Quality Account 2010/11 June 2011
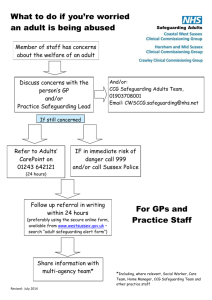
advertisement

Quality Account 2010/11 June 2011 Contents Part 1 Interim Chief Executive’s Statement Page 4 Introduction Page 6 Part 2 Improvement Priority 1: Patient Safety Page 8 Improvement Priority 2: Clinical Effectiveness Page 10 Improvement Priority 3: Patient Experience Page 12 Improvement Priority 4 – Staff Experience Page 13 Review of services Participation in Clinical Audits Page 14 Goals Agreed with our Commissioners Page 17 Statements form the Care Quality Commission Page 20 Data Quality Page 21 Part 3 Review of Quality Performance Page 24 Clinical Effectiveness – Productive Ward Page 24 Patient experience – Complaints Management Page 25 Patient Experience – Patient Environment Action Team Page 26 Safety – Infection Control Page 27 Conclusion Page 28 2 Part 1 A statement on quality from the Interim Chief Executive Statement from Ralph W. McCormack, Interim Chief Executive, Outer North East London Community Services (ONEL CS) I am delighted to present the first Quality Account produced by ONEL CS. Its purpose is to explain the quality of care we provide and how we are seeking to improve quality. It contains a review of the quality of services provided by the Trust in the financial year 2010/11 and an outline of our plans to further improve quality in 2011/12. In the report High Quality Care for All published in June 2008 Lord Darzi defines quality as comprising three domains; safety, effectiveness and patient experience. ONEL CS is committed to increasing the standard of quality through improving the safety and effectiveness of our services and the experience of our service users and carers whilst using them. We have successfully implemented a web based incident reporting management system (DatixWeb) which links to the National Reporting and Learning System (NRLS). Our incident reporting processes have enabled us to develop a comprehensive quarterly governance report which provides data on trends in, for example, patient and staff safety incidents. In the first six months of 2010/11 (latest available data from the NRLS) we were among the top primary care organizations with inpatient facilities in the NHS London region for reporting patient safety incidents. The majority of these (90.2%) resulted in low or no harm to the patients concerned. In 2011-12 it is our intention to continue to improve incident reporting rates and to implement the use of the Global trigger Tool in our inpatient services. This tool investigates randomly selected patient health records in order to identify whether undetected incidents have occurred during an episode of care. The organization will learn from these findings to improve the care and treatment for patients in the future. We are pleased to report that there have not been any ‘never events’ reported in ONEL CS in 2010/11. Never events will be a key priority in 2011/12 and we will continue to raise awareness of the expanded list of events and the requirement to report them throughout 2011/12. There has been an intense focus on safeguarding activity across the organisation’s services throughout 2010/11. This commenced with a comprehensive scoping exercise the outcome of which was the development of a high level action plan which has been implemented to ensure a robust assurance framework is in place as well as clear processes to monitor learning from incidents and sharing of best practice. ONEL CS has placed particular emphasis on ensuring that policies and procedures are in place and that staff have undertaken safeguarding training to an appropriate level. A robust plan is in place to improve the training uptake further in 2011/12. 4 A new Visible Leadership programme was been introduced in 2010/11. ONEL CS believes that creating a strong organisational safety culture is a fundamental responsibility of leaders and that visible leadership activity is needed to help shape and reinforce this. It is our intention to roll out the Visible Leadership programme to include community settings during 2011/12. In 2010/11 1,551 patients completed a patient satisfaction questionnaire. 98.5 per cent of these patients felt that they were treated with dignity and respect. We will continue to survey users of all our services during 2011/12. Outer North East London Community Services has maintained an excellent record of performance in preventing and controlling healthcare associated infections. During 2010/11, no patients contracted a Meticillin Resistant Staphylococcus aureus (MRSA) blood stream infection (known as a bacteraemia) in any of our inpatient settings. I can confirm that to the best of my knowledge the information in this Quality Account is accurate and represents our performance in 2010-11 and our priorities for continuously improving quality in 2011/12 Ralph W. McCormack Interim Chief Executive 5 1. Introduction Welcome to our inaugural Quality Account. ONEL CS is the largest community provider in London with a turnover of approximately £90 million per annum, a staff base of over 1,600 people delivering services across the London Boroughs of Havering, Redbridge and Waltham Forest. The organisation serves a population of approximately 750,000 people with a significant variation in prosperity, diversity and health issues across the geography. Certain services such as those provided from the Long Term Conditions Centre (formerly the Disablement Services Centre) provide for a much wider geographical area. Full details of our services are available on our website: http://www.onelcommunityservices.nhs.uk/. Community based services are at the heart of a modern and flexible NHS. As the main provider of community services across North East London Improving quality for our patients and for the public we serve is fundamental to us and at the heart of everything we do. Quality accounts are annual reports to the public from providers of NHS health services about the quality of services provided. They aim to enhance the accountability of the provider to the public. Ordinarily we would publish a Quality Account annually to assure our service users, carers, commissioners, and the wider community of our commitment to quality in all that we do. However, ONEL CS is in the process of transferring to a foundation trust and is unlikely to publish any further Quality Accounts in its own right. The transfer is expected to complete in the coming months and, once finalised, we will contribute to the Quality Account of our new organisation. In the report High Quality Care for All published in June 2008 Lord Darzi defines quality as comprising three domains; safety, effectiveness and patient experience. ONEL CS is committed to increasing the standard of quality through improving the safety and effectiveness of our services and the experience of our service users and carers whilst using them. 6 Part 2 Priorities for improvement and Statements relating to the quality of services provided 2. Priorities for Improvement 2.1 Priority 1 – Patient Safety The Health and Social Care Bill 2011 introduced for the first time a defined legal duty for the NHS to continuously improve patient safety. ONEL CS intends to contribute to this commitment in 2011/12 by concentrating on the following areas: 2.1.1 Patient Safety Incidents We have successfully implemented a web based incident reporting management system (DatixWeb) which links to the National Reporting and Learning System (NRLS). Our incident reporting processes have enabled us to develop a comprehensive quarterly governance report which provides data on trends in, for example, patient and staff safety incidents. In the first six months of 2010/11 (latest available data from the NRLS) we were among the top community organisations with inpatient facilities in the NHS London region for reporting patient safety incidents. The majority of these (90.2%) resulted in low or no harm to the patients concerned. We see this, together with a high level of reporting, as evidence of an open reporting culture. We thank and commend our staff for ensuring that accidents, incidents and near misses are reported so that we can learn from such incidents and make the care we provide safer. In 2011-12 it is our intention to continue to improve incident reporting rates and to implement the use of the Global trigger Tool in our inpatient services. This tool investigates randomly selected patient health records in order to identify whether undetected incidents have occurred during an episode of care, and in studies has identified ten times more serious incidents than other methods used to detect adverse incidents in hospital care (Classen D C et al 2011). The organisation will learn from these findings to improve the care and treatment for patients in the future. 2.1.2 Never Events Never Events are serious, preventable patient safety incidents that should not occur if the available preventative measures have been implemented. ONEL CS has implemented the national never event reporting process with our Associate Directors directly accountable for any never events occurring in their area of responsibility and commissioners recovering the entire cost of any episode of care in which a never event occurred. The number of never events has been expanded to 22 in 2011/12, from 8 in previous years although some are not relevant to the services offered by ONEL CS. The never events that could occur in services provided by ONEL CS are: 8 • • • • • • • • • • • • • • • • Wrong site surgery (existing) Wrongly prepared high-risk injectable medication (new) Maladministration of potassium-containing solutions (modified) Wrong route administration of oral/enteral treatment (new) Maladministration of insulin (new) Overdose of midazolam during conscious sedation (new) Opioid overdose of an opioid-naïve patient (new) Suicide using non-collapsible rails (existing) Falls from unrestricted windows (new) Entrapment in bedrails (new) Transfusion of ABO-incompatible blood components (new) Misplaced naso- or oro-gastric tubes (modified) Failure to monitor and respond to oxygen saturation (new) Air embolism (new) Misidentification of patients (new) Severe scalding of patients (new) We are pleased to report that there have not been any never events reported in ONEL CS in 2010/11. Never events will be a key priority in 2011/12 and we will continue to raise awareness of the expanded list of events and the requirement to report them throughout 2011/12. 2.1.3 Serious Incidents ONEL CS is committed to providing a safe environment to care for patients. We follow national guidance on keeping our patients safe and are committed to staff training and learning from incidents. When a serious incident does occur, ONEL CS has a responsibility to ensure there are systematic measures in place for safeguarding people, property, resources and reputation. This includes responsibility to learn from these incidents to minimise the risk of them happening again. A serious incident requiring investigation is defined as an incident that occurred in relation to NHS-funded services and care resulting in: unexpected or avoidable death; serious harm; a scenario that prevents or threatens to prevent a provider organisation’s ability to continue to deliver healthcare services; allegations of abuse; adverse media coverage; a never event. During 2010-11 ONEL CS reported 58 serious incidents to NHS London, compared with eight in 2009/10. Reasons behind this increase include: • Recent changes to the reporting criteria for serious incidents under which organisations are now required to report additional categories of incidents, such as grade three and four pressure ulcers. Grade 3 ulcers are superficial ulcers with full thickness skin loss and damage to the underlying tissues but not extending further. Grade 4 ulcers are deep ulcers with 9 damage to the muscle, bone or other underlying structures. These ulcers are often painful and affect quality of life. • ONEL CS’ increasing emphasis on patient safety and quality, with a heightened awareness of the need to report incidents amongst staff across the organisation. Excluding pressure ulcers the number of serious incidents reported to NHS London by ONEL CS in 2010/11 was unchanged from 2009/10 at eight. During 2011-12 ONEL CS will be undertaking further work to identify trends and issues related to incidents. 2.2 Priority 2 - Clinical Effectiveness 2.2.1 Venous Thromboembolism (VTE): Reducing the Risk Following the issue of guidance relating to VTE, simply blood clots in veins, by the National Institute for Health and Clinical Excellence (NICE) ONEL CS has been implementing the recommendations of this guidance in order to reduce the risk of patients getting a deep vein thrombosis or pulmonary embolism when admitted to our inpatient facilities. Reducing this risk is a national goal and ONEL CS is working hard to ensure that all of the guidance is fully implemented over the coming year. As is the case with other NICE guidance, the information has been circulated throughout the organisation and reported levels of compliance and supporting documentary evidence is collated by the governance department to provide assurance of implementation. Assessment of the risks of VTE is relevant to the majority of our inpatients therefore the first line of action will be to audit the current implementation of the guidance and then prepare an action plan for the NICE best practice to be rolled out. An audit of patients has demonstrated that our patients are receiving care in line with this guidance and received all necessary interventions. 2.2.2 Safeguarding There has been an intense focus on safeguarding activity across the organisation’s services throughout 20010/11. This commenced with a comprehensive scoping exercise the outcome of which was the development of a high level action plan which has been implemented to ensure a robust assurance framework is in place as well as clear processes to monitor learning from incidents and sharing of best practice. A Safeguarding Committee has been established as a formal sub-group of the Governance and Standards Committee. The group aims to provide strategic monitoring of all safeguarding issues. 10 ONEL CS has placed particular emphasis on ensuring that policies and procedures are in place and that staff have undertaken safeguarding training to an appropriate level. How we are performing training our staff is given in the tables below. A robust plan is in place to improve the training uptake further in 2011/12. Course Staff Group Frequency of attendance % staff trained by 31.03.2011 Safeguarding Vulnerable Adults All Clinical staff in direct contact with adults Every 3 years 92% Course Staff Group Frequency of attendance % staff trained by 31.03.2011 Safeguarding Children Level 1 Training All Non Clinical Staff working in healthcare settings Every 3 years 76% Course Staff Group Frequency of attendance % staff trained by 31.03.2011 Safeguarding Children Level 2 Training All Clinical Staff Every 3 years 34% Course Staff Group Frequency of attendance % staff trained by 31.03.2011 Course Staff Group Frequency of attendance % staff trained by 31.03.2011 Safeguarding Children Level 3 Training (as previously reported prior to the New Safeguarding Children Strategy) All clinical staff working with children, young people and/or their parents/carers and who can potentially contribute to assessing, planning, intervening and evaluating the needs of a child or young person and parenting capacity where there are safeguarding/child protection concerns One session to be attended every three years 51% Safeguarding Children Level 3 Training (Following implementation of Safeguarding Children Strategy) All clinical staff working with children, young people and/or their parents/carers and who can potentially contribute to assessing, planning, intervening and evaluating the needs of a child or young person and parenting capacity where there are safeguarding/child protection concerns Yearly - Every Year professionals must undertake a minimum of one level 3 training session facilitated by ONEL CS and one relevant LSCB training session 6%. This figure represents the staff who have been trained following the new requirements which have only recently been published. The new requirements must be implemented by 2013. A new Safeguarding Children Training Strategy has been implemented. The strategy outlines the Safeguarding Children training requirements for all staff and has been developed as recommended by the Safeguarding Children and Young People: roles and competences for health care staff Intercollegiate Document (September 2010). This is to be implemented within three years. Therefore ONEL CS will work towards these requirements over a period of 12 months. Reporting for level 3 will continue to be provided for the previous requirements and the new requirements during this time. 11 A Safeguarding and Dignity champion model has been rolled out to ensure safeguarding is embedded in practice. 2.3 Priority 3 - Patient Experience 2.3.1 Visible Leadership A new Visible Leadership programme was been introduced in 2010/11 ONEL CS believes that creating a strong organisational safety culture is a fundamental responsibility of leaders and that visible leadership activity is needed to help shape and reinforce this. The programme takes the Associate Director of Quality and Standards/Lead Nurse and other members of the senior nursing team out onto the wards on a regular basis. This enables them to have first hand knowledge of issues affecting patients and staff and to troubleshoot them there and then. Time is spent looking at key indicators of patient care, including pressure ulcer risk assessment, nutrition assessment, patient observations, administration of medicines, nutritional assessment, fluid management, hand hygiene, environment, intravenous cannulation, privacy and respect and record keeping. Audits of the key indicators are carried out at each visit and results fed back to the wards and used to raise standards The programme has been received positively by the wards, who have welcomed the additional support from senior nurses. Standards of care are improving and ideas shared between wards and sites to improve patient experience. It is our intention to roll out the Visible Leadership programme to include community settings during 2011/12. 2.3.2 Patient Surveys The Patients Association’s report ‘Listen to Patients, Speak up for Change’ highlighted the issue of poor dignity and nutrition in elderly care and, more recently, led to the CQC dignity and nutrition inspection programme in 100 acute hospitals across the country. Patient surveys are of great importance to ONEL CS and are a barometer of how good a job we are doing in making sure our patients have the best possible experience when accessing our services. In 2010/11 1,551 patients completed a patient satisfaction questionnaire. 98.5 per cent of those patients who returned their questionnaires felt that they were treated with dignity and respect. We will continue to survey users of all our services during 2011/12. 12 2.4 Priority 4 – Staff Experience Improving and measuring staff satisfaction is a very important part of ensuring that we can provide the best care and experience for our patients. ONEL CS participates in the NHS National Staff Survey each year, and the results for the 2010 survey are summarised below: In the 2010 survey, we scored amongst the best 20% of similar organisations in England for: • Percentage of staff feeling satisfied with the quality of work and patient care they are able to deliver • Percentage of staff working extra hours • Percentage of staff appraised in last 12 months • Percentage of staff appraised with personal development plans in last 12 months • Percentage of staff reporting errors, near misses or incidents witnessed in the last month • Percentage of staff having equality and diversity training in last 12 months However, we also scored amongst the lowest 20% of similar organisations in England with worsening performance, when compared to 2009, in the following areas: • Percentage of staff feeling valued by their work colleagues • Support from immediate managers • Staff motivation at work • Percentage of staff believing the trust provides equal opportunities for career progression or promotion The survey questions are divided into four separate categories and we are concerned that many of our low scores fall into the following categories: • To provide all staff with clear roles, responsibilities and rewarding jobs. • To provide support and opportunities for staff to maintain their health, well­ being and safety 13 • To engage staff in decisions that affect them, the services they provide and empower them to put forward ways to deliver better and safer services In 2011/12 we intend to examine the issues raised by the survey results in more detail and to establish the reasons behind them although it is anticipated that a prolonged period of organisational change will emerge as one important factor. We will also consider how we can make improvements which will have a real impact on staff morale, and we will involve different staff groups to help us design action plans to deliver these improvements. 2.5 Review of Services During 2010/11 Outer North East London Community Services provided and/or sub-contracted 67 NHS services. Outer North East London Community Services has reviewed all the data available to them on the quality of care in 100% of these NHS services. The income generated by the NHS services reviewed in 2010/11 represents 97 percent of the total income generated from the provision of NHS Services by Outer North East London Community Services for 2010/11. 2.6 Participation in Clinical Audits During 2010/11, three national clinical audits and no national confidential enquiries covered NHS services that Outer North East London Community Services provides. During that period Outer North East London Community Services participated in 67% clinical audits and no national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that Outer North East London Community Services was eligible to participate in during 2010/11 are as follows: • Falls and Bone Health Audit • Continence Care Audit The national clinical audits and national confidential enquiries that Outer North East London Community Services participated in, and for which data collection was completed during 2010/11, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. 14 Audit Falls and Bone Health Audit Continence Care Audit % Cases Submitted 50% (100% of eligible patients) 100% The reports of 2 national clinical audits were reviewed by the provider in 2010/11 and Outer North East London Community Services intends to take/has taken the following actions to improve the quality of healthcare provided: Falls and Bone Health Audit • Secured funding for a falls coordinator • Development of a Falls Policy that uses a pragmatic prompting risk assessment template • Development of a falls record sheet to be completed by ward doctors • Review of nurse staffing levels at night and weekends • Raise the profile of the Day Hospital Falls Service • Enhance incident reporting of falls • Ensure systematic falls assessment on admission for all patients • Review of patient’s care plan and medication following a fall Continence Care Audit • Annual review of all long term users of the Continence service • Provide basic training and continence awareness to all professionals including healthcare • Clarify referral pathways for continence services • Introduce simplified assessment for continence services The reports of 130 local clinical audits were reviewed by us in 2010/11 and Outer North East London Community Services intends to take/has taken the following selected actions to improve the quality of healthcare provided. National Patient Safety Week – Screen it out audit • Awareness of the use of nutritional screening in promoting wound healing and preventing pressure damage has been raised. • Introduction of the Malnutrition Universal Screening Tool and training package. • Consultation with the District Nursing teams in Redbridge and Waltham Forest to ensure a consistent approach to nutritional screening will take place. • The Visible Leadership ward round will audit nutritional screening during its visits 15 Dietetic Audit – Havering • Dieticians to explain to patients in more detail the reason why the patient has been referred to see a Dietitian. • Trialling the Expectations of Diet Therapy letter with the booked admission letter that we currently send to community patients asking patients to ring in and book an appointment at a time and date suitable to them. Productive Ward • Refurbished wards to enhance the privacy and dignity of the patients and to eradicate same sex accommodation. • Modified Early Warning Score (MEWs) policy introduced and all staff now using the MEWs scoring system (a simple, physiological score that may allow improvement in the quality and safety of management provided to patients) • Process mapping patients admission procedure Blood Transfusion • Blood transfusion care plan reviewed • Blood transfusion leaflet to be given to patients receiving transfusion Reducing Harm from Omitted/Delayed Medicines (NPSA 009) • • • • Introduction of critical medicines guideline Training programme Parkinson’s UK Campaign ‘Get it on Time’ Recording by prescribers of patient’s weight on the drug chart where appropriate Harold Hill Clinic – Essence of Care Audit of Safety • • • • • • • Person running the clinic takes responsibility for orientating each patient. Devised generic post operative care plans Training for staff to identify substance abuse Privacy and Dignity policy Open up the waiting area so staff can see patients and vice versa Screens in treatment room Make Patient Advice and Liaison Service leaflets available in the waiting areas Liverpool Care Pathway (LCP) in respect of end of life care Audit • Reviewed current document with palliative care locality links • Lead nurse to continue visiting clinics to provide education on end of life issues and using the LCP. • Collected information as to why LCP was not used in some cases 16 • Investigated possible reasons why LCP not used in some localities • Protocol for what constitutes a Multi-Disciplinary Team in the case of implementing the LCP • LCP documentation review disseminated to all staff. • To ensure all staff are aware of the Department of Work and Pensions leaflet and how to obtain them if they run out. Syringe Driver Audit • Significant improvement in the prescribing and administering of end of life drugs. • All clinics are using the same documentation regarding administration and authorisation of medications. • Continue to purchase syringe driver training from St Francis hospice. Other Topics • Better management and provision of lone worker devices for staff • Small identification wristbands procured for patients with small wrists • Staff were made aware that patients with a known risk need to wear a red wristband as well as patients with known allergies • Standardise the format for recording on patient wristbands • Promote awareness that among staff that patients should only be wearing one wristband • Enhance incident reporting in relation to missing notes/patient information when patients are transferred from other hospitals • Purchase of new commodes for one in-patient unit • Re-education of staff with regard to cleaning commodes. • Relocation of Havering continence service to improve privacy and dignity 2.7 Goals Agreed With Our Commissioners A proportion of Outer North East London Community Services income in 2010/11 was conditional on achieving quality improvement and innovation goals agreed between Outer North East London Community Services and any person or body they entered into a contract, agreement or arrangement with for the provision of NHS services, through the Commissioning for Quality and Innovation (CQUIN) payment framework. Common quality improvement and innovation goals were agreed with our three main commissioners for 2010/11: • The implementation by ONEL CS Adult Service community nursing of personalised care plans for those with long term conditions to enhance management in the community and reduce hospital admissions. - reduction in falls in NHS/other provided care 17 - reduction in catheter related Urinary Tract Infections - reduction in pressure sores - reduction in dehydration • The implementation across community nursing of the Liverpool Care pathway in respect of End of Life Care with a high threshold to be set in respect of the numbers of patients dying on the Liverpool Care pathway. • The implementation of personalised care plans for those on the End of Life Care pathway with the care plan identifying preferred place of care. The scheme to incentivise the wide application of preferred place of care and measure and reward an excellence performance defined by high rates of death in preferred place of care. • The application of the acute CQUIN in respect of thromboembolism to ONEL CS community beds. Further details are available electronically at: http://www.institute.nhs.uk/commissioning/pct_portal/2010%1011_cquin_sche mes_in_london.html In addition to our CQUIN goals a range of key performance indicators (KPI) were agreed separately with our three main commissioners for 2010/11. They were monitored on a monthly and quarterly basis and reported back to the commissioners at Monthly Contract/Performance Meetings: Adult Services Generic KPIs • • • • • • • • • • • Ethnicity Monitoring Number of Avoided Admissions Access (18 weeks from general practitioner referral to treatment) Safeguarding: Staff training Safeguarding: Case Management Personalised Care Planning Improving Productivity Service User Experience 100% of patients have received a care plan Achievement of two agreed Essence of Care Standards 100% of staff have received Adult Safeguarding training Dentistry • • • • Change in decayed, missing & filled teeth levels in 5 year olds Equity of access to dental health services Change in oral health knowledge and skills Change in number of nursing homes with oral health care plans 18 • In-service training for social care staff • Reducing Inequalities Inpatients • • • • Number of delayed discharges Number of avoided admissions Number of very high intensity users Unplanned admissions End of Life Care • 75% of End of Life Care patients on Liverpool Care Plan • 95% of patients with life limiting conditions have a recorded preferred place of death District Nurse/Community Matrons • Venous leg ulcer healing rate at 12 weeks for 50% of patients, 24 weeks for 75% of patients, with a stretched target of 2% for every additional year (leg ulcer clinics) • 100% response to referral within 48 hours • Less than 5 non-elective admissions as a result of long term conditions per year on active caseload. • 100% of patients have a named Community Matron • 90% compliance with wound care formulary for ONEL CS Havering staff Diabetes • Number of Dose Adjustment For Normal Eating (DAFNE) education sessions • Number of Diabetes Education and Self-Management for Ongoing and Newly Diagnosed (DESMOND) education sessions Other Adult Services • 100% of onward referrals being reported • Number of occasions that Psychological Support was provided to service users/patients • 100% of patients have an annual community Parkinson’s medication review • 100% of active caseload have their preferred place of care recorded • 100% of patients have a nutritional plan agreed with acute trust and the patient Childrens Services 19 • 100% of those children requiring a Individual Care Plan will be done • 100% of new birth visits within 10 - 14 days • 100% Children Centres/Early Years Centres to have a named Health Visitor • 95% new mothers screened for Postnatal Depression within 6 - 8 weeks • 100% of babies to receive 1 year check • 95% of children at 2 years of age to receive 2 year check • Every child under 4 years subject to Child Protection Plan will have a named Health Visitor • 100% of new mothers to receive Breast Feeding information at 10-14 days • 100% of new mothers to receive Immunisation Information at every contact • 100% staff have access to accredited UNICEF training • 4 Positive Parenting Programmes per year have a named Health Visitor • 100% of practitioners assess safeguarding supervision every 3 months • Number of child protection cases • Compliance with safeguarding policy and procedures • Percentage of children in Reception with height and weight recorded who are obese • Percentage of children in Year 6 with height and weight recorded who are obese • Immunisation rates for children • Total no. of BCG 12 – 13 yrs 2.8 Statements from the Care Quality Commission (CQC) Havering Primary Care Trust as the current host organisation of Outer North East London Community Services is required to register with the Care Quality Commission and was registered, and therefore licensed to provide services, in March 2010. Havering Primary Care Trust has no conditions on registration and the Care Quality Commission has not taken enforcement action against Havering Primary Care Trust during 2010/11. Havering PCT/Outer North East London Community Services has not participated in any special reviews or investigations by the CQC during the reporting period. However, the CQC did perform an unannounced inspection on 25th May 2010 to assess whether we are adequately protecting patients, workers and others from healthcare-associated infection. The inspection, which assessed compliance against the 14 measures within the Hygiene code, found no cause for concern regarding our compliance with the regulation on cleanliness and infection control. 20 2.9 D ata Quality A great deal of data is created and used by the NHS. This includes information which helps providers of healthcare and GPs to track patients and to make sure that all relevant information about them and their treatment, such as test results, is in the right place and can be found by the relevant staff. It is very important that the data is accurate and up to date, and NHS organisations are required to report on data collection and accuracy every year. Hospital Episode Statistics measure how NHS organisations collect and use information from patients when they are referred for treatment or attend hospital. All UK residents are allocated an NHS number which identifies them anywhere within the NHS, and we must include this number on all the records we hold on a patient. The patient’s General Medical Practice code identifies the patient’s GP and the practice the GP works in. Both pieces of information are key patient safety tools, as they help to ensure that the correct treatment is given to the correct patient, and that data such as test results and information on a patient’s treatment are sent to the right GP at the right practice. Outer North East London Community Services submitted records during 2010/11 to the Secondary Uses Service for inclusion in the Hospital Episode Statistics which are included in the latest published data. 2.9.1 Statement on Relevance of Data Quality and Actions to Improve Data Quality Outer North East London Community Services will be taking the following actions to improve data quality. This initiative will continue as we move to the new organisation. • To detail the scope of ONEL CS’ approach to improving data quality for the purpose of ensuring that the minimum standards laid down by British Telecom (BT), the London Programme for Information Technology (LPfIT) and the Information Quality Assurance Programme (IQAP) for the migration of records from databases & systems to RiO, data quality of existing bespoke databases and information systems holding patient data • To outline the framework and governance structure for monitoring activity against an agreed community dataset, eg NHS number, ethnicity etc • To provide a data quality improvement strategy for all services on Rio and all other systems with a continual data quality monitoring plan. • To provide the Commissioners with a continuous improvement tool for services in particular ensuring that the NHS number coverage is maintained at 95% or more. 21 • To ensure all services are responsible for standardising practices for data capture and reporting procedures & policies, across ONEL CS. • To ensure that robust, written processes and procedures for capture, recording and processing of data. • All the relevant areas of the Information Governance (IG) programme regarding Information Quality Assurance are investigated and action plans implemented to achieve the required levels. • To run exception and audit reports on a regular basis to feedback to users of systems so all amendments and corrections can be made, to ensure the highest level of data quality is held. • All statutory reports and requirements are met and dealt with in timely and accurate manner for all submissions. • Benchmarking for KPIs and CQUINs. 2.9.2 NHS Number and General Medical Practice Code Validity Outer North East London Community Services submitted records during 2010/11 to the Secondary Uses service for inclusion in the Hospital Episode Statistics which are included in the latest published data. The percentage of records in the published data: • which included the patient’s valid NHS number was: 99.9% for admitted patient care; and 99.8% for out patient care; • which included the patient’s valid General Medical Practice 100% for admitted patient care; and 100% for out patient care; 2.10 Information Governance Toolkit Attainment Levels Havering Primary Care Trust/Outer North East London Community Services Information Governance Assessment Report score for 2010/11 was 67% and was therefore graded red. The areas which needed strengthening were assurance regarding information security, clinical information and corporate information. Further work is underway to improve this position. 2.11 Clinical Coding Error Rate Outer North East London Community Services was not subject to the Payment by Results clinical coding audit during 2010/11 by the Audit Commission. 22 Part 3 Review of quality performance 3. Review of Quality Performance 3.1 Clinical Effectiveness - Productive Ward (Releasing Time to Care) Releasing Time to Care – the Productive Ward initiative is a national programme of work supported by the NHS Institute of Innovation and Improvement (NHSI). The project was embraced by the organization with board level support and initiated across three wards at St Georges Hospital with the project eventually progressing to all our inpatient units. It was clear that our ward teams have a number of competing priorities for their time and resources and delivering the fundamentals of nursing care, medicines management, ward rounds, meal rounds, admissions and discharging of patients, infection control, length of stay and administration. Valuable time is consumed looking for equipment, people, keys, linen, medicines, serving meals in an inefficient way and searching for information. Time is wasted when there is a lack of clarity about who is supposed to be doing what and in what order. The Productive Ward has empowered our ward teams by working through modules and toolkits, to reduce inefficiencies and waste, thereby releasing nursing time to be reinvested into direct patient care. It has given staff the opportunity to take responsibility for their own measures of care such as infection rates, falls as well as patient and staff satisfaction. The Productive Ward contains eleven modules focused on key activities. Following preparation, wards received facilitated support from the project team. This gave the ward teams the tools and techniques to implement the three foundation and one process module. Thereafter ward teams were able to implement the remaining modules through the support of the modern matron, practice development team and Executive team. The Productive Ward programme of work is aligning with other key initiatives within the Trust, e.g. essence of care benchmarks and service redesign pathway. Progress of the Productive Ward programme of work has been further enhanced by the better management of beds and support from the Estates and Facilities department and has resulted in supporting the same sex accommodation agenda. Initial results are positive from the performance measures. We have evidence of a reduction in overall complaints, reduced length of stay and a positive response to both staff and patient questionnaires about their experiences. Staff have become innovated in terms of utilizing their time during a shift and they have developed some simple, achievable, and timely ways of enhancing the patient’s experience which are realistic and measurable. Some examples have been the introduction of protected meal times, the red tray system to 24 ensure any patients who are at risk of malnutrition are fully supported during meal times. 3.2 Patient Experience - Complaints Management Valuable patient experience is provided via numerous channels including: • • • • • Complaints Patient Advice and Liaison Service (PALS) Comment/suggestion cards Compliments Website Outer North East London Community Services operates an integrated complaints and PALS service which ensures that dissatisfaction is dealt with in the most timely and effective manner whilst taking into account the wishes of the complainant. A risk assessment tool is used to facilitate this process. There is a complaint action planning process to ensure that learning takes place in order to improve services and minimise future complaints. The action planning process is audited to ensure that actions are taken. In 2010/11, we received 108 formal complaints, compared with 139 in 2009/10 – a decrease of around 22%. This decrease in the number of complaints is likely to be because of increased activity by PALS who can resolve issues in the early stages so that they do not escalate into formal complaints. 97% of complaints were acknowledged within three working days. We agree with each complainant a date by which we will complete our investigation and provide them with a final response. 75% of complaints were responded to by the agreed date and in cases where deadlines are not met, the complainant is updated as to the reasons why not and a new deadline is negotiated. The most common topics for complaints in 2010/11 were: • • • • • Clinical treatment (43%) Attitude of staff (17%) Communications – written and verbal (12%) Appointment delays (8%) Other (20%) issues including accessibility to services, failure to follow processes and admission and discharge arrangements Complainants who are not satisfied with their complaint response may approach the Parliamentary and Health Service Ombudsman (PHSO) and request that their complaint undergoes an independent review. During 2010/2011 the Trust received notification that 4 complainants had taken their complaints to the Ombudsman. The Ombudsman declined to investigate one of these, and the other 3 are still outstanding. 25 During 2011/12, the Complaints and PALS Team will focus on improving the data which lies behind complaints so that the Trust has a better understanding of the specific causes and issues which lead to complaints being submitted. A new version of the local risk management system (Datix) will be used to help with this process. This system is a database which contains information regarding all types of incidents, risk assessments and complaints and enables a joined up approach to risk management . The team will continue its rolling training programme to help engender a greater understanding of the complaints process amongst complaint investigating officers and frontline staff. 3.3 Patient Experience - Patient Environment Action Teams (PEAT) PEAT is an annual self assessment of inpatient healthcare sites in England that have more than 10 beds. It is a benchmarking tool to ensure improvements are made in the non-clinical aspects of patient care including food, cleanliness, infection control, privacy and dignity patient and environment (including bathroom areas, lighting, floors and patient areas). During the assessment process each criterion is given a score from 1 (unacceptable) to 5 (excellent). Assessments are carried out by our staff (nurses, matrons, catering and domestic service managers, executive and non-executive directors, dieticians and estates staff). Patients, patient representatives and members of the public are also part of this assessment process. The assessment results help to highlight areas for improvement and share best practice across healthcare organisations. The 2010/11 PEAT results for Outer North East London Community Services inpatient units are given in the table below. These assessments were undertaken between January and March 2011: Environment Food Privacy and Dignity Acceptable Good Good Good Good Good Ainsley Rehabilitation Unit Excellent Good Excellent Highams Court Excellent Good Excellent St George’s Hospital Galleon and Heronwood Unit 26 3.4 Safety - Infection Control Outer North East London Community Services has maintained an excellent record of performance in preventing and controlling healthcare associated infections. During 2010/11, no patients contracted a Meticillin Resistant Staphylococcus aureus (MRSA) blood stream infection (known as a bacteraemia) in any of our inpatient settings. Since January 2011 acute trusts have been required to report Meticillin Sensitive Staphylococcus aureus (MSSA) bacteraemia and the Infection Control Team for ONEL CS will review any new diagnoses of this organism. There have been three MSSA bacteraemias found within ONEL CS from January 2011. Root cause analyses have been performed for these three cases and these have not highlighted any specific issues within ONEL CS in­ patient areas. For Clostridium difficile infection the rate is also very low. Within all the three in-patient areas, there have been only four Clostridium difficile positive patients in the year 2010/11. These cases have been reviewed and there is no evidence of cross infection between any of the cases. This is a much lower incidence than would be expected from the number and type of patients that are within these units. There have been no outbreaks of infectious disease during 2010/11. In particular we note that there were no outbreaks of norovirus within the in­ patient settings this winter which is a significant achievement for which we thank and congratulate our ward staff. ONEL CS has a planned programme of infection control audits covering the following areas: • • • • • Hand hygiene – looks at resources, ensuring that hand hygiene materials are available for staff and that staff are aware of their responsibilities. There are also more frequent hand hygiene audits performed which look at the practice of staff relating the opportunities for hand hygiene against the uptake Environment – looks at the condition of the environment, damage to fixtures, fittings and decorations as well as the quality of cleaning of all of these Ward/Departmental kitchens – making sure that risks of food poisoning are reduced as much as practically possible. Part of the yearly infection control audit, but also reviewed following yearly deep clean Waste and linen handling and disposal – ensuring local policy is being complied with and appropriate segregation is performed Safe handling and disposal of sharps – make sure sharps bins are fully assembled and that sharps are being dealt with appropriately 27 • • Management of patient equipment – reviewing local decontamination of equipment Clinical practices – ensuring that staff are compliant with the local polices and procedures Results of the audits are fed back to managers with a report and an action plan giving timescales for completion of issues. 3.5 Conclusion In the introduction to this quality account we set out what the quality account was and why it is important. This account is our opportunity to provide information and assurance that we are providing patient care that is safe, effective and efficient. Whilst this is the only account due to be published by ONEL CS, the work we have started and the improvements we have made will be carried forward with us as the services we provide move in to North East London Foundation Trust. 28