 0.91, A = 0.92, A = 0.87, A = 0.92, A = 0.95, A = 0.92, A = 0.87, A = 0.87, A = 0.87, A = 0.90, A = 0.92, A = 0.92, A = 0.86, A = 0.90, F(1,42)= 5.24, F(1,42)= 8.23, F(1 ,42 ) = 3.26, F(1,42 ) = 4.24, F(1,42) = 3.72, F(1,421 = 6.51, F(1,42)= 3.92, F(I.42) = 2.23, F(I 42 ) = 3.76, F(1 . 42 ) = 6.27, F(1,42)= 6.45, F(1.42 ) = 6.29, F(1.42 ) = 4.62, F(1i42)= 3.53, F(1,42)= 3.82, P = 0.027* P = 0.006* P = 0.078 P = 0.046* P = 0.061 P = 0.014* P = 0.054 P = 0.143 P= 0.060 P = 0.016* P = 0.015* P = 0.016* P = 0.037* P = 0.067 P = 0.057 F(142) = 7.03, P= 0.011* F(1,42i= 4.49, P = 0.040' GRF SD for A/P and M/L measures were divided by body weight (N) and multiplied by 100. Statistical significance (P< 0.05). AJP,anterior/posterior; M/L, medial/lateral; COP, center of pressure; GRF, ground reaction force: ES, effect size; A, Wilks' Lambda. DISCRIMINATING UNSTABLE AND STABLE ANKLES Medicine & Science in Sports & Exercisee 401 GRF Standard Deviation COP Standard Deviation 10.9 0.9 0.8- -7 0.8- 0.7 - 0.7- S0.6- 0.6 0.5. 0.5 ~0.4- 040.30.2 7/ 0.10 0.3- -AllP 7 - - - - 0.20.1- Di.g 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1-Specificity Diagonal -- -- 0 1 AIP - 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1-Specificity 1 FIGURE 1-ROC curves for ground reaction force (GRF) SD. Anterior/posterior (A/P) GRF SD and medial/lateral (M/L) GRF SD discriminated between ankle groups. However, M/L GRF SD had greater accuracy than A/P GRF SD in discriminating between ankle groups. The diagonal dotted black line divides the area of the graphs into the upper and lower 50%. FIGURE 2-ROC curves for center-of-pressure (COP) SD. Neither anterior/posterior (AIP) COP SD nor medial/lateral (M/L) COP SD were accurate in discriminating between ankle groups. The diagonal dotted black line divides the area of the graphs into the upper and lower 50%. computer software package version 2.0 (MotionSoft Inc., Chapel Hill, NC) converted digital data to GRF vectors. Data were filtered using a second-order recursive low-pass Butterworth digital filter with an estimated optimum cutoff frequency of 12.53 Hz (4,26-28). Table 2 presents definitions of static and dynamic force plate measures calculated to evaluate balance. Static force plate measures analyzed in both anterior/posterior (A/P) and medial/lateral (MWL) directions included the following: GRF SD; COP SD; mean, maximum, and total COP excursion; and mean and maximum COP velocity. COP area was also analyzed for static balance. A/P and M/L time to stabilization examined dynamic balance and were calculated using the vibration magnitude curve fitting technique (27,28). Greater magnitudes of force plate measures were indicative of impaired balance. Statistical analysis. A stepwise discriminant function analysis determined 1) the force plate measure differences between groups with univariate F-tests; 2) the percentage of subjects with FAI and subjects with stable ankles that were correctly classified as having FAI or stable ankles, respectively; and 3) the force plate measures that accurately discriminated between ankle groups. Effect size (ES) values were calculated using Cohen's (5) ES d to indicate the degree of differences between ankle groups on univariate F-tests. Cohen (5) defines low, medium, and high ES as 0.30, 0.50, and 0.80, respectively. The stepwise discriminant analysis regressed force plate measures on group membership. In other words, this analysis determined force plate measures that predicted group membership. Thus, force plate measures that predicted group membership were accurate at distinguishing between ankle groups. Additionally, the percentage of individuals classified correctly as having ankles with functional instability or stable ankles was identified with the discriminant analysis. Accuracy values for discriminating between groups were determined by calculating the area under the curve (AUC) for receiver operating characteristic (ROC) curves. ROC curves plot sensitivity (true-positive rate) versus 1-speficity (false-positive rate), describing how sensitivity and false-positive rate vary together. The full area under the ROC curve was used as an index to classify the accuracy of force plate measures. Perfect accuracy is indicated by an AUC of 1.0, whereas a no apparent accuracy is indicated by an AUC of less than or equal to 0.50 (17,22). Thus, force plate measures were more accurate at discriminating between ankle groups as AUC values approached 1.0. A traditional academic point scale was used to classify the accuracy of the AUC for discriminating between ankle groups with force plate measures (0.90-1.00 = "excellent"; 0.80-0.89 = "good"; 0.70-0.79 "fair"; 0.60-0.69 = "poor"; and 0.50-0.59 = "fail") (17,22). SPSS version 13.0 (SPSS, Inc., Chicago, IL) was used for statistical analyses. The alpha and the asymptotic 402 Official Journal of the American College of Sports Medicine Mean COP Excursion 1 0.9 0.8 0.7 06 0.5 0.4 0.3 0.2 --- - 0.1 A/P Diagonal _MtL 0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1 1-Specificity FIGURE 3-ROC curves for mean center-of-pressure (COP) excursion. Medial/lateral (M/L) mean COP excursion accurately discriminated between ankle groups, whereas anterior/posterior (A/P) mean COP excursion did not. M/L mean COP excursion had greater accuracy than A/P mean COP excursion in discriminating between ankle groups. The diagonal dotted black line divides the area of the graphs into the upper and lower 50%. http://www.acsm-msse.org Maximum COP Excursion Mean COP Velocity 1,- I1- 0.9- 7 0.9. 0.8- 0.80.7- 0.7, 0.60.5- 0.4 0.3 7 7 7 S0.6- 7 0.5- "00.4S0.3- AIP 02///0.11 - - - - 0.2- Diagonal 0 , 7/ Z AI/P Diagonal 0.1- -MIL , U // MI L i 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1 0 1-Specificity 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1 1-Specificity FIGURE 4-ROC curves for maximum center-of-pressure (COP) excursion. Neither anterior/posterior (A/P) maximum COP excursion nor medial/lateral (M/L) maximum COP excursion were accurate in discriminating between ankle groups. The diagonal dotted black line divides the area of the graphs into the upper and lower 50%. levels were set a priori at P < 0.05 to indicate statistical significance. FIGURE 6-ROC curves for mean center-of-pressure (COP) velocity. Anterior/posterior (A/P) mean COP velocity and medial/lateral (M/L) mean COP velocity discriminated between ankle groups. However, M/L mean COP velocity had greater accuracy than A/P mean COP velocity in discriminating between ankle groups. The diagonal dotted black line divides the area of the graphs into the upper and lower 50%. The ROC curves for static and dynamic force plate measures are presented in Figure 1 (GRF SD), Figure 2 (COP SD), Figure 3 (mean COP excursion), Figure 4 (maximum RESULTS ferences were found for A/P COP SD, A/P mean COP COP excursion), Figure 5 (total COP excursion), Figure 6 (mean COP velocity), Figure 7 (maximum COP velocity), Figure 8 (COP area), and Figure 9 (time to stabilization). Table 4 reports the percentage of subjects correctly classified into their respective groups as well as the AUC and the asymptotic significance for force plates measures. The AUC values had accuracy ratings of "fair" for A/P GRF SD, MIL GRF SD, M/L total COP excursion, M/L mean COP velocity, and A/P time to stabilization. The AUC values had ac- excursion, A/P maximum COP excursion, M/L maximum COP excursion, A/P total COP excursion, M/L maximum curacy ratings of "poor" for A/P COP SD, M/L COP SD, A/P mean COP excursion, MiL mean COP excursion, A/P max- COP velocity, or COP area. imum COP excursion, A/P total COP excursion, A/P mean Table 3 reports means + SD and ES for static and dynamic force plate measures. The FAI group had greater force plate values than the stable ankle group for A/P GRF SD, MIL GRF SD, M/L COP SD, M/L mean COP excursion, M/L total COP excursion, A/P mean COP velocity, M/L mean COP velocity, A/P maximum COP velocity, A/P time to stabilization, and M/L time to stabilization. No group dif- r r Q L IF Total COP Excursion rr L Maximum COP Velocity 0.9 0 "1l 0.8 0.7- 0.7 0.61 .•0.6 7/ 0.5 M/L 0.4 m 0.4 S0.3 0.3- 02 020.1- ---- Diagonal 0O v 0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1-Specificity ,J 1 FIGURE 5-ROC curves for total center-of-pressure (COP) excursion. Medial/lateral (M/L) total COP excursion accurately discriminated between ankle groups, whereas anterior/posterior (A/P) total COP excursion did not. M/L total COP excursion had greater accuracy than A/P total COP excursion in discriminating between ankle groups. The diagonal dotted black line divides the area of the graphs into the upper and lower 50%. DISCRIMINATING UNSTABLE AND STABLE ANKLES 0.1 0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1-Specificity FIGURE 7-ROC curves for maximum center-of-pressure (COP) velocity. Anterior/posterior (A/P) maximum COP velocity accurately discriminated between ankle groups, whereas medial/lateral (M/L) maximum COP velocity did not. A/P maximum COP velocity had greater accuracy than M/L maximum COP velocity in discriminating between ankle groups. The diagonal dotted black line divides the area of the graphs into the upper and lower 50%. Medicine & Science in Sports & Exercisea 403 COP Area 10.90.8- /7 /////7 0.7- 7/ 7 0.60.5- 0.4- 7/ 7 0.2 0.1 0 0 Area 0.1 -/ DiegonI ." _1-_ 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1 I-Specificity FIGURE 8-ROC curve for center-of-pressure (COP) area. COP area was not accurate in discriminating between ankle groups. The diagonal dotted black line divides the area of the graphs into the upper and lower 50%. COP velocity, A/P maximum COP velocity, M/L maximum COP velocity, COP area, and M/L time to stabilization. The MJL maximum COP excursion failed to discriminate between ankle groups. Accuracy scores indicated that five force plate measures had ratings of "fair." The stepwise discriminant analysis indicated, however, that the M/L GRF SD and the A/P time to stabilization were the most accurate force plate measures for discriminating between ankle groups (Wilks' lambda (A) = 0.76, F(2 ,41) = 6.45, P = 0.004). Furthermore, the stepwise discriminant analysis indicated that the M/L GRF SD slightly out performed A/P time to stabilization for discriminating between ankle groups (Wilks' lambda (A) 0.84, F(1,42) = 8.23, P = 0.006). DISCUSSION Although 10 force plate measures identified group differences, the M/L GRF SD and the A/P time to stabilization were Time -To-Stabilization 1 0.9, 0.8. 0.70.6 - 0.5 0.4 0.3 A/P 0.2 0.2- I-Specificity FIGURE 9-ROC curves for time to stabilization. Anterior/posterior (A/P) time to stabilization accurately discriminated between ankle groups, whereas medial/lateral (M/L) time to stabilization did not. A/P time to stabilization had greater accuracy than M/L time to stabilization in discriminating between ankle groups. The diagonal dotted black line divides the area of the graphs into the upper and lower 50%. 404 Official Journal of the American College of Sports Medicine TABLE 4. Discriminant accuracy for force plate measures. % Correctly Force Plate Classified AUC A/P GRF SO M/L GRF SO A/P COP SO M/L COP SD A/P mean COP excursion M/L mean COP excursion A/P maximum COP excursion M/L maximum COP excursion A/P total COP excursion M/L total COP excursion N/P mean COP velocity M/L mean COP velocity A/P maximum COP velocity M/L maximum COP velocity COP area A/P time to stabilization M/L time to stabilization 65.9 682 59.1 59.1 56.8 56.8 54.5 47.7 63.6 65.9 61.4 65.9 61.4 56.8 56.8 61.4 54.5 0.70 0.73 0.62 0.64 0.65 0.69 0.60 0.57 0.63 0.70 0.68 0.70 0.67 0.63 0.60 0.72 0.64 Asymptotic Significance 0.021 0.011* 0.185 0.110 0.080 0.034* 0.755 0.439 0.133 0.024* 0.038* 0.024* 0.050* 0.156 0.296 0.012* 0.121 Statistical significance (P _<0.05). A/P, anterior/posterior; M/L, medial/lateral; COP, center of pressure; GRF, ground reaction force. the most accurate force plate measures for discriminating between ankle groups. However, accuracy scores indicated that M/L GRF SD performed slightly better than A/P time to stabilization at discriminating between ankle groups. These results provide evidence for choosing M/L GRF SD and A/P time to stabilization as primary force plate measures for evaluating static and dynamic balance deficits associated with FAI, respectively. These static and dynamic force plate measures might assist researchers in detecting balance impairments that might otherwise go undetected during static or dynamic single-leg balance tests with less accurate measures. Additionally, M/L GRF SD and A/P time to stabilization measures might help researchers in detecting individuals at risk for sprains or help researchers determine the efficacy of an injury prevention program. Although less accurate than M/L GRF SD, A/P GRF SD and several COP measures detected static balance impairments associated with FAL. Our significant COP force plate measures for detecting ankle group differences indicate that subjects with FAI swayed excessively and quickly compared with subjects with stable ankles. Swaying quickly is associated with greater accelerations of the center of mass, which was quantified in the GRF SD force plate measures. Thus, greater A/P GRF SD and M/L GRF SD resulting from greater GRF indicates that subjects with FAI had greater center of mass accelerations than subjects with stable ankles. We speculate that sensorimotor deficits associated with FAI might have impaired subjects' ability to control or to detect changes in center of mass positions. Damaged articular, musculotendinous, and cutaneous receptors associated with FAT have been purported to disrupt sensorimotor function by diminishing messages related to ankle joint movement and position to afferent pathways (10,11,19). These deficits could lead to reduced postural reflex responses and consequently diminish stabilizing moments that are important in maintaining balance. Additionally, sensorimotor deficits have been implicated in causing subjects with FAI to balance closer to http://www.acsm-msse.org their limits of stability (18). Given this significant infonnation, we speculate that sensorimotor deficits associated with FAI might have caused subjects' center of mass to accelerate to their limits of stability without adequate stabilizing moments. Furthermore, sensorimotor impairments and strength deficits associated with FAI might have also contributed to increased time to stabilization values in subjects with FAT. Evidence indicates that subjects with recurrent ankle sprains have impaired sensorimotor reflexes during dynamic balance (25). Sufficient sensorimotor reflexes are essential for controlling balance. Additionally, eccentric plantarflexion strength deficits of the foot have been associated with FAI (9). Eccentric strength of the plantarflexors is important in energy absorption after landing; however, plantarflexors of the foot have been underused in producing deceleration moments after landing (32). On the basis of this information, we hypothesize that subjects with FAI might have underused potentially weak plantarflexors of the foot after landing, impacting their ability to develop adequate deceleration moments to control their center of mass after landing. Additionally, a delay in sensorimotor reflexes might have decreased the time subjects with FAT had to develop deceleration moments to stabilize the center of mass. Consequently, muscle force requirements might have increased to produce deceleration moments in very short periods of time for subjects with FAT. Subjects with stable ankles likely had adequate muscle force to develop appropriate deceleration moments to stabilize their center of mass and lower extremity very quickly. Subjects with FAI, however, might have gone longer without adequate deceleration moments, consequently increasing stabilization times. We did not directly measure moment generation capabilities of ankle muscles in this study, and future research should explore relationships between ankle moment production, muscle activation, and time to stabilization to confirm our contention. We recommend that researchers use MJL GRF SD for static single-leg balance and A/P time to stabilization for dynamic single-leg balance to discriminate ankles with functional instability and stable ankles. This recommendation is based on our results that indicate the M/L GRF SD and the A/P time to stabilization had the greatest accuracy scores of 0.73 and 0.72, respectively. Interestingly, ES were greatest for the univariate F-tests of M/L GRF SD (0.92) and A/P time to stabilization (0.80). Thus, these high ES indicate that these measures distinguish between ankle groups. These findings are not surprising, as Goldie et al. (15) reported that the MIL GRF SD was a good predictor of single-leg balance deficits, and M/L GRF SD was greater in individuals with a history of inversion ankle sprains than individuals with stable ankles (16). Additionally, A/P time to stabilization has consistently detected differences between ankles with functional instability and stable ankles (4,26-28,39). Using these two force plate measures might help researchers detect balance impairments associated with FAT. DISCRIMINATING UNSTABLE AND STABLE ANKLES Additional static force plate measures with slightly less accuracy than M/L GRF SD might also be used to discriminate between ankle groups. Fifteen percent (2/13) and 23% (3/13) of our traditional COP sway measures had AUC values classified as "fair" (AUC values >0.70) and "poor" (AUC between 0.67 and 0.69) with statistically significant asymptotic values, respectively. Although these significant COP measures were not better than M/L GRF SD at discriminating between ankle groups, the following static force plates measures could be additional measures included in single-leg balance assessments to discriminate between ankles with functional instability and stable ankles: 1) "fair" measures: A/P GRF SD, M/L total COP excursion, and MIL mean COP velocity; and 2) "poor" measures: M/L mean COP excursion, A/P mean COP velocity, and A/P maximum COP velocity. The remaining 62% of our static force plate measures with AUC values less than or equal to 0.66 and asymptotic values greater than 0.05 should not be used to discriminate between ankle groups. Reasons for certain COP measures being inaccurate for discriminating between ankle groups than other COP measures during static balance are not currently known. We speculate that the dimensions of the foot may have negated the effect of sensorimotor deficits associated with FAT on static balance. The long A/P dimension of the base of support allowed subjects in both ankle groups to use long excursion paths to maintain stability in the A/P direction. Additionally, our data indicate that subjects in both groups might have swayed excessively and very quickly in the short M/L base of support at some point during single-leg balance, causing maximum excursions and maximum velocity measures to lack sensitivity in discriminating between ankle groups. A/P time to stabilization might have been more accurate than M/L time to stabilization at discriminating between ankle groups as a result of the anterior jump protocol perturbing sagittal plane stability. Wikstrom et al. (40) recently reported that a lateral jump protocol increased M/L dynamic postural stability scores over an anterior jump protocol in subjects with stable ankles. A lateral jump protocol might tax frontal plane postural control more than an anterior jump protocol. We speculate, therefore, that a lateral jump protocol might increase the accuracy of M/L time to stabilization in discriminating between ankle groups. Future research should explore the accuracy of A/P and M/L time to stabilization measures in distinguishing between ankle groups with lateral jump protocols. We did not control for the type of athletic shoes worn in our study. Subjects wore running and cross-trainer athletic shoes. Differences in shoe support or soles could have affected balance and introduced variability into our data. Future research should explore the impact of different athletic shoes on our static and dynamic balance tasks. An additional limitation to our study was subject spectrum bias. Balance deficits associated with FAT could be similar to Medicine & Science in Sports & Exerciseg, 405 balance impairments associated with other ankle injuries. In the first 3 wk after an ankle sprain injury, for example, balance impairments have been present in subjects with acute ankle sprains (8). Future research should examine the accuracy of force plate measures in discriminating between ankles with functional instability, stable ankles, and other ankle pathologies. CONCLUSION The M/L GRF SD and the A/P time to stabilization accurately discriminated between ankle groups. Our results provide evidence for choosing M/L GRF SD and A/P time to stabilization as primary force plate measures for evaluating static and dynamic balance deficits associated with FAI, respectively. Other noteworthy static force plate measures that did not perform as well as M/L GRF SD and A/P time to stabilization but still accurately discriminated between ankle groups were as follows: A/P GRF SD, M/L mean COP excursion, M/L total COP excursion, A/P mean COP velocity, M/L mean COP velocity, and A/P maximum COP velocity. Traditional COP and GRF force plate measures were examined in our current study, and we recommend that future research examine the ability of other nontraditional nonlinear and spatiotemporal single-leg stance force plate measures (e.g., time to boundary, approximate entropy) or dynamic force plate measures (e.g., dynamic postural stability index) to discriminate between ankles with functional instability and stable ankles. Finally, researchers should identify ankles at risk for sprains or determine the efficacy of an injury prevention intervention program with force plate measures that discriminate between ankles with functional instability and stable ankles. The authors thank Carol Giuliani, P.T., Ph.D., and Richard G. Mynark, Ph.D., for their roles as committee members on Dr. Ross' dissertation. Manuscript preparation was supported by the Department of Health and Human Performance at Virginia Commonwealth University, Richmond, VA. Data collection for this research was conducted as part of Dr. Ross' doctoral dissertation at the University of North Carolina at Chapel Hill. Data were collected in the Sports Medicine Research Laboratory in the Department of Exercise and Sport Science at the University of North Carolina at Chapel Hill. The results of the present study do not constitute endorsement by the American College of Sports Medicine. REFERENCES I. Bahr R, Kartsen R, Lian 0, Ovrebo R. Incidence and mechanisms of acute ankle inversion injuries in volleyball: a retrospective cohort story. Am J Sports Med. 1994;22:595-600. 2. Baier M, Hopf T. Ankle orthoses effect on single-limb standing balance in athletes with functional ankle instability. Arch PhYs Med Rehabil. 1998;79:939-44. 3. Bosien W, Staples 0, Russell S. Residual disability following acute ankle sprains. JBone Joint Surg. 1955;37:1237-43. 4. Brown C, Ross S, Mynark R, Guskiewicz K. Assessing functional ankle instability with joint position sense, time to stabilization, and electromyography. J Sport Rehabil. 2004;13:122-34. 5. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale (NJ): Lawrence Erlbaum Associates; 1988. p. 274-5. 6. Cornwall M, Murrell P. Postural sway following inversion sprain of the ankle. J Am PodiatrMed Assoc. 1991;81:243-7. 7. Eils E, Rosenbaum D. A multi-station proprioception exercise program in patients with ankle instability. Med Sci Sports Exerc. 2001;33(12):1991-8. 8. Evans H, Hertel J, Sebastianelli W. Bilateral deficits in postural control following lateral ankle sprains. Foot Ankle lnt. 2004;25: 833-9. 9. Fox J, Docherty C, Schrader J, Applegate T. Eccentric planterflexor torque deficits in participants with functional ankle instability. JAthl Train. 2008;43:51-4. 10. Freeman M. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg. 1965;47:669-77. 11. Freeman M, Dean M, Hanham 1. The etiology and prevention of functional instability of the foot. J Bone Joint Surg. 1965;47B: 678-85. 12. Frid6n T, Z5tterstr6m R, Lindstrand A, Moritz U. A stabilometric technique for evaluation of lower limb instabilities. Am J Sports Med. 1989;17:118-22. 13. Garrick J, Requa R. The epidemiology of foot and ankle injuries in sports. Clin Sports Med. 1988;7:29-36. 406 Official Journal of the American College of Sports Medicine 14. Gauffin H, Tropp H, Odenrick P. Effect of ankle disk training on postural control in patients with functional instability of the ankle joint. Int J Sports Med. 1988;9:141-4. 15. Goldie P, Bach T, Evans 0. Force platform measures for evaluating postural control: reliability and validity. Arch Phys Med Rehabil. 1989;70:510-7. 16. Goldie P, Evans 0, Bach T. Postural control following inversion injuries of the ankle. Arch Phys Med Rehabil. 1994;75:969-75. 17. Hanley J, McNeil B. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982; 143:29-36. 18. Hertel J, Olnsted-Kramer L. Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait Posture. 2007;25:33-9. 19. Herel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. JAthl Train. 2002;37:364-75. 20. Isakov E, Mizrahi J. Is balance impaired by recurrent sprained ankles? Br J Sports Med. 1997;31:65-7. 21. Konradsen L, Ravn J. Prolonged peroneal reaction time in ankle instability. Ilt J Sports Med. 1991;12:290-2. 22. Lasko T, Bhagwat J, Zou K, Ohno-Machado L. The use of receiver operating characteristic curves in biomedical informatics. J Biomed Inform. 2005;38:404-15. 23. Matsusaka N, Yokoyama S, Tsurusaki T, Inokuchi S, Okita M. Effect of ankle disk training combined with tactile stimulation to the leg and foot on functional instability of the ankle. Am JSports Med. 2001;29:25-30. 24. Michell T, Ross S, Blackburn T, Hirth C, Guskiewicz K. Functional balance training, with or without exercise sandals, for subjects with stable or unstable ankles. J Athl Train. 2006;41: 393-8. 25. Perrin P, Bene M, Perrin C, Durupt D. Ankle trauma significantly impairs postural control: a study in basketball players and controls. Int J Sports Med. 1997;18:387-92. 26. Ross S, Guskiewicz K. Examination of static and dynamic http://www.acsm-msse.org 27. 28. 29. 30. 31. 32. postural stability in individuals with functionally stable and unstable ankles. Clin J Sport Med. 2004;14:332-8. Ross S, Guskiewicz K. Single-leg jump-landing stabilization times in subjects with functionally unstable ankles. J AthW Train. 2005;40:298-304. Ross S, Guskiewicz K. Effect of coordination training with and without stochastic resonance stimulation on dynamic postural stability of subjects with functional ankle instability and subjects with stable ankles. Clin J Sport Med. 2006;16:323-8. Ross S, Arnold B, Blackburn J, Brown C, Guskiewicz K. Enhanced balance associated with coordination training with stochastic resonance stimulation in subjects with functional ankle instability: an experimental trial. J Neuroeng Rehabil. 2007;4:47. Rozzi S, Lephart S, Sterner R, Kuligowski L. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29:478-86. Schaap G, de Keizer G, Marti K. Inversion trauma of the ankle. Arch Orthop Trauma Surg. 1989;108:272-ý Self B, Paine D. Ankle biomechanics during four landing techniques. Med Sci Sports Exerc. 2001;33(8):1338-44. DISCRIMINATING UNSTABLE AND STABLE ANKLES 33. Smith R, Reischl S. Treatment of ankle sprains in young athletes. Am J Sports Med. 1986;14:465-71. 34. Staples 0. Result study of ruptures of lateral ligaments of the ankle. Clin Orthop Relat Res. 1972:85:50-8. 35. Tropp H, Ekstrand J, Gillquist J. Factors affecting stabilometry recordings of single limb stance. Am J Sports Med. 1984; 12:185-8. 36. Tropp H, Askling C, Gillquist J. Prevention of ankle sprains. Am J Sports Med. 1985;13:259-62. 37. Tropp H, Odenrick P, Gillquist J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Jlt J Sports Med. 1985;6:180-2. 38. Tropp H. Pronator muscle weakness in functional instability of the ankle joint. lnt J Sports Med. 1986;7:291-4. 39. Wikstrom E, Tillman M, Borsa P. Detection of dynamic stability deficits in subjects with functional ankle instability. Med Sci Sports Exerc. 2005;37(2):169-75. 40. Wikstrom E, Tillman M, Schenker S, Borsa P. Jump-landing direction influences dynamic postural stability scores. J Sci Med Sport. 2008;11:106-11. Medicine & Science in Sports & Exercise& 407 COPYRIGHT INFORMATION TITLE: Balance Measures for Discriminating between Functionally Unstable and Stable Ankles SOURCE: Med Sci Sports Exercise 41 no2 F 2009 The magazine publisher is the copyright holder of this article and it is reproduced with permission. Further reproduction of this article in violation of the copyright is prohibited.