QUALITY ACCOUNT 2012/13 ’S HOSPICE
advertisement

ST LUKE’S HOSPICE
QUALITY ACCOUNT
2012/13
The staff were excellent, caring and made a huge difference’
‘Absolutely an amazing caring place’
We found the hospice very calming and very clean and staff/volunteers
all helpful and a pleasure. Nice environment to visit.’
1
PART 1:
Trust Board Chairman’s/Chief Executive’s Statement
This Quality Account for St Luke’s Hospice is produced in accordance with the requirements
of NHS (Quality Accounts) Regulations 2010 and NHS Act 2006. It covers all service
provision, therefore the report not only satisfies those regulations but more importantly, it
gives the Hospice an opportunity to demonstrate how quality is central to everything that the
Hospice does within its walls and further afield within the hugely diverse community it
serves.
St Luke’s Hospice provides services for NHS Brent and Harrow. Funding mechanism for
NHS services is through the National Contract (Community) and represents approximately
only 33% of the costs required to maintain the hospice clinical services. The
Commissioners have acknowledged in this contract that no way does their contribution cover
the full cost to the Hospice of providing the services commissioned and that the
Commissioners benefit from the charitable fundraising activities of the Hospice to make up
the shortfall from public funds. NHS recurrent income has either remained static or been
reduced for the past few years and is being reduced further for the forthcoming year. In light
of the current national financial climate, this puts undue pressure on the hospice providing
clinical services to the NHS.
The remaining income, 67%, is generated through a wide range of fundraising activities. This
includes donations, the operation of a network of charity shops, traditional and innovative
fundraising events, legacies and a hospice lottery and some income through activities such
as education. In all this the hospice relies on the generosity of the community which values
so highly the services provided. Of course, there is always a degree of uncertainty around
this income and even more so in the current financial climate of recession
I am pleased to present this Quality Account for 2012/13 and, to the best of my knowledge,
the information contained therein is accurate.
M R Coward
M R Coward
Chief Executive
St. Luke’s Hospice
2
MISSION STATEMENT:
“To provide specialist palliative care free of charge to people with
advanced progressive illnesses, which addresses their physical,
emotional, social and spiritual needs thus enhancing their quality
of life and supporting their families and carers”
INTRODUCTION
To achieve our mission, the Hospice provides a range of patient and family clinical services
through provision of In-Patient, Day-Care and Outpatient services as well as developing
community services through its Hospice at Home service and specialist Community
Palliative Care team. This is all underpinned by a comprehensive training and education
programme. St. Lukes also funds and supports 6 monthly training posts for General
Practitioners. The central aims of clinical provision are to provide and continue to develop
high quality services
Clinical services are supported by a range of administrative and fundraising functions. These
functions are vital in support of clinical service delivery and our aim is to contain their cost.
We thank all organisations and individuals who have shown their support and appreciation in
various ways over the year.
The Hospice employed an average of 85 full-time equivalent paid staff in 2012, with a further
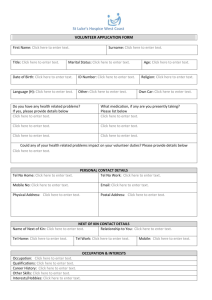
38 employed in the trading subsidiary. They are supported by a cohort of some 800 unpaid
volunteers. These volunteers cover a wide range of activities for the Hospice, which
includes:
Shop Volunteers
Driving patients to and from Day-Care
Working in Day-Care and the In-Patient Units
Complementary therapy volunteers
Gardening
Receptionists
Fundraising
Administrative support
Bereavement support
The support of our volunteers is of vital importance to the St Lukes. They save the Hospice
a considerable amount of money by performing tasks that would otherwise have to be done
by paid staff. Moreover, they are representatives of and ambassadors to the communities
the Hospice serves and thus bring to patient care an extra dimension of support and help
3
that is the quintessence of hospice care and which distinguishes it from palliative care in
other settings. The development of volunteers is an on-going project.
Provision of Services and Funding
During the reporting period 2012 St Luke’s Hospice predominantly provided services to two
NHS organisations, Brent and Harrow. The hospice has reviewed and made available to
them data on the quality of care provided to the population of these areas. However, it
should be noted that care has also been given to a small number of Barnet patients, an
increase on previous years.
The income generated from the NHS for the services reviewed in 2012 represents 33% per
cent of the total income required for the provision of End of Life Care clinical services at St.
Lukes. All financial information can be found in our financial reports on our website
(www.stlukes-hospice.org)
Patient and Public Involvement
Open Days
St. Lukes offers care to a very diverse population. In order to ensure that all our local
communities and healthcare partners are aware of the range of services we provide, we hold
a series of Open Days throughout the year, for healthcare professionals and community
groups. Staff are on hand with information boards to demonstrate the quality of care we
provide and to discuss and answer any questions people may have. We can also show the
various ways in which we aim to meet cultural and religious requirements. One way of
demonstrating our commitment to equality and diversity is an appropriate display in the
reception area recognising different cultural/religious festivals, which is always appreciated
by the visitors, patients, staff and volunteers of the hospice. We also hold two specific open
days for carers which are run by our Patient and Family Support Services and show how we
can support carers in their journey through to bereavement .
Patient and Carer Feedback
Through Day Care and our Patient and Family Support Services, we run regular
patient/carer forums and evaluations to get feedback on services provided, to ensure we are
meeting the needs of our population both clinically, emotionally and culturally, and also to
inform any service improvements we may make. The changes in our Day Care routines
were informed by holding patient forums to understand what would improve patients
experience in Day care.
We run two anonymous surveys. One is a visitor’s survey, which is an internal survey,
currently carried out annually but will be increasing to twice a year. We are also part of a
national patient survey, run by Help the Hospices and Kent University, which is run every
two years. This provides useful information that can be benchmarked against other
hospices nationally. The outcomes of both these surveys have been excellent with mainly
positive responses on the quality of care. Most concerns have been minor but action plans
are developed to address these. One area highlighted was access to information and this
has been raised as one of our priorities for 2013.
“I had no idea you were here, I am so glad I attended today, it’s a real
comfort to know you are here”
“You have done a fantastic job in reassuring me that in my dad’s last days he
will be in great hands and treated with respect. Thank you”
4
SERVICE IMPROVEMENTS
Priorities for 2013
St. Lukes is committed to continuous improvement. Progress is on-going to develop a
Quality Management System in order to evidence the existing quality of services, prepare for
the CQC requirements and demonstrate a culture of ‘continuous improvement’ throughout
the services. The aim not only being to ensure that St.Lukes are fully compliant with all
national regulations and meeting their statutory requirements, but also to ensure we are a
“learning organisation” which continuously strives to improve the quality of our services
through feedback and evaluation of what we do.
The hospice has chosen a set of priorities for 2013 to support our ethos of attention to
quality improvement, patient safety and care, patient experience and clinical effectiveness.
1. Formation of Clinical Risk, Governance and Quality Framework
to include:
a. Falls Management – Implementation of Falls Prevention Policy, Assessment Tool
and Audit.
b. Review of Sharps Management
c. Further development of Clinical Audit Group
2. Development of End of Life Training programme for Social
Workers following on from initial work with Harrow Social Services who requested
support in educating their teams.
3. Development of 5 day individualised End of Life training
programme for GPs to promote and improve End of Life care within primary care.
4. Production of New Patient Information for IPU and Day Care in
response to comments from both Patients’ and visitors’ Surveys.
5. Development of Communication Training Programme in order to
meet requirements of Peer Review.
6. Introduce Clinical Supervision Programme for Staff in response to
comments in the Staff Survey.
5
Outcomes from Priorities in 2012
(1) Development of Lone Worker Risk Assessment Tool & Policy update
In line with legislation and national policy and guidelines, it was recognised that a joint approach to
staff safety should be established within the clinical services of the hospice, particularly relating to
those who operated as lone workers. There was also a lack of consistency identified in the risk
assessment documents and tools used within clinical services. It was agreed that the service
managers and their teams would review and update Policy and procedures for lone workers,
especially within services going out into the community.
All staff have received training regarding the new Lone Worker policy. All clinical members of the two
teams, Community and Hospice at Home are issued with mobile phones and personal alarms. Within
the auspices of Hospice at Home, all patients prior to a visit are risk assessed by the team of
Registered Nurses, from either the information on the referral form or verbally from the referrer
(Clinical Nurse Specialist or Hospital Discharge Team). A Lone Worker/Home Visit Rapid Risk
Assessment is completed. If it is indicated there may be a risk then two people would visit e.g. if the
referral form requests a Healthcare Assistant to visit, but the patient is bed bound then two Healthcare
Assistants would visit with regard to Manual Handling guidelines. The Specialist Community team
have also been using assessment tool. Both teams will audit and review the policy and assessment
tool at the end of a year.
(2) IT – Our system for qualifying patient care services to progress to
transferring paper patient care records onto a computerised patient record
system
In order to meet the changing health care environment and requirement to provide more detailed
patient information the hospice has invested in a computerised patient record system, iCARE. The
collection of robust data is important to identify the level of activity, equitable access to our services
and support a good quality management system. A senior clinical manager has led the
implementation of Phase 1, together with limited external support from the provider company.
Phase one has included the inputting of demographic patient data, and enabled the organisation to
track individual patients’ journeys through hospice services. The organisation is now working on the
development of reports from the system to increase available information in relation to patient activity.
Phase Two will include the development of holistic patient assessment within the system, which can
be shared between all hospice services; and the introduction of chronological patient notes
entries. This will prevent duplication of information, and enhance communication between the Multidisciplinary teams across all hospice services.
(3) Introduction to Palliative Care for Non-Cancer Patients - Sowing the Seeds
The heart failure project with Brent PCT, highlighted difficulties in identifying patients at the transition
point to a palliative stage of a non-cancer illness. Although patients in the last weeks of life are
considered for end of life care, failure to access palliative and supportive care at an earlier stage
leads to reduced options and lack of advanced care planning for this group. The project was to offer
a programme to this patient group to introduce them to the role of the hospice, of palliative care, and
associated services on offer in a non-threatening way, taking a holistic approach to the care of this
patient group with a view to improving symptom management. Particular focus was to be given to
building links with BME groups who are not currently accessing end of life care for non-cancer
6
conditions, and by working collaboratively with referring health professionals, build a programme
which meets their needs.
Patients with heart failure, respiratory disease and renal failure attended the programme. Referrals to
the community palliative care team for patients with a non-malignant diagnosis have increased over
the past year and are forming an increasing part of the community caseload. Health care
professionals are increasingly recognising the role of specialist palliative care in caring for such
patients. This indicates that one of the key outcomes identified at the outset, i.e. increased
understanding of the role of palliative care amongst referrers, has been achieved. The majority of
referrals came via the clinical nurse specialists’ links with heart failure and respiratory nurse
specialists and reflected the diverse ethnic community in which St. Lukes is based.
This work has helped to provide a more equitable service to those patients with end stage, long term,
non-malignant conditions. It increased awareness amongst patients, carers and family of the role
palliative care services can play alongside medical management for this patient group. Patient and
carer evaluation forms indicated that views and perceptions of the hospice had been changed by
attending the Sowing the Seeds course. Information given during the sessions increased patients and
carers knowledge regarding the benefits and services available. Strategies for managing symptoms
will have empowered both patients and carers. Within the organisation, awareness has been raised of
the increasing role for palliative care in caring for patients with non- malignant conditions. In the wider
health community the profile of palliative care for such patients has also been raised. Health care
professionals’ knowledge and understanding of palliative care has increased for this group of patients
and will prompt them to refer patients earlier in their disease trajectory.
Staff involved in the ‘Sowing the Seeds’ project have increased their own knowledge and
understanding of non- malignant conditions. This will enable them to act as a resource for the
hospice, sharing this knowledge with those not directly involved. The work to promote a palliative care
approach to patients with non- malignant conditions continues, with joint working and initiatives with
clinicians in the local secondary care Trust.
(4) Hospice at Home Volunteers project
The Hospice at home team recognised that sometimes highly skilled professionals were undertaking
tasks that may be carried out by appropriately trained volunteers. Volunteers were already being used
successfully in clinical settings on the IPU and Day Care. They wanted to ensure that the service was
operating both efficiently and effectively, giving the most appropriate care to patients. Funding was
made available from the St. James Foundation enabling recruitment and training of sufficient numbers
of volunteers to assist with care of our diverse patient group.
Two Open Days were held for prospective volunteers at St Lukes in September 2012 and March 2013, at
which prospective volunteers were introduced to our Hospice at Home service and told how their integration
within it would enhance our established service. Each potential volunteer received an information pack
containing role descriptions and training programme. The first wave of volunteers has attended the required
mandatory and informal training sessions alongside a practical demonstration of ‘how to perform a bed bath’.
Opportunity was made available for the volunteers to practise this procedure (on a willing nurse).
These volunteers are now visiting patients under the direct supervision of the Registered Nurse, offering
support to the family carer. Feedback from this small group of families has been positive which demonstrated
the value of this new service. This service is providing specialist care giving confidence to carers to enable
them to leave the patient and socialise, which they may not feel confident to do with generic agencies. A
second open session was held in March with 6 new volunteers commencing their training in May.
It has proved challenging to recruit the ‘ideal’ volunteer who has appropriate skills or who has an interest to
learn new skills, despite using a wide range of advertising media plus the St. Luke’s website. St Lukes is
situated in a richly diverse area of North West London with a large multi-cultural population and it would be
good for volunteers to match that diversity.
(5)
Day Care Review & Re-Organisation of Day Care Activities
7
Several mitigating circumstances identified the need to review Day Care Services. The 2010-11
external Patient Survey produced some comments from patients regarding the time they spent on day
care unit when active medical treatment was not being given. There was also some concern that the
service was not being fully utilised. Then, there was another cohort of patients who had completed
their three month episode and, although no longer clinically dependent, because of the complexities
of their condition could benefit from continued attendance. In order to ensure that there are patient
led outcomes, the Day Care clinical staff carried out several patient focus groups to ascertain the
views and suggestions of day care patients. An action plan was developed taking into account
patient views.
Following this review, we have reviewed patient activities and recruited additional volunteers to
enhance the complementary therapy service for Day care, and also to offer art and craft activities to
patients. We also developed “themed” days for patients, celebrating the Queens Diamond Jubilee
and the London 2012 Olympics with activities related to these national events. Patients appear to
benefit from distraction from their illness or condition by engaging in different activities and are always
keen to participate. This also allows patients to focus upon their quality of life and build social
support from their peers.
The majority of patients that attend have complex physical symptoms, which are followed up by the
nursing team who refer to the medical team for treatment or a review of medication. Co-ordination of
care is maintained with the other Health Care Professional involved in the patient’s care.
To fully utilise the Day Care Service, an additional day was added to provide care for patients’ with
long term chronic degenerative diseases who have complex problems. A pilot study is being held for
these patients’ using the Palliative Care Outcome Scale to assess their physical and psychological
symptoms.
“Really thankful and grateful for all the support that I have from you…”
Quality and Performance:
The latest CQC review 2012 resulted in the following statement. All reviews can be seen on
the CQC website.
‘Staff were competent and very kind, and they were very happy with the care they received.
They said they could choose their meals and have something to eat and drink whenever
they wanted. They told us staff always consulted them and involved them in making
decisions about their care and support needs.
Comments from patients included "I feel involved deeply, these people are a class above,
their attitude and understanding proves to me this is the right place", "I feel the staff
understand my needs" and "you are not just a number, but a person".
Patients confirmed that staff provided them with choices, listened to them and explained
clearly all care and support options. They told us that they were offered a choice of
activities which they could participate in if they wanted to or choose not to and their
decision was always respected. Patients provided us with examples of activities that they
enjoyed.
Patients told us that staff protected their privacy and dignity. They told us that they felt safe
as a patient cared for by the hospice and knew who to talk to if they had a worry or
concern.
During our visit we saw staff interact with people in a respectful and sensitive manner.
8
Staff spoke of enjoying their job supporting and caring for people in the hospice. They told
us there was good staff teamwork and they felt well supported by the manager and by
other staff.
The hospice had monitoring systems in place to ensure that the service provided to people
was always a quality service”.
3.1 Review of Activity and Performance
St Luke’s Hospice – total services
2012 has seen a marked increase in activity across most services. St. Luke’s services
support the local aim to keep patients out of hospital where appropriate.
3.1a
Inpatient Unit Services 2012– Brent & Harrow
IPU Activity 2012 - Brent & Harrow
900
800
700
600
500
400
300
200
100
0
770769
613603
Q1 2012
Q2 2012
Q3 2012
Q4 2012
73 72 81 79
9
Beddays
Patients
9 10 10
Ave LoS
“There are no words to give my thanks for the holistic haven of good card you have
given my father….. Every single person he has met here has been friendly, helpful,
smiling, caring, empathetic or treating him with respect and dignity” (IPU patient)
3.1b
Day Care & Outpatient Services 2012 – Brent & Harrow
9
Day Care Activity 2012 - Brent & Harrow
700
623
600
593
Q1 2012
467 482
500
Q2 2012
400
Q3 2012
300
Q4 2012
200
88
66
100
87
0
0
Patients
Booked attendencies
(No information on patient numbers for Q2)
“*** spoke with such thanks for all the friendship, support and professional help she
received throughout the time she spent at St. Lukes. She loved, laughed, cried and lived
with you all” (Day Care patient)
3.1e Hospice At Home – Brent & Harrow
120
100
Hospice at Home Referrals 2012 - Brent &
Harrow
89
81
84
85
80
60
2012
40
20
0
Q1
Q2
Q3
Q4
“Many, many thanks for your support during my husband’s illness. It was a great
relief to know that I could call on you. My grateful thanks to the Hospice at Home
team, who were marvellous carers” (community and HatH patient)
3.2f Community Services - Brent North
10
Brent North Community Caseload - 2012
200
182
156
150
104 102
116 117
125
138
141
153 160 160
100
year 2012
50
Jan
Feb
Mar
Apr
May
Jun
Jul
Aug
Sept
Oct
Nov
Dec
0
“We want to say a big Thank you for all your kindness – without it I could not
have coped. You were there always for us! Much appreciated and never
forgotten” (community patient)
3.1g Family Services and Support
“Thank you for all your help and support, your kindness, thoughtfulness and dedication in
caring for Uncle and our family. It is very much appreciated not only by myself but all the
11place because of people like you.
family too. The world is a better
3.1h
Bereavement Support
Bereavement Service Statistics 2012
350
Deaths
300
250
Service Users Accessing
Support
258
200
Bereavement Telephone
Support Sessions
150
100
Bereavement Support Oneto-One Sessions (Staff and
Volunteers)
50
0
“Feel good I am not only one in this world. Someone is there for me”
3.2
Quality Markers
Below are the quality markers St. Lukes have been using to demonstrate our commitment to
maintaining quality services. The infection control ones are mandatory .
12
Number of patients admitted with MRSA
2
Number of patients contracting MRSA
when in the hospice’s care
0
Number of patients admitted with C
Difficile infection
1
Number of patients contracting C Difficile
infection when in the hospice’s care
0
No of Falls Minor
30
No. of falls Major
1
Number of formal complaints received
0
Number of required actions specified by
the Care Quality Commission
0
Number of recommendations made by
the Care Quality Commission
0
For 2013 we will be introducing new local quality markers for the hospice.
Ethnicity monitoring to embrace the
diversity of the area we serve and ensure
promotion of equal access to hospice
services
Patient Reported Outcomes in Day Care,
showing where improvement has been
achieved through attendance to Day Care.
3.3 Clinical Audit
As one of its priorities for 2013, the hospice is reviewing its internal audit programme with
the further development of the Clinical Audit Group. The group will be developing tools to
aid staff with proposal of new audits, updating of current audits and measurement standards
attached to them and prioritising which audits should be carried out within constrained
resources. The group has also identified that training would be beneficial to all staff to give a
better understanding of the advantages of robust audits and promote quality assurance.
Audits carried out in 2012
Pharmacy provision and Medicines Management
MRSA/C.Diff incident reporting
Patients acquiring Pressure Sore
Management and prevention of Sharps injury
Toilet/Bathroom Cleaning
13
Hand washing
Telephone Advice Service
Patient Care Documentation across all services
All audits are followed through with action plans and monitored accordingly with changes to
practice made or training sessions provided where necessary.
Audit Reports will be presented to staff and Board of Trustees to inform any possible service
developments, necessary changes to practice and policies, training needs and indeed to
compliment all staff on areas of good performance.
3.4 Training and Education
St. Lukes is a keen advocator of education, training and professional development for all
members of the multi-disciplinary team (MDT)
Various members of the MDT contribute to the design, implementation, delivery, facilitation
and support of education. Inter-professional education can break down barriers between
health care professionals groups and promote learning from and with each other (NHS Plan
2000). Interdisciplinary function is generally the aim of specialist palliative care teams with
members contributing from their particular expertise (Crawford & Price 2003) to offer the
best quality of life for the inpatient (Johnston 2005)
Inter-professional learning can be more effective in clinical settings not classrooms, where
students are dealing with real life situations (Finch 2000) and because different health care
professionals commonly meet and work together rather than independently usually for the
common aim of patient care. And so learning is delivered with a classroom setting and in
the clinical areas.
3.4a
TRAINING PROGRAMME
In-house training programmes to meet the needs of those new to working within
palliative care, including nurses (RNs and CNS) and social workers
The Palliative Care Development Programme (PCDP) for registered nurses
Social Work Palliative Care Development Programme – newly qualified social
workers or those new to palliative care, developed in house
CNS Development Programme
Further Development of existing Clinical staff to working within St. Lukes
Senior Health Care Development Programme in Specialist Palliative Care,
developed in house – new, innovative programme to extend the role of HCA’s who
are already qualified to NVQ 3 level (or equivalent).
Intravenous Drug Administration Training
Mentorship Training and Support
Presentation skills training – 2 half-day workshops for senior clinical staff
14
Weekly Doctors Clinical governance session
Clinical Support
Clinical Supervision
Other Training for all members of the Multi-disciplinary team
Monthly Clinical teams education session
Basic Communication Skills
Monthly Multi-Disciplinary ‘Topic’ Teaching
Mandatory Training Calendar
Further Training for external Health Care Professionals.
Medical students mentored and coached
GP registrars mentored and coached.
Principles of Palliative Care {degree level} Module’ (accredited by University of
West London) Open to Registered Nurses and Allied Health Professionals, for
hospice staff and external healthcare workers who wish to increase their
knowledge in end of life care
Pre-registration Student Nurses Placements
Half Day Study day for GP Training Scheme
Pre and Post Graduate social work students
Education sessions for End of Life issues for Nursing Home nursing staff
3.4b Staff Development and Training Achievements 2012
o
6 x HCAs completed the senior HCA programme
o
2 x 6-month training placements for GPs
o
Ward manager completed BSc in Palliative Care Nursing
o
11 x external students passed the Principles of Palliative Care module and
7 x internal students (hospice staff) passed the module also.
Each was awarded 20 credits at level 6 by the UWL.
o
Senior Nurse Manager completed Masters degree in Management & Leadership
o
15 x Medical students mentored and coached
o
12 x GP registrars and 1 Trustee mentored and coached.
o
1 x Trustee mentored and coached.
o
14 X Student Nurses Placements
o
1 x HCA completed Edexcel level 3 Diploma in Health & Social Care at Stanmore
College
o
Nursing Home training – 60 participants over four month period.
15
3.5 Service Improvement Projects
The hospice has been requested by the Harrow CCG to work with other providers to support
improvement in the commissioning of local End of Life Care services through development
of a new integrated model for delivering these services to Harrow patients.
Development of Heart Failure and Frail Elderly palliative care services.
“Thank you so much for your empathy, kindness and professional
help and care of our dear Mother. Words cannot express our
gratitude. We will never forget your generous and kind nature, from
the bottom of our hearts we thank you again2
A huge thank you for looking after our Mother. You made her final days so much more
bearable with your loving care and attention, not to mention helping us, her family, by
providing endless cups of tea and kindness.
3.6 Feedback from Clinical Commissioning Groups and
stakeholders
(a)
Brent Clinical Commissioning Group
To date, only informal comments received from the newly appointed Brent
commissioner. (to be updated at future date)
(b)
Harrow Clinical Commissioning Group
No response from Harrow
(c)
Harrow Healthwatch
“Thank you for inviting Healthwatch Harrow to make its response to St Luke’s
Hospice 2012/13 Quality Accounts.
16
We are pleased to read about the good work the Hospice has done during the last
year and wish it all the best in achieving its objectives set out under the heading of
‘Service Improvements, priorities for 2013’ in the Quality Accounts.
We are keen to work with you in our monitoring capacity as well as a critical friend by
providing feedback and support where practical.
Yours sincerely,
Ash Verma
Interim Chair, Healthwatch Harrow”
(d)
Brent Healthwatch
“Healthwatch Brent has only been in existence since April 1 2013. We have not yet
had chance to ask patients from St Lukes about their experiences there so these
comments are based solely on reviewing the quality account we received from St
Lukes. We are pleased to say that St Lukes QA was the only one we received
directly from a provider. They had obviously made an effort to ensure that we
received the account. We found the report to be coherent and clearly written with a
wealth of evidence included to back up statements. The description of the value
provided by volunteers was clear and appropriately acknowledged. We particularly
found the patient testimonies useful. There was a clear explanation as to how
patient and carer feedback obtained had informed strategic priorities. We also found
that the report was clear on how the priorities from 2012 had been actioned and what
else remained to be done. The report showed how quality underpinned the work of
St Lukes. There was a clear explanation as to why certain sections were not relevant
and why. The report will be a useful benchmark for Healthwatch Brent against which
to compare other providers’ reports.”
Best wishes
Ann O’Neill
Executive Director
17
BELOW ARE THE MANDATORY STATEMENTS REQUIRED FOR
QUALITY ACCOUNTS UNDER THE NHS (QUALITY ACCOUNTS)
REGULATIONS 2010 AND NHS ACT 2006 AND SUPPORTING
REGULATIONS, FOR ALL NHS FUNDED SERVICES.
4.
STATEMENT OF ASSURANCE FROM THE BOARD
The following are a series of statements that all providers must include in their Quality
Account. Many of these statements are not directly applicable to specialist palliative care
providers
4.2a.
Review of Services
St. Lukes provides the following services which are jointly funded through charitable
contributions and the NHS.
Inpatient Unit
Medical Outpatients
Hospice at Home
Day Care Unit
Specialists Community Services – North Brent
Family Support Services, including bereavement support services
In addition the hospice has provided the following services through charitable funding or
grants only:
4.2b
Complementary Therapy and Physiotherapy Services
Carer Support Services
Participation in National Clinical Audit
As a voluntary provider of specialist palliative care St Luke’s Hospice is not eligible to
participate in any of the national clinical audits or national confidential enquiries. This is
because none of the 2012 audits or enquiries related to specialist palliative care.
The Hospice will also not be eligible to take part in any national audit or confidential enquiry
in 2013 for the same reason.
However, the hospice does take part in a biennial national patient survey, administered by
Help the Hospices and Kent University, which enables the hospice to be benchmarked for
quality against other providers. We will be taking part in this survey between September
2012 – May 2013.
We also have an internal audit programme.
18
4.2c.
Research
St. Lukes is not currently involved in any research programmes.
4.2d.
Use of the CQUIN payment framework
As part of the NHS National Contract, St. Lukes is part of the CQUIN payment framework. A
proportion of St. Luke’s income in 2012 was conditional on achieving quality improvement
and innovation goals agreed between NHS Brent and Harrow and St. Lukes. These are
currently related to Advanced Care Plans and Preferred Place of Care/Death.
What this means?
2.5% of our NHS payment is non-recurrent and dependent upon the hospice reaching the
identified target performance.
4.2e.
Care Quality Commission
The CQC register St Luke's Kenton Grange Hospice Harrow & Brent to carry out the
following legally regulated activities:
Transport services, triage and medical advice provided remotely
Treatment of disease, disorder or injury
Diagnostic and screening procedures
Ms. Geraldine Burke is responsible for these services as the Registered Manager and
Responsible Individual under the Care Quality Commission (Registration) Regulations 2009,
and Health & Social Care Act 2008
Where they are registered to do this:
St Luke's Hospice Kenton Grange Hospice Harrow & Brent
Terms of this registration relating to carrying out this regulated activity
The Registered Provider must ensure that the regulated activity transport services, triage
and medical advice provided remotely is managed by an individual who is registered as a
manager in respect of that activity at or from all locations.
4.2f
Data Quality
As a voluntary provider of Hospice Care, St Luke’s Hospice does not submit records to the
Secondary Users service for inclusion in the Hospital Episode Statistics. However, we do
provide quality and activity statistics for contract monitoring, for statutory financial annual
reports and for various bids for funding.
19
4.2g. Information Governance Toolkit attainment levels
St. Luke’s score for 2012 for information Quality and Records Management was not
assessed using the Information Governance Toolkit. This toolkit is not suitable for our
systems
4.2h. Clinical coding error rate
This information is not relevant for the Hospice to provide. As a voluntary sector provider of
Hospice Care services we do not subscribe to the Secondary Users service for inclusion in
the Hospital Episode Statistics. We are currently on block contract and provide activity data
for information purposes only.
20