The American Journal of Sports Medicine
advertisement

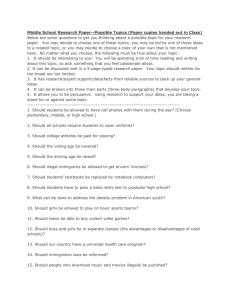
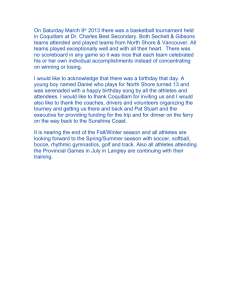
The American Journal of Sports Medicine http://ajs.sagepub.com/ The Development and Validation of a Functional Assessment Tool for the Upper Extremity in the Overhead Athlete Frank G. Alberta, Neal S. ElAttrache, Scott Bissell, Karen Mohr, Jason Browdy, Lewis Yocum and Frank Jobe Am J Sports Med 2010 38: 903 originally published online March 24, 2010 DOI: 10.1177/0363546509355642 The online version of this article can be found at: http://ajs.sagepub.com/content/38/5/903 Published by: http://www.sagepublications.com On behalf of: American Orthopaedic Society for Sports Medicine Additional services and information for The American Journal of Sports Medicine can be found at: Email Alerts: http://ajs.sagepub.com/cgi/alerts Subscriptions: http://ajs.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 7, 2010 The Development and Validation of a Functional Assessment Tool for the Upper Extremity in the Overhead Athlete *yz MD, Neal S. ElAttrache,y MD, Scott Bissell,y§ MD, Karen Mohr,y PT, Frank G. Alberta, y Jason Browdy, || MD, Lewis Yocum,y MD, and Frank Jobe,y MD From yKerlan-Jobe Orthopaedic Clinic, Los Angeles, California, zHackensack University Medical Center, Hackensack, New Jersey, §Sports Medicine Partners, Orthopedics and Rehabilitation Therapy PC, South Windsor, Connecticut, and ||Advanced Orthopaedics of Clayton, St Louis, Missouri Background: There are no validated upper extremity instruments designed specifically to evaluate the performance and function of overhead athletes. Current shoulder and elbow scoring systems may not be sensitive to subtle changes in performance in this high-demand population. Hypothesis: The scoring system developed in this study will be valid, reliable, and responsive in the evaluation of overhead athletes. Study Design: Cross-sectional study; Level of evidence, 3. Methods: Based on the results of a pilot questionnaire administered to 21 overhead athletes, a final 10-item questionnaire was developed. Two hundred eighty-two healthy, competitive overhead athletes completed the new questionnaire, as well as 2 established upper extremity questionnaires, and were self-assigned into injury categories: (1) playing without pain, (2) playing with pain, and (3) not playing due to pain. Correlations between the scores and differences between injury categories were measured. Responsiveness testing was performed in an additional group of 55 injured athletes, comparing their scores before and after an intervention. Results: The new score showed high correlation with the Disabilities of the Arm, Shoulder and Hand (DASH) score and the DASH sports/performing arts module. The new score correctly stratified overhead athletes by injury category (P \ .0001). The new score also demonstrated excellent responsiveness, varying appropriately with improvements in injury category after treatment of injuries (P \ .05). Conclusion: The new patient-reported instrument is valid and responsive in the evaluation of overhead athletes. Reliability was also demonstrated for the 13-item pilot questionnaire. The results support its use for the functional assessment of overhead athletes in future studies. Keywords: sports medicine; arthroscopy; upper extremity; assessment; score; overhead of daily living and only notice their injury or manifest symptoms during competition. Currently, there are no validated instruments that are designed to measure the functional status of the upper extremity in the overhead athlete. Recently, validated instruments for use in outcomes research have become more widely used.6,10,12,14,19 A number of specific shoulder and elbow measurement tools exist.1,3,8,9,13,15-18,21 Only the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire evaluates the entire upper extremity. However, it is not specific to the shoulder or elbow. It remains difficult to evaluate treatment outcomes within this group. In the past, the standard for evaluating the outcome of the overhead athlete (specifically, baseball players) has been the ability to return to the same level of competition for Overhead athletes place high demands on their upper extremities during training and competition. Injuries to the shoulder and elbow are very common in this group of athletes. Many of these athletes continue to compete effectively despite their injuries. It has been our experience that these athletes may have no limitations in activities *Address correspondence to Frank G. Alberta, MD, Hackensack University Medical Center, 30 Prospect Avenue, Hackensack, NJ 07601 (e-mail: falberta@njorthoclinic.com). The authors declared that they had no conflicts of interest in their authorship and publication of this contribution. The American Journal of Sports Medicine, Vol. 38, No. 5 DOI: 10.1177/0363546509355642 Ó 2010 The Author(s) 903 Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 7, 2010 904 Alberta et al The American Journal of Sports Medicine one season after rehabilitation or surgery.2 This standard does not account for those players who changed positions, styles, intensity, or duration of competition. A combination of instruments may be used to measure functional status of the shoulder and elbow. This would require that the athlete fill out a large number of scores that have significant overlap, which in turn, are difficult and onerous to grade and interpret. With these difficulties in mind, we sought to develop and validate an efficient and reliable patient-administered questionnaire to measure the functional status of the upper extremity in the overhead athlete. This tool would aid in the accurate assessment of overhead athletes after injury, treatment, and/or surgery and provide a performance-based measure of outcomes in this high-demand patient population. MATERIALS AND METHODS Development and Validation of Initial Pilot Questionnaire The objective of development was a patient-athlete–administered questionnaire that requires little time to administer, is easily readable, uses visual analog scales (VASs), and focuses on functional parameters for athletes. We specifically excluded objective measurements from the scope of the questionnaire. The rating system for the athlete’s shoulder proposed by Tibone and Bradley20 was used as background to develop the new items into a cohesive questionnaire. Potential items were gathered from physicians, athletic trainers, and physical therapists directly involved with the care of overhead athletes. The authors also reviewed the literature and currently available scoring systems to evaluate questions in use as well as generally accepted measures of outcome for the shoulder and elbow. Instructions were given to the contributing health care professionals to design items that were not exclusive to any single sport and not specific to the shoulder or the elbow individually. Once all items were gathered, duplicate suggestions were removed or combined into single questions, and an initial 13-item questionnaire was formulated. The questions were formatted similar to a VAS. Athletes were instructed to place a mark on a 10-cm line indicating the current level of performance and/or function of the involved extremity; the far right represents a higher function/level of performance. The examiner measures the distance of the mark from the far left of the scale (representing 0) to the nearest millimeter and records it in centimeters. For example, if an athlete’s mark is measured as 96 mm from point 0 on the VAS, the score for this question is 9.6 of 10. Of the 13 items, 5 were very specific to function and athletic performance (questions 6-11) and were weighted equally to represent 50% of the total score. The remaining 8 items measured symptoms (ie, pain, instability, etc) related to the upper extremity (questions 1-5) or interpersonal relationships related to performance (questions 12-13) and comprised the remaining 50%. The senior authors determined the final weighting scheme to be used in the pilot testing phase, with the emphasis placed on the performance-specific measures. Initial Questionnaire Item Screening Twenty-one currently competing intercollegiate overhead athletes (baseball and softball) completed a demographics cover sheet, the DASH questionnaire, the DASH sports/ performing arts module, and the 13-item pilot questionnaire. The DASH was included in the comparison for its excellent reliability and its inclusion of the shoulder and elbow.1 The DASH sports/performing arts module was chosen as the only existing score designed for the athlete’s upper extremity. On the initial pilot questionnaire, athletes were asked to rate each item for its importance to them from 1 (least) to 5 (most) to analyze the relevance of the individual questions as judged by the athletes themselves. We carried out an exploratory factor analysis (principle components) to determine which items have a strong, positive factor loading on the first factor. In addition, we computed the Cronbach a intra-item reliability coefficient, an average of the intra-item correlations, because the intraitem reliability should be high if an item is to be retained. Finally, we analyzed the mean importance rating for each item as determined by the athletes themselves. To evaluate test-retest reliability, the athletes were asked to fill out the same questionnaire 4 weeks later, with the importance ratings omitted. Players who had a significant change in their injury status as defined by being out of competition secondary to injury were excluded from reliability testing. The 4-week interval was chosen so that recall of the questions was minimized, yet significant changes in injury status were unlikely to occur. We computed the test-retest interclass correlation and the mean test-retest differences and standard deviation (SD) of these differences. Questionnaire Validation Two hundred eighty-two intercollegiate and professional overhead athletes completed the final 10-item KerlanJobe Orthopaedic Clinic (KJOC) score questionnaire as well as a demographic intake sheet. The demographic data collected included sports participation and injury history. The final question on the demographic sheet asked the athlete to assign himself/herself in 1 of 3 categories: (1) playing with no pain, (2) playing with pain, or (3) not playing due to pain. A confirmatory factor analysis was carried out, and nonparametric subgroup comparisons were made. The Kruskal-Wallis test was used to compare median scores between sports/activity, between those with a history of an injury and those without, between those who were currently injured and those who were not, between those treated for an injury and those not treated, and between the 3 injury categories listed above. Medians were compared with nonparametric tests instead Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 7, 2010 Vol. 38, No. 5, 2010 Functional Assessment Tool for the Upper Extremity 905 TABLE 1 Factor Analysis and Reliability in Screening Sample (n 5 21), 13 Items Item Range Factor Loadinga P Value 10.0 9.2 10.0 9.2 5.3 6.1 9.1 10.0 10.0 10.0 10.0 3.6 5.7 0.762 0.727 0.579 0.939 0.567 –0.037 0.738 0.931 0.929 0.950 0.931 –0.002 0.591 \.001 .0003 .0075 \.001 .0092 .8779 .0002 \.001 \.001 \.001 \.001 .9944 .0061 1 2 3 4 5 6 7 8 9 10 11 12 13 a Mean Importance (1-5 Scale) Test-Retest Mean Differenceb Test-Retest SD Differenceb Test-Retest Correlationb .673 .674 .514 .895 .618 .005 .676 .909 .899 .895 .891 .034 .608 4.1 4.5 3.9 4.0 2.5 2.5 3.7 4.3 3.7 3.8 3.5 1.7 2.1 0.75 0.93 –0.37 0.62 0.02 0.24 0.12 0.35 –0.22 0.08 0.49 –0.19 0.75 1.33 1.99 3.26 1.93 2.94 1.14 1.64 2.39 1.56 1.51 2.60 1.78 1.57 0.93 0.76 0.54 0.84 –0.10 0.80 0.86 0.74 0.89 0.89 0.72 0.02 0.61 a Correlation with the factor. n 5 18. b of parametric mean comparisons because the KJOC and DASH scores tend to have a skewed distribution. Treatment Responsiveness Responsiveness of the questionnaire to changes in athletic functional status was tested using an additional group of 55 injured overhead athletes, separate from the 282 above. Each athlete completed the KJOC questionnaire before treatment, then underwent an intervention (rest, therapy, and/or surgery) and was then asked to complete a posttreatment follow-up questionnaire. Demographic data including the athlete’s self-assessment of playing category were again collected as previously described. Median scores or score changes were compared between groups using the nonparametric Kruskal-Wallis test, and withingroup change P values were computed with the paired Wilcoxon signed-rank test. While the medians more appropriately show the typical value because the score distribution may be skewed, the mean and standardized mean (Z 5 effect size 5 mean/SD) score and Z score difference are also reported. RESULTS Development and Test-Retest Reliability of Initial Pilot Questionnaire Table 1 summarizes the factor analysis and reliability results of the original 13 items in the 21 subjects completing the pilot questionnaire. Eighteen of the 21 subjects had test-retest reliability data available for review. The remaining 3 athletes had a change in their injury status and therefore were excluded from the reliability testing. The first factor accounted for 67% of the variation across the 13 items. All items of the KJOC score were positively correlated with the factor except for item 6. Two items were weakly correlated (items 6 and 12), 2 items were moderately correlated (items 3 and 5), and 9 items were strongly correlated (.0.72). Items 6 and 12 were omitted because they poorly correlate with the other items and the composite factor and because they were of low importance, particularly item 12. Item 12 also had poor reliability. Item 5 was omitted because it had poor reliability, was only moderately correlated with the overall factor, was not of high mean importance, and had a rather narrow range. Items 3 and 13 were retained, although they only had moderate correlation with the overall factor because, unlike item 5, they had reasonable reliability. When in doubt, the item was retained rather than prematurely omitted. The factor analysis was performed again using the remaining 10 items for both the original 21 athletes and again on our larger dataset of 282 athletes. The factor loadings for the larger dataset were very similar except for items 4 and 7. Based on this and for simplicity, the final 10item questionnaire is based on an equally weighted sum of all 10 items (Figure 1). The unweighted 13-item KJOC score had a Pearson correlation of 0.81 with the DASH score and 0.85 with the DASH sports/performing arts module, respectively. After removing 1 item from each of the previously described categories (athletic performance, symptoms, interpersonal relationships) based on the analysis above, the unweighted 10-item KJOC score had correlations of 0.84 and 0.86, respectively, with the DASH scores. Eight of the final 10 items were strongly correlated with the factor (correlation .0.72), while the other 2 were moderately correlated (items 3 and 13 in Table 2). Test-retest intraclass correlation coefficients were higher than the DASH for both the original 13-item questionnaire and the 10-item final questionnaire (0.861 and 0.881 vs 0.835) and significantly higher than the DASH sports/performing arts module (0.563). Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 7, 2010 906 Alberta et al The American Journal of Sports Medicine Kerlan-Jobe Orthopaedic Clinic Shoulder & Elbow Score Name_______________________________ Age_______ Sex___________ Dominant Hand (R) ______ (L) _____ (Ambidextrous) __________________ Date of Examination_____________________________ Sport __________ Position __________ Years Played __________ Please answer the following questions related to your history of injuries to YOUR ARM ONLY: YES NO 1. Is your arm currently injured? h h 2. Are you currently active in your sport? h h 3. Have you missed game or practice time in the last year due to an injury to your shoulder or elbow? h h 4. Have you been diagnosed with an injury to your shoulder or elbow other than a strain or sprain? h h If yes, what was the diagnosis? _______________ 5. Have you received treatment for an injury to your shoulder or elbow? If yes, what was the treatment? (Check all that apply) h Rest h Therapy h Surgery (please describe): ___________________ h h h h h h h h Please describe your level of competition in your current sport: (Use Professional Major League, Professional Minor League, Intercollegiate, High School as the choices) 6. What is the highest level of competition you’ve participated at?_____________ 7. What is your current level of competition? _____________________________ 8. If your current level of competition is not the same as your highest level, do you feel it is due to an injury to your arm? Please check the ONE category only that best describes your current status: h Playing without any arm trouble h Playing, but with arm trouble h Not playing due to arm trouble Instructions to athletes: The following questions concern your physical functioning during game and practice conditions. Unless otherwise specified, all questions relate to your shoulder or elbow. Please answer with an X along the horizontal line that corresponds to your current level. 1. How difficult is it for you to get loose or warm prior to competition or practice? Normal warm-up time Never feel loose during games or practice 2. How much pain do you experience in your shoulder or elbow? Pain at rest No pain with competition 3. How much weakness and/or fatigue (ie, loss of strength) do you experience in your shoulder or elbow? Weakness or fatigue preventing any competition No weakness, normal competition fatigue 4. How unstable does your shoulder or elbow feel during competition? “Popping out” routinely No instability (continued) Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 7, 2010 Vol. 38, No. 5, 2010 Functional Assessment Tool for the Upper Extremity 907 5. How much have arm problems affected your relationship with your coaches, management, and agents? Left team, traded or waived, lost contract or scholarship Not at all The following questions refer to your level of competition in your sport. Please answer with an X along the horizontal line that corresponds to your current level. 6. How much have you had to change your throwing motion, serve, stroke, etc, due to your arm? Completely changed, don’t perform motion anymore No change in motion 7. How much has your velocity and/or power suffered due to your arm? Lost all power, became finesse or distance athlete No change in velocity/power 8. What limitation do you have in endurance in competition due to your arm? Significant limitation (became relief pitcher, switched to short races for example) No endurance limitation in competition 9. How much has your control (of pitches, serves, strokes, etc.) suffered due to your arm? Unpredictable control on all pitches, serves, strokes, etc. No loss of control 10. How much do you feel your arm affects your current level of competition in your sport (ie, is your arm holding you back from being at your full potential)? Cannot compete, had to switch sports Desired level of competition Figure 1. Kerlan-Jobe Orthopaedic Clinic shoulder and elbow score. Cross-sectional Validation of Final Questionnaire The final 10-item questionnaire was administered to 282 professional and intercollegiate athletes (Table 3). Seventy-five percent (n 5 211) were baseball players, and 88% (n 5 252) were men. One hundred ninety-one athletes were currently competing or had competed in the past at the professional level of their sport. A factor analysis using the 10 items confirmed that all 10 items have a strong correlation with the overall factor. All but 2 have a correlation of 0.82 or larger. All but one of the factor loadings were above 0.70 (item 7 is the exception). Therefore, the final KJOC score was defined for simplicity as the unweighted sum of the items, making a score with a maximum value of 100. The KJOC scores by current status category are shown in Table 4. All cross-category comparisons revealed significant differences. Players with a history of either shoulder or elbow injury had median KJOC scores significantly lower than players with no history of injury (Tables 5 and 6). The KJOC scores among athletes in category 1 with a history of treatment for a shoulder or elbow injury scored significantly lower than those with no history of injury treatment (median, 92.0 vs 99.3; P \ .0001) (Table 7). Significant differences were found in all cross-category Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 7, 2010 908 Alberta et al The American Journal of Sports Medicine TABLE 2 Assessment Factor Loadings, 10 Items TABLE 3 Athlete Demographics Item n 5 21 n 5 282 Demographic 1 2 3 4 7 8 9 10 11 13 Percentage variation accounted for 0.764 0.729 0.574 0.940 0.738 0.931 0.930 0.951 0.931 0.585 70.2% 0.825 0.880 0.893 0.740 0.583 0.798 0.905 0.908 0.892 0.922 74.0% Age, y Mean Median Gender Male Female Sport Baseball Pitcher Other Swimming Volleyball Water polo Tennis Diving Football Softball Golf comparisons regardless of whether the shoulder or the elbow was injured. Scores for players in like categories were not significantly different when shoulder and elbow injuries were compared. Treatment Responsiveness The final questionnaire was administered to 55 injured overhead athletes who subsequently underwent an intervention (rest, therapy, and/or surgery) (Table 8). These 55 were not part of the 282 or 21 above. Twenty-four of these 55 athletes (46%) completed a follow-up questionnaire at a median of 430 days (range, 63-564) after the first questionnaire. There were no significant differences between those athletes available for follow-up and those who were not for age, years played, and dominant hand (Table 8). The overall median change in the KJOC score was 18.3 points (P 5 .0089) for the 24 respondents. Eleven of the 24 respondents (46%) improved their injury category to uninjured (category 1) by the time of follow-up. These 11 injured athletes who returned to play without pain (category 1) significantly improved their KJOC score a median of 28.2 points (range, 2.9-60.7; P \ .05). The remaining 13 injured athletes who continued to report functional impairment had a median change of only 2.8 points (range, –26.2 to 11.1) in their KJOC score, which was not statistically significant. This difference in the 2 groups was statistically significant (P 5 .0002) (Table 9). DISCUSSION Valid outcome assessment tools are becoming more desirable to aid in clinical research as well as to improve patient care. Traditional objective measures of outcomes such as range of motion, strength, and radiographic variables have been called into question.9 These have been found to be poor indicators of functional and psychological health. Patient-reported measures of quality of life generated by the patient have been shown to be more reliable and valid.11 Furthermore, it has been clearly demonstrated that the physician is a poor judge of patient outcome.5 With athletes, the level of functioning once the patient returns to competition is the true outcome measure most n 23.7 22.0 251 31 215 112 103 38 12 5 5 2 2 1 1 important to that patient. Therefore, it follows that the patient-athlete is the best judge of his or her outcome. Overhead athletes may not manifest symptoms during activities of daily living, and existing outcomes measures may not detect problems resulting from the demands of their training and competition. The purpose of this study was to develop and validate a reliable and responsive outcome assessment tool for overhead athletes. Currently, only the Conway scale has been used to address an athlete’s functional status following injury.2 This scale has not been validated, has only been applied to the elbow, and has not been used for sports other than baseball. We attempted to design a questionnaire that was not specific to a single sport, was simple to administer and score, and was equally effective at evaluating the shoulder and the elbow. The only currently available validated score that fits these criteria is the DASH score. Therefore, we chose the DASH and the DASH sports/ performing arts module as the comparisons for our score. Because the DASH score was validated on a normal population, we hypothesized that this score would be reliable (ie, reproducible) when testing normal athletes. We further hypothesized that the KJOC score would be more valid and responsive than the DASH or the DASH sports/performing arts module in this specific patient population. We chose VAS as the format for the current questionnaire. The VAS was chosen because of its ease of generation and slightly higher sensitivity to change when compared to a Likert scale.4 Likert scale choices are often confusing and difficult to generate because it can be challenging to generate nonmutually exclusive answers. In contrast, Likert scales are easier and less time-consuming to score. Despite this limitation, our instrument is not onerous to score and is not very time-consuming. Our initial pilot phase of the study focused on developing a relevant questionnaire that was easy to administer and score. Factor analysis and Cronbach a for the 13 original items were used to determine the validity of the Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 7, 2010 Vol. 38, No. 5, 2010 Functional Assessment Tool for the Upper Extremity 909 TABLE 4 Kerlan-Jobe Orthopaedic Clinic (KJOC) Score by Category (n 5 282)a Category 1: playing without pain 2: playing with pain 3: not playing n Minimum Q1 Median Mean Q3 Maximum SD SEM 212 46 24 50.0 14.3 12.7 91.8 45.7 35.6 97.5 64.1 44.9 94.4 61.0 44.3 100.0 73.2 55.6 100.0 97.9 79.3 7.8 20.0 16.2 0.5 2.9 3.3 a Q1, first quartile; Q3, third quartile; SEM, standard error of mean. Descriptive statistics for the KJOC scores by category show little overlap between groups with tight clustering. The differences among the 3 groups are all statistically significant with P 5 .0006 or smaller (Kruskal-Wallis test). TABLE 5 Kerlan-Jobe Orthopaedic Clinic (KJOC) Score by History of Injury (n 5 282)a Injury Type Elbow Shoulder Other None n Minimum Q1 Median Mean Q3 Maximum SD SEM 33 68 11 169 24.2 12.7 63.1 28.0 74.6 45.6 79.5 92.1 88.4 64.1 99.4 97.6 80.0 64.7 89.0 93.3 97.4 86.4 100.0 100.0 100.0 100.0 100.0 100.0 23.3 24.7 13.5 11.2 4.1 3.0 4.1 0.9 a Q1, first quartile; Q3, third quartile; SEM, standard error of mean. Comparison of players with history of shoulder or elbow injury to uninjured players (includes all players currently injured). construct in measuring functional performance. Range of motion questions were originally incorporated into the questionnaire because of the biomechanical importance of full, unrestricted range of motion in this population. However, the questions that attempted to have the athletes assess their own range of motion did not perform well in either correlation, nor did they vary much. Based on the clear statistical inferiority, these items were removed. After the modifications, the instrument’s reliability improved from 0.86 to 0.88. Estimates of acceptable reliability have ranged from 0.85 to 0.94 when the instrument is being used to make a treatment decision for a specific patient.7,22 While retest reliability was very good for the DASH, the KJOC score outperformed the DASH among our athletes. The final step in validation of the KJOC score involved the description of the population norms and the comparison of groups within that population. The administration of the KJOC score to the large sample size had the added intention of quantifying clinically relevant variations in the score through the comparisons among athletes with injuries. The KJOC score accurately stratified athletes by injury category, with median scores significantly different from each other in all cross-category comparisons. Athletes with a history of injury, a current injury, or an inactive status scored significantly lower than their uninjured counterparts. When an athlete returned to competition after an intervention, the median change in the KJOC score was highly significant and returned to near normal for uninjured athletes. Our study had several strengths. Our clinic services a highly active and demanding professional, collegiate, and recreational population of athletes. This population exposure allowed a unique experience with injuries in TABLE 6 P Values for Pairwise Comparisons (Kruskal-Wallis) Group Versus Group Elbow Elbow Elbow Shoulder Shoulder Other Shoulder Other None Other None None P Value .0022 .2347 .0003 .0013 .0000 .7376 high-level overhead athletes, as well as with their outcomes after treatment. Furthermore, the KJOC score represents the only available assessment tool specifically designed for the overhead athlete. We followed established and accepted protocols in the development and validation of this questionnaire. We acknowledge several limitations of our study as well. The relative lack of existing comprehensive upper extremity scores for comparison makes analysis of a new score difficult. The DASH score and DASH sports/performing arts module were the only 2 existing validated tools that met our criteria. Reliability testing of the questionnaire was not performed on the larger sample size and is only calculated based on the pilot group of athletes. Furthermore, the cohort group used for responsiveness testing had a low rate of follow-up (46%). Descriptive statistics showed there were no differences between those athletes who returned for follow-up and those who did not for age, years played, and dominant hand (Table 8). Further clinical studies using this new score are necessary. As specific shoulder or elbow problems are evaluated using the Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 7, 2010 910 Alberta et al The American Journal of Sports Medicine TABLE 7 Kerlan-Jobe Orthopaedic Clinic (KJOC) Score With and Without History of Injurya Treatment History None Yes n Minimum Q1 Median Mean Q3 Maximum SD SEM 119 93 50.0 62.6 94.2 86.5 99.30 94.20 96.22 91.98 100.0 100.0 100.0 100.0 6.8 8.3 0.627 0.859 a Q1, first quartile; Q3, third quartile; SEM, standard error of mean. Comparison of players in category 1 (playing without arm trouble) with or without a history of treatment for an injury to the shoulder or elbow. Kruskal-Wallis statistic 5 18.74, P \ .0001. TABLE 8 Comparison of Injured Athletes Lost to Follow-up With Those for Whom Full Data Are Available Age, y Years played Pretreatment score Male gender Right-hand dominant Follow-up Lost to Follow-up 19.8 11.2 59.4 11/24 21/24 20.9 10.9 50 27/31 27/31 P Value .1786 .696 .0409 \.001 .5496 TABLE 9 Change in Kerlan-Jobe Orthopaedic Clinic (KJOC) Score After Treatmenta Group KJOC pretreatment Pretreatment only No improvement Improvement KJOC posttreatment No improvement Improvement KJOC posttreatment minus pretreatment change No improvement Improvement n Minimum Median Maximum Mean SD Standardized Mean (Z) 31 13 11 15.7 23.6 33.9 51.4 59.2 63.3 94.9 77.5 86 51.1 57.2 62.0 19.2 14.1 14.4 2.66 4.07 4.31 13 11 23.3 72.4 57.5 89.4 75.2 97.4 55.8 87.9 15.4 7.8 3.61 11.29 13 11 –26.2 2.9 2.8 28.2 11.1 60.7 –1.4 26.0 11.3 15.4 –0.13 1.69 a Standardized mean 5 Z 5 mean/SD. KJOC score, it will be necessary to continually reassess the ability of the score to accurately stratify and predict the level of play for these overhead athletes. Our new patient-reported instrument is valid, reliable in its pilot form, and responsive in the tested population of adult overhead athletes. This questionnaire may provide more clinically relevant information when used for overhead athletes compared to existing traditional shoulder and elbow scoring instruments. These encouraging results support the use of our new questionnaire for the functional assessment of overhead athletes in future studies. ACKNOWLEDGMENT The authors acknowledge the contributions of Jeffrey Gornbein, DrPH, UCLA SBCC/Department of Biomathematics, David Geffen School of Medicine, for his extensive guidance and support of the statistical design and analysis. REFERENCES 1. Atroshi I, Gummesson C, Andersson B, Dahlgren E, Johansson A. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: reliability and validity of the Swedish version evaluated in 176 patients. Acta Orthop Scand. 2000;71(6):613-618. 2. Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes: treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74(1): 67-83. 3. Dawson J, Fitzpatrick R, Carr A. The assessment of shoulder instability: the development and validation of a questionnaire. J Bone Joint Surg Br. 1999;81(3):420-426. 4. Guyatt GH, Townsend M, Berman LB, Keller JL. A comparison of Likert and visual analogue scales for measuring change in function. J Chronic Dis. 1987;40(12):1129-1133. 5. Haworth RJ, Hopkins J, Ells P, Ackroyd CE, Mowat AG. Expectations and outcome of total hip replacement. Rheumatol Rehabil. 1981; 20(2):65-70. 6. Johanson NA, Liang MH, Daltroy L, Rudicel S, Richmond J. American Academy of Orthopaedic Surgeons lower limb outcomes assessment instruments: reliability, validity, and sensitivity to change. J Bone Joint Surg Am. 2004;86(5):902-909. Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 7, 2010 Vol. 38, No. 5, 2010 Functional Assessment Tool for the Upper Extremity 7. Kelley TL. Interpretation of Educational Measurements. Yonkers, NY: World Books; 1927. 8. King GJ, Richards RR, Zuckerman JD, et al. A standardized method for assessment of elbow function: Research Committee, American Shoulder and Elbow Surgeons. J Shoulder Elbow Surg. 1999;8(4):351-354. 9. Kirkley A, Alvarez C, Griffin S. The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: the Western Ontario Rotator Cuff Index. Clin J Sport Med. 2003;13(2):84-92. 10. Kirkley A, Griffin S. Development of disease-specific quality of life measurement tools. Arthroscopy. 2003;19(10):1121-1128. 11. Koran LM. The reliability of clinical methods, data and judgments (first of two parts). N Engl J Med. 1975;293(13):642-646. 12. Kreibich DN, Vaz M, Bourne RB, et al. What is the best way of assessing outcome after total knee replacement? Clin Orthop Relat Res. 1996;331:221-225. 13. L’Insalata JC, Warren RF, Cohen SB, Altchek DW, Peterson MG. A self-administered questionnaire for assessment of symptoms and function of the shoulder. J Bone Joint Surg Am. 1997;79(5):738-748. 14. Lingard EA, Katz JN, Wright RJ, Wright EA, Sledge CB. Validity and responsiveness of the Knee Society Clinical Rating System in comparison with the SF-36 and WOMAC. J Bone Joint Surg Am. 2001;83(12):1856-1864. 15. Lo IK, Griffin S, Kirkley A. The development of a disease-specific quality of life measurement tool for osteoarthritis of the shoulder: the Western Ontario Osteoarthritis of the Shoulder (WOOS) index. Osteoarthritis Cartilage. 2001;9(8):771-778. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587-594. Mohtadi N. Development and validation of the quality of life outcome measure (questionnaire) for chronic anterior cruciate ligament deficiency. Am J Sports Med. 1998;26(3):350-359. Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res. 1991;4(4):143-149. Saleh KJ, Mulhall KJ, Bershadsky B, et al. Development and validation of a lower-extremity activity scale: use for patients treated with revision total knee arthroplasty. J Bone Joint Surg Am. 2005;87(9): 1985-1994. Tibone JE, Bradley J. Evaluation of treatment outcomes for the athlete’s shoulder. In: Matsen FA, Fu FH, Hawkins RJ, eds. The Shoulder: A Balance of Mobility and Stability. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1993. Turchin DC, Beaton DE, Richards RR. Validity of observer-based aggregate scoring systems as descriptors of elbow pain, function, and disability. J Bone Joint Surg Am. 1998;80(2):154-162. Weiner EA, Stewart BJ. Assessing Individuals. Boston, MA: Little Brown; 1984. 16. 17. 18. 19. 20. 21. 22. For reprints and permission queries, please visit SAGE’s Web site at http://www.sagepub.com/journalsPermissions.nav Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 7, 2010 911