Leadership for cultural change
advertisement
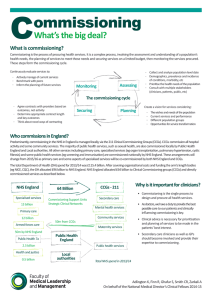
System changes & impact on the NHS Nigel Edwards John Reform on one page Commissioning – Fragmented Providers – more autonomous & plural Regulation – confused Change drivers – competition, choice, integration and direction Secretary of State – in theory taken out of day to day issues Rules of the new system – not clear yet New landscape..... New organisations/bodies The Mandate NTDA NHS Trust Development Authority 112 Trusts FT Pipeline (Jan 2012) CSS What does it all mean? Uncertainty Accountability – who is really responsible for what Decision making – Competition & mergers – Procurement Strategy No strategy function Many different actors A more local focus Agreement & implementation harder Strategy & the wider system Issues about the size of some CCGs in relation to the wider system Federated arrangements are not present in many places and are hard to make work Signs of the strategy gap being filled NHS England will develop a strategy – Seven work streams – Rationalisation of tertiary care – New offer from primary care – New financial regime Bill McCarthy talking about regional planning Will AHSNs do some of this? But, still more pressures to change Commissioning guidance A focus on quality – E.g. Signs that NHS England will be pushing 24/7 consistency This has particular implications for out of hours surgery Known unknowns - Behaviour The intention was to break the system and change the culture – did enough get broken? How will the people in the new bits of machinery actually behave? What will happen when things start to unravel? Do the players understand the new architecture & behave accordingly? Changes in primary care Worrying situation on demand and workforce A possibly unanticipated change also driven by static GMS funding is a realisation that primary care needs to change too More federated arrangements emerging New contracts Arrangements for out of hours likely to change Integration Much enthusiasm for this but it is hard to do Part of the problem is complexity and overlap created by multiple initiatives and projects There are big opportunities but it is harder to do than it first appears Procurement and payment mechanisms are an issue It costs before it pays Concerns Financial situation in health and particularly social care Plans to deal with this are not very convincing A significant number of organisations in difficulty No very clear way forward for the trusts that will not make FT status On the upside New ideas and commissioners with a clinical focus A shift to commissioning on outcomes rather than input and process (I hope) Health and Wellbeing Boards A strong consensus that change is required Questions and discussion n.edwards@kingsfund.org.uk