Quality Accounts 2012-13

Quality Accounts 2012-13
Contents
Part 1: Statements on Quality from Trust Special Administrator ........................... 4
Part 2: Looking forward – Priorities for Quality Improvement 2013-14 ................ 5
Statement of Assurance on NHS services provided at SLHT ................................ 14
Review of 2012/13 Priorities for Improvement ................................................... 15
Staphylococcus Aureus
(MRSA) ........................................... 34
Goals agreed with commissioners – using CQUIN framework .............................. 69
SLHT Quality Accounts 2012-13 Page 2 of 95
Part 4: Auditor’s assurance report ....................................................................... 95
SLHT Quality Accounts 2012-13 Page 3 of 95
Part 1: Statements on Quality from Trust Special Administrator
I am pleased to present this year's Trust Quality Account, albeit in the difficult circumstances surrounding the Trust's placement in the Unsustainable Provider
Regime and the planning for the dissolution of SLHT before the autumn. I would like to place on record a tribute to the staff of SLHT who for the past four years, set against a challenging financial environment, have consistently pushed forward the quality of care.
Low infection rates have become embedded at SLHT's hospitals and we have improved mortality rates. The challenge for everyone involved in the transition and the new organisations is to make sure that these gains are protected and moved forward. At the same time, the integration with new organisations is an opportunity for us all to learn from the best practice and culture of each other. In line with the recommendations of the Francis Report this must happen, and from my short period at SLHT I have seen the staff respond positively to the challenge in spite of the personal uncertainty that the transition entails.
In the past year there has been good progress on some of last year's priorities including an overall reduction in the total number of hospital acquired pressure ulcers, and excellent progress on VTE patient risk assessment and implementation of prophylaxis. Within the last two months of the year we have also achieved the national targets for Dementia screening and referral. This Quality Account again identifies these as key priorities, alongside continued work on falls prevention with a focus on reducing the level of harm. In support of the recommendations from the
Francis Report and the 6 C‟s outlined in the Nursing Strategy „Compassion in Practice‟ by the Chief Nursing Officer NHS England, we have identified a priority that focuses on care delivery with compassion and empathy.
The results from the 2012 National Inpatient Survey identify the need for a continued focus on some key areas that have a direct impact on the patient‟s overall experience. These results are being shared at every level within the organisation to develop a meaningful response with the required commitment to make the necessary changes in practice to improve the patient‟s experience. For the remaining lifetime of the Trust, I will make sure that these issues continue to be addressed.
I know that the Trust has worked effectively with patient representatives, through
LINKs and the Patient Experience Strategy Group. The joint work on cleanliness has for example had a major positive impact on environmental cleanliness and low infection rates.
I think it is hugely important that these relationships are maintained and that this collaborative work continues in the new organisations.
SLHT Quality Accounts 2012-13 Page 4 of 95
To the best of my knowledge, the information in the document is accurate.
Caroline Taylor, Trust Special Administrator
Part 2: Looking forward – Priorities for Quality Improvement 2013-14
2.1 Priorities for Improvement
When setting the priorities for improvement in 2013-14 a number of factors have been considered. We will continue to focus on those 2012-13 priority areas that we have made progress on, but which require further efforts to achieve sustainability.
We have also taken into consideration:
Key emerging theme from the Francis Report in relation to delivering care with compassion
Results from the National Inpatient Survey
Internal discussions within SLHT
Key areas for improvement as outlined by our commissioners and the Local
Involvement Networks
2.1.1 Patient Experience:
Nurses delivering care with compassion and empathy
Why have we chosen this measure?
We acknowledge that it is every staff member‟s responsibility to deliver the care they give with compassion and empathy and we will continue to challenge behaviours and attitudes when they are not in line with our Trust values. We have decided this year to have a particular focus on the nursing workforce which includes health care assistants (HCAs).
We believe that the majority of our nurses are caring professionals who are committed and deliver compassionate care. However, findings from the Francis
Report (chapter 23 focusing on nursing), outlines fundamental failures within care delivery and acknowledges that these failures are not limited to one organisation.
Why is this important?
The results from our National Inpatient Survey 2012 shows that we are in the bottom 20% of Trusts in meeting patients‟ expectations in terms of having confidence in the nurses treating and caring for them. Patients have also told us that the emotional support that they are receiving could be improved.
SLHT Quality Accounts 2012-13 Page 5 of 95
What we will measure
Patient’s confidence in nurses’ caring for them
Nurses delivering care with compassion and empathy
How we will measure it
Gaining feedback from interactive sessions with patients e.g. Fishbowl sessions
Senior Nurses (Ward Manager and above) seeking patients, carers and relatives feedback regularly and showing evidence of feedback received and actions taken
Evidence of comfort rounds and Matron‟s ward rounds and actions being taken as a consequence. Evidence of monitoring through site based leadership teams.
Feedback from Executive Team walkabouts
Comparison of numbers and themes from complaints and PALs enquiries
Evidence of learning in practice from complaints
Feedback from the Friends and Family Test and a range of inpatient surveys
Feedback via internet
SLHT Quality Accounts 2012-13 Page 6 of 95
2.1.2 Friends and Family Test
Why have we chosen this measure?
As part of a national initiative from the Department of Health, the Trust has been implementing the „family and friends test‟. As part of this initiative we are required to ask 100% of inpatients who are discharged from hospital and 100% of adult patients who have attended A&E and who have been discharged from A&E without being admitted to hospital the following question: How likely are you to recommend our ward/A&E department to friends and family if they needed similar care. There are 6 possible responses to this question ranging from extremely likely to extremely unlikely and don‟t know. Patients are also asked to indicate the main reason for their answer which includes a range of options including: cleanliness, waiting time, compassion and empathy and staff attitude and behaviour. The results from the questions are reported externally to the Trust and are available to the public to review. From the autumn of 2013 this will be rolled out into midwifery services.
Why is this important?
It is important for us to understand the overall experience that patients have had in our care. It is anticipated that the results from the questions and the follow up questions will provide a mechanism to identify poor performance and to encourage staff to make improvements where services do not live up to expectations of our patients.
What we will measure
The total number of responses to the question for patients who have been discharged from hospital
The total number of responses from patients who have been discharged from A&E
The total number of responses from individual wards and departments
The responses to the follow up questions which will enable us to identify areas for improvement
How we will measure it
We are using a range of methods to facilitate patient feedback as follows:
The use of Ipads in the A&E departments, discharge lounges and wards.
The use of cards to complete for patients to complete prior to their discharge from hospital- these are available in the Trust but are also included in the patients discharge medication
The ability of patients to provide feedback from home using the icon on the Trust internet site.
We have the support of volunteers to encourage patients to provide responses to this question.
SLHT Quality Accounts 2012-13 Page 7 of 95
2.1.3 Care of patients with dementia
Why have we chosen this measure?
We are responsible for delivering high quality care to patients with dementia and for ensuring that we are supporting and meeting the needs of carers. Significant progress has been made in quarter 4 of 2012-13 in terms of screening, risk assessment and referral, if required, for specialist diagnosis. In 2013-14 there will be a continuing focus on the complete dementia pathway to build upon the work already done at the PRU and QEH sites.
Why is this important?
Improving the care of patients with dementia in general hospitals is a national
CQUIN, concern and priority. Research and audits have demonstrated the need for transforming the care that these patients receive and supporting dignity in care for elderly patients. A significant aspect of this is ensuring that the nutritional and hydration needs of elderly patients are met and that practices at mealtimes provide as supportive an environment as possible to facilitate this.
What we will measure
Dementia screening
Dementia risk assessment
Referral for specialist diagnosis
Experience of carers
How we will measure it
% of all patients aged 75 and over who have been screened following admission to hospital
% of all patients aged 75 and over, who have been screened as at risk of dementia, who have had a dementia risk assessment within 72 hours of admission to hospital
% of all patients aged 75 and over, identified as at risk of having dementia, who are referred for specialist diagnosis. Target 90% for all measures by site each month.
Quarterly surveys of carers experience
Implementation of protected mealtimes
Quarterly audits of a sample of case notes of elderly patients / patients with dementia focusing on evidence of meeting nutritional and hydration needs and the use of the Malnutrition Screening
Tool (MUST)
Collaborative Protected mealtime audits with external stakeholders to include the use of Red
Trays
SLHT Quality Accounts 2012-13 Page 8 of 95
2.1.4 Emergency Care Pathway
Why have we chosen this measure?
The emergency care pathway is crucial in ensuring that patients are treated and managed by the right person, at the right time within the right environment. The timeliness of the treatment and / or intervention is vital in ensuring the best possible patient outcomes and experience. This relates not only to patients discharged from the emergency department but also to those patients requiring an inpatient admission to one of the admission units and / or speciality inpatient wards.
Why is this important?
The Trust has struggled to sustainably deliver against the 4 hour wait target and unloading patients from ambulances within the specified times due to limited capacity during periods of high activity. Both Accident and Emergency (A&E) departments have seen increases in attendances and for some months a higher level of acuity in those attending. There are multiple factors that impact on the Trust‟s ability to deliver against this target and it is recognised and acknowledged that this is a wider health economy issue and thus requires a fully integrated response with commissioning and social care partners.
To ensure that our patients receive the highest quality treatment and care as quickly as possible we need to deliver against this target consistently.
What we will measure
Accident and Emergency department performance targets
Patients‟ experience within the
Accident and Emergency department
How we will measure it
Accident and Emergency department performance indicators included in the
Quality & Safety report
National Emergency department survey
Friends and Family Test
Local surveys
Themes within complaints
SLHT Quality Accounts 2012-13 Page 9 of 95
2.1.5 Quality of discharge and information provided
Why have we chosen this measure?
Feedback from a range of stakeholders including our patients, community partners, our commissioners, GPs and Healthwatch (formally LINks) have highlighted poor standards of discharge in a range of areas including: quality; timeliness and lack of discharge summaries; lack of appropriate referrals to community nurses; and lack of patients understanding of medications on their discharge.
The National Inpatient Survey results from 2012 indicate the ongoing need for improvement in all indicators related to discharge from hospital. This triangulates with complaints that have identified poor discharge as a theme.
In addition the Trust has received a number of quality alerts and safeguarding alerts which have identified concerns with discharge arrangements from SLHT.
Why is this important?
Arguably discharge from hospital is the most crucial part of the patients‟ pathway. It is critical to provide a safe and comprehensive handover to other Heath and Social
Care Partners in order to support ongoing care and promote independence.
What we will measure
Effective communication to GPs and Health and Social Care
Partners on discharge
To ensure that patients and/or their carers are provided with all of the information they need to support them when they are discharged
How we will measure it
Feedback from Commissioners, GPs and community partners
Monitor themes highlighted in quality alerts, safeguarding alerts and complaints receive
The national patient surveys of in-patient care
Emergency Department Surveys
National Maternity Survey
Feedback from patients from
real time feedback using iPads.
Feedback from the Friends and Family Test
Audit of discharge summaries
Report on quarterly readmission rates
SLHT Quality Accounts 2012-13 Page 10 of 95
2.1.6 Venous Thromboembolism (VTE)
Why have we chosen this measure?
The key focus of this priority remains the reduction of avoidable death, disability and chronic ill health. Significant progress has been made over the last two years on ensuring patients have had the appropriate risk assessment, making sure patients are prescribed appropriate medication and given information about VTE. These measures will continue to be monitored but in 2013/14 the focus will also be on completing Root Cause Analysis (RCAs) on confirmed cases of pulmonary embolism and deep vein thrombosis that are acquired in hospital.
Why is this important?
VTE prevention remains part of the national CQUIN scheme with the aim of wherever possible reducing avoidable death, disability and chronic ill health from VTE.
What we will measure
% of all adult inpatients who have had a VTE risk assessment on admission to hospital using the clinical criteria of the national tool
(target 95%)
How we will measure it
Continue to report on UNIFY and SLHT‟s Quality and Safety Report
Completion of Root Cause
Analysis (RCA) Reports
Number of RCAs reports completed against the actual occurrence of hospital acquired VTE and evidence of learning / changes in practice
SLHT Quality Accounts 2012-13 Page 11 of 95
2.1.7 Clostridium difficile Infections (CDI)
Why have we chosen this measure?
SLHT has always aimed to drive forward improvements in reducing healthcareassociated infections (HCAI) to ensure that patients receive safe care that conforms to nationally agreed best practice, and which leads to reductions in the incidence of
CDI and MRSA. Although SLHT has met this aim, we breached our agreed trajectory by 3 cases of CDI and therefore we need to ensure continued focus for 2013/14 to achieve continued reductions in incidence of CDI. Priority actions are being taken to ensure focus on prescribing, hand washing, the environment, isolation and surveillance.
Why is this important?
SLHT wants to continue to ensure that patients who use our services are less likely to acquire CDI compared with other similar organisations and that they will have confidence that this would be the case when using our services.
What we will measure
Number of patients acquiring
Clostridium difficile
infection
Progress against SLHT‟S Infection
Prevention Programme 2013-14 and action plans
How we will measure it
Each case is confirmed by microbiology and reported within SLHT‟s Quality and Safety report
Monitoring of programme and action plans at the Infection Prevention Committee
SLHT Quality Accounts 2012-13 Page 12 of 95
2.1.8 Prevention of Pressure Ulcers
Why have we chosen this measure?
Over the previous three years SLHT has made significant progress in reducing hospital acquired pressure ulcers (HAPUs). This is particularly the case for grade 3 and 4 pressures ulcers whereas grade 2 ulcers remain a challenge for us. Evidence from the NHS Safety Thermometer pilot data suggests that it is possible to achieve a
50% reduction by having strong and focussed leadership, by using high quality evidence e.g. NICE guidance and resources from the Harm Free Care programme and by working across the local health and social care economy.
Why is this important?
Most pressure ulcers are preventable and our data from last year demonstrates that we still have improvements to make in reducing our grade 2 pressure ulcers and maintaining a zero tolerance for grade 3 and 4 ulcers.
What we will measure
Zero tolerance for grade 3 and 4 ulcers
How we will measure it
Actual numbers of hospital acquired pressure ulcers monthly by grade
Reducing grade 2 ulcers by at least 30% in 2013/14
Root Cause Analysis (RCA) of all grade 3 and 4 ulcers and a sample of grade 2 ulcers (each month) using a modified RCA tool to identify key learning and determining if ulcers were or were not preventable
SLHT Quality Accounts 2012-13 Page 13 of 95
2.2 Statement of Assurance on NHS services provided at SLHT
During 2012-13, SLHT provided a wide range of hospital services for patients in
Bromley, Bexley, Woolwich and other areas at three main sites. These comprise the
Princess Royal University Hospital in Bromley, Queen Mary‟s Hospital, Sidcup and
Queen Elizabeth Hospital, Woolwich. The Trust also provides services at Orpington
Hospital, Beckenham Beacon and Erith Hospital.
SLHT has reviewed all the data available on the quality of care in all of these NHS services, through our performance framework and clinical governance arrangements
.
The income generated by the NHS services reviewed in 2012-13 represents 100 per cent of the total income generated from the provision of NHS services by South
London Healthcare NHS Trust for 2012-13.
SLHT Quality Accounts 2012-13 Page 14 of 95
Part 3: Looking back – Review of 2012/13
3.1 Review of 2012/13 Priorities for Improvement
In our Quality Account for 2011-12 we prioritised a number of areas where we wanted to focus our quality improvement efforts. In this section, we look back at our performance over the last 12 months to identify those areas where we achieved our objectives and those where there is still room for improvement.
Our priorities for improvement in 2012/13 were chosen following discussion in the
Trust and with the Local Involvement Networks. They also reflect the priorities in the
Commissioning for Quality and Innovation (CQUIN) schemes, which were agreed with our commissioners.
3.1.1 Patient experience
What we measured How did we measure it
Patient‟s rating of hospital food
Patient‟s experience of leaving hospital: Making sure patients understand their medicines and any side effects
Organisation of out-patient clinics
Making sure staff support patients with any worries or fears they might have
The national inpatient surveys of in-patient care and care in our Emergency Departments.
Our patient experience iPads have been used to provide us with
real-time patient feedback
with tailor-made questions for individual services.
For our internal surveys that provide us with real time feedback from patients we have continued to work with volunteers and LINk colleagues who have supported patients to provide feedback.
SLHT Quality Accounts 2012-13
What did we do and what was our Performance in 2012/13
Page 15 of 95
Our key priorities were:
Patient‟s rating of hospital food
There are three questions that relate to food and nutrition as part of the
National inpatient survey as follows:
How would you rate the quality of hospital food?
Were you offered a choice of food?
Did you get enough help from staff to eat your meals?
The results from the 2012 National inpatient survey indicate a continued requirement for us to make improvements to the quality of food for patients.
Our score for the question related to quality is in the 20% of worst performing trusts. We have scored about the same as other Trusts for the questions relating to choice of food and getting enough help from staff.
In the past year there has been continued focus through the Corporate food and nutrition steering group on a range of initiatives to support patient‟ rating of the quality of food. The group agreed a trust wide catering Strategy which sets out 10 Trust wide principles for delivering a good patient meal service across the whole of South London Hospital premises. The ten principles include the use of red trays, protected mealtimes, and the use of plate covers for patient meals.
There has been a review of the content of the menus on each site and a range of changes have been implemented over the year to standardise and improve the quality of food for patients. New Menus were introduced on to the PRUH site in July 2012 after a lengthy consultation which included LINk colleagues. Our catering providers have introduced a new hand held electronic system for collecting menus across the Trust which are been implemented. These will ensure timelier ordering of food to meet patient choice. The Trust has a structure for the monitoring and assurance of catering services using a site-based approach. The types of auditing that the
Trust undertakes are:
Contractor catering audits
Trust Food audits
Patient Forum Food Audits
Quarterly PEAT inspections
Annual National Patient Satisfaction Audits
The results from Internal audits relating to the quality of food have been more positive compared to the results from the National inpatient survey, however it is clear that continued effort is needed to improve the overall quality of food that patients have in hospital.
SLHT Quality Accounts 2012-13 Page 16 of 95
Our key priorities were:
Patient‟s experience of leaving hospital
What did we do and what was our Performance in 2012/13
There is a whole section in the National inpatient survey that relates to
„Leaving hospital‟ that includes 15 questions around all aspects of the discharge experience, including questions relating to medication on discharge. For seven of those questions our scores are in the bottom 20% of worse performing Trusts; this includes the question relating to patients understanding their own medicines. The scores for the remaining questions are about the same as other Trusts.
A discharge action group was established last year to address some of the concerns and feedback relating to discharge from hospital. Membership of this group included external colleagues from LINk and other health and social care staff from a range of services. A hospital discharge book was revised by the group and is now being used in practice to support patients and their families with the complexity of discharge planning. The book holds details that are relevant and personal to each patient and forms a record of advice for them. In addition to this booklet a patient information leaflet was developed to provide patients and family/ carers with key information relating to their hospital stay and to prepare them for discharge from hospital.
Making sure patients understand their medicines and any side effects
A number of actions were taken to support patients with their discharge medication which were supported by the Trust Chief Pharmacist.
The overall aim of the work was to ensure that all patients are issued with a personalised discharge summary which includes pertinent information relating to a range of issues for example; important test results, diagnosis/explanation of what happened, any outpatient appointments required, advice on self-care and/or prevention of reoccurrence, brief medication explanation and schedule, telephone number to call with questions or concerns.
An example of some of those actions that were taken are as follows:
Promotion of medicines information service and helpline across SLHT- this service provides a help line for patients that they can call for support with any questions relating to medication. A card is placed in every patients discharge medication.
Identification of high risk drugs so that pharmacy staff provide counselling on these drugs to patients at discharge.
There has been continued effort on improving the Interface with junior doctors to ensure that discharge medication is written in a timely fashion.
This would allow patients can be counselled with their medication.
SLHT Quality Accounts 2012-13 Page 17 of 95
Our key priorities were:
What did we do and what was our Performance in 2012/13
Organisation of out-patient clinics
As part of our plans to improve the organisation of outpatients a full review of administrative functions was undertaken to ensure that patients have clear points of contact in relation to the organisation of their outpatient appointment.
In addition to this there has been continued focus around reducing wait time for appointments for patients. The Trust is compliant with the 95% non admitted referral to treatment standard. (RTT)
Making sure staff support patients with any worries or fears they might have
There is one question in the National inpatient survey relating to this issue as follows: Did you find someone on the hospital staff to talk to about your worries and fears? The scores for this question places us in the bottom 20% of worse performing trusts.
To support patients in raising any worries and anxieties that they may have when they are in hospital this question was added into a document that is used to undertake „comfort rounds‟ that are carried out in all wards during the day.
The aim of a comfort round is to ensure that every patient is reviewed on at least a two hourly basis and that they are supported with any care needs that may be required immediately, which may include the provision of a drink or support in going to the toilet. Staff have been encouraged to integrate this question into this round so that patients realise that they are able to share any concerns that they have.
SLHT Quality Accounts 2012-13 Page 18 of 95
3.1.2 Care of Patients with Dementia
The care of patients with dementia was a national CQUIN in 2012/13 and continues to be a national CQUIN and priority for 2013/14. Our performance against this priority is detailed in the table below. Although we didn‟t fully meet our targets required for the whole of quarter 4 we have since fully met the 90% target for
February and March 2013. In addition we have secured resources to sustain this improvement throughout 2013/14.
What we measured
Performance 2012/13
Dementia screening
How we measured it
% of all patients aged 75 and over who have been screened following admission to hospital
In quarters 1, 2 and 3 although a percentage of patients were screened, assessed, and referred the data collection process was not robust and fully reliable. For
February and March the results are as follows:
Feb 2013 PRUH = 97%, March
PRUH = 99%
Feb 2013 QEH = 98%, March QEH
= 97%
Dementia risk assessment
Referral for specialist diagnosis
% of all patients aged 75 and over, who have been screened as at risk of dementia, who have had a dementia risk assessment within 72 hours of admission to hospital
Feb 2013 PRUH =100%,
March PRUH = 100%
Feb 2013 QEH =100%,
March QEH = 100%
% of all patients aged 75 and over, identified as at risk of having dementia who are referred for specialist diagnosis
Feb 2013 PRUH = 100%, March
PRUH = 100%
Feb 2013 QEH = 100%, March
QEH = 100%
SLHT Quality Accounts 2012-13 Page 19 of 95
3.1.3 Venous Thromboembolism (VTE)
VTE is a major cause of mortality, long-term disability and chronic ill health. During
2012-13 we extended our focus from simply assessing whether patients have had an appropriate risk assessment when they are admitted to hospital, to making sure patients are prescribed appropriate medication (prophylaxis) and are given information about VTE.
Our performance against the 4 measures we set is as follows:
What we measured
VTE Risk
Assessments
VTE Prophylaxis
VTE Information
How we measured it
% patients who have a
VTE risk assessment on admission
% of patients who are prescribed appropriate prophylaxis
% patients given information about VTE
Performance 2012/13
SLHT performance on risk assessments has been steady throughout the year, meeting or exceeding the 90% national target in each of the last 10 months.
Performance for the last 2 years is shown in Figure V1 below.
Audit shows 90% of patients have appropriate thromboprophylaxis
(target 90%)
Recent audit shows 65% of patients have information available at admission and 100% at discharge (target 60%)
VTE Prevention
Numbers of patients with a pulmonary embolism or deep vein thrombosis following surgery (Dr
Foster)
SLHT performance has been equal to, or better than, the national average throughout the year.
SLHT Quality Accounts 2012-13 Page 20 of 95
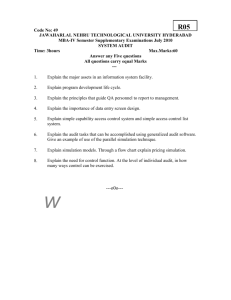
Figure V1: % of Patients Assessed for VTE 2011/12 &
100%
90%
80%
70%
60%
50%
40%
30%
20%
10%
0%
2011/12
2012/13
Target
Apr May June Jul Aug Sept Oct Nov Dec Jan Feb Mar
3.1.4 Fractured neck of femur
The clinical pathway for patients with a fractured neck of femur (hip) has been reviewed, to make sure we provide coordinated and effective care to patients who have had a hip fracture, from the point at which they are admitted to hospital to their return home. Our aim is to speed up the treatment times of this procedure so that as many patients as possible have surgery within 36 and 48 hours of admission.
What we measured
The proportion of patients admitted with a diagnosis of fractured neck of femur having surgery within 36 or 48 hours of admission
How we measured it
% patients having surgery within 36 hours
% patients having surgery within 48 hours
Table H1
Performance 2012/13
See table
See table
H1
H2 & H3
Hip Fracture surgery within 36 hours
England average 2011 *
PRUH
QEH
Q1
67%
58%
87%
Q2
67%
67%
75%
Q3
67%
85%
74%
Q4
67%
78%
80%
SLHT Quality Accounts 2012-13 Page 21 of 95
Table H2
Hip Fracture surgery within 48 hours (within normal working hours)
England average 2011 *
PRUH**
QEH**
Table H3
Q1
82%
86%
93%
Q2
82%
79%
81%
Q3
82%
93%
85%
Q4
82%
91%
89%
Hip Fracture surgery within 48 hours (not in normal working hours)
England average 2011 *
PRUH**
QEH**
Q1
0.9%
2.6%
1.1%
Q2
0.9%
0%
2%
Q3
0.9%
0%
0%
Q4
0.9%
0%
0%
* The England average is taken from the 2012 National Hip Fracture database (NHFD) annual report. SLHT data is locally derived from 2012/13 data downloaded from the
NHFD where we have tried to replicate the national methodology. National data for
2012/13 will not be available until the 2013 NHFD annual report is published.
** Note: It is not Trust policy to operate on fractured neck of femur patients after
10pm at night
The data for 2012/13 reflects the significant work that has been undertaken at SLHT to improve the pathway for patients who experience a fractured neck of femur. This will continue in 2013/14 with the Trust working towards compliance with the 11 standards from London Quality and Safety Programme: Fractured neck of femur pathway.
SLHT Quality Accounts 2012-13 Page 22 of 95
3.1.5 Clostridium difficile Infections (CDI)
CDI is bacteria that is present in the gut of up to 3% of healthy adults and 66% of infants. It is the most important cause of healthcare associated diarrhoea. However,
CDI rarely causes problems in children or healthy adults as it is kept in check by the normal bacterial population of the intestine. When certain antibiotics disturb the balance of bacteria in the gut, CDI can multiply rapidly and produce toxins which cause mild to severe diarrhoea. People who have been treated with antibiotics, people with serious underlying illnesses and the elderly are at greatest risk – over
80% of CDI infections reported are in people aged over 65 years.
Our performance against the measures we set is as follows:
What we measured
How we measured it Performance 2012/13
Number of reported cases of
CDI
Incidence of CDI
59 cases of CDI were reported, showing significant improvement from 2011-12, but exceeding the target of 56 cases in the year ( see Fig. CDI1 )
Antimicrobial prescribing
Hand hygiene
Cleanliness
Isolation
Compliance to the antimicrobial care bundle will demonstrate 95% compliance, and performance will be maintained above this level
Hand hygiene initiatives will be in place at the point of care and compliance will be monitored, to ensure a minimum 95% compliance by staff by end quarter 4 2012-
13.
Trust Management Audits of cleanliness will demonstrate compliance with the performance standards set out in Trust policy for the relevant risk areas.
All patients with potentially infectious diarrhoea will be isolated as soon as possible, and within 2 hours of onset
April 2013: Improvement noted up to 75% compliance in Jan
2013, but has slipped back down in March 2013 to 48%.
Further work in progress to drive improvement
April 2013: Hand hygiene compliance has remained high, but only achieved the 95% compliance standard in quarter
2 2012-13. Data is: Q1 = 90.18,
Q2 = 95.06, Q3 = 89.97, Q4 =
91.98
April 2013: Monitoring in place and demonstrates improving standards overall, with Trust monitoring demonstrating that in most areas the minimum cleanliness performance standards are consistently achieved.
April 2013: Datix monitoring demonstrates this is not a significant issue, though an
SLHT Quality Accounts 2012-13 Page 23 of 95
of diarrhoea to minimise the risk of infection to others.
Monitoring of the number of incidents of delayed isolation. episode of delayed isolation was a root cause of an increase in cases on one of the wards at
QEH in Jan/Feb 2013.
What Action Are We Taking?
The key issues which reduce avoidable
Clostridium difficile
infection are prudent antimicrobial prescribing, hand hygiene, isolation, and cleanliness. Actions in place in the Trust focus on these elements.
The Trust continues to implement a programme of hand hygiene awareness, using the „talking walls‟ approach which has been successful in many countries. A programme of monthly audit of staff compliance with hand hygiene, including „bare below the elbows‟ is in place in each area to check on practice and drive up standards.
The Trust has an isolation flowchart in place, which is used as a quick guide for staff to ensure anyone with potentially infectious diarrhoea is moved into a single room quickly.
Pharmacist ward rounds highlight any issues with antimicrobial prescribing, and consultant microbiologists and antimicrobial pharmacists meet with medical staff in a variety of departments to jointly review how prescribing can be improved. Monthly
SLHT Quality Accounts 2012-13 Page 24 of 95
antimicrobial prescribing care bundle audits are performed and results are fed-back to all consultants.
A programme of audits of key infection prevention practices is in place across the
Trust, and includes isolation practice. This monitors a range of issues important to protect patients and staff from infection. Results are fed back to clinical staff and used to take action at local level so that high standards are maintained.
Weekly formal audit of cleanliness standards is performed within the Trust, by a team which includes a Trust monitoring officer, cleaning contractor, patient representative, and members of the nursing and infection prevention teams. These audits are performed on a random sample of areas, with all areas being monitored over a period of time. It is enormously beneficial to have patient representation on these audits, as these volunteers provide a „patients-eye view‟ and an independent check of our process and standards. SLHT is enormously grateful for the support we have received from key members of Local Involvement Networks to support this programme in 2012-13.
As well as routine monitoring of standards, in response to a case of
Clostridium difficile
infection, a rapid audit of standards is performed on the ward to identify any areas that could be improved to reduce the risk of infection to patients. This includes audit of cleanliness and environmental standards as part of the weekly formal monitoring audits.
Each case is investigated via the national ‘learning through action’ root cause analysis tool, and the outcome is then scrutinised further for additional learning, with the Medical Director leading Executive Review Panels for cases in any areas of concern
SLHT Quality Accounts 2012-13 Page 25 of 95
3.2 Mortality
Hospital Standardised Mortality Ratio
The hospital standardised mortality ratio (HSMR) is an internationally recognised measure of quality of care. The ratio gives an indication of death rates for patients admitted to a hospital. Because the ratio is standardised, rates of HSMR can be compared across different hospitals. The HSMR is a measure of overall mortality
(deaths) but it should be used in conjunction with other measurements in the assessment of a hospital‟s overall quality of care. HSMRs compare the number of expected deaths with the number of actual deaths. If the HSMR for a hospital is higher than 100 there may be a need to investigate why.
In 2011/12 the HSMR for SLHT was 87.3, which means that the Trust had fewer deaths than expected for the patient group it had treated. For 2012/13 the HSMR data has only been finalised by Dr Foster to January 2013 – the Trust‟s HSMR is currently 95.2, again indicating fewer deaths than expected.
HSMR 2011/12 & 2012/13
140
120
100
80
60
40
20
0
2011/12
2012/13
Target <100
Apr May June Jul Aug Sept Oct Nov Dec Jan Feb Mar
SLHT Quality Accounts 2012-13 Page 26 of 95
3.3 Safety Thermometer
The Safety Thermometer is a tool used to capture the incidence of four 'harms' to patients admitted to hospital. Every patient is surveyed on one day every month and the number of the following „harms‟ is recorded: pressure ulcers; falls; urinary tract infections in patients with catheters; and new VTEs. The tool has been implemented since July 2012 by all NHS Trusts in England and now that the data collection is well established it can be used for benchmarking and to improve the number of patients having a harm free admission to hospital.
The 4 areas of harm covered by the safety thermometer are:
Falls Management
Pressure Ulcers
Catheter & UTI
New incidence of Venous Thromboembolism (VTE)
SLHT performance and benchmarking against other Trusts in England is set out below.
SLHT Quality Accounts 2012-13 Page 27 of 95
300
250
200
150
100
50
3.3.1 Falls management
The chart below compares the total number of falls that were reported in 2011/2012 and 2012/2013. There were a total of 2517 reported falls for the year 2012/2012 compared to 1699 falls in 2012/2013. This is a 32% reduction in the total number of reported falls incidents for the year.
Falls 2011/12 & 2012/13
2011/12
2012/13
2.00%
1.50%
1.00%
0.50%
0.00%
0
Apr May June Jul Aug Sept Oct Nov Dec Jan Feb Mar
The chart below compares the SLHT results from the national safety thermometer data for falls incidences (July 2012 to March 2013) with the National results. The results indicate that the incidence of falls at SLHT is above the national average. It should be noted however that the data from the safety thermometer related to falls may include patients who have fallen in a care setting, for example nursing home, residential home and which may include falls at home, if in receipt of district nursing, in the previous 72 hours to the survey being undertaken.
SLHT Falls v England Average
3.00%
England
SLHT
2.50%
Jul Aug Sep Oct Nov Dec Jan Feb Mar
SLHT Quality Accounts 2012-13 Page 28 of 95
The Falls Management Steering Group has supported the implementation of the following actions to reduce falls incidents:
Introduction of Falls Alarm Mats
In some areas of the Trust we have introduced falls mats which are used for Patients who have been assessed as at medium risk of falling. The initial focus has been to introduce the mats on wards where patients with dementia are cared for on both the
QE and the PRUH sites. In discussion with ward staff there is a view that these are proving to be of some assistance in preventing falls for some patients. As a result we hope to continue to implement the mats more widely across the Trust.
Use of low beds and bed rail policy
We have reviewed the guidance for staff to access and use „low beds‟ for patients who are at risk of falling out of bed. In addition to this we have updated our policy for staff when using bed rails to support patients who may be at risk of falling out of bed and are not at risk of climbing out over bed rails.
Introduction of volunteer role
We have developed a role outline for volunteers who are placed on to support patients who are at risk of falling - the focus on this is around providing some company for patients.
Introduction of a carer’s charter
This has been introduced in practice along with guidance for staff. The purpose of the charter is to provide some simple advice relating to how we can welcome support and engagement from carers when they wish to be involved in caring for family or friends. This is particularly helpful for those patients who may be at increased risk of falling as we can be more response and flexible with visiting hours.
Weekly review of falls incidents
On each of the sites we have a weekly meeting with matrons where the total numbers of incidents relating to falls and pressure ulcers are reviewed and validated.
These meetings have provided the opportunity for discussion about sharing ideas and strategies to support patient care in practice. This includes how groups of patients at risk of falling are nursed in the one bay.
3.3.2 Pressure ulcers
The chart below compares the total number of hospital acquired grade two pressure ulcers that were reported in 2011/2012 with 2012/2013. The data demonstrates good progress in a reduction of grade 2 pressure ulcers in the first two quarters of the year however this progress was not sustained. The total numbers of hospital acquired pressure ulcers including all grades have continued to reduce from 371 in
2011/2012 to 303 in 2012/2013 which is an 18% reduction.
SLHT Quality Accounts 2012-13 Page 29 of 95
3
2
1
0
6
Grade 2 Pressure Ulcers 2011/12 & 2012/13
40
35
30
25
20
15
10
5
2011/12
2012/13
0
Apr May June Jul Aug Sept Oct Nov Dec Jan Feb Mar
The chart below compares the numbers of hospital acquired grade 3 and grade 4 pressure ulcers that were reported in 2011/2012 and 2012/2013. The data indicates a comparable position with little overall change in the total numbers reported for both years.
Grade 3 & 4 Pressure Ulcers 2011/12 &
2012/13
2011/12
2012/13
5
4
Apr May June Jul Aug Sept Oct Nov Dec Jan Feb Mar
The chart below shows that the prevalence of pressure ulcers for all grades at SLHT compares favourably with the national average (figures from national safety thermometer data collection July 2012 to March 2013). This data includes patients who may have been developed pressure ulcers within 72 hours of admission and as such would not be deemed to be hospital acquired.
SLHT Pressure Ulcers v England Average
SLHT Quality Accounts 2012-13 Page 30 of 95
7.00%
6.00%
5.00%
4.00%
3.00%
2.00%
1.00%
0.00%
Jul Aug Sep Oct Nov Dec Jan Feb
England
SLHT
Mar
SLHT Quality Accounts 2012-13 Page 31 of 95
3.3.3 Catheter & Urinary Tract Infections (UTIs)
The chart below shows the prevalence of patients with Catheter associated UTIs
(Urinary Tract Infections) on the days of the survey. This may include patients who were on treatment for a UTI prior to admission (from the national safety thermometer data July 2012 to March 2013).
There has been an increase of approximately 1% in the percentage of patients diagnosed with a urinary tract infection. This is currently being investigated.
SLHT Urinary Tract Infections v England Average
5.00%
4.50%
4.00%
3.50%
3.00%
2.50%
2.00%
1.50%
1.00%
0.50%
0.00%
England
SLHT
Jul Aug Sep Oct Nov Dec Jan Feb Mar
3.3.4 New VTE
Preventing VTE was a Trust priority during 2012-13. Performance against our targets is described in section 3.1.3.
SLHT Quality Accounts 2012-13 Page 32 of 95
95%
90%
85%
80%
75%
70%
65%
60%
3.4 Stroke services
SLHT has consistently met the standard of at least 80% of patients spending 90% of their stay in the stroke unit. Performance in January 2013 fell below 80% due to capacity issues in the Hyper-Acute Stroke Unit (HASU). A plan has been put in place to improve the Emergency Department (ED) to HASU pathway and performance has been compliant since.
SLHT routinely monitors Stroke Unit performance against the Stroke Networks standards, Royal College of Physicians (RCP) guidance, NICE guidelines and
Accelerating Stroke Improvement (ASI) metrics. SLHT performance data is also uploaded to the Sentinel Stroke National Audit Programme (SSNAP).
Patients Spending at least 90% of admission on a Stroke Unit :
2011/12 & 2012/13
100%
2011/12
2012/13
Target
Apr May June Jul Aug Sept Oct Nov Dec Jan Feb Mar
SLHT Quality Accounts 2012-13 Page 33 of 95
4.5
4
3.5
3
2.5
2
1.5
1
0.5
0
3.5 Methicillin Resistant
Staphylococcus Aureus
(MRSA)
Staphylococcus aureus
is a common bacterium (germ) which lives harmlessly on the skin or in the nose of around 30% of people. These germs sometimes cause skin infections such as boils, abscesses and spots. Methicillin is an antibiotic. MRSA means that the germ has become resistant to treatment with this antibiotic, and usually several others as well. Consequently there are a limited number of antibiotics which can be used to treat MRSA infections.
The Trust has had great success in driving down the number of cases of MRSA bacteraemia in recent years, and this has continued in 2012-13.
The national target for 2012-2013 was no more than 2 cases of Trust-apportioned
MRSA bacteraemia. From April-December there were no cases reported, but in
January 2013 there were 2 cases. Investigation confirmed that these were not linked. One case was not causing patient infection, and the other was caused by a community strain of MRSA, with little the Trust could have done to prevent the infection. Learning from both cases is being implemented in practice.
There were no more cases in 2012-13, and the Trust ended the year on target, with
2 cases. The Trust target for 2013-14 has been set at 0 cases.
Chart MRSA1: MRSA YTD 2011/12 & 2012/13
2011/12
2012/13
Target
Apr May June Jul Aug Sept Oct Nov Dec Jan Feb Mar
The chart above shows that we had only 2 cases of MRSA bacteraemia during 2012-
13, which met the national target of <=2 cases. Both cases occurred in January
2013.
SLHT Quality Accounts 2012-13 Page 34 of 95
3.6 Patient safety incidents
The number of patient safety incidents reported during 2012-13 was 10% less than the total reported in 2011-12. The table below shows the number of reported patient safety incidents for year 2012-13, compared to the previous year.
Patient Safety Incidents
The trust places great importance in maintaining the level of reporting from previous years and has taken action to ensure incidents are reported by all staff groups. The profile of incident reporting is being emphasised at Care Group governance meetings and staff are reminded to report not only actual incidents that occur but also those that are near misses.
SLHT Quality Accounts 2012-13 Page 35 of 95
3.7 Participation in Clinical Audits
3.7.1 National Clinical Audits
During 2012-13, 36 national clinical audits covered NHS services that South London
Healthcare NHS Trust (SLHT) provides.
During that period the Trust participated in 33/36 (92%) of national clinical audits which it was eligible to participate in.
The 3 national clinical audits that the Trust was eligible to participate in and did not are detailed below. Data for some audits, such as the cardiac arrest audit is already collected locally.
Cardiac arrest
Heavy menstrual bleeding
Pulmonary Hypertension
The national clinical audits that the Trust participated in during 2012-13 are listed in the table below alongside the number of cases submitted to each audit as a percentage of the number of registered cases required by the terms of the audit.
Table CA1: National Clinical Audit the Trust Participated in during 2012/13 showing the number of cases submitted as a percentage of the number of cases required by terms of each audit
National Clinical Audit
National Parkinson‟s Audit
Cardiac Rhythm management (Pacing/Implantable Defibrillators)
Adult Cardiac Interventions (e.g. Angioplasty)
Heart Failure
Myocardial Ischaemia (MINAP)
Intensive Care Audit / Case Mix Programme (ICNARC)
TARN / Trauma Audit & Research Network
Fever in Children
Renal Colic
Adult Community Acquired Pneumonia
Non invasive Ventilation (NIV) – Adults
Lung Cancer (LUCADA)
SINAP Stroke Improvement National Audit
Chronic Pain (National Pain Audit)
National Bowel Cancer Audit Programme
Oesophago-gastric Cancer
Hip, Knee and Ankle Replacements (National Joint Registry)
% Cases
Submitted
100%
100%
95%
100%
100%
100%
100%
100%
100%
100%
95%
100%
100%
100%
55%
100%
65%
SLHT Quality Accounts 2012-13 Page 36 of 95
National Clinical Audit
National Hip Fracture Database
Elective Surgery (National PROMS Programme)
Blood Sampling and Labelling
Paediatric Asthma
Paediatric Pneumonia
Epilepsy12 (Childhood Epilepsy)
Paediatric Diabetes
Neonatal Intensive and Special Care (NNAP)
National Audit In Patient Diabetes Audit (NADIA)
National Dementia Audit
Fractured Neck of Femur
Consultant Sign-off 2013
Potential Donor Audit (NHS Blood & Transplant)
Chronic Obstructive Pulmonary Disease (COPD)
Acute Kidney Injury (AKI)
The reports of 14 national clinical audits were reviewed by the Trust in 2012/13.
These are listed below outlining the actions that the Trust intends to or has taken to improve the quality of healthcare provided.
% Cases
Submitted
100%
100%
100%
80%
100%
100%
100%
100%
100%
75%
96%
100%
100%
100%
81%
3.7.1.1 Fever in Children Audit
Audit Objective
This audit was undertaken to identify and compare the treatment of feverish children
(under 5 years of age) presenting in QE Hospital, Emergency Department against
College of Emergency Medicine Clinical Standards and against National Institute for
Health and Care Excellence (NICE) Guidance.
Improvements in Care
The upward trend in achieving the recommended standards of care was noted in the report as commendable, and clearly demonstrates that the department is working hard to improve quality. Measurement of pulse rate, temperature, oxygen saturations, GCS score and compliance with the NICE guidance on investigations and treatment in 100% of febrile children is particularly good and staff have been commended on their performance.
Improvement actions were identified in the documentation of respiratory rate and capillary refill time, as part of the child‟s initial assessment; these areas have been addressed through a series of educational meetings with doctors & nurses in order to improve the level of care provided.
SLHT Quality Accounts 2012-13 Page 37 of 95
3.7.1.2 Renal Colic Audit
Audit Objective
The aim of this audit was to look at the care of adult patients with renal colic on admission to the QE Emergency Department (ED) against College of Emergency
Medicine Clinical Standards. The audit focused on the assessment, treatment of renal colic, the documentation of pain severity and the prompt delivery of pain relief.
Improvements in Care
The results demonstrated that the recording of pain severity and the length of time spent in the ED was recorded in 98% of cases, this being a significant improvement compared to previous audit results. However, provision of quicker pain relief, the reassessment of pain levels, and the documentation of tests results in patient‟s notes were identified as areas where improvements are required.
Awareness has been raised on the results of this audit and care standards expected for this group of patients through educational meetings with both medical and nursing staff. This will help ensure that these patients receive prompt pain relief on admission and improve documentation in line with recognised best practice.
A flow chart for the management of renal colic in the ED is being developed to standardise the management for these patients and streamline their care in the ED.
3.7.1.3 Fractured Neck of Femur Audit
Audit Objective
This audit was undertaken to review the standards of treatment for patients presenting to Emergency Departments (EDs) with a fractured neck of femur against the clinical standards set by the College of Emergency Medicine.
98% of patients in severe pain (pain score 7 to 10) should receive appropriate analgesia within 60 minutes of arrival or triage whichever is the earliest
75% of patients should have an X-ray within 60 minutes of arrival or triage whichever is the earliest
98% of patients should be admitted within 4 hours of arrival
Improvements in Care
A review of the report showed that 83% of patients with severe pain received pain relief within one hour. A teaching programme has been implemented for medical and nursing staff to ensure they understand the importance of prompt pain relief along with the introduction of an „Integrated Care Pathway‟ to manage and record pain relief and treatment throughout the patient‟s journey from triage to admission.
SLHT Quality Accounts 2012-13 Page 38 of 95
Patients‟ receiving an x-ray within 60 minutes was recorded as 27% against a college standard of 75%. This prompted immediate action and the following has been implemented to address this; discussions between radiology and the EDs to ensure patients requiring a hip x-ray are prioritised with the intention that they are x-rayed within 30 minutes of arrival or triage whichever is the earliest.
Time in the department awaiting admission to ward areas was reported to be less than 4 hours for only 63% of patients against a college standard of 98%. The Trust is continually monitoring admission rates, and reviewing bed planning to improve timely admissions.
3.7.1.4 Chronic Obstructive Pulmonary Disease Discharge Audit
Audit Objective
The purpose of this audit was to ensure all patients admitted with exacerbation of
Chronic Obstructive Pulmonary Disease (COPD) are assessed before discharge by the
Respiratory Nurses.
Improvements in Care
The audit demonstrated that there were key areas for improvement around assessment prior to discharge; inhaler technique, and the referral system. The following changes have been implemented:
A discharge pathway for exacerbation of COPD has been produced which includes an assessment of the patient by a Respiratory Nurse prior to discharge.
This assessment will ensure the following areas of patient care have been implemented:
That the patient is using their inhaler correctly and so gaining maximum benefit from the medication
If required, an oxygen alert card is given to the patient which informs others about the strength of oxygen that can be given
That all referrals for outpatient follow up appointments have been made, specifically to the community team, pulmonary rehabilitation team and smoking cessation team
Future plans will include involving general practitioners supplying emergency medicines to known COPD patients if required.
3.7.1.5 National Diabetes Inpatient Audit
Audit Objective
The National Diabetes Inpatient Audit was a one day audit that reviewed the care diabetic patients received when admitted to hospital.
SLHT Quality Accounts 2012-13 Page 39 of 95
Improvements in Care
The findings of the report that were relevant to the Trust were around the provision of a diabetic foot care team and foot assessments on admission. These findings linked with the 2012/13 Trusts Commissioning for Quality and Innovation targets and a local Trust audit (see Local Audits: Diabetic Foot Problems)
The following improvements have been made by the Trust:
The diabetic foot care team has been reviewed to ensure that it includes a diabetologist; diabetic nurse specialist; podiatrist and a surgeon so that all diabetic patients are seen by the correct specialists
A standardised foot assessment tool has been added to the emergency medical admissions documentation, which requires all diabetic patients admitted into hospital to have a documented feet assessment regardless of their medical condition
A referral process is in place for patients with foot problems so that immediate and appropriated treatment can be given
3.7.1.6 Sentinel Stroke National Audit
Audit Objective
The results of the 2012 Sentinel Stroke National Audit demonstrated significant improvement in all aspects of service provision. Eight domains of the stroke service organisation were audited:
Acute care
Organisation of care
Specialist roles
Interdisciplinary services
Neurovascular/TIA clinics
Quality improvement, training and Research
Team meetings
Communication with patients and careers
Improvements in Care
The overall SLHT performance across all the above domains placed the PRU in the top 25% of Trusts nationally. For the following areas, performance was under 90% and actions implemented:
Organisation of Care : There were no Stroke/Neurology Early Supported Discharge
Services available to SLHT at the time of this audit. This changed in October 2012, when an Early Supported Discharge Team (ESDT) was put in place for Bromley
SLHT Quality Accounts 2012-13 Page 40 of 95
patients. This Team has been very successful and has facilitated early discharge for a number of patients. An ESDT pilot was also put in place in February 2013 for
Greenwich patients.
Specialist Roles: There is still limited access to Clinical Psychology services. SLHT has developed a robust internal screening pathway for the identification of reduced mood of stroke patients. Additionally there are no services to support stroke patients to return or remain at work, and to provide educational or vocation training. These results will be highlighted in the next Stroke Strategy meeting which includes representation from Local Commissioners.
Interdisciplinary Services: Six day working is in place for Physiotherapy and to a lesser extent Speech and Language Therapy. All services continually monitor their staffing levels to ensure on–going compliance with the required standards.
Communication with Patients and Carers: Consultant Stroke Physicians will review ways to allow stroke out-patients access to their management plan.
3.7.1.7 Adult Cardiac Interventions Audit: angioplasty
Audit Objective
This audit looked at the number of people who had had a cardiac infarction (heart attack), the treatment pathways for these patients and the quality of care given. By participating SLHT is able to ensure that standards of treatment and care are in line with the national standards and best practice.
Improvements in Care
A new cardiac pre-assessment clinic has been started. This will mean that the waiting list, booking and organisation of angioplasty procedures are undertaken by the Cardiac Team, giving patients a single point of contact which will improve patient experience.
3.7.1.8 Cardiac Rhythm Management Audit
Audit Objective
A database of implantable pacemakers has been in existence since the late 1970s.
Implantable Cardiac Defibrillators (ICD), a treatment to prevent sudden cardiac death were added to the database in 1988. Implantable devices to assist in the management of heart failure were added to the audit in 1998.
The aim of the audit is to look at activity, trends and outcomes in pacing and ICDs, and to improve the care of patients who undergo these procedures.
Improvements in Care
A care pathway has been developed to identify and assess patients who require pacemakers and ICDs. This means that patients at high risk of a life threatening cardiac arrhythmia will be promptly identified. It is anticipated that this will increase
SLHT Quality Accounts 2012-13 Page 41 of 95
the number of patients who receive these implants. The out of hours service will also be reviewed and a protocol developed so that patients continue to receive prompt treatment and if required referral to tertiary centres.
3.7.1.9 Paediatric Asthma Audit
Audit Objective
This audit uses the British Thoracic Society Guideline recommendations for the
Management of Asthma to benchmark clinical performance in five key areas; basic demographic information, initial hospital assessment, initial hospital tr eatment, discharge planning, and follow ‐ up against aggregated national data.
Every child with wheezing or asthma, over one year of age, admitted into participating hospitals for more than 4 hours was included in this national audit.
Improvements in Care
For most children, initial treatment is clearly highly effective with short lengths of stay of a day or less. The following areas were identified as needing improvement:
Discharge planning: 41% of children/parents were recorded as having received a written discharge plan
Device technique assessed: 44% of children were recorded as having their device use checked
Planned actions:
The introduction of a discharge checklist to include an asthma device technique assessment for children who can self administer
The development of an Asthma Parent Proficiency Template, (a written record of training provided and of parental practice being checked), to include core proficiency in asthma device technique for all children who are unable to self administer
3.7.1.10 National Hip Fracture Database
Audit Objective
The National Hip Fracture Database is a joint venture of the British Geriatrics Society and the British Orthopaedic Association, and is designed to facilitate improvements in the quality and cost effectiveness of hip fracture care. It allows care to be audited against evidence-based standards and enables local health economies to benchmark their performance in hip fracture care against national data.
Improvements in Care
Each patient who attends SLHT with a hip fracture is measured against the evidencebased standards. The Trust has improved the time patients wait to have their surgery so that the majority of patients receive their operation within 36 hours of
SLHT Quality Accounts 2012-13 Page 42 of 95
admission. The Trust has achieved this by providing a dedicated Trauma Theatre six days a week and ensuring that patients with fractured hips take priority, with surgery being performed by a senior Orthopaedic surgeon. This has had a positive impact on patient recovery time resulting in a reduced length of stay.
As part of the hip fracture care pathway patients now receive care from both an
Orthopaedic Team as well as a Geriatrician. This dual care provides the patient with preventative care as well as the immediate surgical intervention required to fix their fracture.
The Trust is now taking steps to admit patients with hip fractures to dedicated
Orthopaedic ward. This has proved challenging with increased admissions during the winter period, but if a bed on an Orthopaedic ward cannot be provided immediately a transfer will be arranged as soon as is possible.
3.7.1.11 National Neonatal Audit
Audit Objective
The purpose of this National Neonatal Audit is to assess whether babies admitted to neonatal units in England receive consistent care and to identify areas for improvement in relation to delivery, and outcomes of that care.
Improvements in Care
Following participation in this Neonatal Audit the following areas were identified for improvement in relation to delivery and outcomes of care:
100% of premature babies born under 32 weeks gestation must be screened for
Retinopathy (a disease of the eye) within the designated timescale for their gestational age
Within 24 hours of admission 100% of parents/carers should have a documented consultation with a senior member of the neonatal team
SLHT has submitted detailed action plans to the Royal College of Paediatricians in order to achieve these directed national standards. This includes the introduction of extensive staff training as part of staff induction along with email communications and presentation of the latest annual report.
3.7.1.12 National Oesophago-Gastric Cancer Audit
Audit Objective
SLHT is part of the National Cancer Network. Following recommendations from the
Network, patients attending SLHT with Oesophageal dysplasia are referred to the appropriate Cancer Centre (in this case St Thomas' London).
Improvements in Care
SLHT Quality Accounts 2012-13 Page 43 of 95
The National policy is that patient care is improved by centralisation and hence concentration of expertise at specific sites.
3.7.1.13 National Heart Failure Audit
Audit Objective
Heart Failure is a complex clinical syndrome whereby the hearts ability to pump blood around the body is reduced. It is associated with a high annual mortality, especially if poorly treated. The effects of Heart Failure on quality of life cannot be underestimated. Optimal management results in better prognosis with fewer symptoms and an increased life expectancy. The aims of the audit were:
To assess whether patients were cared for in a Cardiology ward with specialist consultants and nurses
To assess the number of patients prescribed appropriate cardiac medications on discharge
Improvements in Care
The audit showed that 61% of patients were cared for in the appropriate clinical setting and on average 92% of patients were discharged from hospital with the appropriate cardiac medications. In response to these results the following improvements have been made:
Multi-professional training has been implemented ensuring that all healthcare professionals are competent in the identifying and treating of patients with Heart
Failure
Stickers have been produced and placed within patients‟ notes listing appropriated medications in order to assist doctors with prescribing
Through improved joint working with the local community Heart Failure services and the implementation of monthly meetings, there has been an increased number of patients being referred out to community heart failure services.
The next stage of the improvement plan will be to produce an integrated care pathway, which will ensure best clinical practice across all wards areas as recommended by the NICE guidelines for heart failure.
3.7.1.14 Myocardial Ischaemia National Audit
Audit Objective
This is a comparative national audit of the management of heart attack patients against agreed national standards (i.e. NICE guidance).
Improvements in Care
SLHT Quality Accounts 2012-13 Page 44 of 95
The audit showed that nationally there has been a year on year fall in the percentage of heart attack patients who die within 30 days of admission to hospital.
The audit demonstrated the need for specific care pathways. In response to this the
Trust has introduced two treatment pathways to identify:
Patients requiring immediate emergency treatment, i.e. angioplasty, and
Patients requiring treatment within 96 hours
This has allowed patients to be treated in the most appropriate clinical environment and receive expert cardiac care and advice.
3.7.2 Local Clinical Audits
The reports of 33 local clinical audits were reviewed by the Trust in 2012/13 and the
Trust has or intends to take the following actions to improve the quality of healthcare provided.
3.7.2.1 Critical Care Outreach Team
Cardiac Arrest Audit
The audit was undertaken to ensure there is continuous monitoring of medical emergency and cardiac arrest activity within the Trust estate, and to ensure our response is optimal in terms of compliance with Resuscitation Council UK guidelines.
As a result of the audit the reporting strategy for cardiac arrest activity has moved from paper to electronic with the 24/7 Critical Care Outreach Team responsible for its completion. This will ensure that audit return will be maximised and therefore more reflective of clinical activity than the previous system.
The aim of the audit was to determine compliance with RCUK guidance, which can be difficult to ascertain in real-time, to clinical indicators of response performance.
Going forward the aim will be to measure resuscitation interventions based on „time lapsed „so for example, we aim to have the first shock or the first cardiac arrest drug within 2 minutes of collapse. This has already influenced the training strategy where the Trust has provided funding for more clinicians to attend Immediate and
Advanced Life Support courses. The Resuscitation Service has enhanced the availability of special equipment to allow clinicians to provide resuscitation drugs quicker and is now looking to provide clinical areas with automated CPR machines.
Do Not Attempt Resuscitation Audit
The purpose of this audit was to determine if „Do Not Attempt Resuscitation‟ (DNAR) forms were completed as per Trust policy.
The audit showed that not all fields on DNAR forms are routinely completed, in particular documenting discussions between health professionals, and health professionals and the patients‟ relatives and friends. This prompted the need for a new DNAR strategy which is near completion, and is based on the work of the
SLHT Quality Accounts 2012-13 Page 45 of 95
National Confidential Enquiry into Patient Outcome and Death (NCEPOD) report 2012 and other NHS Trusts.
The Critical Care Outreach and Resuscitation Service have produced a „Treatment
Escalation Pathway (TEP)‟ form and guideline. This project will entwine with the current DNAR form and offer senior doctors a formal template that reduces the complexity of higher escalation of care (e.g. Intensive Care Unit) for patients deemed not fit for resuscitation. Introduction of this project will raise awareness of the escalation process which is in addition to that on standard resuscitation training, and will include workshops to raise awareness of the need to improve and record communications between health professionals and the patient‟s relatives and friends.
Patient at Risk Score Audit
The Patient at Risk (PAR) system is used across SLHT for the early recognition and escalation of the deteriorating patient through appropriate monitoring and adequate clinical response. This audit was undertaken to determine if the monitoring and recording of clinical observations and PAR score is embedded into everyday practice.
Audit results confirmed that there is high compliance with monitoring and recording clinical observations and PAR scores across SLHT. However the Trust is continually striving to improve care to patients and as such was one of the first Trust in the
South East of England to adopt the Royal College of Physicians „National Early
Warning System (NEWS)‟ and in doing so replaced the Patient at Risk (PAR) system.
Both systems are completed for each set of vital signs, with each sign attributed a score. The NEWS/PAR score is an aggregated figure that activates a specific clinical response; the higher the score, the quicker and more skilled the response. Evolution towards the NEWS was based on the successful introduction of standardised PAR scoring across the Trust (91% of patients are scored). However for the first time it took into account current training resources and clinical availability of both human
(doctors and nurses) and institutional (Critical Care Outreach/Intensive Care Unit) assets. The system is designed to be quick, diligent and easier to complete which is a crucial tool in identifying and escalating deteriorating patients so they receive rapid and appropriate treatment.
Resuscitation Equipment on Resusciataires Audit
The audit was undertaken to determine if there is consistent availability of resuscitation equipment to the adult and paediatric emergency response teams.
The actions resulting from this audit include; a revised resuscitation trolley checklist which will be introduced alongside a laminated booklet detailing illustrations of the equipment. The checklist will be rationalised to ensure that items/equipment that are rarely used are removed, and prevent overstocking, making it easier and quicker for ward level teams to check. Target training of registered and non-registered nursing
SLHT Quality Accounts 2012-13 Page 46 of 95
staff by the Critical Care Outreach and Resuscitation Services on life support sessions will provide further support and reinforcement of this strategy.
3.7.2.2 Family Health Care Group and Safeguarding Children
Accuracy and Completeness of Post Natal Discharges Audit
Accuracy of information sharing post discharge from the maternity unit within the hospital is an essential requirement of safeguarding children practice to ensure safe outcomes for new born babies. Following the merger of the three Trusts there was an increased need for the majority of discharges to be faxed to other sites and it became apparent that the quality of discharges varied.
This audit looked at the following areas retrospectively; completion of discharge forms; availability and correct use of SLHT front/header sheet, process for „in and out‟ of area referrals, and process for sending faxes at discharge.
The audit revealed high compliance with correctly completing the discharge forms, i.e. 93%, with a SLHT front/header sheet being available in 81% of cases. The font/header sheet is used to act as a prompt for all shared information. Work is being continued to embed the use of the SLHT front/header sheet into everyday practice which results in timely and appropriate sharing of information.
To avoid any breach in confidentiality faxes should be sent in line with SLHT policy i.e. phone to advise a fax is being sent and request acknowledgement that the fax has been received. The audit revealed that 98% of information sent by fax was to the correct site.
Child Protection Plan and the Under 18 Checklist
This audit was carried out to determine if the Child Protection Plan list and Checklist for risks is checked for all children who attend the Children and Young Peoples
Assessment Unit at QM.
The results of the audit showed that the Child Protection Plan list was checked in
85% of cases and the findings of the check was recorded in the medical record. The checks, which are recorded in the medical record, ensure that children subject to
Child Protection Plans are notified to Children‟s Social Care in order to ensure their safety. These results show that, while the checking is being done for the vast majority of patients, the target of 100% compliance is still not being met.
All staff dealing with children attend safeguarding children education on induction to
SLHT, and attend annual updates which reinforce the need to carry out these checks to ensure child safety.
Fetal Blood Sampling Audit
The audit was undertaken to assess the indication for Fetal Blood Sampling (FBS) and to determine if the results are correctly interpreted and clearly documented.
SLHT Quality Accounts 2012-13 Page 47 of 95
Results showed that the indication for FBS was correct in all cases (n=20/20), and results were interpreted accurately and a plan for Cardiotocography review was clearly written.
Areas of practice that need improvement include documentation of maternal position during FBS, and a clear plan of when FBS should be repeated by the obstetrician.
Results are under review and an action plan is being developed.
Midwifery Contact with Allocated General Practitioner Audit
Good practice dictates that Community Midwives should make regular contact with
General Practitioners (GPs). This audit looked to determine how often midwives made contact with GPs in order to discuss cases, and whether the contact was face to face, by telephone or in writing.
Fifty-five percent (55%) of midwives who completed a questionnaire felt they made regular contact with their GPs which in the main was „contact in writing‟. Findings highlighted that there is a significant variation across the Trust i.e. a quarter of midwives surveyed at PRU make regular contact with their GPs in contrast to over
90% of midwives surveyed at QM who make regular contact.
To improve communication between midwives and GP‟s it has been recommended that Community Midwife Managers specify the minimum frequency of GP contact from midwives, and reaffirm the importance and relevance of face to face contact and discussion.
Perineal Trauma Audit
Perineal Trauma Management guidelines were measured against when auditing practice for the suturing of women who has sustained perineal trauma following childbirth.
An assessment of the perineum had been documented in 90% of case notes, whilst only 65% had details of a rectal examination documented. To address this issue the importance of performing and documenting the rectal examination was included in the annual mandatory training for midwives and doctors.
All women who sustained a 3 rd or 4 th degree perineal tear were sutured by an appropriately trained doctor in theatre as per guideline recommendations.
Additionally 94% of all women who required suturing were sutured within the recommended time scale of one hour following delivery which indicates a high standard of practice and care.
By ensuring that an assessment and repair of the perineum is completed within designated timescales by an appropriately trained health care professional, aids the healing process and reduces the risk of infection.
Swab Counting in Theatre Audit: Maternity Unit PRU
SLHT Quality Accounts 2012-13 Page 48 of 95
It is essential that the maternity services follow procedures which ensure swabs are never left inside a woman after perineal suturing. The purpose of this re-audit was to determine if the „swab count section‟ on the perineal suturing proforma in the case notes is routinely completed indicating that swab counts were undertaken.
Snap shot audits were carried out over three consecutive months during 2013/14
(April to June). Initial results in April showed 70% compliance with documenting the pre and post swab count. The importance of documenting the swab count was reiterated at each staff handover at the beginning of each shift. Additionally individual feedback was given to non-compliant practitioners. During the subsequent two months compliance improved to 82% and 90% respectively.
Newborn Feeding Audit
The purpose of this audit was to assess whether newborn feeding support was given to mothers following childbirth, and whether this support was given within the designated timescales as set out by SLHT clinical guidelines and United Nations
Children's Funds steps to „Baby Friendly Initiative‟.
The audit found that 92% of women included in the audit had skin to skin contact with their babies following delivery. Ninety Seven percent (97%) had been offered newborn feeding support within 6 hours of the birth of their babies.
The audit revealed that documentation of the first feed following delivery was not routinely recorded. The importance of documenting the first feed has now been included at mandatory breast feeding training sessions.
SLHT Quality Accounts 2012-13 Page 49 of 95
3.7.2.3 Medicine
Percutaneous Endoscopic Gastrostomy Insertion Aftercare Audit
A Percutaneous Endoscopic Gastrostomy (PEG) tube is a feeding tube that is inserted directly into the stomach by means of an endoscopy. It is used in patients who cannot swallow normally, for example after a stroke. In 2010 the National Patient
Safety Agency issued an alert because a number of patients had had complications shortly after insertion of a PEG and there had been delay in recognising and acting on these complications. In order to improve the aftercare SLHT introduced warning labels for insertion in the patient notes to notify nurses, patients and their carers of signs that might indicate an early PEG complication. In addition an aftercare checklist was introduced on which the vital signs, such as temperature, pulse and blood pressure could be documented after PEG insertion.
Notes for nine patients who had PEG insertion, after the changes were introduced, were audited. The warning labels were put in the notes of six of the nine cases, and the aftercare checklist was included in the notes of five patients. Unfortunately, the aftercare checklist was used for only one patient. There were no deaths associated with PEG insertion.
The results were presented at a departmental clinical governance meeting. The proposed action is to make the Endoscopy Unit responsible for inserting labels in the notes before the patient returns to the ward after the PEG has been inserted. The
Endoscopy Unit nurses will initiate observations after the procedure using the aftercare checklist and will hand this on to the ward staff to continue the observations. A re-audit will be carried out to ensure changes have been implemented and embedded into practice.
Rapid Access Chest Pain Clinic Audit
This is the first full financial year audit for the Rapid Access Chest Pain Clinic
(RACPC) at the PRU site of SLHT. The RACPC has been nurse-led with Consultant
Cardiologist support since October 2010.
The aim of the RACPC is the early diagnosis and treatment of patients with new onset chest pain, in accordance with the National Service Framework (NSF) for
Coronary Heart Disease (CHD) (2000), and the National Institute for Health and
Clinical Excellence (NICE): Chest Pain of Recent onset guidance (2010).
The clinic is held on average four days per week, with four patients per session who have been referred by their General Practitioner (GP). All patients‟ case studies are discussed with a Consultant Cardiologist on the day of clinic and a management plan agreed.
This audit aimed to measure:
Waiting times from GP referral to Rapid Access Chest Pain Clinic assessment against the NSF for CHD (2000) target of 2 weeks
SLHT Quality Accounts 2012-13 Page 50 of 95
Whether patients presenting with stable angina received clinical care in line with the
NICE Chest Pain of Recent onset guidance (CG95)
Whether appropriate referrals for diagnostic investigations were made in line with
NICE Quality Standard (21): Stable Angina
The audit demonstrated that all the above standards were met, but showed that there needs to be improvement in the feedback of investigations results to the
RACPC clinic, in particular getting a copy of the angiogram reports. To ensure that these results are received, the dictated reports are to be copied to the Rapid Access
Chest Pain nurse, and then entered onto the database. This will benefit patients as a clear diagnosis based on anatomical tests will be readily available. It will benefit the service delivered to patients as the clinical practice can be reviewed, potentially resulting in better quality care and a reduction in costs.
Reducing the Harm Caused by Misplaced Nasogastric Tubes Audit
The purpose of the audit was to assess current practice and adherence from nursing staff and doctors to the National Patient Safety Agency Alert recommendations on reducing the harm caused by misplaced Nasogastric Tubes (NGT) in adults at SLHT.
The audit demonstrated that
39% of healthcare staff were using the recommended documentation for the insertion/reinsertion of nasogastric tubes in adults
78% of healthcare staff were using PH testing as the first line method for confirming the position of the nasogastric tube although
Healthcare staff were monitoring NGT position at least once a day 78% of the time
This has led to the following recommendations/actions:
Results of the audit will be communicated to consultants, senior nurses and the dietetic team highlighting current practice and the need for improved adherence to the guidance.
Discussions are underway with nursing managers regarding the development of a training programme for new and existing staff to ensure that health professionals understand how to use the documentation and the care that is required to ensure the correct position of the nasogastric tube
Continue to provide training to new junior doctors within their training programme to make them aware of the NPSA policy, how to use the documentation and when the nasogastric tube position needs to be confirmed and/or monitored
Continue to ensure that junior doctors undertake the online learning module „x-ray interpretation‟
SLHT Quality Accounts 2012-13 Page 51 of 95
SLHT Quality Accounts 2012-13 Page 52 of 95
Central Venous Catheter Line Infection in Parenterally Fed Patients at QE
Audit
Central Venous Catheter (CVC) line infections can be problematic in patients who are fed Parenteral Nutrition (PN), as the high glucose content renders the fluid an ideal breeding ground for microorganisms.
Approximately 3 in every 1000 patients admitted to hospital in the UK acquires a bloodstream infection, and nearly one third of these infections are related to Central
Venous Access Devices (National Evidence-Based Guidelines for Preventing
Healthcare-Associated Infections in NHS Hospitals in England (EPIC 2 guidelines)).
The aim of the audit was measure the rate of infection in CVC lines for PN fed patients at QE, and establish whether the clinical practice of line changes in these patients followed the EPIC 2 guidelines.
The audit identified that out of 52 episodes of line insertions 8% developed an infection which is relatively low for this group of patients. However the removal/changes of lines were often performed unnecessarily and not in line with
EPIC 2 guidelines which recommend not routinely replacing central venous catheters as a method to prevent catheter-related infection.
As a result of the audit the following actions have been, or are in the process of, being implemented:
An immediate cease in the practice of removing/changing CVC line without a valid reason which must be documented in the care record
An education and training programme to be organised for staff nurses on wards regularly dealing with PN patients. This will cover the use and care of CVC lines and
PN bags
Updating PN guidelines to include greater emphasis on infection control and advice on the frequency of line changes
A further audit will be performed once these actions have been fully implemented to determine their effectiveness in reducing the infection rate to a target of 0%
Limitation of Medical Treatment for Adults Requiring Intensive Care Audit
The aim of this audit was to assess the Limitation of Medical Treatment Care within the QE Intensive Care against the guidelines of the Intensive Care Setting (2003) looking at:
Whether the decision is made on clinical grounds
Who makes the decision
Whether patient‟s wishes are considered
Care of the family throughout the process with regards to privacy
SLHT Quality Accounts 2012-13 Page 53 of 95
Audit results demonstrate that all decisions in relation to withdrawal of treatment were made by consultants on medical grounds, taking into account wherever possible the patient‟s wishes. Almost all family members were offered access to privacy during this process.
Training of communication skills and breaking bad news for all intensive care unit clinicians has been implemented. Intensive care unit clinicians are being encouraged to involve junior doctors in this process. Access to privacy for patients and their families is being reviewed.
Management of Gallstone Pancreatitis at PRU Audit
The purpose of this audit was to improve the outcomes for patients who have pancreatitis secondary to gallstones.
Pancreatitis is a common cause for patients to come into hospital with abdominal pain. This is a serious condition and has the potential to make patients very unwell, occasionally warranting admission to the intensive care unit. The most common causes for inflammation of the pancreas in the UK are alcohol intake and stones in the gall bladder. We specifically wanted to make sure that patients with pancreatitis secondary to gallstones are getting the best management.
We looked at the patient records of 103 patients who have been admitted to the PRU with gallstone pancreatitis and compared their management with the National guidelines. The guidelines state that patients with gallstone pancreatitis should have their gall bladders removed within two weeks of their discharge from hospital; our audit showed this is only being achieved in 11% of patients. The guidelines also state that all patients with gallstone pancreatitis should be managed by the same surgical team; our audit showed that patients were being looked after by six different surgical consultants.
Patients who are admitted to hospital with gallstone pancreatitis will now be urgently listed on the next available operating list to have their gall bladders removed. This means that operations will be carried out sooner to try and avoid further episodes of pancreatitis secondary to gallstones. This is based on national „best practice‟ guidance.
Staff will be advised that all patients who are admitted with gall stone pancreatitis should be looked after by the same surgical consultant while they are in hospital.
This will mean that patients are looked after by doctors who have the most experience in managing this condition and will enable better continuity of care. This change is based upon national guidance.
Diabetic Foot Problems: Inpatients and Outpatients Audit
Two audits were undertaken in response to the following National Institute for
Health and Care Excellence (NICE) guidance recommendations:
SLHT Quality Accounts 2012-13 Page 54 of 95
Diabetic patients admitted to hospital with foot problems should be referred to the multidisciplinary foot care team within 24 hours of the initial examination of the patient‟s feet (NICE Clinical Guideline 119), and
As part of the annual review of diabetic patients, trained personnel should examine patients‟ feet to detect risk factors for ulceration (NICE Clinical Guideline 10).
Diabetic Inpatient audit
The aim of this audit was to see if diabetic patients admitted to hospital had their feet assessed within 24 hours of being admitted, and if they had a foot problem, whether they were referred to the appropriate specialist team within 24 hours of their foot assessment.
Results for this audit demonstrated that although foot assessments are not routinely performed, all diabetic patients (100%) admitted with foot problems were referred to a specialist team for further treatment. This resulted in the following improvement being implemented:
A standardised foot assessment tool has been added to the emergency medical admissions documentation, which requires all diabetic patients admitted into hospital to have a documented feet assessment regardless of their medical condition.
An education session on diabetes has been added to the doctors „medical induction programme‟ to ensure that all doctors know how to use the foot assessment tool and record the information.
The referral process for patients with foot problems has been modified so that it is the same across QE and PRU sites.
Diabetic Outpatient Audit
This aim of the outpatient audit was to determine the number of foot assessments completed within the last 12 months n the diabetic outpatient clinics on QE and QM sites.
Results for this audit showed that 95% of diabetic patients attending diabetic outpatients had their feet assessed within the last 15 months. This timeframe took into account rearranged appointments outside of the Trust‟s control, i.e. patient unable to attend appointment.
It was agreed that no changes should be made at present and that a re-audit should take place after one year to ensure that the high compliance rate is maintained.
Management of Patients with High Potassium Levels Audit
High potassium levels are extremely dangerous and a potential medical emergency, it is therefore necessary to audit local practice.
SLHT Quality Accounts 2012-13 Page 55 of 95
This audit compared local practice to national guidelines (The Renal Association, July
2012) on the management of patients with high potassium levels, to see if local practice met the standards set by these guidelines.
The national guidelines target is 100% for all standards set. This audit highlighted that SLHT are not meeting these targets in any standards.
12 lead ECG for patients with a potassium equal or above 6.0mmol/L (66%)
Repeat ECG post treatment (20%)
Evidence of continuous ECG monitoring (63%)
Treatment with insulin-glucose infusions for those with potassium levels above
6.5mmol/L (89%)
Serum potassium rechecked within 2 hours of treatment (72%)
Blood glucose test within 1 hour of treatment (18%)
Availability of guidelines on wards and emergency departments (6%)
This has resulted in the development of guideline to standardise the recognition, assessment and management of patients with high potassium levels. This document will set out a structured approach and pathway of care, based on national guidance, to ensure patients with high potassium levels receive timely and agreed treatment and subsequent monitoring.
Teaching sessions have been delivered to junior doctors at their teaching days to increase awareness of national guidelines and management approach so there is a standardised treatment regime for patients with high potassium levels.
Use of Computerised Tomography Scans for Patients with Suspected
Pulmonary Embolism Audit
The aim was to audit practice against national guidelines on „how patients who have a suspected Pulmonary Embolism (PE) (Clot in the main artery of the Lung) presenting with chest pain or shortness of breath‟ are selected for a Computerised
Tomography (CT) scan
(Venous Thromboembolic Disease: guidelines for management & role of thrombophilia testing, NICE 2012).
The results demonstrated that 35% patients with suspected pulmonary embolism were received a CT scans on the same day as they presented. A further 40% of patients were scanned the following day.
To improve patient selection a patient risk assessment tool needs to be included on the radiology request form. A decision will be made on the best tool to use and how to implement it.
SLHT Quality Accounts 2012-13 Page 56 of 95
In line with national guidelines all patients who do not receive a scan on the same day should have their blood thinned with anticoagulants (the treatment for pulmonary embolism). Results showed not all patients had this treatment. The proposed plan is to implement guidelines via the intranet to ensure patients are managed in line with best practice guidance.
Recording Chest X-ray interpretation in Patient’s Notes Audit: Urgent and
Emergency Cases
The aim of this audit was to assess how many chest x-rays carried out by the
Emergency Department had a written opinion by the clinician at the time, i.e. when the evaluation of these chest X-rays would influence the management of the patient.
Planned improvements:
Feedback audit results at doctors‟ education sessions regarding their responsibility to document chest x-ray findings and the relevance this has in practice.
Create reminders to staff to document x-ray findings e.g. reminder messages on the computer screens, create a box on the "Emergency Department cards" (patient assessment documents) for chest x-ray findings. This will actively remind staff to document their findings, and prevent significant findings to be ignored or missed.
Videofluoroscopy Report Template Audit
The aim of the audit was to establish whether the SLHT Speech Therapy
Videofluoroscopy report template meets the minimum reporting standards stipulated by the Royal College of Speech and Language Therapists (2006; 2007).
The audit demonstrated that over 86% of reports met the majority of the reporting standards.
The key areas of non compliance were the inclusion of clinical questions, the feeding history of the patient, whether investigations had been reviewed/ordered, and the involvement of other professionals.
Following this audit the reporting template will be reviewed so that it incorporates the correct criteria to ensure correct completion. A review of staff training will also be undertaken so that everyone understands the national minimum reporting criteria and what is required for compliance.
SLHT Quality Accounts 2012-13 Page 57 of 95
3.7.2.4 Infection Prevention
Hand Hygiene Audit
Hand hygiene is recognised to be the most fundamental practice required to protect patients from infection. Clinical areas across SLHT are required to perform an audit of staff hand hygiene each month, measured against the World Health Organisation
‘My 5 moments for hand hygiene’ standards. In addition the Infection Prevention
Team also perform hand hygiene audits in a random sample of areas. The audits also monitor compliance with the Department of Health ‘bare below the elbows’ initiative.
The Trust has set a high standard of 95% for full compliance, in order to drive up standards and provide the maximum protection for our patients. Results show the following:
Month Apr
12
May June July Aug Sept Oct Nov Dec Jan
13
Feb Mar
86 90 93 94 94 95 93 91 86 90 91 92 Percentage
Compliance
This demonstrates a reasonable level of compliance with hand hygiene standards.
The results are reviewed by clinical leaders, and action taken at local level upon each audit to address any areas of concern or non-compliance by staff. The results demonstrate the need for most areas to continue their focus on hand hygiene in
2013, and the programme has been included again within the 2013-14 infection prevention audit programme for the Trust.
The Trust also has in place a programme of hand hygiene awareness via staff training, and monthly poster changing in clinical areas to refresh the message, based upon the successful „talking walls‟ programme in Geneva, and the National Patient
Safety „clean your hands‟ campaign which ran for several years. Alcohol hand gel is available where national guidance advises it should be, at „the point of care‟, and this is also monitored on a regular basis in clinical areas. The Trust will continue to make effective hand hygiene a high priority.
Clostridium difficile Infection
The Department of Health has a range of ‘high impact intervention’ audit tools for use specifically to reduce the risk of infection for patients. These are all part of the SLHT annual audit programme, including high impact intervention 7 ‘ Clostridium difficile infection’. These audits monitor key aspects of the care of patients who develop
Clostridium difficile infection. They are performed frequently/daily by infection
Prevention Nurses. Results show the following:
Month
Percentage
Compliance
Apr
12
May June July Aug Sept Oct Nov Dec Jan
13
Feb Mar
96 96 99 91 99 96 98 99 100 100 96 99
SLHT Quality Accounts 2012-13 Page 58 of 95
3.7.2.5
Any gaps in care are identified while the Infection Prevention nurse is on the ward, and feedback to the clinical staff for action. These audits continue as part of the management of patients with Clostridium difficile infection as part of the 2013-14 audit programme, along with a broad programme of work to stop patients from developing the infection.
Pharmacy Department
Antimicrobial Prescribing: Point Prevalence Antimicrobial Audit
The audit was undertaken to assess the quality of antimicrobial prescribing in terms of choice of antibiotic, route of administration and duration of therapy at SLHT.
At any one time, approximately one third of hospital in-patients are prescribed antimicrobials. Similarly, this audit found that 32% of hospital in-patients at SLHT were prescribed at least one antimicrobial agent. Though fewer in-patients were included in this audit relative to last year, antimicrobial prescribing at SLHT rose by
8%. A number of factors may explain this. Bed closures, since the last audit, accounts for the reduced number of patients and the rise in antibiotic use may reflect the inclusion of surgical prophylaxis and the higher turnover of acute admissions, particularly seen at the QE site.
There were demonstrated improvements in the choice of antibiotic prescribed, the route of administration and the documented duration of therapy since the last audit in 2011. During the audit a 110 interventions were made by the Antimicrobial
Management Team to optimise antimicrobial use. This commonly involved stopping antimicrobials. Despite improvements in documentation of a stop or review date, this was only achieved in 65% of cases. Since this audit, stop/review stickers have been implemented to highlight antibiotics in need of a documented duration. A number of wards have also introduced a system to flag patients for antibiotic review at the daily wards rounds. In addition, a new drug chart with a specific antimicrobial prescription section and automatic stop/review dates is due to be piloted.
Antibiotics should be used for the shortest possible time to treat an infection effectively to prevent the risk of side-effects and further infections developing. The audit revealed that 45% of patients were receiving intravenous antibiotics for more than two days, which has increased from previous years. Whilst this audit did not look at whether these patients were medically stable to be discharged, it suggests that perhaps more patients can be identified and offered Out-Patient Antimicrobial
Therapy, delivered either by District Nurse at home or via the Ambulatory Care service. This is in place at QE site and being proposed at PRU.
Antimicrobial Care Bundle Audits
The purpose of the audit was to assess the quality of antimicrobial prescribing using a set of prescribing standards (“care bundle”) which together produce better
SLHT Quality Accounts 2012-13 Page 59 of 95
outcomes. The standards used are: documentation of allergy status; documentation of an indication for the antibiotic(s); documented duration or review date; appropriate route of administration; and compliance with SLHT antimicrobial guidelines and policies. Audits are conducted monthly on all wards and feedback is shared to highlight areas for improvement.
Elements of care that are consistently achieved according to the standard set
(100%) are the documentation of allergy status and administration of antibiotics via an appropriate route of administration. The documented indication and choice of appropriate antibiotic(s) are generally performed well. Results are shared with consultants so that areas for improvement can be addressed with prescribers. Wards are targeted for teaching sessions and Antimicrobial Management Team support through the use of these audits so that prescribing of antibiotics can be delivered in a safe and effective manner.
Since the audits were initiated, the documentation of treatment duration or review dates has improved (from 52% to 60-80%). However, continued efforts to achieve further this care element are necessary. Stop/review stickers for the drug charts and patient notes have been implemented to highlight patients prescribed antibiotics in need of a documented duration. A number of wards have also introduced a system to flag patients for antibiotic review at the daily wards rounds. In addition, a new drug chart with a specific antimicrobial prescription section and automatic stop/review dates is due to be piloted. Antibiotics should be used for the shortest possible time to treat an infection effectively to prevent the risk of side-effects and further infections developing.
Medicine Administration Errors in Stroke Patients with Dysphagia Audit
A review into the medication management of patients with dysphagia within SLHT revealed that there was no formal SLHT policy or guidance for staff. However, there are comprehensive guidelines on the management of dysphagia in stroke patients from the Royal College of Physicians. Adherence to these guidelines means all patients admitted to the Trust, who have had a stroke, have their „swallow‟ screened by a dysphagia trained nurse. Moreover, if an abnormal swallow was identified, they would have further assessment and care by a speech therapist.
As a consequence of this review it was decided to audit the Trust‟s management of medicine administration for patients with dysphagia. It was felt that the stroke units were the optimal setting to launch a pilot audit looking at medicine administration
(both in terms of pharmacological, diet and fluid requirements) in patients with dysphagia.
The benefit of using stroke patients as a population to study dysphagia management is there is a high incidence of dysphagia in patients after stroke, and the dysphagia management guidelines meant it would be easy to identify a population for our sample.
SLHT Quality Accounts 2012-13 Page 60 of 95
Following these results, the Trust is in the process of implementing a project involving a multifaceted response. An education program has been initiated on dysphagia and medicine administration to the SLHT pharmacy and speech therapy teams. Plans are in place to disseminate the audit results through local governance, and offer training to other teams involved in medicine administration in this population; i.e. nursing and medical staff. A policy will be developed which will provide clear guidance with regards to medicine administration in patients with dysphagia in line with best practice.
Quality of Once Daily Dose Gentamicin Prescribing and Monitoring Audit
Gentamicin is a very effective antibiotic and is recommended at SLHT for the treatment of a number of infections including sepsis and as an alternative agent for infections in patients with a penicillin allergy. Once daily Gentamicin dosing is recommended to optimise the therapeutic effect of the antibiotic and minimise toxicity. A dosage calculation is required, which is based on the patient's weight and renal function.
Following the 2011 audit results, the Trust has taken measures to improve the accuracy of Gentamicin prescribing following the 2011 audit results. These include the introduction of an electronic Gentamicin dose calculator, a 24/7 laboratory service to test for Gentamicin Therapeutic Drug Monitoring levels, staff training and improved accessibility of policies and guidelines on the Trust Intranet.
A re-audit was undertaken to measure the quality of prescribing and monitoring of
Gentamicin in adults at SLHT and to ascertain whether this is in accordance with the
SLHT guidelines.
Overall, Gentamicin prescribing and monitoring has improved at SLHT following a number of strategies to raise the standards following the audit in 2011. Further actions under consideration for improving the accuracy of Gentamicin prescribing and monitoring include:
Better documentation of patient height and weight
Dissemination of training slides to all doctors
Updating the guidelines to simplify the processes involved and references to resource aids
Improving the availability of the therapeutic drug monitoring stickers or incorporation into the drug chart to assist with taking and monitoring of levels.
Safe and Secure Storage of Medicines Audit
Ensuring that medicines are safely stored at ward level in line with Department of
Health guidelines is a key responsibility for Trusts. The aim of this audit was to
SLHT Quality Accounts 2012-13 Page 61 of 95
determine whether medicines were stored safely at SLHT and to identify what measures needed to be taken, if any, to ensure medicines are stored securely.
This results of this audit demonstrated that considerable improvements have been made since previous audits. A number of further recommendations have been made e.g. produce a guide to the management of fridge thermometers in wards, review storage of fluids on wards and ensure all fluids are stored in locked areas.
Venous Thromboembolism Audit
The underlying principle for auditing Venous Thromboembolism (VTE) is improve VTE risk assessment in adult patients at admission to ensure appropriate thromboprophylaxis is given and to prevent venous thromboembolism which is potentially fatal.
Several audits were undertaken in the year which focused on VTE risk assessment, appropriate thromboprophylaxis and information on VTE provided to patients admitted to hospital.
VTE risk assessment has improved from around 80% in April 2012 to around 90% currently. This should ensure appropriate thromboprophylaxis, and prevent hospital acquired VTE.
Audits show that approximately 80% of patients risk-assessed received appropriate thromboprophylaxis. When looking at appropriate thromboprophylaxis following orthopaedic surgery, 100% of patients were prescribed extended thromboprophylaxis appropriately.
One audit focused on patient information at admission which demonstrated that 77% of patients had written information available. Further work was carried out to ensure patients receive information on discharge which resulted in VTE being included in the pharmacy information leaflet that accompanies all drug prescriptions that patients are given when they are discharged home.
Following each audit, performance is fed back to care groups to improve nursing and consultant engagement in improving risk assessment and the availability of written information to patients. Repeat audits are planned for 2013/14.
3.7.2.5 Surgery
Breast Screening with B3/B4 Needle Biopsy Audit
Needle Core Biopsy (NCB) is frequently used in assessing screen-detected breast lesions.
Uncertainty remains over appropriate management of NCBs reported as „uncertain malignant potential‟ (B3) or „suspicious of malignancy‟ (B4). This audit aimed to establish positive predictive values (PPVs) for malignancy on excision biopsy, for different classifications of B3 and for B4 NCBs.
SLHT Quality Accounts 2012-13 Page 62 of 95
Between 2000/2010, 5324 patients underwent NCB, including 14G (ultrasoundguided) and 10G vacuum assisted biopsies (stereo-guided). Four hundred and forty four (n= 444) were B3 (8.3%) and 38 (0.7%) B4. NCBs reported as B3 were classified by pathological subtype and PPVs for malignancy calculated for each subtype. Outcomes following B4 NCB were also assessed.
The overall PPV for malignancy for B3 NCBs was 25% and for B4 NCBs was 74%.
The PPVs for each subtype of B3 classification were as follows: papillary 14%, atypical intraductal epithelial proliferation 35%, phyllodes 11%, lobular 47%, complex sclerosing lesion/radial scar 6%, columnar cell 29%.
The overall PPV for malignancy for B3 NCBs was 25% and for B4 NCBs was 74%.
The PPVs for each subtype of B3 classification were as follows: papillary 14%, atypical intraductal epithelial proliferation 35%, phyllodes 11%, lobular 47%, complex sclerosing lesion/radial scar 6%, columnar cell 29%.
The following improvements were implemented in the South East London region
Breast Units in 2012 providing a consistent standard of care across the region and improving the likelihood of patient recovery:
NCBs reported as B4 have a high likelihood of malignancy and are surgically removed
Atypical B3 subtypes are treated as suspicious and preferably surgically removed
Decisions regarding further assessment are made in a multidisciplinary setting so the patient benefits from a broad range of experience
Colonoscopy Completion Rate and Complications Audit
An audit was carried out to evaluate the colonoscopy completion rate at PRU. The
British Society of Gastroenterology (2011) standard for completion, i.e. successful, colonoscopies is 90%. A re-audit was then carried out to determine if improvements had been made.
The initial audit revealed a completion rate of 86.7%. Causes of failure were identified as: loopy colon; instrument failure; narrow lumen; acute angulation ; patient discomfort and Pathology encountered.
Following the audit Endoscopists attended training to improve their technique; smaller size scopes were used when appropriate e.g. for narrow lumen; sedation or general anaesthetic was used for low pain threshold patients.
Upon re-audit the completion rate had increased to 90.2% which is slightly better than the National Standard. Improving the completion rate reduces the need for repeat procedures and results in earlier diagnosis, reduced risk, less inconvenience to patients and lower costs.
Gastro-Jejunostomy Stricture Following Laparoscopic Gastric Bypass for
Obesity Audit
SLHT Quality Accounts 2012-13 Page 63 of 95
When Gastro-jejunal anastomosis (joining the stomach to the small intestine) is part of laparoscopic gastric bypass operation for obesity then stricture (narrowing at the junction of the stomach with small intestine) can occur. This leads to further treatment to dilate the stricture or, if this is not successful, the surgery may need to be repeated. There are no National guidelines but International studies indicate a rate of no more than 7.3%.
An audit in 2011/12 revealed a 9.7% incidence of stricture. The following changes to practice were made to decrease the incidence of stricture:
The surgical method for joining the stomach to the small intestine
The brand of stapler used to connect the join
The spacing of the staples
A repeat audit of a total of 238 patients who had the operation performed using the new techniques, between February and July 2012, showed no clinical evidence of stricture (narrowing). This demonstrates an improvement in surgical practice and patient outcome.
Reducing Day Surgery Cancellations Audit
The study was conducted on the QE site over a 6 month period. The aim was to determine the number and reason for day surgery cancellations. The study revealed a 27% cancellation rate. Various reasons for cancellation were recorded which included; bed not available, booking administration errors and equipment issues. By far the largest reason was patient did not attend (DNA) or cancelled. Ten percent of cancellations were made on the day of surgery which is over double the rate of the benchmark (Kings College Hospital).
To reduce cancellations due to „bed not being available‟ a management decision was made to move the majority of day case surgery to QM (i.e. where beds are available) which was implemented from January 2013. Further work is required to address issues around DNA.
Timing of Out of Hours CT Scans Audit
A computerised tomography (CT) scan, also known as a CAT scan, uses X-rays and a computer to create detailed images of the inside of your body. The CT department at QEH aims to perform all emergency CT scans within one hour of them being requested. This audit is to determine whether the department is meeting this target and, if not, to identify the cause.
Ninety-seven percent (97%) of patients who attend the CT department had the CT scan within one hour of the request. This demonstrates a high standard of practice and with no immediate actions required.
Adult Emergency General Surgical Admission pathway Audit
SLHT Quality Accounts 2012-13 Page 64 of 95
In 2011 a review of London hospital based acute medicine and emergency general surgery found that there was wide variability in consultant involvement in the assessment and management of acutely unwell patients, especially overnight and at the weekend. As a result, London Health Programmes developed evidence based clinical quality standards. This audit looked at those standards in relation to
Emergency Surgical Admissions.
The findings were:
• Consultant review 12 hours post admission (60%)
• Patient seen on twice-daily ward rounds by consultant (21%)
• Urgent imaging within 12 hours (73%)
• On call anaesthetic consultant involved in all emergency operations (57%)
• Consultant to consultant ITU referrals (67%)
Recommendations from this audit include the development of a surgical protocol and surgical emergency admission proforma which are currently under review.
Surgical Endodontics carried out in a Maxillofacial Department at QM Audit
This audit aimed to measure the quality of follow up and outcomes following surgery for apisectomy.
The audit revealed that 25% of patients who had an apisectomy did not have a post surgery follow up appointment at SLHT. Of the patients who had a follow up appointment the first appointment varied from 2 weeks to 2 months, and these patients reported:
Experiencing pain (8%)
Swelling (17%)
The following improvements were identified:
Continual professional development in weekly teaching program for updates on new filling materials and techniques
A document (proforma) was developed which enabled all clinicians to follow a systematic review at initial appointment ensuring the apisectomy procedure was prescribed correctly and appropriately. It also provides a feedback mechanism that secondary care clinicians can use to report and update the GDPs with a detailed letter which is also copied to the patient
The proforma also includes a review section to ensure patients are monitored throughout their recovery before being discharged to the GDP. It provides a source of information for future clinicians to audit the outcome of the surgical procedure so that services can be improved
SLHT Quality Accounts 2012-13 Page 65 of 95
3.8 National Confidential Enquiries
National confidential enquiries are studies which cover many different aspects of medical and surgical care. National reports are published which make recommendations to improve the quality of care and Trusts are required to participate in these studies. Depending on the subject of the study, enquiries may be more or less relevant to the Trust.
The national confidential enquiries that the Trust participated in, and for which data collection was completed during 2012/13, are listed below alongside the number of cases submitted to each enquiry. The trust participated in all the national confidential enquiries for which it was eligible.
This included studies into bariatric surgery (for weight loss); cardiac arrest procedures; alcohol related liver disease; and Subarachnoid haemorrhage – study of patients with aneurysmal subarachnoid haemorrhage, looking both at patients that underwent an interventional procedure and those managed conservatively. The studies into Bariatric Surgery and cardiac arrest procedures have been published and considered by the Trust and actions agreed.
Table N1: bariatric surgery
Cases included
Clinical questionnaire returned
Case notes returned
3 3 3
Table N2: cardiac arrest procedures
Sites participating
Organisational questionnaire returned
3 2
Cases included
Prospective forms returned
Questionnaires returned
Case notes returned
Sites participating
14 16 9
Table N3: alcohol related liver disease
Cases included
Prospective forms returned
Case notes returned
9
Sites participating
2 6 5 6
Table N4: subarachnoid haemorrhage
Tertiary Secondary
Organisational questionnaire returned
2
4
Case notes Sites
Organisational questionnaire returned
2
Organisational
SLHT Quality Accounts 2012-13 Page 66 of 95
Cases included
5
Cases
Excluded
3
Questioner returned questioner returned returned participating questionnaire returned
0 2 5 4
Please note this study is still open and figures have not been finalised.
1
SLHT Quality Accounts 2012-13 Page 67 of 95
3.9 Research – participation in clinical research
During the year from 01/04/2012 to 31/03/2013 South London Healthcare Trust
(SLHT) was involved in 164 clinical research studies in 21 specialties (see table below).
Patients were recruited from NHS services provided or sub-contracted by SLHT, with all research activities approved by a research ethics committee. In total, 984 patients were recruited to these trials, exceeding our target of 875 for the year.
Participation in clinical research demonstrates the Trust‟s commitment to improving the quality and range of treatments we offer and to making our contribution to the wider health R&D agenda. Our active participation in research and the development of innovative treatments contributes to improved patient outcomes.
Oral and Gastrointestinal
Cancer
Reproductive Health and Childbirth
Cardiovascular
Musculoskeletal
Skin
Eye
Inflammatory and Immune System
Neurological
Metabolic and Endocrine
Meds for Children
Diabetes
Generic Health Relevance
Injuries and Accidents
Infection
Stroke
Mental Health
Respiratory
Blood
Dementias and Neurodegenerative Diseases
Renal and Urogenital
SLHT used national systems to manage the studies in proportion to risk. The
National Institute for Health Research (NIHR) supported 127 of these studies through its research networks.
SLHT Quality Accounts 2012-13 Page 68 of 95
3.10 Goals agreed with commissioners – using CQUIN framework
A proportion of South London Healthcare NHS Trust (SLHT) income in 2012-13 was conditional on achieving quality improvement and innovation goals between the
Trust and commissioners, through the Commissioning for Quality and Innovation
(CQUIN) payment framework.
Further details of the agreed goals for 2011/12 and for 2012/13 are available from
Jennie Hall (Deputy CEO/ Chief Nurse) by emailing jennie.hall1@nhs.net
In 2012/13, income equal to 2.5% of the value of our main acute contract, which covers most of our NHS services, was conditional on achieving CQUIN goals agreed with our host commissioner, Bromley PCT.
In addition we also agreed CQUIN payments linked to our work in Specialised
Services, which are commissioned by the London Specialised Commissioning Group.
We have accounted for achieving 70% of our Regional and National CQUIN-related goals in 2012/13 for which we received a payment of £6.6m* out of a maximum of
£9.4m. This has not yet been agreed and signed off by the Host Commissioner.
We also achieved 100% of our Specialist Commissioning CQUIN-related goals in
2012/13 for which we received a payment of £47k* out of a maximum of £47k.
Overall, we have accounted for achieving 70% of our CQUIN-related goals in
2012/13 for which we received a payment of £6.7m* out of a maximum of £9.5m.
* All data above is subject to Q4 sign off which will be confirmed in July 2013
The full list of the 2012/13 schemes is illustrated in the table below.
CQUIN schemes 2012/13
No CQUIN Description
VTE risk assessment and prophylaxis
1 To reduce avoidable death, disability and chronic ill health from venous thromboembolism by ensuring timely risk assessment, prophylaxis and education.
2
Patient Experience (personal needs)
The indicator is a composite, calculated from 5 survey questions. Each describes a different element of the overarching patient experience theme "responsiveness to personal needs of patients".
SLHT Quality Accounts 2012-13 Page 69 of 95
3
The elements are: 1) Involvement in decisions about treatment/care, 2) Hospital staff being available to talk about worries/concerns, 3) Privacy when discussing condition/treatment, 4) Being informed about side effects of
medication,
5) Being informed who to contact if worried about condition after leaving hospital.
Safety Thermometer (harm free care data submissions)
To reduce harm.
To allow the comparison of safety data on a national level
4
Dementia (FAIR – Find, Assess, Investigate and Refer)
Identification of at least 90% of patients aged 75 and over following emergency admission to hospital, using the dementia case finding question and those with delirium and dementia.
Diagnostic assessment and investigation of at least 90% of those patients who have been assessed as at-risk.
The referral of at least 90% clinically appropriate cases for specialist diagnosis of dementia and appropriate follow up.
Cardiology (identifying and recording symptoms and signs of specified conditions)
5
6
7a
7b
The Trust is required to demonstrate adherence to evidence-based practice and engagement with primary and community care by:
Providing documentary evidence of shared development in pathways, referral guidelines and audits etc.
Providing evidence of joint working relationships between acute and community sectors e.g. joint posts, consultants in the community.
Production of evidence-based, appropriate patient information for these conditions.
Providing evidence of sharing expertise e.g. attendance at relevant PCT meetings etc.
The Trust will engage with commissioners to allow auditing of care plans and documentation relevant to this scheme.
To quantify the quality and productivity gains as a direct result of this CQUIN initiative and determine how this will be realized
Nutrition (robust nutritional screening, protected mealtimes, use of „Red Trays‟).
Procedures and policies in place to meet patient‟s nutritional needs.
Establishment and participation in multidisciplinary meetings including all stakeholders in health and social care economy
Trust to ensure evidence is identified and circulated for the creation of a nutrition policy and practice framework by the multidisciplinary stakeholders group
To improve the overall prevention and management of foot problems in patients with diabetes
Development and implementation of a new pathway for these patients
Management of HBa1c in pregnant women with diabetes
SLHT Quality Accounts 2012-13 Page 70 of 95
8
9a
9b
9c
9d
10
11a
11b
To ensure all women receive appropriate management for their diabetes during pregnancy
Medicine Optimisation – Integrated formulary
This is to be achieved via shared medicine guidelines across primary and secondary care and/or through an integrated formulary.
Evidence of achieving a 25% reduction in grade 2 and 3 pressure ulcers by 2013 and meeting the quality schedule and data reporting requirements
Evidence of no grade 4 pressure ulcers (zero allowed) (unless formally de-escalated by NHSL) and meeting the quality schedule and data reporting requirements
Evidence of meeting a 25% reduction of total number of falls by quarter 4 and meeting the quality schedule and data reporting requirements
Evidence of meeting a 33% reduction of numbers of falls resulting in high and catastrophic „harm‟ by quarter 4 and meeting the quality schedule and data reporting requirements
Communication and engagement
The focus of this CQUIN is to improve partnership working and communication between primary and secondary care particularly in relation to patient discharge and follow up care.
Smoking Cessation
Identification and referral to smoking cessation service. Development and delivery of training programme for key staff.
Alcohol – screening an intervention within identified wards and departments
12
13a
13b
14
Cancer – working with the cancer network to improve staging for cancer
Ophthalmology (Education)
Ophthalmology. Educational support / clinic sessions for optometrists seeking to be involved in glaucoma shared care and the development of secondary care led community eye-care initiatives for patients with Ocular Hypertension
(OHT)/Stable Glaucoma.
Ophthalmology (Communication with original referrers)
Improving general ophthalmology referral feedback to community optometrists
Data Quality
To deliver a quality information and business intelligence service to commissioners that enables informed planning and decision making. SLHT are required to fulfil deliverables through the joint Business Intelligence Project
Team (BIPT) and improved data quality outcomes in monthly reporting.
3.11 What others say about the Trust
Statements from the Care Quality Commission
South London Healthcare NHS Trust (SLHT) is required to register with the Care
Quality Commission (CQC) and its current registration status is
registered without conditions
.
The CQC has not taken enforcement action against SLHT during 2012-13.
SLHT Quality Accounts 2012-13 Page 71 of 95
CQC investigations or reviews during 2012-13
During the course of 2012-13 the Trust was subject to unannounced inspection visits by the CQC, and was deemed to be compliant with most outcome measures.
However, we did not demonstrate compliance with Outcome 21: Records at
Orpington Hospital, for which a detailed action plan has been implemented. The
Trust submitted evidence of compliance by the end of April 2013.
The other outcome for which compliance issues were identified was Outcome 9:
Management of Medicines. This related to the safe storage of medicines at the
Queen Elizabeth Hospital (QEH) and Princess Royal University Hospital (PRUH) sites.
Again, immediate action was taken to address the issues identified. A follow up visit by the CQC noted improvements had been made, which moved the Trust from a position of moderate to low concerns, with further minor improvements required.
The Trust expects to submit evidence of compliance with this outcome by the end of
May 2013.
The Trust received two alerts from the CQC during the course of the year, one related to Maternity, concerning the readmission rates of (non-elective) women admitted following delivery and the other related to patients admitted with cardiac dysrhythmias who subsequently died.
Both areas have been subject to review. A response to the Maternity Outlier report has been shared with the CQC. In relation to the cardiac dysrhythmias alert each case was subject to a detailed clinical review, and no specific concerns regarding care and treatment were identified. A detailed case by case response has been shared with the CQC.
SLHT Quality Accounts 2012-13 Page 72 of 95
3.12
3.12.1
Data quality
Statement on relevance of Data Quality & actions to improve Data
Quality
South London Healthcare Trust (SLHT) continued to work closely with its commissioners in South East London during 2012/13 to improve its Data Quality from the moment patient data is entered onto the Patient Administration System, to the point where the activity is reported to the national Secondary Uses Service for the NHS (which is the public record of the patient care that the Trust delivers for patients).
We will continue to drive Data Quality improvement by:
Ensuring we maintain the correct demographic details for all of our patients.
Highlighting any issues and addressing them through training and procedures for staff.
Monitoring and reporting data quality throughout the Trust and comparing our progress to other NHS Trusts
3.12.2 NHS Number and General Medical Practice Code Validity
SLHT submitted records during 2012/13 to the Secondary Uses Service for inclusion in the Hospital Episode Statistics.
The following two areas of Data Quality are particularly important for patient safety
(to be able to identify patients appropriately and to communicate patient information to the correct GP practice). The figures below demonstrate an improvement in data quality throughout 2012/13 (the 2011/12 figures are in brackets).
The percentage of records based on the Trust Data Warehouse which included the patient‟s valid NHS number was:
99% (99%) for admitted patient care;
99% (95%) for out-patient care; and
98% (97%) for accident and emergency care.
The percentage of records based on the Trust Data Warehouse which included the patient‟s valid General Medical Practice Code was:
99% (98%) for admitted patient care;
99% (98%) for out-patient care; and
98% (95%) for accident and emergency care
SLHT Quality Accounts 2012-13 Page 73 of 95
3.12.3 Payment by Results Coding Review
PRUH
In 2012/13, an audit of ante/postnatal coding was undertaken. The error percentages are as follows:
Primary
Diagnosis
8.9%
Secondary
Diagnosis
28.6%
Primary
Procedure
0%
Secondary Procedure
100%*
QE 6.0% 11.6% 0 0
3.12.4
* the records in this audit included very few procedures. There was only one secondary procedure in the audit. This one secondary procedure was incorrectly coded, hence the 100% error rate reported. All primary procedures were coded correctly.
Information Governance Toolkit attainment level
SLHT Information Governance Assessment Report overall score for 2012/13 was
68%. Three out of the 45 requirements did not meet the required standard (Level 2) and were graded red (Information Governance Toolkit Grading Scheme). The Trust has plans in place to attain Level 2 for these 3 requirements by the end of
September 2013.
There have been no Serious Incidents (SI) relating to data breaches during 2012/13.
3.12.5 Clinical coding error rate
In order to continue improvements in the coding error rate, SLHT Coding department will put emphasis on the following:
TRAINING (Information Governance Level 3)
Continue to roll out a training programme to all levels, to include:
Foundation course
Workshops for Obstetrics, Circulatory, Neoplasm, T&O
Refresher Course
Pre ACC workshop
Continual mentoring for trainees
AUDIT (Information Governance Level 2)
Continue to roll out an audit programme, to include:
SLHT Quality Accounts 2012-13 Page 74 of 95
Specialties
Individual Coders
O/P & A/E
Site
VALIDATION (Information Governance Level 2)
Continue to work with Clinical staff to validate diagnosis and procedure abstracted from the case note.
SLHT Quality Accounts 2012-13 Page 75 of 95
3.13
3.13.1
Review of Mandatory Quality Indicators
Summary Hospital-level Mortality Indicator
SHMI measures deaths that happen both in an NHS hospital and that occur within 30 days of discharge from a hospital stay. It is the ratio between the actual number of patients who die following a treatment at the trust and the number that would be expected to die on the basis of average England figures, given the characteristics of the patients treated there.
SHMI gives an indication for each hospital trust in England whether the observed number of deaths within 30 days of discharge from hospital was higher than expected, lower than expected or as expected when compared to the national baseline.
Jan 11–Dec 11 Apr 11–Mar 12 Jul11–Jun 12 Oct 11–Sep 12
SHMI score
0.9457
Comparison with 142 NHS Trusts:
0.9852
Range = 0.6849 to 1.2107
1.0157 1.0334
Mean = 1.0005
SLHT ranked 82 nd from 142
SLHT considers that this data is as described for the following reasons:
SLHT has procedures in place to review both HSMR and SHMI mortality indicators
The reviews so far have shown that most of the patients within the high SHMI cluster were elderly patients with complex co-morbidities
These patients also had an extended length of stay within hospital whilst waiting for the most appropriate placement at discharge
SLHT intends to take the following actions to improve the indicator and percentage, and so the quality of its services, by :
Continuing to review both HSMR and SHMI mortality indicators
3.13.2 % patient deaths with palliative care coded at either diagnostic or specialty level
SLHT Quality Accounts 2012-13 Page 76 of 95
This is an indicator designed to accompany the Summary Hospital-level Mortality
Indicator (SHMI). The SHMI makes no adjustments for palliative care. This indicator gives a measure of the deaths occurring under palliative care conditions for each provider reported in the SHMI.
SLHT rate = 28.9% (data for 12 months Oct 2011 – Sep 2012)
Mean = 18.9%
SLHT ranked 129 th from 142 NHS Trusts
SLHT considers that this data is as described for the following reasons:
This indicator requires further analysis within SLHT to fully understand our data and our position
During standard reviews of data we have identified that this group of patients have attended the hospital mainly due to inability to cope at home with current support or have required hospital admission for management of new symptoms by the underlying disease
SLHT intends to take the following actions to improve the indicator and percentage, and so the quality of its services, by:
Reviewing this patient group in greater detail to ensure that the reason for admission is / has been accurately coded. Once we have fully understood the detail behind this data we shall be in a position to respond appropriately.
SLHT Quality Accounts 2012-13 Page 77 of 95
3.13.3 Patient Reported Outcome Measures
Patient Reported Outcome Measures (PROMs) are a way of collecting information on the effectiveness of the care provided to patients as perceived by patients themselves. Since 1st April 2009, information has been collected and reported for
hip and knee replacements
,
groin hernia
and
varicose vein surgery
. Patients undergoing these procedures are invited to complete a questionnaire before their operation and a later questionnaire following their operation. This measures their improvement following their operation. The latest finalised data which is available from the NHS
Information Centre dates from Apr 2010 to Mar 2011 and is described in the table below. PROMs are scored in a number of ways. The index used in this report is based on a combination of five key criteria concerning patients‟ general health.
These are:
Mobility
Self-care, e.g. washing and dressing
Usual activities, e.g. work, study, housework, family or leisure activities
Pain/discomfort
Anxiety/depression
The value is presented as “adjusted average health gain”, with 1 being the maximum score. The higher the value, the higher the perceived improvement in health reported by the patient following treatment. The data are the most recent available, covering the 12 months April 2010 to March 2011.
Adjusted average health gain (EQ-5D index case mix adjusted health gain)
Procedure
SLHT
2009-10
England
2009-10
SLHT
2010-11
England
2010-11
Groin hernia 0.112 0.082 0.08 0.085
Hip replacement
Varicose veins
Knee replacement
0.385
0.262 n/a
0.411
0.295
0.395
0.318 n/a
0.405
0.299
SLHT considers that this data is as described for the following reasons:
The data in the table suggests that for all 3 procedures the average health gain is within the expected range when compared with data for England during 2010-11
Knee replacements demonstrate the most significant improvement
SLHT intends to take the following actions to improve the indicator and percentage, and so the quality of its services, by:
SLHT Quality Accounts 2012-13 Page 78 of 95
SLHT will continue its focus and monitoring of health gains within these procedures
3.13.4 Readmission within 28 days of discharge
Data are presented as “standardised to 2006-07”, meaning we can compare performance using readmission rates from 2006-07 as a baseline. Data for SLHT are only available from 2009-10 when the Trust was formed.
(i) Age 0 to 14
Readmission rate
Banding 1
2009 - 10
6.12%
B1 n/a
2010 - 11
8.03%
B1
-31.21% % performance change from previous year
England average 10.18 10.15
1 5 band comparison against national average where B1 = significantly better than the national average at the 99.8% level
(data for 12 months Apr 2010 – Mar 2011)
SLHT considers that this data is as described for the following reasons:
The data shows that the readmission rate continues to be significantly better than the national average for this age group
SLHT intends to take the following actions to improve the indicator and percentage, and so the quality of its services, by:
No specific actions are planned but SLHT will continue to monitor this closely
Local data for 2011/12 and 2012/13 indicates the readmission rate remains below the national average
SLHT Quality Accounts 2012-13 Page 79 of 95
(ii) Age 15 or over
Readmission rate
Banding 1
% performance change from previous year
2009 - 10
10.98%
W n/a
2010 - 11
12.46%
A1
-13.48%
England average 11.16 11.42
1 5 band comparison against national average where
A1 = significantly poorer than the national average at the 99.8% level
W = national average lies within expected variation (95% confidence interval)
(data for 12 months Apr 2010 – Mar 2011)
SLHT considers that this data is as described for the following reasons:
The data suggests that the readmission rate for the over 15 age group was consistent with the national average in 2009/10 but was below the national average in 2010/11
Earlier in the year the trust‟s position was above the national average but in August and September the data showed that the trust was below the national average showing an improving performance
SLHT intends to take the following actions to improve the indicator and percentage, and so the quality of its services, by:
SLHT monitors readmissions using the Dr Foster Real Time Monitoring tool and this shows that the readmission rate for 2011/12 and for April to October 2012/13 is consistent with the national average
Monitoring identified that the readmission rate was being affected by data quality issues when patients transferred between hospital sites and these have now been addressed
SLHT continues to monitor the readmission rate closely and will investigate and work closely with partners to understand and address material trends
3.13.5 Responsiveness to the personal needs of patients
Consultation feedback indicated that personalisation and service responsiveness are important issues for inpatients. This indicator aims to capture patients‟ experience of this.
The indicator is a composite, calculated as the average of 5 survey questions from the inpatient survey. Each question describes a different element of the overarching theme, “responsiveness to patients‟ personal needs”.
SLHT Quality Accounts 2012-13 Page 80 of 95
1.
Were you involved as much as you wanted to be in decisions about your care and treatment?
2.
Did you find someone on the hospital staff to talk to about your worries and fears?
3.
Were you given enough privacy when discussing your condition or treatment?
4.
Did a member of staff tell you about medication side effects to watch for when you went home?
5.
Did hospital staff tell you who to contact if you were worried about your condition or treatment after you left hospital?
Average weighted score of 5 questions relating to responsiveness to inpatients' personal needs (Score out of 100)
SLHT score
England average
2009-10 2010-
11
61.8
66.7
61.7
67.3
2011-
12
61.7
67.4
The data above is the average score for the 5 questions as listed above which are included in the National inpatient survey
The Trust has made improvement in questions 1, 3 and 5 compared to last year‟s scores which is positive
However scores for questions 2 and 4 have not improved from last year - the scores are in the bottom 20% of worse performing trusts.
SLHT intends to take the following actions to improve the indicator and percentage, and so the quality of its services, by:
3.13.6
The Trust will be meeting with key stakeholders on each site of the Trust to identify and agree key action to be taken. This work will be integrated with the development of a site based action plans in response to the results from the 2012 National inpatient survey.
% of staff who would recommend the trust to family or friends
(from NHS National Staff Survey 2012)
47% of staff agreed or strongly agreed with the statement “If a friend or relative needed treatment, I would be happy with the standard of care provided by this
Trust.” This compares to 41% in 2011.
The staff survey recorded a summary score of 3.21 in response to the question “staff recommending the Trust as a place to work or receive treatment”. This compares to
3.07 in the 2011 survey. For scale summary scores, the minimum is 1 and the maximum 5. The Trust therefore improved on the overall summary score from the
SLHT Quality Accounts 2012-13 Page 81 of 95
2011 position (with the higher the score the better in this indicator), however the national average was 3.57 and therefore the Trust recorded a lower than average response.
Staff perception of the Trusts commitment to patient care as first priority is reported to have increased in the 2012 staff survey, and it is not therefore surprising that the
%of staff agreeing that they would recommend the Trust to friends and family has increased
SLHT intends to take the following actions to improve the indicator and percentage, and so the quality of its services, by:
Continuing to seek staff feedback about their perception of service delivery and recommendations for service improvement
Recognise and disseminate examples of good quality care from staff across the Trust so that staff are aware of achievements and improvements in service delivery.
Feedback to staff who raise concerns/escalate issues for example SUI‟s/Datix reports, so that staff are assured that action has been taken to address concerns.
3.13.7 % of admitted patients who were risk assessed for VTE
SLHT score
England average
Q1
86.9
93.4
Q2
90.5
93.8
Q3
90.3
94.1
Q4
92.9
SLHT considers that this data is as described for the following reasons:
During 2012-13 we extended our focus from simply assessing whether patients have had an appropriate risk assessment when they are admitted to hospital, to making sure patients are prescribed appropriate medication (prophylaxis) and are given information about VTE
SLHT intends to take the following actions to improve the indicator and percentage, and so the quality of its services, by:
Continuing to report on VTE risk assessment on UNIFY and feedback results to Trust staff via SLHT‟s Quality and Safety Report
Completion of Root Cause Analysis (RCA) Reports for
3.13.8 Rate per 10,000 bed days of cases of CDI for patients aged 2+
2007-08 2008-09 2009-10 2010-11 2011-12
SLHT Quality Accounts 2012-13 Page 82 of 95
SLHT rate
England average
70.8
93.3
41
54.9
26.5
36.7
16.9
29.6
20.8
21.8
(Data prior to April 2009 for Bromley Hospitals NHS Trust, Queen Elizabeth Hospital NHS
Trust and Queen Mary‟s Sidcup NHS Trust are combined)
SLHT considers that this data is as described for the following reasons:
Nationally it is recognised that the rate of infection, taking account of the number of patients treated per day/year, is a more accurate measure of performance than a numerical target. Health Protection Agency benchmark data shows that SLHT continues to have a better rate of infection per 10,000 bed-days than the average for
London and for England. Patients at SLHT therefore have less chance of acquiring
Clostridium difficile
infection than they would in the „average‟ hospital.
SLHT has taken the following actions to improve the indicator and percentage, and so the quality of its services, by:
The key issues which reduce avoidable CDI are prudent antimicrobial prescribing, hand hygiene, isolation, and cleanliness. Actions in place in the Trust focus on these elements.
The Trust continues to implement a programme of hand hygiene awareness, using the „talking walls‟ approach which has been successful in many countries. A programme of monthly audit of staff compliance with hand hygiene, including „bare below the elbows‟ is in place in each area to check on practice and drive up standards. There was some difficulty in ensuring all areas participate in this programme, but increased focus has been put into place through Matrons to make sure it is happening consistently.
The Trust has an isolation flowchart in place, which is used as a quick guide for staff to ensure anyone with potentially infectious diarrhoea is moved into a single room quickly. Monitoring has shown that compliance is generally good with this requirement, though there are occasional lapses. When these are detected the ward sister is contacted and asked to ensure the staff member involved is reminded of the standards required.
Pharmacist ward rounds highlight any issues with antimicrobial prescribing, and consultant microbiologists and antimicrobial pharmacists meet with medical staff in a variety of departments to jointly review how prescribing can be improved. Monthly antimicrobial prescribing care bundle audits are performed and results are fed-back to all consultants. Some areas now achieve high scores on the care bundle audit, indicating very good practice. This is not yet consistent throughout the trust and additional work is going on in key areas where improvement could be made.
A programme of audits of key infection prevention practices is in place across the
Trust, and this includes isolation practice. This monitors a range of issues important to protect patients and staff from infection. Results are fed back to clinical staff and used to take action at local level so that high standards are maintained.
SLHT Quality Accounts 2012-13 Page 83 of 95
Weekly formal audit of cleanliness standards is performed within the Trust, by a team which includes a Trust monitoring officer, cleaning contractor, patient representative, and members of the nursing and infection prevention teams. These audits are performed on a random sample of areas, with all areas being monitored over a period of time. It is enormously beneficial to have patient representation on these audits, as these volunteers provide a „patients-eye view‟ and an independent check of our process and standards. SLHT is enormously grateful for the support we have received from key members of Local Involvement Networks to support this programme in 2012-13.
As well as routine monitoring of standards, in response to a case of CDI, a rapid audit of standards is performed on the ward to identify any areas that could be improved to reduce the risk of infection to patients. This includes audit of cleanliness and environmental standards as part of the weekly formal monitoring audits.
Each case is investigated via the national „learning through action‟ root cause analysis tool, and the outcome is then scrutinised further for additional learning, with the Medical Director leading Executive Review Panels for cases in any areas of concern.
3.13.9 Patient Safety Incidents
(i) number and rate of incidents reported
No. Of incidents reported = 3,355
Rate = 3.93 per 100 admissions
Compared with data from 39 comparable large acute trusts in England:
Mean no. of incidents reported = 4,060 (SLHT ranked 27 th from 39)
Range = 859 to 6,485
Mean rate = 6.69 (SLHT ranked 36 th from 39)
Rate per 100 Range = 1.99 to 13.61
Rate per 100 admissions
National ranking
2011-12 (Apr - Sept)
5.8
Middle 50% of reporters
2012-13 (Apr - Sept)
3.93
Lowest 25% of reporters
Note: The data for 2011-12 and 2012-13 refers to a 6 month period from April to Sept. The data for the last 6 months of 2012-13 has not yet been published by the NRLS (the National
Learning and Reporting Service)
SLHT considers that this data is as described for the following reasons:
The trust has undergone major organisation changes, with several wards opening and closing during this period
SLHT Quality Accounts 2012-13 Page 84 of 95
Following the Trust‟s move into administration the rate of staff turnover has increased making it more difficult to maintain the level of reporting from the previous year
Variations in reporting by some staff groups
SLHT has taken the following actions to improve the indicator and percentage in
3.2.9 (i), and so the quality of its services, by:
Raising the profile of incident reporting at Care Group governance meetings
Reminding staff to ensure they report not only actual incidents that occur but also those that are near misses
Producing trend and theme reports for care groups, ensuring that lessons learned are fed back into practice
Providing training and support for clinical staff in incident reporting processes
Ensuring that ward managers are identified as the „incident handler‟
Producing a monthly report for ward areas to showing progress and actions for incidents reported by the ward
(ii) % of incidents that resulted in severe harm or death
April 2011 to Sept
2011
April 2012 to Sept
2012
No. of incidents
SLHT rate
National rate
National ranking
34
0.6%
0.7%
23/41
Data from HSCIC for periods 1 st April to 30 th September
37
1.1%
0.7%
36/39
SLHT considers this data is as described for the following reasons
The number of incidents that were uploaded to the national database in the period
April to September 2012 that had been deemed to have resulted in severe harm and or death have been subject to subsequent verification and investigation. This has resulted in a more accurate assessment of the severity of the incidents recorded including, in some cases, a downgrading of the incident. The Trust position, therefore, for this period is that there were 24 patient safety incidents in which severe harm or death occurred (and not 37 as reported by HSCIC).
SLHT Quality Accounts 2012-13 Page 85 of 95
There will, on rare occasions, be occasions where there is either late reporting of an incident or, following further review, the severity is changed even after data may have been uploaded and published nationally.
Some incidents on the Trust risk management system were not uploaded to the
NRLS in the period April to October 2012. These related to patients seen as outpatients and in all cases there were no incidents in this group in which severe harm and or death had resulted.
SLHT intends to take the following actions to improve this indicator, and so the quality of its services, by:
Reminding staff that the severity of the incident should be based on the actual harm that occurred to the patient
Providing training in the grading of incidents
Undertaking a Patient Safety Culture Survey, with the results being used to inform further training requirements
SLHT Quality Accounts 2012-13 Page 86 of 95
3.15 Statements provided from our commissioners, LINks & OSCs .
The Trust is grateful for the considered responses from all our stakeholders. These have been helpful and, where appropriate, have been reflected in the Quality Accounts 2012-13.
Comments from Bexley Clinical Commissioning Group
Thank you for submitting a draft copy of SLHT's 2012/13 Quality Accounts for comments, for inclusion in your stakeholder response section of the report. This was noted and discussed at our internal Quality and Safety working group on the 23rd May 2013. Please see below our comments as requested:
We can confirm that the content of the quality accounts for 2012/13 pertaining to our contractual agreement is accurate and correct, reflecting information that has been reported monthly at our joint clinical quality review group throughout 2012/13.
The quality accounts demonstrate that a great deal of good work has been done while working through a very challenging period for the Trust and for staff. We note that in the past year there has been progress on some of last year's priorities including an overall reduction in the total number of hospital acquired pressure ulcers, and excellent progress on
VTE patient risk assessment and implementation of prophylaxis. SLHT also achieved good performance against the national targets for dementia screening and referral. It is noted that the HSMR continues to be less than the national average.
The CCG commends the Trust on working in partnership with commissioners to address quality issues that have arisen during the year and with regards to the future, we are pleased to note the list of priorities for improvement in the report. Quality of discharge and the emergency care pathway have been areas for discussion in our meetings and it is reassuring to see these included in your measures. In addition, we would like to see the following areas referred to in the quality accounts:
1) Reference to Frances Report
We would like to see a Trust response to the „Frances Report‟ including measures that are being taken to implement recommendations from this report. The CQUIN based on the
Frances recommendations we have put in place for 2013/14 should support you in this and through capturing the learning from incidents.
2) Safeguarding Reporting
We would like to see a reference to SLHT safeguarding reporting as part of the quality accounts as there is no reference in the quality accounts to safeguarding and how well SLHT performs their duties under safeguarding. The safeguarding CQUIN we have put in place for
2013/14 should support you in this.
3) Assurance of Quality through transition
We know transition can be a challenging period and we would like to see included assurance about what measures are in place around workforce and continuity and safety of services.
SLHT Quality Accounts 2012-13 Page 87 of 95
In Summary
We believe that there has been good progress in terms of quality of care and that these gains must be protected in transition and there is on-going improvement and innovation.
We look forward to working with the SLHT team and its successor organisations throughout the 2013/14 CQUIN scheme and transition to any new arrangements. We expect that working together the new provider structures will provide the expected opportunities and shared learning in patient experience, patient safety and clinical effectiveness.
Yours sincerely
Simon Evans-Evans
Director of Governance & Quality
Comments from Bromley Clinical Commissioning Group
Thank you for the opportunity to comment on SLHT's quality account for 2012. Firstly I would like to echo the statement from the Trust Special Administrator in the beginning of the account. There has also been excellent engagement from senior staff throughout what has clearly been a very difficult time for the organisation and for staff personally. There has consistently been a high level of commitment to the quality assurance and improvement agenda along with an openness and willingness to engage from staff.
There is much to commend in the report but, as the Trust itself acknowledges, a number of significant challenges. The CCG notes that there has been improvement since the Trust was formed in a number of areas including a reduction in the incidence of hospital acquired grade 3 and 4 pressure ulcers, a reduction in the number of falls, and a reduction in the number of hospital acquired infections. The CCG supports the continued attention on these areas. A number of areas do however need a continued and renewed focus.
Clinical Quality Review Group
The CCG, in conjunction with other commissioners of services from the Trust (Bexley and
Greenwich CCGs) runs the Clinical Quality Review Group (CQRG) which meets monthly. The
Trust has engaged extremely well with this group providing high level senior clinical input through the Medical and Nurse Directors as well as other senior staff. The Trust has responded to challenges and CGRG has monitored improvement action plans closely over the year.
Quality Improvement targets
The CCG agrees with and supports the areas identified as targets for the coming year. The
CCG agrees there needs to be a level of focus on dementia. This area has been subject to a
CQUIN for two years now and we welcome the fact that the Trust has secured funding for
13/14. There is an opportunity to capitalise on this work.
SLHT Quality Accounts 2012-13 Page 88 of 95
In general we welcome the aspirations within this section in particular the emphasis on implementation of Francis Inquiry into Mid Staffordshire Hospital Report and also the Chief
Nursing Officer„s strategy for “Compassion in Practice”.
The CCG recognises the work that the Trust has carried out on nutrition within the organisation and would like to suggest this continue as a priority quality improvement area particularly in light of the 2012 inpatient survey results.
The CCG believes that Commissioning for Quality and Innovation (CQUIN) should be seen as an integral tool to improving quality within the Trust. There have been some good outcomes achieved through the CQUIN initiative but the CCG believes more emphasis could be put on improving quality through innovation within the organisation.
Audits
The feedback from audit contains quite a few results which show non compliance with standards. A range of measures are planned or are being implemented, but this raises questions about whether these improvements are achievable against a backdrop of change as a result of the TSA recommendations and the improvement priorities identified. We recognise implementation of the range of measures required will pose a challenge for the
Trust in the coming year.
Consideration by Bromley Quality Assurance sub -committee
The draft report has been considered by Bromley‟s‟ Quality Assurance sub-committee. The committee recognised the challenge in delivering the quality improvements for 2013/14 against a backdrop of enormous change for the Trust and personal uncertainty for staff.
The committee will receive the final report and monitor the Trust‟s progress against the targets for 2013/14.
Sonia Colwill
Director of Quality, Governance and Patient Safety
June 2013
Comments from Greenwich Clinical Commissioning Group
1. Background:
The
draft
South London Healthcare NHS Trust (SLHT) Quality Account for 2012/13 and NHS
Greenwich Clinical Commissioning Group‟s response will be reviewed by the NHS Greenwich
Clinical Commissioning Group‟s Quality Committee on 19 TH June 2013.
The coordination of feedback on the quality account has been historically undertaken across Bexley, Bromley and Greenwich CCG‟s Governance Leads, who welcome the opportunity to respond to this document. This is the NHS Greenwich Clinical Commissioning Group response as part of this joint process.
SLHT Quality Accounts 2012-13 Page 89 of 95
NHS Greenwich Clinical Commissioning Group is committed to working closely with South
London Healthcare NHS Trust to ensure the on-going delivery of high quality services. NHS
Greenwich Clinical Commissioning Group has established processes for regularly review of quality issues with SLHT via regular Clinical Quality Review Group Meetings (CQRG) as well as a number of other quality review mechanisms. The Terms of Reference and membership of the CQRG have been drawn up via the Commissioning Support Unit and agreed by all
BBG commissioners.
Commissioners have maintained a good overview of quality through the CQRG and are mindful and sensitive to the difficulties the Trust faces during transition. NHS Greenwich
CCG commends the staff of SLHT who have worked consistently with commissioners, in an open and transparent manner, to resolve quality issues raised. SLHT senior staff have worked closely with commissioners on a number of initiatives. An example of this includes a number of clinician to clinician meetings between SLHT and NHS Greenwich Clinical
Commissioning Group, responding to quality issues raised via the CCG Quality Alert system and SLHT strived to make significant improvement. During 2013, Commissioners have initiated a Pressure Ulcer Working Group, which seeks to share good practice of pressure ulcer management across all providers, attended by adult safeguarding leads, SI managers and commissioners. SLHT have participated positively in this work.
2. Quality Account 2013/14
The opening statement of the Quality Account reflects the environment and transition and the commitment of staff should be commended. Integrating positively with the new clinical commissioning groups has been part of this.
The Quality Account emphasis on priorities for improvement for 2013/14 includes the key emerging themes from the Francis Report in relation to delivering care with compassion and key areas for improvement as outlined by commissioners and the Local Involvement
Networks. SLHT has set in place measures on assessing patient‟s confidence in nurses caring for them and on nurses delivering care with compassion and empathy, taking into consideration results from the National Inpatient Survey 2012. SLHT are building on the work they have done in relation to Care of Patients with Dementia and are improving their performance on the national CQUIN with resources secured to sustain improvements throughout 2013/14.
SLHT has clearly outlined priorities for 2012/13. Issues arising, where performance targets were not met, have been addressed in the quality improvement goals. There is evidence that CQUINs have being used as an enabler to better achievement and this has been specified.
3. Clinical Audit, Research and National Confidential Enquiries
Participation in National Audits is clearly illustrated with SLHT participating in 92% of national clinical audits that it was eligible to participate in. The Quality Account illustrates improvements in care as a result of audit undertaken in the following areas: Fever in
SLHT Quality Accounts 2012-13 Page 90 of 95
children, renal colic, fractured neck of femur, COPD, diabetes, stroke (placing PRU in the top
25% of Trusts nationally), angioplasty cardiac rhythm, paediatric asthma, hip fracture, neonatal care, cancer, heart failure, and myocardial Ischaemia. 33 local clinical audits were undertaken and SLHT participated in national confidential enquiries on bariatric surgery, cardiac arrest procedures, alcohol related liver disease and subarachnoid haemorrhage. The
Quality Account illustrates that during the year SLHT was involved in 164 clinical research studies in 21 specialities and the CQUIN schemes agreed with commissioners for 2012/13.
NHS Greenwich Clinical Commissioning Group acknowledges that there have been no CQC enforcement actions during 2012/13 .
4. Areas of notable good practice are outlined:
Overall reduction in the total number of Hospital Acquired Pressure Ulcers (HAPUs).
Excellent progress on VTE patient risk assessment and implementation of prophylaxis.
Achievement of national targets for Dementia screening and referral.
Continued work on falls prevention.
3. Quality Improvement priorities for 2013/14 have been reviewed and agreed to be:
Key emerging themes from the Francis Report in relation to delivering care with compassion.
Working on the results from National Inpatient Survey
Key areas for improvement as outlined by commissioners and LINKs
Implementation of the Friends and Family test
Care of patients with dementia
Emergency Care Pathway
Quality of discharge
Venous Thromboembolism
Continued focus on
Clostridium difficile
Infections
Prevention of pressure ulcers
Nicola Havutcu – Director of Governance & Quality
Maggie Aiken – Associate Director of Governance & Quality
NHS Greenwich Clinical Commissioning Group
June 2013
Comments from Royal Borough of Greenwich: Healthier Communities and Older
People Scrutiny Panel
Introduction
The future of the Trust has been a major focus of the Panel‟s 2012/13 work programme; the first Trust Special Administrator (TSA) presented his report and draft recommendations to the Panel in November 2012 and the Council‟s response to the TSA‟s consultation was
SLHT Quality Accounts 2012-13 Page 91 of 95
discussed at its meeting in December 2012. The implications of the dissolution of the Trust will form an important part of the Panel‟s 2013/14 work programme.
The Panel recognises the importance of high quality hospital services to the continued health and wellbeing of local residents and is determined to undertake its role in ensuring that quality services are provided by the successor Trusts.
Detailed comments on Quality Accounts
Part 1: Statements on Quality from Trust Special Administrator
The Panel recognises the challenges involved for Trust staff during this transition period and notes that the recommendations of the Francis Report will be taken into account as the new organisations are created.
Part 2: Looking forward - Priorities for Quality Improvement 2013-14
The Panel notes the Trust‟s eight priorities for improvement which cover important service areas and correspond with themes in its work programme for 2013/14,for example, the
Francis Report‟s focus on providing care with compassion. Also understanding patients‟ experiences of the care they have received; emergency care and control of infection.
The Panel supports the Trust‟s prioritisation of emergency care during 2013/14 because it is concerned about the increase in attendance at both hospital A&E departments and the higher level of acuity in those attending. The Panel shares the Trust‟s concern regarding its performance against the 4 hour wait target and recognises that this is influenced by issues relating to the wider health economy.
Part 3: Looking back - Review of 2012/13
The Trust‟s review of its performance against its 2012/13 priorities for improvement, showed many instances where it met its objectives and some areas where there is room for improvement.
3.1 Review of 2012/13 Priorities for Improvement
3.1.1 Patient experience
It was noted that the 2012 National Inpatient Survey indicated that there was still a need to improve the quality of food for patients and the Panel will monitor the Trust‟s Catering
Strategy to assess whether the patient meal service improves. Another area that the survey indicates needs to improve is patients finding a member of staff to talk to about their worries and fears. The Panel will monitor the effectiveness of the „comfort rounds‟ of the wards designed to ensure that every patient is reviewed on at least a two hourly basis and that they are supported with any care that is needed immediately.
3.2 Mortality
The Panel recognised that although the Hospital Standardised Mortality Ratio had worsened
(2011/12 87.3, 2012/13 95.2) it still indicated fewer deaths than expected. Mortality rates is
SLHT Quality Accounts 2012-13 Page 92 of 95
an area that the Panel will focus on in its 2013/14 work programme and will wish to see improvements in the SLHT successor Trusts.
3.3 Safety Thermometer
The Panel noted that the data on the „four harms‟ covered by the safety thermometer tool: falls management; pressure ulcers; catheter and Urinary Tract Infection and Venous
Thromboembolism showered generally good performance and clear plans for improvement in those areas where services needed to improve.
3.7 Participation in Clinical Audits
The Panel noted the reports of the 14 national clinical audits that the Trust had participated in during 2012/13. The reports identified areas of good practice and a number of important lessons that had been learnt and the Panel supports the resulting service improvements that have been implemented.
For example, there has been good performance in stroke services and dealing with hip fractures and the need for improvement in providing prompt pain relief in instances of renal colic and fractured neck of the femur. However, there needs to be an improvement in the number of patients with gallstone pancreatitis who have their gall bladder removed within two weeks of their discharge from hospital. The Panel wishes to reiterate the importance of the service improvements being fully embedded into SLHT successor Trusts.
3.11 What others say about the Trust
Statements from the Care Quality Commission (CQC)
The Panel was pleased to note that following CQC unannounced inspection visits the Trust was deemed to be compliant with most outcome measures and when not compliant had undertaken immediate action to address the issue.
Joint Comments from Bexley, Bromley and Greenwich Healthwatch Organisations
The Healthwatch organisations for Bexley, Bromley and Greenwich welcome the opportunity to comment on the SLHT Quality Account for 2012-13. Please note that Healthwatch was established on 1st April 2013, replacing Local Involvement Networks (LINks). Recognising that Healthwatch is in its embryonic stage, we are unable to provide as detailed a commentary as LINks have provided in previous years. We look forward to compiling a full a thorough commentary next year.
We have compiled a joint response to the Quality Account this year using feedback from all three LINks/ Healthwatchs.
We recognise the difficult circumstances that the Trust has been placed under during 2011-
13 due to Unsustainable Provider Regime and the process of dissolving the Trust.
We welcomed the opportunity to be involved in the setting of the priorities and were pleased to contribute highlighting what we feel accurately reflects the issues that matter to
SLHT Quality Accounts 2012-13 Page 93 of 95
patients. We look forward to working with the Trust and incoming providers in the coming year to achieve significant progress on the priorities identified.
Patient experience – Nurses delivering care with compassion and empathy
We congratulate the Trust for recognising the importance of this in light of the Francis report and the results following the National Inpatient Survey in 2012. All three LINks had received public feedback highlighting their concern on this matter and so are pleased it has been set as a priority.
Care of patients with dementia
Recognising that Bromley and Bexley have two of the highest ageing populations across the
London boroughs, the need for and importance of dementia screening and adhering to the complete dementia care pathway is vital. Following from our comments last year regarding the LINks‟ concerns about the lack of communication with carers, we are pleased to see quarterly surveys of carers‟ experience will be conducted.
Emergency Care Pathway & Quality of Discharge and Information.
We note that the Trust will be working more closely with commissioners and social care partners and look forward to our involvement in the design and implement of the action plan for both these priorities.
Prevention of VTE, CDI and Pressure Ulcers
We remained concerned with the number of VTE, CDI and Pressure Ulcers reported by the
Trust despite it being a Quality Account priority year and year.
We look forward to continue working in partnership with the Trust and incoming providers to help deliver the best possible patient experience and health outcomes across the boroughs.
Comments from Age UK Bromley and Greenwich
This is a comprehensive document with recommendations for maintenance of good care and improvements where needed. I am however not entirely sure for whom this report is intended. It would be of value for other health disciplines - CCG's, Public Health, Community
Services. However if it is intended for charitable organisations and the general public I am concerned that the language is not really directed at such an audience. I recognise that a lot of work went into to producing this and I would hope that it was accessible to as many interested parties as possible.
Lynda Stimson
Vice Chair Age UK Bromley and Greenwich
SLHT Quality Accounts 2012-13 Page 94 of 95