Quality care, closer to you Quality Account 2011/12

Quality care, closer to you
Quality Account 2011/12
PCH Final 20 June 2012 Page 1 of 62
Chief Executive’s statement
Our transformational quality journey
This is our second Quality Account and I am very pleased to report that we have achieved many of the goals and commitments that we set out last year and are on track to meet many others.
In October 2011, Community Health Services, previously part of NHS Cornwall and the
Isles of Scilly transferred to the new community interest company Peninsula Community
Health. Community interest companies (CIC) are a type of social enterprise set up specifically for organisations operating for the benefit of the community, rather than for the benefit of Shareholders. We are commissioned by NHS cornwall and Isles of Scilly
(PCT) to provide services to NHS patients so, first and foremost, commissioners will ensure services are provided that meet local needs and are of a high quality.
We are regulated by Community Interest Company Regulator and registered with
Companies House. The regulator ensures that the appropriate governance structures are in place. As a Community Interest Company we are "asset locked" which means that any surpluses made must be reinvested for the good of the community.
We are also registered with the Care Quality Commission which, as before, will routinely inspect us to ensure we continue to provide high quality, safe services.
As part of our commitment to being open with our community, we hold our monthly Board meeting in public, papers being available on the website. Corporate information about
Peninsula Community Health, such as our Board of Directors and our annual reports will, when available, be posted on this website.
As Peninsula Community Health we are committed to provide excellence in treatment and care – which is safe, sensitive and responsive to the individual. Our vision is ‘Quality care, closer to you’
PCH Final 20 June 2012 Page 2 of 62
Quality Care
•
We will strive to give care that meets the highest standards
•
Our care will be safe, accessible, effective and provide the best possible outcomes
•
We will seek out better practice and exemplar care and implement it to further improve our patients’ outcomes
•
We intend to be an organisation that is seen as excellent in ensuring dignity and compassion in the way we deliver our services
•
We will train, develop and support our staff to enable them to deliver excellent care
•
We want to be proud of the healthcare we deliver
Closer to you
•
We will review where we provide services to ensure they are in the right place at the right time
•
We will listen to the needs, concerns and suggestions from our patients and carers
•
We will work with our commissioners to ensure our services meet the needs of the local population
Our organisational focus on improving quality is driven by innovative and bespoke patient experience metrics which enable us to capture and use realtime patient feedback in ways few other UK health organisations are able to do.
If we can provide Quality Care, closer to you then we can have a Great future. We don’t want to be a healthcare provider that simply does what is required of it – we have greater aspirations than that.
Great Future
•
We want to thrive as a healthcare provider, not just survive
•
We want to attract, train and use the talent that exists around us
•
We want our commissioners to be confident in us and in what we can create together
•
We want to be a place of choice for people to work
•
We want to reach out beyond the boundaries of health and be a major player in our community, society and the wider economy
•
We want to attract investment and funding because we deliver our promises and have innovative and creative approaches
Our priority is to improve the quality of services in terms of clinical outcomes, patient safety and patient experience. We are able to report some very positive achievements in the last year in areas such as reducing healthcare associated infections, improving safety with medicines and reducing harm from falls in our community hospitals.
PCH Final 20 June 2012 Page 3 of 62
Peninsula Community Health Board is committed to making further improvements to the quality of services delivered to patients. In January 2011 we joined organisations within the region to share practice and learning to improve safety and care for our patients. We have focused our efforts initially on further reducing healthcare associated infection, reducing the risk of venous thromboembolism (VTE) and care of the deteriorating adult.
Peninsula Community Health Board is committed to continuous quality improvement and promoting a culture of care delivery to improve the experience of our patients. To demonstrate our commitment to improving safety, the Board has committed to undertake patient safety walkrounds, providing an opportunity for Board members to meet with staff, patients and their families to talk to them about the care we provide, discuss any concerns they may have, and agree priorities for improvement.
This has been a challenging year, and I extend my appreciation to all staff within Peninsula
Community Health for their hard work and continued focus on improving patient safety and experience. Despite these challenges we have achieved all our CQUINs for 2011/12 and this is a great achievement for which we all should be proud.
This Quality Account is endorsed and approved by the Board of Peninsula Community
Health which believes that the information contained within it is accurate. I hope you find it an interesting and informative document.
Kevin Baber
Chief Executive
Peninsula Community Health CIC
PCH Final 20 June 2012 Page 4 of 62
1.0
2.0
2.1
2.2
2.3
2.4
2.5
2.6
Priorities for Improvement 2012/13
Review of Services provided
Care Quality Commission
Research
Audit participation
Goals agreed with commissioners
Data Quality
Information Governance
3.5
3.6
3.7
3.8
2.7
3.0
Clinical Coding Error Rate
Review of our Quality and Safety Performance 2011/12
3.0.1 Performance Review – The priorities we identified in 2011/12
3.0.2 Identification and Management of the Deteriorating Patient
3.0.3 Venous Thromboembolism
3.0.4 Reducing Avoidable Pressure Ulcers
3.0.5 Ensure effective pathways of patient care
3.0.6 Patient Information
3.0.7 Improving the patient experience
3.1
3.2
Maintaining Essential Standards for Registration with the Care Quality
Commission
NHSLA Assessment
3.3
3.4
The Musculoskeletal Interface Service
Parkinson’s Disease Service
NHS Southwest Early Warning Trigger Tool
Equality Delivery System Assessment and Equality Objectives
Respiratory Nurse Service
Reducing harm from falls
3.9 Community Cardiac Services
3.10 Medicines Management
3.11 PEATS
3.12 Nursing Metrics and Patient Experience Measurement during 2010/11
PCH Final 20 June 2012 Page 5 of 62
21
23
23
24
25
18
19
19
19
20
7
12
12
12
12
16
17
18
30
30
32
33
25
25
28
36
38
40
41
4.1
4.2
4.3
4.4
4.5
5.0
6.0
3.13 Privacy and Dignity Visits
3.14 Eliminating Mixed Sec Accommodation (ESMA)
3.15 Complaints and Compliments
3.16 Staff Survey 2012
3.17 Key Quality Performance Indicators
3.18 NHS Southwest Quality and Safety Improvement Programme
4.0 Response to this report from our stakeholders
Cornwall Overview and Scrutiny Committee
Isles of Scilly Overview and Scrutiny Committee
Link4Scilly
Cornwall LINk
NHS Cornwall & Isles of Scilly/Kernow Clinical Commissioning Group
Conclusion
Glossary
PCH Final 20 June 2012 Page 6 of 62
55
57
58
59
54
54
55
45
46
46
49
52
53
54
1.0 Priorities for Improvement 2012/13
How we identify our quality improvement priorities
Our quality monitoring systems capture information throughout the year about the quality of services we provide and the risks to service users. We continually monitor the experiences of patients and how we perform against the range of national standards.
We strongly believe in the importance of establishing meaningful dialogue with patients, patients’ representatives and carers, to help us develop our quality improvement plans for the coming year. In February/early March 2012, the potential priorities for inclusion in the
Quality Account were circulated to the following bodies asking their opinion as to the level of priority of each subject:
•
Overview and Scrutiny Committees for both Isles of Scilly and Cornwall
•
Cornwall LINKs
•
LINk4Scilly
•
Royal Cornwall Hospital
•
Plymouth Hospitals NHS Trust
•
Cornwall Partnership Foundation Trust
•
Peninsula Community Health staff
•
PCH Non Executive Directors
•
NHS Cornwall and Isles of Scilly
•
Cornwall League of Friends
•
PCH Specialist Nurses
•
PCH District Nurse Lead
Peninsula Community Health, in collaboration with the above groups, has established five quality improvement priorities for 2012/13. We have organised them into three domains, consistent with the core domains for quality patient care identified by Lord Darzi in the ‘NHS
Next stage Review: High Quality Care for All’. They reflect what we believe are the priority areas for achieving the best possible outcomes for those we serve:
•
Patient safety
•
Clinical effectiveness
•
Patient experience
These quality improvement priorities are detailed on the following pages and include the development of work that is already underway as well as new work that we consider to be equally important.
PCH Final 20 June 2012 Page 7 of 62
Domain
Patient
Safety
Priority
Improving the nutrition of patients in hospital – nutrition is a high priority across healthcare and is an area that the Care Quality Commission has highlighted as falling below standard and below public expectations nationally.
Improving clinical documentation – during 2011 a great deal of work was undertaken to redesign and improve the inpatient documentation. To further this work, all other clinical documentation across our community services require review – to ensure patients are informed and consent to plans of care. An area of particular concentration will be in regard to patients discharges from hospital, ensuring that patients remain fully informed and consentual to the discharge plan – this has been added following the consultation.
Clinical
Effectiveness
Improving dental pathways for patients with Learning Disabilities with an emphasis on prevention and dental hygiene.
Protect the quality of care and dignity of patients with dementia.
Patient
Experience
Complaints handling – to improve the timeliness of complaints handling, to enhance the quality of root cause analysis and investigation of incidents and ensure learning across the organisation – this has been added following consultation.
Patient Safety
Priority 1
Improving the nutrition of patients in hospital
Within our community hospitals we already have robust monitoring systems of patients nutritional input, but we can always do more and strive for better.
Within the next 12 months a Nutritional Group will be set up with the following objectives:
•
Developing further nutrition as a nursing quality indicator to benchmark the quality of patient care
•
Developing a multidisciplinary nutrition team to ensure a whole system approach to nutritional care and act as a specialist resource to frontline staff
•
•
Measure the impact of The Productive Community Hospital on nutritional care
Ensure the 10 key characteristics for Good Nutritional Care in hospitals are being implemented
•
•
Scope the recruitment and training of volunteers to assist patients at mealtimes
Ensure effective methods to manage the transition from hospital to home, by improving communication regarding nutritional care
•
Test new care systems relating to hydration
PCH Final 20 June 2012 Page 8 of 62
Priority 2
Improving clinical documentation
During 2011 a great deal of work was undertaken to redesign and improve the inpatient documentation across all our community hospitals.
To further this work, all other clinical documentation across our community services require review – to ensure patients are informed and consent to plans of care.
An area of particular concentration will be in regard to patients’ discharges from hospital, ensuring that patients remain fully informed and consensual to the discharge plan.
Clinical Effectiveness
Safety
Priority 3
Improving dental pathways for patients with Learning Disabilities with an emphasis
on prevention and dental hygiene.
We want to work with other care providers to ensure that all possible dental health promotion and care takes place, to reduce the need for patients with learning disabilities requiring teeth removal under general anaesthetic. This will target dental hygiene and include work with a range of other agencies across Cornwall.
Patient Experience
Priority 4
Protect the quality of care and dignity of patients with dementia
In February 2011 the South West Dementia Partnership developed a set of common standards and published a report that aimed to make a significant contribution to improving care and services in community and general hospitals across the South West for patients admitted for elective or emergency treatment or care. Some of the patients within this group will already have a confirmed diagnosis prior to their admission to hospital, many others will not have yet been assessed or diagnosed but will have a range of dementia related symptoms. The standards within the document embrace both groups.
We are currently benchmarking each individual hospital against the South West Hospital
Standards in Dementia Care. We will then progress to developing a Shared Dementia
Care Improvement Plan and implement local action plans. Collectively these plans will form the basis of our workforce training and education plans in relation to the care we deliver to patients with Dementia, their families and carers.
Once this exercise is complete an organisational implementation plan will be devised and presented to the board for approval. Once approved, we will work to implement locally and report regular progress.
We already have key areas of excellence relating to the care of patients with dementia within our organisation. We will acknowledge and celebrate these areas of innovation and promote the sharing of best practice across the whole organisation.
PCH Final 20 June 2012 Page 9 of 62
We are also working to build alliances with our third sector colleagues and partner organisations to ensure that we work across boundaries and provide a smooth transition for patients along the Dementia Care Pathway.
A programme of work will be taking place at Poltair and St Austell Community Hospital from
May to November. The main focus of this work programme is to ensure that we are providing high quality patient centered care, meeting the individual needs of each patient and driving up the quality and standards of care provided. We are adopting a multidisciplinary approach and are working closely with Dr Rod Bland, Consultant in Elderly
Care at Royal Cornwall Hospital and members of his team, patients’ families and carers, therapists, clinical staff, Adult Care and Support and our third sector partners.
The aim of the programme is to work towards creating a care pathway for people with dementia, as well as proactively initiating early assessment and swift referrals to appropriate support services for people who come into our hospitals that have not been diagnosed with dementia prior to their admission. Education and training will be provided to all the clinical team ensuring that we promote best practice and that our staff are fully equipped with the knowledge and expertise to be able to care for people with dementia and understand the support services available in the wider community setting.
We are also aiming to raise the standards of knowledge and skills in staff being able to proactively deal with patients that can become acutely distressed and confused on our wards. We aim to provide training on both wards to enable staff to increase their skills and feel confident in the way they manage and de-escalate situations. We will specifically target interactions, environments and documents relating to people who have communication disabilities. The training will be designed to raise awareness in three key areas
•
•
•
How to improve your interactions
How to improve your environment
How to improve your documents
Key components of this will explore how we engage with people with communication disabilities in making services accessible, reviewing scenarios and developing action plans and next steps.
We will engage with a number of multi disciplinary professionals to ensure that the training provided is high quality and reaches our expectations.
The learning and education resources available on the South West Dementia Partnership website are free to access and enable learners to work through a comprehensive learning pathway. They are all web based within an e learning platform so can be accessed widely by the workforce and do not necessitate time away from practice.
PCH Final 20 June 2012 Page 10 of 62
Aims of the Programme:
•
Increase staff awareness of patient centred care and the production of patient centred care plans
•
Increase the initiation of early diagnosis of dementia
•
Increase knowledge and skills in relation to the completion of capacity assessments and understanding of deprivation of liberty and safeguarding issues
•
Increase the knowledge and skills of all staff in relation to dementia
•
Devise a care pathway and flow chart for patients with dementia
•
Reduce the delays that occur for people with dementia within our hospitals
•
Increase the use of purposeful occupation in both pilot sites
•
Work in a much more collaborative way with our 3 rd
sector providers and partner organisations
Outcomes:
•
Decreased incidents relating to safeguarding issues
•
Reduction in the length of stay for people with dementia
•
Increased patient and carer satisfaction
•
Reduction in the amount of incidents of patients experiencing distress
Dementia Care Mapping
Dementia Care Mapping (DCM) is a method designed to evaluate quality of care from the perspective of the person with dementia. It is used in formal care settings such as hospitals, care homes and day care. It is based on the philosophy of person centred care, which promotes a holistic approach to care that upholds the personhood of the person with dementia. The process of using DCM involves briefing staff and clients about DCM in the area to be mapped, observing a number of people with dementia over a period and recording information about their experience of care, analysing and interpreting the data and then feeding it back to staff. This information is then used to draw up an action plan to bring about change and improvements. DCM has also been used as a focus for staff training and development and as an aid to care planning.
We are planning to send two members of staff on the training course so that we can start to map the quality of care provided to our patients with dementia.
Priority 5 Complaints Handling
To improve the timeliness of complaints handling, we will enhance the quality of root cause analysis and investigation of incidents and ensure learning across the organisation. We encourage patients to tell us how we can improve services. When patients make complaints about our services we want to ensure we provide feedback regarding our investigations in a timeframe which the patient feels is realistic and shows them how seriously we take any complaint.
In investigating complaints we want to ensure that learning is shared throughout the organisation and that patient outcomes are reviewed. We will reorganise the method by which we investigate complaints, and restructuring who will undertake investigations of serious incidents.
PCH Final 20 June 2012 Page 11 of 62
2.0 Review of Services provided
During 2011/12 Peninsula Community Health provided and/or sub-contracted 36 NHS services. The income generated by the NHS services reviewed in 2011/12 represents
100% of the total income generated from the provision of NHS services by Peninsula
Community Health for 2011/12.
Peninsula Community Health works from over 100 locations throughout Cornwall and the
Isles of Scilly including 14 community hospitals. Peninsula Community Health reviews all the data in regard to these services monthly.
2.1 Care Quality Commission
Peninsula Community Health is required to register with the Care Quality Commission and its current registration status is without condition.
The Care Quality Commission has not taken any enforcement action against Peninsula
Community Health during 2011/12.
Peninsula Community Health is compliant with the regulations/outcomes as set out in the
Health and Social Care Act 2008.
Peninsula Community Health has not participated in special reviews or investigations by the Care Quality Commission as at 31st March 2012.
The Care Quality Commission has visited 5 of our community hospitals. The most recent visit was in January 2012, where no serious concerns were raised. Two improvement actions were required, referring to lack of documentation in some discharge plans and prescribing practices for patients on multiple medications. Both have an action plan, progress with which is reported to the Board.
2.2 Research
In 2010/11 Peninsula Community Health recruited two research nurses. These nurses work with the Research team at Royal Cornwall Hospital to enhance the research to improve patient outcomes.
2.3 Audit participation
Clinical Audit
Clinical audit is a systematic process of improving the quality of patient care by looking closely at current practice, evaluating the quality of care provided to patients based on best practice and nationally set clinical standards, modifying it where necessary and evaluating the outcome.
PCH Final 20 June 2012 Page 12 of 62
The main aim of clinical audit is to provide assurances that the clinical services are meeting the needs of service users and at the same time providing internal assurance that staff are following best practice based on research evidence.
Peninsula Community Health is committed to improving the quality and outcomes of patient care by establishing a culture where high quality clinical audit can be sustained. The 2011-
12 Audit Plan incorporated a programme of approximately 40 clinical audits in addition to a record keeping audit of all services and national clinical audits which the organisation was eligible to participate in.
National Clinical Audit Participation
Although it is not mandatory for community health services to undertake national clinical audits it is seen as good practice.
During 2011/12, Peninsula Community Health participated in 100% of the national clinical audits which it was eligible to participate in. Peninsula Community Health participated in no national confidential enquiries.
The national clinical audits that Peninsula Community Health participated in, and for which data collection was completed during 2011-12 are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry.
Number of cases submitted
Number of cases submitted as a percentage of required
cases
Parkinson’s occupational therapy audit
Parkinson’s physiotherapy audit
20
20
100%
100%
Peninsula Community Health has also taken part in the Continence national audit pilot which is testing new technology for national audit before being rolled out nationwide. An action plan will be compiled once the final report is received.
Peninsula Community Health has also recently taken part in the new Intermediate Care national audit. This will be reported in 2012-13 and an action/improvement plan put in place following receipt of the final report.
Improving services through participation in national audits
The reports of the two Parkinson’s national audits will be reviewed once received and an action plan put in place.
Clinical audit is supported by the Governance team. All local clinical audits are reported to and monitored by the Clinical Quality and Safety Committee. Reports are reviewed and action plans for quality improvement are reviewed through this committee.
PCH Final 20 June 2012 Page 13 of 62
The following table lists pertinent audits that were carried out throughout 2011-12. It is, by the dynamic nature of audit, not fully comprehensive, but includes all relevant information for significant audits and action plans.
Local Audit Actions planned/taken
Community Hospitals
After Death analysis
The audit demonstrated a clinical awareness of recognising changing/deteriorating condition and identification of expected death but highlighted a lack of confidence in acknowledging expected death with patients, families and carers. As a result there will be an education programme put in place to support the roll out of the Gold Standards Framework pilot to help build confidence among clinicians.
Snapshot audit regarding the quality of referrals to the podiatry specialist musculoskeletal clinics
Resuscitation equipment audit
Record keeping audit
The audit identified that Podiatry musculoskeletal referral forms are not being universally completed by podiatrists in podiatry specialist musculoskeletal clinics and in a number of cases all appropriate information was not detailed on the referral forms. As a result an action plan has been put in place to deliver more training to podiatrists on correct completion of the form and to deliver more training on diagnosis and treatment of podiatric musculoskeletal conditions via supervision, mentorship and group training. Action to reinforce the message to podiatrists that the musculoskeletal podiatry referral form should be employed when was implemented. A re-audit will take place in April 2012 to monitor service improvement as a result of the actions taken.
The audit identified that not all sites had sealable dressing trolleys. In line with the CQC compliance assessment sealable trolleys are now at all sites. A full operational check of all MRX defibrillators to be undertaken and documented on a weekly basis. Trolley contents to be limited to those in the agreed equipment list unless variations are agreed by the resuscitation team. Repeat audit planned for 2012/13
A comprehensive record keeping audit was undertaken of all services. One of the key areas identified was use of the NHS number on all documentation. This is to be reinforced through team meetings in each service. Other service specific areas for improvement were identified for each service and are the subject of individual service action plans to be communicated via service team meetings. A re-audit in the next 12 months will monitor the effectiveness of the action plans in maintaining and improving record keeping quality. Overall, there was an improvement in the findings compare with the audit in previous years.
PCH Final 20 June 2012 Page 14 of 62
Missed doses audit
Compliance of antibiotic prescribing audit
Clinical Quality
Prescribing-
Prescription Chart
Audit
An audit was undertaken to investigate the causes of missed medication to support the NPSA/2010/RR009 Alert and CQC
Essential Standards Safeguarding and Safety Management of
Medicines. On some wards the number of missed doses was above the target level. The results of the audit have been communicated to all nursing staff. Further actions planned are for all wards to be checked to ensure they have access to the missed doses National Patient Safety Agency alert guidelines. A review of the critical list and Standard Operating Procedure for
Delayed and Omitted Doses is to be undertaken as well as ongoing monitoring of incident reporting of missed doses and feedback to staff.
The audit identified that compliance with guidelines was up from
86% in March to 95% in September and documentation of the indication for the antibiotic was 100%. To further improve performance refresher training is being providing for nursing staff to update skills to administer IV antibiotics. Nursing staff are being trained to access microbiology results and request antibiotic review. The results of the audit have been shared with the community hospitals, prescribers, and other health delivery partners in Cornwall. Training has also been provided on the risks of Colostridium Difficile from antibiotic prescribing.
The standard of documentation in this audit was found to be generally high when compared to the ‘Policy for the Safe
Ordering, Prescribing and Administration of Drugs in Community
Hospitals and Minor Injury Units’. Following the audit a number of actions have been identified which will be monitored through annual Prescription Chart audits to identify improvements in clinical documentation. The results of the audit have been circulated to all staff and prescribers. Training is being planned for nursing staff on documentation on the new drug chart.
Training is also planned for prescribers on safe prescribing using the new drug chart. The drug chart will be further developed to facilitate compliance with Prescribing and Administration guidelines as per agreed Peninsula Community Health policy.
PCH Final 20 June 2012 Page 15 of 62
2.4 Goals agreed with commissioners
CQUIN – A proportion of Peninsula Community Health income in 2011/12 was conditional on achieving quality improvement and innovation goals agreed between Peninsula
Community Health and our commissioners NHS Cornwall & Isles of Scilly. The 2011/12
CQUINs in the chart below have all been achieved.
CQUINs 2011/12
Venous-thromboembolism
1
To reduce avoidable death, disability and chronic ill health from Venous-thromboembolism (VTE)
Patient Experience
2
To implement the nursing metric system across community services to include patient survey showing an improvement in patient experience
3
End of Life Care
Increasing number of patients who have expected deaths and are placed on the Liverpool
Care Pathway in community Hospitals
4
Long Term Conditions
All patients over the age of 75 screened for frailty on admission to community hospitals
5 Personalised Care Planning
Improve personalisation of care planning and self-management
6
7
Community MEWS
Stroke NICE Quality Standards
100% of all in patients in community hospitals should have CMEWS completed according to
CHS policy
Patients with stroke are offered a minimum of 45 minutes of each active therapy that is required for a minimum of 5 days a week.
8 Prescribing
Full (Level 2) Medicines Reconciliation completed for 95% of inpatients within 24 hours or admission to the Community Hospital
The philosophy of the framework is to bring health gains for patients recognising quality improvements and innovation and rewarding Peninsula Community Health with a percentage of income.
The CQUINs for 2012/13 have been agreed with NHS Cornwall & Isles of Scilly and they are:
National: Venous-thromboembolism
1
To reduce avoidable death, disability and chronic ill health from Venous-thromboembolism (VTE)
PCH Final 20 June 2012 Page 16 of 62
2
3
4
5
6
7
8
National: Patient Experience
National: Dementia
National: Safety Thermometer
To improve patient experience in 3 areas identified as requiring improvement in community hospitals through the patient experience metrics
Improve awareness and diagnosis of dementia, using risk assessment, in a community hospital setting
Improve collection of data in relation to pressure ulcers, falls, urinary tract infections in those with a catheter and venous-thrombus emboli.
Local: Reduction in avoidable emergency admissions
To reduce avoidable emergency admissions of frail elderly patients
Improve the care of patients with long term conditions
Increase telehealth across cornwall
Support Plymouth’s ‘Shifting settings of
Care Programme’
To reduce the length of stay at Liskeard Hospital
Support Plymouth’s ‘Shifting settings of
Care Programme’
To increase Chronic obstructive pulmonary disease rehabilitation in line with the National
Institute of Clinical Excellence
9 Improve patients’ outcomes To Improve outcomes for 2 specific conditions
2.5 Data Quality
Good data quality is an indicator that an organisation has robust systems and methods for capturing accurate information about their patients. Peninsula Community Health submitted records during April 2011 – March 2012 to the Secondary User Service for inclusion in the
Hospital Episode Statistics which are included in the latest published data. These are one of the measurements that the Care Quality Commission use within the monthly Quality and
Risk Profile, to monitor our ongoing compliance. As per the SUS Data Quality Dashboard
Apr11-March12, the percentage NHS number compliance:
NHS number compliance:
Inpatient = 100%
Outpatient = 100%
Minor Injury Units = 97.9%
GP Practice compliance:
Inpatient = 100%
Outpatient = 100%
Minor Injury Unit = 98.5%
PCH Final 20 June 2012 Page 17 of 62
2.6 Information Governance
Peninsula Community Health Information Governance Toolkit for 2011/12 has scored 75%.
This area of work was also subject to an internal audit during 2011/12.
2.7 Clinical Coding Error Rate
Peninsula Community Health was not subject to the Payment by Results clinical coding audit during 2011/12 by the Audit Commission.
PCH Final 20 June 2012 Page 18 of 62
3.0 Review of our Quality and Safety Performance 2011/12
3.0.1 Performance Review – The priorities we identified in 2011/12
PATIENT SAFETY
3.0.2 Identification and Management of the Deteriorating Patient
We said all patients were to have observations undertaken by staff who are trained to identifiy the early warning signs of deterioration – and they are.
Early identification of a deterioration of a patients condition and ensuring that they receive the correct treatment in a timely manner, not only reduces harm, but reduces the length of time a patient will need to spend in hospital and improves the quality of their recovery.
We have implemented a new patient observation chart across all our community hospitals which includes an early warning score calculated from the results of those observations.
The early warning score identifies the patients who are at risk of deterioration and alerts the staff to the required action to take; this may be to call a doctor, alert the senior nurse, or to increase the frequency of observations further, depending on the level of risk of deterioration identified.
A new observation policy has been published to guide staff, and all patients in all community hospitals have a full set of observations including the early warning score, recorded twice per day as a minimum.
As you can see from the chart above, the number of patients having twice daily observations has increased month on month and at March 2012 100% patients in all our community hospitals received twice daily observations.
We have also implemented a new communication tool for staff to use to alert medical staff to deterioration in a patient. This tool is called SBAR (Situation, Background, Assessment
PCH Final 20 June 2012 Page 19 of 62
and Recommendation). It provides a structured, standardised method of communication and assists staff in ensuring messages are delivered and received effectively.
Staff training in use of the tool has been completed.
Each month we check compliance to undertaking observations and that the right action has been implemented, by completing the Nursing metrics indicators.
3.0.3 Venous Thromboembolism
Prevention of Venous Thromboembolism (VTE) – undertaking risk assessment and appropriate preventative treatment for all patients admitted to a community hospital
We believe that 100% of our patients should receive assessment and treatment and we are working hard to achieve this.
VTE is recognised as a condition that causes a significant number of deaths per annum, many of which could be avoided; it is estimated that 25,000 people die needlessly every year. Fulfilling the NICE screening and treatment guidelines will save lives and prevent avoidable stays in hospital.
As you can see from the charts, we have consistently improved our position and by March
2012, 98% patients have a VTE risk assessment and 100% of these are on appropriate preventative treatment.
PCH Final 20 June 2012 Page 20 of 62
During 2009/10 patient risk assessments and treatment policies were developed and implemented across all community hospitals in Community Health Services, in line with
National Institute of Clincal Excellence Guidelines. This guidance states that 90% of all patients should have a VTE assessment on admission.
We monitor compliance monthly and any drop below 90% requires immediate action. This priority will form one of our CQUINs and shows our commitment to reducing unnecessary harm and death.
‘
We aim to provide patient care that is safe, effective and high quality for all patients and service users.
Patient safety is the organisation’s number one priority.’
Helen Newson
Director of Nursing and
Professional Practice
3.0.4 Reducing Avoidable Pressure Ulcers
Prevention and Management of Pressure Ulcers
Zero tolerance of avoidable pressure ulcers
Understanding why pressure ulcers occur and working to prevent avoidable occurrences is an area of work that has been a priority for us in Peninsula Community Health throughout
2011/12.
All pressure ulcers, developed before, during or after admission to hospital, are reported by staff using a nationally recognised grading system. All occurrences of grade 3 and 4 pressure ulcers have a detailed investigation, called a root cause analysis. Any learning about how the ulcer may have been prevented is shared across all our services.
A new form of risk assessment and monitoring of all patients’ skin, called the Skin Bundle, has been implemented in our community hospitals. Many of our hospitals have no reported pressure ulcers that have developed after a community hospital stay for over a year.
The Tissue Viability team is managed by a Lead Practitioner who provides strategic lead and clinical leadership to two Tissue Viability Nurse Specialists (TVNS) who provide
PCH Final 20 June 2012 Page 21 of 62
assessment, education and support across CHS. The TVNS’ work closely with Tissue
Viability Link nurses across the NHS and independent sector. The Tissue Viability Service works closely with all members of the multidisciplinary team, secondary care, Social
Services, the independent sector and voluntary groups in order to ensure seamless care for the patient and carers.
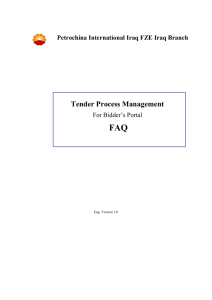
Community Hospitals achieved a 50% reduction in the year 2010-2011, a further 30% reduction has been achieved this year (2011-2012). The aim is to reduce by a further 20%.
C ommuni t y H os pi t a l s I nc i de nc e 2 0 1 1 - 2 0 1 2
65
60
55
50
45
40
35
32 32
30
25
20
15
22
17
16
21
17
21 21
15
18
10
5
0
APRIL
10
M AY
0
JUNE
10
6
JULY
8
A UG
2
6
SEPT OCT
M ON T HS
4
1
NOV
1
DEC
2
JAN
3
FEB
3
0
M ARCH
ADMITTED WITH
UNAVOIDABLE
DEVELOPED ON WARD
Cumulat ive 2009- 2010
Cumulat ive 2011 Cumulat ive 2010
We recognise that the existing good performance of our hospitals needs to be maintained and we are working towards a zero tolerance of any preventable pressure ulcer across all our services, not just hospitals.
PCH Final 20 June 2012 Page 22 of 62
Clinical Effectiveness
3.0.5 Ensure effective pathways of patient care
As patients move from differing care providers and from inpatient to community, we want to ensure appropriate follow-up, continuity of clinical care, reducing length of stay and reducing delayed discharges
Embedded improving quality is ensuring we are providing not just the right services, but also in a place where the patient feels most comfortable and promotes their independence.
As patients move from differing care providers and from inpatient to community, we want to ensure appropriate follow-up, continuity of clinical care, reducing length of stay and reducing delayed discharges. Peninsula Community Health continues to be a key member of the implementation of the Early Intervention Teams, where services will be provided seamlessly and in a manner that is timely for the needs of the patient.
95% of all relevant Peninsula Community Health Staff have received training in undertaking personalised care plans for patients with a long term condition.
Frailty screening has been introduced in all community hospitals to ensure that frail elderly patients are identified and are offered a comprehensive multidisciplinary assessment with a personalised care plan. As of the end of March 2012, 95% of appropriate patients within our community hospitals have received a frailty assessment.
Tele-health continues to expand. Telehealth allows patients to record vital signs such as blood pressure using simple-to-use biometric equipment installed in their homes.
Telehealth Nurses, community matrons and specialist nurses, who can intervene early if they are needed, monitor the data remotely. Telecare packages are also being provided to help people with dementia or at risk of falling to stay at home more safely, using devices that track movements and prevent incidents such as the bath overflowing. Patients are more able to understand and take control of their care and remain where they want - in their own homes. For telecare users there is reassurance to the clients and carers.
The Telehealth service is run centrally through a team of 15 people (13 FTE). This comprises a Telehealth Lead / Manager, clinical team of Telehealth Nurses, Field Staff and administrators. Eighty percent of the clinical monitoring is carried out through the central service and twenty percent through the community matron and specialist nurse teams.
As mentioned within our priorities for 2012/13, we will work hard to improve care for patients with Dementia and their families.
3.0.6 Patient Information
Patient Information
To improve the quality of information provided to patients when they come
into a community hospital
We recognise that coming into hospital can be a very stressful time for patients, their carers and family. From the information we have gathered this year from patients, visitors and
PCH Final 20 June 2012 Page 23 of 62
family we know that we need to improve the information we provide to patients on their admission to hospital.
The Community Hospital matrons continue to update leaflets, ensuring that information such as ward telephone numbers, times for meals, the availability of food and drink 24 hours a day, identifying the patient’s doctor and when they visit, is included in this leaflet.
Information leaflets have been developed for people with Learning Difficulties. These have been developed together with the CHAMPS. Information leaflets include:
•
About the Learning Disability Liaison Nurse Service
•
Traffic Light Hospital Passport
•
How to make a complaint
•
Comment Card
•
Leaving Hospital
•
Consent – Saying Yes or No
•
Carer’s Information
Patient Experience
3.0.7 Improving the patient experience
Improve the patient experience within the Community Hospitals and in the wider community services
We want to ensure that all patient feedback is utilised to improve future experiences and we want to show the local community how important their comments and concerns are to us. We will use the ‘you said we did’ methodology.
Throughout 2011/12 we have gathered patient experience feedback from all inpatient areas. This information allows real time changes of practice and provides patients with assurance that we take their concerns seriously. Peninsula Community Health has developed its own bespoke tool for gathering this information and means we can be responsive and quick to change the questions if we find more detailed analysis is required about an area of concern.
One year on, the Patient Experience Metrics demonstrate consistent and sustained good results for:
•
Patients who say they find the ward (including bathrooms and toilets) ‘very’ clean
•
Patients who say that staff ‘always’ clean their hands between caring for different patients
•
Patients who say they have not shared a sleeping area with a member of the opposite sex.
Notable improvements over the year are
•
Patients who say they receive enough help from staff to eat their meals
PCH Final 20 June 2012 Page 24 of 62
•
Patients who say they are not bothered by noise at night
•
Patients who say they receive enough information about their medications
•
Patients who say they feel involved in decisions about their care and treatment.
These improvements have been achieved by staff responding to the metrics results and patient comments in an effort to improve the care they deliver. Noise at night is a good example as feedback prompted the purchase of waste bins with slow-closing lids. It also served as a reminder to staff to make increased effort to reduce the noise they make at night. Staff have also said that when they give medications to patients, they take a little more time to ask the patient whether they would like to know more about their medicines.
There are some areas where there is still room for further improvement:
•
Patients who say they like the food
•
Patients who say they have been given enough information about their condition and treatment
•
Patients who feel they have been talked to about their discharge from hospital.
These three issues will be addressed formally, with action plans, during 2012/13.
Other areas of our Quality Performance in 2011/12
3.1 Maintaining Essential Standards for Registration with the Care
Quality Commission
Peninsula Community Health is required to register with the Care Quality Commission and its current registration status is without condition. The Care Quality Commission has not taken any enforcement action against Peninsula Community Health during 2011/12.
Peninsula Community Health is compliant the regulations/outcomes as set out in the Health and Social Care Act 2008. Peninsula Community Health has not participated in special reviews or investigations by the Care Quality Commission as at 31st March 2012.
3.2 NHSLA Assessment
There was no formal assessment for general NHSLA standards during 2011/12.
3.3 The Musculoskeletal Interface Service
Background and Introduction
The Musculoskeletal (MSK) Interface Service started life as the Orthopaedic Triage Service in December 2005 as a project developed by the West and Central Cornwall Primary Care
Trusts. The North and East joined shortly after and the service became know as the
Orthopaedic Clinical Assessment Service (OCAS) and now the MSK Interface Service.
Originally the Service only dealt with patients with hip and knee problems but it has expanded to included shoulder patients and there is also a small spinal pilot running.
PCH Final 20 June 2012 Page 25 of 62
The Service was originally staffed by Orthopaedic Specialist Physiotherapists and an
Orthopaedic Specialist Occupational Therapist but since 2010 there have also been GP’s with Special Interest (GPwSI) working alongside.
There is currently no GPwSI working within the East Cornwall part of the service, primarily due to no pilot being developed in this area. It is anticipated that as the Interface expands further, GP commissioners may consider authorising additional resource.
The MSK Interface Service also provides specialist Occupational Therapy intervention for both home assessment and specialist bracing. There have been an increasing number of braces provided to patients. Specialist bracing can lead to a reduction in the need for surgery in some patients, supporting an in year cost saving.
There has also been a small spinal interface pilot running since 2010 funded jointly by
Practice Based Commissioning savings and Peninsula Community Health. This pilot is due to end and is hoped to be extended if resources become available.
1. Referral Rate (excluding Spinal Pilot)
Referrals are received by ‘Choose and Book’ and written referral, either directly from the
GP’s/Physiotherapists or via the Kernow and Sentinel Referral Management Centres.
There has been a significant increase in referrals into the MSK Interface with 668 additional referrals being received in Apr – Dec 2011, compared to 2009, and 440 more compared to the same period in 2010. This increase has been in the mid and West Cornwall service.
Referrals Received by MSK Interface Apr to Dec 2009 - 2011
250
200
150
100
2009
2010
2011
50
0
April May June July Aug Sept Oct Nov Dec
2009
2010
103
116
129
116
117
159
145
129
110
149
160
134
140
189
77
201
92
108
2011 147 202 225 197 200 215 191 226 138
2. Clinic Sites
The MSK Interface Service offers clinics across the county and patients are able to access that which is most convenient for them
Clinics are currently held at the following locations:-
PCH Final 20 June 2012 Page 26 of 62
•
St Barnabas, Saltash
•
Liskeard Community Hospital
•
Launceston Community Hospital
•
Stratton Hospital
•
Bodmin Hospital
•
St Austell Community Hospital
•
Newquay Hospital
3. Key Headlines
•
Camborne & Redruth Community
•
•
•
•
•
•
Hospital
St Michaels Hospital, Hayle
West Cornwall Hospital
Helston Medical Centre
Truro Health Park
Falmouth Hospital
Falmouth Health Centre
•
Mid and West Cornwall clinics (excluding Spinal Pilot)
85% of all patients seen have been managed within the primary and community setting
88% of all patients were seen within 4 weeks of receipt of referral
64% of all patients were seen by Orthopaedic Specialist Physiotherapists
36% of all patients were seen by GPwSI
Number of patients: Number
New patients seen
Follow-ups seen
New patients referred to secondary care
Follow-up patients referred to secondary care
Number of joint injections given
DNA
Patients referred to Physiotherapy
1296
464
191
74
108
10
198 (11% of total contacts)
Patients referred to Interface OT
X-rays requested
MRI’s requested
Ultrasound requested
241 (14% of total contacts)
142 (8% of total contacts)
48 (3% of total contacts)
27 (2% of total contacts)
PCH Final 20 June 2012 Page 27 of 62
•
East Cornwall clinics
64% of all patients seen have been managed within primary and community setting
95% of all patients were seen within 4 weeks of receipt of referral
Number of patients: Number
New patients seen
Follow-ups seen
357
88
New patients referred to secondary care
Follow-up patients referred to secondary care
Number of joint injections given
DNA
Patients referred to Physiotherapy
Patients referred to Interface OT
X-rays requested
128
36
2
0
63 (14% of total contacts)
33 (7% of total contacts)
8 (2% of total contacts)
MRI’s requested 7 (2% of total contacts)
Ultrasound requested 0
•
The East Cornwall clinics have a higher percentage of hip patients which require greater referral into secondary care and a very low percentage of shoulder patients many of whom are managed without secondary care referral.
•
There are also more injections carried out in the Mid and West Cornwall clinics and this is due to the higher percentage of shoulder patients being seen.
3.4 Parkinson’s Disease Service
During 2011/12 the Parkinson’s team has undertaken the following projects to improve patient and quality:
Patient Experience within Royal Cornwall Hospital
- added a red flag onto the Hospital PAS system so that the Parkinson’s Nurse Specialist team is alerted when a patient is admitted to hospital
Promotion of self management
- Piloting telehealth through use of symptom monitoring for people with Parkinson’s
PCH Final 20 June 2012 Page 28 of 62
Improving Patient Experience at Diagnosis
- Improving the care pathway from GP through to medical consultant and subsequently the
Parkinson’s Specialist Nurse through development of the Parkinson’s Map of Medicine.
- Undertaking a patient survey entitled “Patient’s Experience of Referral, Access and
Consultation” to benchmark current services
- Exploring new ways to improve referral, access and consultation
Access to Therapy Services
- Physiotherapy, Occupational therapy and Speech & Language therapy participated within the national Parkinson’s UK national audit to benchmark therapy services.
Provide Equitable Service for people with Parkinson’s
- Two disease specific education / exercise groups for people newly diagnosed and those with more advanced PD have been running in the West of the county. Funding has been obtained to pilot 4 groups over Mid / North & East Cornwall. These will run in 2012 / 2013.
Improve Patient Experience, Communication between Cornwall & Devon Parkinson’s
Services
- A neurologist from Derriford Hospital has taken over the running of the Parkinson’s clinic at Liskeard on a monthly basis. This improves patient experience and enable Cornish patients to be cared for locally.
Formalising the Care Pathway for people requiring Apomorphine Therapy / Deep
Brain Stimulation
- Two clinics are co-ordinated by the Nurse Consultant for people with Parkinson’s requiring the above treatments.
Continuation of Parkinson’s Hubs
- Three Hubs run for people with Parkinson’s over the county. This was initially a collaboration between Cornwall & Isles of Scilly PCT, The James Parkinson’s Centre
(Charity Organisation) and the Rotary Club. These take place on a monthly basis and enable people with Parkinson’s to seek education, support, exercise etc. http://www.csupport.org.uk/wp-content/uploads/2012/03/826-NCS-QIPP-publication-FINAL-
NO-MARKINGS.pdf
(pg 21)
Proposed Plan for 2012 / 2013
Improving the hospital experience for people with Parkinson’s disease so that medications are provided on time and delayed discharges / readmissions do not recur
- Audit patient experience of Hospital admissions April 2012
- Provide education, information to people with PD when admitted to Hospital
- Promote the Red Flag within Hospital PAS system
- Provide education to Pharmacists within RCHT and develop of a check list for use when
Pharmacists visit the wards.
- Work with Service Development team at RCHT to improve the Hospital experience for people with Parkinson’s
- Work with SWAST to ensure medications are taken into Hospital with the patient
PCH Final 20 June 2012 Page 29 of 62
Promotion of Self Management
- Develop Parkinson’s database to enable personalised care plans to be uploaded onto the database. Parkinson’s teams can then down load the PCP when a patient is admitted to
Hospital etc
- Provide PCP template to people with Parkinson’s through educational events / hubs
- Further develop telehealth/telecare for the Parkinson’s service looking at providing step down services for some people with Parkinson’s.
Provide equitable service for people with Parkinson’s
To pilot 2 newly diagnosed groups within the St Austell and Bodmin / Camelford area. To pilot 2 other groups within the same areas for people with more advanced Parkinson’s
Continuation of the Parkinson’s Hubs
- To promote self management, empowerment and to reduce follow up appointments within the Hospital out patient department
3.5 NHS Southwest Early Warning Trigger Tool
This tool identifies the potential for deteriorating standards in the quality of care delivered by a team in a ward area. It provides a set of organisational indicators which when taken together, give an indication of how well an individual team is functioning. Every month each ward completes the tool and it allows the ward sisters and their teams to identify if there is any particular area that may compromise the quality of care.
3.6 Equality Delivery System Assessment and Equality Objectives
The Equality Delivery System is an assurance tool through which organisations can assess their performance against the Public Sector Equality Duty 2010. It requires an organisation to rate and evidence performance against four EDS outcomes within which there are 18 factors.
For each outcomes, one of four grades can be chosen:-
Excelling Purple
Achieving
Developing
Green
Amber
Undeveloped Red
Excelling – indicates a high quality practice, and evidence of full partnership working and innovation
Undeveloped – practice is poor and/or evidence is not available and /or local interests have not been engaged.
Following engagement with stakeholders and staff, a self assessment with the EDS framework has been developed for Peninsula Community Health.
PCH Final 20 June 2012 Page 30 of 62
Consultation and Engagement
EDS grades must take into account stakeholder views across all protected groups and if there is a disparity of view on the grading applied, the views of stakeholders must take precedent. We have also used the recent Staff Survey and Health and Well Being data and extensive patient feedback eg. Nursing Metrics, in considering our ratings.
PCH has contributed to a range of events to promote Equality, Human Rights and the
Equality Delivery system including:
•
March 2011 - Multi-agency Inclusion event to develop a number of equality objectives for Cornwall and the Isles of Scilly
•
November 2011 - A Cornwall and Isles of Scilly-wide event at the Eden Project to introduce the principles of the Equality Delivery system and our plans for engaging with stakeholders;
•
January 2012 - A specific Learning Disability focus group to discuss our Equality activities and self assessment of our progress against the EDS outcomes;
•
January 2012 - A PCH staff focus group to discuss our Equality activities and self assessment of our progress against the EDS outcomes;
•
February 2012 - Two Cornwall and Isles of Scilly focus groups with members of the public and representatives of the voluntary and community sector (VCS);
•
November 2011 & February 2012 - Discussion about the single equality objectives for Cornwall and Isles of Scilly at the multi-agency Equality and Human Rights
Partnership
In setting our Equality objectives we have responded to the single equality objectives already agreed for Cornwall and Isles of Scilly, as well as feedback from focus groups which informed our assessment against the Equality Delivery system, and the range of resources including workforce the Staff Survey, patient and local demographic data.
We intend to focus on a number of core areas, mainly with a systems focus, in the coming year, which, once achieved, will help us to bridge gaps in our Equality intelligence, enabling us to identify some more qualitative objectives for forthcoming years.
The objectives for PCH for 2012-13 are proposed as follows:
1 To develop consistent protocols and standards around accessible information ensuring availability in a variety of formats thereby enabling patients to make informed choices about their healthcare**
2 To increase and improve the standard and collection of equalities monitoring data for patients and staff in order that PCH can clearly identify gaps and focus appropriate service provision to individuals and groups in the community; and to enable PCH to recruit / support underrepresented groups in the workplace**
3 To develop a learning and development package which supports staff to better understand the links between equality, human rights, enabling patient choice and enhancing patient experience
PCH Final 20 June 2012 Page 31 of 62
4 To improve the under-representation within the PCH workforce, with a specific focus on age (under 30 age group), gender (male) and employees with a disability **
** These objectives are part of the 9 Single Equality objectives for Cornwall and Isles of
Scilly
Work is continuing around these objectives to ensure that they are SMART and that each has an action plan attached.
3.7 Respiratory Nurse Service
The Respiratory Nursing Service is a county wide specialist service for adults with respiratory conditions such as Asthma, Chronic Obstructive Pulmonary Disease (COPD) and Pulmonary Fibrosis, and children with Asthma. This service provides direct care to patients and education for health and social care professionals.
Respiratory disease is set to rise to the 3 rd
most common cause of death in the world by
2020 (WHO, Lopez and Murray 1998). This condition affects 6% of men and 4% of women
(Barnes 1998).
Pulmonary rehabilitation programme for patients with COPD has been proved to reduce hospital admissions (Griffiths et al, 2000). Pulmonary rehabilitation has been shown to improve exercise tolerance and breathlessness and also to improve quality of life (Clinical
Review, 2011). Patients are encouraged to continue to exercise on their own or in an exercise group run by volunteers. This Cornish model has been running for 12 years and is recognised by the British Lung Foundation as part of the work involved in caring for respiratory patients in Cornwall.
As well as supporting pulmonary rehabilitation the respiratory service enhances patient care and experience by offering community hospital Arterial Blood Gas clinics and occasionally blood gasses taken in the home when the patient is unable to travel. This important service allows patients to be seen closer to home as many patients on oxygen find it difficult to travel far because of their disease.
Highlights of 2011-12
•
The team were part of an audit looking at Patient experience of pulmonary rehabilitation
(Discussed in Patient Experience Section)
•
There is a new post pulmonary rehabilitation group at Newquay. This aims to keep patients exercising once they have gone through a pulmonary rehabilitation programme.
•
The team is presently implementing a new pulmonary rehabilitation programme at
Torpoint.
•
Continued close liaison with the Walking group at the Eden Project. This again is for patients who have been through pulmonary rehabilitation. This walking group was featured in the British Lung Foundation ‘Breathing Space’ magazine in March 2012
•
Arterial Blood Gas clinics in the community hospitals and community settings. This is an excellent service for respiratory patients as it saves them having to travel to the district general hospital.
PCH Final 20 June 2012 Page 32 of 62
•
We continue to meet our targets for seeing patients started on long term oxygen therapy, and support hospital discharge patients with respiratory conditions.
We continue to provide teaching to other health care professionals to enhance respiratory patient care.
Plans for 2012-13
•
Improve the service for pulmonary rehabilitation and blood gas clinics in the county.
•
Continue to support and encourage the patient led groups to keep going and helping to support post pulmonary rehabilitation patients.
•
To improve communication with the acute hospitals to identify respiratory patients started on oxygen therapy so that they might be supported at home. Also any respiratory patients discharged from hospital to be followed up by a respiratory nurse for advice and education.
•
To provide teaching to other health care professionals to enhance respiratory patient care.
3.8 Reducing harm from falls
Peninsula Community Health has a team dedicated to the reduction in falls but there are also many other services which contribute to the shared aim of reducing falls and the harm caused by falls.
Within the Community hospitals we have seen a reduction in the harm caused by falls and in reduction in the overall number of falls. On review we feel this is due to a number of initiatives introduced during 2011/12.
PCH Final 20 June 2012 Page 33 of 62
Intentional Rounding
This is a method of ensuring regular, documented observation and assessment of inpatients identified at risk of falls. It is similar but not the same as ‘specialing’, where a patient is in need of one to one care. Policy includes guidance on intentional rounding and a specific care plan for documentation. The decision to use intentional rounding as part of a person centred care plan would be a local ward based decision taking into account the appropriate risk assessment.
Immediate assessment after a fall on the ward
The policy has considered NICE guidance on head injury to support best practice about the immediate assessment after a fall to ensure that no further harm is caused by inappropriate interventions. New inpatient documentation was commenced in October 2011, which provides a post falls care plan. Staff have to follow all the actions required and this has ensured patients get the right treatment post fall. An example of this is on the next page:
PCH Final 20 June 2012 Page 34 of 62
PCH Final 20 June 2012 Page 35 of 62
We have also redesigned the cotside/bedrail risk assessment and the staff feel this is much easier to use and helps in planning falls prevention care
3.9 Community Cardiac Services
Over the last two years there has been a review of the community cardiology services
(nursing and physiotherapy) followed by a complete service redesign.
The review and changes were in response to the Strategic Health Authority ambition to deliver comprehensive services, including cardiac rehabilitation to a wider group of cardiac patients. The Service has been redesigned to ensure that it meets the requirements within the DOH National Commissioning pack (DOH May 2010), the National Service
Specification and British Association of Cardiac Rehabilitation (BACR) standards.
The aim of the service is to ensure that the Cardiac Rehabilitation and Heart Failure services meet national priorities and local needs.
To ensure that some elements of Chapter 8 of the National Service Framework for
Coronary Heart Disease (management of arrhythmias, March 2000) and Quality Marker 2 of the National Stroke Strategy (Dec 2007), management of risk of stroke in patients with atrial fibrillation is achieved.
PCH Final 20 June 2012 Page 36 of 62
Improvements achieved to date include:-
•
The multi-skilling of existing staff to ensure they are competent to deliver all aspects of care required for both the rehabilitation pathways and the management of the more complex cardiac patients. Staff have accessed training including degree level heart failure courses, angioplasty plan training (facilitated patient management plan),
BACR courses on exercise for cardiac patients and the BHF Brief Motivational
Interviewing course.
•
The ability to offer a comprehensive cardiac rehabilitation programme to a larger number of patients including patients post myocardial infarction, coronary artery bypass surgery, valve or transplant surgery, post insertion of internal cardiac defibrillators and following elective or emergency coronary angioplasty.
•
The ability to offer an individual menu of choice to all patients, which includes core components of cardiac rehabilitation, lifestyle and risk factor management, cardio protective drug therapy / optimisation, exercise provision and psychosocial well being.
•
The case management of complex / unstable cardiac patients including patients with heart failure and those requiring palliative care.
•
The provision of high Supervision, as well as low Supervision exercise groups, across the county, so that more patients (including those with co-morbidities) are able to access an exercise component (ensuring the groups meet BACR standards).
•
The provision of data to the National Association of Cardiac Rehabilitation database.
•
Improving the identification of patients with Atrial Fibrillation by supporting public engagement events providing opportunistic pulse checks, and educational sessions to all clinical staff at every opportunity, on improving the diagnosis of Atrial
Fibrillation and stroke risk stratification.
Community cardiology services are delivered by Cardiac Specialist nurses, physiotherapists and physiotherapy support workers. The services are delivered in numerous ways (dependant on patient need) either within the patients own home, within a clinic or group setting and / or by telephone support.
The nurses are all BHF sponsored nurses. This ensures that they have an annual education / development grant. Clinical mentorship, which is invaluable, is provided by a consultant cardiologist, who facilitates at least four sessions yearly.
The Cardiac Services lead also works for 1 day a week with the Peninsula Heart and
Stroke Network on wider service improvement issues.
PCH Final 20 June 2012 Page 37 of 62
3.10 Medicines Management
The safe management and prescribing of medicines is a priority. The Pharmaceutical advisers have continued to provide practical advice and support to many healthcare professionals over the past 12 months.
2 of the CQUINs targets for 2011/12 have been medicine management focused. The venous thrombembolism target of attaining 95% of all patients admitted to a community hospital to have a completed documented VTE assessment is now well embedded in daily clinical practice, shown by the majority of units achieving 100% at monthly audit. In addition, 95% of those patients must be treated correctly and again we are able to demonstrate through audit this is being achieved. From the information collected at audit the VTE policy and audit tool have both been revised to support improved patient outcomes.
The second CQUINs target related to medicines management was to attain 95% of all patients admitted having their medicines reconciled to ensure that they are receiving the correct medication during their hospital stay. This CQUINs target has proved a challenge to collect the evidence. “Getting Medicines Right” is everyone’s responsibility- doctors, nurses, pharmacists and therapists should all play a part in ensuring that the patient receives the correct medication. Transferring patients between one care setting and another increases the risk of medicines being omitted or errors occurring in dosage etc.
A “Getting medicines right on admission” form has been developed and is now being trialled on all wards. The form prompts staff to request, collect and use certain types of information to ascertain that the patient is prescribed the correct medication. At least 2 different sources of information (e.g. patient’s own medicines, GP medication profile,
Discharge prescription) must be used to allow a full (level 2) Medicines Reconciliation to be performed by the medical practitioner. Data has been collected monthly since October
2011 when the form was first introduced. The baseline at this time for completing medicines reconciliation was 70% of all patients. With regular input from the pharmaceutical advisers the target of 95% of all patients admitted was achieved by the end of March 2012. The success of this year will be used to embed this important practice into the medical admission clerking process.
PCH Final 20 June 2012 Page 38 of 62
These 2 work streams are also part of the NHS South patient safety and improvement programme. This programme has provided materials and information to support the team in moving these projects forward to ensure the CQUINs targets are achieved.
Audit forms a very important role in demonstrating good patient care as well as highlighting areas of practice that may require change to improve patient clinical outcomes and safety.
The medicines management audits completed in 2011/12 have built on the experience and results of the previous year’s audit work. All 14 community hospitals were visited and a review of prescribing, administration and safe handling and storage of medicines was conducted at each site. As well as providing immediate feedback to the senior nurse on duty on the day the audit was conducted, results have been discussed with staff at all levels and action plans developed as necessary to support changes in practice.
Areas covered in the audit programme this year were:
•
Safe and secure handling and storage of medicines
•
Review of prescription charts
•
Prescribing of medicines, administration, missed doses
•
Prescribing of sip feeds, analgesics, “when required medicines”,
•
Use of pain assessment charts
•
Antibiotic prescribing
•
Antipsychotic prescribing
•
Controlled drugs
Results from these audits have been covered in more detail in another part of this report.
The audit work together with recommendations made by the Care Quality Commission following their visit to 5 community hospitals in March and April 2011 has supported the work to revise the inpatient prescription chart. The new prescription chart will be a booklet, divided into sections, which as well as listing the patient’s current medication will provide prescribers and nursing staff with important information on the safe prescribing and administration of medicines. The VTE assessment tool and “getting medicines right” forms will be incorporated into this document.
Trials of the new paperwork started in November 2011 and changes made at each stage of the trial. The next step will be to trial a small number of the new charts on each unit before going to print. The plan is to introduce, with training, a new prescription chart to the whole organisation by summer 2012.
Monitoring medication incidents and providing advice and extra training in response to these incidents forms a very important part of the pharmaceutical advisers role. The standard operating procedures for the management of controlled drugs have been revised and reissued during 2011 and this was supported by a series of workshops and training sessions for registered nursing staff. PCH works closely with, and is an active member of, the Local Intelligence Network for controlled drugs in Cornwall where information is shared and support and learning provided to manage controlled drugs safely in our community in line with national and local guidelines.
To continue to provide best care for our patients close to home, PCH has been reviewing its policy and procedures on the administration of intravenous medication and is developing a training package to support frontline staff.
PCH Final 20 June 2012 Page 39 of 62
Medicines management now appears as a regular agenda item on the Matrons, Joint
Sisters and District Nurses Forums providing opportunities for the sharing of information. A monthly “Pharmacy update” is produced by the Pharmaceutical Advisers. This provides the opportunity for the Pharmaceutical Advisers to inform and update staff of any important medicines management related topics.
Looking forward to 2012/13 we hope to launch the new prescription chart in summer 2012, continue to provide training in medicines management, and controlled drugs, support the work of the Non medical prescribers within PCH and build on the IV training programme.
We will strengthen the links already established with our nursing and therapy teams by attending their regular forums and ensuring medicines management is always included on the agenda.
In 2011 the policy for self administration of medicines by patients while in hospital was ratified. For 2012, the plan is to have a campaign to highlight the importance of this policy to support patients’ independence on discharge from hospital, and improve patients understanding and compliance with their medicines.
3.11 PEATS
The chart below shows the PEATS scores for 2011. The provider is shown as NHS
Cornwall and Isles of Scilly. These inspections took place prior to the formation of
Peninsula Community Health.
Organisation Name
CORNWALL AND ISLES OF SCILLY PCT
Organisation Code
5QP
Site Name
LAUNCESTON GENERAL HOSPITAL
CORNWALL AND ISLES OF SCILLY PCT
CORNWALL AND ISLES OF SCILLY PCT
CORNWALL AND ISLES OF SCILLY PCT
CORNWALL AND ISLES OF SCILLY PCT
CORNWALL AND ISLES OF SCILLY PCT
5QP
5QP
5QP
5QP
5QP
LISKEARD COMMUNITY HOSPITAL
STRATTON HOSPITAL
BODMIN COMMUNITY HOSPITAL
ST AUSTELL COMMUNITY HOSPITAL
FOWEY HOSPITAL
Site Code Environment % Food % Privacy & Dignity %
5QP04 84.85% 95.65% 86.67%
5QP07
5QP09
5QP11
5QP13
5QP14
96.94%
74.32%
95.81%
89.74%
81.14%
89.86%
71.01%
97.10%
91.30%
82.61%
90.77%
89.23%
94.44%
100.00%
90.77%
CORNWALL AND ISLES OF SCILLY PCT
CORNWALL AND ISLES OF SCILLY PCT
CORNWALL AND ISLES OF SCILLY PCT
CORNWALL AND ISLES OF SCILLY PCT
CORNWALL AND ISLES OF SCILLY PCT
CORNWALL AND ISLES OF SCILLY PCT
5QP NEWQUAY HOSPITAL
5QP FALMOUTH HOSPITAL
5QP15
5QP16
5QP CAMBORNE REDRUTH COMMUNITY HOSPITAL5QP17
5QP HELSTON COMMUNITY HOSPITAL 5QP18
5QP POLTAIR HOSPITAL
5QP EDWARD HAIN COMMUNITY HOSPITAL
5QP19
5QP20
87.43% 95.65%
80.13% 86.96%
89.66% 89.86%
92.03% 86.96%
81.10% 82.61%
90.01% 92.75%
98.46%
78.33%
93.85%
96.92%
75.56%
97.14%
CORNWALL AND ISLES OF SCILLY PCT 5QP ST MARY'S HOSPITAL 5QP21 91.52% 97.10% 98.33%
During 2011/12 Peninsula Community Health has continued to invest in the ward/hospital and health centre environments, to enhance patient experience. A number of wards have been redecorated and a major refurbishment of Stratton Hospital is underway, which will greatly improve the inpatient areas.
Poltair Hospital has undergone major building work to maintain and enhance patient safety.
PCH Final 20 June 2012 Page 40 of 62
3.12 Nursing Metrics and Patient Experience Measurement during
2010/11
Measuring, monitoring and improving Patient Experience
A key objective of reporting patients’ and carers’ experiences is to assure the organisation that those experiences have been listened to, acted upon and have influenced change in services and patient care. Crucial to being able to report the patient and carer experience is the effective collection and recording of their experiences, making it as easy as possible for patients, their families and carers to share their experiences with us. To improve the patient and carer experience it is important that there are the systems and processes by which those reported experiences are translated into action for improvement.
There is no single or simple route to understanding patients’ experiences and it is necessary to draw on a wide range of sources and types of information – formal and informal, real time and periodic, quantitative and qualitative, ad hoc and systematic.
Triangulating these various sources of intelligence to assess the reality of the situation is key.
Work undertaken during 2011/12:
Patient Experience Metrics
During 2011/12, the collection of Patient Experience Metrics was implemented and embedded across all Community Hospitals in Cornwall and the Isles of Scilly. This process is where patients, and sometimes relatives, are interviewed using a set of ‘patient experience’ questions. Every month all wards are visited by a member of staff whose usual role is not within that hospital team – this independence provides a degree of unbiased objectivity. Depending on the size of the ward, up to 10 patients (and sometimes relatives) are interviewed.
During the year the questions set have been revised and expanded to cover all the most important aspects of patient experience in a hospital ward. Answers to the questions provide monthly quantitative data – the ‘metrics’ – which is reported to the PCH Board.
Further discussion and probing of answers provides qualitative data that is fed back to the
Ward Manager and Matron by means of a monthly qualitative report. This methodology has proved very sound, providing context for the metrics. Reporting back patient views and actual comments is extremely powerful. Often this feedback is very positive and encouraging to staff, and when there is negative feedback this motivates immediate attention to issues that arise.
Findings have been discussed within 3.6
Hospital food
Food and drink served in hospitals is very important for a patient’s nutrition, and is also a very important part of their day and sense of wellbeing. Areas of work this year have included:
PCH Final 20 June 2012 Page 41 of 62
•
A pilot has taken place to offer an additional choice of a cooked breakfast and to ensure that both porridge and Readybrek are available for breakfast where previously only one choice was on offer. This is now being implemented on all wards.
•
Ward staff are being advised about food service, particularly on the larger wards where service always started at the same end and patients served last sometimes said their food was cold or choices had run out. Staff have been advised to alternate service and to take special care that food does not cool down before serving to the last patients.
•
An Oral Nutrition and Hydration Steering Group has now been set up. This Group will lead the development of an Oral Nutrition and Hydration Strategy to improve the quality of nutritional and hydration care that patients receive. The key objectives of the
Strategy will be to ensure patients’ nutritional and hydration needs are identified and met, and to improve patients’ enjoyment of the food and drink by ensuring suitable choices, the best possible quality and served in the best possible way. The Steering
Group will oversee planning and implementation of the Strategy and receive reports on performance from Patient Experience Metrics, Nursing Metrics, PEATS Inspections and ad hoc contract monitoring.
Information about condition and treatment
This is more difficult to address because there is a significant number of patients who say that they do not want to know more about their condition and treatment, preferring to ‘leave it to the doctor’. Some have said they feel they wouldn’t understand and would worry more.
However, this results in those patients who might want to know more, not receiving the explanations and information they would like to have.
•
Actions for the coming year will require that nursing and medical staff work together to ensure that patients are given information and have more opportunity – during ward rounds and after – to ask questions.
Being spoken to about discharge from hospital
Many patients say that no one has spoken to them about their discharge from hospital when it often transpires that staff say they have spoken to them about it and sometimes they have even have provisional discharge plans in place. It seems that some patients answer ‘No’ to this question if they haven’t yet got a definite discharge date so there is perhaps something in how this question is asked. It is also possible that patients might forget about initial conversations about discharge if it does not seem a reality to them at the moment.
•
The Hospital Discharge Leaflet will be included in bedside folders as part of the standard patient information provided to each patient. This leaflet provides room for staff and patients to write in details about discharge and will hopefully serve as a concrete reminder to patients that their discharge from hospital is being managed.
Parkinson’s Service
A survey of patients’ experience of referral, access and consultation in the Parkinson’s
Service was undertaken during 2011. The aims of the survey were:
•
To have a greater understanding of the timeframe from the onset of symptoms of
Parkinson’s, to first consulting their GP.
PCH Final 20 June 2012 Page 42 of 62
•
To understand patient experience from GP referral to a medical Consultant: how long this process took, choice of hospital and the quality of the first consultation.
•
To understand when the role of the Parkinson’s Specialist Nurse was highlighted to the patient and when referral took place.
•
To understand whether patients feel their follow up care fulfills their needs.
•
To explore patients’ views on having elements of their follow up care coordinated by the Parkinson’s Specialist Nurse, referring back to the Consultant when necessary.
Action planning is underway and potential topics for action under consideration are:
•
Increasing public awareness of the value of early diagnosis and treatment
•
Work with GP’s to procure more timely diagnosis and referral in compliance with NICE
Clinical Guidelines.
•
Ensuring patients know they can choose which hospitals provide appointments with
Consultants
•
Ensuring a focus on involving family members from the outset.
•
Ensuring patients leave their first appointment more knowledgeable, feeling listened to and that they could ask questions.
•
Enabling earlier input from the Parkinson’s Specialist Nurse
Migrant Workers
Cornwall is host to 8-13,000 migrant workers annually. Most migrant workers are treated well by employers who comply with legislation and health and safety obligations. However, migrant workers are often vulnerable and are not always able to seek help independently.
Often their supervisors are the same nationality and might not be closely supervised themselves which puts them in a great position of power over the workers. Migrant workers typically access health services by a 999 emergency call, by the out of hours GP service, walk in centres and Minor Injury Units. Supervisors often accompany the workers to hospital and expect to do the interpreting. There could be many reasons why they might withhold some information from the patient e.g. if they are on piece rate and will want the worker back at work as soon as possible. They might also intimidate them not to speak honestly about accommodation, health and safety training, working hours and conditions etc.
The Migrant Workers Safety Net, developed by Inclusion Cornwall, is a document for frontline staff who may encounter migrant workers. It gives concise and useful information about how best to help and support them. Inclusion Cornwall was invited to talk to Senior
Managers and to the MIU Forum to raise awareness of this and launch the Safety Net in our MIUs.
Physiotherapy Outpatients
LINk in Cornwall say they have received feedback that outpatient physiotherapy is difficult to access and requested that they be able to undertake a survey in PCH Physiotherapy
Outpatients. We have worked collaboratively with them to develop a questionnaire that will both answer questions that LINk members have and also provide data for our service to monitor the experience of patients. In the meantime we have checked our waiting times and found them to all be well within target waiting times.
PCH Final 20 June 2012 Page 43 of 62
Plans for 2012/13
Patient Experience Metrics
Measurement of key patient experience indicators will now be rolled out to other community services. A question set is currently being piloted with patients of the District Nursing
Service. Early indications are that a regular postal survey of 10 questions will be a better methodology than telephone interviews. Whilst provision could be made on the comment card for qualitative responses, it would lose the element of further probing of responses to questions. Including a tick box for patients who agree to be telephoned for a further interview is being considered.
TB Immunisation Service – Patient experience questionnaire survey
A questionnaire is being developed to measure the experience of people who bring their children for TB immunisation. As the majority of respondents do not speak English as a first language the questionnaire will be translated into the appropriate language. As well as providing information to inform us about the quality of the service provided, this exercise will also serve to demonstrate that we make reasonable adjustments to listen to the views of people with protected characteristics .
Dental Services – Patient experience questionnaire survey
A questionnaire is being developed to measure the experience of people accessing PCH
Dental Services. The objectives of this survey will be to ensure compliance with CQC
Standards around respect and dignity, consent to care and treatment, provision of information, personalised care, oral hygiene and dietary advice, cleanliness and infection control, information about medications and the care environment.
A separate piece of work targeted towards the care of people with Learning Disability in
Dental Services is also planned.
Dementia
Alongside a project to improve the care and welfare of people with dementia across PCH services, we will be developing a tool to measure patient and carer experience for people with dementia and their carers. This will help to compensate for the fact that the Patient
Experience Metrics tool is not suitable for collecting data from patients with communication and cognitive problems and they are therefore excluded from this process.
It is hoped that through this work, we will be able to develop a set of tools that can be used to measure patient and carer experience for people with a range of cognitive and communication problems caused by stroke, aphasia, brain injury, more profound learning disability and specifically for people with dementia.
Learning Disability
PCH is working to achieve full compliance with the Mencap Charter to ensure our services are accessible to people with Learning Disability (LD) and that we meet their needs.
Working with us are ‘CHAMPS’. CHAMPS are employees of Health Promotion; they are people with LD who represent patients with LD. The CHAMPS are currently undertaking assessments of the Minor Injuries Units and Outpatient Departments in all our Community
PCH Final 20 June 2012 Page 44 of 62
Hospitals. They are currently working through a programme of ‘pre-assessment’ where they make a planned visit to a hospital and use their audit tool to assess:
•
Whether staff know how to contact their LD Liaison Nurse
•
Whether staff know about and use ‘Hospital Passports’
•
Whether they have easy to understand information about health and health procedures
•
Whether staff have an understanding of and awareness of ‘reasonable adjustments’,
Mental Capacity laws and advocacy services
•
How they are spoken to
•
Whether they can find their way around
The LD Liaison Nurses together with the CHAMPS will then undertake a training programme in all our community hospitals (informed by the pre-assessments) to ensure that staff are informed and better able to meet the needs of people with LD. Following the training programme the CHAMPS will then make another round of unannounced visits to repeat the assessment.
Information leaflets have been developed for people with LD. These have been developed together the CHAMPS. Information leaflets include:
•
About the Learning Disability Liaison Nurse Service
•
Traffic Light Hospital Passport
•
How to make a complaint
•
Comment Card
•
Leaving Hospital
•
Consent – Saying Yes or No
•
Carer’s Information
These leaflets are due to be printed and in use before the final unannounced assessments.
3.13 Privacy and Dignity Visits
Dignity in Care Assessments
Dignity in Care Assessors assist NHS Cornwall & Isles of Scilly in achieving their key priority ‘ensuring patients and service users are treated with dignity and respect’ by monitoring the privacy and dignity standards set out in service level agreements with providers. They do this through unannounced visits to observe care environments, talking to patients and staff, and completing a Dignity in Care Audit Tool which covers the safety, cleanliness and maintenance of the patient environment; privacy, dignity and modesty; communication with patients; and equality and diversity issues.
All wards were visited during 2010/11 and action plans were produced in response to all issues found. Progress updates and reports have been given regularly to the Dignity in
Care Assessors Group, the last one in December 2011.
A new round of visits is now underway for 2012/13 and we look forward to receiving the assessment reports. These reports make a significant contribution to improving the patient experience in our hospitals. The Assessors study the ward environment, and ward activity, though the eyes of the service user. In so doing they highlight things that can be
PCH Final 20 June 2012 Page 45 of 62
overlooked during day to day ward activity such as ‘sticky’ locks and shower curtains that don’t quite meet, and they challenge perceived transgressions in maintaining patient modesty. In particular, their observations of inappropriate storage of equipment has been instrumental in forcing this difficult issue up the agenda. There are enormous constraints on storage space in our community hospitals, and a seemingly ever increasing amount of equipment. Matrons and ward teams have responded to this problem by rationalising equipment and, sometimes very creatively, finding alternative storage solutions.
3.14 Eliminating Mixed Sex Accommodation (ESMA)
Peninsula Community Health is fully compliant with ESMA and submits a monthly report.
No breach has occurred since reporting commenced in December 2010.
3.15 Complaints and Compliments
Peninsula Community Health takes seriously all complaints, comments and suggestions about our services. During the year 2011-2012 we received 111 complaints, 70 of which were made in writing and 41 were made verbally to staff. One of these was passed with consent to another NHS organisation to investigate and 6 were withdrawn. The remaining
104 complaints were about community health services.
254 PALS contacts were received during this year. 79 of these were referred with consent to other organisations for action and response, and one was not taken forward. The remaining 174 PALS contacts were about community services provided by CIOS
Community Health Services and latterly by Peninsula Community Health. Of these, 67 raised issues and concerns about care received. The remaining 107 sought advice, support or information or offered feedback. There were 45 requests for interpretation and translation services during this period.
The table below details the complaints and PALS contacts recorded during this period, in relation to the services concerned and compares 2011/12 performance with 2010/11
2010-11 2011-12
SERVICE
Community Dental Services
Community Hospital Services
Community Nursing Services
Physiotherapy Services
Podiatry Services
Complaints PALS Complaints PALS
7
58
10
7
1
6
74
20
16
11
15
47
14
10
2
24
45
15
16
11
Occupational Therapy
Adult SALT
Children’s Services (incl. child SALT)
Macmillan Services
RATS & CATS Services
1
0
5
3
3
6
1
6
2
0
0
0
0
2
0
PCH Final 20 June 2012 Page 46 of 62
0
2
0
0
0
Continence Services
Other Community Services
Interpretation/Translation
Services provided by other orgs
Withdrawn/not taken forward
Passed to Claims Department
Totals:
0
7
0
10
6
2
1
18
141
100
0
0
2
9
4
1
5
0
2
14
45
79
1
0
120 402 111 254
Top Five Issues arising from Complaints and PALS
There were some complainants and PALS contacts that raised one issue, and others raised concerns about more than one aspect of care. Of the concerns relating to Peninsula
Community Health, the 111 complaints received in 2011-12 raised a total of 149 issues.
PALS received 175 contacts about Peninsula Community Health provided services during the period, including 67 contacts raising 73 concerns. The issues raised by complainants and via PALS related to 23 services and were spread across 68 locations. The following table shows a breakdown of the top 5 issues raised during this year, compared with those raised in the previous year.
ISSUE/Category
All aspects of clinical treatment
Access to services (incl. admission, discharge, transfers, outpatient appointments, delays, cancellations, transport and waiting times)
Communication/information to patients
Attitude of staff
Aids, appliances, equipment, premises
2010-11
57
18
34
22
6
34
53
20
13
13
51
16
29
29
7
2011-12
Complaint PALS Complaint PALS TOTAL
55
60
15
11
7
106
76
44
40
14
Actions and Learning arising from Complaints and PALS
We place an emphasis on resolving complaints and PALS concerns as quickly and effectively as possible, and in a way that is both proportionate and agreed with the complainant. The investigation of individual complaints identifies actions to be taken to reduce the risk of the complaint recurring. Work is ongoing across Peninsula Community
Health to ensure that learning from individual complaints is spread across the organisation.
Where any part of a complaint is upheld, the complainant always receives an apology, an explanation and information about the actions identified and taken to address the issue.
Some PALS issues require a level of investigation and the same principle applies where the findings agree with any aspect of an issue. There are also occasions when suggestions are made, for example to improve an environment or a service procedure and, where appropriate these ideas are acted upon.
Listed below are some examples of the actions identified during this year following investigation of complaints and concerns:
PCH Final 20 June 2012 Page 47 of 62
•
Outpatient nurses will advise the receptionist if clinics are delayed or running late – so that patients can be kept up to date
•
Nurses now offer refreshments and advise patients of on site facilities if they are waiting a long time for their appointment – and document that this has taken place.
•
Use of new inpatient documentation as prompt & written evidence for discharge planning. Ensure the discharge leaflet is given to patients/relatives/carers to keep them up-to-date and part of the patient’s discharge plan
Performance monitoring under the Local Authority Social Services and National
Health Service Complaints (England) Regulations 2009
94.8% of all complaints received were acknowledged within 3 working days. 97% of the complaints pertaining to Community Health Services/Peninsula Community Health received a final response within a timescale agreed with the complainant
100
85
70
2009-10
2010-11
2011-12
Q1 Q2 Q3 Q4
% Acknowledged within 3 working days
100
85
70
2009-10
2010-11
2011-12
Q1 Q2 Q3 Q4
% Final response within timescale agreed with complainant:
NHS Information Agency Grading:
> Level 1: 79% and above = well above average
> Level 2: 70 – 79% = above average
Referrals to the Health Service Ombudsman and to Professional Bodies
The Parliamentary and Health Service Ombudsman has responsibility for the second stage of the NHS Complaints Procedure. One referral was made during this period, relating to care received in a Minor Injury Unit. Following an initial screening review, the PHSO decided not to investigate this case.
Independent Complaints Advocacy Service (ICAS)
PCH Final 20 June 2012 Page 48 of 62
This statutory service is free, independent and confidential. The advocates assist people if they wish to complain about their NHS care, and support them through the process, as well as helping them consider the outcome they would like to achieve. 5 complaints were made through ICAS during this year.
3.16 Staff Survey 2010
Peninsula Community Health participates annually in the Staff Survey undertaken by
Quality Health. This is a voluntary survey but has a significant participation rate throughout the health sector.
The majority of questions asked are standard and cannot be changed although we do have a minimal influence in some areas.
The surveys are undertaken in October each year and the results published each New
Year.
Each year, results are published for the organisation and benchmarked against other community health providers.
Staff Survey 2010
The areas of action identified from the staff survey results of 2010 were:-
- Senior Management Communications and Engagement
- Health and Well Being
- Bullying and Harassment
Actions have been completed as per the action plan however, results from 2011 show that these actions have had a mixed impact.
A review of the plan has identified that the plan lacked smart goals and focus and therefore a more focussed approach has been adopted this year.
Staff Survey 2011
Overall, the Staff Survey results for 2011 are very positive. In comparison to 2010, the results have largely remained the same. As the survey was completed by staff during the time of transfer in October 2010, maintaining our current positive position is significant.
A presentation was received from Quality Health to the Board in March 2012 to provide further detail on the results. Several questions were asked at the time to the Quality Health representative and feedback has been received as below:-
1. You asked for some NHS wide statistics on the numbers of staff who say that they are thinking about leaving.
The figures for the different types of trusts are as follows:
PCH Final 20 June 2012 Page 49 of 62
Acute 31%
Ambulance 37%
MH Trusts 29%
Provider Organisations doing PCT questionnaire 28%
The lower figure relating to the question 15c 'As soon as I can find another job, I will leave this Trust.' is a far better indicator of serious intention to leave - your score is 16% on this
(those who answered agree and strongly agree). The national score is 15%.
2. You asked for a more detailed break down of the staff who were surveyed.
The sample was a random sample provided to us from yourselves according to our instructions so should be representative of all of your staff.
3. You asked for some more info on the people who didn't respond.
We know that in general we get less response from medical staff and manual staff. Our data manager is looking into this in more detail and I will pass on any further information to you as soon as possible.
4. You asked for a breakdown per hospital.
This is available on the Quality Health extranet where you can also do a break down by any of the variables including age, gender, ethnicity, site etc. Let me know if you need log in details for this.
5. You asked for more information on the violence against staff question
Yes, this is clearly very subjective. It will be very small numbers on bullying, harassment and violence it will be useful for you to look at the actual figures for this rather than a percentage. The percentages in terms of the violence question can be percentages of very small numbers. If you have got a number of people, say 10 people, we could look at the results and see if there is any pattern. We can let you know if this was the case. Again, this would have to be very carefully done because of confidentiality.
6. You asked about how service providers are being involved in the development of staff survey and any changes to the questionnaire next time?
There is a consultation process every year about staff survey and you will need to talk to the DH regarding this. DH with survey centre do all the developmental work on the questionnaire. There should be info on the DH website about this.
7. You asked about who else looks at the survey results. How are the results of it disseminated?
They are published on a national website which anybody can go onto. I'll send the link to the website on to you. They are analysed by the survey centre for the DH. QH do analysis on them as well and we disseminate that info to the trusts that we work with.
On the questions of the statistical significance of male response rate, feedback was not received from Quality Health. However, reference back to PCH equality statistics show that
PCH Final 20 June 2012 Page 50 of 62
the ratio of males to females employed is 1:9 Therefore, the low response rate from males is proportionate.
Staff Survey Action Plan
The Staff Survey results have also been shared with the Joint Partnership Committee and representatives from this committee have worked with HR colleagues to develop the action plan.
The key areas of action identified from the results are:-
- Communications and Engagement
- Bullying, harassment and abuse
- Health and Well Being
- Work Life Balance
Progress against the action plan will be provided to PCH Board on a quarterly basis.
PCH Final 20 June 2012 Page 51 of 62
Safeguarding
3.17 Key Quality Performance Indicators
Quality Scorecard March 2012
Category
Infection Control
Safety
Patient Experience
CQUINNs
Early Warning Trigger Tool
Incidents
Compliance with National
Requirements
Complaints
Indicator
Rates of Clostridium Difficile
MRSA Bacteraemia
Hand Hygiene Compliance
Inpatient Mortality
Nursing Metrics
Mixed Sex Accommodation
Patient Experience Metrics
Standard Required
11 for whole year
No specific CHS target but there is a Local Health Community
Target TBC of which we contribute.
95%
Unadjusted
Month on month improvement
100%
Month on month increase
To reduce avoidable death, disability and chronic ill health from Venous-thromboembolism (VTE) through
Q1 90% Q2 92% Q3 94% Q4 95% risk assessment
95%
10% improvement across 4 areas. Year end target: Nutrition
To implement the nursing metric system across community services to include patient survey
Increasing number of patients who have expected
Hydration 53% Pain management 30% Tissue Viability 78% Falls
84% deaths and are placed on the Liverpool Care Pathway Q1 40% Q2 50% Q3 65% Q4 80% in community Hospitals
90% patients over the age of 75 screened for frailty
Q3 60% Q4 90% and case managed.
Improve personalisation of care planning and selfmanagement
Q3 60% Q4 95%
100% of all in patients in community hospitals should
Q1 20% Q2 60% Q3 80% Q4 100% have CMEWS completed according to CHS policy
Patients with stroke are offered a minimum of 45 minutes of each active therapy that is required for a Q1 30% Q2 40% Q3 50% Q4 60% minimum of 5 days a week.
Full (Level 2) Medicines Reconciliation completed for
95% of inpatients within 72 hours or admission to the Community Hospital
Q3 75% Q4 95%
Monthly scoring of ward based risk factors Any ward scoring 13 or more may be at risk of cause for concern
New SUIs delared in month
Open SUIs in total
Open SUIs exceeding 45/60 day deadline
Number of total patient incidents
Number of inpatient falls
2
0
4
4
266
115
99%
1
0
3
3
233
32
Number of inpatient falls causing harm 43 7
Number of medication incidents
Number of new Never Events in the month
Cumulative number of Never Events
New Grade 3/4 pressure areas reported within the month
Number of CAS/NPSA alerts not actioned within timescale
Number of CAS/NPSA alerts not closed within deadline within the month
NICE - where PCH is non-compliant or compliance not known
Number of new complaints within the month
Number of Complaints which remain open after 25 days
Number of red or amber RAG rated complaints which remain open
New indicator January 2012
New indicator January 2012
New alerts made within the month
23
0
0
0
0
0
8
4
26
0
0
5
0
0
0
5
Oct-11 Nov-11 Dec-11
12
3 new
Total 15
3 new
Total 18
0 1 0
Jan-12
1 new
Total 19
0
98.44% 90%
12.38% 12.46% 9%
87.00% 88.00% 91%
100% 100% 100%
87% 86%
98%
90%
94%
88%
Feb-12
2 new
Total 21
0
92%
Mar-12
1 new
Total 22
0
Trend
93%
12.34% 11.11% 9.75%
93% 92%
100% 100%
89%
95%
100%
90%
↑
↑
↑
↔
↑
↓
97%
1
4
7
3
268
108
33
27
0
0
4
0
0
0
7
2
96%
0
7
12
1
227
128
32
15
0
0
7
0
0
0
4
14
7
96% 98%
87.71%
96%
95%
100%
60%
98%
1
2
0
13
14
0
0
0
0
0
1
12
0
250
0
5
0
250
87
9
Corrected
29
25
105
43
19
0
0
0 0
0
0
0
9
0
10
90% ↑
93%
↑
94% ↑
96% ↑
0
↑
↑
↑
↑
↑
↑
↑
↓
↔
↔
↔
↑
↔
↓
↔
↔
↑
↔
↔
↔
↓
↑
↑
↑
PCH Final 20 June 2012 Page 52 of 62
3.18 NHS Southwest Quality and Safety Improvement Programme
In line with the national QIPP Safe Care Work-stream known as “Safety Express”, NHS
South West has developed a programme called The Quality and Patient Safety
Programme.
In November Community Health Services (now Peninsula Community Health) joined the programme. The objectives of the programme continue to be:
•
Reduce Mortality by 15%
•
Reduce Adverse events by 30%
•
Develop and build a culture of patient safety and quality improvement
•
Build long term sustainability through increased capacity and capability for improvement at all levels
•
Build on existing work and integrate other national and local initiatives into a coherent whole
•
Achieve 95% reliability on all care processes identified in the programme
•
To share learning on a regional basis
Peninsula Community Health is committed to achieving the aims of this programme and reducing harm. The specific aims of the programme participant organisations are:
•
Pressure ulcers (III &1V) reduced 80% in hospital
•
Pressure ulcers (III &1V)reduced 30% in community
•
CAUTI (catheter acquired urinary tract infection) reduced by 50%
•
Serious injury from falls reduced by 50%
•
VTE events reduced
•
Reduction in unplanned transfers to secondary care
•
Standardised care of the deteriorating patient.
As you will see in the rest of the report, we have already seen improvements in reducing harm from falls, venous thromboembolus and standardising care for the deteriorating patient. We have also seen improvement in reducing urinary infections with those patients who have urinary catheters.
PCH Final 20 June 2012 Page 53 of 62
4.0 Response to this report from our stakeholders
A number of stakeholders have been consulted and previous feedback has been utilised to ensure that the report addresses areas and priorities of importance to them. The responses are in italics to show the text has been transcribed exactly as submitted to us by
our stakeholders. The responses are as follows:
4.1 Cornwall Overview and Scrutiny Committee
Cornwall Council’s Health and Adults Overview and Scrutiny Committee (HAOSC) agreed to comment on the Quality Account 2011-2012 of Peninsula Community Health (PCH). All references in this commentary relate to the period 1 April 2011 to the date of this statement.
The Committee has concerns about the provision of dentistry for those people unable to access universal services, and wishes to see an ongoing commitment to maintain and enhance service provision.
There is disappointment at the staffing issues which has led to temporary closures of a community hospital and at aspects of infection control. The HAOSC seeks reassurance that in future staffing levels will fulfil the needs of the community and that the will be a maintained spotlight on infection control in all Peninsula Community Health settings.
In relation to complaints, the Committee wishes to see the emphasis change to the satisfactory outcome of complaints rather than purely numbers of complaints received by
PCH and PALS.
The Committee is pleased that teleheath continues to be a priority and it is hoped that
Cornwall will continue to be a leader in this along with the positive work undertaken in respect of clinical care.
The HAOSC believes that the Quality Account is a good reflection of the services provided by the Trust, and provides a comprehensive coverage of the provider’s services.
Peninsula Community Health response: We thank the Cornwall Overview and
Scrutiny Committee for their comments regarding the Quality Account. Ensuring safe staffing levels within all our services is very important to us. We apologise that during 2011/12 we have, on occasion, closed or reduced the number of inpatient beds. Patient safety and high quality care is our number one objective and, to maintain this, sometimes we have had to reduce inpatient beds. We will continue to link closely with our stakeholders to ensure we get this right in the future.
4.2 Isles of Scilly Overview and Scrutiny Committee
The Council of the Isles of Scilly Health Overview and Scrutiny Committee wishes to endorse the Quality Accounts for 2011/12.
The islands value the services provided by the Community Hospital on St Mary’s and we would like to continue to develop its use in bringing health services closer to the patient.
We would like to focus efforts around the Health and Social Care Hub to ensure that
PCH Final 20 June 2012 Page 54 of 62
people with long term conditions have the support they need to continue to live independently.
Peninsula Community Health response: We thank the Isles of Scilly Overview and
Scrutiny Committee for their comments regarding the Quality Account. We fully support, and will continue to be a key member of the team, which are developing the
Health and Social Care Hub for the Isles of Scilly.
4.3 LINk4Scilly
Link4Scilly endorses this Quality Account.
The response to our own community survey shows that people value and appreciate the island based services provided by Peninsula Community Health – our Community Hospital, nurse led Minor Injuries Unit and Community Nursing Service are all considered to be good.
The work undertaken at the Hospital to accommodate an improved X-ray facility will enhance this service.
Feedback regarding services provided by visiting therapists, particularly physiotherapy and podiatry, indicates that need outweighs the level of provision, but this is a commissioning issue.
We have reported consistent feedback about the Dental service on the islands and look forward to seeing how the result of the Peninsula Community Health dental patient survey compares.
Through an oversight, LINks did not receive a list of priorities for 2012-13 earlier this year, but we welcome the inclusion of improvement around hospital discharge and the focus on patient experience.
The Quality Account details Peninsula Community Health’s own patient surveys and PALs contacts and complaints, and next year it would be good to see an acknowledgment of
LINk feedback, and how it is taken into account. Our experience is that Peninsula
Community Health, and in particular the Team Leader at St Marys Hospital, are responsive to community views and concerns. This could be better communicated.
The establishment of Peninsula Community Health and the transfer of services in 2011 appears to have been well managed. We at LINk felt that we were kept informed and there was some good community engagement early in the process.
Peninsula Community Health response: We thank LINk4Scilly for their comments regarding the Quality Account. Unfortunately LINk4Scilly did not receive the draft priorities, which were sent by post. Even so, we did resend them and gave
LINk4Scilly opportunity to comment, and we are very grateful for their response. We will ensure that in future Quality Accounts, LINk feedback and the improvements it brings, are discussed.
4.4 Cornwall LINk
Do the priorities of the provider reflect the priorities of the local population?
Unfortunately LINk was not able to have any input into setting the priorities for inclusion in this account, but LINk is pleased to see that it’s feedback was acknowledged in the list of suggested topics that were circulated for prioritisation by stakeholders in February 2012.
PCH Final 20 June 2012 Page 55 of 62
On review of the top five priorities for improvement, LINk welcomes PCH’s focus on ensuring that patients are kept fully informed of their discharge plan. Likewise the improved dental pathways for people with learning disabilities are encouraged.
With regard to the care and dignity of patients with dementia as a priority, the aims for improvement are encouraging and LINk is hopeful that these will make a difference to the support given to people with dementia and their families who are outside of a care setting.
It is disappointing for LINk that one of the suggested topics for improvement circulated in
February 2012, which was not chosen for inclusion in the top five priorities, is staff attitudes. This is disappointing considering the work that LINk has been doing over the year to address staff attitudes in health and care settings when dealing with socially excluded groups.
LINk is pleased to see that the Hospital Discharge Leaflet and patient’s bedside folder will be utilised to give the patient as much information as possible about their discharge.
Discharge from hospital remains an ongoing issue which is fed into LINk. Peninsula
Community Health’s quality account reinforces this by identifying that action plans are needed to address patients who feel that they have not been talked to about their discharge from hospital. LINk would welcome PCH sharing these action plans to understand how this process will be improved, as well as understanding what actions will be taken, how this will be measured and how it will be fed back.
LINk is pleased to see a clear explanation of how the Equality Delivery System will be implemented by PCH, in particular the four objectives which have been outlined for the forthcoming year. In terms of the objective around a “learning and development package which supports staff to better understand the links between equality, human rights…. enabling patient choice and enhancing patient experience”, LINk welcomes this. The need for more training for healthcare staff, focussing on the differing needs that minority groups in Cornwall have when accessing healthcare has been a focus of LINk’s work, and LINk is pleased that PCH have acknowledged this.
LINk is pleased to see that the collaborative piece of work around Physiotherapy
Outpatients, specifically physiotherapy for people with long term conditions is acknowledged. LINk found the joint working to be successful and look forward to seeing the results.
It is disappointing to see that the PEATS inspections indicate that Falmouth and Poltair hospitals are performing worse than other hospitals for privacy and dignity. It would be encouraging to know that this is being addressed by PCH in some way and that developments are planned to improve the performance. It would be helpful know specifically what issues were raised under privacy and dignity as this is not documented.
The importance of patient feedback is clearly acknowledged in the PCH Quality Account and there is a firm commitment to improving the patient experience. There is a dedication to utilising this feedback to make positive changes, and LINk welcomes this approach. It would be reassuring for LINk to understand how patient experience is influencing PCH’s priorities for improvement. The draft of the report did not include the findings from the patient experience metrics (page 40) so it is hard to gauge how the priorities reflect PCH’s own patient feedback.
PCH Final 20 June 2012 Page 56 of 62
Is the Quality Account clearly presented for patients and the public?
In the draft document that LINk in Cornwall received, there are some acronyms in the document which are not explained. There is a disparity in some sections which clearly explain issues for example the Equality Delivery System, and other sections that do not explain issues fully.
In some places it is difficult to understand the measures around performance as no specifics are given around how things are going to be achieved, for example under the review of quality and safety 2011/12. Some sections are missing information, e.g. page 46 refers to a list of actions following complaints and no such actions are shown.
LINk in Cornwall is unable to comment on the staff survey as this section was not included in the draft version received.
Peninsula Community Health response: We thank Cornwall LINk for their comments regarding the Quality Account. Unfortunately Cornwall LINk did not receive the draft priorities, which were sent by post. Even so, we did resend them and gave Cornwall
LINk opportunity to comment, and we are very grateful for their responses. Although staff communication was not identified in the priorities for 2012/13, we are committed to improving staff communication and attitude and although not identified as a specific priority we feel this is embedded in all our priorities. In everything we do, maintaining patient privacy and dignity and ensuring they are involved in their care is of great importance. In regard to last year’s PEATs results – both Poltair and
Falmouth Hospitals have undergone estates works to improve the environment, and this has been well received by patients and staff.
4.5 NHS Cornwall & Isles of Scilly/Kernow Clinical Commissioning
Group
NHS Cornwall and Isles of Scilly (NHSCIOS)/Kernow Clinical Commissioning Group is pleased to have the opportunity to comment on the Quality Account 2011/12 for Peninsula
Community health (PCH) and welcomes the approach the organisation has shown in developing and setting out its plans for quality improvement. There are routine processes in place with PCH to agree, monitor and review the quality of services throughout the year covering the key quality domains of safety, effectiveness and experience of care.
The Quality Account presents a overview of a wide range of quality improvement work being undertaken. We note the continued progress that has been made in: reducing avoidable harm through Venous Thromboembolism risk assessment, understanding why pressure ulcers occur, medicines management and falls within the community hospitals. In addition the growth of the telehealth service for patients with long term conditions.
We have reviewed and can confirm the information presented in the Quality Account appears to be accurate and fairly interpreted, from the data collected. However in order to give a balanced view we would wish to see information relating to learning from Serious
Incidents. In terms of the performance against the 2011/12 CQUIN goals PCH achieved all the quality stretch targets.
PCH Final 20 June 2012 Page 57 of 62
The report presents work undertaken to measure, monitor and improve the patient experience through patient experience metrics, however it would be helpful for the
Organisation to further develop staff engagement.
The Clinical Commissioning group looks forward to working with the Organisation throughout the year to achieve more efficient integrated pathways delivering high quality services to patients, especially with community nursing teams.
We are pleased to see that the priorities chosen for 2012/13 have been identified with key stakeholder involvement. In addition to those highlighted in the Account we would wish the
Organisation to also focus on the following that have not been selected as a priority:
•
•
•
•
Patient flow through community hospitals, particularly delayed discharges
Timeliness and learning from Serious Incidents
Development of early intervention teams with health and social care across 7 days
Community acquired infections
Peninsula Community Health response: We thank NHS Cornwall & Isles of
Scilly/Kernow Clinical Commissioning Group for their comments regarding the
Quality Account. In regard to the four areas highlighted in the response – although they have not been identified as priorities within the Quality Account, there are existing workstreams to improve all of these areas. Also, all of these areas form part of our quality monitoring monthly, which is reported to the Commissioners.
5.0 Conclusion
It is hoped that you have found our Quality Account an interesting and helpful document, and that it has re-assured you that Peninsula Community Health is committed to improving the quality and safety of services it delivers as well as engaging with and involving its local community and service users.
If you have any comments, or questions about any of the information it contains or any of
CHS services please do not hesitate to contact our Patient Advice and Liaison Team
(PALS) on 01326 435885.
PCH Final 20 June 2012 Page 58 of 62
6.0 Glossary
Acute Trust
Audit Commission
A trust is an NHS organisation responsible for providing a group of healthcare services.
An acute trust provides emergency and planned hospital services.
The Audit Commission regulates the proper control of public finances by local authorities and the NHS in England and Wales. The
Commission audits NHS trusts, primary care trusts and strategic health authorities to review the quality of their financial systems.
It publishes independent reports highlighting risks and good practice, to improve the quality of financial management in the health service. In addition, the Commission works with the Care Quality Commission to conduct national value-for-money studies.
Visit: www.audit-commission.gov.uk
Board of Peninsula Community Health CIC The Board is accountable for setting the
Care Quality Commission
Clinical Audit
Commissioners of services strategic direction of the organisation, monitoring performance against objectives, ensuring high standards of corporate governance and helping to promote links between the organisation and the community. The Board has 10 members and includes the Chairman, Chief Executive, four Executive Directors and four Non-
Executive Directors
The Care Quality Commission (CQC) is the independent regulator of health and social care in England. It replaced the Healthcare
Commission, Mental Health Act Commission and the Commission for Social Care
Inspection in April 2009. The CQC regulates health and adult social care services provided by the NHS, local authorities, independent healthcare providers and voluntary organisations. Visit: www.cqc.org.uk
Clinical audit measures the quality of care and services against agreed standards and suggests or makes improvements where necessary
These are organisations that buy services on behalf of people living in a defined geographical area. They may purchase services for the population as a whole, or for individuals who need specific care, treatment and support. Healthcare services are commissioned by primary care trusts.
PCH Final 20 June 2012 Page 59 of 62
Commissioning for Quality and Innovation
(CQUIN)
Complaint
Department of Health
Dignity
Discharge
Hospital Episode Statistics (HES)
Information Governance
Local Involvement Networks (LINks)
Social services are commissioned by local authorities
A report into the future of the NHS, entitles
‘High Quality Care for All’ 2008, included a commitment to make a proportion of providers’ income conditional on quality and innovation. This is achieved through the
Commissioning for Quality and Innovation
(CQUIN) payment framework. Visit www.dh.gov.uk
This is an expression of dissatisfaction that can relate to any aspect of a person’s care, treatment or support. It can be expressed orally, through gestures or in writing.
The Department of health is the department of the UK government responsible for policies on health, social care and the NHS
(England only).
Dignity is concerned with how people feel, think and behave in relation to the worth and value that they place on themselves and others. To treat someone with dignity is to respect them as a valued person, taking into account their individual views and beliefs.
The point at which a patient leaves hospital to return home; or is transferred to another service: or the provision of a service is formally concluded.
This is a data warehouse containing a vast amount of information on the NHS, including details on all admissions to NHS provider hospitals and outpatient appointments in
England. HES is an authoritative sourced used for healthcare analysis by the NHS, government and many other organisations.
Information Governance is concerned with the structures, policies and practices in place to ensure the confidentiality and security of health and social care service records.
LINks are comprised of individuals and community groups such as faith groups and residents associations, working together to improve local services. Their job is to find out what the public like and dislike about local health and social care, and then feed the views back to the people who plan and run these servies. They may talk directly to healthcare professionals about a service that is not being offered or make
PCH Final 20 June 2012 Page 60 of 62
National Confidential Enquiry into patient
Outcome and Death - NCEPOD recommendations about an existing facility
NCEPOD is an independent body concerned with maintaining and improving standards. Of medical and surgical care. It does this by reviewing the management of patients and undertaking confidential surveys and research, which are then
National Institute for Health and Clinical
Excellence - NICE published for the public’s benefit.
NICE is an independent organisation responsible for providing national guidance on promoting good health and preventing and treating ill health
This is the national unique patient identifier NHS Number that makes it possible to share patient information across the whole of the NHS, safely, efficiently and accurately.
Overview and Scrutiny Committees (OSC) Since January 2003, all local authorities with responsibilities for social care have had the power to review and report on local health services. Overview and Scrutiny
Committees have taken on this role, and have been instrumental in helping to plan services and bring about change. They bring democratic accountability into healthcare decision-making and make the
NHS more responsive to local communities.
This is a person who receives health or Patient social care through a regulated activity.
Patients are defined ‘service users’ in the
Health and Social Care Act 2008.
Patient Environment Action Teams - PEATs PEAT is an annual inspection of inpatient facilities at healthcare sites across England with more than 10 beds. PEAT is selfassessed and inspects standards including food, cleanliness, infection control and patient environment. The scheme was established in 2000. It acts as a bench-
Primary Care Trust - PCT marking tool to ensure that improvements are made in the non-clinical aspects pf a patient’s experience.
PCTs are part of the NHS in England and responsible for improving the health of local people. They provide a range of community health services: funding for general practitioners and medical prescriptions: and commission hospital and mental health services from appropriate providers. By
April 2012, PCTs will be abolished and they will be replaced by a consortia of GPs, who will manage the budgets.
PCH Final 20 June 2012 Page 61 of 62
Privacy and dignity
Providers
VTE – Venous- Thromboembolism
To respect someone’s privacy involves recognising when they would like to be alone (or with family or friends), and showing sensitivity to their wishes for a private conversation and preventing others from looking or listening in. To treat someone with dignity is to respect them as a valued person, taking into account their individual views and beliefs.
Providers are the organisations that provide
NHS services, for example NHS trusts, community interest companies, voluntary sector organisations.
A venous thrombosis is a blood clot
(thrombus) that forms within a vein.
Thrombosis is a medical term for a blood clot occurring inside a blood vessel. A classical venous thrombosis is deep vein thrombosis (DVT), which can break off
(embolize), and become a life-threatening pulmonary embolism (PE). The conditions of
DVT and PE are referred to collectively with the term venous thromboembolism
PCH Final 20 June 2012 Page 62 of 62