Quality Account 2011/12 Looking after you locally
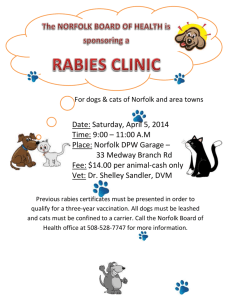
advertisement

Quality Account 2011/12 Looking after you locally 2 Norfolk Community Health and Care NHS Trust Our Health Visitors see more than 1,000 new families every month We deliver health services to over 400 schools and colleges Our Community Nursing teams have around 108,000 face-to-face contacts with patients every month We have 3,000 We have around 300 members of dedicated NHS staff across the county patient beds in Norfolk NCH&C receives Our School Nurses hold 16,500 1,300 referrals from GPs and other healthcare professionals every month More than 3,000 patients per year are admitted to our community hospitals face-to-face appointments with children each year We deliver more than 70 different services in and around Norfolk Quality Account Norfolk Community Health and Care NHS Trust 3 Contents Part 1 Part 3 1.1 Statement on quality 4 1.2 Our vision for the future 6 Part 2 2.1 Priorities for quality improvement (2012/2013) Review of quality performance in 2011/12 24 3.1.1 Overview 24 3.1.2 Summary of positive achievements in the last year 24 7 3.1.3 Staff achievements 25 3.1.4 Commissioning for Quality and Innovation 27 3.1.5 Performance highlights 28 3.1.6 Clinical quality and Quality Goals 31 3.1.7 Patient experience 37 3.1.8 Learning from incidents and complaints 44 Safeguarding adults and children 49 2.1.1 Annual priorities and Quality Goals for 2012/2013 7 2.1.2 Patient experience in 2012/13 8 2.1.3 Commissioning for Quality, Innovation, Productivity, Prevention (QIPP) 9 2.1.4 3.1 Our staff - workforce planning and development 11 3.1.9 2.1.5 Performance monitoring for 2012/13 12 3.1.10 Effectiveness of care 2.2 Statements of assurance from the Board 14 3.2 2.2.1 Review of services 14 2.2.2 Participation in clinical audits 15 2.2.3 Participation in clinical research 18 2.2.4 Goals agreed with commissioners 19 2.2.5 Statement from the Care Quality Commission 19 2.2.6 Data quality 21 2.2.7 Information Governance Toolkit attainment levels 23 Clinical coding error rate 23 2.2.8 3.2.1 51 Explanation of who has been involved and engaged with 56 Third Party Statements 56 The content of this Quality Account has been endorsed by the Trust Board and has taken into account feedback from our lead commissioners, and our local population via the representative organisations, LINks and the Health Overview and Scrutiny Committee. We trust that you will find our Quality Account informative and helpful in reviewing our progress against our key priorities for the forthcoming year. If you would like this publication in large print, Braille, alternative format or in a different language, please contact us on 01603 697300 and we will do our best to help. design: woolfdesigns.co.uk 4 Quality Account Norfolk Community Health and Care NHS Trust 1.1 Statement on quality Welcome to Norfolk Community Health & Care NHS Trust’s (NCH&C) Quality Account for 2011/12. We hope that you enjoy reading about our activities and achievements over the previous year and that you gain some valuable insight into our plans and priorities for the next year. NCH&C is an independent health and care organisation which is part of the National Health Service (NHS), employs NHS staff and provides NHS health and care to local people. We serve a population of around 870,000 people in and around Norfolk, making us one of the largest providers of NHS community health and care services in the country. Our aim is to constantly improve our patients’ lives by providing you with the best care, close to where you live. We currently employ over 2,300 whole time equivalent substantive members of staff. 80% of these are clinicians; healthcare professionals such as doctors, dentists, nurses, health visitors and physiotherapists. The remainder are the people who help to keep our services running, or who support our patients and clients during their stay with us or in planning their appointments. Specialised care for all Our specialist teams all across Norfolk provide personalised health and care services for everyone, from babies to the elderly. Our health visitors provide services covering pregnancy and the first 5 years of life, while children are cared for in schools by our school nurses. We help to keep people healthy with our Smokefree Norfolk service, and work with patients to regain their independence and quality of life after a brain injury, stroke or fall. We also provide end-of-life care services within people’s homes or specialist inpatient units, to allow people to pass away comfortably and with dignity. We care for the most disadvantaged and vulnerable in our communities who can find it very difficult or daunting to access the right healthcare, for example sex workers and homeless people, and we support people of all ages with Learning Disabilities, empowering them to live healthy and independent lives. Range of services The trust delivers a diverse range of 34 clinical services that are organised into 3 main business units; children’s services, specialist services and a locality unit (comprising north, south, west and central localities) through which the bulk of NCH&C’s services are provided. This new structure is a result of a reorganisation that took place in January 2012 to ensure that our services operate from the same area as the new GP Clinical Commissioning Group boundaries across Norfolk to better serve the population. Frail Older People Many of the Trust’s targets for 2011/12 were specifically aimed at the care of patients within this group and included clinical improvements in patient safety in a number of areas. These include; catheter acquired urinary tract infections, reduction of avoidable pressure ulcers, end of life care, personal health planning, nutritional care, and admissions avoidance for patients over 65 years old on a case manager/community matrons case load. Telehealth and telecare are active components of managing case load numbers and helping the elderly with long term conditions manage their health. In 2011/12 a significant programme of work has been delivered in the community specifically around the use of telehealth home pods by community teams and currently 170 telehealth units are deployed with NCH&C patients. This technology has been well received by patients and many of our clinicians, ensuring patients can be supported at home in managing their long term condition. The Trust has Part 1 1.1 Statement on quality worked collaboratively with the Norfolk and Norwich University Hospital Foundation Trust to deliver this programme. We recognise that there is still more work to do to improve our IT communication systems to support the practical application of telehealth care. We will continue to engage clinicians in the development and implementation of telehealth care to ensure that the benefits of this new technology bring to patients are fully realised. During 2012/13 we will continue to build on existing achievements and learning from our experiences in 2011/12. Telecare is also integral to the falls and dementia pathways. NCH&C has recently recruited four ‘Falls Champions’ to support the work of preventing injurious falls. They have received training for Telecare from Norfolk County Council and are also receiving dementia awareness training from Norfolk and Suffolk NHS Foundation Trust. In turn, the champions are in the process of delivering training to the community integrated teams to widen awareness of dementia care and falls prevention across the Trust. Dementia care As part of a Norfolk-wide initiative NCH&C approached a wide range of key stakeholders and partners over the past year to help inform the design of the first stage of an integrated community dementia pathway across Norfolk. Partners in this process have included commissioners, social services, Norfolk and Suffolk NHS Foundation Trust, 3rd sector (Age UK, Alzheimer’s Society), Healthwatch and acute provider organisations. The fundamental aim of this pathway design has been to deliver against the Department of Health’s nine outcomes for dementia which captured what people with dementia say about their expectations of health and social care systems. The integrated community dementia pathway steering group have designed a pathway which following a successful pilot, is now being implemented across all the localities within Norfolk. Critical to this success has been the joint care approach between both NCH&C integrated community teams and community mental health teams. This ensures that the patient and carer have an appropriate Care Co-ordinator or Case Manager. 5 To ensure that the increase in prevalence of dementia is recognised and that patients are treated with respect and dignity by skilled staff, NCH&C is in the process of implementing an extensive training programme. The Trust is also a partner of a Health Innovation and Education Cluster (HIEC) with private and public sector partners whose focus is dementia. Our palliative care co-ordinators have trained over 500 staff on dementia and end of life care whilst working in partnership with Age UK and the Alzheimer’s Society. This work has been shared at national end of life conferences. Admission avoidance NCH&C plays a significant role in the local health economy. Our Trust has helped local people to avoid over 1,000 acute hospital admissions in less than five months for those patients over 65 years old who are on a Case Manager’s or Community Matron’s caseload. This equates to one avoided emergency admission per GP practice, per week. Our Trust will continue to offer excellent service to people right across Norfolk, but we will also enable more people from outside of Norfolk to benefit from our expert community health and care. We will work to bring expertise and good ideas from across the UK to Norfolk, allowing our patients to benefit from best practice from across the NHS. 6 Quality Account Norfolk Community Health and Care NHS Trust 1.2 Our vision for the future More and more people in Norfolk and surrounding areas are living with long term conditions, such as diabetes and heart disease. Our population of frail and elderly people is also growing. As the population ages, and more people are affected by illnesses caused by lifestyle choices, such as smoking, the types of services needed by our community is changing. We will aim to develop new services, often in partnership with others, to meet these changing needs, from tackling childhood obesity to improving care for older people with dementia. We want to help keep our patients well – providing care as early as possible, to help them avoid having to stay in an acute hospital, or supporting them to return home as quickly and safely as possible after a hospital stay. This Quality Account has been developed in conjunction with our annual planning processes which has produced the Annual Plan for 2012/13 and is part of the Trust’s Annual Report. The content of this Quality Account has been endorsed by the Trust Board and has taken into account feedback, where provided from our lead commissioners, our local population via Norfolk LINks and Norfolk County Council’s Health Overview and Scrutiny Committee. I hope you will find our Quality Account informative and helpful in reviewing our progress against our key priorities for the forthcoming year. The information supporting the content of this Quality Account is, to my knowledge, accurate and published by the Board on 27th June 2012. As a provider of community based health and care, we can act as the ‘glue’ between different services provided by the NHS, social care and others, so our patients can benefit from joined up care. Michael Scott Chief Executive Part 2 2.1 Priorities for quality improvement (2012/13) 2.1.1 Annual priorities and Quality Goals for 2012/13 7 2.1 Priorities for quality improvement (2012/13) The Trust’s vision is to “Look after you locally”. We will improve the quality of people’s lives, in their homes and community, through providing the best in ‘joined up’ care. The starting point for the Trust is the patient which means that quality is at the heart of everything NCH&C does. Our vision is supported by the way the Trust structures its services and wherever possible, our services are delivered in an integrated way with social care. The Trust was a successful pilot of Integrated Care Organisations (ICOs) with GPs and social care and we will continue to build on this foundation and increase its scale. The Trust’s vision will also be delivered through the achievement of a number of corporate objectives and its commercial strategy. The Trust’s longer term corporate objectives are: • Improving quality for patients and the public and offering the best patient experience in the East of England • Transforming services – being the commissioners’ first choice provider and being the positive alternative to acute hospital care • Building the organisation – The Trust wants to be the first choice employer for staff and be a clinically led, high performing organisation • Building sustainability – to deliver a long term financial model that demonstrates value for money, delivers innovative services and meets the requirements of the Trust’s regulators • Building reputation – to be the first choice for patients, Clinical Commissioning Groups and play a leading role within the local health economy 2.1.1 Annual priorities and Quality Goals for 2012/13 The Trust Board identified seven priorities for 2012/13 that bring together our strategies and service developments which go towards achieving the Trust’s objectives. These annual priorities are; 1. To improve the quality of the Trust’s services for patients 2. To deliver excellent services and delight our customers 3. To truly inspire our staff 4. To embed the locality based service model 5. To achieve the Trust’s Financial Targets 6. To grow the Trust’s services and focus on the right services 7. To achieve Foundation Trust status Each of these priorities is supported by a number of objectives and more detailed milestones. Both the priorities and milestones were developed after involving clinicians and managers outside of the Board. 8 Quality Account Norfolk Community Health and Care NHS Trust The Quality Goals for NCH&C for 2012/13 2.1.2 Patient experience in 2012/13 The Trust is utilising the Safety Thermometer, a national data collection programme to measure four potential ‘harms’; venous thromboembolism (VTE), pressure ulcers, catheter acquired infections and falls. The first submission was made in March 2012. The data gives a snapshot in time and cannot show trends at this stage, but it is recognised that its value will increase in future and the Trust will participate in the programme fully this year. Our vision for Patient Experience and Involvement is that NCH&C is a patient focused organisation actively seeking the views of our patients and carers and engaging them in shaping and developing our services whilst consistently providing high level, quality care. We want our patients to have the very best experience of community services in the East of England. The Quality Goals for 2012/13 are: 1. Implement safety thermometer targets in four key areas: • Achieve 95% Venous Thrombo-embolism assessments for inpatients by December 2012 • 50% reduction in Catheter acquired urinary tract infections by December 2012 • Reduction in the levels of injurious falls in our inpatient units to four per 1,000 OBDs • Eradication of avoidable pressure ulcers (as below) 2. Deliver zero avoidable Pressure Ulcer target by December 2012 (Grades 2–4) 3. Improve patient satisfaction to 70% very satisfied and no area < 50% 4. Implement the net promoter score system and meet target set for inpatients 5. To achieve ‘you’re welcome’ accreditation in school nursing service 6. To achieve UNICEF ‘baby friendly’ accreditation at level 2 We genuinely want to work with our patients and local community so that together we make a difference to the experiences of our current and future patients and design and provide our services around their needs. In 2012/13 the Trust aims to build on an excellent year of patient experience in 2011/12 (see section 3.1.7) by implementing the following projects: • Demonstrate improvements in patient experience using the “Net Promoter Score” • Review results from the Community Services Survey and implement actions as required • Continue to embed patient stories within NCH&C ensuring the methodology is utilised where there is a targeted need for in depth information, deliver more training and consider involving Healthwatch members as interviewers alongside NCH&C staff • Work in partnership with services to support locally managed surveys and other methodologies for capturing patient/carer experiences • Work in partnership with NCH&C members and external voluntary organisations ensuring effective patient engagement/involvement • Work in partnership with NCH&C Learning Education and Development Team ensuring staff have the core skills, beliefs and values necessary for a good patient or carer experience • Work with Kings College, London to participate in a research project to seek views of parents into the health visiting service Part 2 2.1 Priorities for quality improvement (2012/13) 2.1.3 Commissioning for Quality and Innovation Scheme for 2012/13 Advocacy - Net Promoter NCH&C has made good progress in the use of the net promoter methodology in 2011/12 and will continue to develop this tool as a key indicator of patient satisfaction and service quality. This is a standardised approach with a single metric to obtain real-time monitoring of patient experience. The ‘net promoter’ score captures perceptions of the local population about the health care they have received. The score is the difference between the proportion of people surveyed who said they would recommend the local service and the proportion who said they would not. Net promoter methodology remains in its infancy within the Trust and it will be further developed within the next year. All NCH&C inpatient units will participate in the survey from April 2012 to March 2013. A minimum of 10% of the weekly footfall of patients will be asked the question on the day of discharge or up to 48 hours post discharge. They will also have the opportunity to leave any comments. A baseline net promoter score will be established during month 1 and a 10 point improvement score agreed over the next year. Alongside this survey, a methodology will be developed for use within community based services and implemented later in the year. 9 2.1.3 Commissioning for Quality and Innovation (CQuIN) Scheme for 2012/13 The CQuIN scheme requires Primary Care Trusts (PCTs) to commission for quality and innovation through discussing, agreeing and monitoring quality indicators with providers. A CQUIN scheme is the locally agreed package of quality improvement goals and indicators, which in total, if achieved, enables the provider to earn its full CQUIN payment. A CQUIN scheme should address the three domains of quality: safety, effectiveness and patient experience; and reflect innovation. Indicators should be realistic so that a provider is able to have a reasonable expectation that they can achieve the requirements. Achieving the indicator set will enable providers to receive a quality based payment. The monies to meet the cost of this payment will come from incentivising a proportion of annual uplift of contract values of 2.5% for 2012/13 divided into three elements; • 0.5% for four national indicators • 1.0% for locally agreed indicators • 1.0% for a system wide indicator based on reducing emergency admissions into the acute hospitals These indicators will be set within the contract as part of the established quality schedule and monitored by the PCT through clinical review. 10 Quality Account Norfolk Community Health and Care NHS Trust NCH&C and NHS Norfolk & Waveney have agreed a set of quality measures to be assessed as part of the CQUIN initiative which focus on the following areas for 2012/13: Goal Description of Goal No Quality Domains Indicator Name National/Local/System-wide 1 To reduce avoidable death, disability and chronic ill health from Venous-thromboembolism (VTE) Safety VTE risk assessment and prophylaxis National 2 To improve responsiveness to personal needs of patients/carers Patient experience VOICES survey Local 3 Improve collection of data in relation to pressure ulcers, falls, urinary tract infection in those with a catheter, VTE Safety NHS Safety Thermometer National 4 Development of the Care pathway for patients risk assessed as having dementia by the acute providers in collaboration with other providers Patient safety Effectiveness Experience Dementia Pathway National 5 Patient satisfaction: “How likely is it that you would recommend this service to friends and family? Patient experience Net promoter National 6 Partnership Working Safety Assurance process System wide 7 Provision of a dedicated community nurse for each GP practice to support admission avoidance Patient experience Effectiveness Dedicated community nurse for GP practices Local 8 Pharmaceutical care plans for “at risk” patients Safety Medicines Management Local 9 End of Life care - For NCH&C care home facilitators to roll out training for ACP/Preferred place of care (PPoc) and ensure that PPoC is utilised where clinically appropriate. 20 Care homes will be targeted and supported. Patient experience End of Life care Local 10 Improve the care of paediatric patients in the community through the introduction of an Intravenous therapy (IV) service Patient experience Effectiveness Paediatric care Local 11 Achieve improved outcomes for patients of the community nursing and therapy service in 5 key areas Effectiveness Community nursing and therapy outcome indicators Local 12 Avoid acute hospital admissions through effective case management of those at greater risk of admission Effectiveness Case Management of high risk patients Local Part 2 2.1 Priorities for quality improvement (2012/13) 2.1.4 Our staff - workforce planning and development 11 2.1.4 Our staff - workforce planning and development The NCH&C Trust Board has approved a Workforce Strategy that provides a long term strategic framework under which exists a number of more detailed workforce plans and strategies such as Organisational Development, Talent and Leadership and Health and Wellbeing. The Workforce Strategy contributes to our overall strategy and is integrated with other supporting strategies such as our Clinical Strategy, Estates Strategy and Information Management and Technology (IM&T) strategy. The Workforce Strategy is to ensure that we have a workforce that is affordable, the right shape and has the capacity and capability to deliver excellent health care for the people we serve. It outlines the range of interventions that will provide the workforce with the skills, knowledge and development to sustain the organisation, ensure they are committed and aligned to our strategic objectives and enable them to have fulfilling careers. Staff engagement is at the centre of achieving our aspiration to deliver high quality patient care. Our response to the staff survey results is to prioritise staff engagement. The workforce strategy contains a number of strategic objectives: Develop clinically led workforce planning The Trust aims to establish clinically led workforce planning with full integration between corporate and operational services. Recently more integrated workforce planning has taken place for example with project teams set up to support tenders. This model was particularly successful in our winning Sure Start bid. We will encourage and build on this model in all our workforce planning activities. Provide quality education and development opportunities for all our staff The strategy describes how the Trust will provide high quality education, training and development for the workforce, ensuring that skills are developed to support the provision of high quality, patient focused care. The Trust’s approach to training includes a focus on care, compassion and personalised care and technical skills as well as leadership and management. To truly inspire our staff The Trust’s Organisational Development (OD) Strategy will ensure the processes, structures, systems and culture necessary to achieve our vision is achieved. Central to this strategy is staff engagement. The Trust has well developed and shared organisational values including a supporting behaviour framework. Promote staff health and well being The Trust’s Health and Well Being Strategy supports the Workforce Strategy and acknowledges that the work, health and well being of our employees are interlinked. The Trust will ensure that managers have the key skills, knowledge and ability to support employees at work, to manage absence and also work with staff to ensure issues which may impact negatively on staff health are identified and minimised. Quality Account Norfolk Community Health and Care NHS Trust Where possible, and where common data is available, we will be looking to benchmark against other community trusts. The functionality of the Trust’s ICARUS reporting system will continue to be developed during 2012/13. Incorporating data from other departments, such as Human Resources and from other systems (such as DATIX) will be actively explored to enhance the scope of reporting performance information. 2.1.5.1 Planned changes to performance reporting for 2012/13 Quality Accounts The National Quality Board has recently considered how to foster readers’ understanding of comparative performance whilst maintaining local ownership. They have subsequently recommended the introduction of mandatory reporting against a small set of quality indicators for inclusion in Quality Accounts that are due to be published in June 2013. The intention is that trusts will be required to report: • Their performance against these indicators As shown below, as at March 2012 the Trust has achieved 90.4% against the national target of 90% VTE assessments. For 2012/13 the target will be 95% by December 2012. The Trust’s aim is to maintain its excellent performance and ensure that any under performance is escalated quickly and effectively to the Trust’s Medical Director. The increase to 95% will be supported by location specific plans led by the Modern Matron in charge of the inpatient units. Percentage of VTE assessments completed on admission to NCH&C inpatient units 100% 95% 90% 85% 80% 75% 70% 65% 60% 55% 50% pr -1 1 ay -1 Ju 1 n1 Ju 1 l-1 A 1 ug -1 Se 1 p1 O 1 ct -1 N 1 ov -1 D 1 ec -1 Ja 1 n1 Fe 2 b12 M ar -1 2 NCH&C will be ensuring that our reporting systems will report at locality level and align with our Clinical Commissioning Groups (CCGs). Percentage of admitted patients risk-assessment for Venous Thromboembolism (VTE) M 2.1.5 Performance monitoring for 2012/13 A 12 Actual cumulative Local standard in month: 90% Actual: Reporting against the indicators is not mandatory for 2011/12, however, NCH&C have reviewed the indicators and have provided a summary against those that are relevant to our organisation and for which we have current data under ‘Domain 5: Treating and caring for people in a safe environment and protecting them from avoidable harm’. 83.6% total year to date 90.4% March 2012 • The national average • A supporting commentary, which may explain variation from the national average and any steps taken or planned to improve quality Service spec trajectory Local performance: Achieving Part 2 2.1 Priorities for quality improvement (2012/13) 2.1.5 Performance monitoring Rate of patient safety incidents and percentage resulting in severe harm or death Reduction in harm incidents The table below shows incident data collected via DATIXweb from April 2011 to March 2012 and a reduction in the number of severe harm incidents is noted. These figures demonstrate that only 2.14% of incidents over the period April 2011 to March 2012 resulted in severe harm or unexpected death. 13 The National Patient Safety Agency (NPSA) report from 1 April to 30 September 2011 states that NCH&C’s reporting rate = 102.3 incidents reported per 1,000 bed days (compared with other community trusts) places the organisation in the highest 25% of reporters compared with 19 primary care organisations with inpatient provision in the East of England. The NPSA states: “Organisations that report more incidents usually have a better and more effective safety culture. You can’t learn and improve if you don’t know what the problems are.” Month April May June July Aug Sept Oct Nov Dec Jan Feb Mar Total No Harm 157 147 191 208 184 181 180 200 193 208 264 215 2328 Low 97 125 150 183 193 171 204 236 231 248 254 282 2374 Moderate 21 35 32 38 35 27 32 37 27 34 40 33 381 Severe 4 6 7 10 14 10 11 10 5 8 4 5 94 Unexpected death 1 0 0 3 3 2 0 2 1 1 4 0 17 Total 280 313 380 432 429 391 427 485 457 499 566 535 5194 14 Quality Account Norfolk Community Health and Care NHS Trust 2.2 Statements of assurance from the Board 2.2.1 Review of services During the period April 2011 to March 2012 Norfolk Community Health & Care NHS Trust (NCH&C) provided and/or sub-contracted 34 NHS services. NCH&C has reviewed all the data available to them on the quality of the care in 34 of these NHS services. The income generated by the NHS services reviewed in 2011/12 represents 97% per cent of the total income generated from the provision of NHS services by NCH&C for 2011/12. All services are subject to monthly risk assessment through the use of an Early Warning Trigger Tool (EWTT). The Trust has introduced it to act as an early warning system to flag up potential quality and patient safety issues before they occur. Implementation of the tool should reduce the number of Serious Incidents Requiring Investigation (SIRIs), reduce the risk of an unfavourable CQC report and prevent services going into crisis. The original tool was produced by the National Patient Safety Agency (NPSA) in response to the quality of care at Mid Staffordshire NHS Foundation Trust and has been adapted locally to better reflect community services. Patient views and experience are integral to the tool and is reflected in the use of patient surveys and the level of complaints received. Since September 2011 staff across community teams and the inpatient units assess their areas against a checklist with weighted scores, which resulted in an overall RAG-rated score and an indication of what action is required: Green rating (score of 10 or less) No action required, re-assess area next month Amber rating (a score between 11 and 15) Undertake full risk assessment and agree action plan for ‘red’ items within one month. Add to local risk register Red rating (a score of 16 or more) Inform line manager immediately and undertake full risk assessment within one week. Produce an action plan for red items within one week The data from the tool is reviewed monthly in order to identify services with potential issues, as well as identifying key themes common to a number of teams or departments. Key risks are escalated to the Trust’s Management Team and Executive Directors. (see section 3.1.8 for more details) The Trust Board also receives a monthly Integrated Performance Report, which focuses on a number of domains including patient safety, quality and risk. The data is presented in a dashboard format, using RedAmber-Green (RAG) ratings to highlight any areas of adverse performance supported by a narrative explaining the reason for the variance, and actions being taken to mitigate future risks impacting on performance. The Board also receives a Quality and Risk report which provides more operational detail on those areas reported in the IPR. This report is also presented to the Quality and Risk Assurance Committee, and includes the following areas; • Serious Incidents requiring investigation (SIRIs) • Medication Incidents • Falls • Pressure Ulcers • Infection rates • Complaints and compliments Part 2 2.2 Statements of assurance from the Board 2.2.1 Review of services 2.2.2 Participation in clinical audits 15 2.2.2 Participation in clinical audits During April 2011 – March 2012, 6 national clinical audits and 1 confidential enquiry covered NHS services that NCH&C provides. During that period NCH&C participated in 33.3% of national clinical audits and 0% of national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that NCH&C was eligible to participate in during April 2011 – March 2012 are as follows: Name of National Audit Lead organisation Participation from NCH&C? Epilepsy12 Royal College of Paediatrics and Child Health Yes National Diabetes Audit NHS Information Centre Yes Heart Failure Audit National Institute for clinical outcome research (NICOR) No – there was no applicable data available within collection period Sentinal Stroke Audit Royal College of Physicians No – there was no applicable data available within collection period (Led by the Norfolk & Norwich Hospital) Continence Care Audit Royal College of Physicians No – there was no applicable data available within collection period Stroke improvement national audit Royal College of Physicians No – there was no applicable data available within collection period Name of National Confidential Enquiry Applicable to NCH&C? Participation from NCH&C? National Confidential Enquiry into Patient Outcome and Death (NCEPOD) Yes No - there was no applicable data available within the collection period. 16 Quality Account Norfolk Community Health and Care NHS Trust The national clinical audits and national confidential enquiries that NCH&C participated in, and for which data collection was completed during April 2011 – March 2012, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. Name Lead organisation Epilepsy12 Royal College of Paediatrics This is a retrospective audit reviewing data from and Child Health 2010/11 which the acute trusts collect National Diabetes Audit NHS Information Centre The report of two clinical audits – Epilepsy12, and the National Diabetes Audit were reviewed by the provider in April 2011 – March 2012 and NCH&C intends to take the following actions to improve the quality of healthcare provided: Description of actions: • Epilepsy12 – training for all consultant paediatricians who work across the pathway covered by NCH&C, the Norfolk and Norwich University Hospitals NHS Foundation Trust, and the Queen Elizabeth Hospital King’s Lynn NHS Foundation Trust • National Diabetes Audit – The 2010/11 Audit is currently in progress. The NDA report will be published in June 2012 (the NHS Information Centre for Health and Social Care) Number of cases submitted or percentage of numbers of registered cases required Unable to quantify as data collected and cases submitted by GP practices across Norfolk Part 2 2.2 Statements of assurance from the Board 2.2.2 Participation in clinical audits Local clinical audits The reports of 32 local clinical audits were reviewed by the provider during the period from April 2011 to March 2012 and NCH&C intends to take the following actions to improve the quality of healthcare provided: Description of a selection of actions: • Reducing harm from omitted or delayed delivery of medicines in hospital – has achieved the following results: • Reduced the number of patients experiencing an omitted or delayed dose (from 65% to 48%) • Reduced the average number of omitted or delayed doses occurring (from 4.34 doses/patient to 2.06 doses/patient) • Reduced the potential harm caused by omissions or delays in the administration of medicines (from an average risk score of 5.75 to 3.06) • Improved practices around the administration of medicines • Increased awareness amongst staff about this issue and the need for accurate and complete records of medicines administration. 17 • Essence of Care – Dignity and Respect, local consent form devised and implemented • Paracentesis (procedure to drain fluid from the abdomen), Guidelines updated to include that it is appropriate to consider draining to dryness in patients with peripheral oedema • Pressure Ulcer (annual, mandatory), a standardised process implemented to ensure a patient has a Waterlow assessment completed within 6 hours of admission and baseline risk assessments of the MUST nutrition tool are completed, continence and mobility/moving and handling assessments are also completed for all patients • Safeguarding Supervisor’s (Children’s Services), the safeguarding team to arrange a workshop on group supervision and group dynamics • Vestibular baseline audit, following initial gap analysis findings, to re-audit and develop a business case to present to our commissioners to expedite the diagnosis and management of ‘dizzy’ patient’s within NCH&C care • Falls assessment audit, an audit was carried out in November 2011 to determine the number of patients who had a Falls Assessment within 48 hours of admission to our inpatient units. The results from this audit demonstrate that we achieved 92%, a 11% improvement on our quarter two audit results • Hand hygiene audits, the Infection Control Team conduct monthly ‘hand hygiene’ audits at localities and in 2011/12 results across the trust provided a high level of assurance of 99% compliance across the organisation 18 Quality Account Norfolk Community Health and Care NHS Trust 2.2.3 Participation in clinical research The number of patients receiving NHS services provided or sub-contracted by NCH&C in 2011/12 that were recruited during that period to participate in research approved by a research ethics committee was 690. This is an increase of 42% compared with 2010/11 period and shows evidence of NCH&C’s expanding research portfolio. Participation in clinical research demonstrates NCH&C’s commitment to improving the quality of care we offer and to making our contribution to wider health improvement. Our clinical staff stay abreast of the latest possible treatment possibilities and active participation in research leads to successful patient outcomes. NCH&C were involved in conducting 49 research studies during 2011/12 showing a moderate (5%) increase compared with the 2010/11 reporting period. However 65% of studies were national portfolio, compared with 35% in the previous year. 18 of these studies were new projects which were given permission to start in 2011/12. Median approval time was 36 days which is an improvement on last year’s median approval time of 47 days. During 2011/12 five of our clinical teams have been supported in their clinical research activity by the Comprehensive Local Research Network (CLRN) funded Research Site Initiative Scheme, which aims to develop research activity within community care teams and enable teams to host national portfolio research studies to recruit to time and target. All but one of the five teams has been successful in hosting at least one national portfolio study in 2011/12. It is anticipated that teams will build on this success during 2012/13, and that the outcomes of these studies will, in the future, help to inform innovations in the delivery of high-quality care to improve the health and well-being of our patients. There were 29 clinical staff participating in research (as participants) approved by a research ethics committee at NCH&C during 2011/12. This represents an increase of 62% on last year’s figures. Stroke Research Studies Over the 2011/12 period NCH&C conducted seven clinical research studies within the area of stroke (care/rehabilitation). Over the same period, mortality amenable to mortality rate from causes preventable in stroke rehabilitation changed from the previous year by 2.5%. The improvement in patient health outcomes in the area of stroke rehabilitation at NCH&C demonstrates that a commitment to clinical research can lead to better treatments for patients. Research bursaries Research bursaries are awarded to enable staff to develop their research ideas with academic partners into fully funded research proposals Two of last year’s (2010/11) research bursaries awarded to staff at NCH&C have resulted in full applications for funding to the National Institute for Health Research (NIHR) Research for Patient Benefit Scheme in 2011/12 in the area of Person Centered Care for dementia, and complicated grief for people with learning difficulties; the outcome for both is awaited. Two further research bursaries have been awarded in 2011/12. For the 2011/12 period NCH&C has not recorded any publications that have arisen as a result of our involvement in NIHR research. We plan to collect such information during 2012/13 and will be able to report on this activity in next year’s Quality Account. Part 2 2.2 Statements of assurance from the Board 2.2.3 Participation in clinical research 2.2.4 Goals agreed with commissioners 2.2.5 Statement from Care Quality Commission (CQC) 2.2.4 Goals agreed with commissioners Use of the Commissioning for Quality and Innovation (CQuIN) payment framework A proportion of NCH&C’s income during April 2011 to March 2012 was conditional on achieving quality improvement and innovation goals agreed between NCH&C and any person or body they entered into a contract, agreement or arrangement with for the provision of NHS services, through the CQuIN payment framework. Further details of the agreed goals for April 2011 to March 2012 are set out in Part 3 of the Quality Account and for the period April 2012 to March 2013 can be found in Part 2.1 19 2.2.5 Statement from the Care Quality Commission NCH&C is required to register with the Care Quality Commission (CQC) and its current registration status is ‘registered without restrictive conditions’. From April 2011 to October 2011 NCH&C had the following conditions on its registration: April 2011 – Registration with the CQC was confirmed, we were however registered with the following conditions: a. The Registered provider must not carry on the regulated activity “Treatment of Disease Disorder or Injury” in the Local Discharge Unit at HMP Norwich, Knox Road, Norwich, Norfolk, NR1 4LU. This condition was in place following a visit the CQC undertook at HMP Norwich when authorising another provider’s registration. They found that the Discharge Unit did not comply with the regulations because it did not protect people’s right to privacy, dignity, choice and confidentiality. b. The Registered Provider must ensure that the regulated activity of “Accommodation for people who require nursing or personal care” is managed by an individual who is registered as a manager in respect of the activities at or from all Locations. This condition was imposed as the CQC confirmed that this regulated activity must be managed by a ‘registered manager’ as the service is seen to have a social care aspect. There were three Locations affected by this condition, (Mill Close an adult respite unit, Little Acorns and Squirrels both children’s respite units). 20 Quality Account Norfolk Community Health and Care NHS Trust And has taken the following actions: Condition a) To ensure privacy and dignity is maintained at all times, NCH&C ensured that the room is only utilised by one clinician at any time. Two benches have been installed in the recess outside the adjudication room providing a waiting area a few metres away from the consultation room. It will not be possible for any waiting prisoners to overhear any consultations. Privacy screens have also been allocated to the room to protect peoples privacy and dignity. By making the above changes we now protect people's rights to privacy, dignity, choice and confidentiality 3rd June 2011 – NCH&C had confirmation from the Care Quality Commission through issue of a Notice of Decision that the condition applied to our registration, restricting it from providing “Treatment of Disease Disorder or Injury” from the treatment room in the Local Discharge Unit at HMP Norwich, has now been lifted. Condition b) Registered Managers at each of our [3] respite units were appropriately registered with the CQC and the condition regarding these respite units was removed in September 2011 23rd November 2011 – our most recent and up-todate Certificate of Registration was issued without restrictive conditions The Care Quality Commission has not taken enforcement action against NCH&C during the period April 2011 to March 2012. NCH&C has participated in special reviews or investigations by the Care Quality Commission relating to the following areas during April 2011 and March 2012: Three inspections were made within our Joint Community Learning Disability Teams (which are registered through Norfolk County Council) and one within our Learning Disability Adult Respite Unit during the period April 2011 to March 2012. The results are as follows: • Western Joint Community Learning Disability Team was meeting all the essential standards of quality and safety • City Joint Community Learning Disability Team was meeting all the essential standards of quality and safety • North Joint Community Learning Disability Team was meeting all the essential standards of quality and safety but to maintain this it was suggested that we made improvements to ensure we have local systems in place to monitor the quality of the service • Mill Close Adult Respite Unit was found to be meeting the essential standards of quality and safety as listed below: • Outcome 1: People should be treated with Dignity and Respect • Outcome 4: People should receive safe, appropriate care • Outcome 7: People should be protected from abuse • Outcome 16: The service should have quality checking systems in place NCH&C intends to take the following action to address the conclusions or requirements reported by the CQC: • Develop a local feedback questionnaire which will be sent to users of the service with a pre-paid envelope. NCH&C has made the following progress by 31st March 2012 in taking such action: • A local feedback questionnaire has been developed which will be sent to users of the service with a pre-paid envelope. In addition there is established Norfolk County Council feedback systems in place, whereby clients and carers can comment on care /services received. Both Norfolk County Council and NCH&C also have compliments and complaints pathways in place Part 2 2.2 Statements of assurance from the Board 2.2.6 Data quality 2.2.6 Data quality Good quality information underpins the effective delivery of patient care and is essential if improvements in quality of care are to be made. Improving data quality, which includes the quality of ethnicity and other equality data, should improve patient care and improve value for money. NCH&C will be taking the following actions to improve data quality: A number of data quality reports have been designed to monitor a range of key performance indicators on a monthly basis, and the Secondary Uses Service (SUS) dashboards are reviewed regularly in relation to national key indicators. A selection of these indicators are also reported to monthly performance meetings where operational services are held to account for the quality of data held on SystmOne and the Patient Administration System (PAS). These reports are held on a networked drive to ensure they are accessible to key staff involved in the monitoring and reporting of performance and activity data. The Trust has a Data Quality Strategy which will be critical to a number of the Trust’s priorities and objectives, including improving the quality of patient care, compliance with the Information Governance Toolkit version 9 and the need to introduce and monitor the Community Information Data Set (CIDS). This strategy is underpinned by a Data Quality Policy. The purpose of this policy is to ensure the highest standards of data quality throughout NCH&C are achieved. This policy is for all staff collecting and using data and they must adhere to the local and national standards as laid out in this policy. 21 22 Quality Account Norfolk Community Health and Care NHS Trust The Trust has established a Data Quality Forum (DFQ) chaired by the Assistant Director for Performance. The purpose of this forum is: • To assist NCH&C to work to a common set of principles over data quality issues • To share experience, ideas and examples of good practice in business units and corporate functions in taking forward the data quality agenda • To assist NCH&C in the delivery of the data quality agenda in support of key national initiatives, eg, Transforming Community Services Quality Indicators, patient safety, QIPP, and the NHS Outcomes Framework • To action collectively-agreed data quality initiatives • To assist business units and corporate functions in raising the profile of data quality at a local level and making the linkages with the wider agenda outlined in above • To provide a forum for co-ordination of user issues, support arrangements and developments for Data Quality reporting • To review where available, local and national benchmarking resources to identify any issues of data quality and consider the necessary actions required • To review the Data Quality Dashboard against local benchmarks and targets as defined in the Data Quality Improvement Plan, and to monitor trends over time in order to assess progress in improving data quality • The role and function of the DQF has been recently reviewed to ensure it meets the Trust’s strategic and policy objectives in relation to data quality • External validation of our information systems has been undertaken during 2011/12 by our internal auditors and action plans have been developed to further improve these systems NHS Number and General Medical Practice Code Validity NCH&C submitted records during 2011/12 to the SUS for inclusion in the Hospital Episode Statistics which are included in the latest published data under organisation code RY3. The percentage of records in the published data which: • included the patient’s valid NHS number was: • 100% for admitted patient care • 100% for out patient care • included the patient’s valid General Medical Practice code was: • 100% for admitted patient care • 100% for out patient care Part 2 2.2 Statements of assurance from the Board 2.2.7 Information Governance Toolkit attainment levels 2.2.8 Clinical coding error rate 23 2.2.7 Information Governance Toolkit attainment levels NCH&C Information Governance Assessment Report overall score for 2011/12 was 66% thereby achieving compliance at Level 2 and was graded by NHS Connecting for Health as follows: Assessment Level 2 Exempt Total requests Overall score Grade Version 9 (2011-12) 40 1 41 66%* Satisfactory * 66% is the target score for achieving level 2 as set by NHS Connecting for Health and represents a % of all requirements met which are individually weighted The Information Governance toolkit is available on the Connecting for Health website: www.igt.connectingforhealth.nhs.uk The Information Quality and Records Management attainment levels assessed within the Information Governance Toolkit provide an overall measure of the quality of data systems, standards and processes within an organisation. 2.2.8 Clinical coding error rate NCH&C was not subject to the Payment by Results (PbR) clinical coding audit during 2011/12 by the Audit Commission. 24 Quality Account Norfolk Community Health and Care NHS Trust 3.1 Review of quality performance in 2011/12 3.1.1 Overview The Trust has had a challenging year on a number of fronts that are described in detail below. An external review was published into a service previously run by the Trust that offered a number of criticisms and which has significantly shaped the efforts of the Trust during the year. Nevertheless, the year has also seen significant achievements such as high patient satisfaction, a significant tender win and the introduction of new roles to support admissions avoidance to an acute hospital. 3.1.2 Summary of positive achievements in the last year The Trust is proud of its many achievements in the last year. Building on its values of pioneering, personalised care delivered closer to people’s homes, the Trust has delivered exciting and challenging projects and celebrated growth in nationally recognised services. The Trust was proud to be designated as an Early Implementer Site for the national health visiting programme. This designation recognised the high quality of our services and the Trust’s ability to innovate within the field of service redesign. In 2011/12 the Trust continued to deliver significant capital development projects in partnership with commissioners and local communities. New building projects were commenced and/or completed at both North Walsham and Aylsham that will bring a new range of services closer to these communities. Continuing the theme of innovation, one of the Trust’s school nurses received an award for innovation from Anglia Ruskin University for his invention that is designed to help children taking their medication for asthma. The Trust’s Falls Service also received a runner up commendation from the East of England as part of their Celebrating Success Awards. The Trust was awarded a contract worth in excess of £21m for the delivery of 31 Sure Start Children’s Centres that were tendered by Norfolk County Council. This award built on the Ofsted rated ‘outstanding’ delivery of the Trust’s current 3 centres. Part 3 3.1 Review of quality performance in 2011/12 3.1.1 Overview 3.1.2 Summary of positive achievements in the last year 3.1.3 Staff achievements 25 3.1.3 Staff achievements Living our values awards spanned a range of roles within NCH&C from consultants, community nurses, technical instructors and occupational therapists to education facilitators. The award categories are reflective of our Trust’s four values: 1. Home and Community – Someone who regularly demonstrates that they exist to improve the lives of our patients, whenever and wherever needed Winner – Community Integrated Team, North Walsham 2. Pioneering – Someone who looks for innovative and more efficient ways of delivering care to our patients Winners – Palliative Care Coordinators 3. Personalised care – They strive to understand each individual patient’s total needs and join up their health and care requirements Winner – Occupational Therapist, City 4 Team 4. Enabling our people – This colleague is an incredible motivator or encourages others to be the best they can Winner – Education Facilitator (Palliative Care) Colman Hospital I would like to offer my congratulations to each of the winners, as well as the nominees. They truly embody our Trust’s values and I would like to congratulate them on receiving this recognition... I have been deeply impressed by the many examples of colleagues striving to deliver the best possible care and to further improve services for our patients. These dedicated staff are true ambassadors of NCH&C…” Michael Scott, Chief Executive Finalist at national awards A community nurse and care manager was named as a finalist in the national General Practice Awards, ‘Nurse of the Year’ category. Based at Sapphire House, Norwich, Tracey Blazey was one of just over 200 nominations in this category put forward by colleagues. Tracey, who has 30 years’ NHS experience was nominated for the consistently high-quality of care she provides to adults who have learning disabilities. Queen’s Nurse honour A Specialist Neurology Nurse was awarded the title of ‘Queen’s Nurse’ in recognition of her commitment to delivering further improved community-based care. Katrine ‘Trine’ Kiertzner, who has 25 years’ nursing experience, received the title from community nurses’ charity the Queen’s Nursing Institute. The title aims to unite nurses who have promoted high standards of care and encourages them to champion new ways of delivering innovative practices. 26 Quality Account Norfolk Community Health and Care NHS Trust Improving teenagers’ mental health School Nurse, Bernadette Osterberg, is rolling out a trial project to provide innovative care for high school students who have a history of self-harm, substance abuse and risk-taking behaviours. Bernadette aims to improve their mental wellbeing by facilitating joined up care, working with partners such as Child and Adolescent Mental Health Services (CAMHS) and the Mancroft Advice Project (MAP) to enable young people to get access to counsellors, youth workers, and advisers. Family praises ‘absolutely fantastic’ Community Matron A Community Matron has been hailed as ‘an amazing ambassador of the NHS and mankind’ by the family of a former patient. Fiona Baldwin received the praise after caring for the patient at their home for over a year. In a letter, the family said “Fiona showed such competence, care and support to the whole family… and despite mum’s poor health, she would perk up at just the sound of Fiona’s voice... As a person I think she is a truly wonderful lady… and my family extend our warmest thanks to her.” Certificates of recognition Each month we celebrate the commitment of our staff to the continued delivery of excellent care and support. Staff receive a Certificate of Recognition at the Management Forum and are named in the staff newsletter, ‘The Exchange’. Compliments and ‘Thank you’s’ to our staff Below are selections of the hundreds of compliments our staff receive over the course of a year: Beech Ward, NCH Many small acts of kindness noticed. All added to the tranquil, positive atmosphere of the ward... Pulmonary Rehab Service, Kelling Hospital I can bend to put my socks on which I couldn’t before. A very good team, which I hope will continue to help a lot more old codgers... Cranmer House, Fakenham My husband was very lucky to have landed within your ‘embrace’. You run a superb ship. Congratulations... Alder Ward, NCH Dads last days were made so much better than they could have been... Staff at the Mulberry Unit, NCH You are all earth angels... Community Nursing and Therapy team, NCH You all smile which means a lot to us old ‘uns’ Patient aged 92 ½... District Nursing Thank you so much for your support in making Dad’s last days easier for him to bear, at home, with loved ones… Foxley Ward, Dereham Hospital Thanks for all the staff for all their help and friendship for my speedy recovery. I have enjoyed my time with you… Speech and Language Therapy Team The support I received was excellent and my speech has improved greatly. I still have difficulties recalling words, but I continue to use the helpful strategies that you taught me... Part 3 3.1 Review of quality performance in 2011/12 3.1.4 Commissioning for Quality and Innovation (CQUIN) 27 3.1.4 Commissioning for Quality and Innovation (CQUIN) NCH&C has made excellent progress against its CQUIN Scheme by quarter in 2011/12 bringing our total CQUIN earnings for the last financial year to circa £1.25m. CQUINs are contractual commitments which encourage progress to be made within key areas of local services. As a reward for meeting these commitments our Trust will now receive significant investment from our commissioners which is funding that can be used to make further improvements in the future. Indicator Quarter 1 Achievement/Outcome Quarter 2 Quarter 3 Quarter 4 Increase number of patients provided with telehealth in the community and audit the outcomes 85% 100% 100% TBC Use of the End of Life, Gold standard framework 100% 66% No payment due 100% Use of the End of Life, Liverpool Care pathway 100% 100% 100% TBC Medicines management 100% 100% 100% 100% Patient satisfaction - Adults 100% 100% No payment due 100% Patient satisfaction – Children’s services 100% 100% No payment due 75% Reduction in injurious falls No payment due No payment due No payment due 100% Improve carer experience - Adults 100% 100% 100% 100% Improve carer experience – Children’s 100% 100% 100% 100% Achieve UNICEF accreditation stage 1 No payment due No payment due 100% 100% TOTAL 96% 98% 100% TBC 28 Quality Account Norfolk Community Health and Care NHS Trust 3.1.5 Performance highlights Areas of achievement During 2011/12 the Trust had a number of important targets to achieve or maintain. One of the key performance targets to be achieved was the 18 week wait Referral to Treatment (RTT) target, where 100% of admitted and non-admitted patients had to receive a definitive treatment or intervention within 18 weeks of referral. Throughout the year, NCH&C made significant improvement with most services either achieving the target on a consistent basis, or being close to 100%. The one service that did not meet this until the end of March 2012, was podiatric surgery. Throughout the year, and in line with the previous year, NCH&C maintained low levels of delayed transfers of care. On average, patients whose discharge was delayed for non-medical reasons occupied only 4.1% of beds, compared to 4.4% the previous year. There are no contractual targets in place for this measure. This improvement in the discharge process is as a result of the implementation of the ‘Productive Ward’ across NCH&C’s community hospitals. Analysis of the data from Norfolk and Norwich University Hospitals NHS Foundation Trust (NNUH) suggests there may be circumstances that cause regular and significant peaks in demand for community beds. If the peak in demand is unavoidable, the commissioner will need to decide whether to increase capacity or accept delays will occur. In 2010/11 the Trust experienced nine cases of C.diff. For 2011/12, NCH&C had a ceiling of no more than nine cases for C.diff and one for MRSA bacteraemias. By the end of March 2012, there were eight reported cases of C.diff and no MRSA bacteraemias. All reported cases have been subject to Root Cause Analysis (RCA) to review lessons learned. As part of the Provider Management Regime (PMR) with NHS Midlands and East, NCH&C is required to report the number of items delivered to patients from its Central Equipment Store. Throughout the year, the Trust delivered in excess of 23,600 items of which more than 99.3% were delivered within seven days of receipt of a referral. The SHA target is 100% of items delivered within seven days. From April 2011, the NHS East of England (prior to the clustering of strategic health authorities), requested that the Trust commence reporting of Venous Thromboembolism (VTE) assessments for patients admitted to its community hospitals. The Trust established a locally agreed trajectory, against which it would be monitored, and to then achieve the national target of 90% compliance by February 2012. By January 2012 the 90% target was achieved. Part 3 3.1 Review of quality performance in 2011/12 3.1.5 Performance highlights 29 Meeting targets 2011/12 Indicator Target or upper ceiling 2011/12 performance Trend MRSA bacteraemia No more than one case during 2011/12 0 cases Stable MRSA screening - elective patients 100% of patients having planned surgery screened for MRSA 100% Stable Clostridium difficile No more than nine cases during 2011/12 8 cases Stable Delayed transfers of care No more than 6% of beds occupied by patients whose discharge is delayed for non-medical reasons 4.1% Stable Venous Thromboembolism Percentage of admissions who had a VTE (VTE) assessments assessment undertaken 90.4% Increasing Community equipment store >99% of items delivered within seven days of receipt (CES) response within seven days 99.4% of a referral Stable Health visiting 95% or more of mothers receiving a New Birth Visit within 28 days of birth 97.1% Stable Injurious falls Achieve a reduction in the number of falls resulting in harm per 1,000 Occupied Bed Days 4.03 Declining 30 Quality Account Norfolk Community Health and Care NHS Trust Areas of non-delivery There was one consistent variant to 18 week performance. This was within the Podiatric Surgery Service. During the year a number of operational actions were introduced and underpinned by comprehensive analysis and modelling of demand, capacity, backlog and activity. This enabled the service to work towards full compliance with the 18 week wait target. A performance notice and exception notice were issued (without incurred financial penalty) which remains in place at the time of writing. This service has been 18 week compliant since April 2012. The Smoking Cessation service agreed an annual target for 2011/12 with NHS Norfolk of 2,700 quits. Despite a comprehensive restructure of the service to deliver the quit target, achieving the necessary level of referrals supported by a strong conversion rate proved challenging. It became apparent during the year that the Trust was starting to deviate from its trajectory and a number of actions were established to improve referrals rates. However, the subsequent referrals generated were not sufficient to recover the level of quits required, and as such the Trust failed this target. For 2012/13, the Trust will work in partnership with NHS Norfolk and Waveney to understand the demographic context of the targets and look at new ways of working with partner organisations to improve quit rates and referrals. A target of 2000 quits has been set for 2012/13 by the commissioners. The focus for the service for the coming year will be to achieve its target of 2000 quits including an impact on target groups such as routine manual workers and to demonstrate how it has supported the wider health system in achieving their overall target of 6000 (see section 3.1.10 (d) research project). The Trust was commissioned by NHS Norfolk and Waveney to provide a Continuing Health Care assessment service. Throughout the year, the Trust failed to achieve NHS Norfolk and Waveney’s target of 100% of assessments undertaken within 28 days of referral. Although this was in part, compounded by factors related to external agencies, the management of the service transferred to NHS Norfolk and Waveney in February 2012 in order that they may take control of a wider strategy around continuing care. Missing targets 2011/12 Indicator Target or upper ceiling 2011/12 performance Trend 18 weeks Referral to Treatment 100% of patients seen within 18 weeks of referral 98.7% Stable Smoking cessation To achieve 2,700 successful quits during 2011/12 2,051 Declining Part 3 3.1 Review of quality performance in 2011/12 3.1.6 Clinical quality and Quality Goals 3.1.6 Clinical quality and Quality Goals This section outlines the Trust’s progress against national and regional quality improvement priorities as well as the Trust’s own priorities and Quality Goals from 2011/12 under the following headings; • Patient safety – protecting people from harm • Effectiveness of care – promoting a culture of continuous improvement through audit and research projects and implementing NICE guidance • Patient experience – listening to what our service users think Our Quality Goals for 2011/12 were developed through the annual planning process and reported in the forward-looking section of our Quality Account for 2010/11 and linked to the Trust’s Quality Improvement Strategy. They are listed as follows: 1. To reduce levels of pressure ulcers 2. To reduce levels of attributal clostridium difficile (C. Diff) 3. To reduce levels of MRSA bacteraemia 4. To reduce levels of falls resulting in serious harm 5. To reduce levels of medication errors Under the Patient Experience heading we also set the following goals (see section 3.1.7 for details): 1. Establishment of a patient experience tracker tool (CQuIN indicator 5) 2. Carer satisfaction surveys (CQuIN indicator 7) 3. Improvement of the Ipsos Mori areas that scored <50% (Communication, Environment, Information and involvement) 31 Quality Goal 1 - To reduce levels of pressure ulcers The Trust is committed to achieving the aim of eliminating all avoidable pressure ulcers by December 2012 and this is our top clinical improvement priority for 2012/13. To achieve this aim the Trust has set up a strategy group which is chaired by our Chief Executive and has clinical and corporate support on the steering group. To support this activity, the following task and finish groups have been formed: • Clinical improvement and outcomes • Partnership working and patient engagement • Performance and improvement • Education, clinical competencies and skills training During 2011/12 NCH&Creported 111 serious incidents requiring investigation (SIRIs) of grade 3 and 4 pressure ulcers. The Trust has sought to encourage a positive reporting culture and has held a number of learning events to raise awareness of the positive effects of reporting all incidents and Pressure Ulcers specifically. At the beginning of 2011, NCH&C agreed a variation on deadlines for pressure ulcer reporting with NHS Norfolk and Waveney (NHSN&W). It was agreed that the full root cause analysis 45 day report would not be required but instead a more detailed seven day update would be submitted. In order to closely monitor the ambition to eliminate Grade 2, 3 & 4 avoidable pressure ulcers, a change in SIRI reporting requirements to NHSN&W and the Midlands and East Strategic Health Authority has been agreed as from May 2012. 32 Quality Account Norfolk Community Health and Care NHS Trust Three workshops have been held across the county to launch the new Prevention and Management of Pressure Ulcer policy which were well attended by our clinical staff. Each of the three sessions included shared learning, e-learning, incident reporting, the use of pressure relief equipment, Nutrition Malnutrition Universal Screening Tool (MUST) tool and Waterlow scoring training. An important outcome of the workshop was to resource the clinical leaders to train their teams in the use of the management tools. This was achieved. This is being followed up through the provision of a number of ‘roadshows’ for all teams in 2012/13. In the last year, the Trust set a target of 100% of older people identified as at risk to be assessed within 48 hours of admission using the MUST tool in line with the local QIPP target. Against this 48 hour assessment target whilst quarter 4 results were lower than quarter 3 we can report an overall improvement for the year of 8%: Qtr 1: 80.5% Qtr 2: 85.4% Qtr 3: 90.3% Qtr 4: 87.6% Outcomes from the recent organisation-wide pressure ulcer audit will be used to inform the focus of the clinical improvement programme. The Trust has also engaged with the SHA Expert Pressure Ulcer Group and the Tissue Viability Network Group, and is seeking to implement a tissue viability team through additional commissioning income and via internal resources. Going forward, the Trust will continue roll out of the Safety Thermometer for the four ‘harms’ which includes the recording of pressure ulcer data (see 2.1.1 for more information). Quality Goal 2 – Reduction in healthcare acquired infections (HCAI) During 2011/12 the Infection Prevention and Control (IPC) team have worked closely with NHS Norfolk to further develop key information packs for MRSA and Norovirus which are in use within NCH&C and the community generally. We have endeavoured to work closely with all healthcare providers within Norfolk to develop a joint response to Norovirus and the issues it causes across the health economy. Following the Chief Nursing Officer’s letter of March 2011 and as discussed below we have developed a Clostridium Difficile (C.diff) scrutiny group which will allow us to more accurately report our levels of C.diff. In the future (2012/13) the Trust plans to work with NHS Norfolk to develop a business case for an IPC liaison nurse to develop IPAC within primary care ensuring high risk patients are identified and treated for MRSA and closely monitor patients at risk of a relapse of C.diff. The IPC team also hope to further engage with primary care in protecting patients from healthcare acquired infections across Norfolk. Part 3 3.1 Review of quality performance in 2011/12 3.1.6 Clinical quality and Quality Goals 33 b. To reduce levels of attributable Clostridium difficile (C.diff) Following a period of four months with no C.diff cases occurring, NCH&C has reported one new case for January 2012. This brings our total for the year April 2011 to March 2012 to eight cases against an annual ceiling of nine. This compares to nine cases in 2010/11. • An Infection Control Nurse attends a pan Norfolk meeting regularly to update on progress • A Catheter Care Policy: Competencies and Guidelines has been completed and is awaiting approval • Regular training has been organised for staff via the Trust’s Training Department C.diff cases against a monthly trajectory April 2011 2 to March 2012 6 5 4 3 2 1 0 pr -1 M 1 ay -1 Ju 1 n11 Ju l-1 1 A ug -1 Se 1 p1 O 1 ct -1 N 1 ov -1 D 1 ec -1 Ja 1 n1 Fe 2 b1 M 2 ar -1 2 • A working definition of CAUTI has been agreed with the Consultant Microbiologist A scrutiny group is convened, for each case of C.diff, which discusses the findings of the root cause analysis. Number of Cases The monitoring of catheter acquired infections is of high importance to NCH&C. The Trust aims to reduce catheter acquired infections by 50% by December 2012 in line with a local QIPP target. In working towards this target a clinical task force has achieved the following outputs in the last year: A a. Catheter Acquired Urinary Tract Infection (CAUTI) NCH&C has a robust procedure in place which dictates that all C.diff positive specimens are also tested for lactoferrin, in line with national guidance. A positive lactorferrin result indicates an inflammatory response within the bowel, ie, a true infection rather than colonization. This ensures only true cases of C.diff infection are reported and not cases of colonization. 2011-12 Trajectory • A pathway has been completed and approval is awaited for a ‘trial without catheters’ to be carried out by the continence team • Intermittent self catheterisation assessment and training is ongoing as per NICE guidelines • A catheter care plan has been completed • Appropriate measures and baselines have been put in place to inform work going forward. This was required before a formal target could be put in place 2010-11 Actual 2011-12 Actual c. To reduce levels of MRSA bacteraemia There were no cases of MRSA bacteraemia in 2011/12. This compares to one case in 2010/11. Quality Account Norfolk Community Health and Care NHS Trust Inpatient falls reported by degree of harm 100 60 40 20 No harm Moderate harm Low harm Severe harm 12 ar -1 2 bFe M 1 12 n- Ja 1 D ec -1 1 -1 -1 ct ov N O Se p- 1 11 1 -1 l-1 ug Ju A 1 11 n- Ju -1 ay A pr -1 1 0 M Number 80 This improvement has been a result of significant and ongoing work around reducing falls across units to the point that further significant reductions are not expected as current evidence-based interventions and improvement techniques have now been put in place. The evidence seems to back this up suggesting there was a step change earlier in the year at which point the average has stabilised rather than continuing to improve. As such performance is expected to remain at this level if techniques are continued and with no other changes arising (e.g. change in patient profile). Falls/1000 OBD performance - inpatient units 7.0 6.5 6.0 5.5 5.0 4.5 4.0 3.5 3.0 2.5 2.0 pr -1 1 ay -1 Ju 1 n11 Ju l-1 1 A ug -1 Se 1 p1 O 1 ct -1 N 1 ov -1 D 1 ec -1 Ja 1 n1 Fe 2 b1 M 2 ar -1 2 The graph below shows the degree of harm of patient falls from April 2011 to March 2012. M The aim for 2011/12 was to improve outcomes for patients in inpatient units through the reduction of falls to meet or be below 4.4 per 1000 Occupied Bed Days (OBD). The graph below demonstrates the inpatient falls compared to 1000 OBD for April 2011 to March 2012. March saw average Injurious Falls/OBD results again fall well below last year’s performance and significantly below the CQuIN target of 4.4. This has led to a final year average against the CQuIN marker of 4.0 Injurious Falls/1000 OBD down from 5.2 last year. There remains significant variation month by month, and unit by unit, as even a small number of falls can raise this figure very quickly. A Quality Goal 3 – To reduce levels of falls resulting in serious harm Falls/1,000 OBD 34 2011/12 Performance 2011/12 Target 2011/12 Average Part 3 3.1 Review of quality performance in 2011/12 3.1.6 Clinical quality and Quality Goals Clinical Audit An audit was carried in November 2011 to determine the number of patients who had a falls assessment within 48 hours of admission to our inpatient units. The results from this audit demonstrate that we achieved 92%, an 11% improvement on our quarter two audit results. An action plan was produced in quarter one following the guidance from Patient Safety First. The action plan has been updated demonstrating the actions carried out during quarter three, such as a programme of training, an environment review, an assistive technology pilot on one of the wards and the roll-out of the ‘intentional rounding’ pilot. Falls Service named ‘runner up’ NCH&C’s Falls Prevention Service was named as runner up at the NHS East of England Strategic Health Authority’s ‘Celebrating our Success’ Awards last year. The service was shortlisted in the ‘Whole Health Economy Engagement’ category for its work to help people avoid a fall by providing proactive interventions and support to at-risk patients. The team ensured over 444 unnecessary hospital admissions due to falls were avoided between April and June 2011. They developed a joined up approach alongside other NCH&C services and partners – such as GPs, Norfolk County Council, NHS Norfolk and care homes – to identify and provide care to patients at risk of suffering a fall. Falls Champions have also been introduced to deliver training to other clinicians to help them to identify causes of falls and consider effective interventions. The corporate objective of fewer than 20 incidents of moderate harm or above has been achieved with 13 occurring in the period April 2011 to March 2012. The following graph shows the trend of severity since April 2011, and indicates that moderate harm incidents are stable at between 1 to 3 per month (mean = 1), low harm incidents increasing very gradually, and no harm incidents increasing steadily, indicating the continuing development of a healthy reporting culture. This still represents a very small proportion of the activity involving medicines within the Trust. Breakdown of incidents by severity, with trends 80 70 60 50 40 30 20 10 0 pr -1 M 1 ay -1 1 Ju n11 Ju l-1 1 A ug -1 1 Se p11 O ct -1 1 N ov -1 1 D ec -1 1 Ja n12 Fe b1 M 2 ar -1 2 The low rate of falls within our inpatient units demonstrates that patients are continuing to receive high quality and safe services from our Trust. Injurious falls present a significant risk to the health and independence of patients as they can extend a patient’s length of stay or even result in an acute hospital admission. Quality Goal 4 – To reduce levels of medication incidents A Patient safety 35 No harm Moderate harm Low harm The dip in no harm incidents reported in March needs further investigation. The number of incidents in the prison setting has reduced since a peak in November; 30 incidents were reported in November, and only 13 in March. This gradual reduction was off-set by an increase in the in-patient units due to a focus on reporting all incidents of delayed or omitted doses, which related to ongoing audits as part of the CQUIN scheme. However, in-patient units reported 41 no harm incidents in February, but only 16 in March. The reduction in no harm incidents may also be related to other factors such as low staffing numbers or end of year tasks that have taken the focus off incident reporting were there was no harm. The split of medication incidents across the Trust is mostly in proportion with previous months, with the majority being reported in the prisons and inpatient units. 36 Quality Account Norfolk Community Health and Care NHS Trust Controlled Drugs Incidents The incidents occurring involved a range of different issues, including missed doses, syringe driver issues, wrong patient administration and management of CD stocks. For quarter 4 (January 2012 – March 2012) there were no incidents resulting in moderate harm. Controlled drug incidents by month and severity • Reduced the number of patients experiencing a omitted or delayed dose (from 65% to 48%) • Reduced the average number of omitted or delayed doses occurring (from 4.34 doses/patient to 2.06 doses/patient) • Reduced the potential harm caused by omissions or delays in the administration of medicines (from an average risk score of 5.75 to 3.06) 25 20 Number This campaign has, over the course of the last 12 months, demonstrably: • Improved practices around the administration of medicines 15 10 • Increased awareness amongst staff about this issue and the need for accurate and complete records of medicines administration. 5 Percentage change in mean risk score M ar -1 2 12 12 bFe 1 nJa D ec -1 1 1 -1 ov N ct -1 11 Low harm O 1 p- -1 ug Se A 11 l-1 1 n- No harm Ju Ju -1 1 ay M A pr -1 1 0 7 Moderate harm 6 5 4 Clinical Audit: Reducing harm from omitted or delayed delivery of medicines in hospital: 3 2 In February 2010 the NPSA issued an alert warning of the risks of delaying or omitting the administration of medicines in inpatient units. To ensure that this alert was embedded thoroughly into practice and there was a demonstrable improvement, it was decided that the inpatient units would be audited and a campaign run to raise staff awareness and implement the required actions. The audit found that there is much good practice occurring and the vast majority of medicines were administered at the right time and recorded correctly and appropriately. 1 0 Q2 Q3 Q4 Target This graph shows that the mean risk score has reduced from an average of 5.75 in the baseline audit to 3.06 in the quarter 4 audit. This is very close to the target of 3. The units that have not yet achieved the agreed targets for this audit will be asked to produce an action plan to remedy their local issues. These units will then be re-audited within 3 months to check progress. All units will be re-audited annually to ensure that this issue remains high on the agenda. There are still areas where the Trust can improve, such as reducing interruptions during medicine rounds, ensuring robust systems are in place for recording administration and reviewing prescription charts, and these should continue to be monitored locally. There should also be an annual audit of prescription charts with the audit targets set in this campaign as the baseline standard. Part 3 3.1 Review of quality performance in 2011/12 3.1.7 Patient experience 37 3.1.7 Patient experience 3.1.7.1 Patient and carer surveys Patient experience is a main pillar of NCH&C’s strategy to keep the patient at the centre of all that we do. The following patient and carer experience survey work has taken place as part of the delivery of NCH&C Patient Experience and Involvement Strategy April 2011 – March 2013. Work will continue into 2012/13 before a refreshed strategy based on findings from this period will be implemented. Early studies show some excellent results for the Trust and are described below. Picker Inpatient Survey Results NCH&C commissioned the Picker Institute Europe to conduct a survey among inpatients staying in the Trust’s community hospitals. Face-to-face interviews were conducted in 13 community hospitals by professional market research interviewers during February 2011. A total of 122 (48%) of patients from participating hospitals took part in the survey which is an excellent response rate. The overall ratings were as follows: • 97% of respondents rated care as excellent, very good or good (39% excellent, 45% very good, 13% good) • 97% said they would recommend the hospital to others (83% said definitely while 14% said probably) • 90% of respondents felt they were always treated with respect and dignity by hospital staff • Almost nine out of ten patients (86%) felt that the nurses caring for them were always responsive to their needs • 89% felt they were involved in decisions about their care and treatment (67% definitely and 23% to some extent) The Trust has taken a number of actions as a result of recommendations: • Healthy food options are always available and nutritional booklets are utilised with the patient to support them in selecting healthy food options and the catering satisfaction survey has been updated to include a question about healthy food options being available. • Provision of ward information on admission and a general patient information booklet has been developed and agreed. Unit specific detailed information is currently being developed based on an agreed template. 38 Quality Account Norfolk Community Health and Care NHS Trust Local Patient Experience Surveys Adult services 3551 local surveys were completed to gather feedback and subsequently improve patient experience focusing attention on adult services at Norwich Community Hospital and St James Clinic, King’s Lynn; Orthopaedic Triage, MSK Physiotherapy, Podiatry and Biomechanics. The methodology used to collect data was through the patient experience software system Meridian where information is collected in a variety of ways: • electronically through email • through a touch-screen kiosk • through paper surveys The reporting of all results was service specific. There were three key themes for the survey; information/ involvement, environment and communication as well as ‘general’ covering overall satisfaction and would you recommend this service. All surveys went live on 1 July 2011 and continued until end February 2012. The key results are show below: 3551 surveys completed Survey Theme 97.4% overall satisfaction across all surveys Overall satisfaction rating General 96% Information/Involvement 95% Environment 100% Communication 98% The comments received resulted in a number of actions: • Improved service specific information has been developed including information on what to expect at first appointment. Patient Information leaflets have been produced for all four services and are sent with appointment letters • Improved directions and parking information at Norwich Community Hospital is now issued; a new site map has been produced giving clearer details on parking and directions to the site and once on site • Improved signage at Norwich Community Hospital has been put up from the car park to main reception for clinics and clearer signage once inside the main building for clinic areas has been added • Improved Biomechanics and Orthopaedic Triage waiting areas at Norwich Community Hospital through both areas being de-cluttered, clear notices now being displayed in Biomechanics welcoming patients to the service and the reception staffed regularly, notice board displays have been updated in Orthopaedic Triage. This work is in progress currently Part 3 3.1 Review of quality performance in 2011/12 3.1.7 Patient experience 39 Children’s Services The comments received resulted in a number of actions: A programme to gather and improve information to be used to improve children and families experience focusing attention on clinics provided at Upton Road Children’s Centre, Norwich was delivered during 2011/12. • Existing Patient Information leaflets have all been updated to include additional information requested prior to first appointment The methodology used to collect data was through the patient experience software system Meridian’ where information is collected in a variety of ways; electronically through email, through a touch-screen kiosk or paper surveys with the reporting of all results service specific. There were three key themes for the survey; information/involvement, environment and communication as well as ‘general’ covering overall satisfaction and would you recommend this service. All surveys went live on 1 July 2011 and continued until end February 2012. The results of this survey are shown below: 1015 surveys completed 95.2% overall satisfaction across all surveys • Improved waiting area for children of all ages; additional toys acquired • A more accessible version of the survey was developed via an easy-read format Local Carer’s Experience Surveys Within the Trust a holistic approach to care is championed and carer and family feedback is of significant importance to us in measuring our overall performance. Two surveys were delivered in 2011/12 with this group specifically in mind. A carer’s satisfaction survey was carried out focussing on interactions with Case Managers and in the Trust’s residential short breaks service for children. The methodology used in both surveys was a system called ‘health feedback’ consisting of a very simple A5 size survey card completed manually, online or via a free phone number. The surveys commenced in July 2011 and ran to December 2011. In addition to the survey questions respondents were also asked for their comments. The findings were as follows: Adult services: Survey Theme Overall satisfaction rating General 92% Information/Involvement 91% Environment 99% Communication 96% •100% felt they were always or usually treated with respect by staff • 99% of carers felt they were involved as they wanted to be • 99% felt the information they were given had been very or fairly helpful • 95% felt very satisfied with the overall experience, 5% fairly satisfied • 91% felt they were very satisfied with the way staff communicated with them 40 Quality Account Norfolk Community Health and Care NHS Trust As a result of this survey, the following key actions have been taken: As a result of this survey, the following key actions have been taken: • Improved information leaflets have been drafted and will be personalised to each area • Improved involvement of parent/carers in the planning of care for the child; each child will have a full review of their short breaks care package six monthly • Commitment has been taken to ensure a change of Community Matron will be well communicated and explained to carers • A carers focus group took place in March 2012 to discuss survey results, actions and future recommendations • Named member of staff responsible for organising the booking with Parents/carers contacted by phone if their booking needs to be amended giving them as much notice as possible • A privacy and dignity action plan is being written for each unit. To maintain this during personal care “stop” and “go” signs have been placed on toilet and bathroom doors. Each child will also have a name plate and a photograph on their room during each stay to identify personal space • Increased communication is aided through a newsletter which has been developed to improve communication between parents/carers and the units • A re-survey took during March 2012 to determine if actions put in place have improved satisfaction Community Services Survey – February 2012 Children’s services: • 96% parents/carers felt very or fairly involved in the planning of care for their child • 65% said there had been no changes to their booking with 35% saying it had been changed only once or twice • 55% said they were very satisfied with the allocation change, 25% fairly, 15% neither satisfied nor dissatisfied • 74% felt their child had always been treated with respect with 26% saying usually • 52% felt very confident their child’s individual needs had been met, 43% fairly • 70% said staff had been very helpful with 30% saying fairly helpful • 70% were very satisfied with their overall experience of the service and 30% were fairly satisfied NCH&C took part in a community services survey, coordinated by Hounslow and Richmond Community Healthcare for all community trusts. Patient Perspective has been commissioned to conduct the survey and provide analysis and reporting to each participating trust. The survey focused on Podiatric Surgery, Continence, Paediatric Speech and Language Therapy (SALT), Adult SALT and Wheelchair Services. The survey closed at the end of March 2012 and results show comparative data for NCH&C with five other community trusts. Scores for privacy, dignity and respect gave the highest scores for NCH&C, closely followed by the quality of service received and inclusion in discussions about care. Lower comparative scores were recieved for patients being told how long the time of waiting for an appointment was likely to be, transport to and from hospital and the opening hours of services. Part 3 3.1 Review of quality performance in 2011/12 3.1.7 Patient experience 41 3.1.7.2 Patient Stories Advocacy – Net Promoter A key objective within NCH&C Patient Experience & Involvement Strategy April 2011 to March 2013 is to “embed patient stories as an in-depth qualitative methodology in NCH&C”. The Trust has made a number of service improvements as a result of this work. NCH&C has made good progress in the use of the net promoter methodology in 2011/12 and will continue to develop this tool as a key indicator of patient satisfaction and service quality. The results from 2011/12 specifically relating to net promoter are as follows: • SureStart Children’s Centre at Bowthorpe, West Earlham and Costessey has increased communication within GP surgeries, local libraries and schools about services offered at the Centre. The content of a “Stay and Play” session had been altered to meet the requested needs of parents attending with their children. The centre was assessed in 2011 as “outstanding” by Ofsted and commended on their use of parent stories, requesting more were conducted. From the Picker Institute Survey 2011 • Starfish West Learning Disability & Behaviour team have a new service leaflet designed for parents/carers and have improved the referral process from Paediatricians into the service. • Colman Centre for Specialist Rehabilitation Services has involved patients more in the discharge planning process and has improved transition processes from in-patients to outpatient services. 97% said they would recommend the hospital to others (83% said definitely while 14% said probably). 3% said they would not. From the Adult Services Survey 2011/12 94.5% said they would recommend the service to a friend or relative if they needed similar treatment, care or advice (85.5% very likely while 9% said fairly likely). Just under 1% were very or fairly unlikely to recommend. From the Children’s Services Survey 2011/12 95% said they would recommend the service to a friend or relative if they needed similar treatment, care or advice (79.5% very likely while 15.5% said fairly likely). 3% were very or fairly unlikely to recommend. Comparison to results in 2010 Survey results from 2011/12 show a significant improvement compared to the results of the Ipsos MORI Patient Experience Survey in 2010 where 68% of patients were very likely to recommend and 58% of parent/guardians. 42 Quality Account Norfolk Community Health and Care NHS Trust 3.1.7.3 Six Lives Programme – improving access to healthcare for people with a learning disability The Trust has embraced the challenge of implementing the Six Lives programme with commitment. Several projects have been delivered to improve the quality of care given to patients with a learning disability and their experience of the Trust’s services. A new protocol ‘Improving Access to Healthcare for People with a Learning Disability’ has been developed and the ‘Information for Patients’ policy has been reviewed and reflects the requirement to provide accessible information to all patients. Both documents have been launched and are available on the Trust’s intranet. A three-tiered approach to staff training has been agreed: 3. Learning Disability Champions – the development of a full day programme is underway The Patient Experience and Involvement Team will adopt a range of approaches to ensure both patient and carer satisfaction and involvement in service development is embedded within processes. This has commenced with one focus group already being held and a programme of activity is planned during 2012 whereby representatives will attend the existing Carer’s Forums across the county to listen to views and action plan accordingly. The patient story methodology will also be used to capture experiences of patients with learning disabilities and their carers which will provide depth to the data captured and further strengthen the evaluation process. A process for flagging patients with a learning disability on electronic patient systems is available. These processes also prompt staff to document any reasonable adjustments that are made to meet individual needs. Work is underway to develop a system for those services not currently using these electronic systems. The Project Lead will continue with monthly steering group meetings to ensure actions against the evaluation phase of this project are carried out and reported on as appropriate e.g. patient and carer experience surveys, Essence of Care audits. A programme of specific audits will also be conducted, commencing in June 2012. 1. Basic learning disability awareness – provided as part of Trust induction and all existing staff have received a basic awareness information sheet 2. Learning disability awareness – two hour training session available to all staff but as a minimum all Team Leaders are required to attend and cascade to their teams (over 300 staff have attended to date) A programme of work for the next 12 months will embed into practice the policies and processes that have been developed to support compliance against Six Lives and ensure sustainability. This programme includes the review of care planning documentation to facilitate the recording of any reasonable adjustments that are being made within the in-patient units and training for teams using SystmOne so that the method adopted to flag patients and record any reasonable adjustments is clearly communicated. 3.1.7.4 Single Sex Accommodation The Trust continues to prioritise patient privacy and dignity. During 2011/12 there have been no breaches of any milestones as set out in NCH&C’s Eliminating Mixed Sex Accommodation (EMSA) plan and therefore no financial penalties incurred. Further, there were no reportable breaches of single sex accommodation. The Trust expects this performance to continue into 2012/13. Part 3 3.1 Review of quality performance in 2011/12 3.1.7 Patient experience 43 3.1.7.5 Patient Environment Action Team (PEAT) Results for 2011 It should be noted that as from 10 May 2012 St Michaels hospital closed and services were transferred to the new build North Walsham Hospital. In April 2012, the National Patient Safety Agency confirmed NCH&C’s PEAT results 2011 for environment, food and privacy and dignity for each hospital within our organisation as follows: Any required improvements to the buildings/ environment will be conducted as part of the 2012/13 capital and minor works plan. The results of PEAT are published on the NHS Information Centre website www.ic.nhs.uk and are also available to the public on www.data.gov.uk Site Name Environment Score Food Score Privacy and Dignity Score Colman Hospital Good Good Good Norwich Community Hospital Good Good Good Dereham Hospital Acceptable Excellent Good North Walsham Hospital Acceptable Good Good St Michaels Hospital Good Good Excellent Kelling Hospital Acceptable Good Good Swaffham Community Hospital Acceptable Excellent Good Ogden Court, Wymondham Good Good Excellent Cranmer House, Fakenham Good Excellent Excellent Benjamin Court, Cromer Good Good Excellent 44 Quality Account Norfolk Community Health and Care NHS Trust 3.1.8 Learning from incidents and complaints Complaints and Compliments From April 2011 to March 2012 NCH&C received 192 complaints, in comparison to 195 during the year 2010/11. The Trust continues to use the number of complaints as a clear indicator of patient satisfaction alongside our patient experience programme. Two main themes arising from analysis of complaints include the single point of referral, which is under review, and attitude of staff, which is also receiving attention from our internal training team. New courses are under development focussing on customer care and professional behaviours. Patient compliments are also measured and this year the Trust has received around 335 compliments. The dedication and commitment of our frontline staff is a recurring theme of the compliments received. (see section 3.1.3 for a summary) Learning from complaints is collated from the Service Managers following an investigation and communicated across the organisation via the Quality & Risk monthly report (seen at Quality & Risk Assurance Committee and the Trust Board) which is published on the Trust’s website and through the monthly staff newsletter. Themes from complaints are taken to the senior clinical management team (CMT) for discussion and forward planning. Serious Incidents Requiring Investigation (SIRIs) and Never Events Serious Incidents are reported into a central team and information is collated via DATIX a web-based risk management tool. The Executive team see every serious incident and are able to ensure that corporate support for investigations is given to operational teams where required. Themes from serious incidents inform learning events which are held quarterly and attended by senior clinicians and management. The SIRI log and tracker are presented at the Trust’s Clinical Management Team monthly to share learning and information across all clinical teams. From April 2011 to March 2012 NCH&C have reported 136 SIRIs, these can be broken down as shown below. From April 2011, NCH&C and NHS Norfolk made the decision in line with national best practice to report all grade 3 and 4 pressure ulcers as a SIRI. This led to an increase in the numbers reported. NCH&C reported two allegations of potential abuse. One is still under investigation and a member of staff has been dismissed for allegedly abusing an adult patient. NCH&C reported on a competency issue which involved an agency nurse. The nurse is currently under an interim order by the Nursing and Midwifery Council (NMC) and suspended from practice. There were six unexpected deaths in the inpatient units and all were investigated (four were referred to the Coroner) and none identified as attributable to the care or competence of the staff. Part 3 3.1 Review of quality performance in 2011/12 3.1.8 Learning from incidents and complaints Breakdown of SIRIs by type 2011/12 SIRI information Total Apr 2011 to March 2012 45 National Patient Safety Agency Report (NPSA) Pressure Ulcer Acquired under care of NCH&C - Grade 3 75 Pressure Ulcer Acquired under care of NCH&C - Grade 4 36 The National Patient Safety Agency have recently published its latest Patient Safety Incident Report. The report demonstrates that NCH&C are amongst the highest 25% of reporters within its cluster. The NPSA states “That organisations that report more incidents usually have a better and more effective safety culture.” Abuse 2 Incident reporting across NCH&C has steadily increased since the implementation of DATIX Web together with increased training and awareness promoted throughout the organisation. Professional competence 1 Patient Accident 10 Unexpected Death 6 Medication 2 Information / Documentation 1 Child Protection 1 Infection control 1 IT 1 Pressure Ulcer Acquired outside the care of NCH&C Expected Death Self harming behaviour Media interest (potential) Other Total 136 Never Events The Department of Health have produced an updated list of 25 “never events” for use in the NHS in 2012/13. These incidents are considered unacceptable and eminently preventable. The Trust is pleased to report it has had no ‘never events’ during 2011/12. The number of incidents under the type “Implementation of care and ongoing monitoring / review” is significantly higher than other organisations within the cluster, this is largely due to the increase in pressure ulcer reporting. The NPSA state “not all organisations apply the national coding of harm in a consistent way, which can make comparison of harm profiles of organisations difficult”. As part of the final approval process of incidents, the Quality & Risk team ensure that the national coding of harm is used in a correct and consistent way before submission of incidents to the NPSA. We are assured that the figures within the report accurately reflect the actual degree of harm caused to patients as described by the NPSA requirements. The report indicates that we have a higher than average rate of low harm incidents however we have a lower level of moderate harm incidents. We also have a higher level of severe harm incidents, this is mainly due to increased pressure ulcer reporting as all Grade 4 pressure ulcers should be graded as severe harm. 46 Quality Account Norfolk Community Health and Care NHS Trust Learning from incidents During 2011/12 the Quality & Risk team facilitated three learning events for our clinical staff; the first was regarding the prevention and management of pressure ulcers, the second regarding insulin dependent patients and patients requiring INR testing and management and the third was aimed at ‘Enabling people to die in comfort and with dignity’. Attendees heard from expert speakers about how partnership working can deliver the best patients outcomes in end of life care. It was also an opportunity to discuss the new regional ‘Do Not Attempt Cardio-Pulmonary Resuscitation’ form and launch our Trust’s revised Resuscitation Policy. The aim of these events is to share learning and good practice across the Trust with the ultimate aim of improving quality. Four Learning Events are being arranged during 2012 to celebrate ‘best practice’ and to give staff an opportunity to discuss how further improvements can be delivered. Each event will be themed around real-life incidents or issues which have been reported by our staff and patients and will be a chance to share the subsequent learning from these issues. The topic for the next event, due to take place in May 2012 will be regarding the principles of good record keeping and data quality which will also discuss the results of the annual organisation-wide record keeping audit. Learning from Downham Market Health Centre Arguably the most significant quality related event for the Trust during 2011/12 was the publication of the independent report by Collingham Healthcare Education Centre (CHEC) (a consultancy specialising in reviews into GP practice), into the circumstances surrounding the Downham Market Health Centre. This was a nurse led Primary Medical Service (PMS) GP practice. There were four serious incidents requiring investigation (SIRIs) that occurred within the practice in March and July 2010 and January and February 2011. The review concluded that the practice had fallen below the managerial radar of the Trust and therefore the standards of care fell below the excellent services we would aspire to and patients should expect. The review found no direct evidence of patient harm as a result of the failings identified. The review concluded with a number of recommendations for various organisations. The recommendation for NCH&C was that the Trust should reflect as an organisation on the contents of the review, acknowledge its responsibility, put in place robust measures to translate the findings into its organisational culture and to ensure that failures described here can never be repeated. The circumstances and criticisms rightly informed the organisation. Athough the Trust no longer provides these services the Trust Board and teams have reflected extensively and continues to do so on the circumstances and their wider implications. The Trust had already begun to address the concerns identified in the CHEC report and had developed an action plan that was later adapted into a wider project to embed quality systems across the organisation. Key interventions and improvements during the last year include the introduction of monthly Business Unit Performance Meetings. These triangulate in detail quality, financial and performance information for teams and services. A number of staff have moved on and the medical leadership of the Trust has been strengthened with the appointment of a substantive experienced Medical Director with increased hours as well as an experienced associate Medical Director. A closure report detailing all the learning points and actions taken was approved at the public Board meeting in April 2012 and can be found on our website: www.nchandc.co.uk Part 3 3.1 Review of quality performance in 2011/12 3.1.8 Learning from incidents and complaints 47 Each month, staff across community teams and the inpatient units assess their areas against a checklist with weighted scores, which results in an overall RAG-rated score and an indication of what action is required: • Score of 10 or less - Green rating No action required, re-assess area next month • A score between 11 and 15 - Amber rating Undertake full risk assessment and agree action plan for red items within one month. Add to local risk register • A score of 16 or more - Red rating Inform line manager immediately and undertake full risk assessment within one week. Produce action plan for red items within one week The Trust now has six months’ of assessments of the EWTT, and there are some clear recurring themes which are common across many teams and units, and which will need to be addressed at a local level. These include: • Staff not updating clinical records within 24 hours of the contact taking place • No formal feedback obtained from patients during the last 12 months (e.g. questionnaires or surveys) Early Warning Trigger Tool • Vacancy rate higher than 3% (2 points) or 6% (3 points) In September 2011, the Trust introduced an Early Warning Trigger Tool (EWTT) adapted from the NPSA’s tool to be more relevant to a community setting, to act as an early warning system to flag up potential quality and patient safety issues before they occur. The indicators explicitly capture the circumstances of Downham Market such as change in senior clinicians and staffing. The tool is completed by all teams on a monthly basis. During the year the threshold for escalation has been lowered to ensure more services are subject to increased scrutiny. Implementation of the tool should reduce the number of Serious Incidents Requiring Investigation (SIRIs), reduce the risk of an unfavourable CQC report and prevent services going into crisis. The chart on page 48 shows the frequency with which themes were occurring in March 2012. The Trust also reviewed those services that had the potential to share possible characteristics with Downham Market – such as small or geographical isolated. The Board has also approved a Board Assurance and Escalation framework to articulate the process of how concerns and risks flow from the frontline services to the Board. The Board also reviewed its board assurance framework which identifies the high level strategic risks which are linked to the Trust’s obectives In addition, an extensive programme of service visits has been completed by both Executive and Non-Executive Directors and a programme for 2012/13 is being developed. 48 Quality Account Norfolk Community Health and Care NHS Trust Early Warning Trigger Tool Trust-wide frequency of themes (March 2012) Two or more formal complaints in a month No evidence of resolution to recurring themes, eg, complaints, medication errors, falls (excluding pressure ulcers) New Serious Incidents Requiring Investigation (SIRIs) reported in month No evidence of effective multidisciplinary/multi-professional team working Extreme demands on service exceeding capacity to deliver (eg, pandemic, norovirus, outbreak) Unfilled shifts is higher than 6% Cleanliness audits not performed No monthly review of key quality indicators by Business Unit meetings No involvement of Team Leader in Business Unit or Trust meetings Hand hygiene audits not performed Ongoing investigation or disciplinary investigation (including RCAs & infection control RCAs) Department/office appears untidy More than 5% of shifts covered by bank, excess hours and agency Annual appraisals completed within last 12 months below 88% No evidence of adequate clinical supervision in place Mandatory training compliance below 88% Change or absence of a Lead Clinician (within last six months) Overspent against budget New or no line manager in post (within last six months) Sickness and maternity absence rate higher than 4.5% Vacancy rate higher than 3% (2 points) or 6% (3 points) No formal feedback obtained from patients during the last 12 months (eg, questionnaires or surveys) Staff not updating clinical records within 24 hours 0 10 20 30 40 Frequency of theme occuring 50 60 Part 3 3.1 Review of quality performance in 2011/12 3.1.9 Safeguarding Adults and Children 3.1.9 Safeguarding Adults and Children ‘Together we are stronger’ making vulnerable people safer was an event aimed at keeping children and adults in Norfolk safer by more joined up working between our staff and others was held in October 2011. The Department of Health Lead for Safeguarding Adults was one of the keynote speakers at the event which aimed to help the NHS, Police and Council staff share their experiences on some of the complexities of dealing with safeguarding issues and to find effective solutions. Safeguarding Arrangements in NCH&C NCH&C has established Executive and Non-Executive Leads for both Safeguarding Adults and Children as follows: • Director of Operations, Executive Lead for Safeguarding both Adults and Children • Non-Executive Lead for Safeguarding Children • Non-Executive Lead for Safeguarding Adults NCH&C has well established, highly experienced operational Leads for safeguarding children who provide comprehensive training and supervision for staff and also provide expert interventions for reviews, reports and clinical input. The post of Head of Adult Safeguarding and Transfer of Care was recruited to in May 2011 and will facilitate the implementation of the No Secrets guidance within clinical practice, it will also provide assurance to the board through evidence reporting and by supporting staff in the management of Safeguarding issues, training and linking with external partner agencies. Main Issues for Safeguarding Adults Safeguarding Adults is an evolving area of practice; whilst the severe cases of physical abuse is clearly recognised by staff, areas such as neglect, poor care and patient experience are not easily seen as reportable safeguarding concerns. The key issues for Safeguarding Adults in the last year have been: • Lack of recognition of abuse • Not referring patients early enough to the Multiagency Safeguarding Team • Lack of understanding on management of abuse victims • Poor understanding of the Mental Capacity Act, consent and Deprivation of Liberties 49 50 Quality Account Norfolk Community Health and Care NHS Trust Organisational Learning Opportunities There are many ways in which NCH&C intends to raise awareness of important safeguarding issues including, formalising the organisational leadership and direction, disseminating policies and procedures and implementing training and supervision. NCH&C is committed to taking all opportunities to share learning from safeguarding activities and serious cases and is holding a conference for NCH&C staff and our partners to raise awareness and influence practice. Main Issues for Safeguarding Children The current key issues for safeguarding children in the last year: • Nationally and locally there has been a rise in the number of looked-after children (LAC) and a rise in the level of need across the tiers of intervention • In line with changes to national guidance all safeguarding children training has been reviewed and a new training strategy enacted • There have been two multi-agency management reviews • Multiagency Safeguarding children and LAC arrangements in Norfolk have been inspected by the Office for Standards in Education (OFSTED) and the Care Quality Commission (CQC) in June 2011 • The impact of reduction in support services offered by other agencies due to financial constraints The conference entitled “Together we are stronger” took place on 5th October 2011 and 130 delegates, including staff from other organisations, heard how NHS, police, council, and voluntary sector staff can implement even more effective support for vulnerable adults and children. Shared learning from the event is now being taken forward by our Safeguarding Team, which will consider how we can further improve our processes and staff training and work even more closely with our partners. NCH&C safeguarding teams have produced quarterly reports for adults and children to the Trust Board this year. These reports have identified the main issues and NCH&C strategic approach to minimising the associated risks for the organisation. It highlights the significant progress made in strengthening the leadership for both adults and children and the progress made against compliance with national policy and guidelines. It also details some of the priorities for the coming year. Part 3 3.1 Review of quality performance in 2011/12 3.1.10 Effectiveness of care 3.1.10 Effectiveness of care a. National Institute for Health and Clinical Excellence (NICE) NICE have devised a number of audit tools for new guidance which is being released, and this has been positively received by NCH&C clinicians as it provides them with an ‘off the shelf’ resource for sharing new guidance with colleagues. NICE have also produced an online ’pathway tool’ which provides quick and easy access, topic by topic, to the range of guidance from NICE, including quality standards, technology appraisals, clinical and public health guidance and NICE implementation tools. These pathway tools are simple to navigate, and allow staff to explore in increasing detail NICE recommendations and advice, giving clinicians confidence that they are up to date with everything NICE have recommended. ‘Hot topic’ pathways include; Diabetes, Dementia, Hypertension, Chronic Obstructive Pulmonary Disease. Six audits based upon NICE guidance were put into this year’s clinical audit plan: 1. Transient Loss of Consciousness – CG109 2. Female continence (NCH&C audit proposal based on CG97 – Lower Urinary Tract Infections in Men 3. Depression – NICE Clinical Guideline 90 4. Hypertension – NICE Clinical Guildeline127 5. Osteoporosis (re-audit) – NICE Technology Appraisal161 6. Osteoarthritis – NICE Clinical Guideline 59 51 Two other pieces of NICE guidance were flagged as being relevant to NCH&C services, but did not necessarily initiate a clinical audit to be undertaken; 1. PH32 Skin Cancer Prevention – prevention using public information, sun protection, resources and changes to the environment (January 2011), this guidance was used to implement a plan of action by Children’s Services • Undertake a baseline audit to determine level of activity with regard to sun safety messages within Health Visiting and School of Nursing services • Review activities for sun safety within short-break services, Sure Start Children’s Centres and Nurseries • Develop plan for consistent delivery of seasonal safety in the sun messages across all services • Assess if there are any training needs to support implementation of the guidance 2. CG133 Self Harm – Longer Term Management (November 2011), this guidance was flagged as relevant by prison healthcare services, and action planning will follow. 52 Quality Account Norfolk Community Health and Care NHS Trust b. National Clinical audits Links with other organisations Active participation in National Clinical Audits means that we can review NCH&C’s performance against similar community provider trusts, allowing us to benchmark our performance as an organisation. Participation in National audits are also reported in our annual Quality Account which is a public document. These national audits follow individual patient pathways which cross primary and secondary care. To follow is a brief description of how this worked for each of our national audits: Each year the majority of National Audits available on the National Clinical Audit and Patient Outcome Programme (NCAPOP) are ‘acute trust’ focused, but a list of those which are applicable to us as a ‘provider’ trust are circulated to clinicians at the end of each year, to establish interest and clinical commitment to conduct these audits within NCH&C. Due to the size and remit of these large national audits, data is collected over a period of months and then collated and analysed by either a Royal College or a nominated charity before release of the final report in quarter 2 or 3 of the following year. Within 2011/12 NCH&C participated in 3 National Audits, namely; National (Adult) Diabetes Audit, Epilepsy12 (this was year 3 of 3 of this children’s National audit), and the Parkinson’s National Audit which was run by ‘Parkinson’s UK’. Reports from all three of these national audits should be made available in Q2/3 of 2012/13 Parkinson’s Audit – our Specialist Nurses provided ‘community data’ which was used to track the progress of patients diagnosed with Parkinson’s Disease following discharge from the Norfolk and Norwich University Hospital NHS Foundation Trust hospital. National Epilepsy12 (Children’s) audit – NCH&C worked with the Paediatric specialists in the Norfolk and Norwich University Hospital NHS Foundation Trust hospital in order to follow patient pathways and measure clinical care received in both the Acute and community environment against best practice standards produced by the Royal College of Paediatrics and Child Health (RCPCH). National Diabetes Audit (Adults) – our Diabetes Specialist Nurse team in the west of the county worked closely with GP consortia in order to record data against adult Diabetic patients for the National Diabetes Audit (Adults), and for the purposes of this audit this information was used to demonstrate the effectiveness of individual patient journeys through primary to community care. Part 3 3.1 Review of quality performance in 2011/12 3.1.10 Effectiveness of care 53 c. Local Clinical audit project statistics for 2011/12 The table below demonstrates the breakdown of projects registered by type between 1st April 2011 and 31st March 2012. Type of project Examples Number % of total clinical audits Priority 1 Internal ‘must do’ audits CQuIN audits, Schedule 16 (Commissioning Audits), NICE Technology Appraisals (TAs). 22 33% Priority 2 ‘External ‘must do’ audits National Clinical Audits, National Service Framework Audits 8 12% Priority 3 Operational business unit priority audits Service specific audits, baseline audits for business case proposals etc 11 16% Priority 4 Clinical interest audits Clinical speciality led audits, NICE (other than TAs) 26 39% 67 100% Total 2011/12 saw a number of ‘service evaluation’ style audits using ‘levels of assurance’ which are taken from the 2012 NCH&C clinical audit template. They recognise ‘high’ as over 85% compliance, ‘moderate’ as between 60% - 84% compliance, and ‘low’ as below 59% compliance against clinical audit standards. • 33% gave high assurance, including hand hygiene, essential steps and the community hospitals antibiotics audit • 53% provided moderate assurance and these included: safeguarding children’s supervision and reducing harm from omitted and delayed medicines 14% • Those audits providing low assurance were generally due to small or insufficient sample sizes being audited 33% High Moderate Low 53% Of the 67 proposed audits, 33 were completed during 2011/12: 54 Quality Account Norfolk Community Health and Care NHS Trust A summary of these are as follows: d. Research & Development • “Safeguarding Children – Supervisors Audit”, which provided moderate (73%) assurance, that Safeguarding Supervisors working within Children’s Services were receiving adequate support and training in their professional roles (June 2011). NCH&C patients with venous leg ulcers take part in biggest ever leg ulcer study • “Reduction of Falls/preventing falls and reducing harm from falls”, which provided high (92%) assurance that in-patient units within community hospitals were completing a falls assessment within 48 hours of admission, this service evaluation was a CQUIN target, and was achieved. • “Reducing the harm from omitted and delayed medicines in hospital. A re-audit of NCH&C inpatient units, December 2011”, provided moderate assurance that teams and individuals were adhering to National Patient Safety Agency (NPSA) guidance to reduce occurrences of missed and delayed medicines given in our community in-patient sites. • The Infection Control Team conduct monthly ‘hand hygiene’ audits at localities and in 2011/12 results across the trust provided high assurance (99%) Patients with venous leg ulcers under the care of NCH&C’s community nursing teams in Norwich, Long Stratton, Diss and Dereham have been involved in a piece of research that is looking at two different treatments used to treat this debilitating, long-term condition. The study is the largest ever of its kind in the UK, involving more than 30 Trusts. It will provide the latest evidence on which treatment is most effective, ie, has a faster healing time, by comparing four-layer bandaging with compression hosiery (stockings). The results, (due out in autumn 2012) will enable community nurses to offer the best treatments to patients, in line with this new evidence. As a result of this it is hoped that the length of time patients need to be treated for leg ulcers in the future will be significantly reduced. Part 3 3.1 Review of quality performance in 2011/12 3.1.10 Effectiveness of care 55 Norfolk Sure Start Centres involved in national programme of research Important research involving users of NCH&C’s Stop Smoking service Several Sure Start Children’s Centres run by NCH&C are involved in a five-year national research programme which aims to improve understanding of children’s accidents and effect a change in behaviour with parents and families around child safety. The project looks at the following areas: A study looking at the effectiveness and costeffectiveness of a set of eight booklets (called Forever Free) designed for the prevention of smoking relapse in people who have stopped smoking for at least four weeks was launched in July 2011 at NCH&C. This large study (it requires 1,400 people to take part) involves Stop Smoking Advisors who will recruit four-week quitters over a period of 21 months, with telephone follow-ups at three and 12 months post quit. Study participants are randomly allocated to receiving either the intervention, the self-help booklets, or to usual care, the current NHS leaflet. To date, 388 people have been recruited. • house fires • falls • scalds • poisoning As part of the research, an injury prevention briefing (IPB) on specific aspects of injuries in the home to preschool children is being developed that will be tested in a group of children’s centres, including Norwich. The briefing will be sent to centres in four study areas: Nottingham, Bristol, Newcastle and Norwich. Some will also receive support from the project team to help them take forward key messages in the IPB. When the 12-month study has been completed the study team will roll-out a revised briefing outside the study areas. The research will show whether, as a result of Centre staff using the briefing, there are changes in some families’ home safety behaviour, and ultimately this should result in a reduction in children’s injuries and hospital admissions. The study hopes to show that people receiving the new booklets ‘stay quit’ for much longer than those who do not. The booklets may prove to be a useful tool advisors can use to help people who suffer smoking relapse within six months of the end of NHS Stop Smoking treatment to stay smoke-free. Research study offers support for recovering stroke patients who have communication difficulties A study examining the effectiveness of specialist skills for hospital staff in communicating with recovering stroke patients with aphasia (a communication disorder which affects speaking and understanding), has been running for just over a year at NCH&C’s stroke unit. The first phase of the study has provided staff training in ‘supported communication’ techniques. The second phase, beginning in late 2012, will involve patients in Norfolk with moderate to severe aphasia after a first stroke who will receive care from staff trained in ‘supported communication’ and compare their health outcomes with a group of patients in Cambridge who will receive normal care from their local stroke rehabilitation therapy team. The research findings will determine how effective this new technique has been from both the staff and patient perspective. It is hoped that the research will lead to recommendations for a staff training protocol for wider implementation across the NHS. 56 Quality Account Norfolk Community Health and Care NHS Trust 3.2 Explanation of who has been involved and engaged with • LINk and Public Involvement at Trust Board meetings and other committees, including Quality & Risk Assurance Committee, Patient Experience Steering Group and PEAT inspections • Development of the Integrated Business Plan (IBP) by Board members and clinical reference group • Development of the Annual Plan by Executive Directors, Assistant Directors and clinicians • Quality & Risk Assurance Committee provides assurance to the Board and has a LINk representative in attendance • Third party commentary requested from Norfolk LINk, NCC Health Overview and Scrutiny Committee and NHS Norfolk & Waveney Comments from Norfolk Health Overview and Scrutiny Committee The Norfolk Health Overview and Scrutiny Committee has decided not to comment on any of the Norfolk provider Trusts' Quality Accounts for 2011/12 and would like to stress that this should in no way be taken as a negative comment. The Committee has taken the view that it is appropriate for Norfolk's Local Involvement Network to consider the Quality Accounts and comment accordingly. Comments from Norfolk LINk Norfolk LINk welcomes the Community Health and Care Trust’s approach to improving services as set out in the Quality Account. We agree with the priorities identified for 2012/13. We hope that staffing levels are commensurate with the activity needed to achieve the Quality Goals. The Trust has a very good approach to stakeholder involvement. This is based on our experience of being involved in meetings where service issues are discussed in-depth; our ability to obtain information easily from the Trust; and our involvement in ‘Patient Stories’. We know that the Trust is also actively engaging with other stakeholders such as Age UK Norfolk to gather the views of patients from diverse backgrounds. We are pleased that the Trust is looking towards indepth surveys for qualitative information about the patient experience. Although it was only in 2012 that the ‘Patient Stories’ initiative got off the ground, we can confirm that this is now well-underway with LINk volunteers being trained to record patient stories. However Norfolk LINk is not convinced that “Net Promoter” is a suitably valid tool for accurate measurement of the patient experience where respondent numbers are less than 60 per cent. Regarding patient safety issues, the Trust is yet to act on two safety issues that we raised with the Stroke Rehabilitation Unit after a visit in November 2011. These were around the absence of emergency/help pull cords inside toilets and showers; and clear access to the fire evacuation area. We are pleased to see that the Account has several examples of the outstanding staff working within the Trust and can confirm that several initiatives are in progress, eg, improving care for older people with dementia. Part 3 3.2 Explanation of who has been involved and engaged with Comments from NHS Norfolk and Waveney Statement of Information Verification within the Quality Account submitted to NHS Norfolk by Norfolk Community Health & Care NHS Trust June 2012 NHS Norfolk and Waveney as lead commissioners for Norfolk Community Health & Care NHS Trust are pleased to support the Trust in its publication of the 2011/12 Quality Account. We have reviewed the mandatory data elements required within this account and can confirm that those included are consistent with that known to NHSN&W. The report presents detailed and comprehensive information relating to the quality and safety of care delivered within the prioritised areas identified by the Trust. The Quality Goals for 2012/13 are relevant and are substantiated by involvement with the clinical quality and patient safety agenda via the Commissioning for Quality & Innovation payment framework (CQuIN) We commend staff for their work to improve outcomes within these areas and we look forward to the inclusion of an update on achievements in these areas in next year’s Quality Account. 57 NHSN&W have appreciated the continued support of the clinical quality review meetings which are vital in assuring the local population that services contracted from the Trust are safe and of good quality. They enable discussions to take place concerning new initiatives and current thinking and practice. They also facilitate challenges regarding current performance. With the elimination of avoidable Grade 2, 3 & 4 pressure ulcers being an ambition for NHS Midlands and East, it is clear that through the implementation of data collection via the NHS Safety Thermometer and the Trust’s Pressure Ulcer Clinical Improvement Programme that the Trust is supportive of this ambition. The Trust acknowledges the learning that arose from the Downham Market Health Centre enquiry and the findings of the independent report commissioned by the SHA. The Trust outlines where the learning has led to significant changes in organisational processes in order to assure that the failures described will not be repeated. This has been a year in which the Trust has demonstrated improvements in many areas and we look forward to working alongside them in supporting their quality initiatives in the coming year. Andrew Morgan Chief Executive Officer NHS Norfolk & Waveney Head Office: Elliot House, 130 Ber Street, Norwich NR1 3FR Online: www.norfolkcommunityhealthandcare.nhs.uk Telephone: 01603 697300