Hypermobility, injury rate and rehabilitation in a professional football Richard Collinge
advertisement
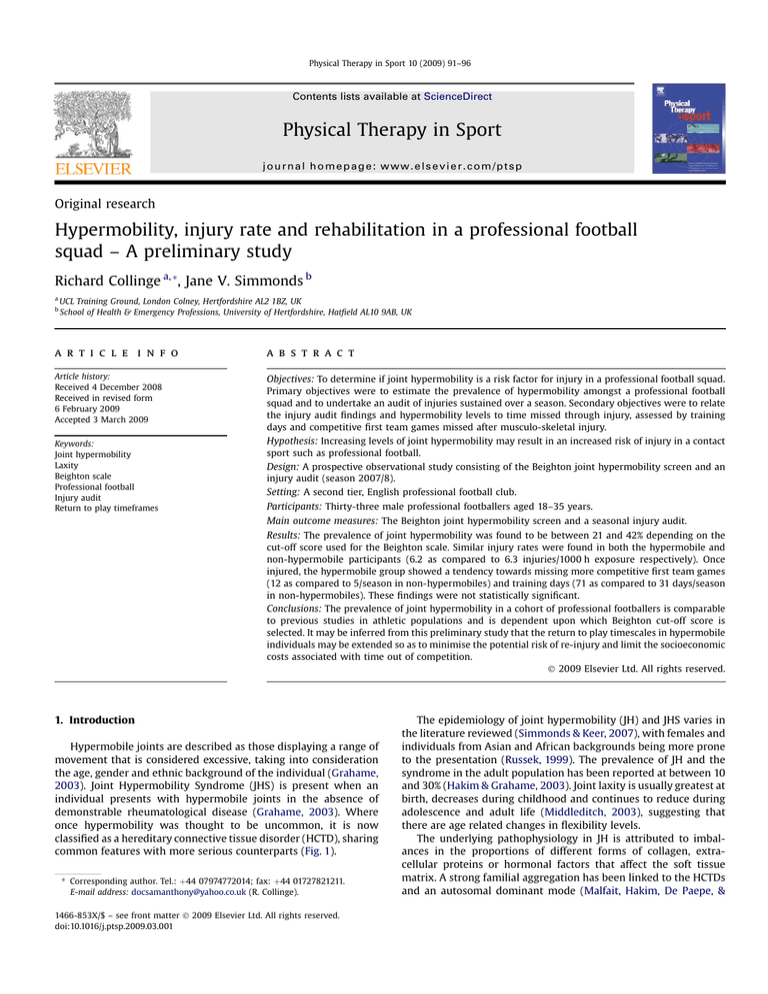
Physical Therapy in Sport 10 (2009) 91–96 Contents lists available at ScienceDirect Physical Therapy in Sport journal homepage: www.elsevier.com/ptsp Original research Hypermobility, injury rate and rehabilitation in a professional football squad – A preliminary study Richard Collinge a, *, Jane V. Simmonds b a b UCL Training Ground, London Colney, Hertfordshire AL2 1BZ, UK School of Health & Emergency Professions, University of Hertfordshire, Hatfield AL10 9AB, UK a r t i c l e i n f o a b s t r a c t Article history: Received 4 December 2008 Received in revised form 6 February 2009 Accepted 3 March 2009 Objectives: To determine if joint hypermobility is a risk factor for injury in a professional football squad. Primary objectives were to estimate the prevalence of hypermobility amongst a professional football squad and to undertake an audit of injuries sustained over a season. Secondary objectives were to relate the injury audit findings and hypermobility levels to time missed through injury, assessed by training days and competitive first team games missed after musculo-skeletal injury. Hypothesis: Increasing levels of joint hypermobility may result in an increased risk of injury in a contact sport such as professional football. Design: A prospective observational study consisting of the Beighton joint hypermobility screen and an injury audit (season 2007/8). Setting: A second tier, English professional football club. Keywords: Joint hypermobility Laxity Beighton scale Professional football Injury audit Return to play timeframes Participants: Thirty-three male professional footballers aged 18–35 years. Main outcome measures: The Beighton joint hypermobility screen and a seasonal injury audit. Results: The prevalence of joint hypermobility was found to be between 21 and 42% depending on the cut-off score used for the Beighton scale. Similar injury rates were found in both the hypermobile and non-hypermobile participants (6.2 as compared to 6.3 injuries/1000 h exposure respectively). Once injured, the hypermobile group showed a tendency towards missing more competitive first team games (12 as compared to 5/season in non-hypermobiles) and training days (71 as compared to 31 days/season in non-hypermobiles). These findings were not statistically significant. Conclusions: The prevalence of joint hypermobility in a cohort of professional footballers is comparable to previous studies in athletic populations and is dependent upon which Beighton cut-off score is selected. It may be inferred from this preliminary study that the return to play timescales in hypermobile individuals may be extended so as to minimise the potential risk of re-injury and limit the socioeconomic costs associated with time out of competition. Ó 2009 Elsevier Ltd. All rights reserved. 1. Introduction Hypermobile joints are described as those displaying a range of movement that is considered excessive, taking into consideration the age, gender and ethnic background of the individual (Grahame, 2003). Joint Hypermobility Syndrome (JHS) is present when an individual presents with hypermobile joints in the absence of demonstrable rheumatological disease (Grahame, 2003). Where once hypermobility was thought to be uncommon, it is now classified as a hereditary connective tissue disorder (HCTD), sharing common features with more serious counterparts (Fig. 1). * Corresponding author. Tel.: þ44 07974772014; fax: þ44 01727821211. E-mail address: docsamanthony@yahoo.co.uk (R. Collinge). 1466-853X/$ – see front matter Ó 2009 Elsevier Ltd. All rights reserved. doi:10.1016/j.ptsp.2009.03.001 The epidemiology of joint hypermobility (JH) and JHS varies in the literature reviewed (Simmonds & Keer, 2007), with females and individuals from Asian and African backgrounds being more prone to the presentation (Russek, 1999). The prevalence of JH and the syndrome in the adult population has been reported at between 10 and 30% (Hakim & Grahame, 2003). Joint laxity is usually greatest at birth, decreases during childhood and continues to reduce during adolescence and adult life (Middleditch, 2003), suggesting that there are age related changes in flexibility levels. The underlying pathophysiology in JH is attributed to imbalances in the proportions of different forms of collagen, extracellular proteins or hormonal factors that affect the soft tissue matrix. A strong familial aggregation has been linked to the HCTDs and an autosomal dominant mode (Malfait, Hakim, De Paepe, & 92 R. Collinge, J.V. Simmonds / Physical Therapy in Sport 10 (2009) 91–96 Ehlers-Danlos Marfan Classic vascular types Aortic dilatation Ectopia lentis Marfanoid habitus Stretchy skin, Papyraceous scars Joint Hypermobility Skin striae (Syndrome) Osteopenia Osteoporosis Fractures Osteogenesis Imperfecta Fig. 1. A flow diagram showing the relationship between joint hypermobility (syndrome) and the heritable disorders of connective tissue (adapted from Grahame, 2003). Grahame, 2006). The manifestation of this genetic encoding is the subsequent effect upon the connective tissue matrix; namely the collagens, fibrillins, elastins and proteoglycans. It is the make up of the connective tissue matrix that determines an individual’s flexibility, as well as joint capsule, ligament and tendon mechanical properties. It has been suggested that it is the abnormal ratio of type III:type I collagen that results in the decreased tissue stiffness common to JH patients, with the thin and elastic type III collagen becoming more prevalent within the soft tissue matrix (Russek, 1999). Tissue biopsies have supported the hypothesis that it is the interference with the processing of the N-propeptide of either a-chain (a1 or a2) of type I collagen or mutations in the production of type V collagen that result in hypermobile presentations (Malfait et al., 2006). Another mutation in a non-collagenous molecule, called tenascinX, has also been suggested as a predisposing factor towards JH (Schalkwijk et al., 2001; Zweers, Dean, van Kuppevelt, Bristow, & Schalkwijk, 2005), whilst elevated levels of IGF-1, insulin and growth hormone have also been discovered in JHS patients (Denko & Boja, 2001). It has been suggested that proprioceptive acuity is reduced in hypermobile subjects. This has been reported at the knee (Hall, Ferrell, Sturrock, Hamblen, & Baxendale, 1995) and proximal interphalangeal joints of the finger (Mallik, Ferrell, McDonald, & Sturrock, 1994). It has also been suggested that joint hypermobility may affect other afferent apparatus of the nervous system and subsequently lead to chronic, sensitised pain states (Grahame, 2003) and in the longer term, osteoarthritis (Al Rawi & Nessan, 1997; Jonsson, Valtysdottir, Kjartansson, & Brekkan, 1996). At present, the optimum level of flexibility required to prevent injury when participating in sporting activity is not clear and may vary between muscle groups and probably sports (Dadebo, White, & George, 2004). A knowledge of where athletes fall in the spectrum of joint mobility may influence intervention and understanding of their complaints (Boyle, Witt, & Riegger-Krugh, 2003) and it has been postulated that athletes at either end of the flexibility spectrum are likely to be more at risk of injury (Stewart & Burden, 2004). Indeed, individuals presenting with generalised joint laxity have been reported to have an increased risk of Anterior Cruciate Ligament (ACL) injury to the knee (Ramesh, Von Arx, Azzopardi, & Schranz, 2005), with the risk increasing five fold in female football players who demonstrate hyperextension postures of the knee (Myer, Ford, Paterno, Nick, & Hewett, 2008). The implications for hypermobile subjects competing in sport have produced conflicting results in the literature, mainly due to the diversity of both contact and non-contact sports studied but also due to inconsistencies in study design. Hypermobile athletes have been shown to have an increased risk of injury in American football (Nicholas, 1970), amateur rugby (Stewart & Burden, 2004) and netball (Smith, Damodaran, Swaminathan, Campbell, & Barnsley, 2005), whilst contradictory evidence has been published for lacrosse participants (Decoster, Bernier, Lindsay, & Vailas, 1999) and American Collegiate athletes (Krivickas & Feinberg, 1996). To date, no studies have examined whether hypermobility is a risk factor for injury in a professional football squad. On a more general level, Hardin, Voight, Blackburn, Canner, and Soffer (1997) report a slower rehabilitation course for individuals presenting with joint hypermobility, highlighting the need for effective screening and preventative programmes to manage hypermobile athletes and limit the socioeconomic costs associated with sports injuries. The primary objective and hypothesis of this research was to estimate the prevalence of JH in a professional football squad and to determine if increasing levels of joint hypermobility, measured using the Beighton scale (Beighton, Soskolne, & Solomon, 1973), results in an increased risk of injury in a professional football squad. The issue of the cut-off score that denotes hypermobility diagnosis has caused much confusion in the hypermobility literature. There is no universal agreement on a threshold for JH; some researchers use a Beighton score of 4 or 5/9, other researchers use a Beighton scale score of 6/9 and still other researchers use a modified score of 3/5 (Russek, 1999). The latter is scored out of 5 by combining the scores obtained by the left and right peripheral joint tests. For the purposes of this study, the cut-off scores utilised by Stewart and Burden (2004) in a study of rugby players, where a score of 4 or greater represents hypermobility and 7 or greater represents excessive hypermobility, will be considered. The cut-off score of 4 points also correlates with the criteria used in the Revised 1998 Brighton Criteria (Grahame, Bird, & Child, 2000). Boyle et al. (2003) found the Beighton scale to have good to excellent reliability in screening individuals aged 15–45 years, with intra-rater reliability reported at 81% when a cut-off score of 5 or greater was selected. This scoring classification will also be referred to in this study. Secondary objectives of this study were to relate the seasonal injury audit findings and hypermobility levels to time missed through injury, assessed by training days and competitive first team games missed after musculo-skeletal injury. 2. Methods 2.1. Participants Thirty-three professional footballers signed to a second tier English team for the 2007/8 season volunteered for the study. The participants were aged 18–35 years and had all signed professional contracts. All players were available to train on a full time basis and were eligible for selection for first team fixtures. Demographic information for the participant group can be seen in Table 1. When analysed by player position, the breakdown of the participant group consisted of three goalkeepers, eleven defenders, nine midfielders and ten attackers (Fig. 2). Three of the players were carrying injuries over from the 2006/7 season (two players had undergone ACL reconstructions and the other internal fixation of a tibial fracture) and were classified as having been injured at the start of the study on 1st July 2007. R. Collinge, J.V. Simmonds / Physical Therapy in Sport 10 (2009) 91–96 93 Table 1 A table representing demographic data of the participant group (one standard deviation, data range). Participant number Mean age – years Mean career length – years Mean height – cm Mean weight – kg Lower limb dominance 33 24.4 (4.8, 18–35 years) 7 (4.8, 1–17 years) 179.2 (6.2, 165–192.5 cm) 82.6 (9, 67.3–109.6 kg) Left ¼ 6 Right ¼ 27 Ethical approval was obtained from the University College London ethics committee. Informed consent was obtained from all participants prior to entering the study. 2.2. Study design A prospective observational study design was undertaken. Participants were invited to take part in a 20 min assessment session with the principal investigator (RC) in August 2007, incorporating the Beighton scale as a measure of hypermobility status (Table 2). An anonymous questionnaire was also completed, with participants allocated individual identification numbers, which included ethnic background, age, playing position, career length as a professional footballer, lower limb dominance, height and weight. Lower limb dominance was defined as the leg that the participant would strike a ball with instinctively for maximal distance. Details of previous and/or current injury that may have affected any component of the test procedure were documented. Based upon the classification used by Stewart and Burden (2004), which was based on rugby players, the participant’s Beighton scores were analysed in accordance with the criteria shown in Table 3. The classification laid out by Boyle et al. (2003) was also considered. 2.3. Injury audit The Football Association (England) guidelines on injury reporting state that ‘‘an injury can be received during training or competition and prevents the injured party from participating in normal training or competition for more than 48 h, not including the day of the injury’’ (Hawkins, Hulse, Wilkinson, Hodson, & Gibson, 2001). Absence from training or competition through sickness and non-musculo-skeletal causes were not included in the audit. The nature and mechanism of injury (contact or non-contact), the number of days training missed, the number of injuries per season and the number of competitive first team games missed were recorded by the principal investigator (RC) for the 2007/8 football season (1st July 2007–4th May 2008). An impartial colleague who was blind to the test protocol collected the injury 9% 30% Goalkeepers audit data. Descriptors of the anatomical site of injury, side of injury (dominant versus non-dominant, left versus right), soft tissue or osteo/arthrogenic and grade of injury if radiological input had been sought were utilised. In addition, a diary of the total hours training and match play was kept throughout the season by the principal investigator (RC) so that exposure rates could be calculated. 2.4. Statistical analysis Descriptive statistics using Microsoft Excel and the Vassar statistical packages (www.faculty.vassar.edu/lowry/VassarStats) were used to determine mean values pertaining to the demographic data collected. The significance level for all statistical tests was set at p 0.05, with a power analysis for the study reporting a value of 69% (www.dssresearch.com) and necessitating the use of non-parametric statistical analysis. Chi-squared statistical analysis was used to determine if there was a significant difference in injury risk and subsequent rehabilitation time between hypermobile and non-hypermobile participants. 3. Results Of the thirty-three participants who volunteered for the study, four had to be followed up by telephone questionnaire to report injury data as they had been transferred to rival clubs in January 2008. The study group consisted of 51% non-Caucasian and 49% Caucasian participants. 3.1. Hypermobility status When analysed by the Stewart and Burden (2004) cut-off criteria, fourteen participants (42%) scored 4 or more points on the Beighton scale, qualifying as a hypermobile presentation, whilst four participants (12%) presented with scores greater than seven, representing excessive hypermobility. A lower figure of 7 participants (21%) scored 5 or more points to qualify as a hypermobile presentation as described in the criteria by Boyle et al. (2003). The mean (1SD) Beighton score for the group was 3.3 (2.8). Fig. 3 represents the spread of scores on the Beighton scale for the group. When the Beighton results were examined by the number of positive findings for each of the nine joints and manoeuvres tested, it was clearly evident that the knee joints presented with the highest number of positive tests (45 tests/68%). Defenders 34% Midfielders Attackers 27% Fig. 2. A pie chart representing the positional make up of the football squad for season 2007–2008. Table 2 The nine point Beighton hypermobility scale (0 ¼ negative test, 1 ¼ positive test). Test participant ability to: Left Right Passively extend 5th metacarpophalangeal joint >90 Passively appose thumb to volar aspect of forearm Passively hyperextend elbow >10 Passively hyperextend knee >10 Actively place hands flat on floor without bending knees Total¼ 0/1 0/1 0/1 0/1 0/1 0/1 0/1 0/1 0/1 /9 R. Collinge, J.V. Simmonds / Physical Therapy in Sport 10 (2009) 91–96 Table 3 The subcategories of the Beighton scale (adapted from Stewart & Burden, 2004). Beighton score Subject group 0–3 4–6 7–9 Tight/non-hypermobile Hypermobile Excessively hypermobile Days Training Missed 94 80 71 60 31 40 20 0 Beighton +ve Beighton -ve Beighton Classification 3.2. Injury risk The total number of injuries sustained by the squad was 67 over the season 2007/8. Data analysis with a Beighton cut-off score of 4, showed a nonsignificant difference in individual injury risk between the hypermobile (6.2 injuries/1000 h exposure) and non-hypermobile groups (6.3 injuries/1000 h exposure, c2, p ¼ 0.22). 3.3. Number of training days and competitive games missed through musculo-skeletal injury Fig. 4. A bar chart representing the average number of days training missed by individuals through musculo-skeletal injury when screened using the Beighton scale (cut-off score set at 4 or more in accordance with Stewart & Burden, 2004). When the data were divided into osteo/arthrogenic injury as compared to soft tissue injuries, no significant difference was found between the two groups (c2, p ¼ 0.92). 4. Discussion 4.1. Hypermobility status 3.4. Nature of injuries sustained A total of 28 injuries were sustained by the hypermobile group and 39 in the non-hypermobile group. The nature of injury between contact and non-contact mechanisms failed to produce any statistically significant findings between the hypermobile and non-hypermobile subject groups (c2, p ¼ 0.79). 3.5. Anatomical site of injury Frequency The lower limb was the main site of injury across both groups (83% of injuries). The knee and ankle joints were the most common sites of injury, with the former being most commonly injured in the non-hypermobile group (6 injuries as compared to 4 in the hypermobile group) and the ankle most commonly injured in the hypermobile participants (6 injuries as compared to 4 in the non-hypermobile group). 10 9 8 7 6 5 4 3 2 1 0 9 7 4 3 3 3 2 1 1 0 0 1 2 3 4 5 6 7 8 9 Beighton Score Fig. 3. A bar chart representing the distribution of Beighton scores across the thirtythree professional footballers. The prevalence of JH noted in the current study at 42% was higher than previously reported in the literature by Stewart and Burden (32%, 2004) and Decoster et al. (24%, 1999). These different values may be attributable to different sized participant groups in these studies, the different Beighton cut-off score selected in the latter study or potential differences in ethnic backgrounds and competition demands between the sporting groups studied. If a cut-off score of 5 is selected, then the incidence of hypermobility in the current study is reduced to 21% and may therefore correspond more favourably to the findings of Decoster et al. (1999). Although the sample size limits the external validity of this preliminary study, interesting and important trends were seen. Firstly, it can be seen that there were a high number of positive Beighton test results for knee hyperextension (68%) in accordance with the 69% found by Decoster et al. (1999) in male and female lacrosse players. Ramesh et al. (2005) found a knee hyperextension prevalence of 37% in a control group that suggests that participants in kicking sports may well show increased levels of knee hyperextension. Further research is required to clarify whether these findings are common to the non-sporting population and comparison to other sports is required. Extrapolation of the research findings could then be pooled to determine if such presentations are attributable to genetic factors or are indeed acquired through participation in football, especially when the mean (1SD) number of career years in the professional game was 7 years (4.8 years) in this study. Grahame (1999) comments that joint range can be increased into the hypermobile range by the sheer hard work of training. It must be considered that with the development of Football Academies, designed to nurture young Number Of Games Missed The results showed that with the Beighton cut-off score set at 4, individuals in the hypermobile group missed on average 71 days’ training as compared to 31 days in the non-hypermobile group over season 2007/8 (c2, p ¼ 0.08, Fig. 4). In terms of competitive first team games missed, there was no statistically significant difference between the two groups over season 2007/8. It is interesting to note that the hypermobile group missed on average 12 games as compared to 5 in the non-hypermobile group after sustaining musculo-skeletal injury (c2, p ¼ 0.21, Fig. 5). 15 12 10 5 5 0 Beighton +ve Beighton -ve Beighton Classification Fig. 5. A bar chart representing the average number of competitive first team games missed by individuals through musculo-skeletal injury when screened using the Beighton scale (cut-off score set at 4 or more in accordance with Stewart & Burden, 2004). R. Collinge, J.V. Simmonds / Physical Therapy in Sport 10 (2009) 91–96 talent, some players had been with the present club since the age of 8 years. This could potentially lead to acquired movement patterns and the knee joints may be susceptible to hyperextension forces due to the open chain nature of the kicking action. These findings may partly explain the high incidence of knee osteoarthritis in retired professional footballers, reported at 49% (Turner, Barlow, & Heathcote-Elliott, 2000). When the Beighton scores were analysed by ethnic group, there was insufficient data to detect a trend. Further large scale investigation is warranted in this area to validate the conflicting findings of Smith et al. (2005), who reported an absence of ethnic trends related to hypermobility levels in female junior netball players, and Russek (1999) who comments upon African individuals in the general population presenting with increased levels of hypermobility as compared to Caucasian individuals. 4.2. Injury risk The average individual injury risk over the 2007/8 season was 2.0 per player, which is higher than the 1.3 injuries per player per season reported by Hawkins et al. (2001). The interpretation of this study suggests that the injury risk appears to be very similar between the hypermobile and nonhypermobile players in this professional football group. The average injury risk in hypermobile participants (6.2 injuries/1000 h exposure) is almost identical when compared to the non-hypermobile group (6.3 injuries/1000 h exposure, c2 p ¼ 0.22). These findings concur with Decoster et al. (1999) who reported an injury risk of 4.7 injuries/1000 h exposure in male lacrosse players and 2.3 injuries/1000 h exposure in hypermobile subjects as compared to a statistically insignificant 3.5/1000 h in the nonhypermobile group. The lower injury exposure rates in the lacrosse study may be explained by the different Beighton cut-off score employed by Decoster et al. (1999) and the differing demands of lacrosse as compared to professional football. The authors also fail to provide details of the training and match-play demands associated with lacrosse which makes direct comparison difficult. Krivickas and Feinberg (1996) also found that there was no difference in injury risk between hypermobile and non-hypermobile American Collegiate athletes from a diversity of disciplines. There are currently no other published studies looking at injury risk and rehabilitation time for hypermobile athletes in professional football with which to make direct comparison. The explanation as to why both participant groups presented with similar injury exposure risks in the current study may be attributable to the emphasis placed upon preventative medicine in the sporting domain. The ethos at the football club studied is based upon pre-habilitation sessions, where squad members are screened from a biomechanical and orthopaedic perspective in pre-season. Players subsequently undertake twice weekly preventative exercise programmes, set by the Physiotherapy and Strength and Conditioning teams, in order to minimise the risk of injury. Although the small sample size and difficulty in comparing ‘‘like for like’’ injuries between the two groups hinders the wider extrapolation of the findings of this study, the hypermobile group may have been successfully targeted and set appropriate individual programmes that may have served to reduce their risk of injury. 4.3. Training days and competitive games missed through musculo-skeletal injury The current study has found that there is a strong trend between the two groups when the data is interpreted in terms of the average number of training days and first team games missed by individuals in each group through musculo-skeletal injury. The hypermobile 95 group showed a trend towards increased training time and match play missed once they had sustained an injury. Although not statistically proven from this study and direct comparison of injuries was not possible between players, this relationship is worthy of further investigation as there is a dearth of data published in this field and future findings could be important in designing rehabilitation programmes and modifying timeframes for injured hypermobile individuals. The trends found in this study infer that although the injury risk/1000 h is similar between hypermobile and non-hypermobile professional footballers, when hypermobile players sustain a musculo-skeletal injury, such individuals take longer to get back to competition. This inference concurs with the work of Hardin et al. (1997) who suggest that return to play timescales maybe longer in hypermobile individuals, a factor that may have socioeconomic consequences for the athlete, team and club alike. Potential explanations for the extended rehabilitation timeframe in hypermobile individuals may revolve around the inability of hypermobile individuals to lay down mature (type I) collagen during the healing process. Hormonal factors, such as IGF-1, may play a part in the control of this process (Denko & Boja, 2001), possibly due to its effect on metabolism and the healing process evident after injury. When this theory is combined with the decrease in proprioceptive acuity described in hypermobile individuals (Hall et al., 1995; Mallik et al., 1994), the potential risk of reinjury may be assumed to be higher in hypermobile individuals if an awareness of the extended timescales of rehabilitation is not considered. Ferrell et al. (2004) have reported that symptoms associated with hypermobility can be reduced through compliance with a closed kinetic chain (CKC) exercise programme and it may be hypothesised that CKC and proprioceptive exercises should be included in preventative and rehabilitation programmes for hypermobile individuals. These findings may be important in managing the symptoms associated with JH and preventing the longer term sequelae of osteoarthritis in hypermobile individuals, as reported by Jonsson et al. (1996). This study certainly suggests that further research is warranted in the hypermobility field utilising a larger sample size, with calculations suggesting that 60 participants would raise the power of the study to greater than 90% with p 0.05 (www.dssresearch. com). The findings could provide valuable information for physiotherapy and other rehabilitation professionals when considering the extended timescales of rehabilitation in hypermobile individuals and delaying the onset of loaded and functional exercises so as to prevent the risk of re-injury and longer term sequelae. 4.4. Limitations and future developments Future large scale research is warranted and should aim to further explore the trends identified in this study. This is the first piece of work presented examining hypermobility in professional football and should act as a stimulus for multi-centre trials in the sporting domain. The limitations of this provisional study are primarily the small sample size utilised. The study could be improved upon by incorporating assessment of other joints in addition to those tested by the Beighton scale. Hakim and Grahame (2003) criticise the Beighton scale for its lack of consideration of joints that fall outside of the five tested. To augment the accuracy of data collected, future studies may therefore incorporate the Contompasis score (McNerney & Johnston, 1979) or the 10 point Hospital del Mar scoring system designed by Bulbena, Duro, and Porta (1992). These assessment tools may be more specific than the Beighton scale in a lower limb dominant sport such as football. 96 R. Collinge, J.V. Simmonds / Physical Therapy in Sport 10 (2009) 91–96 Future research may also include the Revised 1998 Brighton Criteria (Grahame et al., 2000) and the 5 Point Questionnaire (Hakim & Grahame, 2003). However, because of the inclusion of historical hypermobility questioning and chronic pain in the criteria, these tools may not be sensitive enough to identify the phenotype in sporting populations. Consideration should be given to other features included in the Brighton criteria; namely skin laxity, striae and papyraceous scarring which may assist in identifying the phenotype in young, athletic populations. Consideration must also be given to the fact that the current study assessed participants using the Beighton scale after the completion of training sessions. This provisional study provides an insight into joint hypermobility in an elite football squad that has not previously been published in the literature. The post-training assessment period provided the only viable window of opportunity to assess participants and therefore the impact of ballistic activity and changes in visco-elastic properties of the soft tissues are accepted as limitations of this study. 5. Conclusion This preliminary study investigated the prevalence of hypermobility in a professional football squad and the incidence of injury over the 2007/8 season. Although the injury rates were similar between the hypermobile and non-hypermobile individuals, interesting trends were observed suggestive of extended return to play timeframes in hypermobile individuals that warrant further larger scale studies. The findings are potentially important for rehabilitation professionals in designing and implementing rehabilitation programmes so as to minimise the risk of re-injury and the socioeconomic implications that this may bring in sporting populations. Future studies should look to use the template of this study so that trends in hypermobility level and return to play timeframes can be explored further and extrapolated to the Sports Medicine fraternity. Conflict of interest There are no financial or personal conflicts of interest with any other person or organisation that could inappropriately influence this work. Funding None. Ethical approval Ethical approval was obtained from the University College London ethics committee. Informed consent was obtained from all participants prior to entering the study. Acknowledgements University College and King’s College London MSc Sports Physiotherapy Departments and Players and Staff from the Championship Football Club used in this study. References Al Rawi, Z., & Nessan, A. H. (1997). Joint hypermobility in patients with chondromalacia patellae. British Journal of Rheumatology, 36, 1324–1327. Beighton, P. H., Soskolne, L., & Solomon, C. L. (1973). Articular mobility in an African population. Annals of the Rheumatic Diseases, 32, 413–417. Boyle, K. L., Witt, P., & Riegger-Krugh, C. (2003). Intrarater and interrater reliability of the Beighton and Horan Joint Mobility Index. Journal of Athletic Training, 38(4), 281–285. Bulbena, A., Duro, J. C., & Porta, M. (1992). Clinical assessment of hypermobility of joints: assembling criteria. Journal of Rheumatology, 19, 115–122. Dadebo, B., White, J., & George, K. P. (2004). A survey of flexibility training protocols and hamstring strains in professional football clubs in England. British Journal of Sports Medicine, 38, 388–394. Decoster, L. C., Bernier, J. N., Lindsay, R. H., & Vailas, J. C. (1999). Generalised joint hypermobility and its relationship patterns among NCAA lacrosse players. Journal of Athletic Training, 34(2), 99–105. Denko, C. W., & Boja, B. (2001). Growth hormone, insulin and insulin like growth factor-1 in hypermobility syndrome. Journal of Rheumatology, 28(7), 1666–1669. Ferrell, W. R., Tennant, N., Sturrock, R. D., Ashton, L., Creed, G., Brydson, G., et al. (2004). Amelioration of symptoms by enhancement of proprioception in patients with joint hypermobility syndrome. Arthritis and Rheumatism, 50(10), 3323–3328. Grahame, R. (1999). Joint hypermobility and genetic collagen disorders: are they related? Archives of Disease in Childhood, 80, 188–191. Grahame, R. (2003). Hypermobility and hypermobility syndrome. In R. Keer, & R. Grahame (Eds.), Hypermobility syndrome, recognition and management for physiotherapists (pp. 1–14). Edinburgh: Butterworth Heinemann. Grahame, R., Bird, H. A., & Child, A. (2000). The revised (Brighton 1998) criteria for the diagnosis of benign joint hypermobility syndrome. Journal of Rheumatology, 27, 1777–1779. Hakim, A. J., & Grahame, R. (2003). Joint hypermobility syndrome: an update for clinicians. International Journal of Advances in Rheumatology, 1(4), 131–138. Hall, M. G., Ferrell, W. R., Sturrock, R. D., Hamblen, D. L., & Baxendale, R. H. (1995). The effect of the hypermobility syndrome on knee joint proprioception. British Journal of Rheumatology, 34, 121–125. Hardin, J. A., Voight, M. L., Blackburn, T. A., Canner, G. C., & Soffer, S. R. (1997). The effects of ‘‘decelerated’’ rehabilitation following anterior cruciate ligament reconstruction on a hyperelastic female adolescent: a case study. The Journal of Orthopaedic and Sports Physical Therapy, 26, 29–34. Hawkins, R. D., Hulse, M. A., Wilkinson, C., Hodson, A., & Gibson, M. (2001). The association football medical research programme: an audit of injuries in professional football. British Journal of Sports Medicine, 35, 43–47. Jonsson, H., Valtysdottir, S. T., Kjartansson, O., & Brekkan, A. (1996). Hypermobility associated with osteoarthritis of the thumb base: a clinical and radiological subset of hand osteoarthritis. Annals of the Rheumatic Diseases, 55, 540–543. Krivickas, L. S., & Feinberg, J. H. (1996). Lower extremity injuries in college athletes: relation between ligamentous laxity and lower extremity muscle tightness. Archives of Physical Medicine and Rehabilitation, 77, 1139–1143. Malfait, F., Hakim, A. J., De Paepe, A., & Grahame, R. (2006). The genetic basis of the joint hypermobility syndromes. Rheumatology, 45, 502–507. Mallik, A. K., Ferrell, W. R., McDonald, A. G., & Sturrock, R. D. (1994). Impaired proprioceptive acuity at the proximal interphalangeal joint in patients with the hypermobility syndrome. British Journal of Rheumatology, 33, 631–637. McNerney, J. E., & Johnston, W. B. (1979). Generalized ligament laxity, hallux abducto-valgus and the first metatarsocuneiform joint. Journal of the American Podiatric Medical Association, 69, 69–82. Middleditch, A. (2003). Management of the hypermobile adolescent. In R. Keer, & R. Grahame (Eds.), Hypermobility syndrome, recognition and management for physiotherapists (pp. 51–66). Edinburgh: Butterworth Heinemann. Myer, G. D., Ford, K. R., Paterno, M. V., Nick, T. G., & Hewett, T. E. (2008). The effects of generalised joint laxity on risk of anterior cruciate ligament injury in young female athletes. American Journal of Sports Medicine, 36(6), 1073–1080. Nicholas, J. A. (1970). Injuries to knee ligaments. JAMA: The Journal of the American Medical Association, 212(13), 2236–2239. Ramesh, R., Von Arx, O., Azzopardi, T., & Schranz, P. J. (2005). The risk of anterior cruciate ligament rupture with generalised joint laxity. The Journal of Bone and Joint Surgery. British Volume, 87-B, 800–803. Russek, L. N. (1999). Hypermobility syndrome. Physical Therapy, 79(6), 591–599. Schalkwijk, J., Zweers, M. C., Steijlen, P. M., Dean, W. B., Taylor, G., van Vlijmen, I. M., et al. (2001). A recessive form of the Ehlers–Danlos syndrome caused by tenascin-X deficiency. New England Journal of Medicine, 345(16), 1167–1175. Simmonds, J. V., & Keer, R. J. (2007). Hypermobility and the hypermobility syndrome. Manual Therapy, 12(4), 298–309. Smith, R., Damodaran, A. K., Swaminathan, S., Campbell, R., & Barnsley, L. (2005). Hypermobility and sports injuries in junior netball players. British Journal of Sports Medicine, 39, 628–631. Stewart, D. R., & Burden, S. B. (2004). Does generalised ligamentous laxity increase seasonal incidence of injuries in male first division club rugby players? British Journal of Sports Medicine, 38, 457–460. Turner, A. P., Barlow, J. H., & Heathcote-Elliott, C. (2000). Long term health impact of playing professional football in the United Kingdom. British Journal of Sports Medicine, 34, 332–337. Zweers, M. C., Dean, W. B., van Kuppevelt, T. H., Bristow, J., & Schalkwijk, J. (2005). Elastic fibre abnormalities in hypermobility type Ehlers–Danlos syndrome patients with tenascin-X mutations. Clinical Genetics, 67(4), 330–334. Websites www.dssresearch.com. www.faculty.vassar.edu/lowry/VassarStats.