Quality Account 2012 1
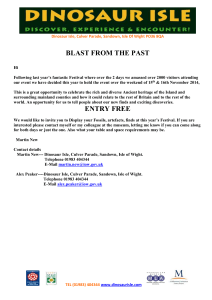
advertisement
Quality Account 2012 Version 1.0 22 May 2012 1 Contents 1 2 2.1.1 2.1.2 2.1.3 2.1.4 2.1.5 2.1.6 2.1.7 2.1.8 2.1.9 2.2 2.2.1 2.2.2 2.2.3 2.2.4 2.2.5 2.2.6 2.2.7 2.2.8 3 3.1.1 3.1.2 3.1.3 3.1.4 3.1.5 3.1.6 3.1.7 3.1.8 3.1.9 3.1.10 3.1.11 3.1.12 3.1.13 3.2 3.3 3.4 3.5 Foreword Part 1: Chief Executive’s Statement on Quality Part 2: Priorities for Improvement for 2011/12 and Development of the Quality Account Key Priorities for Improvement 2012/13 Priority 1: Improving Mortality Rates Priority 2: Prevention and Management of Pressure Ulcers Priority 3: Improving Access to Level 1 and Level 2 Child and Adolescent Mental Health Services (CAMHS) Priority 4: Improving Nutrition and Meal Times Priority 5: Improving the Experience of Children and Young People Presenting in Psychiatric and Emotional Crisis Priority 6: Learning Disabilities and Dementia Priority 7: Improving Record Keeping Priority 8: Reduction in 28 Day Readmissions in Mental Health Statements of assurance from the Board Review of services Dashboards and scorecards Patient safety walkrounds Participation in clinical audits Research Goals agreed with commissioners What others say about the provider Statements from the Care Quality Commission Data Quality Part 3: Review of Quality Performance 2010/11 Identification and response to the deteriorating patient and hospital at night Prevention of Venous Thromboembolism Prevention of pressure ulceration Reduction in 28 day readmission rates in mental health Improving the pathway for clients with alcohol addiction Improving stroke care Community, outpatient and home antibiotic therapy Improving the experience of children and young people in psychiatric and emotional crisis Other Performance Information Healthcare associated infections (HCAI) Complaints and compliments Workforce Baseline Equality Delivery System Self Assessment Statements provided by Commissioning PCT, LINks; OCS and Patient Council Statement of Directors’ Responsibility Changes made to the final version of the Quality Account How to provide feedback on the account 3 4 6 6 7 7 9 10 11 12 16 16 18 18 18 18 19 23 23 25 25 26 27 27 30 31 33 34 36 38 41 43 44 46 46 49 50 53 54 54 Appendix 1: Stakeholders engaged in the development of the Quality Account 2 FOREWORD Welcome to the third and final Quality Account to be published by NHS Isle of Wight. On the 1st April 2012 provider services moved into the newly created Isle of Wight NHS Trust. The Quality Account this year sets out the achievements and challenges for quality and quality improvement within NHS Isle of Wight and outlines the ongoing and new quality priorities for the Isle of Wight NHS Trust. The Quality Account for publication in 2013 will be produced by the new Isle of Wight NHS Trust In the Quality Account this year you will find details of the ongoing work to reduce the incidence of pressure ulcers both at St Mary’s Hospital and for patients in the community in the care of our services such as the District Nursing Service and the Intermediate Care Team. Pressure ulcers are considered to be an indicator of the quality of nursing care being provided and since establishing our zero tolerance approach during 2011/12, the numbers have been steadily reducing, we still have more to do but we are heading in the right direction. A key area of focus over the last two years has been reducing the number of incidents when a patient’s condition deteriorates so that they have a cardiac arrest whilst in one of our wards. The establishment of the Critical Care Outreach Team means that the number of cardiac arrests occurring in the main inpatient wards has reduced from around 10 a month to 1 or 2 a month. This is a significant achievement and supports our work to improve the fundamental standards of patient care in all settings. The Quality Account is not a full reflection of all the high quality care that is being provided by healthcare professionals on the Isle of Wight, it is just a snapshot of key areas. Other successes not detailed in the main body of the document include the continued low caesarean section rate within the maternity service and the recent success of Prison Healthcare Services with their nationally recognised condom scheme. It is impossible to ensure that all services are covered within this publication; however it should be recognised there is a huge amount of high quality care being provided on a day to day basis across all services. During 2012/13 we are strengthening our message about quality care with the adoption of the guiding principle, Quality care for everyone, every time this principle is at the core of everything we do and we will be working with staff in all settings to ensure this is the common shared goal and that the people of the Isle of Wight will want their healthcare provided by the Isle of Wight NHS Trust Carol Alstrom Chief Nurse and Director of Infection Prevention and Control 3 PART 1 Chief Executive’s Statement on Quality This Quality Account outlines the successes and challenges in quality improvement across the services provided by the integrated healthcare services provided on the Island. The NHS on the Isle of Wight is in a significant period of change, with the creation of the new Isle of Wight NHS Trust from 1st April 2012 and the transfer of provider services from the Isle of Wight Primary Care Trust into the new organisation. At the same time, changes are continuing in relation to commissioning and public health which will not be complete until 2013. Amongst all this change providing high quality patient care remains the top priority. The Isle of Wight NHS Trust provides the Isle of Wight’s acute, ambulance, community, mental health and prison health services. Our vision is to be an excellent and trusted provider of integrated patient focussed services that are globally admired. Our guiding principle as a Trust is that we seek to provide quality care for everyone, every time. Our vision is underpinned by five strategic objectives based around the themes of quality, innovation, productivity, prevention and reform. Our guiding principle, vision and strategic objectives for the new Isle of Wight NHS Trust are summarised as follows: During 2011/12 we have seen significant achievements including a further reduction in the number of inpatient cardiac arrests, the incidence of hospital acquired Clostridium difficile 4 cases has dropped to record lows, and the number of pressure ulcers continues to reduce moving us closer to our zero tolerance objective. Mortality figures released in the autumn of 2011 indicated that there was a potential problem at St Mary’s but extensive work has been undertaken including reviews of clinical care and this has highlighted improvements in practice, and I am pleased to report that mortality figures are improving steadily. During 2012/13 we will keep the focus on pressure ulcers, considered to be a key indicator of the standard of basic nursing care alongside a new priority relating to improving nutrition and meal times, continuing the work on mortality rates, enhancing care for people with learning disabilities and dementia, improving record keeping and supporting the transfer to an electronic patient record, and continuing to focus on reducing readmissions in mental health. Other areas of focus will include child and adolescent mental health and supporting children in psychiatric and emotional crisis. The Quality Account has been developed in partnership with clinical staff from across health services on the Isle of Wight, and has also included input from patient representatives with our Patient’s council having a clear view on the objectives for the coming year. We confirm that to the best of my knowledge the information contained within this 2011/12 Quality Account is accurate and we hope that you will find it an interesting read. Kevin Flynn Debbie Fleming Chief Executive Isle of Wight NHS Trust Chief Executive Isle of Wight NHS Primary Care Trust SHIP Cluster 5 PART 2 2.1 Priorities for Improvement 2.1.1 Key Priorities for Action 2012/13 The Isle of Wight NHS Trust Board in consultation with key stakeholders, including Patients Council; LINks and staff groups has identified eight overarching priorities for quality improvement during 2012/13. These priorities are derived from the performance over the past year against quality and safety indicators; national and regional priorities and are outlined here in more detail. The priorities include aspects from across the organisations to reflect the complexity of the Isle of Wight NHS Trust and include aspects of patient safety, clinical effectiveness and patient experience. Performance against all priorities will be reported to the Board by the monthly performance report (quality section) A wide range of stakeholder consultation has been undertaken prior to the development of the 2011/12 Quality Account, to support the identification of priorities for the coming year and to ensure key elements of quality are included. Service users have been invited to contribute to the decision making process to agree the priority areas for improvement for 2012/13. Invitations to comment have also been posted on the organisations website and advertised in the local media. The priorities were formulated into a long list and following consultation this list was revised and prioritised on the basis of feedback to create the final eight priorities. Extensive staff consultation has taken place on the content of the quality account, both clinical and non-clinical via a range of meetings and other methods including an invite to contribute via the organisation’s staff e-bulletin. A committed group of staff have been involved in regular meetings about the quality account, specifically designed to support the production process, this group has been led by the Chief Nurse and supported by a wide range of staff. A full list of those involved can be found in Appendix 1 6 PATIENT SAFETY 2.1.2 PRIORITY 1: IMPROVING MORTALITY RATES The organisation was identified in the autumn of 2011 to have a Hospital Standardised Mortality Ratio (HSMR) of 124 and a Standardised Hospital Mortality Index (SHMI) of 118.9 for the year 2010/11, the second worst in the country. Work had already commenced 12 months earlier on improving coding practice and since the autumn of 2011 the mortality action plan has been expanded to cover clinical practice, coding practice and other aspects of service provision which may impact on the mortality rates. The latest Dr Foster data puts the HMSR for April 2011 – January 2012 at 111 (rebased figure), and the SHMI for June 2010 – June 2011 at 116, showing an improvement on the previous position, however we are not satisfied with that level and are continuing to drive the action plan to reduce this figure even further. The action plan now includes the introduction of care bundles for a range of conditions including sepsis and hospital acquired pneumonia, will be building on the work of the critical care outreach team in supporting patients who are at risk of deterioration to prevent that occurring and further work to strengthen best practice in clinical coding. During 2012/13 the focus will remain on improving mortality rates, focusing specifically on the care of emergency elderly patients and improving the care and support they receive. It is anticipated that during 2012/13 the HMSR will continue to reduce to below 110 and the SHMI will continue to see a downward trend. Monitoring and Measurement of Progress / Key Performance Indicators. Measure SHMI HSMR Source of Data NHS Information Centre Dr Foster analysis tools . Frequency Data collected of Collection and Reported by Quarterly Medical Director Monthly Chief Nurse 2.1.3 PRIORITY 2: PREVENTION AND MANAGEMENT OF PRESSURE ULCERS Pressure ulcers remain a key indicator of the quality of nursing care provided both in hospital settings and in the community. During 2012/13 further work will be undertaken to embed the zero tolerance approach to healthcare acquired pressure ulcers particularly those developing in patients whilst they are in hospital or in the care of the district nursing service. It is a key priority area for the Isle of Wight NHS Trust in ensuring quality care for everyone, every time. Pressure ulcers (also commonly referred to as bed sores) cause distress and pain to patients when they occur. The organisation has continued its strong commitment and focus over the last three years in reducing the occurrence of these ulcers. The key indicators this year differ slightly from those included in the previous two years Quality Accounts, as they focus on the number of patients who are harmed by the occurrence of these ulcers, rather than regarding each ulcer as an individual event. Ongoing work in this area focuses on: • Embedding the Zero Tolerance to pressure ulcers across all sectors • Continuing to implement key actions from the Organisational Action Plan for Pressure Ulcers, where the focus is now on not just supporting the process of care 7 • • for patients, but empowering nurses to lead in improving this aspect of patient safety. The recognition of the importance of the Tissue Viability link role as a key function in each clinical area to support the quality of pressure area care across the Organisation. Continuing to standardise the documentation relating to Intentional Rounding and Patient Safety Checks to further drive improvements in patient care at the bedside. The key standards set out below will be subject to audit. The audit will highlight over the course of the year the further improvements made as a result of the initiatives outlined above. Our key outcome measures will be a reduction in the harm caused to patients by pressure ulcers. The measurements proposed for this year are in line with the NHS Outcomes Frameworks for Patient Safety: Monitoring and Measurement of Progress / Key Performance Indicators. Measure Percentage of patients admitted who develop a pressure ulcer grade 2 and above Prevalence of pressure ulcers grade 2 and above, in the hospital setting on a month by month basis Reduce the number of patients with grade 3 and 4 pressure ulcers by 25% based on 2011/12 baseline Source of Data Datix incident monitoring system NHS Safety Thermometer Datix incident monitoring system Frequency Data collected of Collection and Reported by Monthly Nutrition and Tissue Viability Service Monthly Collected by ward teams/collated by Nutrition and Tissue Viability Service Monthly Nutrition and Tissue Viability Service 8 PATIENT EXPERIENCE 2.1.4 PRIORITY 3: IMPROVING ACCESS TO LEVEL 1 AND LEVEL 2 CHILD AND ADOLESCENT MENTAL HEALTH SERVICES (CAMHS) The National Workforce mapping exercise identified that a Community Child and Adolescent Mental Health Service (CAMHS) model would provide a more effective and broader based service to the Island community, and commissioning supported the redesign of the service alongside national benchmarking. A full service specification and quality framework are in place to support the achievement of the quality indicators identified in the national guidance. Lack of appropriate targeted services in the tiers below the Specialist Child and Adolescent Mental Health Services led to inappropriate referrals into the specialist part of the service which prevented timely access to appropriate services for children and families on the Island. In order to improve access to the service including encompass new ways of working by ensuring people with the right skills are in the right place at the right time, maintaining the You’re Welcome status, and being part of national data collection and benchmarking exercises, it was necessary to restructure the administrative team to ensure that we are able to support all clinical staff within the service to meet these high standards. The newly reconfigured Community CAMHS service provides access to primary care mental health workers as well as specialist services to promote timely response to assessment and treatment at the appropriate level. Staff are currently implementing a consultative approach together with colleagues in education, social care and children’s health. The new service specification is supported by a comprehensive quality framework drawn from National benchmarking and the You’re Welcome Standards. Monitoring of these standards are through local and national structures such as the performance information team and You’re Welcome Monitoring. The service recently achieved an award from “Check it Out” which is a young people’s service user led group who undertake mystery shopper type monitoring. Monitoring and Measurement of Progress / Key Performance Indicators. Measure 100% of patients seen within 18 weeks from referral to treatment Source of Data PAS system Frequency of collection Quarterly Data collected and reported by Collected by Office Manager and reported by Performance Information Department The 18 weeks referral to treatment measure above is applicable to all patients referred to medical practitioners and other clinicians. This will be monitored through the Patient Administration System and reported for patients referred in each quarter. The report will be available fourteen to sixteen weeks after the end of the quarter; therefore the quarter 1 data will be available in late October 2012. 9 2.1.5 PRIORITY 4: IMPROVING NUTRITION AND MEAL TIMES The Trust is involved in a project called ‘Safe and Productive care of Older People’ part of a national pilot with the NHS Institute for Innovation and Improvement. As part of the multi-professional project, the organisation is focusing on improving and maintaining the nutritional status of patients on Newchurch Ward. This will be used to test some assumptions about food and nutrition and to devise strategies for improvement. There is national concern that patients in hospital can become malnourished. Reports from Age Concern and the Care Quality Commission highlight this as a patient safety risk. It is a key priority area for the Isle of Wight NHS Trust in ensuring quality care for everyone, every time. There is a national screening tool in use to assess nutritional status of patients. This is known as the MUST tool (Malnutrition Universal Screening Tool) and is used routinely when patients are admitted and repeated according to the level of risk associated with each patient. Treatment and reassessment or referral to dieticians may result from a score which indicates that the patient has or is at risk of malnutrition. Weight and Body mass index are recorded as part of the MUST scoring. The Safe and Productive Care of Older People project is examining nutrition on one ward in the first instance. Measures will be used to examine compliance with MUST scoring, weight lost or gained during in-patient episodes and data from the Datix incident reporting system, patient surveys and complaints. Photographs of meals at lunchtime will also be taken for analysis by staff. Protected mealtimes will be used to enhance patient safety and experience at mealtimes following data collection and analysis. The learning from the project on Newchurch Ward will be shared across the organisation and rolled out to all relevant areas. The measures that follow will be used to plan, undertake improvements, analyse the results and make further changes as necessary. Monitoring and Measurement of Progress / Key Performance Indicators. Measure Compliance with recording MUST, Effective care planning and referral as necessary can be seen in nursing notes and records Weight of patients on admission and at discharge to include BMI Food and fluid experience of patients Source of data Patient notes and nursing records including MUST scoring sheet. Patient records and nursing notes 1. Patient and relative survey 2. Datix and compliments and complaints data 3. Photographic data Frequency of collection Monthly 10 sets of notes Data collected and Reported by Modern Matron – CCU / Newchurch Each admission and discharge 1. Monthly survey 2. Data from last 12 months 3. At beginning and end of the project Ward Sister Newchurch Ward 1. Ward Sister Newchurch Ward 2. Project Administrator 3. Nutritional and Tissue Viability Nurse Specialist 10 2.1.6 PRIORITY 5: IMPROVING THE EXPERIENCE OF CHILDREN AND YOUNG PEOPLE PRESENTING IN PSYCHIATRIC AND EMOTIONAL CRISIS The changes in the Mental Health Act 2007 section 31 ensured the rights of children and young people to be accommodated, in hospital, in an age appropriate environment and appropriate measures taken to address their needs in accordance with the Children’s Act (1989 and 2004), Human Rights Act (1998), the Mental Capacity Act (2005), Family Law Reform Act (1969) as well as the United Nations Convention on the Rights of the Child. The Act prescribes that young people should have appropriate physical facilities, staff with the right training, skills and knowledge to understand and address their specific needs. An upgrade to one of the existing inpatient beds on the small Paediatric Unit commenced on 27th February 2012 and is scheduled to be completed by the end of April 2012. The upgrade will provide: • • • • A shower room with toilet in the ‘adolescent area’ of the main ward. A bedroom and lounge area equipped with anti-ligature fixtures and fittings. Doors to the corridor which are two-way opening to prevent ‘barricading’, but able to be closed to provide exclusive use of the area. Separate external access, to avoid challenging behaviour being witnessed by other patients, when children/young people arrive under a section 136 of the Mental Health Act or in a heightened state of emotion. This will include a ramp for wheelchair access, and will provide an additional fire escape for the whole ward. Whilst providing this facility, the multi-purpose use of this room can be retained, and benefit the health and mental well-being of all child or adolescent patients, especially those with chronic life-limiting disease requiring hospital treatment. Benefits to patient and carer groups • Children and young people can be assessed by appropriately trained professionals. • This area can be used for children and adolescents who are challenging in their behaviour away from the ward thus preserving their dignity in a safe environment; it may also be used for a time limited period for children and adolescents who are awaiting a specialist mainland placement for a maximum period of 24 hours. • The separate access created as part of this work, this will improve the privacy and dignity of those children brought to the ward under section 136 of the Mental Health Act. • For other children and families on the ward, it will improve their safety and avoid any emotional distress possibly caused by observing children or adolescents with challenging behaviours. Benefits to staff • Staff can care for children and young people in a safer environment and can call on colleagues to assist if required • Improved existing fire exit at end of ward which will be wheelchair and bed friendly. • Staff will require continued training to manage challenging behaviour. During 2012/13 the Isle of Wight NHS Trust will continue to monitor this key indicator ensuring children and young people are cared for in age appropriate environments 11 Monitoring and Measurement of Progress / Key Performance Indicators. Measure No children aged 16 or under will be admitted to an adult mental health ward The number of children admitted to other places (including Mainland Specialist Mental Health Units/Children’s Ward) Source of Data Frequency of Collection Data collected and Reported by Exception Reporting Form / DATIX System Monthly Team Leader CAMHS CAMHS Patient Database Monthly Team Leader CAMHS 2.1.7 PRIORITY 6: LEARING DISABILITIES AND DEMENTIA A: Improving the experience of people with a learning disability using St Mary’s Hospital Anyone of us may experience anxiety and stress when coming into hospital for treatment either as an inpatient or an outpatient. If you have a learning disability this anxiety is often heightened because of communication difficulties and unfamiliar surroundings and people. The needs of people with a learning disability can often be compounded by additional conditions such as epilepsy or mental health issues. Mencap the leading learning disability charity produced a report titled Death by Indifference in 2007 which was followed by the Michael Inquiry published by the Department of Health in 2008 highlighting the difficulties people with learning disabilities can often have in accessing a range of general health services. The Parliamentary and Health Ombudsman’s ‘Six Lives’ Report published in 2009 required all health services to make reasonable adjustments to improve the care and treatment of people with a learning disability In order to support people with a learning disability with outpatient appointments and admissions the Community Learning Disability Nurses based at the Arthur Webster Clinic in Shanklin work with individuals ,families and services to ensure adjustments are made to account of their individual needs. In addition to this there is now a Learning Disability Liaison Nurse based at St Mary’s Hospital to ensure that each department understands the needs of people with a learning disability. They are able to help with planned and unplanned admissions to the hospital, including training staff; providing advice to reduce behaviours often generated through the anxiety of an admission. Additional support is often required with nutrition and hydration, pain relief, communication and support to carers. The Liaison Nurse also has a key role in discharge planning to avoid re admissions. Working on conjunction with the ward or departmental team the Liaison Nurse and Community Learning Disability Nurses can ensure that national experiences of poor care for this vulnerable group do not happen locally. During 2012/13 the Isle of Wight NHS Trust will review the support provided to in-patients with a learning disability to ensure their care is appropriate and necessary adjustments are made to support the delivery of effective care. Monitoring appropriate medicines management relating to psychotropic and anti-epileptic medication for people with learning disabilities admitted to St Mary’s Hospital will also be undertaken to ensure this is in line with best practice guidance. 12 Monitoring and Measurement of Progress / Key Performance Indicators. Measure All in-patients with a learning disability who require adjustments in their care will receive support from the Liaison Nurse or CLDN. Survey of the continued use of psychotropic and anti epileptic medication for patients with a learning disability coming into hospital Source of data Liaison Nurse service Liaison Nurse and Community Learning disability nurses Frequency of collection Quarterly Data collected and reported by Learning Disability Liaison Nurse Quarterly Learning Disability Liaison Nurse B: Enhancing Care Provision to Patients with Cognitive Impairment / Sensory Impairment / Communication Difficulties A national review by the Alzheimer’s Society of aspects of care prioritised by older people and carers emphasised the importance of care which is person centred, in that the person with dementia is treated as an individual and takes into account their perspective within a supportive environment. The observations for this audit were carried out in each case by staff from the hospitals in which participating wards were situated. The overall finding from ward observations is that care and communication is generally reactive and based on an organisationally set, task-driven routine rather than being person-focused, flexible and proactive. • • • • • On most hospital wards there is little evidence of a person-centred ward approach or “culture”, or that the care received by patients is generally person-centred The content of the staff/patient encounter is mainly task related and delivered in a largely impersonal manner. There are periods of care-based activity interspersed with inactivity, leading to lack of attention, lack of stimulation and boredom for patients. The environment is often impersonal and not dementia friendly, with excess noise at times, and a lack of orienting cues, dementia aids or areas for socialising. There is inconsistency in the quality of communication. People with dementia experienced differences in the approach of individual staff members, or between groups of staff (such as pharmacy/housekeeping) or both. In some cases, some elements of care delivery were positive (explanations and information were consistently given to patients) while other elements of care delivery in the same ward were clearly not (staff not knowing the patient as a person, for example, using the name by which the patient preferred to be addressed, or allowing time to communicate). “Pockets” of positive, person-centred care were found in the practice of individual staff members, or as elements of ward practice. Only a handful of wards reported ward practice which was person-centred more often than not. It is apparent that there is considerable scope to develop and enhance person-centred care for people with dementia. The aim should be to initiate a progression from the currently dominant culture of task based care to one in which there is an integral focus on 13 the person. Taking a proactive approach and having a timely and attentive response to people with dementia also means that their discharge is likely to be more appropriately facilitated, impacting on costs, as identified by the Alzheimer’s Society (National Audit of Dementia Care in General Hospitals 2011) The Isle of Wight NHS Trust is committed to improving the care of people with dementia, particularly as many as 1 in every 4 of our patients could be suffering from some degree of dementia. To support the Alzheimer’s Society document “This is Me” (a passport type document supporting person centred care) will be completed by ward staff in conjunction with patients and their relatives whenever possible. The completed document will be available at the end of the bed of every patient who has a cognitive impairment and/or sensory impairment or communication difficulties. This document will inform and aid staff to provide person centred care relevant to each individual. Monitoring and Measurement of Progress / Key Performance Indicators Data collected Frequency Measure Source of Data of Collection and Reported by Increase in the proportion of people with a cognitive / sensory/ or communication Audits undertaken by impairment who have the Memory Service Liaison Quarterly Memory Service “This is Me” document Team completed and available at the end of their beds. Improvement in the quality Audits undertaken by of information recorded Memory Service Liaison Quarterly Memory Service within the “This is me” Team document. C: Raising Awareness and Improving the Quality of Care for People with Dementia In the UK there are approximately 750,000 people known to be living with dementia. This number is expected to almost double within 30 years. Up to 70% of hospital beds are occupied by older people and it has been suggested by the Department of Health in 2011 that up to half of these may be people with a cognitive impairment including dementia. The identification and management of people with cognitive impairment in hospital is vital to improving the experience and outcomes for patients. This includes the importance of being able to meet nutritional and physical care needs as well as the recognition and understanding of needs relating to communication and emotional support. People with dementia are at heightened risk of developing symptoms such as agitation, distress, or behaviour can become aggressive when in hospital. (National Audit of Dementia 2011). A lack of appropriate assessment during admission indicates that care needs can be overlooked and it is important to be sure that people with dementia are managed with awareness and understanding so that attention to all aspects of care are met well within the hospital setting. 1000 Lives plus – below are a list of interventions to improve care for people with dementia on general hospital wards • Identify on day of admission if person already has diagnosis of dementia. If so, liaise immediately regarding care needs in relation to dementia (including medication) with family and professional carers, and commence discharge planning. 14 • • • • • • • • • Where there is no previous history of dementia, check history with family/other carers or people offering support Assess for delirium and ensure appropriate treatment Seek advice from liaison service for older adults with mental health problems, especially where additional needs identified from risk assessment in relation to challenging behaviour Assess environmental needs – e.g. safety, stimulation, need for single room Assess needs for assistance and maintaining skills, e.g. with meals, toileting, self care, and build into care plan accordingly Review all psychotropic medication on admission Assess for capacity for major decisions and where the person lacks capacity, follow the best interests process Carers to be involved in care-planning for the person in relation to discharge planning If the patient has a diagnosis of dementia when being discharged: all carers offered carers assessment During 2012/13 all patients of 75 years and over screened and where appropriate referred on to the Memory Service for specialist assessment and support Monitoring and Measurement of Progress / Key Performance Indicators. Data Collected Frequency Measure Source of Data of Collection and Reported by 90% of all patients aged 75 and over admitted to wards will follow the Patient Administration Monthly TBC dementia pathway and will System (PAS) be screened within 72 hours of admission 90% of all patients aged 75 and over, who have been screened as at risk of dementia will require a risk assessment using the agreed hospital risk assessment tool 90% of all patients aged 75 and over, who screened positively for dementia and had a risk assessment completed, who are referred for specialist assessment by the Memory Service team either on the ward or as an outpatient within the community Patient Administration System (PAS) Monthly TBC Patient Administration System (PAS) Monthly Memory Service 15 CLINICAL EFFECTIVENESS 2.1.8 PRIORITY 7: IMPROVING RECORD KEEPING In the autumn of 2011 a workshop was held with a range of clinical staff and managers to explore the issues relating to record keeping and establish a clear direction to improve standards of record keeping within the organisation. During 2012/13 that action plan will be followed through to completion, setting in place clear standards and expectations, revising and updating documentation and supporting the transition to electronic patient systems via the introduction of the e-care logic system. Monitoring and Measurement of Progress / Key Performance Indicators. Frequency Data Collected Measure Source of Data of Collection and Reported by Audit of Patient Records Quality Team with support Audit report Twice a year wider organisation Monthly review of nursing Productive Ward Ward Sisters / records via Productive Monthly Dashboard Charge Nurses Ward audit Other organisational wide Quality Team audits such as Mortality At least 2 with support will report on quality of Audit report other audits wider record keeping based on a organisation standardised tool 2.1.9 PRIORITY 8: REDUCTION IN 28 DAY READMISSIONS IN MENTAL HEALTH During 2011/12 mental health services carefully monitored readmission rates and work was undertaken to understand which patients are readmitted and why. During the coming year work will continue to ensure further improvement in readmission rates. Community mental health services will be undergoing a period of reorganisation during the period. Changes to services will include the provision of evidence based care to all service users. Inpatient services will work closely with community services to align treatment approaches and build upon the communication improvements made in the last year to ensure that discharged service users needs are met. Delivery of services will support a recovery model. The Mental Health Foundation describes recovery as “care focused on supporting recovery and building the resilience of people with mental health problems, not just on treating or managing their symptoms”. Work to address the re-admission rate will focus on appropriate discharge planning including: • • • Wellness Recovery Action Plan (WRAP) CPA and standard care plan Realistic contingency plans agreed with patient. 16 Wellness Recovery Action Plan (WRAP) was created by Mary Ellen Copeland, an author, educator and mental health recovery advocate in the USA. Mary Ellen describes WRAP as:" a tool that can aid an individual’s recovery and its underpinning principles support the recovery approach. WRAP is a systematic way of monitoring wellness, times of being less well and times when experiences are uncomfortable and distressing. It also includes details of how an individual would like others to support them at these different times.” Recovery emphasizes that, while people may not have full control over their symptoms, they can have full control over their lives. Locally it is recognised that successfully encouraging a patient to develop a WRAP and agreeing realistic contingency plans with the patient, carer and involved professionals is key to successfully managing crises and may avoid the need for readmission to hospital. Quarterly audits will be undertaken throughout 2012/13 to establish and monitor the number of patients who have WRAP plans and agreed contingency plans in place. Monitoring and Measurement of Progress / Key Performance Indicators. Measure Readmission rate to be addressed through appropriate discharge planning including:• Wellness Recovery Action Plan (WRAP) • CPA and standard care plan • Appropriate contingency plans to be agreed with patient Readmission rate to inpatient services with 28 days, 60 days and 90 days. Source of Data Local audit against standards and improvement targets agreed with Commissioners PAS Frequency of Collection Data Collected and Reported by Quarterly Business and Performance Manager – MH and LD Monthly PIDS/ Business and Performance Manager – MH and LD 17 2.2 Statements of Assurance from the Board 2.2.1 Review of Services During 20011/12 the Isle of Wight NHS Primary Care Trust provided and/or sub-contracted 86 NHS services. The Isle of Wight NHS Primary Care Trust has reviewed all the data available to them on the quality of care in 61 of these NHS Services. The income generated by the NHS services reviewed in 2011/12 represents 65.14 per cent of the total income generated from the provision of NHS Services by the Isle of Wight NHS Primary Care Trust for 2011/12. 2.2.2 Dashboards and Scorecards The strategy of allowing staff to access self serve information via a range of online dashboards remains a key priority. This has resulted in a great deal of positive feedback during the past 18 months and requests for further developments continue to be received. One of the early dashboards to be developed was the Clinical Quality Indicators dashboard. This has been made available to relevant staff throughout the organisation and reviews both current performance and trends in the following indicators of quality at directorate level: • • • • • • • Clinical Risk Complaints / Good News Patient Claims Healthcare Associated Infections Patient Falls Reported Incidents Serious Incidents Requiring Investigation In addition to the Clinical Quality Dashboard a range of further dashboards have been developed to allow a focus on different aspects of clinical quality for example a hospital mortality dashboard has been developed, and two dashboards that focus on prescribing and pharmacy. These along with other dashboards are used at the monthly directorate performance reviews as part of the overall performance management process. The aim is to highlight positive performance as well as areas for concern. This focus enables appropriate action to be taken to address performance issues with the aim of improving overall clinical quality. 2.2.3 Patient Safety Walkrounds The organisation has continued to undertake a programme of Patient Safety Walkrounds throughout the year. Dr Allan Frankel, an Anaesthetist from Boston, USA, designed the idea of Patient Safety Walkrounds. The aim of the walk round process being to: 1. Increase the awareness of safety issues among all staff; 2. Make safety a priority for senior leaders by spending a dedicated time promoting a safety culture; 3. Educate staff about patient safety concepts such as incident reporting; 4. Obtain and act on information gathered that identifies areas for improvement; 5. Build communication and relationships with frontline staff. 18 Over the course of 2011/12 a total of 23 Walkrounds took place covering acute services including inpatient wards at St Mary’s Hospital, Mental Health and Learning Disabilities Services, Community Services, including District Nursing and Intermediate Care, the Ambulance Service and Prison Healthcare. These were attended by a team of two reviewers; an Executive Director and a Senior Medical Consultant or the Chief Nurse. The Head of Quality – Commissioning for the PCT Cluster also attends some of these walkrounds. The walkrounds focused on issues of patient safety, but were an opportunity for Senior Executives to visit front line areas to see services for themselves, and for staff to highlight both successes and challenges to the executives. Each Walkround involved a tour of the area and a discussion with area staff and lasted around 60-90 minutes. The programme has continued to be well received by staff. . The majority of the actions identified that needed to be addressed by the staff and executive team, included the improvement of the environment, acquiring more equipment, and improving staffing through recruitment or organisational change. A follow up of the action plans resulting from the walkrounds have shown that a number of actions have been completed including a number of areas that have had estates work undertaken to improve the environment; installation of telecommunications equipment to improve the communication process; computer equipment has been ordered and a number of actions have been taken to review and address the issue of staffing levels in the areas that identified this as an issue. 2.2.4 Participation in Clinical Audits During 2011/2012, 39 national clinical audits and 1 national confidential enquiry covered NHS services that NHS Isle of Wight provides. During that period NHS Isle of Wight participated in 77% national clinical audits and 100% national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. During 2010/2011, 41 national clinical audits and 1 national confidential enquiries covered NHS services that NHS Isle of Wight provides. During that period NHS Isle of Wight participated in 95% national clinical audits and 100% national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that NHS Isle of Wight was eligible to participate in during 2011/12 are outlined in the table below: The national clinical audits and national confidential enquiries that NHS Isle of Wight participated in during 2011/12 are outlined in the table below: The national clinical audits and national confidential enquiries that NHS Isle of Wight participated in, and for which data collection was completed during 2011/12 are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. 19 Name of audit Peri-and Neo-natal Participated % cases submitted Perinatal mortality (MBRRACE-UK) Yes All cases - ongoing Neonatal intensive and special care (NNAP) Yes All cases – ongoing Children Paediatric pneumonia (British Thoracic Society) No Paediatric asthma (British Thoracic Society) No Pain management (College of Emergency Medicine) Childhood epilepsy (RCPH National Childhood Epilepsy Audit) Yes 100% Yes Diabetes (RCPH National Paediatric Diabetes Audit)* No 100% Data collection not due to start till May 2012 Acute care Emergency use of oxygen (British Thoracic Society) Adult community acquired pneumonia (British Thoracic Society) Yes Non invasive ventilation -adults (British Thoracic Society) Yes Data analysis still ongoing Data Entry still ongoing Data Entry still ongoing Cardiac arrest (National Cardiac Arrest Audit) Severe sepsis and septic shock (College of Emergency Medicine) Yes All Cases - ongoing Yes All cases - ongoing Adult critical care (ICNARC CMPD) Yes Potential donor audit (NHS Blood and Transplant) Seizure management (National Audit of Seizure Management) Yes All cases - ongoing 100% of deaths from ITU and AandE are recorded and submitted Yes 100% Yes Long term conditions Diabetes (National Adult Diabetes Audit) No Heavy menstrual bleeding (RCOG National Audit of HMB) Yes Chronic pain (National Pain Audit)* Yes Ulcerative colitis and Crohn's disease (UK IBD Audit) Parkinson's disease (National Parkinson's Audit) Adult asthma (British Thoracic Society) Yes Audit not commenced this year nationally Data Entry still ongoing All cases -ongoing Registered - Round 4 due to begin in 2012/13 No*** Yes 100% Hip, knee and ankle replacements (National Joint Registry) Yes All Cases – ongoing Elective surgery (National PROMs Programme) Yes 87% Acute Myocardial Infarction and other ACS (MINAP) Yes All cases - ongoing Heart failure (Heart Failure Audit)* Yes All cases - ongoing Elective procedures Cardiovascular disease 20 Name of audit Participated Acute stroke (SINAP)* No % cases submitted Pilot audit – not mandatory Cardiac arrhythmia (Cardiac Rhythm Management Audit) Yes All cases – ongoing Lung cancer (National Lung Cancer Audit) Yes All cases - ongoing Bowel cancer (National Bowel Cancer Audit Programme) Yes All cases - ongoing Head and neck cancer (DAHNO) Yes Oesophago-gastric cancer (National O-G Cancer Audit) Yes All cases - ongoing Not due to complete till October 2012 Hip fracture (National Hip Fracture Database) Yes All cases – ongoing Severe trauma (Trauma Audit and Research Network) Yes 96% Prescribing in mental health services (POMH) Yes 100% Schizophrenia (National Schizophrenia Audit) Yes 100% Blood transfusion Bedside transfusion (National Comparative Audit of Blood Transfusion) Medical use of blood (National Comparative Audit of Blood Transfusion) Yes 100% Cancer Trauma Psychological conditions No* Health promotion Risk factors (National Health Promotion in Hospitals Audit) No No lead identified for this – Quality Team not advised of audit (I have now registered for next year to be notified ) Not Mandatory audit End of life Care of dying in hospital (NCDAH) No** NCEPOD Studies Alcoholic Liver Disease Total: 40 Yes Data collection still ongoing 31 In relation to the following audits, these were not participated in for the reasons stated below: *The Hospital Transfusion Committee and the NHS Blood Transfusion lead, considered the audit carefully, unfortunately it was decided that due to lack of capacity by staff required to undertake the audit participation at the time was not possible. 21 ** The National Audit Team advised the Trust that prior to participating in the audit it was essential to embed the Liverpool Care Pathway prior to commencement, and as version 12 had only just been launched the decision was taken not to participate. ***Decision taken that the resources of the team should be used to resolve the local ward understanding of medication assessment as a priority rather than participate in the audit. NCEPOD have released finalised data following the studies undertaken during 2009/10 which were reported in last year’s Quality Account (2010/11) and our response rates are confirmed below: • Surgery in Children’s Study response rate 100% (1 case only applicable) • Perioperative Care Study response rate 54% • Cardiac Arrest Procedures is still underway. The reports of 7 national clinical audits were reviewed by the provider in 2011/12 and the Isle of Wight NHS Trust intends to take the following actions, amongst others, to improve the quality of healthcare provided: • Implement a Policy for ‘Safe Provision of Paediatric Surgery and Anaesthesia’ in line with NCEPOD recommendations. • Hand held records have been implemented for patients which ensures that they have had the correct blood monitoring before lithium prescriptions are re-issued. • Work is ongoing to support the prescribing of antipsychotic drugs in children with ADHD by paediatricians; work is currently ongoing on a shared care protocol with GPs. The reports of 31 local clinical audits were reviewed by the provider in 2011/12 and the Isle of Wight NHS Trust intends to take the following actions to improve the quality of healthcare provided: • Revise and implement new documentation to improve record keeping and enhance patient care. • Education of medical and nursing staff regarding the recommendations of NPSA in the checking of nasogastric tube insertion • Poster on paediatric prescription to inform all staff of the expected standards for prescribing to be displayed in paediatric doctors office Clinical Audit Prize The annual competition for the Clinical Audit Prize is open to all staff who have undertaken an audit within the NHS Isle of Wight during the previous financial year. The shortlisted finalists present their audit project to an invited audience, which includes senior staff from across the organisation who judge the projects based on the structure and outcome of the audit project. In June 2011, the third year of the competition, the winners were Dr Divya Sharma and Dr Evgenia Katsoni who undertook a Trust wide audit of record keeping establishing effectiveness of medical note taking within NHS Isle of Wight. This scheme will continue within the new Isle of Wight NHS Trust 22 2.2.5 Participation in Clinical Research The number of patients receiving NHS services provided or sub-contracted by the Isle of Wight NHS Primary Care Trust in 2011/12 that were recruited during that period to participate in research approved by a research ethics committee was 943 [as at 2 April 2012]. Participation in clinical research demonstrates the Isle of Wight NHS Primary Care Trust’s commitment to improving the quality of care we offer and to making our contribution to wider health improvement. Our clinical staff stay abreast of the latest possible treatment possibilities and active participation in research leads to successful patient outcomes. The Isle of Wight NHS Primary Care Trust actively enrolled patients to 36 recruiting clinical research studies on the National Institute for Health Research (NIHR) Clinical Research Network Portfolio. These studies involved the clinical specialties of Cancer including Clinical Genetics, Diabetes, Mental Health, General Practice, Cardiovascular, Ambulance, Neuro-rehabilitation, Immunology and Inflammation, Injuries and Emergencies, Public Health, Reproductive Health and Childbirth and Respiratory. There were 33 clinical staff participating in research approved by a research ethics committee at the Isle of Wight NHS Primary Care Trust during 2011/12. In the last three years, the impact of research activities of the David Hide Asthma and Allergy Centre has been substantial and continues to deliver high impact publications and facilitated the development of further funding applications. Furthermore, it has had a direct impact on the development of two clinical research fellows who benefited from the expert tuition of Professor Wilfred Karmus, Professor and Graduate Director for Epidemiology at the University of South Carolina, USA. Professor Karmus has a long record of long distance collaboration with the Centre as an academic partner. It has already improved our clinicians understanding of two areas of medicine; (i) their better understanding of exhaled nitric oxide, atopy and asthma means that they now know that exhaled nitric oxide is not the useful marker of asthma control that they once thought it was and (ii) their whole childhood eczema paper will help clinicians understand the prognosis of children and teenagers with eczema particularly as less children outgrow these problems as originally thought. Our engagement with clinical research shows our commitment to transparency and desire to improve patient outcomes and experience across the NHS but equally demonstrates our commitment to testing and offering the latest medical treatments and techniques. 2.2.6 Goals Agreed with Commissioners A proportion of Isle of Wight NHS Primary Care Trust’s income in 2011/12 was conditional on achieving quality improvement and innovation goals agreed between Isle of Wight NHS Primary Care Trust and any person or body they entered into a contract, agreement or arrangement with for the provision of NHS services, through Commissioning for Quality and Innovation payment framework (CQUINs). Further details of the agreed goals for 2011/12 and for the following 12 month period are available at the following web link: http://www.institute.nhs.uk/commissioning/pct_portal/cquin.html. 23 A summary of CQUIN achievement during 2011/12 is laid out on the next page, highlighting the schemes for each contract held within NHS Isle of Wight Provider Services AMBULANCE 1. To achieve a defined set of national targets (Gateway CQUIN) - Achieved 2. Admission avoidance – See and Treat by Paramedics and ECPs - Achieved 3. Patient experience – personal needs – Achieved ACUTE 1. VTE Prevention – Achieved 9 out of 12 months (paid monthly) – Achieved 9 months (75%) 2. Patient experience - personal needs – based on Getting it Right data – Achieved 90% 3. Achievement of national targets (Gateway CQUIN) 16 targets - 14 Achieved / 2 Failed 1) Total time spent in the emergency department equal to or greater than 4 hours (95th percentile) and 2) Referral to treatment time waits, admitted median 4. Unscheduled Care Hub process development and utilisation – Achieved 5. End of Life Care: To improve end of life care for patients cared for in the acute setting Part a) Provider staff training and development for end of life care – Achieved Part b) Provider to set up systems and processes for identifying patients who are dying, to ensure their end of life care is supported through a well documented - Failed 6. Supporting change in lifestyle through brief intervention for inpatients over 16 years Part a) To improve health by ensuring that all in-patients over 16 years who smoke are identified and provided with a brief intervention and support on quitting and to develop an action plan to extend to other lifestyle choices - Failed Part b) To improve health by ensuring that all in-patients over 16 years who smoke, are identified and offered (on an opt out basis) with a brief intervention and support on quitting - Achieved MENTAL HEALTH 1. Involving carers of service users and measuring carer satisfaction – Achieved 2. Alcohol strategy: integrated alcohol pathway and inpatient detoxification - Achieved 3. Review the use of Antipsychotic Drugs in Dementia - Achieved 4. Transition from Specialist CAMHS Model to Community CAMHS Model of Service Achieved COMMUNITY 1. To achieve a defined set of national targets (Gateway CQUIN) – Achieved 2. Admission Avoidance through a reduction in falls – Achieved 3. Improved rehabilitation outcomes through the configuration of rehabilitation services – Achieved 4. Analysis of health needs of children, young people and their families – Achieved 5. Improved Case Management of NHS Funded Care clients – Partially Achieved 80% PRISON 1. Achievement of national targets (Gateway CQUIN) - Achieved 2. Prison Health Performance and Quality Indicators – Achieved 50% 3. Patient experience - Personal needs - Achieved 4. Improved outcomes against the Quality Outcomes Framework - Achieved 24 2.2.7 What Others Say about the Provider Statements from the CQC Isle of Wight NHS Primary Care Trust was required to register with the Care Quality Commission until 31st March 2012 and its registration status was registered up until that date. Isle of Wight NHS Primary Care Trust had the following conditions on registration – no conditions Isle of Wight NHS Trust is required to register with the Care Quality Commission and its current registration status is registered from 1st April 2012. Isle of Wight NHS Trust has the following conditions on registration – no conditions The Care Quality Commission has not take enforcement action against Isle of Wight NHS Primary Care Trust during 2011/12. Isle of Wight NHS Primary Care Trust has participated in special reviews or investigations by the Care Quality Commission relating to the following areas during 2011/12 – Review of Compliance, St Mary’s Hospital and two Mortality Reviews relating to complex elderly with a primary respiratory diagnosis (1) and primary cardiac diagnosis (2) Isle of Wight NHS Primary Care Trust/Isle of Wight NHS Trust intends to take the following action to address the conclusions or requirements reported by the CQC as outlined below Isle of Wight NHS Primary Care Trust has made the following progress by 31st March 2012 in taking such action as outlined below Review of Compliance – St Mary’s Hospital During September 2011 the CQC undertook an unannounced visit at St Mary’s Hospital, visiting the Maternity Unit, Medical Assessment and Admissions Unit, Colwell Ward, Luccombe Ward, and the Emergency Department. They reviewed 7 outcomes and found 2 were fully compliant, 4 were compliant but actions needed to maintain compliance and 1 was identified as having areas of non-compliance. This related to concerns about the Medical Assessment and Admissions Unit (MAAU), and focused on outcome 4, care and welfare of people who use services. They were concerned that patients within the MAAU were not always provided with the care they needed. A comprehensive action plan has been in place and a follow up report was issued to the organisation on 27th March 2012. This confirmed that the organisation was now compliant but to maintain this further improvement is needed to strengthen record keeping on the unit. A plan is in place to ensure best practice is embedded within the Unit. Mortality Reviews In January 2012 the CQC contacted the organisation with two mortality outlier alerts relating to care of emergency admissions with HRG D99 – complex elderly with a respiratory system primary diagnosis and HRG E99 – complex elderly with a cardiac primary diagnosis, relating to patients who died between October 2010 and June 2011. The report was sent to the CQC in February 2012 outlining the details of the reviews completed and a summary of activity relating to mortality within the organisation. At the time of writing this CQC have requested additional information which has been forwarded 25 to them but no further response from the CQC has been received. Actions arising from the review include • Developing speciality level review of deaths • Reviewing MEWS scoring • Development of an inpatient heart failure clinical nurse specialist post • Review of compliance with the do not attempt cardio-pulmonary resuscitation policy and Liverpool Care Pathway for end of life care. 2.2.8 Data Quality i) Statement on relevance of Data Quality and actions to improve data quality High quality information is a vital asset, both in terms of the clinical management of individual patients and the efficient management of services and resources. It plays a key part in clinical governance, service planning, performance and business management that all help to demonstrate the quality of the services we provide. Therefore the Trust views Data Quality as an essential element of delivering high quality health care service. Whilst some elements of our data quality are extremely high work to monitor and improve data quality is ongoing in order to drive continual improvement. Some of the actions that we have been working on include: Establishment of a Counting and Coding Project – this project will address any areas where data capture could be improved, as well as providing assurance that activity data accurately reflects care provided. The benefits of complete and consistent data delivered through this project include: - Enablement of patients and commissioners to compare services, based on quality Enablement of effective benchmarking analysis Provision of clear understanding of the needs of service users Supporting the consistent application of the PbR tariff and a consistent basis for savings and investment plans Supporting the delivery of better care through accurate, timely funding The Trust is subject to a series of Audits that cover elements of data quality (both internal and external undertaken to review various business processes - Payments by Results, Clinical Coding, Information Governance) where these have highlighted either poor data quality or risks to data quality recommended remedial actions will be implemented. ii) NHS Number and General Medical Practice Code Validity The Isle of Wight NHS Primary Care Trust submitted records during 2011/12 to the Secondary Uses service for inclusion in the Hospital Episode Statistics which are included in the latest published data. The percentage of records in the published data: - which included the patient’s valid NHS number was: 97.7% for admitted patient care; 99.2% for outpatient care; and 97.1% for accident and emergency care. 26 - which included the patient’s valid General Medical Practice Code was: 100% for admitted patient care; 100% for outpatient care; and 100% for accident and emergency care. iii) Information Governance Toolkit Attainment Levels The Isle of Wight NHS Primary Care Trust’s Information Governance Assessment Report score overall score for 2011/12 was 74% and was graded pink. 85% of staff were compliant with the mandatory Information Governance training at the end of the financial year for 2011/2012. iv) Clinical Coding Error Rate The Isle of Wight NHS Primary Care Trust was subject to the Payment by Results clinical coding audit during the reporting period by the Audit Commission and the error rates reported in the latest published audit for that period for diagnoses and treatment coding (clinical coding) were: Primary diagnoses incorrect (3.5%) Secondary diagnoses incorrect (11.65%) Primary procedures incorrect (2.35%) Secondary procedures incorrect (1.7%) The error rates shown are inclusive of both coder error and non-coder error, there were 70 secondary diagnosis errors found 48 of which were non-coder (Generally missing information related to co-morbid conditions) and 22 coder errors. The Clinical Coding Manager continues to work closely with the Clinical teams to raise awareness of the importance of all information being provided on the discharge summaries. Work is ongoing with the roll out of a Clinical Coding Tick List which promotes the collection of co-morbid conditions (Secondary Diagnoses).The Clinical Coding Manager intends to attend all individual specialty directorate meetings to continue to promote improvements in this area. The Clinical Coding team were made aware of their errors and subsequent support, training and guidance has been made available. 27 PART 3 3.1 Review of Quality Performance 3.1.1 Identification and response to the deteriorating patient and hospital at night Introduction Identification and management of the deteriorating patient has been a priority for the organisation for a number of years, with a particular focus on the introduction of a Modified Early Warning System (MEWS) to identify patients whose condition is starting to deteriorate to ensure appropriate action can be taken at the right time. Despite this action, there are still some instances of a lack of compliance with the MEWS policy, which is demonstrated by the occurrence of avoidable admissions to the Intensive Care Unit. This identified improvement priority is closely linked to the Hospital at Night programme and some areas of improvement will overlap, complement and support improvement in shared key performance indicators. The Hospital at Night / out of hours scheme came into being following implementation of the European Working Time Regulations (EWTR), and was initially piloted by four Trusts and supported by the NHS Modernisation Agency. It is a change programme that uses a multi-professional approach to delivering high quality standards of care. It typically involves changing the staff mix at night by developing a team of highly skilled advanced night nurse practitioners and reducing the reliance upon Doctors in training. The scheme involves developing staff competencies to cover a wide range of interventions, but that has the capacity to call in specialist expertise when necessary. From a patient’s perspective, this means that the nearest available person with the appropriate skills will be diverted to treat the patient, rather than waiting for one specific person. In real terms, patients will be treated quicker. Hospital at Night also applies to weekends/out of hours and can even apply to the emergency admissions side of the normal working day. It is essential that the system is properly followed. Hospital at Night advocates safer practice and supports safer training, whilst improving patient outcomes and quality of care. The effective and safe management of patients in hospitals during the out of hour’s period has emerged as a key challenge for NHS organisations in recent years. The Hospital at Night project sets out to improve response times to deteriorating patients by signposting the nearest appropriately skilled person to undertake any treatment needed. Actions taken in the Last Year 1. Due to the success of the Critical Care Outreach Service that was implemented in April 2010 the service hours have been increased and the service now operates 7 days a week 08:00 – 20:30 hours. This is a nurse led service that has been developed within the existing budget for the Intensive Care Unit. The service is an adjunct for the general ward based teams to support them in caring for patients who are critically ill or have potential to develop such an Illness and/or the potential for their condition to deteriorate. The Critical Care Outreach Service is there to support, educate and empower ward based teams and not to take over or take responsibility away from the ward based teams for their patients. 28 2. A successful business case was approved for the implementation of three Advanced Nurse Practitioner posts which will be an additional role to the workforce in the hospital at night team and will also provide cover for the Critical Care Outreach Service at night. This development came from the hospital at night work stream that forms part of the acute care pathway project being undertaken within the organisation. 3. Root cause analysis of cardiac arrests that occur within in-patient areas have been undertaken since October 2011 and this has driven down these adverse events significantly and we are now pushing forward with a zero tolerance of cardiac arrest. 4. Root cause analysis of readmissions to the intensive Care Unit has supported a significant reduction in numbers since the Critical Care Outreach Team has been in place. 5. The hospital at night project team has successfully implemented a multidisciplinary team night handover process that is chaired currently by the Night Co-ordinator. This ensures all patients are handed over to the new oncoming team, high risk patient’s identified and other relevant operational factors are taken into account. 6. On-going Monthly Ward based audits for the compliance against the MEWS policy. 7. After a successful Introduction of a tracking tool of deteriorating and at risk patients this will now be used for other specialties to help identify at risk patients who may have risk factors that may be missed. 8. Continued delivery of multidisciplinary education within the organisation to support the identification and response to the deteriorating patient. This includes the ALERT course, a host of resuscitation training courses and daily informal bedside teaching from the Critical Care Outreach Service. Chosen Performance / Quality Indicators The chosen indicators to demonstrate improvement were decided upon from local decision making and based on recommended measurements from the National Patient Safety Agency work stream on deterioration. These included the following measures: 1. No serious incidents requiring investigation relating to the non recognition and response to the sick patient 2. Compliance with the local modified early warning scoring system (MEWS) policy for deteriorating patients 3. Reduced unplanned admissions to the Intensive Care Unit 4. Reduced readmissions to the Intensive care Unit 5. Reduction in the number of cardiac arrests 29 Impact of Actions on Indicators 1. Reduction of Serious Incidents Requiring Investigations relating to ‘failure to rescue deteriorating patients. Month January February March April May June July August September October November December 2010 0 0 0 0 0 0 1 0 0 0 0 0 2011 0 0 0 0 0 0 0 0 0 0 0 0 2012 0 0 0 2. Compliance with MEWS Policy 3. Reduce Unplanned Admissions to Intensive Care from Wards 30 4. Reducing Readmissions to Intensive Care (compared to total number of admissions) 2009 Readmissions January February March April May June July August September October November December 1 1 1 1 1 3 2 0 0 2010 2011 2012 Admissions Readmissions Admissions Readmissions Admissions Readmissions Admissions 25 30 36 28 33 27 24 21 27 24 26 31 1 0 0 0 1 1 0 0 0 1 0 0 30 18 36 20 38 36 22 27 29 29 34 29 0 0 0 28 36 30 29 25 37 27 32 28 27 23 33 0 1 0 2 1 2 1 1 0 2 2 1 5. In-Patient Ward Cardiac Arrests Next Steps We aim to keep the identification and response to the deteriorating patient and hospital at night as a key area for improvement for 2012/13, in order to build on the current success to ensure all the correct measures are in place to sustain what has already been achieved in 2011/12. 3.1.2 Prevention of Venous Thromboembolism Deep Vein Thrombosis and Pulmonary Embolism are the most common serious complications of venous thrombosis, collectively known as Venous Thromboembolism (VTE). VTE is known to be a significant cause of death in hospital patients and treatment of nonfatal symptomatic VTE and related long-term morbidities is associated with considerable cost to the health service. The House of Commons Health Committee reported in 2005 that possibly up to 25,000 people die each year from preventable hospital-acquired VTE in The U.K. Risks of thrombus formation increases with lengthy surgical procedures and periods of immobility. 31 Last year this was identified as one of the Trust priorities and continued to be audited monthly. During 2011/12 the compliance for the year was 92.8% of patients getting the appropriate risk assessment and treatment against the Department of Health target of 90%. It is anticipated that the roll out of e-prescribing will further provide feedback on the VTE status of every patient admitted and as our compliance has been over the 90% target for the year it has been decided that this will not form a priority for this coming year. However, this is still of the utmost importance for our patients and will continue to be monitored by the Trust on a monthly basis and compliance will be reported regularly to the Board. This also forms a national CQUIN scheme for 2012/13. Percentage VTE Data Submissions 100% 98% 96% 94% 92% 90% 88% 86% 84% 82% 80% 92.2% 88.7% 87.1% 91.5% 96.0% 96.6% 89.4% 96.0% 94% 95.3% 94.5% 3.1.3 Prevention of Pressure Ulceration The last year has seen continuing improvements in reducing the rates of hospital-acquired pressure ulcers. This is the third year in which this has been a key priority for the Trust, and the Trust has adopted a zero-tolerance approach to these potentially avoidable events. The key patient safety measures adopted for the last year were: • • Reduction in hospital-acquired pressure ulceration of European Pressure Ulcer Advisory Panel (EPUAP) grade 2 and above to below 2% Reduction in hospital-acquired pressure ulceration of EPUAP grades 3 and 4 to below 0.3%. Both indicators now consistently are above the target set for them at the start of the Quality Account for this year. A number of key initiatives have contributed to these improvements. • The majority of clinical areas, where it is appropriate, have adopted the principles of Intentional Rounding and Patient Safety checks, which seek to embed higher level of vigilance over patients who are particularly at risk of skin breakdown and other safety events, e.g. falls. 32 • There has been a roll out of comprehensive Pressure Area Care and Management plans to support the accurate planning and documentation of care in relation to patients at risk of skin breakdown. • The implementation of an organisational wide Pressure Ulcer Reduction and Management plan which has sought to standardise all clinical areas’ approach to pressure area care, including the issuing to all trained nurses laminated colour picture cards which assist nurses in correctly identification of stages of skin breakdown. • There has been further work on reviewing the most serious types of pressure ulcers (EPUAP grade 3 and 4) which has resulted in action plans which aim to address the root causes and help staff to implement actions which continually improve care of patients in relation to pressure ulcers. The graphs bellow outline the performance for April 2011 to March 2012 33 3.1.4 Reduction in 28 Day Readmission Rates in Mental Health Isle of Wight services have been shown to have a higher than the national average number of people who are re-admitted to hospital within 28 days following a period of treatment as a mental health inpatient. Repeated admissions to hospital can have a negative impact upon patients and those who care for them. There are many factors that impact upon the likelihood of a person requiring repeated admissions. Services need to ensure that they are offering evidence based treatments that are most effective in treating patient’s difficulties. Inpatient and community services need to be offered in a joined up and cohesive way so that people feel adequately supported when they leave hospital. Over the past year there have been a variety of initiatives aimed at smoothing the path between inpatient and community based care. Communication between in-patient and community services has improved ensuring that the post discharge and ongoing needs of patients are considered at the earliest opportunity. This allows support to be in place at the point of discharge. The Crisis Resolution/Home Treatment (CRHT) team continue to offer a vital bridge in facilitating discharge from a hospital setting, by providing intensive home based support in the short term (4-6 weeks average). The service strives to achieve follow- up of all patients within seven days of discharge from hospital as this is shown to be the most vulnerable time for people who have been discharged. Inpatient services have been working hard over the past 2 years to provide a greater range of therapeutic interventions within the inpatient setting. This has proved both effective and popular with service users. Further work has been undertaken to develop a range of interventions with voluntary sector partners in order to provide people with the same kind of intervention and support following discharge from hospital. This is complemented by the range of therapies available within community based mental health services. Recent Audit Commission benchmarking indicates that alongside high readmission rates in mental health, the Isle of Wight has a short average length of stay. This indicates a service model that attempts to help service users’ transition back to the community and is recognised as good practice. The national median for readmission rates is 9% (ranging between 2%-18%). Locally readmission rates to hospital have fluctuated during the year. Rates decreased for the first 2 quarters of the year. There was however a reverse in the trend within the third quarter. Detailed examination of quarter 3 2011/12 data identified:• Repeated admissions of just a few individuals accounted readmissions for the majority of • 25% of patients readmitted were brought to hospital by the police and on assessment a significant number of these did not require in-patient services. • A significant number of the readmissions were for people who were experiencing repeated crises in their lives, often fuelled by addiction problems. These situations can increase the difficulty of ensuring that people receive and accept suitable follow post discharge. 34 Quarter 4 2011/12 data indicates a readmission rate of 8.5% in comparison to 13% for the same period in 2010/11. Percentage Readmissions Data 18% 16% 14% 12% 10% 8% 6% 4% 2% 0% 710 - Adult 715 - Older Persons Total 2011/2012 Qtr 4 2011/2012 Qtr 3 2011/2012 Qtr 2 2011/2012 Qtr 1 2010/2011 Qtr 4 2010/2011 Qtr 3 2010/2011 Qtr 2 2010/2011 Qtr 1 Quarter Overall progress has been made in the reducing the number of readmissions whilst maintaining a short length of stay. However, it is recognised that there further work is required to maintain performance and further reduce the number of readmissions and therefore this indicator will be carried forward as a priority for the 2012/13 Quality Account – see section 2.1.10 for further details. 3.1.5 Improving the Pathway for Clients with Alcohol Addiction It has been estimated that the NHS nationally spends £2.7billion per year treating the needs of people who drink alcohol to a level that is harmful to their health. Alcohol misuse and harmful drinking levels have increased through the last decade. 6% of men and 2% of women are classified as having harmful drinking patterns which will affect their health. In a national study in 2009 it was calculated there were nearly 7000 deaths directly attributable to alcohol misuse. Providing the population of the Isle of Wight with adequate specialist help when they suffer with alcohol addiction has been a constant challenge for drug/alcohol services and wider health services on the Isle of Wight. An important component of this specialist provision is the facilities and expertise to offer people a safe and reliable alcohol detoxification service. For some people this can be safely provided in the home environment with adequate professional and family support. However there are some people for whom this treatment is not advisable or safe due to their medical or other health needs. These people have therefore required detoxification in a hospital setting. Hospital detoxification (Detox) has been offered to people for many years on the Isle of Wight. However there has not been a dedicated resource for people within the hospital setting, meaning that Detox’s have been difficult to plan effectively. The Island Drug and Alcohol Service (IDAS) works with people with harmful drinking problems. Last year there was an increase made in the level of specialist nurse provision for alcohol related problems. However there remained a lack of dedicated hospital 35 provision for patients requiring inpatient services. This meant that IDAS had a growing list of people who required a planned Detox which could not be adequately addressed. It was decided that a dedicated bed would be designated within Sevenacres mental health unit for this purpose. In August 2011 the dedicated bed came into use. Prior to its opening inpatient staff worked closely with IDAS staff to ensure that appropriate and safe treatment was offered to people. It is recognised that people stand a greater chance of success following a Detox if they receive individual sessions preparing them for the Detox. In addition they need to receive relapse prevention sessions post Detox. The plan at the opening of the bed was that people requiring inpatient Detox would receive the pre and post Detox work indicated. The quality indicator was set for the year and stated that there needed to be: • A quarterly increase in the percentage of patients having undertaken preparatory counselling/therapy, completing detoxification and going on to start relapse prevention There was a requirement within the quality indicator for the percentage of people receiving pre and post interventions to rise from 75% in quarter 1 to 85% by quarter 4. The following table shows the percentage of people who have received an inpatient Detox in the Sevenacres bed and whether they completed the pre and post work required. It is clear to see that all people received the preparatory work required. Of those people finishing their Detox, all received the relapse prevention work. All of the targets for the initiative were met Planned Detox Admissions April 2011 - March 2012 100% 80% Pre-Work Completed Detox Post-Work 60% 40% 20% 0% Apr- May- Jun- Jul- Aug- Sep- Oct- Nov- Dec- Jan- Feb- Mar- 11 11 11 11 11 11 11 11 11 12 12 12 Key Series 1 - %people receiving pre work; Series 2 - % people completing Detox; Series 3 - % people completing post work (Please note that the gaps in planned detox’s between May-July was a result of excessive bed pressures in Sevenacres. Throughout the whole period shown there were still people admitted to Sevenacres that required an unplanned Detox. These people fell outside of the scope of the measures in place for this particular quality initiative.) Whilst the chance of continued success is greater for those who receive the appropriate individual support before and after a Detox, there are still situations where people are admitted in an unplanned way and need to receive a Detox. Due to the further investment in IDAS alcohol services it has now been possible to offer those having an unplanned Detox the relapse prevention work when they leave hospital. 36 It is still relatively early days with the provision of this new service. In liaison with IDAS we will provide the inpatient staff with ongoing training to ensure that the service is still offered in a safe way. We also need to find a more refined way to gather service user feedback. This is currently collected alongside all inpatient feedback. Ward managers will address this issue within the next quarter. It is clear that the provision of a dedicated bed has allowed for people to receive the required interventions to make the potential outcomes of their Detox successful and has also allowed IDAS to more easily manage the waiting list that they hold. In the future we will maintain our statistical records so that the Drug Alcohol Action Team (DAAT) can receive reports. 3.1.6 Improving Stroke Care At the Stroke Public Accounts Committee on 24 February 2010, the Department of Health committed the NHS to an accelerated programme of improvement in stroke services for 2010/11 to address areas of the National Stroke Strategy (2007) highlighted by the National Audit Office report in 2009 as needing greater focus to support improvement. This programme, known as Accelerating Stroke Improvement, developed ten measures to enable tracking of progress throughout the stroke pathway. In addition to the Accelerating Stroke markers it has also been agreed with South Central Stroke Network that there will be 8 additional indicators for collection, again addressing quality of care and service throughout the pathway. These priorities are monitored and measured by the South Central Cardiovascular Network on a monthly basis. Progress within each of the markers is reported by the stroke steering group COO, Community Service level agreement and Trust board. Patient survey data, provided by our clinical governance department and regional stroke PPI reports are also important tools used in ensuring that a quality service is delivered to our stroke patients. Over the past year the organisation has continued to be fully committed to improving stroke services in line with these quality markers, building on progress made over the previous 18 months. Key improvements have occurred over the past year throughout the stroke pathway. Our seven day a week TIA (Transient Ischaemic Attack or mini stroke) service has proven successful referrals are now much more appropriate from our GPs and a recently developed TIA information leaflet to be given to patients at the time of referral has lead to a more timely response in relation to high risk patients being seen within 24 hours of referral. Since the Single point of access for Stroke Patients has been introduced the proportion of patients scanned within 1 hour of arrival has improved immensely. In addition since priority has been given to all Stroke Patients being directly admitted to a Stroke Unit via the Emergency Department we have improved performance ensuring where possible they spend at least 90% of their hospital stay on a specialised unit ensuring they receive quality care in line with the national requirements. The Community Stroke Rehabilitation Team has now been in operation for approximately 1 year and by supporting early discharge has contributed to the overall length of stay reducing for stroke patients. The team are consistently performing over and above 37 expected National Targets as can be seen on the pictorial. Patient feedback via surveys re this service has been overwhelmingly positive. Thrombolysis in acute stroke has been delayed. This is simply to ensure that our equipment, training and IT systems and processes are in place to deliver a high level of service to our patients this has taken longer than anticipated. The pictorial below indicates in green where we have achieved our targets, those in red indicate where we need to improve. Quality Markers Apr May Jun Jul Aug Sep Oct Nov Dec Jan Proportion of patients presenting with AF presenting with stroke, anti- 60% 17% 60% 100% 60% 29% 50% 33% 67% coagulated on discharge (60% by April 2011) Proportion of people with high-risk TIA fully 50% 68% 69% 60% 62% 91% 47% 62% 83% investigated and treated within 24 hours (60% by April 2011. Vital Sign) Proportion of patients admitted directly to an acute stroke unit within 4 hours of 58% 50% 36% 14% 57% 40% 92% 73% 83% hospital arrival (90% by April 2011) Proportion of patients spending 90% of their inpatient stay on a specialist 79% 75% 55% 86% 83% 80% 89% 82% 87% stroke unit (80% by April 2011.Vital Sign) Proportion of stroke patients scanned within one hour of hospital arrival (50% by April 11) Proportion of stroke patients scanned within 24 hours of hospital arrival. (100% by April 11) Proportion of patients supported by a stroke skilled Early Supported Discharge team. (40% by April 2011) Proportion of patients and carers with joint care plans on discharge from hospital to final place of residence (85% by April 2011) Proportion of stroke patients that are reviewed at six months after leaving hospital (95% by April 2011) Proportion of patients who have received psychological support for mood, behaviour or cognitive disturbance by six months after stroke. (40 % by April 2011) 14% 47% 27% 48% 54% 57% 52% 64% 52% Feb Mar 40% 100% 33% 94% 93% 62% 61% 64% 63% 74% 50% 79% 56% 50% 48% 100% 100% 100% 100% 100% 96% 100% 100% 100% 100% 100% 100% 57% 44% 78% 54% 57% 48% 55% 63% 67% 69% 43% 100% 100% 93% 100% 100% 100% 91% 95% 94% 94% 100% 86% 0 0 0 73% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 38 Future Plans As indicated above many areas have improved steadily over the past year, for those below target we will continue to monitor, collect data and deliver the message to all staff through Directorate Board Meetings and Ward meetings. As a Trust we are dedicated to ensuring that :• Our service is delivered to all stroke patients in a timely manner. Due to extreme pressure on bed pressures the 4 hour target has not been met, but the Trust will continue to ensure that processes are in place to deliver a seamless pathway from ED to a dedicated Stroke Unit within 4 hours of admission. • We will continue to raise awareness of the key messages of what a stroke is and how it can be managed effectively and efficiently through our GP services and Stroke Steering group where we have a patient representative. • Through training and development of staff in our dedicated Stroke Units we will continue to make certain that delivery of first class Stroke care will continue, standards are met and a quality service will thrive. Improving Stroke Care will not be carried forward into the 2011/2012 quality report however the quality markers will continue to be monitored on a monthly basis via the Isle of Wight NHS Trust monthly performance report. 3.1.7 Community, Outpatient and Home Antibiotic Therapy Over the last year the organisation has provided an OHPAT service (Outpatient and Home Parenteral Antimicrobial Therapy), that aims to deliver intravenous antibiotic care for appropriate cases in the Community rather than in the traditional Hospital setting. Performance against Key Performance Indicators A. Improve patient experience The ethos of the OHPAT service is to provide care that is equivalent to, if not superior to that of inpatient care. The service aims to provide a level of care that focuses on improving the patient journey, whilst maximising patient choice. Since April 2011, the service has provided community based intravenous care for 29 patients that would have ordinarily been treated in the hospital. They were able to go home and enjoy such comforts as sleeping in their own beds, eating their own food, avoiding separation from family, and resuming some kind of normality within their home life. Every patient was visited daily by either a District nurse or the Nurse Specialist for OHPAT with a comprehensive assessment carried out to assess clinical condition. There was also a 24 hour emergency phone number available if any concerns arose. At the end of every patient journey a feedback questionnaire was given, enabling the patient to raise any issues or concerns which could then be used to help further develop future practice. 39 As the graph above indicates, the OHPAT service has provided the release of in excess 700 bed days since April 2011. These patients would normally have been treated within the Hospital, but were able to be cared for within their own home or as an outpatient avoiding prolonged Hospital stay. Patient satisfaction survey results following being treated by OHPAT Percentage 100 99.5 99 98.5 98 97.5 97 April (1)May (1) June (1) July (1)Aug (1) Sept (2) Oct (2) Nov (2) Dec (2) Jan (2) Feb (2) Mar (1) 2011/2012 Every patient that has accessed the OHPAT service has been offered the opportunity to complete a feedback form that assesses satisfaction with the service. As the second graph above shows, the level of satisfaction has been extremely high with very positive comments given. 2. Reduce the number of infections Midline / PICC line insertions 14 12 10 8 6 4 2 0 April M ay June July Aug Sept Oct Nov Dec Jan Feb M arch 40 Midline catheters and PICC’s (Peripherally Inserted Central Catheter) have been introduced within the Trust, as they provide mid to long term intravenous access. April 2011 to March 2012:• The number of Mid / PICC lines inserted is: 76 • Infections occurred from the 76 inserted lines: 2 • Total indwelling time: 1339 days C. Training for further staff to insert midlines At present, the Clinical Care Outreach Team are working in partnership with the Nurse Specialist for OHPAT and a Consultant Anaesthetist to gain competency in the insertion of Midlines by teaming up with either of them whenever a line is required to be inserted. Further extension of this skill will then be explored, but only for selected professionals. Patient story regarding the OHPAT journey, including Midline insertion. “One of the best services available, the patient has nothing to do. I can only praise the scheme. Once Gary was involved the pieces of the jigsaw all began to fall into place, right through to my dates at Southampton General Hospital. It was a great relief as everything was put into place, with all home appointments, daily at first, then every other day. I can only say a very big thank you to you all and may it continue. Well done”. Future monitoring of the service • Review of database’s to ensure ongoing data collection captures: financial data, clinical data, patient outcomes and patient problems. • Weekly virtual ward round. • Ongoing patient questionnaire audit. • Ongoing Consultant and district nurse questionnaire audit. • 3 monthly audit of paperwork documentation. • 6 monthly midline / PICC / CVAD steering group meeting. • 3 monthly OHPAT steering group report. 3.1.8 Improving the Experience of Children and Young People in Psychiatric and Emotional Crisis Following on from the requirement meet the recommendations of Sir Albert Aynsley-Green the Commissioner for Children we have continued to embed the service developments: • Policy regarding admission of young people in emotional and psychiatric crisis • Pathway for accessing specialist child and adolescent mental health provision on the mainland • Introduction of In-reach/Outreach Team We have also implemented the following priorities as outlined in the 2010/11Quality Account: • Exception reports to the Mental Health Quality meeting and all exceptions to the admissions policy are subject to a case review. • Introduction CORC (Clinical Outcome Reporting Consortium) to monitor clinical effectiveness and outcomes in combination with Health of the National Outcome Scales Child and Adolescent (HONOSCA). 41 • • • • • Involving service users in completing questionnaires recording their experience to improve service delivery. Bi monthly paediatric meetings to develop closer working practices and pathways for patient care. The development of Community Child and Adolescent Mental Health service by multidisciplinary co operative training and case management including the use of the Solihull Training Approach. A care pathway was developed to improve patient care of young people on anti psychotic medication. We are developing the Care Programme Approach and Risk Assessments appropriate to the new service. Performance against last year’s measures The measures were as follows:• No children aged 16 or under will be admitted to an adult mental health ward • Collection of baseline data for the number of children admitted to other places (including Mainland Specialist Mental Health Units/Children’s Ward) The good work outlined above has meant that the required target was achieved, with no children aged 16 or under being admitted to an adult mental health ward during 2011/12. However, there were three admissions to Sevenacres, the adult mental health inpatient unit, of children who were aged 17 years. The data relating to numbers of children admitted to other places is outlined in the graph below along with the numbers that were admitted appropriately to the Children’s Ward. This priority will continue to be monitored during 2012/13 as part of the Quality Account process as completion of the specialist facility in the Children’s Ward at St Mary’s Hospital is due in April 2012. 42 3.1.9 Other Performance Information Category A Ambulance response times – April 2011 to March 2012 The Isle of Wight NHS Primary Care Trust has achieved category A ambulance response times in all months except for the 8 minute target in December 2012. The Ambulance service failed to achieve its national target of reaching 75% of Red calls (life threatening) within 8 minutes for the month of December 2011. The actual figure of 74.36% was just 5 calls short for the month. Having carried out a fact finding exercise into why the failure occurred, it is evident that despite the best efforts of all staff concerned and resourcing levels increased to match demand, the volume of Red Calls for the month of December was our highest on record. We had to respond to 86 more Red calls than the previous month of November and 9 more calls than our previous record of 654 calls in October 2011. The total amount of calls responded to by the Island's Ambulance Service in December was 2020 calls. We continue to monitor the patterns of demand and attempt to match resources to meet this, and although the month of Jan 12 continues to challenge us we are confident of reaching the target for this month.” Responsiveness to inpatients’ needs (based on CQC national inpatient survey) Based on the CQC national inpatient survey, for responsiveness to patients’ needs, the trust achieved a score of 67.5. Our local Getting It Right survey data which also captures the relevant responsiveness to needs questions is shown below; this shows that 95% or more patients are satisfied or very satisfied with the care received. Two graphs are included, as the questionnaire was amended from June onwards. 43 3.1.10 HEALTHCARE ASSOCIATED INFECTIONS (HCAI) During 2011/12 NHS Isle of Wight has continued to see improvements in the prevention and management of healthcare associated infections both in the acute hospital and in primary care settings, working with general practitioners to reduce the incidence of Clostridium difficile. Throughout the year performance has been reported on a monthly basis via the performance report and this will continue via the Isle of Wight NHS Trust Board in 2012/13. Meticillin Resistant Staphylococcus Aureus (MRSA) During 2011/12 NHS Isle of Wight has continued its focus on reducing the incidence of healthcare associated infections towards zero in line with the national direction. All patients meeting the national criteria for screening prior to or on admission to St Mary’s Hospital are appropriately screened. During 2011/12 NHS Isle of Wight saw a decrease in the number of patients who developed MRSA bacteraemia whilst in hospital on the Island to 1, during 2010/11 there were 4 cases. Work is ongoing to drive these numbers as low as possible including enhanced blood culture collection training for doctors and nurses, as 44 mentioned full MRSA screening for all patients meeting the national criteria, maintaining high standards of hand hygiene and ensuring best practice in peripheral venous access device management (a cannula or needle entering a vein to provide fluid or medication). There have been no cases of MRSA bacteraemia developing in a patient in the care of St Mary’s Hospital since May 2011. Clostridium difficile 2011/12 saw NHS Isle of Wight report 16 cases of Clostridium difficile infection developing in the care of St Mary’s Hospital, 6 less cases than in 2010/11. The numbers of Clostridium difficile infection occurring within inpatients remained low again during the winter months and ensuring the numbers of this significant healthcare associated infection continue to reduce further remains a key priority for NHS Isle of Wight. The following graph outlines progress made in tackling this infection over the last four years. 45 3.1.11 Complaints and Compliments During 2011/12 the reporting of complaints data has continued to be part of the Chief Nurse’s Quality Report to Board, as well as reported at various other committees as part of performance reports. During the year 299 formal complaints were logged with the Quality Team (305 during 2010/11). The main areas of concern raised in complaints include: • • • • • Clinical care – concerns about diagnosis / treatment. Nursing care – quality of basic nursing care provided. Appointment delays / cancellations in outpatients Communication – failure to communicate / lack of information provided. Staff attitude All complaints within NHS Isle of Wight are investigated and reviewed directly with staff involved, with lessons learnt developed and shared with the wider clinical area. The following positive outcomes and actions have been identified following the review of a selection of complaints in order to prevent similar situations happening again: • • • • • Patient Information leaflets have been reviewed and updated Review of admission paperwork A new transfer criteria has been introduced which will form part of the ward transfer policy A medication timer is now on the ward at all times to ensure Parkinsons medications are given at correct times. Pathology have seconded staff to the team and are looking to recruit in the long term. They have also increased the sample pickups from GP surgeries so that they can increase the number of patients who can have their blood taken at the GP. The numbers of compliments about NHS Isle of Wight services continue to exceed complaints with on average 13 compliments for every one formal complaint received. One of the Non-Executive Directors provides an assurance process to the Board by regularly meeting with the Quality team to review complaints and monitor progress. 3.1.12 Workforce Staff Survey Staff who responded to the NHS staff survey that they agreed or strongly agree that if a friend or relative needed treatment, they would be happy with the standard of care provided by the trust: • Acute 53% (national mean 62%) • Ambulance 45% (national mean 59%) • Mental Health 43% (national mean 59%) Therefore, the average for this organisation is 47% against a national figure of 60% Workforce plan Historically, workforce benchmarking across the NHS South Central area showed that overall Isle of Wight workforce costs are relatively good (seventh lowest out of the 25 organisations surveyed) but also highlighted potential for cost saving. The trust has completely reviewed its annual workforce planning process over the last year, with much 46 closer working with Finance, Performance Information Department, the Programme Management Office and Operational Managers to ensure that the baseline for the forthcoming year is realistic and measurable. This has involved an ongoing review of the workforce component of business plans and the phasing of workforce changes over the year. Key Issues from Directorate Business Plan Directorates have summarised their key workforce drivers arising from service rationalisation or service development in four key areas, as represented by the following graphic. The following are a series of examples from each of the three Clinical Directorates of actions listed under the headings outlined above. Being Fit for the Future All directorates have a renewed focus on Clinical leadership and the development of the lead clinician role as well as the creation of ‘clinical champions’. Programmes are being developed for the enhancement of ‘business skills’ (e.g. Financial awareness, Customer Care), and the engagement of clinicians in the decision-making process. The Leadership Strategy further develops all staff in this area and encourages interdependence, within and between directorates. All directorates envisage more ‘generic’ working and the breaking down and crossover of traditional professional and clinical boundaries. Initiatives such as ‘Let’s Show We Care’ will be used to create a renewed focus on quality and professional behaviour. New skills will also be developed in areas such as the handling of Trauma. Other programmes of work have included the significant reorganisation of the district nursing service following a number of reviews and consultation with key stakeholders to provide a modern and proactive service. Modernising Roles Each Directorate has examples of skill mix and different more appropriate models of delivery. Initiatives range from, the increased use of Apprentices and Volunteers, more nurse-led clinics, the development of the role of Physicians Assistant to free up junior medical staff to provide more effective cover at weekends, the creation of more Advanced Nurse and AHP practitioners, multidisciplinary working across Rehabilitation and Reablement (learning from the Community Stroke Rehabilitation model), and skill mix reviews in Maternity, Outpatients and Community Mental Health Services. 47 Workforce Productivity To support the early focus on productivity in the Strategic Workforce review, initiatives include the development of a Communications centre to support the ‘Single Point of Contact for Patients’, Pathology Service modernisation, the creation of a Trauma Unit and the ‘Hospital at night Model’. Other initiatives are the development of Community AHPs to support seven day discharge and the development of Diagnostic Imaging staff to support seven day diagnostics. A model adapted from services in Bath is being used to focus junior medical staff on out of hours and weekend work and the implications of a ‘Ward Based Consultant’ is being investigated. A ‘Single Front Door’ approach is being developed with the co-location of the Emergency department and the Beacon centre, with closer working with the Medical Assessment and Admissions Unit being planned. Telehealth is being explored for use in Prisons to reduce the need for accompanied visits to Hospital and Dementia service are being reviewed to create an outreach service to support and enable carers in the home environment. Ensuring the Basics Directorates will maintain a focus on getting the basics right. Mandatory Training and appraisal targets will be reinforced and new models of succession planning incorporated into strategy. There will be a continued highlight on the control of short and long term ill health and a renewed focus on communication, development and consequently the ownership and accountability for each role within the organisation and its contribution to service delivery. Through the Health and Wellbeing Strategy and action plan, staff will be supported to develop healthier lifestyles and the Occupational health Department will continue to advise and support back to work after periods of ill health. The above four areas highlight the breadth of initiatives to support the organisations journey to sustainability and foundation trust status, whilst maintaining a commitment to the vision of ‘Quality Care for everyone every time’. In addition to all of the above, a variety of ‘back office efficiency and management optimisation’ schemes are complete or under review: • A comprehensive review of corporate functions has led to the production of detailed SLAs for corporate services, costed and agreed with both Provider and Commissioner • The 100% rollout of the E-Rostering Module • The simplification and standardisation of policies and procedures (E-CRB, Eexpenses, electronic case management, Training Manager Pro 4) • A review of manager self-service for data held on the Electronic Staff Record is being project planned for the second half of the year. Workforce data is monitored through the workforce plan, weekly and monthly key performance indicator monitoring, the integration of data with the Performance Management structure and regular reports to the Trust Board. The business planning process is being revised by the new Programme Management Office to ensure that the three elements of finance, activity and workforce are clearly aligned at the point of plan approval. In addition to the above the Trust has commissioned Conrane Consulting to review the strategic workforce planning process within the Trust and draw comparisons with the Trust workforce baseline and other NHS organisations. This work is scheduled to finish early in the new financial year. The initial analysis suggests that the baseline numbers are comparable to a national average for a population of the size of the Isle of Wight. Further work is being undertaken on productivity measures and a more detailed analysis being 48 compiled in relation to the Medical Assessment and Admissions Unit and Emergency Department Services. 3.1.13 Baseline Equality Delivery System Self Assessment In November 2011 the NHS Equality and Diversity Council launched the Equality Delivery System (EDS); a framework it has developed to assist NHS organisations complies with equality legislation. The Trust has completed a baseline assessment against the four EDS goals. The assessment has involved gathering evidence such as reports, surveys and complaints and working with patients and service users to help us arrive at an initial assessment. Goal Rating 1. Better health outcomes for all Achieving 2. Improved patient access and experience Developing 3. Empowered, engaged and wellsupported staff Achieving 4. Inclusive leadership at all levels Developing Engagement and involvement with a good range different of people with differing needs Engagement and involvement with a limited range of people with differing needs Engagement and involvement with a good range different of people with differing needs Engagement and involvement with a limited range of people with differing needs This initial assessment has helped us develop our Equality Objectives which can be found at http://195.217.160.2/index.asp?record=2049 49 3.2 Statements provided by Commissioning PCT, LINks or OSCs Commissioner Statement in response to the Provider Quality Account 2011/2012 Isle of Wight Clinical Commissioning Group (CCG) and Isle of Wight NHS PCT Commissioners welcomed the opportunity to participate in the governance ‘sign-off’ process and provide a statement in response to the presented Quality Account. The Quality Account was widely shared with representatives of the Clinical Commissioning Group and Senior Commissioners for their comments. ‘The provider’s unique position is recognised; there is a challenge in representing the broad range of services provided - Acute, Mental Health and Learning Disability, Community and Ambulance Services - within a single Quality Account. Whilst the account this year focuses predominantly on acute and mental health and learning disability services, it is pleasing to see the emphasis on patient experience, through a range of quality improvement priorities, reflecting both local and national priorities and the interests of the Clinical Commissioning Group. The Provider has demonstrated quality improvement in the priorities it set out in last year’s Quality Account and has chosen to continue to drive up quality in some of these areas in the coming year, for example ‘prevention and management of pressure ulcers’. Last year Commissioners suggested a focus on ‘Essence of Care’ and whether it could be introduced into the audit programme by the Provider and reflected in the Quality Account for this year. Commissioners are reassured to see the ‘improving record keeping’ priority, as it is felt this will impact positively on care planning and basic care. There has been notable improvement in the achievement of Commissioning for Quality Incentive Schemes (CQUINS), demonstrating quality improvements in all but two areas of health care agreed between commissioner and provider. Whilst the Provider has not detailed how under-achievement in these areas will be addressed, one element - end of life care and the use of the Liverpool Care Pathway - has been agreed as a quality requirement within the 2012/13 contract, and the other – smoking status and brief intervention – has been agreed as a revised Health Promotion CQUIN. The Commissioners would have found a headline summary of the 2012/13 CQUIN schemes informative. Quality Account priorities, together with CQUINS and other quality outcomes in contracts, will be monitored in detail by Commissioners, as part of the performance management of the Provider through monthly Clinical Quality Review Meetings. The robustness of the Provider’s clinical audit process appears to be evidenced by the Provider’s level of participation in audits and level of engagement of health care staff undertaking audits locally. Commissioners would however be interested to understand the Provider’s process for reviewing national audits, as only 7 of the 41 national audits appear to have been reviewed by the provider. In next year’s Quality Account the Commissioner would also like to suggest the inclusion of the outcomes and learning from the review of serious incidents and ‘Never Events’ and more detail of organisational learning as a result of investigating complaints. The Commissioner understands that the quality of patient care can be linked to the health and well being of staff. Whilst workforce is included in the Quality Account there is limited reference to the key findings of the most recent staff survey. Overall, Commissioners and representatives from Isle of Wight Clinical Commissioning Group would commend the Quality Report as a fair reflection of the Provider's positive achievement across the quality agenda and the high level of commitment and effort across a diverse organisation to constantly improve the quality of services provided. 50 Statement by the Chairman of the Health and Community Wellbeing Scrutiny panel for the Quality Account 2012 The past year has been a period of further significant structural change in the health service. Despite these the quality account demonstrates that the needs of patients are not overlooked and it remains the aim of the Trust to deliver a high quality service. The document enables all stakeholders to be aware of the Trust’s priorities for the coming year. Central to these are the views and experiences of patients together with performance monitoring. The information contained within the Joint Strategic Needs Assessment should also be used as an important tool in helping to identify key priorities. The scrutiny panel is building a stronger working relationship with the Care Quality Commission (CQC). It was fortunate to have a local compliance officer at its meeting when the Trust reported on the findings of the CQC after its inspection of St Mary’s Hospital. This relationship will assist the scrutiny panel in focussing on peoples experiences of health care and identify where improvements are required. During the past year the scrutiny panel also met with the Medical Director at St Mary’s to discuss the national review of mortality rates and concerns about the Island’s profile. Members were assured that residents should be confident that they were not at more risk of dying at St Mary’s hospital than any other hospital. The panel intends to follow up on this item during 2012/13. The panel will continue to utilise the quality account to identify where it needs to take a wider overview of social care arrangements. Whilst recognising that collecting data on performance is important to identify progress on key actions the ultimate test of a good service is that of the meeting the needs and expectations of patients. The panel will work with all relevant partner organisations to keep the individual as the main priority of service delivery. Councillor Margaret Webster Chairman Isle of Wight Council’s Health and Community Wellbeing Scrutiny Panel Statement by the Chairman of the IW Local Involvement Network (LINk) Stewardship Group The Isle of Wight LINk is pleased that NHS Isle of Wight’s Quality Account for the coming year reflects several of its workplan priorities. The focus on Mental Health in several areas is welcomed particularly the aim to improve WRAP and contingency planning to decrease the 28 day re-admission rate. The improvement in stroke services over the last 12 months has been observed on 2 visits by the LINk’s Enter & View Panel. The LINk looks forward to seeing the successful launch of the long delayed Thrombolysis service in acute stroke on a follow up visit later in the year. The public and providers of services have said that discharge of vulnerable patients from the hospital late at night and transport (including car parking) continue to be key issues. The LINk would like to continue its work with NHS Isle of Wight to identify solutions to these areas. 51 The IW LINk would like to extend its appreciation to the overwhelmingly positive and professional approach of hospital staff working in uncertain and changing environment, and looks forward to doing so in its transition year to Local Healthwatch. Chris Orchin IW Local Involvement Network (LINk) Stewardship Group Chair. 52 3.3 Statement of Directors’ Responsibilities The directors are required under the Health Act 2009 and the National Health Service (Quality Accounts) Regulations 2010 to prepare Quality Accounts for each financial year. The Department of Health has issued guidance on the form and content of annual Quality Accounts (which incorporates the above legal requirements in the Health Act 2009 and the National Health Service (Quality Accounts) Regulations 2010(as amended by the National Health Service(Quality Accounts) Amendment Regulations 2011). In preparing the Quality Account, directors are required to take steps to satisfy themselves that: • the Quality Report presents a balanced picture of the trust’s performance over the period covered; • the performance information reported in the Quality Account is reliable and accurate; • there are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice; • the data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, and is subject to appropriate scrutiny and review; and • the Quality Account has been prepared in accordance with Department of Health Guidance The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Account. By order of the Board NB: sign and date in any colour ink except black ………….......Date............................................................. Danny Fisher Chairman, Isle of Wight NHS Primary Care Trust (to 31st March 2012) / Isle of Wight NHS Trust (from 1st April 2012) ......................Date............................................................ Kevin Flynn, Chief Executive Isle of Wight NHS Trust (from 1st April 2012) ......................Date............................................................ Debbie Fleming, Chief Executive, Isle of Wight NHS Primary Care Trust 53 3.4 Changes made to the Final Version of the Quality Account – following feedback Following consultation with stakeholders on the draft Quality Account, the following changes have been made:- Section 3.1.1 Identification and response to the deteriorating patient and hospital at night table 4 was updated to include the number of admissions alongside the number of readmissions. Where acronyms/abbreviations were used, full details of the meanings were included as appropriate. Section 2.1.7 Learning Disabilities & Dementia, part B - Additional wording added to last paragraph 'a passport type document supporting person centred care' Section 2.2.3 Patient Safety Walkrounds (2nd paragraph) - addition of wording to form last sentence - 'The Head of Quality – Commissioning for the PCT Cluster also attends some of these walkrounds.' Section 3.1.2 Prevention of Venous Thromboembolism - 2nd paragraph - additional of wording to form last sentence:- 'This also forms a national CQUIN scheme for 2012/13.' Section 2.1.7 Learning Disabilities & Dementia (A: Improving the experience of people with a learning disability using St Mary’s Hospital) - rewording of last paragraph to read ‘During 2012/13 the Isle of Wight NHS Trust will review the support provided to in-patients with a learning disability to ensure their care is appropriate and necessary adjustments are made to support the delivery of effective care. Monitoring appropriate medicines management relating to psychotropic and anti-epileptic medication for people with learning disabilities admitted to St Mary’s Hospital will also be undertaken to ensure this is in line with best practice guidance.’ Section 2.1.7 Learning Disabilities & Dementia (Improving the experience of people with a learning disability using St Mary’s Hospital) - rewording of Measure 1: All in-patients with a learning disability who require adjustments in their care will receive support from the Liaison Nurse or CLDN. Section 2.1.9 Reduction in 28 Day Readmissions in Mental Health - Measure 1, bullet 3: 'Realistic' changed to 'Appropriate' contingency plans to be agreed with patient 3.5 How to Provide Feedback on the Account This important document sets out how we continue to improve the quality of the services we provide. Your Views on Quality We welcome your views and suggestions on our Quality Priorities for 2012/13 set out in Part 2 of this Quality Account. We welcome feedback at any time on our Quality Account. This can be sent to the Quality Team, St. Mary’s Hospital, Parkhurst Road, Newport, Isle of Wight, PO30 5TG or emailed to quality@iow.nhs.uk. You can read more about the national requirements for Quality Accounts on the NHS Choices or Department of Health websites. You can download a copy of this Quality Account from www.iow.nhs.uk (Publications section). 54 APPENDIX 1 Stakeholders engaged in the development of the Quality Account Chief Nurse and Director of Infection Prevention and Control Chief Executive Business and Projects Manager – Quality and Clinical Standards Directorate Provider Quality Manager Head of Communications Communications Assistant Patient’s Council Representatives Local Involvement Networks (LINks) Representatives Isle of Wight Council’s Health and Community Wellbeing Scrutiny Panel Representatives Chief Operating Officer Non Executive Directors Associate Director – Acute Clinical Directorate Associate Director – Planned Clinical Directorate Associate Director – Community Health Clinical Directorate Head of Clinical Services - Acute Clinical Directorate Head of Clinical Services – Planned Clinical Directorate Head of Clinical Services - Community Health Clinical Directorate Clinical Director / Consultant - Acute Clinical Directorate Clinical Director / Consultant - Planned Clinical Directorate Clinical Director / Consultant– Community Health Clinical Directorate Senior Nurse Manager – Mental Health and Learning Disabilities Directorate Head of Governance and Assurance Practice Development Co-ordinators Medical Director Quality Manager Quality Assurance Lead Head of Information Management Information Officer Performance Information Department Business Co-ordinator to the Chief Operating Officer Senior Finance Manager, PbR and Costing Director of Finance and IM&T Director of Human Resources and Organisational Development Senior Human Resources Manager Equality and Diversity Lead Programme Director, Transition Team Leader /Senior Clinician - Community CAMHS Clinical Nurse Specialist for Nutrition and Tissue Viability Infection Prevention and Control Team IV Nurse Specialist Lead Nurse and Advance Nurse Practitioner / Critical Care Outreach Service Research Management and Governance Manager Head of Prison Healthcare Business and Performance Manager – Mental Health and Learning Disabilities Modern Matron – Community Health Clinical Directorate Modern Matron – Acute Clinical Directorate Matrons Action Group Nursing and Midwifery Committee members Clinical Nurse Leaders Forum members Audit Committee Members Hospital Medical Staff Committee members Quality and Patient Safety Committee members 55