Quality Account 2012-13 Quality care, closer to you…
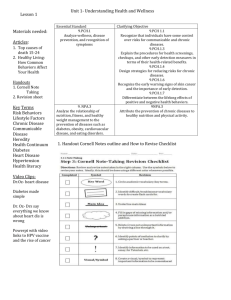
advertisement
Quality Account 2012-13 Quality care, closer to you… Chief Executive’s statement On behalf of Peninsula Community Health (PCH), I welcome the opportunity to present our annual Quality Account to demonstrate our continued commitment to delivering high quality patient care. Whilst there has been much publicity about the quality of care provided to some patients in hospitals in England and Wales over the last year, I am always pleased to receive excellent feedback from our patients and their relatives across both the community and hospital services we deliver. This demonstrates to me that we strive to ensure our patients receive high standards of clinical care, delivered by caring, compassionate staff. We believe and commit to Putting the Patient First by making patient safety and experience our number one priority every day, in other words Quality care closer to you. Despite the continued, challenging economic climate during 2012-2013, we are steadfast in our commitment to maintaining quality, and ensuring our frontline teams are able to undertake their roles as our community expects. We have been working closely with other health and social care partners in Cornwall and the Isles of Scilly, to enable responsive and personalised care to our patients. Some of this work is still in the early stages of change and we are committed to making this work for our patients. In May 2013, PCH Dental Ltd was formed. This company is part of the PCH family and contains all of the dental services we are commissioned to provide. The formation of this company will allow its Board to have a truly focused attention on improving and expanding the services provided. I am pleased that PCH has gained funding for an innovative project called ‘Kinda Magic’. Kinda Magic was one of nine projects chosen from over 100 that entered the Patient Feedback Challenge, which was supported by the Institute for Innovation and Change and the Department of Health in July 2012. The innovative project was to spread PCH’s current good practice in gathering patient feedback and to share the process which was viewed as excellent because it provided metrics at an organisational level as well as providing immediate feedback at ward level. The second part of the project is to develop tools that will enable vulnerable groups of the community, who are currently excluded, to provide feedback. This will include people with cognitive or communication difficulties including people with Dementia. PCH has worked across England with a number of organisations to progress this project and our spread has been wide. This project has attracted both national and local attention, and PCH’s aim is to present and share our tools at an event in October 2013. The Quality Account indicates our priorities for the future and demonstrates and reviews our performance over the past year. This Quality Account allows us to evidence our commitment to continuous, evidence-based quality improvement, to draw your attention to the standards achieved, and the progress we have made, and the approach we intend to continue. It enables you the opportunity to assess the quality of our performance across the healthcare services we offer. Page 2 of 60 I am very pleased that we have been able to improve our services across the communities we serve in 2012/13. The areas of particular achievement include: 69% reduction in the incidence of clostridium difficile No cases of MRSA bacteraemia Nil breeches in Mixed-sex Accommodation Upgrade of x-ray facilities in St Mary’s Hospital, Isles of Scilly Co-location of health and social care staff at St Mary’s Hospital, Isles of Scilly Continued high performance in risk assessing and providing preventative treatment for venous thrombo-emboli Continued high performance in medicines reconciliation across all community hospitals Care of the Deteriorating Patient Implementation of Early Intervention Service in Cornwall Reducing harm from falls Introducing Acute Care at Home across Cornwall Expansion on delivering Nursing and Patient Experience Metrics Maintaining Essential Standards for Registration with the Care Quality Commission Expansion of specialist respiratory services in North and East Cornwall The areas we have chosen as our quality improvement targets for 2013-2014 have once again been set following consultation with the local health scrutiny committees, local involvement networks, our commissioners and importantly, by talking to staff, patients and carers. Progress described within this document is based on data and evidence collected locally and nationally, much of which is presented as part of our performance framework each month and in our public board meetings and to our commissioners. To the best of my knowledge the information given in this document is accurate. Helen Newson Interim Chief Executive Page 3 of 60 1.0 Priorities for Improvement .......................................................................................... 5 2.0 Statements of Assurance from the Board of Directors .......................................... 12 2.1 Care Quality Commission ...................................................................................... 12 2.2 Research ................................................................................................................. 12 2.3 Audit participation.................................................................................................. 13 2.4 Goals agreed with commissioners ....................................................................... 18 2.5 Data Quality ............................................................................................................ 19 2.6 Information Governance ........................................................................................ 20 2.7 Clinical Coding Error Rate ..................................................................................... 20 3.0 Review of our Quality and Safety Performance 2012/13 ........................................ 22 3.1 Performance Review – The priorities we identified in 2012/13 ........................... 22 3.1.1 Nutrition ............................................................................................................ 22 3.1.2 Documentation................................................................................................. 22 3.1.3 Dentistry ........................................................................................................... 23 3.1.4 Dementia Care.................................................................................................. 23 3.1.5 Complaints ....................................................................................................... 25 3.2 Maintaining Essential Standards for Registration with the Care Quality Commission .................................................................................................................. 26 3.3 NHSLA Assessment ............................................................................................... 26 3.4 The East Cornwall Integrated Respiratory Team ................................................. 26 3.5 Parkinsons Disease Service .............................................................................. 31 3.6 Safety Thermometer ........................................................................................... 31 3.7 Blood Transfusion Management ....................................................................... 36 3.8 Safeguarding Adults ........................................................................................... 37 3.9 Nursing Metrics and Patient Experience Measurement during 2012/13 ........ 39 3.10 Eliminating Mixed Sex Accommodation (ESMA) .......................................... 45 3.11 Complaints and Compliments ........................................................................ 45 3.12 Focus on the Isles of Scilly ............................................................................ 51 3.13 PEATs ............................................................................................................... 53 4.0 Response to this report from our stakeholders ...................................................... 54 4.1 Cornwall Overview and Scrutiny Committee ....................................................... 54 4.2 Isles of Scilly Overview and Scrutiny Committee ............................................ 54 4.3 Kernow Clinical Commissioning Group ........................................................... 54 5.0 Glossary .................................................................................................................... 56 6.0 Statement of Directors Responsibilities in Respect of the Quality Account ....... 60 Page 4 of 60 1.0 Priorities for Improvement How we identify our quality improvement priorities Our quality monitoring systems continue to capture information throughout the year, about the quality of services we provide and the risks to service users. We continually monitor the experiences of patients and how we perform against the range of national and local standards. We strongly believe in the importance of establishing meaningful dialogue with patients, patients’ representatives and carers, to help us develop our quality improvement plans for the coming year. In March 2013, the potential priorities for inclusion in the Quality Account were circulated to the following bodies asking their opinion as to the level of priority of each subject: Overview and Scrutiny Committees for both Isles of Scilly and Cornwall Healthwatch IOS Healthwatch Cornwall Royal Cornwall Hospital Plymouth Hospitals NHS Trust Cornwall Partnership Foundation Trust Peninsula Community Health staff PCH Non Executive Directors NHS Cornwall and Isles of Scilly (now Kernow Clinical Commissioning Group) Cornwall League of Friends PCH, in collaboration with the above groups has established five quality improvement priorities for 2013/14. We have organised them into three domains, consistent with the core domains for quality patient care identified by Lord Darzi in the ‘NHS Next stage Review: High Quality Care for All’. They reflect what we believe are the priority areas for achieving the best possible outcomes for those we serve: Patient safety Clinical effectiveness Patient experience These quality improvement priorities are detailed on the following pages and include the development of work that is already underway as well as new work that we consider to be equally important. Page 5 of 60 Domain Priority Source Prevention and Management of Pressure Ulcers – Pressure ulcers are both extremely painful and debilitating. This topic aims to explore a new methodology for investigation of pressure ulcers to enable learning from experience and reduction in numbers of new pressure ulcers. Learning from Complaints Dementia – We want to raise the standards of knowledge and skills in staff being able to proactively deal with patients that become acutely distressed and confused on our wards. We aim to provide education to enable staff to increase their skills and feel confident in the way they manage and de-escalate situations. National Policy Patient Safety National Policy Feedback from Care Quality Commission visits Serious untoward incident learning Learning from complaints Safeguarding and serious incident learning South West Dementia Strategy Learning from Complaints Discharge Planning. Aim to improve effective discharge planning to reduce National Policy length of stay and to ensure patients and Feedback from CQC visits carers are informed and involved in all stages of the process, leading to reduction in readmission rates. Clinical Effectiveness National Policy To safeguard and meet the needs of patients with severe cognitive impairment CQC National Reports we need to improve the way our staff assess and record Mental Capacity and determination of Best Interest. To ensure that they respect the patient’s choice/wishes, they are using and reviewing the process appropriately, that they fully understand what it is for, and that this is communicated appropriately with families Learning from Complaints Patient Experience Implementation Practice (6C’s) of Compassion in National Policy Francis Report Page 6 of 60 Patient Safety Priority 1 Reduction in Pressure ulcers Pressure ulcers are areas of localised damage to the skin and underlying tissue caused by pressure, shear or friction, or a combination of these. Many hospital acquired pressure ulcers can be avoided. What are we going to do: To reduce health care acquired pressure ulcers How much: 25% reduction in hospital acquired pressure ulcers across all clinical areas By When: March 2014 Board Sponsor: Trish Cooper Acting Director of Nursing and Professional Practice Implementation/Programme Lead: Nicci Kimpton Tissue Viability Lead Nurse How are we going to do it: Community District Nursing Teams are working with the Tissue Viability Team to collect reliable data on pressure ulcer figures Intentional Rounding has been spread across the organisation. This means that where required, patients receive regular turns so that they are not lying in the same place for too long. The intentional rounding document will be reviewed to ensure all components of the SKIN Bundle are included. This is a proven method of reducing pressure ulcers and ensures that the following are reviewed regularly: I. Surface - for example, is the patient on the right mattress? II. Skin - is the patient’s skin intact, are there any red areas? III. Keep Moving - does the patient require turning? IV. Incontinence Management - does the patient require help with toileting needs? V. Nutritional Management - is the patient hydrated? We aim to completely eliminate all preventable grade 3 and 4 hospital acquired pressure ulcers To work collaboratively with commissioners, nursing and residential homes and other health and social care providers to identify areas where improved communication and training can aide prevention Priority 2 Dementia care Dementia currently affects 800,000 people in the UK which is expected to rise to over a million people by 2021. What are we going to do: We want to raise the standards of knowledge and skills in staff being able to proactively deal with patients that become acutely distressed and confused Page 7 of 60 on our wards. We aim to provide education to enable staff to increase their skills and feel confident in the way they manage and de-escalate situations How much: 100% of appropriate staff to receive dementia training and every clinical area to have a Dementia Care Champion By When: March 2014 Board Sponsor: Trish Cooper Acting Director of Nursing and Professional Practice Implementation/Programme Lead: Sue Greenwood Dementia Lead How are we going to do it: Having board level commitment to continue to work towards becoming Dementia Friendly Dementia Lead within the organisation Network of Dementia Ward Champions Continue to implement Dementia Care Mapping across the organisation Commitment from the board to review the environment within our community hospitals Continue to promote dementia friendly approaches in our communications Share our plans and progress collaboratively Use local and national networks Produce a Dementia page on our organisation’s website Introduce a communication passport that has been developed locally by another provider Continue to promote “This is me” Continue to work in partnership across the pathway with all providers and volunteering organisations Launch activity of the Dementia Care Action Plan and promote the plan during Dementia Awareness week Introduce volunteers and a befriending service within our organisation Continue to build partnerships and work closely with local voluntary services Working in partnership with all other providers ensure that we promote safety and early discharge with improved personal and community support Working in partnership with all other providers and voluntary organisations ensure that people are not inappropriately admitted and are supported to return home as quickly as possible Promote early diagnosis of dementia by working in partnership with our acute services Continue to improve the way we assess and plan care involving the person with dementia, their relatives and carers Working in partnership with our acute providers ensure that we work together to agree a screening tool that is used consistently across the pathway Continue to work in partnership with the Alzheimer’s society to develop information for clinical areas regarding services available in the community Continue to promote the completion of Dementia Awareness workbooks across the organisation Page 8 of 60 Develop and roll out a training program that sets out to reduce distress amongst our patients with dementia, equipping staff with the knowledge skills and understanding Improve the physical environment within our community hospitals and clinics Carry out a focused piece of work to review and improve our signage across all locations where services are provided Introduce purposeful occupation in at least 6 of our community hospitals Clinical Effectiveness Priority 3 Discharge Planning Effective discharge planning leads to better outcomes for patients and reduces the need for readmission and emergency care. Discharge planning should commence from the very first day of admission and should include collaboration and seamless services from health and social care. What are we going to do: Aim to improve effective discharge planning to reduce length of stay and to ensure patients and carers are informed and involved in all stages of the process, leading to reduction in readmission rates How much: To reduce length of stay in community hospitals to an average of 23 days. By When: March 2014 Board Sponsor: Helen Newson, Interim Chief Executive Implementation/Programme Lead: Nicky Harvey Intermediate Care and EIS Lead How are we going to do it: Baseline review of discharges within the last 6 months, identifying when the patient was ready for discharge and why, if any there was a delay Utilise the learning from this review to identify priority action areas Development of Unscheduled Care Strategic and Operational Groups to lead this work Enhanced training for staff Patient experience metrics to be completed, asking the patients and their carers if they were involved in their discharge planning Priority 4 Safeguarding the needs of vulnerable adults What are we going to do: To safeguard and meet the needs of patients with severe cognitive impairment we need to improve the way our staff assess and record Mental Capacity and determination of Best Interest. To ensure that they respect the patient’s Page 9 of 60 choice/wishes, they are using and reviewing the process appropriately, that they fully understand what it is for, and that this is communicated appropriately with families How much: To ensure that 100% of appropriate staff have received training and are competency assessed By When: March 2014 Board Sponsor: Trish Cooper, Acting Director of Nursing and Professional Practice Implementation/Programme Lead: Jan Summers-Deane Acting Safeguarding Adults Lead How are we going to do it: To monitor and investigate all safeguarding alerts raised, to ensure the best interest of the patients have been met To review the Whistleblowing Policy to ensure it is fit for purpose Patient experience metrics to be completed Patient Experience Priority 5 Compassion in Practice Compassion in Practice is the new three year vision and strategy for nursing, midwifery and care staff drawn up by Jane Cummings, the Chief Nursing Officer for England (CNO) at the NHS Commissioning Board, and Viv Bennett, Director of Nursing at the Department of Health. It was launched at the CNO annual conference in Manchester on December 4th 2012 following an eight week consultation with over 9,000 nurses, midwives, care staff and patients. The vision was underpinned by six fundamental values: care, compassion, competence, communication, courage and commitment - with six areas of action to support professionals and care staff to deliver this excellent care. In particular, the vision identifies that we all need to work together to ensure we meet the needs of older people – the largest group of people who use services - and treat them with the dignity and respect that they deserve in joined up health, care and support services. What are we going to do and how much: Implement all six areas By When: March 2014 Board Sponsor: Trish Cooper, Acting Director of Nursing and Professional Practice Implementation/Programme Lead: Alison Rundle Patient Safety Facilitator How are we going to do it: Implement the actions as shown in the chart overleaf Page 10 of 60 Page 11 of 60 2.0 Statements of Assurance from the Board of Directors This section contains statutory statements concerning the quality of services provided by PCH. These are common to all NHS provider organisations’ Quality Accounts and can be used to compare us with other organisations. During 2012/13 PCH provided and/or sub-contracted 36 NHS services. The income generated by the NHS services reviewed in 2012/13 represents 100% of the total income generated from the provision of NHS services by PCH for 2012/13. PCH works from over 100 locations throughout Cornwall and the Isles of Scilly including 14 community hospitals. PCH reviews all the data in regard to these services monthly. Since May 2013, PCH has a subsidiary company – PCH Dental Ltd, providing NHS Commissioned dental services throughout Cornwall and Isles of Scilly. 2.1 Care Quality Commission In 2012/13, PCH continued to be registered with the CQC to provide regulated activities at 19 locations. Post May 1st 2013 and the formation of PCH Dental Limited, this has reduced to 16 locations. From September 2012 – end of March 2013, the Care Quality Commission visited 18 PCH registered locations, as part of their scheduled inspections programme. All of these visits were unannounced and were not as a result of any concerns raised. Overall, the visits went well and the feedback was very positive. For example, both in the final reports and at verbal feedback, the inspectors described observing care which respected the dignity of patients, patients very satisfied with the care they were receiving and staff appeared knowledgeable and able to implement policies to ensure the safety of patients, such as safeguarding. The final reports show non-compliance in Outcome 14 (Regulation 23) at 3 locations and Outcome 13 (Regulation 22) at one location. The non-compliance relates to clinical supervision and training, and action plans have been created in order to rectify those issues. 2.2 Research In 2012/13 PCH continues to be a research partner working closely with the research team, which is based within the local acute organisation. PCH is informed, and approval sought, for any research taking place within, or near to the services we provide. Page 12 of 60 2.3 Audit participation Clinical Audit Clinical audit is a systematic process of improving the quality of patient care by looking closely at current practice, evaluating the quality of care provided to patients based on best practice and nationally set clinical standards, modifying it where necessary and evaluating the outcome. The main aim of clinical audit is to provide assurances that the clinical services are meeting the needs of service users and at the same time providing internal assurance that staff are following best practice based on research evidence. PCH is committed to improve the quality and outcomes of patient care by establishing a culture where high quality clinical audit can be sustained. The 2012-13 Audit Plan incorporated a programme of over 40 clinical audits in addition to a record keeping audit of all services in addition to any national clinical audits which the organisation was eligible to participate in. National Clinical Audit Participation Although it is not mandatory for community services to undertake national clinical audits it is good practice. During the period April 2012 to March 2013, four national clinical audits and zero national confidential enquiries were relevant to NHS services that PCH provides. During that period, PCH participated in 50% of the national clinical audits and 100% (zero eligible and therefore zero participated in) national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that PCH was eligible to participate in during 2012-13 are as follows: Parkinson’s occupational therapy audit Parkinson’s physiotherapy audit Parkinson’s speech & language therapy audit National Audit of Intermediate Care PCH took part in the physiotherapy and occupational therapy elements of the Parkinson’s audit in 2011-12. Parkinson’s UK advice is “The National Parkinson's Audit takes place every year, but we recommend that services take part every other year to give time for them to respond to the findings”. In light of this advice in 2012-13 PCH did not take part in the physiotherapy and occupational therapy having taken part in 2011-12. Having not taken part in the Page 13 of 60 Speech & Language Therapy Parkinson’s audit in 2011-12, Peninsula Community Health took part in this in 2012-13. The national clinical audits and national confidential enquiries that PCH participated in during 2012-13 are therefore as follows: Parkinson’s speech & language therapy audit Intermediate Care Audit The national clinical audits and national confidential enquiries that PCH participated in, and for which data collection was completed during 2012-13 are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. Parkinson’s speech & language therapy audit Intermediate Care Number of cases submitted Number of cases submitted as a percentage of eligible cases 20 100% 10 100% Improving services through participation in national audits The reports of 1 national clinical audit (report not received yet for Parkinson’s speech & language therapy audit) were reviewed by PCH in the period April 2012 to March 2013 and PCH intends to take or has taken the following actions to improve the quality of healthcare provided National Audit Parkinson’s Physiotherapy Audit (undertaken in 2011 but due to delay in national report action plan developed in 2012) Actions planned/taken Primary Clinicians involved in Therapy and Nursing now have access to published evidence in journals, measures and Pilot group information as an educational resource posted in the Parkinson’s shared drive Parkinson’s Nurse letters referring to physiotherapy are to have date of Parkinson’s diagnosis and information on known previous physiotherapy access Community Physiotherapists have been informed of the common outcome measures and Parkinson’s quick reference cards. These are kept as a resource on the shared drive Band 6 Physiotherapists are offered opportunities for developing skills and competency in PD management and service forward planning e.g. delivering pilot Enhancement of aerobic capacity in Parkinson’s has been identified as a component for management in the Parkinson’s population. This is included in the group exercise in the pilot. Feedback on treatment that targets aerobic capacity is now Page 14 of 60 reported in discharge summaries to referring clinicians to raise awareness of the wider physiotherapist’s role Education of Physiotherapists on the key findings in the audit was fed back to the Community physiotherapy teams through in-service education on Parkinson’s, Team Lead meetings and the Professional forum Intermediate Care Data collected and submitted. Awaiting report Parkinson’s speech & language therapy audit Data collected and submitted. Awaiting report from Parkinson’s UK before formulating action plan Local Audit Clinical audit is supported by the Governance team. All local clinical audits are reported to and monitored by the Clinical Quality and Safety Committee. Reports are reviewed and action plans for quality improvement are monitored by this committee. The reports of 10 local clinical audits were reviewed in the period April 2012 to March 2013 and PCH intends to take or has taken the following actions to improve the quality of healthcare provided. Local Audit Actions planned/taken Record keeping audit A comprehensive record keeping audit was undertaken of all services. Of the 23 standards audited, 18 had improved from the previous year’s audit results. Specific areas for improvement were identified for each service and are the subject of individual service action plans to be communicated via service team meetings. A re-audit in the next 12 months will monitor the effectiveness of the action plans in maintaining and improving record keeping quality Discharge Audit – Medicines Management The 2012 audit showed an increased number of patients at discharge who were provided with a Medicines Reminder Chart to support compliance with medication since 2011 audit A Compliance Aids Assessment tool has been introduced to support staff in identifying patients who would benefit from blister packs and to avoid issuing blister packs if unnecessary Antibiotic Audit Following the 2012 Audit, a focus was placed on reducing the risks of Clostridium Difficile through reductions in the use of inappropriate antibiotic prescribing and promoting the use Page 15 of 60 Clinical Prescribing Audit Missed Doses Audit of local guidelines Updated antibiotic guidelines have led to a significant decrease (40%) in the use of co-amoxiclav in PCH hospitals A number of concerns regarding the sustainability and robustness of safe prescribing, and documentation of administration, were noted in this audit of the community hospital drug chart As a result a new drug chart has been developed to address the issues identified in the audit. The chart allows clear documentation Pharmaceutical Advisers will be delivering staff training on the new drug chart across the county Prescribers, nursing staff and other healthcare professionals have had opportunities to contribute to the contents of the drug chart, to ensure it meets professional requirements to support patient safety This audit highlighted the problem of nursing staff failing to document administration of medication accurately. It was often difficult to ascertain if a dose had been missed or if administration had not been documented. As a result the following action has been taken: When developing the new drug chart, action was taken to ensure it fully supported documentation of drug administration and missed doses (increased space for ‘when required’ medicines and improved layout for documenting accurately on each day the drug chart is in use) Controlled Drugs Audit Action taken to introduce clear plastic bags for storage of patients medications in controlled drugs cupboards, to allow easy identification due to the patient name and drug name being clearly visible Parkinson’s Patient Experience Audit Following the audit, a pathway for acute deterioration in Parkinson’s disease symptoms has been developed for primary/secondary care use PCH has engaged with pharmacists to improve medication management of Parkinson’s patients within both PCH and the Royal Cornwall Hospitals Trust (Acute service provider) Educational programmes have been put in place for Royal Cornwall Hospital Trust and other health organisations staff Allow a Natural Death documentation Audit Process put in place to ensure patients transferring into a PCH community hospital have their existing AND forms reviewed within 72 hours Page 16 of 60 Resuscitation Equipment Audit Following the audit there has been an improvement in the documentation of review dates and patient capacity In the 2012 audit, 21 out of the 28 resuscitation trolleys had improved compared to the 2011 audit in terms of adequate and appropriate levels of emergency equipment being available The need to ensure that all trolleys are kept sealed and required daily and weekly checks undertaken has been reinforced Guidance to be produced for staff on the process for recording all cardiac arrests on DATIX to replace the previous paper recording form Safeguarding Adults & Children Staff Awareness Audit Action plan put in place to increase safeguarding training compliance amongst all staff Campaign to be put in place to raise staff awareness of the appropriate training required for their specific job role Safeguarding Information leaflet circulated to all areas and teams Re-audit planned after 6 months to measure improvement Page 17 of 60 2.4 Goals agreed with commissioners CQUIN – A proportion of Peninsula Community Health income in 2012/13 was conditional on achieving quality improvement and innovation goals agreed between Peninsula Community Health and our commissioners NHS Cornwall & Isles of Scilly. The 2012/13 CQUINs performance are awaiting final approval. National: Venous-thromboembolism To reduce avoidable death, disability and chronic ill health from Venous-thromboembolism (VTE) National: Patient Experience To improve patient experience in 3 areas identified as requiring improvement in community hospitals through the patient experience metrics 3 National: Dementia Improve awareness and diagnosis of dementia, using risk assessment, in a community hospital setting 4 National: Safety Thermometer Improve collection of data in relation to pressure ulcers, falls, urinary tract infections in those with a catheter and venous-thrombo emboli. 5 Local: Reduction in avoidable emergency admissions To reduce avoidable emergency admissions of frail elderly patients 6 Improve the care of patients with long term conditions Increase telehealth across Cornwall 7 Support Plymouth’s ‘Shifting settings of Care Programme’ To reduce the length of stay at Liskeard Hospital 8 Support Plymouth’s ‘Shifting settings of Care Programme’ To increase Chronic obstructive pulmonary disease rehabilitation in line with the National Institute of Clinical Excellence 9 Improve patients’ outcomes To Improve outcomes for 2 specific conditions 1 2 Page 18 of 60 The CQUINs for 2013/14 have been agreed with Kernow Clinical Commissioning Group and they are: 1 National: Safety Thermometer Improve awareness and diagnosis of dementia, using risk assessment, in a community hospital setting 2 National: Patient Experience Implementation of Friends and Family Test 3 Whole System CQUIN - Unscheduled Care Whole System Multi-agency integrated unscheduled care plan 4 Local: Innovation Increase flow and volume through PCH CIC community beds. 5 Local: Hospital Discharge Improve Internal Hospital Discharge Process 2.5 Data Quality Good data quality is an indicator that an organisation has robust systems and methods for capturing accurate information about their patients. PCH submitted records during April 2012 – March 2013 to the Secondary User Service (SUS) for inclusion in the Hospital Episode Statistics which are included in the latest published data. These are one of the measurements that the Care Quality Commission use to monitor our on-going compliance. As per the SUS Data Quality Dashboard April 2012- March 2013: NHS number compliance Inpatient = 99.9% Outpatient = 99.9% Minor Injury Units = 95.8% GP Practice compliance: Inpatient = 100% Outpatient = 100% Minor Injury Unit = 98.1% There is a late data entry issue which is being monitored monthly with performance reviews and local action plans have been initiated. We anticipate that with the introduction of a new clinical IT solution it will significantly reduce any data entry delays as the system will be used real-time. Page 19 of 60 2.6 Information Governance PCH has declared compliance with Level 3 of the Information Governance Toolkit for 2012/13. 2.7 Clinical Coding Error Rate PCH was not subject to a Payment by Results clinical coding audit during 2012/13. Page 20 of 60 Review of our performance in 2012/13 Summary PCH employs 2098 people 734,725 patients were seen by services provided by PCH Physiotherapists carried out a total of 90,542 outpatient appointments There have been 3,867 inpatients in our 14 Community Hospitals in 2012/13 Community nurses undertook 292,435 patient visits 93,588 patients were seen in our Minor Injury Units 40,919 appointments were undertaken by Peninsula Community Health's Dentists Page 21 of 60 3.0 Review of our Quality and Safety Performance 2012/13 3.1 Performance Review – The priorities we identified in 2012/13 3.1.1 Nutrition Improving the nutrition of patients in hospital – nutrition is a high priority across healthcare and is an area that the Care Quality Commission has highlighted as falling below standard and below public expectations nationally. PCH has a very successful Nutrition Group. Within 2012/13, the priority of this group was to identify ways in which to enhance the nutrition of patients within our community hospitals. Meal-times are a priority within all our community hospitals and throughout 2012/13 we have seen an increase in patient satisfaction with not only the quality of food, but also presentation and how much help patients receive. We now offer cooked breakfasts in all hospitals and these have been received very well. Alerts through the ‘Red Tray Initiative’, to ensure staff are aware and assist patients as required with their meals, is now standard throughout all the hospitals. 3.1.2 Documentation Improving clinical documentation – during 2011 a great deal of work was undertaken to redesign and improve the inpatient documentation. To further this work, all other clinical documentation across our community services require review – to ensure patients are informed and consent to plans of care. An area of particular concentration will be in regard to patients discharges from hospital, ensuring that patients remain fully informed and consentual to the discharge plan – this has been added following the consultation. PCH has implemented new and improved documentation throughout the County. The changes have been commended by the Care Quality Commission. Time was taken to ensure that the documentation fit the purpose with small tests of change and comments from staff considered. Patient safety has been a consideration throughout the development of the documentation. CMews (early warning score), a Falls assessment, Frailty score and Pressure ulcer skin bundles recommended by the NHS Southwest Patient Safety Initiative are all included and with the risk assessments, are audited monthly via the Nursing Metrics. The Nursing Metrics scores have improved in all sections since implementation of the new documentation. A training powerpoint was produced and is stored on the ward shared drives for all staff to have unlimited access. This reminds staff of the NMC standards for documentation. For areas where problems have been identified early, face to face training in the use of the documentation has been offered. Care has been taken on the appearance of the documentation so it is now recognisable as PCH’s documents. Page 22 of 60 The Community nurse documentation has been restyled as per the hospital documentation and is currently being printed following extensive trials by the community teams. Outpatient therapy documentation has been reviewed during 2012/13. Updated discharge documentation has been implemented but further work is required in 2013/14 to enhance discharge procedures in collaboration with our health and social care partners. Future plans for 2013/14 include: updating all specialist nursing documentation and the full integration of therapy and other clinical notes within the community hospitals 3.1.3 Dentistry Improving dental pathways for patients with Learning Disabilities with an emphasis on prevention and dental hygiene PCH Dental services have undergone a great deal of organisational change this year, with the resultant formation of PCH Dental Ltd, which is still part of the PCH family. PCH Dental has a lead senior Dentist for the care of patients with learning disabilities and a number of leaflets, providing supporting information have been developed for patients, carers and relatives. Work is on-going with the learning disabilities service to provide support into the clinics and a pilot is taking place in one location, to evidence the positive effect of enhanced reception cover. 3.1.4 Dementia Care Protect the quality of care and dignity of patients with dementia As an organisation we are committed to improving the services we provide to the people of Cornwall who have dementia. A programme of work has been undertaken in a number of our Community Hospitals which has led to some real improvements in relation to: Care delivered on a daily basis Improvements to the caring environment Improvements and understanding of the screening tools used within PCH Raising staff awareness of Dementia across the whole organisation Increased partnership working with all of the 3rd sector charities and organisations Partnerships have grown and developed between all provider organisations within Cornwall NHS We continue to work towards the South West Hospital Standards for Dementia Care Our progress so far has been recognised regionally, a number of staff were invited to present this and share our learning at a regional event in August 2012 held the Strategic Health Authority Page 23 of 60 We have started to review the environments in which we deliver care to look at how we can best support and encourage a healing environment for patients, carers, families and friends Developing and supporting local Dementia Champions in all 14 of our community hospitals is our next exciting step Developing a Dementia Friendly Organisation. We recently presented our first Gold Award to the Day Services Team at Camborne Redruth Community Hospital. This award has been introduced across the organisation and is in recognition of our staff’s continuing commitment to provide the highest quality of care to the community we serve. The team completed an educational workbook based on essential dementia awareness and person centered approaches. Future developments include the introduction of locality based Action Learning Sets which will aim to support our staff in the development of new initiatives and share learning and experiences so that we continually reflect on our practice. Collaboration with Alzheimer’s Society We are delighted to be working in partnership with the Alzheimer’s Society on a number of really exciting initiatives: Three of our community hospitals now have comprehensive information areas that are aimed at any health or social care concern with leaflets that patient’s carers and family members can take away. It also signposts local groups and further support A number of training events are taking place across our organisation which is predominantly aimed at our staff and will look specifically at: 1. The patient experience 2. The family and carer experience 3. A very personal experience of someone who’s family member had dementia We are continually striving to work with all of our partners across health and social care and as a result have carried out Dementia Care Mapping in a number of our hospitals. This process is recognised nationally and will help us to better understand the patient experience. Earlier in 2013, we held a Dementia Champions Day. Organisations present included: AgeUK, Alzheimer’s Society, Volunteer Cornwall, Royal Cornwall Hospitals Trust, Cornwall Partnership Foundation NHS Trust, Cornwall Council, Peninsula Community Health, Arts for Health, League of Friends and Sensory Trust. Page 24 of 60 The Dementia Champions made a pledge to respond to Standard 1 of the 8 Southwest Hospital Standards in Dementia Care: People with Dementia are assured respect, dignity and appropriate care and encompass the top five ingredients ‘SPACE’ for supporting good Dementia care as highlighted by the Royal College of Nursing. Staff who are skilled and have time to care Partnership working with carers Assessment and early identification of Dementia Care plans which are person centred and individualised Environments that are dementia friendly 3.1.5 Complaints Complaints handling – to improve the timeliness of complaints handling, to enhance the quality of root cause analysis and investigation of incidents and ensure learning across the organisation – this has been added following consultation Over the past 3 months, PCH has enhanced the service we provide to the public who raise a complaint or concern. The complaints team now work very closely with the Safeguarding Adults and Children’s team, to ensure that any concern that is raised about care is immediately screened to safeguarding. Historically, the local manager has always undertaken a complaint investigation for their service, but recently we have commenced independent managers undertaking investigations and root cause analysis as required. Complex and serious complaints are now discussed as part of our risk summits, which are held with a non-executive director and executive director, along with service leads. This ensures that the Board is informed of the detail of concerns/complaints, not just an overview. Page 25 of 60 Other areas of our quality performance in 2012/13 3.2 Maintaining Essential Standards for Registration with the Care Quality Commission PCH is required to register with the Care Quality Commission and its current registration status is without condition. The Care Quality Commission has not taken any enforcement action against PCH during 2012/13. PCH has not participated in special reviews or investigations by the Care Quality Commission as at 31st March 2013. 3.3 NHSLA Assessment There was no formal assessment for general NHSLA standards during 2011/12. 3.4 The East Cornwall Integrated Respiratory Team The East Cornwall Integrated Community Respiratory Team (ICRT) was commissioned in late 2012 and became operational on 4.2.13. The team consists of a full time Clinical Specialist Physiotherapist whose role is combined with Team Leadership. Specialist Respiratory Nursing, Occupational Therapy (OT), Speech and Language Therapy (SALT) and Physiotherapy Support Worker are the other posts contained within the team. The existing Respiratory Specialist Nurse post within East Cornwall has also been integrated into this team. The team was commissioned to improve the management of patients with respiratory conditions, specifically Chronic Obstructive Pulmonary Disease (COPD), for adults in East Cornwall. Its remit was to look at drawing together existing infrastructure, the development of clear referral pathways and improving links with acute care providers thereby improving integrated care for patients. The overarching objective of the new team, working in conjunction with other community respiratory resources is to provide care closer to home for patients with respiratory conditions thereby reducing unplanned hospital admissions to Derriford Hospital, Plymouth and Liskeard Community Hospital. In developing the initial business case, the focus was on the management of patients with COPD. The team, however, are managing a wide range of adult patients referred with respiratory conditions. Initial Objectives 1. To increase the capacity and ease of access to pulmonary rehabilitation in East Cornwall 2. To improve communication with referrers and integrated working with other community respiratory resources 3. To understand professional roles within the team and other Peninsula Community Health (PCH) provided services including the Acute Care at Home Team (AC@H) and Community Matron service Page 26 of 60 Pulmonary Rehabilitation Historically, pulmonary rehabilitation has been provided for East Cornwall at Liskeard Community Hospital. These have been cohort groups lead by the Specialist Respiratory Nursing Service with support from physiotherapists within the Community Rehabilitation Teams. From work carried out to predict demand for pulmonary rehabilitation, it was evident that there was a very significant shortfall in capacity in East Cornwall. Modelled estimates of Prevalence of COPD GP Practices (combined) East Cornwall, Eastern Region Public Health Observatory, October 2009 Expected number with COPD in practice Number on QOF register June 2011 2850 1908 QOF register as a percentage of expected prevalence 70% Expected number with MRC score of between 2 5 1278 Capacity for PR before ICRT Current capacity 48 350 (excluding rolling programme) This data captures the expected under diagnosis of COPD in the East Cornwall GP practice area and the increase in capacity for pulmonary rehabilitation since the ICRT has been in post. East Cornwall is a rural area and for some patients access to Liskeard is difficult. As well as the existing Liskeard groups, new groups have been established in: Saltash - St Barnabas Community Hospital Lewannick Village Hall - Launceston Other venues that will provide PR are being sourced at: Torpoint Callington Looe Other changes to the provision of pulmonary rehabilitation include: Full day joint assessments for appropriateness to attend pulmonary rehabilitation. This includes specialist nurse and physiotherapy assessment. The assessment includes functional capacity testing (Incremental Shuttle Walk Test) and a swallow screening Risk stratification of patients per baseline assessment to a specific level of exercise Page 27 of 60 Three levels of exercise at each of the 12 exercise stations – yellow, green and purple. Patients can therefore progress at each station as appropriate Patients exercise for two minutes at each station with an emphasis on pacing and breathing control. The stations alternate between muscle strength/ endurance and cardiovascular for the yellow and green levels and for the purple level full cardiovascular Warm up and cool down 10 – 15 minutes Within the groups, exercise is performed first followed by the education session so that patients can be carefully monitored during their recovery period Education sessions are kept to 30 minutes in duration to maximise participants’ attention span Patient education topics have been reviewed to reflect the skills within the team. All members of the team participate in delivering pulmonary rehabilitation and can cover for other members of the team. This safeguards the running of the groups in the event of sickness / unexpected team absence Outcome measures have been re-evaluated. The Incremental Shuttle Walk test – especially considering statistically significant improvements (Singh et al 2008), HAD score, Chronic Respiratory Questionnaire (self-reported) and patient satisfaction questionnaire are now used Links have been made with third sector support. These include University of the Third Age walking groups, Tamar Valley Walk and Talk groups, the local Breathers and Breathe Easy groups. For patients with transport issues, the Saltash Hopper and The Little Red Bus Company are keen to support the groups in East Cornwall All the above changes are underpinned by the latest evidence supporting clinically effective and safe provision of exercise for patients with COPD. Page 28 of 60 Outcomes of first Saltash Group Pulmonary Rehabilitation Saltash Group 1 Out of 9 people assessed for the programme 6 people completed the programme. There was a 33% combined UTA and DNA drop out rate. There was an average increase of 4.2 additional shuttles completed per person in comparison with initial assessment There was an average increase of 0.26 METs (metabolic equivalents) per person in comparison with initial assessment On average there was a 10.88% improvement in aerobic fitness using the Heart Rate Walking Speed Index (HRWSI). 10% is considered to be significant. The greatest individual improvement was 22.3% There were 2 patients that showed a significant improvement greater than 47.5 meters and 1 patient who achieved greater than 78.7% (Singh et al, 2008) There was an average improvement in the HAD anxiety and depression scores by 1.2 and 0.6 respectively Oxygen Clinics/ Respiratory Consultants – Derriford Hospital Monthly oxygen clinics at both Liskeard and Launceston Hospitals have been running since February. These clinics are run by the PCH Specialist Respiratory Nurses and are supported by two respiratory consultants from Derriford Hospital. They offer follow up reviews for all patients in East Cornwall on oxygen. For new patients, a clinic is due to commence in June, led by the Consultant Respiratory Nurse from Derriford Hospital. Derriford consultants are referring into the service and communication links are good. Patient Feedback from Pulmonary Rehabilitation Patients Comments during Pulmonary Rehabilitation (Quotes are summarised, not patients’ exact wording) “I was able to do some light gardening, weeding for the first time in two years.” “This is my second time of doing pulmonary rehab here in the hospital and I think that it is much better this time around. It is more paced so that I am able to achieve more, rather than going as quickly as I can and then needing 5 minutes to recover.” Page 29 of 60 “I went swimming for the first time since being diagnosed with my lung condition. The breathing techniques and the pacing helped greatly.” “Since starting the group I have lost weight, I have more energy and I feel more motivated to keep active.” “I have bought a step and some weights and have been doing the home based exercise programme regularly. I really enjoy it.” “I have been able to walk back up the garden path without needing to stop due to breathlessness.” “I have found playing golf, especially the walking between holes much easier and I have found that when I’m fishing all day, my stamina to stand all day has improved greatly.” “The education session on inhaler technique has really helped me, it has made such a difference.” “I am now finding that I am thinking about my breathing when I’m doing any activities and I am using the breathing techniques I have learnt. It is helping me a lot.” “The course has been really beneficial, all components.” Conclusion This 3 month evaluation demonstrates real progress in delivering improved respiratory services for patients across the clinical pathway. The admission data looks very encouraging and suggests the impact of partnership working across the respiratory pathway is contributing to fewer emergency admissions. It is very evident from patient feedback that the new service is making a real difference to people’s quality of life. Further evidence of this will be captured with the Clinical Outcome Measures being used by the team. There is currently no wait for patients to attend pulmonary rehabilitation if they are prepared to travel within East Cornwall and the team are able to offer a fast (within 24 hours) service for acute referrals. Page 30 of 60 3.5 Parkinsons Disease Service Here are examples of the innovative work being undertaken within the Parkinson’s Disease service: 1. Joint Parkinson’s / Therapy project Within the west of the county, two disease specific education / exercise groups have previously been developed for people with Parkinson’s. One group aims to provide specific information to newly diagnosed people with Parkinson’s and focuses on effective signposting, engagement with different healthcare professions and empowering people to self manage their condition. This has been combined with preventative exercise. The other group focuses on disease specific education / exercise for those people diagnosed for a longer duration, but aims to prevent problems such as falls. The commissioners agreed to fund two pilots for people newly diagnosed with PD within mid / north & East Cornwall and two further groups within the same areas for people with more advanced disease. These four pilot groups have now been completed. Early evaluation reveals that people felt better equipped to manage their long term condition, not only through the provision of exercise / education, but also through the development of relationships with other group members. More in depth evaluation is currently taking place and the results of these pilot groups will be presented to Kernow Clinical Commissioning Group in the near future. 2. To reduce Parkinson’s Hospital admissions by development of a pathway that identifies the reasons why people with Parkinson’s acutely deteriorate One of the Parkinson’s Nurse Specialists in conjunction with the Parkinson’s team has developed a pathway for primary / community services to identify and manage the acute deterioration of Parkinson’s symptoms. It is known that people with Parkinson’s are admitted to Hospital when infection (for example) may be present. In this situation it is preferable to identify and manage the signs of infection rather than increase Parkinson’s medication. This pathway has been presented to the Prescribing GP leads and forms part of the 2013 – 14 Medicines Optimisation Plan (formerly QIPP). It has been adapted for RCHT use (to reduce Hospital stay) and will form part of an educational event in the near future. The aim will be to reduce Hospital admissions by effective and ongoing use of this pathway. 3.6 Safety Thermometer The NHS Safety Thermometer is a national improvement tool, to assist in reducing harm to patients. The NHS Safety Thermometer was intended to be a local improvement tool for measuring, monitoring and analysing patient harms and ‘harm free’ care. Page 31 of 60 The safety thermometer was developed throughout 2011 with over 160 NHS provider organisations involved in the development and testing. The tool measures four high-volume patient safety issues (pressure ulcers, falls resulting in harm, urinary infection in patients with a catheter and treatment for venous thromboembolism). It was then adopted as a National CQUIN and introduced nationally from April 2012. In the first 12 months the CQUIN was based on successfully implementing the safety thermometer across all applicable services in the organisation. In the initial guidance the inclusions and exclusions were open to interpretation and it was the case that different organisations implemented in different teams. In the main in the first year, most organisations have surveyed inpatients and community/district nurses. This guidance has been clarified for 2013-14. The safety thermometer process involves recording against the four harms one day a month on the same day across the entire organisation. All patients in an inpatient area on the survey day are included, as well as everyone seen in the community on that day. N.B. Patients seen in groups or outpatient clinics are not currently included in the safety thermometer process. Locally it was agreed that to meet the requirement of the 2012-13 CQUIN PCH would be required to implement the safety thermometer in all inpatient wards by April 2012 and all applicable community services by September 2012. Following presentations to Ward Sisters and Matrons the safety thermometer was successfully implemented in all wards in April. In the community a phased approach was taken with District Nurses and some other community services implementing in July and all applicable teams by September. This was achieved through briefings with teams, production of in-house guidance on data collection and recording and good communication links between the Governance team and service leads and team members. Feedback from all teams involved has been very positive and appreciative of the support provided by the Governance team. Since implementation a total of 3290 inpatients have been surveyed with on average over 270 per month. In the community since July 9588 patients have been surveyed for the safety thermometer with an average of over 1065 patients per month. Page 32 of 60 In total 12878 patients have been surveyed. Of these 11518 have suffered no harm 89.44%. A number of these were harms acquired before being admitted to PCH care (for example patients who were admitted with a pressure ulcer). When looking at those with new harms only, acquired since coming under PCH care, 12323 suffered no harm (95.69%). Whilst the safety thermometer is not primarily a benchmarking tool it is worth looking at the national safety thermometer harm levels to ensure PCH is not significantly different to the national picture. When looking at all organisations and all settings the overall harm free care percentage for the year to date at 91.62% is higher than PCH and the new harm free care percentage slightly higher at 96.32% When comparing PCH wards to all community hospital wards we compare slightly better, with 90.94% and 97.33% all harm free and new harm free respectively compared to all community hospital wards of 87.88% and 95.68% When looking at PCH community services compared to all community based services nationally PCH compares slightly less at 88.92% and 95.13% all harm free and new harm free care respectively compared to 91.19% and 96.6% for all community settings nationally. The following charts show PCH performance against the 4 harm measures for combined ward patients and community patients: Percentage of patients with ANY pressure ulcer 11.00% 9.89% 8.00% 8.36% 10.29% 7.55% 8.56% 7.68% 7.25% 6.51% 7.13% 6.57% 6.83% 5.00% 4.26% 2.00% Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar All PCH Services % Median Page 33 of 60 Percentage of patients with evidence of harm from a fall 3.00% 2.77% 2.50% 2.27% 2.12% 2.06% 2.00% 1.50% 1.06% 1.00% 1.07% 1.29% 0.93% 0.90% 0.72% 0.50% 0.60% 0.70% 0.00% Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar All PCH Services % Median Percentage with an in dwelling urethral urinary catheter & receiving treatment for ANY urinary tract infection 3.00% 2.50% 2.44% 2.00% 1.50% 1.54% 1.46% 1.24% 1.07% 1.00% 1.01% 0.71% 0.68% 1.00% 0.50% 0.62% 0.60% 0.00% 0.00% Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar All PCH Services % 1.50% Median Percentage receiving prescribed anticoagulation treatment for treatment of a NEW documented VTE event 1.00% 0.92% 0.85% 0.50% 0.89% 0.65% 0.58% 0.51% 0.36% 0.46% 0.35% 0.38% 0.38% 0.35% 0.00% Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar All PCH Services % Median Page 34 of 60 The final two charts show the two key harm measures. All Harm Free Care Percentage with no PU, harm from fall, urinary infection (in patients with urinary catheter) or NEW VTE (ALL HARM FREE) 95.00% 93.62% 93.00% 91.65% 91.59% 91.67% 91.00% 89.00% 90.66% 89.86% 89.15% 88.67% 88.50% 89.79% 87.00% 86.63% 86.13% 85.00% Apr May Jun Jul Aug Sep Oct All PCH Services % Nov Dec Jan Feb Mar Median New Harm Free Care Percentage with no NEW PU, harm from fall, NEW urinary infection (in patients with urinary catheter) or NEW VTE (NEW HARM FREE) 100.00% 98.00% 98.91% 98.23% 97.14% 96.92% 95.83% 96.00% 95.12% 94.00% 96.63% 95.03% 94.45% 96.17% 94.74% 93.36% 92.00% Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar All PCH Services % Median Page 35 of 60 3.7 Blood Transfusion Management PCH staff administered approximately 900 units of blood per year across the County. Most of these are 2 unit transfusions. In 2012/2013 20% of all blood supplied from the transfusion Laboratory in RCHT was transfused in the Community. Patients are transfused as inpatients or day patients in all the Community Hospitals except Fowey and Poltair: The Acute Care at Home team transfuse patients at home in the mid and west of the County. Blood fridges are in place at Bodmin, St Austell, Newquay, Camborne Redruth, Falmouth, Helston, St Marys, Liskeard, Launceston, St Barnabas and Stratton. To comply with NPSA SPN14 ‘Right Patient-Right Blood’ staff are required to complete transfusion training and face to face competency assessment on a two yearly cycle. Since April 2012 PCH nursing staff have maintained 98% compliance. Training and assessment has been on going in all areas to maintain this level. Staff are assessed by the ward based transfusion assessors who in turn are assessed by the Transfusion Practitioner. In areas where there are blood fridges, staff also complete fridge monitoring competencies to comply with BSQR and MHRA requirements. It is a legal requirement to have 100% traceability of blood products from donor to recipient and to provide evidence of the cold chain of the products. Any deviation is reported on Datix as an incident and investigated. The Transfusion Practitioner submits a quarterly incident report to the clinical quality and safety committee. The low level of incidents demonstrates the benefits of all the training and assessment. There has been a 55% reduction in incidents in year 2012/2013. The following table illustrates the year on year reduction in incidents 35 30 25 20 2009/10 15 2010/11 10 2011/12 5 2012/13 Ot he r iss m ne ar n is tio ip SH OT su e ain es cr ce ab ilit y tra /u ni t co ld ch pr w as te d b X‐ lo od m at ch 0 Page 36 of 60 In 2011/12 there were 60 reported incidents (not including fridge incidents). Most of these were documentation or cold chain errors affecting compliance with MHRA and BSQR regulations; 6.7% of transfusions involved a minor error. In 2012/12 there were just 25 reported incidents Mostly minor documentation and cold chain errors. Overall 2.7% of transfusions involved a minor error, a considerable reduction on previous years. The ultimate aim is to reduce this to 0%. Any incident involving the wrong blood transfused; special requirements not met: unnecessary or inappropriate transfusions: handling and storage errors resulting in unsafe transfusion of products and Right Patient Right Blood administration errors must be reported nationally to SHOT (Serious Hazards of Transfusion). In 2012/13 only two incidents were reported to SHOT. One of these was a transfusion reaction rather than an error and the second was relatively minor with no harm to the patient. A full root cause analysis is completed with every SHOT report and an action plan and further education implemented as required. NPSA SPN14 ‘Right Patient Right Blood’, endorsed by the MHRA, recommended that electronic blood tracking be implemented to improve traceability and patient safety. The Transfusion Practitioner has been working closely with the acute Trusts to ensure a smooth transition into community sites. Currently, relevant staff are being issued with barcoded ID cards, training is planned and equipment being ordered and installed to ensure a smooth transition to new procedures and to ensure our patients are not inconvenienced. 3.8 Safeguarding Adults Ensuring our patients are safe and able to live free from abuse remains our constant priority and we strive to ensure that our staff are equipped to recognise and challenge the signs of abuse and take appropriate steps to safeguard children, young people and vulnerable adults. 2012/13 witnessed a significant county wide increase in reported safeguarding concerns and safeguarding alerts requiring multi agency management and intervention. In recognition and in a robust response to this PCH undertook a review of its existing safeguarding management and practice arrangements, compiling a safeguarding action work plan which scoped the issues and identified positive solutions and focus for the direction of required improvement and change. During December 2012 PCH formed a Safeguarding Unit in order to address the following key priorities: To improve safeguarding management, leadership, supervision and education To develop and align safeguarding alert processes for children, young people and vulnerable adults ensuring that individual rights are protected and promoted Page 37 of 60 To promote patient safety principles and reduce risk through effective management To strengthen and improve engagement with multi agency safeguarding processes improving the quality of safeguarding alert investigation To effectively support staff involved in multi agency safeguarding processes, embedding and sharing the learning identified from these To provide statistical and pertinent data relating to safeguarding trends, themes and concerns to the executive in order to demonstrate compliance and/or effectively assess and manage risk The Unit has focussed its efforts on accessibility and the provision of consistent support and advice to staff via telephone, electronic or face to face contact. Review of the safeguarding alert reporting procedure was undertaken in recognition of the need to streamline the expected interventions taken by staff in order to meet both multi agency and internal governance reporting requirements. This was achieved by adapting the existing incident reporting system – Datix, which staff were familiar with. It was backed up with the introduction of a range of supportive tools and protocols developed to enhance, capture and transfer information both internally and externally in order to facilitate improved communication and record keeping in support of the multi agency safeguarding process. In turn this has resulted in an improvement in the quality of the information contained within the referrals and an increased confidence in staff when reporting their concerns. The PCH Safeguarding Adults Policy was also reviewed in order to reflect the improvements implemented and provides an easy to read resource for staff that ensures that they are able to recognise their personal and organisational safeguarding responsibilities. The Safeguarding Unit monitor, support and provide safeguarding training, reviewing the content of training and education in order to ensure that it is current and continues to reflect legislation. There has been widespread investment in delivery of children’s safeguarding training for many allied therapy services in order to improve compliance and understanding of professional responsibilities. Whilst in respect of adult services the requirement to ensure compliance with the Mental Capacity Act 2005 and Deprivation of Liberty safeguards provides on going challenge. As part of their review of providers in 2012/13, the Care Quality Commission visited all registered locations within PCH and found staff to be knowledgeable regarding safeguarding procedures and consistently knew where to seek advice and what to do if they had a concern. Page 38 of 60 3.9 Nursing Metrics and Patient Experience Measurement during 2012/13 The last year has seen a period of very intensive patient experience activity in PCH. It has been a year of extensive change in the NHS, accompanied by rapidly changing national and local priorities. New initiatives were announced with very short timelines for implementation, and other exciting opportunities for innovative development were seized. This meant some of the work that had been planned to take place during the year had to be delayed in order to focus on meeting newly imposed deadlines. Two major areas of patient experience activity during 2012/13 were: Winning Department of Health funding in the NHS Institute Patient Feedback Challenge. The project, ‘Kinda Magic’ aimed to 1) spread the principles of the PCH methodology of collecting patient experience metrics across the NHS and 2) develop tools to collect patient experience feedback from patients with cognitive and communicative impairment Implementation of the Friends and Family Test, announced by the Government at the end of May 2012 Patient Experience Metrics – adding quality to our metrics We are now starting our 3rd year of collecting Patient Experience Metrics from patients in our community hospitals. Our ‘metrics’ or ‘indicators’ are a set of questions we ask patients during unannounced ward visits. ‘We’ are a team of non-clinical managers or members of our training team who visit wards and talk to patients. We ask them the questions that help us obtain our regular quantitative metrics, but we also have a conversation around their answers and capture their comments. We report this information back to the Ward Manager and Matron. This information helps us all to understand why patients give the answers they do. This is the qualitative information that helps us to target our actions most effectively. Depending on the size of the ward, up to 10 patients (and sometimes relatives) are interviewed. Reporting back patient views and actual comments is extremely powerful. Often this feedback is very positive and encouraging to staff, and when there is negative feedback this motivates immediate attention to issues that arise. During the last year it’s been very evident that staff have really taken ownership of their feedback. There are many examples of where they have acted on patient feedback extremely quickly, sometimes before the end of day. Consistent good practice – responses to questions about patients’ perceptions of cleanliness of their environment patients’ confidence in staff hand hygiene patients saying they have enough to eat and drink patients not sharing their sleeping area with the opposite sex Page 39 of 60 privacy have always scored highly and continue to do so. Improvements – aggregated results show overall improvement during the year as a result of improvement in indicators for patients saying they receive enough help to eat their meals and patients saying they feel involved in decisions about their care and treatment, the latter being a significant improvement. A review of historic data shows that performance of questions about prompt answering of call bell information giving about medications finding staff to talk to about worries and concerns have improved considerably from 2011-12 to 2012-13 Patient Experience Metrics roll out across District Nursing Last year we said we would implement our metrics process across District Nursing Services. After testing it during the year it was implemented during February 2013. A small number of patients from each of the District Nursing caseloads are randomly sampled each month. Selected patients are sent a short questionnaire to complete and a questionnaire for their Carer (if they have one) to complete. Both questionnaires contain a section seeking qualitative comments. Although results are not yet available (due to technical issues with the data analysis process) sight of completed questionnaires at data entry suggests that the majority of patients report high levels of confidence in the service and hold their District Nurses in high regard. TB Immunisation Service – Patient Experience questionnaire survey We said we would measure the experience of people who bring their children for TB immunisation. This has recently been implemented. The questionnaire has been simplified to help people whose first language is not English, and will be available for translation on request. Dental Services – Patient Experience questionnaire survey We said we would measure the experience of people accessing PCH Dental Services. Due to some organisational changes within the service this did not progress as quickly as we hoped but it remains in the plans to carry out this year. A separate piece of work targeted towards the care of people with Learning Disability in Dental Services is also planned. Page 40 of 60 ‘Kinda Magic’ Last year we said we wanted to develop tools to capture patient experience feedback from patients with cognitive and communicative impairment because our patients with dementia, learning disability, aphasia etc. were excluded from our process to collect our Patient Experience Metrics. We seized the opportunity of the NHS Institute Patient Feedback Challenge, launched in May 2012, and submitted a bid for a share of the £1million Department of Health funding to use for the ‘spread and adoption’ of existing good practice in patient experience across the NHS. After a rigorous selection process involving ‘hot houses’ and ‘crowd sourcing’ methodologies, ‘Kinda Magic’ was one of 9 projects selected from over 40 entered. The expert panel recognised the strengths and value of PCH’s methodology of collecting quality patient experience metrics and asked us to ‘spread’ this process to other areas of the NHS. ‘Kinda Magic’ has 2 main aims or ‘phases’: Phase 1 – the spread and ‘adoption’ of the principles of the PCH process of collecting patient experience metrics to other specialities and to other organisations Phase 2 – the spread and ‘adaptation’ of the tools and process to groups of patients usually excluded, those with communicative and cognitive impairment such as dementia, aphasia and learning disability The project got underway in September 2012. With the NHS Institute’s closure in March 2013, only 6 months after starting, there has been enormous pressure to progress the work and achieve its main outcomes during that time. ‘Kinda Magic’ is however a lot more complex in nature than some of the other projects and it has always been acknowledged that work on Phase 2 would need to extend beyond that time. The success of ‘Kinda Magic’ has been astonishing but was made achievable in such a short time because of the work put in by the project participants and spread partners, and because it has been largely ‘event driven’. Phase 1 has completed although there is still work to do to produce the Phase 1 section of a toolkit. Peninsula Community Health Implemented principles of metrics in District Nursing Service Royal Cornwall Hospitals NHS Trust (RCHT) Implemented PCH principles in Eldercare Coventry and Warwickshire Partnership Trust Implemented in mental health inpatient units Implementing in District Nursing Hertfordshire Partnership Foundation Trust Implemented in mental health inpatient units Page 41 of 60 Cornwall Council Adult Care and Support Implementing in Care Homes Interestingly, although each organisation and service is free to decide on their own question set, it is remarkable how similar each question tool is to each other. The tool which is currently in use in Care Homes has been changed very little from the one used in PCH. Phase 2 is continuing. Work on developing and adapting tools to include patients with cognitive and communicative impairment has been organised in workstreams across our spread partners Dementia – led by Peninsula Community Health Learning Disability – led by Royal Cornwall Hospitals Trust Aphasia and Stroke – led by Peninsula Community Health Children/Young People – led by Royal Cornwall Hospitals Trust Mental Health – led by Coventry and Warwickshire Partnership Trust Creative and innovative tools and processes are being further developed. Moving forward, both the tools and the methods employed will now require wider testing and validation. National interest in ‘Kinda Magic’ is growing. In this post-Francis period, ‘quality’ metrics have a value in providing a regular ‘snapshot’ of patient experience across a wide (or full) range of areas. Furthermore, tools and processes to enable all patients to be included are widely sought after. In March 2013, all 9 Patient Feedback Challenge projects were showcased at a national celebratory event in London. The ‘Kinda Magic’ project team were asked to open the presentations and talk about the programme as well as the project. Following this event, other organisations have contacted us for information about our tools and methods. We have also been invited to present ‘Kinda Magic’ to representatives of all 7 Health Boards in Wales in a Masterclass in June. In March, we were invited to showcase ‘Kinda Magic’ on the new NHS Improving Quality stand at Innovation Expo, which gave it wide exposure. We anticipate that there will be tangible progress in produced tools by autumn 2013. Learning Disability PCH is working to achieve full compliance with the Mencap Charter to ensure our services are accessible to people with Learning Disability (LD) and that we meet their needs. Working with us are ‘CHAMPS’. CHAMPS are employees of Health Promotion; they are people with LD who represent patients with LD. Last year the CHAMPS undertook assessments of the Minor Injuries Units and Outpatient Departments in all our Community Hospitals. They wanted to find out: Page 42 of 60 Whether staff knew how to contact their LD Liaison Nurse Whether staff knew about and use ‘Hospital Passports’ Whether easy to understand information about health and health procedures was available Whether staff had an understanding of and awareness of ‘reasonable adjustments’, Mental Capacity laws and advocacy services How they were spoken to Whether they could find their way around The CHAMPS have undertaken assessment visits at all but 2 community hospitals so far. Following the assessment visits, the LD Liaison Nurses together with the CHAMPS have commenced a programme of training sessions in each hospital (informed by the assessments) to ensure that staff are informed and better able to meet the needs of people with Learning Disabilities. When this programme is complete, the CHAMPS will make a second round of unannounced visits to repeat the assessment. Information leaflets have been developed for people with LD. These have been developed together with the CHAMPS. Information leaflets include About the Learning Disability Liaison Nurse Service Traffic Light Hospital Passport How to make a complaint Comment Card Leaving Hospital Consent – Saying Yes or No Carer’s Information These leaflets are due to be printed and will be in use soon. Friends and Family Test The Friends and Family test was implemented in all wards and Minor Injury Units (MIUs) in all our community hospitals in mid-March, 2 weeks ahead of the mandatory implementation date of 1st April 2013. All patients aged 16 and over must be offered the opportunity to answer the question ‘How likely are you to recommend our ward [MIU] to your family and friends if they needed similar care or treatment?’ at or within 48 hours of discharge. Page 43 of 60 A response card is given to every patient on discharge from a ward, or on being seen and sent home from MIU. They can reply on the response card by a Freepost address, or online via the PCH website using the ward/MIU identifier. Staff are not permitted to assist patients to complete the response card but they can give them an information leaflet about it, and remind them on discharge. Whilst the first complete month’s data is still being collected, the data collected so far is very encouraging. Of 223 responses so far entered onto the database: 209 said ‘Extremely likely’ 10 said ‘Likely’ 1 said ‘Neither likely nor unlikely’ 1 said ‘Unlikely’ 1 said ‘Extremely Unlikely’ 1 said ‘Don’t Know’ Most have written comments that are very complimentary in nature, there are a few constructive comments and only 2 negative comments. The following are very typical comments: “Very quick and jovial nurse. Happy and cheerful. A great change to have a happy nurse.” “I received very quick and friendly help when visiting hospital. Very pleased with service.” “Lovely staff that meet you with a smile” “The staff were cheerful, friendly polite and efficient. I was booked in, treated and on my way in 25 mins. The treatment was explained to me as it was ongoing and I was given clear instructions as to how to continue in the next days.” “Everything was efficient, friendly and nothing seemed too much trouble. The care and being looked after was far above which one would expect. My thanks go all out to the unit.” “Very helpful, very professional. Would like to thank the nurses concerned. They were apologetic for the delay in being seen, but this didn't matter. Couldn't get to see GP and would have been sent to you anyway. Wonderful service. Please keep it up!” “The proficient way in which the staff did their work giving one an immediate sense of confidence. The kindness, care taken to explain any suggestions as to what I should do or not do in order to hasten the healing progress. Well done.” Page 44 of 60 NHS Choices and Patient Opinion – Feedback on public websites NHS Choices and Patient Opinion are two popular websites for patients and the public to post feedback on our services ‘Tripadvisor’ style. Use of these websites is on the increase and ratings and feedback are followed by local media and other national and local organisations. Twenty-nine (29) items of feedback were posted during 2012-2013, more than half of which (17) relates to MIUs. All but one item of feedback was positive and praiseworthy of the unit visited. 3.10 Eliminating Mixed Sex Accommodation (ESMA) PCH has remained 100% compliant with eliminating mixed sex accommodation. 3.11 Complaints and Compliments PCH welcomes comments and suggestions about any aspect of our services. We equally value any concerns or complaints to be raised with us in order to ensure we improve the services we provide. During the year 2012-2013 we received a total of 120 complaints across a range of community services, raising a variety of issues as well as some common themes. One of these complaints was passed with consent to another organisation to investigate and 16 were withdrawn or not taken forward by the complainant. The remaining 103 complaints were about community health services and were followed through the complaints procedure. 42 were made in writing and 61 were made verbally to staff. 111 complaints were received in the previous year. A total of 295 PALS contacts were received during this year. 87 of these were about other organisations. The remaining 208 PALS contacts were about community services provided by Peninsula Community Health. There were 62 requests for interpretation and translation services during this period. 254 PALS contacts were received during the previous year. The following charts compare the number of cases received against previous years as follows: Complaints Received: Q1 2009 to Q4 2013 PALS Contacts Received: Q1 2009 to Q4 2013 40 120 30 100 20 80 10 60 0 Q1 Q2 Q3 Q4 2009-10 17 25 27 33 2010-11 30 33 23 34 2011-12 30 33 21 27 2012-13 27 36 22 35 40 Q1 Q2 Q3 Q4 2009-10 97 119 101 110 2010-11 109 83 104 106 2011-12 60 54 62 78 2012-13 72 52 83 88 Page 45 of 60 The following chart shows the number of complaints and PALS contacts received in each month of 2012-13 Complaints and PALS Received 2012-2013 40 30 20 10 Complaints Received Mar-13 Feb-13 Jan-13 Dec-12 Nov-12 Oct-12 Sep-12 Aug-12 Jul-12 Jun-12 May12 Apr-12 0 PALS Received We place an emphasis on resolving complaints and PALS concerns as quickly and effectively as possible, and in a way that is both proportionate and agreed with the complainant. The investigation of individual complaints identifies actions to be taken to reduce the risk of the complaint recurring. Work is ongoing across PCH to ensure that learning from individual complaints is spread across the organisation. Where any part of a complaint is upheld, the complainant always receives an apology. All issues require a level of investigation and the same principle applies where the findings agree with any aspect of an issue. There are also occasions when suggestions are made, for example, to improve an environment explanation and information about the actions identified and taken to address the issue. 94.8% of all complaints received were acknowledged within 3 working days. 97% of the complaints pertaining to PCH received a final response within a timescale agreed with the complainant, including those where an extension was requested and agreed. The following charts show the acknowledgement and final response times over the last four years. % acknowledged within 3 working days 100 2009-10 2010-11 2011-12 2012-13 85 70 Q1 Q2 Q3 Q4 Page 46 of 60 % final response within timescale agreed with complainant: 100 2009-10 2010-11 2011-12 2012-13 85 70 Q1 Q2 Q3 Q4 The Parliamentary and Health Service Ombudsman has responsibility for the second stage of the NHS Complaints Procedure. There were two referrals made during this year. One was made regarding dental treatment, which the Ombudsman decided not to investigate following an initial screening review. The other related to specialist therapy and we are awaiting the outcome of this initial screening process. ICAS is a free, independent and confidential service available to anyone who wishes to make a complaint about their NHS care. This statutory service was launched in 2003 and provides a national advocacy service delivered to agreed quality standards. The organisation has recently been restructured to reflect the concentration on health issues. IHCAS advocates support complainants in making complaints, and assist them to think about what they would like to achieve from their complaint, such as an apology, an explanation or an improvement to NHS services. All complainants who contact the Complaints & PALS Department are given information about their local IHCAS office. Three complaints were made through ICAS during this year. No complaints were made based specifically on issues of Equality or Diversity. All complainants are advised that they should never be discriminated against if they make a complaint, and to let us know immediately if they believe this has happened to them Patient Advice and Liaison Service (PALS) The Patient Advice and Liaison Service (PALS) was introduced by the Department of Health in 2002 to provide advice and support to users of local health services. The PALS service is predominantly telephone based, although an increasing amount of people are using the website to contact PALS. Enquirers raise a wide range of issues; some are simple requests for information and others are more complex, requiring numerous calls and sometimes mediation meetings. The service is available to any member of the public, patients, carers, relatives and staff. Page 47 of 60 The seven national standards for PALS are being used to develop a framework in which to work. This will ensure PCH meets the criteria for the core standards. The seven national standards are: The PALS service is identifiable and accessible to the community served by the organisation; PALS will be seamless across health and social care; PALS will be sensitive and provide a confidential service that meets individual needs; PALS will have systems that make their findings known as part of routine monitoring, in order to facilitate change; PALS enables people to access information about services provided by the organisation, and information about health and social care issues; PALS plays a key role in bringing about culture change in the NHS placing patients at the heart of service planning and delivery; PALS will actively seek the views of service users, carers and the public to ensure services are effective. An integral part of the PALS function is to work alongside other NHS organisations, acting as a liaison between the patients and the service. Calls relating to other providers are passed to the PALS services of those organisations, or advice is given about how they can be contacted. Peninsula Community Health PALS received a total of 295 contacts during 2011-12. The table below shows a breakdown of the types of issue raised by callers: Types of Issues raised with PALs Q1 Q2 Q3 Q4 25 20 15 10 PALS Referral Feedback Interpretation & Translation Complaint PALS Support Information Issue to Resolve 0 Advice 5 Page 48 of 60 Translation and Interpretation Services PALS organises translation and interpretation services which provide face-to-face interpreters and translation of literature for community health staff. This is arranged through Jobline Staffing, Language Line or Cornwall Deaf Association. 62 requests were made during this year, compared with 45 in the previous year. There was a marked rise in Polish interpretation and although requests were made across a range of services, the requests were predominantly for Physiotherapy and Dental appointments. Positive Feedback Although complaints and concerns are formally monitored, it should not be forgotten that these are far outweighed by the number of plaudits received. There are many patients who are very happy with the services provided by the organisation and who appreciate the professional and caring treatment they receive from staff. An array of praise is regularly received by staff in a variety of settings, including numerous cards, flowers, biscuits and chocolates as a mark of thanks for the care staff have provided to patients. Around 600 plaudits have been brought to the attention of the PALS team, although we are aware that not all services and locations regularly advise the department. Work is continuing to encourage services to share these with PALS, to enable this important aspect to be accurately quantified and logged. You said, we did The investigation of individual complaints identifies actions to be taken to reduce the risk of the complaint recurring. Work is on-going across PCH to ensure that learning from individual complaints is spread across the organisation. Where any part of a complaint is upheld, the complainant always receives an apology, an explanation and information about the actions identified and taken to address the issue. Some PALS issues require a level of investigation and the same principle applies where the findings agree with any aspect of an issue. There are also occasions when suggestions are made, for example to improve an environment or a service procedure and, where appropriate, these ideas are acted upon. Page 49 of 60 Below are some examples of the actions taken as a result of complaints and PALS: You Said… We Did… I wasn’t told soon enough that my appointment had been cancelled. We revised our answerphone messaging policy to ensure patients are notified of cancellations at short notice. My child’s orthodontic appointment was cancelled and there’s been a long wait for another appointment. We reviewed the child’s clinical need and arranged an appointment for the following week. My father and I are worried about what will happen next when it’s time for my mother to be discharged from hospital. We arranged a meeting with the matron to discuss the patient’s care in depth, and offer reassurance that the family would be involved in making any decisions about the future. I would like to understand why, when my We arranged a meeting with the matron to father died, his case was referred to the explain how this happened and why. Coroner. How do I access podiatry? We explained and provided the caller with a self-referral form. My son is 17 - why did he have to pay for a prescription from the Minor Injury Unit? We explained that charges applied because he did not meet any of the charging exemptions. I’m concerned about my knee brace, which doesn’t fit properly and is uncomfortable. The physiotherapy team arranged a further appointment to review the knee brace and make any necessary alterations. I took my friend to Bodmin Hospital and we found there were no wheelchairs with footrests. This made my friend feel anxious that he was going to fall out, and compromised his dignity. We are currently making arrangements to rectify this and ensure that wheelchairs with footrests are available to patients and visitors. There’s been a delay in the orthodontist fitting my child’s brace. Having reviewed the child’s clinical needs, we explained the reason for the wait, and that this would not have a negative effect on her child. Page 50 of 60 3.12 Focus on the Isles of Scilly PCH provides hospital and community nursing services on the Isles of Scilly. St Mary’s Hospital continues to provide “in” patient care for a broad variety of conditions and age groups. We have especially been focusing on the reablement of patients who are elderly or who have chronic health problems, to enable them to maintain their mobility and independence. A large number of the staff have received training in this area over recent months. We work closely with Adult Social Care in this, and provide comprehensive information to them when a patient is discharged home to help ensure continuity and progression. We continue to provide initial care and stabilisation of patients with acute and serious health problems prior to transferring them to the mainland for on-going care. Our MIU department is open 24hours a day. All MIU staff have recently completed the Resuscitation Council Paediatric Immediate Life support training. The demise of the BIH helicopter service last year has continued to cause us some logistical problems with getting blood samples, specimens etc. to the mainland & with obtaining Pharmacy supplies especially over the winter months. However, these have now largely been resolved. We are hoping that the “near patient” testing equipment, due to be installed at the hospital in the near future should mean fewer samples have to be sent to the mainland for analysis and should speed diagnosis and improve the service to our patients. In the last 12 months, we have seen the following performance highlights for St Mary’s Hospital: Co-location of health and social care staff at St Mary’s Hospital Continued high performance in risk assessing and providing preventative treatment for venous thrombo-emboli Continued high performance in medicines reconciliation Care of the Deteriorating Patient Implementation of Early Intervention Service Reducing harm from falls Nursing and Patient Experience Metrics Maintaining Essential Standards for Registration with the Care Quality Commission. St Mary’s Hospital found to be fully compliant when visited unannounced by CQC Upgrade of x-ray facilities in St Mary’s Hospital Page 51 of 60 How safe was healthcare on the Isles of Scilly in 2012/13 100% of inpatients received thrombo-emboli risk assessment and treatment No community or hospital medication errors 8 inpatient falls – 2 sustained minor harm – nil other harm 2 hospital security incidents – no harm to patients 2 blood transfusion incidents – no patient harm 4 patients suffered pressure ulcers (3 patients had sustained these prior to admission) No pressure ulcers sustained in our care since April 2012. 100% inpatients at St Mary’s received Medicines reconciliation, reducing the risk of medication errors and improving patient outcomes Patient Experience feedback tells us that in March, patients found their experience in St Mary’s to be 91% positive Isles of Scilly 2012/13 In 2012-13, District Nurses on the Isles of Scilly undertook 3,534 patient visits Throughout 2012-13, St Mary’s Hospital on the Isles of Scilly had a total of 191 inpatients In 2012-13, 2,831 appointments were undertaken by Dentists on the Isles of Scilly Throughout 2012-13, 1,075 patients Were seen by services provided by Peninsula Community Health on the Isles of Scilly Page 52 of 60 3.13 PEATs The chart below shows the PEATS scores for 2012. PEATS (Patient Environment Action Team) visits occur on a yearly basis and are an opportunity for members of the public (Healthwatch) and organisation representatives to visit all the ward and clinical areas to undertake an inspection of the environment and food. Maximum scores are 100% per area of inspection. PEAT WEIGHTING ENVIRONMENT % PRIVACY & DIGNITY % FOOD % CLEANING % BODMIN 80.91 84.62 98.36 95 CAMBORNE REDRUTH 76.42 94.12 95.08 91.6 EDWARD HAIN 77.56 88.89 90.16 83.4 FALMOUTH 80.18 84.29 90.16 88.4 FOWEY 83.81 92.31 91.8 93.3 HELSTON 91.81 86.25 90.16 90.9 ISLES OF SCILLY 91.16 96 90.16 97.1 LAUNCESTON 76.72 73.33 81.97 92.2 LISKEARD 90.83 95.29 95.08 90.1 NEWQUAY 89.77 96 83.61 90.4 POLTAIR 90.13 100 91.8 84.5 ST AUSTELL 90.16 90 91.8 94.6 ST BARNABAS 91.61 98.57 91.8 90.5 STRATTON C L O S E D 89.6 Page 53 of 60 4.0 Response to this report from our stakeholders 4.1 Cornwall Overview and Scrutiny Committee During the consultation for this Quality Account, Cornwall Council was in a pre-election period prior to the 2013 local elections. Whilst the election has now taken place there is to be a new Council governance structure which will include alterations to the health scrutiny function. In the period April 2012 to April 2013 the Health and Adults Overview and Scrutiny Committee has regularly scrutinised Peninsula Community Health. This scrutiny will be undertaken by the new Health and Social Care Scrutiny Committee in the future municipal year. It is expected that Peninsula Community Health will be required to report to the Health and Social Care Scrutiny Committee, its progress against the stated future priorities for quality improvement and performance indicators contained within this Quality Account. 4.2 Isles of Scilly Overview and Scrutiny Committee The Isles of Scilly Health Overview and Scrutiny Committee welcomes the opportunity to contribute to these Quality Accounts. We would like to see further development of the integration of health and social care services on the islands. As part of this we welcome the opportunity to engage with Peninsula Community Health on how to maximise all the available resources on the islands, especially the Community Hospital, to provide seamless service provision. 4.3 Kernow Clinical Commissioning Group Kernow Clinical Commissioning Group (KCCG) welcomes the opportunity to comment on the Quality Account 2012/13 for Peninsula Community Health (PCH). KCCG recognises the approach PCH has developed in setting out its plans for quality improvement and we continue to develop existing processes to agree, monitor and review the quality of services throughout the year. The Quality Account presents an overview of a wide range of quality improvement work being undertaken. We note the continued progress that has been made in: reducing avoidable harm through Venous Thrombo-embolism risk assessment, understanding why pressure ulcers occur, the decrease in cases of CDiff, the expansion of specialist respiratory services in the East and the expansion of Acute Care at Home across Cornwall. KCCG would further highlight the work PCH have carried out improving access to services for patients with Dementia. We have reviewed and can confirm the information presented in the Quality Account appears to be accurate and fairly interpreted, from the data collected. However in order to give a balanced view we would wish to see information relating to learning from Serious Page 54 of 60 Incidents, and will be looking at patient flow and discharge processes through the agreed CQUINs. The Clinical Commissioning group looks forward to working with the organisation throughout the year to achieve more efficient integrated pathways delivering high quality services to patients, especially with community nursing teams. We are pleased to see that the priorities chosen for 2013/14 align with those of KCCG. In addition to those highlighted in the Account we would wish the organisation to also focus on the following that have not been selected as a priority: Patient flow through community hospitals, particularly delayed discharges Ensure relevant recommendations from the Francis report are embedded within the organisation. Page 55 of 60 5.0 Glossary A trust is an NHS organisation responsible for providing a group of healthcare services. An acute trust provides emergency and planned hospital services. Board of Peninsula Community Health The Board is accountable for setting the strategic direction of the organisation, CIC monitoring performance against objectives, ensuring high standards of corporate governance and helping to promote links between the organisation and the community. The Board has 10 members and includes the Chairman, Chief Executive, four Executive Directors and four Non-Executive Directors The Care Quality Commission (CQC) is the Care Quality Commission independent regulator of health and social care in England. It replaced the Healthcare Commission, Mental Health Act Commission and the Commission for Social Care Inspection in April 2009. The CQC regulates health and adult social care services provided by the NHS, local authorities, independent healthcare providers and voluntary organisations. Visit: www.cqc.org.uk Clinical audit measures the quality of care Clinical Audit and services against agreed standards and suggests or makes improvements where necessary These are organisations that buy services Commissioners of services on behalf of people living in a defined geographical area. They may purchase services for the population as a whole, or for individuals who need specific care, treatment and support. Healthcare services are commissioned by primary care trusts. Social services are commissioned by local authorities Commissioning for Quality and A report into the future of the NHS, entitles ‘High Quality Care for All’ 2008, included a Innovation (CQUIN) commitment to make a proportion of providers’ income conditional on quality and innovation. This is achieved through the Commissioning for Quality and Innovation Acute Trust Page 56 of 60 Complaint Department of Health Dignity Discharge Hospital Episode Statistics (HES) Information Governance Kernow Clinical Commissioning Group Local Involvement Networks (LINks) (CQUIN) payment framework. Visit www.dh.gov.uk This is an expression of dissatisfaction that can relate to any aspect of a person’s care, treatment or support. It can be expressed orally, through gestures or in writing. The Department of health is the department of the UK government responsible for policies on health, social care and the NHS (England only). Dignity is concerned with how people feel, think and behave in relation to the worth and value that they place on themselves and others. To treat someone with dignity is to respect them as a valued person, taking into account their individual views and beliefs. The point at which a patient leaves hospital to return home; or is transferred to another service: or the provision of a service is formally concluded. This is a data warehouse containing a vast amount of information on the NHS, including details on all admissions to NHS provider hospitals and outpatient appointments in England. HES is an authoritative sourced used for healthcare analysis by the NHS, government and many other organisations. Information Governance is concerned with the structures, policies and practices in place to ensure the confidentiality and security of health and social care service records. NHS Kernow is the clinical commissioning group for Cornwall and the Isles of Scilly. The Group is formed of 69 local practices who are themselves formed into locality groups. KCCG principal work is to buy health services on behalf of local people. LINks are comprised of individuals and community groups such as faith groups and residents associations, working together to improve local services. Their job is to find out what the public like and dislike about local health and social care, and then feed the views back to the people who plan and Page 57 of 60 National Confidential Enquiry into patient Outcome and Death - NCEPOD National Institute for Health and Clinical Excellence - NICE NHS Number Overview (OSC) and Scrutiny Committees Patient Patient Environment Action Teams PEATs Privacy and dignity run these services. They may talk directly to healthcare professionals about a service that is not being offered or make recommendations about an existing facility NCEPOD is an independent body concerned with maintaining and improving standards of medical and surgical care. It does this by reviewing the management of patients and undertaking confidential surveys and research, which are then published for the public’s benefit. NICE is an independent organisation responsible for providing national guidance on promoting good health and preventing and treating ill health This is the national unique patient identifier that makes it possible to share patient information across the whole of the NHS, safely, efficiently and accurately. Since January 2003, all local authorities with responsibilities for social care have had the power to review and report on local health services. Overview and Scrutiny Committees have taken on this role, and have been instrumental in helping to plan services and bring about change. They bring democratic accountability into healthcare decision-making and make the NHS more responsive to local communities. This is a person who receives health or social care through a regulated activity. Patients are defined ‘service users’ in the Health and Social Care Act 2008. PEAT is an annual inspection of inpatient facilities at healthcare sites across England with more than 10 beds. PEAT is selfassessed and inspects standards including food, cleanliness, infection control and patient environment. The scheme was established in 2000. It acts as a benchmarking tool to ensure that improvements are made in the non-clinical aspects pf a patient’s experience. To respect someone’s privacy involves recognising when they would like to be alone (or with family or friends), and Page 58 of 60 Providers VTE – Venous- Thromboembolism showing sensitivity to their wishes for a private conversation and preventing others from looking or listening in. To treat someone with dignity is to respect them as a valued person, taking into account their individual views and beliefs. Providers are the organisations that provide NHS services, for example NHS trusts, community interest companies, voluntary sector organisations. A venous thrombosis is a blood clot (thrombus) that forms within a vein. Thrombosis is a medical term for a blood clot occurring inside a blood vessel. A classical venous thrombosis is deep vein thrombosis (DVT), which can break off (embolize), and become a life-threatening pulmonary embolism (PE). The conditions of DVT and PE are referred to collectively with the term venous thromboembolism Page 59 of 60 6.0 Statement of Directors Responsibilities in Respect of the Quality Account The Directors are required under the Health Act 2009 to prepare a Quality Account for each financial year. The Department of Health has issued guidance on the form and content of annual Quality Accounts (which incorporates the legal requirements in the Health Act 2009 and the National Health Service (Quality Reports) Regulations 2010 (as amended by the National Heath Service (Quality Accounts) Amendments Regulations 2011). In preparing the Quality Account, directors are required to take steps to satisfy themselves that: The Quality Account presents a balanced picture of the Trust’s performance over the period covered The performance information reported in the Quality Account is reliable and accurate There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice The data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, and is subject to appropriate scrutiny and review; and The Quality Account has been prepared in accordance with Department of Health guidance The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Account. By order of the Board Michael Williams Helen Newson Chairman Interim Chief Executive Page 60 of 60