Quality Report 2012/2013 Page | 77

Quality Report
2012/2013
Page | 77
Page | 78
Birmingh am Women’s NHS Foundation Trust
Quality Report 2012/13
Contents Page
Part One
Statement on Quality from the Chief Executive of the Trust
Part Two
Priorities for improvement and statements of assurance
Participation in National Clinical Audits and National Confidential Enquiries
Recruitment into Research Studies
Use of CQUIN Framework
Care Quality Commission Regulations
Data Quality
Information Governance Toolkit
Clinical Coding Error Rate
Emergency Readmission within 28 days
Responsiveness to personal needs of patients
Recommending the Trust as a provider to Family and Friends
Patients admitted that are risk assessed for VT
Clostridium Difficile Infection
Patient Safety Incidents
Part Three - Other Information
Supplementary Indicators
Patient Safety
Clinical Effectiveness
Patient Experience
Quarterly of Quality Account Indicators
Genetics and Laboratories
Gynaecology
Maternity
Neonatology
Further National Indicators
Annexes
1. Statement from Commissioners
2. Statement of Directors responsibilities
80
101
102
103
104
96
96
96
97
98
100
82
89
94
95
106
106
107
108
114
114
115
116
117
118
119
121
Page | 79
Part 1
– Statement on quality from the Chief Executive of the Trust
Our Vision is:
“To be a leading provider of local, regional and national importance, providing a specialist range of distinct but interrelated services, delivering excellent healthcare, education and training and research and to contribute to th e health and wellbeing of the people we serve.”
Central to our vision is our commitment to improve patient care and the experience it brings
The purpose of this Quality Report is to demonstrate our view of the quality of the NHS services that we provide. The annual reporting guidance for Quality Reports details what we must include to fulfil both the
Department of Health and Monitor’s requirements.
We have set out in this report how we have performed in terms of priorities for improvement in the past year, and we have detailed what our priorities are for 2013/14. For the coming year we are proposing a new deliberately challenging indicator on multiple pregnancy rates. Real improvements in clinical outcomes will
Sub title Sub title Sub title Sub title Sub title
Our Governors have contributed to determining the key priorities for improvement and these have been discussed fully and agreed with our Members Council on 14/05/2013. The completion of the Quality Report has been led by the Trust’s Medical Director and Director of Nursing and Midwifery. However, the document has been developed through involvement with the Trust’s Clinical Directorates, Board of Directors and a number of organisations with whom the Trust works.
In all that we do in relation to quality, understanding patient experience and engaging with women and their families remains central. A new Patient Experience Strategy is being introduced in 2013/14 with a focus on makin g sure the patient’s voice is heard and the patient experience is paramount in helping us make decisions on how to improve what we do as well as designing new services. Our Trust has also just completed a pilot of customer experience training and trained a number of Customer Care Champions. Our Trust is implementing the new Friends and Family Test regime building on our results from last year that are shown in this report.
We actively seek real time feedback from users of all of our service by phone, web and in person. We invite complainants to come in and feedback to staff directly and using the Governors to help us observe care in our clinical area. We have extended the Patient Story to Board initiative to include new ways for patients to record their stor ies for the board to hear if they can’t attend in person.
We are putting all our Sisters, Matrons and Heads of Nursing and Midwifery back into uniform and making sure they are highly visible in all clinical areas so patients can identify and contact them. We have also introduced care rounds on every shift in each clinical area to ensure that patients see and talk to the nurse or midwife in charge of the area and discuss their care needs. Our Director of Nursing and Midwifery and I also do care rounds across a variety of clinical areas in the Trust on a weekly basis in addition to the rest of the
Board doing Walkabouts on a monthly basis.
As a Trust, we are firmly committed to combating healthcare acquired infections (HCAIs) and have in place a
Trust-wide strategy to ensure that our excellent track record is maintained. We have continued to have positive results from the environmental inspections of our hospital.
The Trust is required to register with the Care Quality Commission and its current registration status is registered without conditions. We participated in three special reviews or investigations by the Care Quality
Commission during 2012/13 and in all three we were found to be fully compliant with the standards required.
Page | 80
No document that refers to Quality in the NHS in 2013 is complete without reference to The Mid Staffordshire
NHS Foundation Trust Public Inquiry chaired by Robert Francis QC. Our Trust is developing a full and detailed response to each of the relevant recommendations following the Government’s response. This is being carried out by the Executive team with the input of the Clinical Governance, Informatics and Human
Resources functions. The final response will be shared through the Patient Outcome Committee as the Board
Sub-committee responsible for clinical safety, risk and governance matters. It will then be presented to the
Board of Directors in autumn 2013. The Trust will share its findings and plans this with its governors, commissioners and other identified partners. The response will be published as required by the end of 2013.
This Quality Report sets out our achievements and also our ambitions to continue to be a leading provider of local, regional and national importance. I am satisfied that our report fairly reflects the quality of services we provide, and that the information that supports the document is correct and auditable.
Professor Ros Keeton May 2013
Chief Executive
Page | 81
Part 2 – Priorities for improvement and statements of assurance from the board
Update on Quality Accounts 2012-13 and Main Priorities for 2013-14
This represents our third set of Quality Accounts at Birmingham Women’s Hospital NHS Foundation Trust
(BWNFT or the Trust). In the previous two reports we have kept the same main priorities, however after discussion amongst the clinicians it was proposed to discontinue the indicator regarding actions being completed on time following serious incidents. The reason for this is that whilst we remain dedicated to completing these actions in a timely fashion we believe that the good year on year performance on this has resulted in it being superseded by other priorities within the Trust. Therefore we have replaced this with the aim of achieving multiple pregnancy rates at or below the target of 12% for the coming year. Our other 2 main priorities have not reached our targets and therefore remain clinical priorities.
The Management Board of the Trust and the Board of Directors have agreed to these changes. We have initially discussed this with our Governors, who include members of staff and patients, and have then formally discussed these at Members Council, which includes representatives of our wider constituency. At this meeting they were made aware of the rationale of maintaining two of our previous priorities and elevating the multiple pregnancy rate to a main priority.
Performance of Quality Priorities from 2012/13
Priority 1 - To aim to improve the detection rate of intrauterine growth restriction (IUGR) to 35%
Perinatal mortality has long been recognised as being high in the West Midlands, whilst this is partly accounted for by the population we serve a recurrent theme in our investigation of perinatal deaths is the failure to detect fetal growth restriction. In light of this we have in the past and continue to give a high priority to the detection of IUGR.
This last year we have implemented all the planned initiatives in our previous report with the exception of investigating the benefits of using the first trimester biochemical screening results for trisomy 21 as an additional risk factor for IUGR. These initiatives are listed below:
The Day Assessment Unit will move to a new purpose built facility that is co-located with Triage and
Delivery Suite
The administrator of the Guardian System taking up post and their role in developing the electronic record, aiding real time data collection.
Constant reminders to appropriate clinical staff regarding continuing growth scans until delivery rather than stopping at 36 weeks of gestation, an important change in practice
Increase direct access from community midwives to the Day Assessment Unit, facilitating rapid assessment
Increase the number of midwives and doctors able to perform growth scans out of hours
Re-examine the criteria for serial growth scans
Investigate the benefit of using the results of first trimester biochemical screening for trisomy 21 as an additional risk factor for IUGR
Despite this, as can be seen below, progress on this important indicator has been disappointing. Indeed the dete ction rates appear to have fallen, with a detection rate of 26% for quarter 4, though March’s data showed a 31% detection rate. In light of this we have returned to basics to examine how the original data collected by the perinatal institute was classified and it appears that for the period prior to April 2012 all babies in whom
IUGR was suspected at any point were classified as detected by the Perinatal Institute, regardless of whether subsequent tests resulted in reassuring results. This obviously leads to a higher detection rate than our present definition where only babies that are managed as being growth restricted are included within our group of detected babies. Whilst this gives a lower detection rate it is, we believe, a more realistic assessment of our clinical detection rate of this condition. For the purpose of our present data collection the definition of detection is antenatally predicting babies whose customised both weight is below the 10 th
centile.
Page | 82
2013-14 Initiatives
We therefore plan to continue with this data collection over the coming year and as well as continuing to remind people of appropriate guidelines our initiative for the coming year will be:
To improve the accuracy of the electronic data collection enabling rapid identification of changes in the detection rate enabling focused training to occur
Quality control of ultrasound images used for the estimated fetal weight calculation
Further dissemination of these results to a wider audience, published on trust internet page since Q3
2012/3
Compare practice with recently published Royal College of Obstetricians guidelines
Further Trusts to be contacted to develop a wider base of benchmarking data.
Table 2.1 Percentage Detection Rates of Intrauterine Growth Restriction
Date
Q1-3
09-10
Q4
09-10
10-11 Jan
12
Q1
12-13
Q2
12-13
Q3
12-13
Q4
12-13
West
Mid
10-11
%
Detected
26 31 33 28 18 26 21 26 31
*Please note that data for 11/12 was only available for the month of January 2012 due to problems with data collection, see last year’s accounts.
Monitoring
These results will continue to be monitored by the Clinical Lead for the Day Assessment Unit and the Maternity
Services Directorate, being measured electronically and at least in the first quarter validated by manual audit.
The results will be reported to the Patient Outcomes Committee on a quarterly basis and will be published on a quarterly basis on the Trust’s Quality Dashboard. In addition, as the electronic data collection becomes more robust, this will enable the lead for the Day Assessment Unit to receive rapid feedback.
The Medical Director is the executive sponsor for this metric.
Page | 83
Priority 2 – To ensure that actions are completed on time following Serious Incidents
At BWNFT, as with many other organisations within the NHS, the reporting culture of adverse incidents and the standard of investigation of these is constantly improving. This is generally perceived to be a good thing and organisations with higher reporting rates are considered to be indicative of an open and learning culture.
We felt that examining the proportion of recommendations that have been implemented on time as a result of investigating these incidents is a valuable indicator of the responsiveness of our service to the inevitable incidents that will occur in a complex health care system.
This indicator applied to all directorates and the achievement in each directorate can be seen in Tables 3.9-
3.12. This year we increased our target from last year’s achievement of 88% to 93% by end of Q4 2012/13, a
5% increase. Overall the Trust completion of actions on time for the year was 92.3% (192 of 208 actions). For
Q4 there were only 2 directorates with actions to complete and between them all but one was completed on time, giving a completion of 93.3%. It is for this reason that for future years we opted to continue this metric as part of our additional reporting, not as one of our three main priorities.
Table 2.2 % of Actions Completed on Time
Directorate % Actions Completed on Time
2010/11
Genetics and Labs 80
2011/12
100
Q4 2012/13
Nil relevant
2012/13
75
Gynaecology
Maternity
Neonatology
75
82
85
100
86
98
Nil relevant
100 (7 of 7)
88 (7 of 8 actions)
100
92
90
Total
Monitoring
82 88 93.3 92.3
Although no longer a quality priority we will continue to monitor the performance by directorate on this standard through their quarterly reporting to the Patient Outcomes Committee.
Priority 3 – Increasing the percentage of nursing and midwifery time spent delivering direct care.
This is an important measure for the Trust. It assures us that despite the many and varied tasks nurses and midwives carry out during their busy day, that direct patient care remains their focus. It is audited on a monthly basis using a “time and motion study”. a proforma which was developed nationally as one of the tools for the Productive Ward, is completed, which calculates the percentage of time spent on what it classifies as either “direct / indirect care” a recognised audit tool developed for this purpose.
Evidence shows that higher percentages of direct care improve:
Efficiency of care.
Patient experience.
Safety and reliability of care
Staff well-being and satisfaction with the job they do.
The Trust has been working to improve this percentage continuously so it is disappointing to see a decline in the percentage of time achieved in a number of the clinical areas.
However, this has prompted a Trust wide review of the time spent delivering direct care undertaken by the
Director of Nursing and Midwifery and assisted by the Heads of Nursing and Midwifery. This measure and associated activities will be the subject of a practice improvement project undertaken in conjunction with the
Institute of Healthcare Improvement (IHI).
In the Midwifery Directorate we have increased the numbers of midwives as a result of a skill mix review
(Birthrate Plus) and in 2013/14 will meet the recommended national ratio of 1:28 midwives to women. We are one of the first Trusts to do this and we believe that this, coupled with the improvement work we do, will improve this percentage during the next year.
Page | 84
In the Neonatal Directorate we have also recruited more nurses and have introduced a rolling recruitment and retention programme to ensure consistent levels of skilled neonatal nurses. We are also introducing a new
Matrons post to help focus on family orientated nursing care.
In the Gynaecology Directorate we have reviewed the way the Sister and Shift Co-ordinator roles work and have introduced initiatives to increase the time nurses can spend on direct patient care. We have also looked at the activities carried out by nurses that are not collected as direct patient care, but should be included, such as the telephone advice and support we offer our patients pre and post discharge. We will also evaluate the impact the electronic patient care records are having on direct patient care to ensure that the nurses are not spending excessive time away from the patient bedside to complete the electronic documentation.
Table 2.3 % of direct nursing and midwifery care.
2012/13
Indicator Target
2011 -
12
Q1 Q2 Q3 Q4
2012-
13
RAG status for year
Gynaecology –
Wards 7 and 8
55% 43.5% 45% 43% 42% 39%
42.5%
Maternity
Ward 1 55% 40.5% 40% 28% 55% 56% 44.75%
Postnatal floor 55% 56% 58% 66% 62% 69% 63.75%
Delivery Suite 55% 58% 44% 69% 79% 79% 67.75%
Neonatal 55% 46.5% 44% 47% 30% 44% 42%
2013-14 Initiatives
Skill mix reviews of nursing and midwifery staff twice a year
Introduction of care rounds in all ward areas
Sisters becoming supervisory in clinical areas
Evaluate the impact of electronic patient care records on time spent on direct patient care
Improvement Project with IHI to improve the nursing and midwifery activity flow to increase the percentage of time spent on direct patient care
Monitoring
These results will continue to be monitored by the Professional Heads of Nursing and Midwifery as well as the
Director of Nursing and Midwifery. The results will be reported to the Patient Outcomes Committee on a quarterly basis and wil l be published publicly on a quarterly basis on the Trust’s Quality Dashboard.
The Director of Nursing and Midwifery is the executive sponsor for this metric.
Page | 85
Main priorities for 2013-14
For the year 2013-14 our three main priorities will be:
1. To aim to improve the detection rate of intrauterine growth restriction to 35% see above
2. To achieve a multiple pregnancy rate at or below the target of 12%
3. To increase the percentage of nursing and midwifery time spent delivering direct clinical care from the benchmark figure, see above
We have already described our plans for priorities 1 and 3. Listed below is the plan for our new clinical effectiveness priority for 2013/14.
Priority 2 – Achieve multiple pregnancy rates at or below the target of 12%
The multiple pregnancy rate is defined by the number of pregnancies with more than one fetal heart identified on ultrasound scan following in vitro fertilisation (IVF) or intracytoplasmic sperm injection (ICSI) as a percentage of the total number of pregnancies from IVF and ICSI for the given time period.
Multiple pregnancy is a major risk factor for perinatal mortality and morbidity. In recent years the Human
Fertilisation and Embryology Authority, HFEA have set a target for the rate of multiple births. This rate has been decreasing year on year and from this year will remain static at 10%. A problem of assessing service changes against a multiple birth rate is that there will be a significant time lag between changes in the processes of assisted conception and birth.
At the present time the additional target we have set ourselves is the rate of multiple pregnancies which is more stringent and also more timely in that changes in practice will result in changes in multiple pregnancy rates before the necessary time delay prior to delivery and hence multiple birth. The multiple pregnancy rate will always be higher than the multiple birth rate due to the higher pregnancy loss rate in women with multiple pregnancies. This year’s result of 14% means we have not achieved our ambitious target of 12%; however we did improve our pregnancy rate, see Part 3. In the coming year we aim to decrease our multiple pregnancy rate to 12% whilst maintaining our excellent pregnancy rates.
Table 2.4 Performance against HFEA Target for Multiple Pregnancy
Year* HFEA Target** BWH Fertility Centre Actual***
2009/10
2010/11
2011/12
2012/13
24%
20%
15%
10%
19%
17%
13%
14%*
Page | 86
Table 2.5 Multiple Pregnancy rate by quarter
2011-12 Quarter 1
Quarter 2
Quarter 3
Quarter 4
2012-13 Quarter 1
Quarter 2
Quarter 3
Quarter 4
Multiple Pregnancy Rate %
10
4
12
15
13
22
13
17*
* April to March, except for 2012/13 where the March data is not yet available
**Multiple Birth rate target, most recent target began in Oct 2012
***Multiple Pregnancy Rate
2013-14 Initiatives
In order to reduce the multiple pregnancy and live birth rate while maintaining or improving the pregnancy rate the Fertility team will introduce the following initiatives to increase the uptake of singe embryo transfer:
1. Increase the blastocyst culture and transfer rate to help select the most suitable embryo
2. Patients where the female partner is less than or equal to 37 years will have single embryo transfer if one or more top embryos are available, in both their first and second attempt (cf applied to first attempt only at present)
3. Where the female partner is more than 37 years but less than 40 years, single embryo to be transferred if one or more top quality embryo is available for transfer in their first attempt (double embryo transfer at present)
4. Single embryo transfer in all egg donation cycles if one or more top grade embryos available (new criteria)
5. Single embryo transfer in all cases of blastocyst transfer of top grade in a frozen cycle (new criteria).
The principal driver to achieve the multiple pregnancy target while maintaining the pregnancy rate is to select the best embryo by greater application of blastocyst culture and transfer.
Monitoring
This metric is monitored on a monthly basis via the performance report and on a quarterly basis will be reported to the patient outcomes committee.
The Medical Director is the executive sponsor of this indicator.
Page | 87
Statements of assurance from the board
During 2012/13 the Birmingham Women’s NHS Foundation Trust provided and/or sub-contracted 11 relevant health services.
The Birmingham Women’s NHS Foundation Trust has reviewed all the data available to them on the quality of care in 11 of these relevant health services. The data reviewed covered all there dimensions of quality and where data collection has impeded this it has been mentioned in the relevant part of the report.
The income generated by the relevant health services reviewed in 2012/13 represents 100 per cent of the total income generated from the provision of relevant health services by the Birmingham Women’s NHS Foundation
Trust for 2012/13 .
Table 2.6 Planned Income by Speciality
Service 12/13 Planned Income (£)
Maternity
Fetal Medicine
Clinical Genetics
31,073,508
3,408,669
4,675,538
Laboratory Genetics
Gynaecology
Fertility Care
Neonatal Services
Neonatal Transport
Imaging
Pathology & Lab Services
Physiotherapy
6,585,558
11,220,047
1,182,500
10,936,047
1,570,950
289,615
1,931,341
183,060
Page | 88
Participation in clinical audits and national confidential enquiries
During 2012/13 four national clinical audits and two national confidential enquiries covered relevant health services that BWNFT provides.
During 2012/13 BWNFT participated in three (75%) national clinical audits and two (100%) national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in.
The national clinical audits and national confidential enquiries that BWNFT was eligible to participate in during 2012/13 are as follows:
Blood Sampling and Labelling (National Comparative Audit of Blood Transfusion)
National Pregnancy in Diabetes (NPID) Audit. This data collection is on-going and will be reported in next year’s accounts when completed
National Cardiac Arrest Audit (NCAA)
Neonatal intensive and special care (National Neonatal Audit Programme)
Maternal, infant and newborn programme (MBRRACE-UK)
Medical and Surgical programme: National Confidential Enquiry into Patient Outcome and Death
(NCEPOD) o Subarachnoid Haemorrhage
The national clinical audits and national confidential enquiries that BWNFT participated in during 2012/13 are as follows:
Blood Sampling and Labelling (National Comparative Audit of Blood Transfusion)
National Pregnancy in Diabetes (NPID) Audit on-going data collection to be completed by January
2014
Neonatal intensive and special care (NNAP)
Maternal, infant and newborn programme (MBRRACE-UK)*
Medical and Surgical programme: National Confidential Enquiry into Patient Outcome and Death
(NCEPOD) o Subarachnoid Haemorrhage
The Trust did not participate in the National Cardiac Arrest Audit (NCAA), as there are very few incidents that meet the inclusion criteria, and the participation fee would not provide value for money for the Trust. An in house audit report is produced on a monthly basis, and the Trust also participated in the NCEPOD Cardiac
Arrest Study for Hospitals (report received July 2012).
The national clinical audits and national confidential enquiries that BWNFT participated in, and for which data was completed during 2012/13, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry:
Page | 89
Table 2.7 Participation in National Clinical Audit / Confidential Enquiry
National Clinical Audit /
Confidential Enquiry
Cases Submitted
(Number/Percentage Reported)
Blood Sampling and
Labelling (National
Comparative Audit of Blood
Transfusion)
Neonatal intensive and special care (NNAP)
1 (100%) organisational survey
100% laboratory error logs for May
23 (100%) follow-up interviews
1436/1436 (100%)
– July 2012
Maternal, infant and newborn programme (MBRRACE-UK)
These criteria for the National
Confidential Enquiry changed in January 2013 and for clarity we have included the same definitions for the entire financial year 2012/13, allowing benchmarking in subsequent years to be more applicable.
1 (100%) maternal death (death of pregnant women and women up to one year following the end of the pregnancy (regardless of the place and circumstances of the death)).
8 (100%) late fetal loss (the baby is delivered showing no signs of life between 22+0 and 23+6weeks of pregnancy) 3 of these cases were terminations of pregnancy
35 (100%) stillbirths (the baby is delivered showing no signs of life after 24+0 weeks of pregnancy) 4 of these cases were terminations of pregnancy
41 (100%) neonatal deaths (death of a live born baby
(born at 20 weeks gestation of pregnancy or later or
400g where an accurate estimate of gestation is not available) occurring before 28 completed days after birth) 2 of these cases were terminations of pregnancy
2 (100%) post-neonatal deaths (occurring from the 28th day and before 1 year after birth of infants who have not been discharged from the neonatal unit).
0/0 cases submitted Medical and Surgical programme: National
Confidential Enquiry into
Patient Outcome and Death
(NCEPOD):
Subarachnoid
Haemorrhage
Page | 90
The reports of four national clinical audits were reviewed by the provider in 2012/13 and BWNFT intends to take the following actions to improve the quality of healthcare provided:
Table 2.8 National Clinical Audit Reports Reviewed
National Clinical Audit Action
NCEPOD Cardiac
Arrest Procedures:
Time to Intervene?
(June 2012)
Heavy Menstrual
Bleeding 2 nd
Annual
Report (July 2012)
This report was received by the Clinical Governance Committee on 6 th
July 2012.
The Trust intends to take the following actions:
Revise Do Not Attempt Resuscitation Policies and Resuscitation
Procedures
This report was received by the Clinical Governance Committee on 3rd
August 2012.
The Trust intends to take the following actions:
Neonatal intensive and special care (NNAP)
Data Completeness
Report 2012 (July
2012)
Participate in a case-note review of 20 patients to validate the quality and completeness of patient-reported as well as administrative data
Review internal resources available for national audits to improve response rates for future audits
This report was received by the Clinical Governance Committee on 3
August 2012.
The Trust has taken / intends to take the following actions: rd
Bedside Transfusion
(National Comparative
Blood Transfusion
Audit)
Q1: 34/35 babies have valid data. This reflects considerable input during the year with monthly walkabout clinical governance and case note rounds, educating nursing staff about the importance of completing paperwork later relied on for the Badger summaries and datasets (including this item on recording baby’s first temperature).
Q2 (antenatal steroids) data completeness for the year is 98%.
(129/132) This is a considerable improvement and reflects educational processes to junior staff.
Q3 (ROP screening.) This is recorded at 60%. Actual figure is much higher (98%) as discussed later in report.
Q4 (mothers milk on discharge) Data completeness is 100%.
Q5 (documented consultation with parents). The data completeness for the year is 79% up from 73% last year. This reflects nursing and medical staff education.
Q6-9: N/A
Q10: (encephalopathy, daily consciousness and tone recording) very wide variability in results for NICUs (0% to 100%). BWNFT are benchmarked in the middle.
This report was received by the Hospital Thrombosis and Transfusion
Committee on 22 nd
April 2013.
The Trust intends to take the following actions:
2 patients were not issued with identification wristbands and one patient with a wristband did not have a date of birth recorded on it.
Feedback will be provided to staff and a re-audit carried out in 2013.
Page | 91
The reports of 342 local clinical audits were reviewed by the provider in 2012/13 and BWNFT has taken / intends to take the following actions to improve the quality of healthcare provided:
Table 2.9 Local Clinical Audits Reviewed
Local Clinical
Audits
Actions
Genetics and
Laboratories
Directorate
Gynaecology
Directorate
239 local audits were completed during 2012-13.
A sample of actions the Directorate intends to take / have taken are as follows:
A variety of Standard Operating Procedures (SOPs) are to be updated
As a result of the audit of screening for Downs Syndrome requestors are now informed of incomplete request forms prior to sample analysis
Fibronectin Analyser Usage in Triage:
Staff trained in April 2012,
Give users barcodes to use as their user ID,
Keep a log book next to the fibronectin analyser to record all information regarding patient testing, quality control, lot numbers, problems and troubleshooting,
Laboratory involvement required,
Produce a new standard operating procedure
Pathology Quality Management Audits:
138 audits completed. 277 non-compliances identified of which 18 remain open.
Regional Genetics Laboratories Quality Management System Audits:
85 Audits completed. 58 non-compliances identified of which 25 remain open.
31 local audits were completed during 2012-13.
A sample of actions the Directorate intends to take / have taken are as follows:
World Health Organisation Checklist Audit:
due to poor compliance with full completion of form monthly reporting instigated. 100% of cases audited in March 2013 had a checklist and 100% of checklists used were fully completed. This covered both gynaecology and maternity
Emergency Readmissions:
Incident form now completed for all readmissions
Infection control team review care during first admission of all patients readmitted with potential or actual wound infection.
Infection Control audits:
Instant referral to estates department to undertake environmental repairs: paintwork, cleaning of fans, ceiling ducts
Replacement of covers or mattresses undertaken as necessary but also monitored regularly when making beds.
Equipment / bed spaces now clearly marked when cleaned and ready for use on next patient.
Flooring replaced in inpatient ward kitchens and gynaecology wards
Page | 92
Local Clinical
Audits
Actions
Gynaecology
Directorate
Maternity
Services
Directorate
Neonatal
Directorate
Perioperative Hypothermia:
Undertaken in response to National Institute of Clinical Excellence
Technological Appraisal of use of Inditherm Mattress in preventing inadvertent perioperative Hypothermia. Prospective monitoring of patient temperatures did not show any significant difference when using Inditherm mattress. Results did not support changing current practice.
54 local audits were completed during 2012-13.
A sample of actions the Directorate intends to take / have taken are as follows:
Various amendments made to the electronic clinical record and paper proformas/documentation to improve record keeping and quality of care:
Develop an electronic, user friendly, partogram with K2. In the interim, feedback to staff the importance of recording regular maternal observations on the paper partogram.
Development of a ‘commencement of Cardiotocograph, CTG, screen’ screen, to include reason for CTG, fetal heart with doppler and maternal heart rate.
Fetal Blood Sampling, FBS, screen on K2 to be amended to make easier to document timing of next review and time sample obtained. Remind staff to always use the FBS screen.
Current commencement of oxytocin screen on K2 needs amending to reflect current guideline and practise.
The vaginal birth after caesarean section, VBAC, guideline and Antenatal
VBAC proforma amended to clarify what must be included in a management plan should labour occur early or not as planned.
Update current patient handling form and raised Body Mass Index Antenatal proforma to reflect the guideline.
External cephalic version, ECV, proforma to be developed to prompt promotion of pros and cons of ECV and correct counselling re: ECV.
Induction of Labour, IOL:
New IOL pathway developed by multi-disciplinary team to aid documentation.
This was launched in September 2012. Pathway to be replicated on the K2 electronic system in the future.
Maternal Early Warning Score (MEWS):
Antenatal MEWS chart to be amended to assist staff in identifying the frequency of observations for common conditions of pregnancy. Frequency of observations for postnatal women to be added to the transfer page of the postnatal notes.
18 local audits were completed during 2012-13.
A sample of actions the Directorate intends to take / have taken are as follows:
Audit on Therapeutic Hypothermia in Hypoxic Babies:
- Improve staff education on cooling criteria and importance of passive cooling
- Ensure that all cooled babies get their Magnetic Resonance Imaging in the specified timescale
Page | 93
Local
Clinical
Audits
Actions
Neonatal
Directorate
- Improve electronic patient documentation on Badger particularly about the resuscitation and passive cooling information
The Unexpected Admissions Audit found some babies were admitted to the
Neonatal Intensive Care Unit, NICU for hypothermia. Actions taken / planned in conjunction with the Maternity Directorate include:
- Hats requested for babies on Delivery Suite
- Thermometer used for the newborn temperature after one hour is now given to the woman to keep.
- Review the record keeping around skin to skin care and newborn temperature and respirations following the introduction of a revised labour and delivery record.
Support for Parents:
- Support for Parents pack to be reviewed to ensure correct information is given to parents.
- Leaflets for many conditions are available in the filing cabinet, staff to be made aware of what information is where and importance of documenting when it is given to parents.
- Pink sheets to be signed re the provision of information leaflets to parents within 48 hours of admission by nurses and parents.
- Welcome Meetings commenced for parents to give them information and an opportunity to go through the pink sheets.
Feeding Guidelines Audit:
- Laminated nutrition flow charts and volumes of feed increases charts to be put in blue nursing folders
- Encourage mothers to begin expressing on day of delivery.
Feeding co-ordinator to become more involved in this where appropriate.
Recruitment into research studies
The number of patients receiving relevant health services provided or sub-contracted by BWNFT in 2012/13 that were recruited during that period to participate in research approved by a research ethics committee was
2662. This compares to last year’s figure of 1923, showing an improved recruitment.
Page | 94
Information on the use of the CQUIN framework
A proportion of Birmingham Women’s NHS foundation Trust income in 2012/13 was conditional upon achieving quality improvement and innovation goals agreed between Birmingham Women’s NHS foundation
Trust and any person or body they entered into a contract, agreement or arrangement with for the provision of relevant health services, through the Commissioning for Quality and Innovation payment framework.
Further details of the agreed goals for 2012/13 are available online at: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics
/Publications/PublicationsPolicyAndGuidance/DH_091443 https://www.gov.uk/government/publications/using-the-commissioning-for-quality-and-innovation-cquinpayment-framework-guidance-on-new-national-goals-for-2012-13
Further details for the following 12 month period are available online at: http://www.england.nhs.uk/wp-content/uploads/2013/02/cquin-guidance.pdf
The total value of the income due to CQUIN payments for 2012/13 is £1,736,592. The value achieved for
11/12 that was conditional upon achieving quality improvement and innovation goals was £987,711.
Care Quality Commission Regulations
BWNFT is required to register with the Care Quality Commission and its current registration status is registered without conditions.
The Care Quality Commission has not taken enforcement action against BWNFT during 2012/13.
BWNFT has participated in three special reviews or investigations by the Care Quality Commission relating to the following areas during 2012/13:
Table 2.10 CQC special reviews or investigations
Special Review /
Inspection
Standard(s) Reviewed Outcome
Termination of
Pregnancy
Routine Inspection
Cause for Concern
Inspection
Outcome 21: Records Compliant – no actions required
Outcome 02: Consent to care or treatment
Outcome 04: Care and welfare of people who use services
Outcome 09: Management of medicines
Outcome 14: Supporting workers
Outcome 17: Complaints
Compliant – no actions required
Outcome 6: Co-operation with other providers
Compliant – no actions required
Outcome 16: Assessing and monitoring the quality of service provision
Page | 95
Data Quality
NHS Number and General Practitioner Registration Code Validity
Birmingham Women's NHS Foundation Trust submitted records during 2012/13 to the Secondary Uses
Service for inclusion in the Hospital Episode Statistics which are included in the latest published data. The percentage of records in the published data:
which included the patient ’s valid NHS number was: o 99.53% for admitted patient care o 99.68% for outpatient care; which included the patient’s valid General Practitioner Registration Code was: o 98.3% for admitted patient care; o 99.2% for outpatient care.
The percentage for Accident and Emergency care is not Applicable to the Trust
Information Governance Toolkit attainment levels
Birmingham Women's NHS Foundation Trust's Information Governance Assessment Report score for 2012/13 was 75% and was graded Green - satisfactory.
All require ments met the minimum target Level 2 resulting in a ‘Satisfactory’ score. There was an overall percentage rise from 71% obtained in 2011/12 to 75% in 2012/13, reflecting movement of 4 requirements from
Level 2 to Level 3.
The Trust is undertaking a number of actions to improve and maintain this score:
review business continuity plans and procedures in detail and audit actual compliance.
develop a training plan to ensure IT training is delivered more evenly through the year, thereby reducing the risk on the existing year end rush.
strengthen evidence re the disposal of records to ensure Trust wide compliance with the Records
Management NHS Code of Practice 2006.
continue records review & update evidence so that ALL corporate areas have been audited and a complete inventory has been created which is actively managed.
Page | 96
Clinical coding error rate
Birmingham Women's NHS Foundation Trust was not subject to the Payment by Results Clinical Coding
Audit during 2012/13 by the Audit Commission.
However the Trust did invite an external auditor to conduct an audit in line with the requirements of the
Information Governance Toolkit. They have found the following:
Overall HRG error rate 0.78%
Primary Diagnoses Incorrect 4%
Secondary Diagnoses Incorrect 2.1%
Primary Procedures Incorrect 2.04%
Secondary Procedures Incorrect 1.43%.
These figures should not be extrapolated beyond the sampled services. Coverage of the sample included maternity and gynaecology services only.
Birmingham Women's NHS Foundation Trust will be taking the following actions to improve data quality:
1. Increase the remit of the Data quality group to include all information systems in the Trust
2. Increase the number of data quality indicators for reporting to senior executives and managers within the organisation
3. Use externally generated data quality reports and benchmarking data to improve local quality, and create appropriate plans to manage any issues
4. Continue to run monthly workshops that highlight data quality issues and the underlying processes that drive incorrect data capture.
5. Continually update all policies and procedures that identify good practice with regard to data capture and quality.
6. Create tools to enable users to identify and log errors and manage data quality issues locally and feed these into the incident reporting and risk management systems
Data made available via the Health & Social Care Information Centre
Below follows a series of indicators benchmarked against other Trusts. In some cases only historical data is available for benchmarking.
Summary Hospital-Level Mortality Indicator (SHMI)
As specified in January 2013 by the Information Centre for Health and Social Care, specialist Trusts, such as
BWNFT are exempt from this indicator.
Page | 97
Emergency readmissions to hospital within 28 days of discharge from hospital
The data made available to the NHS foundation trust by the Health and Social Care Information Centre with regard to the percentage of patients aged –
(i) 0 to 14; and
(ii) 15 or over, readmitted to a hospital which forms part of the Trust within 28 days of being discharged from a hospital which forms part of the trust during the reporting period.
Numerator
The number of finished and unfinished continuous inpatient spells that are emergency admissions within 0-27 days (inclusive) of the last, previous discharge from hospital (see denominator), including those where the patient dies, but excluding the following: those with a main speciality upon readmission coded under obstetric; and those where the readmitting spell has a diagnosis of cancer (other than benign or in situ) or chemotherapy for cancer coded anywhere in the spell.
Denominator
The number of finished continuous inpatient spells within selected medical and surgical specialities, with a discharge date up to March 31 st
within the year of analysis. Day cases, spells with a discharge coded as death, maternity spells (based on speciality, episode type, diagnosis), and those with mention of a diagnosis of cancer or chemotherapy for cancer anywhere in the spell are excluded. Patients with mention of a diagnosis of cancer or chemotherapy for cancer anywhere in the 365 days prior to admission are excluded.
The BWNFT considers that this data is as described for the following reasons;
the rate of readmission of people aged <16 shows a slight increase from 2008/9, though a fall from
2011/12. This appears to be within the normal range of readmissions and the total number of these cases per year is approximately 10.
For people aged 16 and over our readmission rates are similar to the average for all Trusts and Acute specialist Trusts. Please note that the Trust data for 2011/12 and 2012/13 has not been standardised for age and sex by the Social care Information Centre, though we do not expect this to change the data significantly.
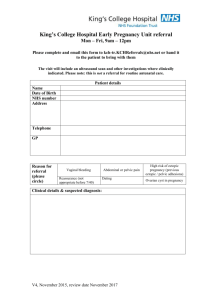
The BWNFT has commenced the following actions to improve this readmission rate;
Provide all gynaecology patients discharged with a contact number to telephone should they have concerns following discharge
Engage in a pilot electronic discharge summary for patients attending the early pregnancy assessment unit
Page | 98
Table 2.11 Emergency readmissions to hospital within 28 days of discharge from hospital: patients of ages
<16
BWNFT
Average
Acute
Specialist
Highest
Acute
Specialist
2012/13
Not available
Not
10.0 available
2011/12
14.3
Not available
Not available
Lowest Acute
Specialist
Average All
Trusts
Not available
Not available
Not available
Not available
Not available
Highest All
Trusts
Not available
Lowest All
Trusts
Not available
Data Standardised to persons 2006/07
Not available
2010/11
6.72
19.84
139.83
0
10.15
128.16
0
2009/10
8.52
6.83
49.28
0
10.18
76.29
0
2008/09
7.29
7.12
28.95
0
10.09
29.85
0
Table 2.12 Emergency readmissions to hospital within 28 days of discharge from hospital: adults of ages 16+
BWNFT
Average
Acute
Specialist
Highest
Acute
Specialist
2012/13
Not
Not
10.7 available available
Lowest Acute
Specialist
Not available
2011/12
11.1
Not available
Not available
Not available
Average All
Trusts
Highest All
Trusts
Not available
Not available
Not available
Not available
Lowest All
Trusts
Not available
Not available
Data Standardised to persons 2006/07
2010/11
9.98
8.75
15.33
0
11.42
53.31
0
2009/10
11.92
8.55
12.85
0
11.16
42.22
0
2008/09
11.08
8.89
13.43
0
10.9
218.67
0
Page | 99
Responsiveness to the personal needs of its patients
The data made available to the NHS foundation trust by the Health and Social Care Information Centre with regard to the trust’s responsiveness to the personal needs of its patients during the reporting period
The BWNFT considers that this data is as described for the following reasons;
This is based on five questions within the national inpatient survey which are combined to give a composite score. It covers the following areas;
1. involvement in decisions re care and treatment,
2. finding people to talk to about worries and fears,
3. privacy when discussing treatment
4. information re medication side effects on discharge
5. were you told who to contact after discharge if you were worried about your condition
In the last year we have improved significantly on three of these and worsened slightly on two. For details of this please see below.
The BWNFT has commenced the following actions to improve this;
The importance of privacy when discussing medical treatments will be stressed in all medical staff appraisals
We are considering including the question regarding side effects of medication within our local surveys next year and the CCG have suggested asking patients to sign that they have had this information at the time of discharge
Future estates developments are being considered and a high priority will be given to the importance of privacy in any new designs
Table 2.13 Responsiveness to the personal needs of its patients
BWNFT
Average SHA
2012
77.1
Highest SHA
Lowest SHA
67.7
79.5
62.1
Average All England 68.1
Highest All England -
Lowest All England -
2011
73.8
67.5
-
-
67.4
85
56.5
2010
75.6
67.2
-
-
67.3
82.6
56.7
The individual questions that were involved in compiling this score are listed below along with their individual scores.
Q32 Were you involved as much as you wanted to be in decisions about your care and treatment?
Q34 Did you find someone on the hospital staff to talk to about your worries and fears?
Q36 Were you given enough privacy when discussing your condition or treatment?
Q56 Did a member of staff tell you about medication side effects to watch for when you went home?
Q62 Did hospital staff tell you who to contact if you were worried about your condition or treatment after you left hospital?
Page | 100
2.14 The individual question scores for BWNFT are as follows:
Trust code SHA name
SHA cluster
Year Q32 Q34 Q36 Q56 Q62 CQUIN
RLU
WEST
MIDLANDS
SHA
Midlands and
East
2012
2011
86.1
76.2
72.4
67.4
82.5
84.6
51.6
52.2
92.6
88.9
77.1
73.8
2010 75.4 67.7 81.1 61.6 92.3 75.6
Staff who would recommend the trust as a provider of care to their family or friends
The data made available to the NHS foundation trust by the Health and Social Care Information Centre with regard to the percentage of staff employed by, or under contract to, the Trust during the reporting period who would recommend the trust as a provider of care to their family or friends.
The BWNFT considers that this data is as described for the following reasons;
This is an independent staff survey of approximately half our staff chosen by a weighted random sample technique and there was a 53% response rate
The BWNFT has commenced the following actions to improve this percentage, and so the quality of its services, by our six point strategy aimed at improving the overall staff survey and patient care. The areas identified include;
Ensure that everyone understands their role/responsibility and how these underpin the delivery of high quality/patient focused care.
Ensure that everyone has a well-structured/quality appraisal.
Reduce incidences of harassment and bullying.
Ensure that everyone feels engaged and able to improve the way they work.
The need to ensure that everyone feels able to recommend the Trust as a place to work/receive treatment.
Increase the percentage of staff who feels the Trust provides equal opportunities for career progression or promotion.
Behind these are a series of detailed plans overseen by the Associate Director of Human Resources. We hope that this plan will facilitate the continued improvement in this indicator.
Table 2.15 Recommend the trust as a provider of care to their family or friends
BWNFT
Average Acute Specialist
Highest Acute Specialist
Lowest Acute Specialist
Average All Trusts
Highest All Trusts
Lowest All Trusts
Staff survey 2012
77
85
93
62
65
94
35
Staff survey 2011
69
86
96
66
62
89
33
Page | 101
Patients who were admitted to hospital and who were risk assessed for Venous
Thromboembolism
The data made available to the NHS foundation trust by the Health and Social Care Information Centre with regard to the percentage of patients who were admitted to hospital and who were risk assessed for venous thromboembolism during the reporting period.
The BWNFT considers that this data is as described for the following reasons;
This data is collected and reported on a monthly basis both internally through the governance committees and externally
The BWNFT intends to take the following actions to improve this percentage, and so the quality of its services;
To develop and use a newly developed admissions document
constant reminders to staff re collection of the data
internal and external publication of our figures
Whilst this level of screening achieved last year’s National CQUIN target we know that the target for 2013/14 will be 95% of all admitted patients will be risk assessed for thromboembolism. At this time those areas within the Trust that use electronic admission have high, approximately 99%, risk screening levels. However, where this is dependent upon paper admissions processes. In 2013/14 these areas will be required to use a newly developed admissions document, one part of which will be the risk analysis for thromboembolism. This together with the constant reminders to staff and internal and external publication of our figures will both improve the process and raise awareness regarding this metric and should result in an increased screening rate.
Table 2.16 Patients who were admitted to hospital and who were risk assessed for venous thromboembolism
Q1
2010-11 (%)
Q2 Q3 Q4 Q1
2011-12 (%)
Q2 Q3 Q4 Q1
2012-13 (%)
Q2 Q3 Q4
BWNFT
Not available
56.5 84.1 93.2 91.8 88.2 90.9 92.9 94.7 92 91
Average
All
Trusts
Not available
52.5 68.4 80.8 84.1 88 90.7 92.5 93.7 94 94.3
91.2
Not available
Highest
All
Trusts
Not available
100 100 100 100 100 100 100 100 100 100
Not available
Lowest
All
Trusts
Not available
0.2 0 11.1 15.7
Not available
32.4 69.8 80.8 80.9 84.6
Not available
Page | 102
Clostridium Difficile infection
The data made available to the NHS foundation trust by the Health and Social Care Information Centre with regard to the rate per 100,000 bed days of cases of C.difficile infection reported within the trust amongst patients aged 2 or over during the reporting period
This is defined as a case where the patient shows signs of C difficile infection, and using the Trusts diagnostic algorithm, which is in line with Department of Health guidance, is assessed as a positive case.
The BWNFT considers that this rate is as described for the following reasons;
as described elsewhere in the document we have not had a case of C difficile since 2010/11 and only
1 in the last 6 years.
The BWNFT intends to take the following actions to improve this rate;
whilst the rate cannot be improved, given the zero occurrence, we are maintaining the high profile of this infection within the organisation by circulating the number of cases on a weekly basis and participating in the cleanliness initiatives such as environmental inspections.
Table 2.17 C. Difficile Infection
2012-13 2011-12 2010-11
0 0 3.2 BWNFT
Average All
Providers
Highest All
Providers
Lowest All Providers
-
-
0
22
52
0
30
62
0
Patient safety incidents reported and patient safety incidents that resulted in severe harm or death
The Data made available to the NHS foundation trust by the Health and Social Care Information Centre with regard to the number and, where available, rate of patient safety incidents reported within the trust during the reporting period, and the number and percentage of such patient safety incidents that resulted in severe harm or death.
Number and Rate of Patient Safety Incidents Reported
A patient safety incident (PSI) is defined as any incident unintended or unexpected that could or did lead to harm for one or more person(s) receiving NHS funded healthcare. The indicator is constructed by the number of PSIs reported to the National Reporting and Learning Service (NRLS).
The BWNFT considers that this data is as described for the following reasons;
This is data from our local incident reporting system that is uploaded on a weekly basis to the NRLS.
Locally, incidents are reported in accordance with the definition described above, and in accordance with local trigger lists derived from relevant royal college guidance, and in accordance with guidance received by commissioners and the local area team. We have taken this wider definition for incident reporting, and encouraged staff that if in doubt, to report it. We would rather over report incidents, than under report them.
Page | 103
The BWNFT has taken the following actions to improve this data, and so the quality of its services:
Regular monitoring and benchmarking with similar Trusts by the Patient Outcomes Committee
(previously the Clinical Governance Committee) regarding the number of Patient Safety Incidents reported on the NRLS.
We are pleased that the number and rate of PSIs reported on the NRLS has increased in each reporting period, however the Trust reports fewer PSIs than the average Acute Specialist Trust. BWNFT will continue to monitoring the number and rate of reported PSIs with the aim of reporting all our PSIs.
Table 2.18 Patient Safety Incidents per 1000 bed days
Oct 12
– Mar 13*
Apr 12
– Sep 12
Oct 11 - Mar 12
Rate Number Rate Number Rate Number
Apr 11 - Sep 11
Rate
Oct 10 - Mar 11
Number Rate Number
BWNFT
–
Local Risk
Management data**
Not applicable
771
BWNFT
–
NRLS data
Not available
Not available
Not applicable
6.2
729
709
Highest
Acute
Specialist
Lowest
Acute
Specialist
Average
Acute
Specialist
Not applicable
871
6.04
Not available
Not available
Not available
Not available
21.71
Not available
Not available
Not available
Not available
2.72
Not available
Not available
Not available
Not available
8
Highest All
Trusts
Not available
Not available
Not available
Not available
432.26
Lowest All
Trusts
Not available
Not available
Not available
Not available
0
Average All
Trusts
Not available
Not available
Not available
Not available
15
693
1935
66
773
8778
0
1529
Not applicable
595
4.06
19.25
2.45
8
141.85
0
14
466
1576
88
656
8461
0
1483
Not applicable
621
3.15
19.21
1.73
7
95
0
13
370
1292
53
566
7283
0
1429
* The data for Oct 12 - Mar 13 is taken from the Trust’s risk management software. This data has not yet been fully validated, and has therefore not all been reported to the NRLS. Data for this period is not due to be finally submitted to the NRLS until 31st May 2013.
** The data taken from the Trust’s risk management software differs from the data reported to the NRLS.
The Trust submits incidents that have been investigated and validated to the NRLS. Any incidents that have not been investigated and validated within the NRLS time limit of 2 months following the reporting period are not recorded in the NRLS data.
Page | 104
The number and percentage of such patient safety incidents that resulted in severe harm or death
These are patient safety incidents (PSI) reported to the National Reporting and Learning Service (NRLS) where the degree of harm is recorded as severe / permanent harm or death, as a percentage of all PSIs reported to the NRLS.
The BWNFT considers that this data is as described for the following reasons;
This is data from our local incident reporting system that is uploaded on a weekly basis to the NRLS.
There is slight difference between our local data compared with the data reported to the NRLS. This is due to some inaccuracies in reporting the clinical outcome for the patient, instead of reporting the severity of harm caused by the incident.
The BWNFT has taken the following actions to improve this data, and so the quality of its services:
Regular monitoring by the Clinical Governance Team of the accuracy of coding patient safety incidents resulting in severe harm and death;
Guidance issued to Clinical Directorate teams to clarify the definition of patient safety incidents resulting in severe harm and death.
Overall, BWNFT aims to report all our PSIs, whilst at the same time reduce the percentage incidents that result in severe harm or death.
Table 2.19 Patient safety incidents resulting in severe harm or death
Oct 12
– Mar 13*
Apr 12
– Sep 12
Oct 11 - Mar 12 Apr 11 - Sep 11 Oct 10 - Mar 11
Rate
Number and %
BWNFT –
Local Risk
Managemen t data**
Rate not applicable
0.13%
1
Rate and %
Number
Rate not applicable
0.14%
2
Rate and %
Number
The system for coding severity of harm was amended in 2012, and therefore data from previous reporting periods is not comparable.
Rate and %
Number
Rate and %
Number
BWNFT –
NRLS data
Not available
Not available
Rate not available
0.56%
4
0.05
0.87%
6
0.06
1.5%
7
0.05
1.6%
6
Average
Acute
Specialist
Not available
Not available
Not available
Not available
0.04 4.35
Highest
Acute
Specialist
Not available
Not available
Not available
Not available
0.17 24
0.02
0.14
2.44
11
0.04
0.22
4.33
45
Lowest
Acute
Specialist
Not available
Not available
Not available
Not available
0 0 0 0 0
Page | 105
0
Table 2.19 Patient safety incidents resulting in severe harm or death continued
Oct 12
– Mar 13*
Average All
Trusts
Not available
Not available
Apr 12
– Sep 12
Not available
Not available
Oct 11 - Mar 12
0.15 13.05
Apr 11 - Sep 11
3.67 12
Highest All
Trusts
Not available
Not available
Not available
Not available
3.76 144 141.85 160
Oct 10 - Mar 11
0.14 12.66
4.68 184
Lowest All
Trusts
Not available
Not available
Not available
Not available
0 0 0 0 0 0
* The data for Oct 12Mar 13 is taken from the Trust’s internal risk management software, and has not yet been fully validated. Data for this period is not due to be finally submitted to the NRLS until 31st May 2013.
** The data taken from the Trust’s risk management software differs from the data reported to the NRLS. The
Trust submits incidents that have been investigated and validated to the NRLS. Any incidents that have not been investigated and validated within the NRLS time limit of 2 months following the reporting period are not recorded in the NRLS data.
Percentage of all PSIs reported by BWNFT
Page | 106
Part 3 – Other Information
Update on Quality Indicators
We have already discussed our progress against the 3 main priority indicators for 2012/13 and our new priority for 2013/14 in Part 2. We will now discuss our progress against the supplementary indicators.
Supplementary Indicators
Patient Safety
Patient Safety Friday Metrics
We have now continued our Patient Safety Friday Metrics for over three years, commencing on 7 January
2010. During that time there have been a few minor changes to the criteria than we monitor, however there has been a steady fall in occurrence of these incidents. In the last 12 months all indicators have decreased except inborn births where the neonatologist was not present at the resuscitation. The increase noted in this indicator immediately alerted us to the possibility of a problem and investigation revealed that;
1. All babies where this was the case were born outside normal working hours when Consultant neonatologists are not resident (outside 9am to 9pm).
2. The increase occurred when the interpretation of the indicator changed from being present at the resuscitation to being present at the birth.
This was not a deliberate change, but rather a misinterpretation.
Once the above were known it was possible to give assurance to the Board of Directors that this increase was not a clinical quality problem, but more a data collection and interpretation issue. This shows the benefit of rapid collection of important outcomes that are widely distributed, inviting comment and challenge that the clinicians welcomed. Undoubtedly there does appear to be year on year improvement in this data encouraging us to continue with this process.
Table 3.1 Patient Safety Friday metrics
Indicator Number of occurrences
MRSA bacteraemia
Clostridium Difficile
Inadvertent bowel or bladder damage during gynaecological surgery
Unexpected returns to gynaecology theatre
Caesarean sections for placenta praevia where the consultant anaesthetist and obstetrician were not present
Inborn babies that require therapeutic hypothermia for presumed peripartum hypoxia
Ventilated inborn babies below 28 weeks gestation where administration of surfactant within 1 hour of birth was not achieved
Inborn births before 25 weeks where the neonatal consultant was not present at the resuscitation when required to be present by the
Trust’s early care guideline
Incorrect laboratory report released by genetics laboratories
2010-11
0
1
Not
Applicable
22
2
1
0
11
2011-12
15
2
Not
Applicable
6
17
2
7
6
3
3 2
2012-13
0
0
5
7
1
10
1
7
Page | 107
Table 3.2
Patients with MRSA bacteraemia/ 100,000 bed days
1,2
2007-
8
0
2008-
9
0
2009-
10
0
2010-
11
0
(1case)
0.31
2011-
12
1 case
1.7
0
2012-
13
0
0
National
Average
1.02
(2011/12)
Patients with C Difficile infection/ 100,000 bed days
1,2
Adjusted Stillbirth rate/
1000 deliveries(Unadjusted, crude rate)
1,2,3,4
0
3.9
(8.5)
0
4.1
(6.7)
0
5.4
(7.7)
2.2
(5.1)
4.5
(6.4)
2.9
(4.6)
17.37
(2011/12)
3.9 in
2007
(5.2 in
2011)
(3.0 in
2011)
Adjusted Neonatal mortality rate/ 1000 deliveries (Unadjusted, crude rate)
1,3,4
2.7
(7.4)
3.1
(6.9)
1
Data items based on nationally agreed definitions
6.3
(7.9)
2
Data source internal reporting
3
2012-13 figures are from March 2012- February 2013
4 Previous year’s figures adjusted for April to March data
2.9
(6.3)
2.9
(6.6)
2.6
(4.7)
As a tertiary maternity service we would expect a high number of complex cases to be transferred to the hospital, and therefore when comparing our stillbirth rate with other parts of the country not only this, but the degree of social deprivation within the community needs to be considered. It has also been recognised that the
West Midlands has a significantly higher proportion of deaths secondary to major congenital abnormalities, hence we have continued to include in our table both the adjusted and crude mortality rates. Given these limitations, for us to achieve an adjusted stillbirth rate that is not significantly different from the national average is a notable achievement. The newer national comparators no longer exclude major congenital abnormalities, an important cause of death amongst our patient population, and hence we have again benchmarked against slightly older national data. In addition we do benchmark ourselves in detail against another major tertiary unit with whom we share our detailed data.
The fact that we are one of only two Neonatal Intensive Care Units within the Southern West Midlands
Newborn Network that care for babies born below 26 weeks gestation, those with the highest mortality rates, means that we would expect to have a higher neonatal mortality rate than the average for England. This is especially true considering the aforementioned social deprivation and care pathways that result in many babies with antenatally identified major congenital abnormalities being born and cared for at BWNFT.
Supplementary Indicators
Clinical Effectiveness
The indicators used in the 2011/12 report have been maintained in order to continue producing longitudinal data in these important topics for the Trust. However one indicator, multiple pregnancy rate following IVF or
ICSI has been made one of our three main priorities for 2013/14 as mentioned above and will be replaced by the per cent of actions completed on time following serious incidents. This is discussed in part 2 above.
Page | 108
Retinopathy of Prematurity (ROP) screening and Treatment
ROP screening is an important quality parameter for premature and small babies. There are Nationally agreed screening criteria as well as detailed time windows for screening and criteria for intervention (laser).
Screening is a Neonatal quality standard, which is registered nationally on the NNAP database. Currently, all babies with gestation less than 32 weeks or birth weight less than 1500 grams are screened.
During the year 2012/13, 125 babies were screened at BWNFT; six babies who fell within the criteria were not screened within the predetermined timeframe. In 2012/13, all missed cases have been systematically identified and where possible brought back to OP for screening. No late retinal disease has been found in this population. This has been the case for all but one baby this year.
Unfortunately, as the screening is then done after the babies’ inpatient stay is complete, this information cannot be added retrospectively to the NNAP dataset as it uses the Badger clinical information system, which only covers the inpatient stay. Therefore, when the 2012 NNAP audit data is available, there may be a discrepancy between the figures quoted here and in the NNAP report.
Additionally, when Q3 results were available, a “helpsheet” was devised in December 2012 for the junior medical staff, who “list” babies for screening on a weekly basis which has made this process more reliable.
Although 95.4% is a decrease from last year’s performance this is mostly due to a relatively poor performance in quarter 1. Despite this the National ROP CQUIN target set by the Commissioners of 92%, was therefore achieved. With regard to our in house target of 99% in quarter 4 this was missed by 1%. However, this represents a single baby that did not have appropriate screening in the entire quarter. This also compares favourably with the data published within the 2012 by the National Neonatal Audit Programme where 82% of babies were screened. Overall this has been an excellent performance over the last 4 quarters and the aim for 2013/14 is to improve our screening rate so that fewer than six babies will miss their screening in the year.
Table 3.3 % babies received ROP screening
Indicator - NNAP
% babies received ROP screening
Target
2012
NNAP 2011/12 Q1 Q2 Q3 Q4
RAG status
92 82 97 86 98 93 98
Page | 109
Clinical pregnancy rates following assisted conception
Couples with female age 19-35 represent the group most likely to conceive and hence are the best group to reflect changes or improvements in practice. The national average pregnancy rate for this group is 36% (red line) and the Fertility Centre objective target is shown by the green line (45%). There appears to be an in year improvement from last years end of year pregnancy rate of 36% to 50% in February 2013. At the time of publication the data for March 2013 was not available however, the pregnancy rate for the year was 41%. This represents an excellent result by the Fertility Centre team.
Chart 3.4
Pregnancy rates per cycle Female age <36
Cancelled operations on the day of surgery
Whilst the absolute number of operations cancelled on the day of surgery has increased from last year’s figure, it is still well within our target. The details of all cases are examined in the theatre users committee and general reasons are discussed with our commissioners in their monthly performance reviews with the directorate. The commonest reason for these non-medical cancellations is an unexpected occurrence during the theatre list, either surgery taking longer than was reasonably expected or interruption of the list for emergency surgery.
During the year we participated in the Midlands and East Enhanced Recovery Pre-operative Assessment
Study. The lessons learnt from this tend to cross organisational boundaries and we have discussed this with our commissioners.
% women seen within 12 weeks of pregnancy
The National Maternity target for pregnant women being seen by the twelfth week of pregnancy has risen year on year from a starting point of 80% and increased to 90%, it has been promoted with the objective of reducing perinatal mortality. Once more we have managed to achieve this target and whilst this is a slight fall in performance from our previous year’s results we do not think that this is significant. Next year we plan to reaudit this with respect to place of abode in order to ensure that the socially disadvantaged community that we serve are not affected disproportionately.
Page | 110
Table 3.5
2007-8 2008-9 2009-10 2010-11 2011-12 2012 -13 National
Average/
Targets
32 Clinical Pregnancy rate for the Fertility
Centre, %
1,2
Cancelled operations on the day of surgery, non medical % of all elective operations
1,2
31 30 34
1.23
(47 cases)
0.47
(20cases)
0.33
(11cases)
32
0.32
(8 cases)
36
0.23 (8 cases)
41
0.68
(15 cases)
0.8
% women seen within 12 weeks of pregnancy
1,2
Not
Available
90 88
1
Data items based on nationally agreed definitions
2
Data source internal reporting
90 94 92.5 90
In all three of these important indicators we have achieved our targets.
Supplementary Indicators
Patient Experience
With one exception the indicators used in the 2011/12 report have been maintained in order to continue producing longitudinal data in these important topics for the Trust. The exception is the replacement of the previously quoted recommendation of the Trust to a friend or relative as found in the inpatient survey. This has been replaced with the Friends and family Test, which is described below. This will provide us with similar information as the previous metric, but is from a larger sample size and can be easily benchmarked. In coming years this will be completed by all Trusts in England.
Complaints answered within time limit agreed with the complainant
One marker of the responsiveness and capability of an organisation is how they respond to complaints. At
BWNFT we have had a long tradition of being open when clinical incidents occur, however in the past our timeliness in responding to complaints has not been of a standard to which we would aspire.
The present national recommendations stipulate that an agreed time limit for the response should be agreed with the complainant. Over the last three years however this response rate has improved from 75% in 2010-
11 to 69% 2011-12 and then to 94% in 2012-13. As can be seen in the tables 3.9-3.12 the Directorates have increased their response rates. This data is sourced locally from the complaints department.
Page | 111
Outpatient survey results
In previous reports we have documented the percentage of patients who had to wait more than 15 minutes for their gynaecology outpatient appointment and of those how many were told how long and why they had to wait. We know that from our most recent survey data 17% of patients waited more than 15 minutes. Of these
42% were told why they had to wait and 27% how long they had to wait. Whilst this is still short of our target, this does represent a significant improvement from the 2009 and 2010 data.
In the forthcoming year we expect that there will be another national outpatient survey and this will allow us to benchmark our progress against other providers.
Table 3.6 Outpatient survey results
Trust Score
2009, National
Survey
Trust
Score
2010
2011
National
Survey
Sept
2011, internal survey
Nov 2011, internal survey
2012/13
Internal Survey
Were you told why you had to wait
Lowest 20% of trusts
10.7% No longer asked in
CQC survey
14% 40% 42%
Were you told how long you would wait
Lowest 20% of trusts
3.5% Lowest
20% of trusts
7% 60% 27%
Inpatient survey the percentage of people who would recommend the Trust to a friend/relative (This has now been replaced by the friends and family test (FFT)).
The friends and family test has been in place in NHS Midlands and East throughout the last financial year.
The BWNFT friends and family test for 2012/13 was governed by the NHS Midlands and East standards, which uses the net promoter methodology to determine whether patients would recommend the hospital to their friends and family.
Answers are split into those that are extremely likely, likely, neither likely nor unlikely, unlikely and very unlikely. Respondents who say they are extremely likely to recommend the hospital are considered promoters whereas those who are neither likely nor unlikely, unlikely and very unlikely are detractors, with likely respondents being neutral. The net promoter score is therefore the proportion of promoters minus the detractors. This can give a score between 100 and -100.
The friends and family score for BWNFT can be seen by a monthly basis below. The baseline score was 64 and our CQUIN target was to either improve by 10 points, to 74, or to increase into the top quartile of Trusts, to 71, by the end of 2012/13. As can be seen from the data below we improved our score from 64 to 73 at the end of the year. In the year the total number of patients surveyed was, 2965 of 15,385 eligible patients, that is a 19.3% response rate.
This data will be collected nationally in 2013/14 therefore allowing further detailed benchmarking. At the present time the data has been sourced from local patient survey results reported to NHS Midlands and East via UNIFY2, the data collection system used by the Knowledge and Intelligence team in the Department of
Health to collect a wide range of performance information.
Page | 112
Table 3.7 FFT scores
Month
April 12
May 12
June 12
July 12
Aug 12
Sept 12
64
80
76
FFT Score
64
65
52
Oct 12
Nov 12
Dec 12
Jan 13
75
80
78
84
Feb 13
Mar 13
75
73
The table below is a comparison as at the end of March 2012/13 with the regional average and the highest and lowest regional providers:
Table 3.8 Regional benchmarking for FFT
Mar-13 Response Rate
BWNFT
NHS Midlands & East average
73 16.9
70
88
18.4
76.1 Highest Provider
Lowest Provider 38 10.1
Page | 113
Quarterly Monitoring of Quality Account Indicators
The Quality Accounts Metrics are monitored by the Patient Outcomes Committee, a subcommittee of the
Board of Directors that is chaired by a non-executive director and now has representation from our commissioners on it. The tables below depict the quarterly reporting by the directorates to the Committee .
Table 3.9 – Genetics and Laboratories
2012/13
2011
Indicator
Targ et
/12 Q1 Q2
Q
3
Q4
2012/
13
RAG status
To ensure actions are completed on time following Serious
Incidents
93% 88%
75
%
75
%
N/
A
N/A 75%
To participate in relevant national audits and confidential enquiries
(include number and % of cases submitted)
National Comparative Audit of
Blood Transfusion – Audit of
Blood Sample Collection and
Labelling:
Organisational survey
Data sheets of rejected samples from May –Jul 2012
Follow-up Interview results
100
%
N /A N/A
100
%
100
%
23
(10
0%)
N/
A
N/A 100%
Increase the percentage of complaints answered within the agreed time limit to 95% in each
Directorate
95% 89%
100
%
100
%
10
0
%
100% 100%
Page | 114
Table 3.10 – Gynaecology
Indicator
2012/13
Target 2011/12
Q1 Q2 Q3 Q4
2012/13 RAG status for year
To ensure actions are completed on time following Serious Incidents
93% 88% 100% 100%
N/A
No new
SI
Q3.
N/A
No new
SI Q4
100%
To increase the percentage of nursing and midwifery time spent delivering direct clinical care to more than 55%
55% 43.5% 45% 43% 42% 39%
42.5%
To participate in relevant national audits and confidential enquiries
(include number and % of cases submitted)
100% 100% 100% N/A N/A N/A
100%
Multiple pregnancy rates below
12% following assisted conception
<12% 13% 13% 22% 13% 17%*
14%
Clinical Pregnancy rate for the
Fertility Centre (fresh embryo transfer)
32% 36% 39% 40% 44% 44%*
41%
Cancelled operations on the day of surgery, non medical % of all elective operations
<0.8% 0.23% 0.17% 0.68% 0.7% 0.99%
0.68%
Increase the percentage of complaints answered within the agreed time limit to 95% in each
Directorate
95% 90% 100% 100% 100% 100%
* this only includes pregnancies for January and February 2013
100%
Page | 115
Table 3.11 – Maternity
Indicator Target 2011/12
2012/13
Q1 Q2 Q3 Q4
2012/13
RAG status
To improve the detection rate of
Intrauterine Growth Restriction (IUGR) 35% 28% 18% 26% 21% 31% 26%
To ensure % actions plans are completed on time following Serious Incidents
93% 86% 82% 100% 100% 100% 92.3%
To ensure % complaints completed on time in the last quarter
% women seen within 12 weeks of pregnancy
>95%
>90%
63%
94%
94% 72% 100% 93% 90%
92% 92% 93% 93% 92.5%
To increase the percentage of nursing and midwifery time spent delivering direct clinical care from the benchmark figure
Ward 1 55% 40.5% 40% 28% 55% 56% 44.75%
Postnatal floor 55% 56% 58% 66% 62% 69% 63.75%
Delivery Suite 55% 58% 44% 69% 79% 79% 67.75%
Maternal Death (MBRRACE-UK) – To participate in relevant national audits and confidential enquiries (include number and % of cases submitted) this was N/A last year as 0 deaths reported
100% 0
1/1
100%
0 0 0 100%
Page | 116
Table 3.12 – Neonatology
Indicator Target 2011/12
2012/13
Q1 Q2 Q3 Q4
2012/13
RAG status
To ensure actions are completed on time following Serious Incidents
93% 88% 83% 94% 93% 88%
91.3%
To increase the percentage of nursing and midwifery time spent delivering direct clinical care to more than 55%
55% 46.5% 44% 47% 30% 44%
42%
To participate in relevant national audits and confidential enquiries
(include number and % of cases submitted)
100% 100% 100% 100% 100% 100%
100%
To improve our Retinopathy of
Prematurity (ROP) screening rate to achieve a 99% screening rate by quarter 4 for this high risk group
99% 97% 86% 98% 93% 98%
95.4%
Increase the percentage of complaints answered within the agreed time limit to 95% in each Directorate
95% 86% 100% 100% 100% 100%
100%
Page | 117
Further National Indicators
As can be seen from the table below the performance of BWNFT exceeded the threshold set for the indicators except for the 31 day wait from diagnosis to treatment for all cancers. Here the threshold was 96% and at BWNFT we achieved 94.1%. This figure is monitored closely by the cancer operation team and this figure represents two patients in Quarter 2 who breeched the target. Importantly there were no further breeches for the remainder of the year, though the denominator data here is only 36 patients in total. Whilst we would obviously aim for all patients to be seen within this time limit we do not feel that we need to alter our systems at this time as we deem them to be appropriate. We also have a further five targets regarding cancer pathways, four of which are National targets and are shown below, and all these targets were achieved.
Table 3.13
Area Indicator Threshold
BWNFT
Performance
2012/13*
Quality
All cancers: 31-day wait for second or subsequent treatment, comprising:
Quality
Quality surgery
All cancers: 62-day wait for first treatment from: urgent GP referral for suspected cancer
NHS Cancer Screening Service referral
All cancers: 31-day wait from diagnosis to first treatment
94%
85%
90%
96%
100%
92%
100%
94.1%
Quality
Patient
Experience
Cancer: two week wait from referral to date first seen all urgent referrals
(cancer suspected)
Maximum time of 18 weeks from point of referral to treatment in aggregate – admitted
93%
90%
95.5%
94.1%
Patient
Experience
Maximum time of 18 weeks from point of referral to treatment in aggregate – non-admitted
95% 96%
Patient
Experience
Maximum time of 18 weeks from point of referral to treatment in aggregate – patients on an incomplete pathway
92% 95.6%
* This data is based on internal data reported to the Board of Directors. However, the data is subject to slight variations up to 8 weeks following the reported time period, due to amendments, on the national Open Exeter computer system, by other Trusts related to shared patients.
Page | 118
Annex:
Statement from NHS Birmingham South Central CCG
Birmingham South Central Clinical Commissioning Group (BSC CCG) as coordinating commissioner for Birmingham Women’s NHS Foundation Trust welcomes the opportunity to provide this statement for their 2012/13 Quality Account.
A draft copy of the Quality Account was received by BSC CCG on the 26th April 2013 and the statement has been developed from the information presented to date. Feedback on the draft account has been received from Birmingham CrossCity CCG, Solihull CCG and NHS England Area
Team as the lead for specialised commissioning.
We have reviewed the content of the Quality Account and confirm that this complies with the prescribed information, form and content as set out by Monitor and the Department of Health.
The information provided within this account is, to the best of our knowledge accurate and fairly interpreted. It identifies where the organisation has done well, where further improvement is required and what actions are needed to achieve these goals.
We have made some specific comments to the Trust directly in relation to their plan and highlighted areas where we feel there needs to be more of a focus. Namely, inclusion of further detail on how levels of improvement are to be measured in 2013/14 and further information on CQUINs regarding outcomes and the levels of improvement achieved in 2012/13. We have requested that further analysis of serious incidents and complaints data are included which reflect themes/ trends and outlines actions implemented as a result of learning. Inclusion of additional workforce data is another key area for focus. We have also proposed that future Quality accounts are aligned with the five domains of the NHS Outcomes Framework.
In addition to these points we have requested an assurance statement on Equality and Diversity and additional information and assurance on safeguarding for both children and adults.
The account reflects a commitment to listen to and understand the experience of women and their families and we welcome the development and implementation of a Patient Experience Strategy in
2013/14. This will build on current initiatives and enable the experience of patients and their families to drive improvements in the quality of care.
Birmingham Women’s NHS Foundation Trust have been successful in increasing the number of midwives during 2012/13 following a skill mix review and have also recruited more nurses to the neonatal directorate. The challenge now for Birmingham Women’s NHS Foundation Trust will be to demonstrate that this and the implementation of actions identified as part of the Trust wide review of time spent delivering direct patient care will impact positively on patient experience in 2013/14.
As detailed in the account, Birmingham Women’s NHS Foundation Trust have made a number of improvements in the serious incident investigation and management process within the Trust. While this is not included as one of the quality account priorities for 2013/14 serious incidents and the appropriate management of these will remain as a core indicator within the quality schedule of the contract. We will continue to work with the Trust as part of the ongoing quality monitoring process to ensure that they build on and sustain these improvements.
The Quality Account reflects a number of the performance quality indicators which are monitored monthly along with areas for improvement at the CCG / Trust Clinical Quality Review Group mandated by the service contract. We are also invited to the Trust’s Patient Outcomes Committee and to Root Cause Analysis meetings following occurrence of serious incidents, reflecting an open and transparent culture.
The Quality Account provides evidence of ongoing commitment by the Trust to continue to improve
Page | 119
the services it provides. We look forward to continuing our partnership with the Trust and in supporting them to deliver this year’s quality targets.
Dr Raj Ramachandram
Chair – Birmingham South Central Clinical Commissioning Group Quality and Safety
Committee
Page | 120
Annex:
Statement of directors’ responsibilities in respect of the Quality Report
The directors are required under the Health Act 2009 and the National Health Service Quality Accounts
Regulations to prepare Quality Accounts for each financial year.
Monitor has issued guidance to NHS foundation trust boards on the form and content of annual quality reports
(which incorporate the above legal requirements) and on the arrangements that foundation trust boards should put in place to support the data quality for the preparation of the quality report.
In preparing the Quality Report, directors are required to take steps to satisfy themselves that:
The content of the Quality Report meets the requirements set out in the NHS Foundation Trust Annual
Reporting Manual 2012/13;
The content of the Quality Report is not inconsistent with internal and external sources of information including:
The minutes and papers of the Board of Directors for the period April 2012 to May 2013
Papers relating to quality that were reported to the Board of Directors over the period April 2012 to May
2013
Feedback from the Commissioners dated 14 th
May, 2013
Feedback from Governors received during the course of the year at meetings of the Members’ Council
The trust’s complaints report published under regulation 18 of the Local Authority Social Services and
NHS Complaints Regulations 2009, which is dated 26 th
July 2012
The national patient survey, dated 16 th
April 2013
The national staff survey, dated 28 th
February 2013
The Head of Internal Audit’s annual opinion over the trust’s control environment dated 24 th
May, 2013
The Care Quality Commission’s Quality and Risk profile dated September 2010 to March 2013.
The Quality Report presents a balanced picture of the NHS foundation trust’s performance over the period covered;
The performance information reported in the Quality Report is reliable and accurate;
There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Report, and these controls are subject to review to confirm that they are working effectively in practice;
The data underpinning the measures of performance reported in the Quality Report is robust and reliable, conforms to specified data quality standards and prescribed definitions, is subject to appropriate scrutiny and review; and the Quality Report has been prepared in accordance with Monitor’s annual reporting guidance (which incorporates the Quality Accounts regulations) (published at www.monitornhsft.gov.uk/annualreportingmanual ) as well as the standards to support data quality for the preparation of the Quality Report, available at www.monitor-nhsft.gov.uk/annualreportingmanual ).
The Directors confirm that, to the best of their knowledge and belief, they have complied with the above requirements in preparing the Quality Report.
Signed by Order of the Board of Directors,
..............................Date.............................................................Chairman
..............................Date............................................................Chief Executive
Page | 121