The Quality of Care Our Patients Receive 2010 - 2011
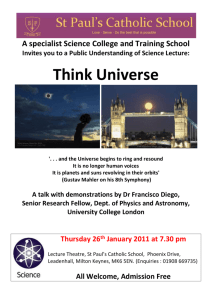
advertisement

Quality Account The Quality of Care Our Patients Receive 2010 - 2011 1 Quality Account GLOSSARY CAMHS COPD CQC CQUIN DoH E4E HCAI IPC LINk MKCHS MKSCB MMSE MRSA NHSLA NICE NPSA PCT PEAT QA QC QIPP QRP RCA R&D RiO TOPAS UTI WICU Children’s and Adolescents Mental Health Service Chronic Obstructive Pulmonary Disease Care Quality Commission Commissioning for Quality and Innovation Department of Health Energising for Excellence Health Care Acquired Infections Infection Prevention and Control Local Involvement Network Milton Keynes Community Health Services Milton Keynes Safeguarding Children’s Board Mini Mental State Examination Meticillin-resistant Staphylococcus aureus National Health Service Litigation Authority National Institute of Clinical Excellence National Patients Safety Agency Primary Care Trust Patient Environment Assessment Team Quality Account Quality Control Quality Innovation Productivity and Performance Quality Risk Profile Root Cause Analysis Research and Development Clinical records data collection system (Rivers of Information) The Older People’s Assessment Service Urinary Tract Infection Windsor Intermediate Care Unit 2 Quality Account Contents Section 1 1. Introduction Page No. 4 Section 2 2. 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 2.10 2.11 2.12 Priorities for 2011/12 Priorities for Improvement Statements of Assurance from the Board Statements to Review Services Participation in Clinical Audit Measuring Participation Measuring Coverage/Recruitment Reviewing Reports of National Clinical Audits Reviewing Reports of Local Clinical Audits Research Goals agreed with Commissioners What others say about the Provider Data Quality 7 12 13 14 15 16 17 18 23 28 32 33 SECTION Section 3 3 Review of 2010/11 3.1 Review of Quality Performance 3.1.1 Patient Safety 3.1.2 Clinical Effectiveness 3.1.3 Patient Experience 3.2 Statements from Local Involvement Networks, Health and Community Wellbeing Select Committee and NHS Milton Keynes 3.3 How to Provide Feedback 36 36 47 53 63 66 3 Quality Account SECTION ONE Introduction High quality care is what we all want to receive. Here at Milton Keynes Community Health Services (MKCHS) maintaining high quality services is our top priority underpinned by good patient safety, clinical effectiveness and patient experience. We aspire to excellence in all of our services which include: Adult Services, Older People’s Services, Children’s Health Services and Mental Health and Learning Disability Services. The quality agenda is a key component of our Quality Innovation Productivity and Performance (QIPP) programme and is threaded through the work that has been undertaken during the last year to transform community services. We understand that the community we serve must have confidence in the services we provide. From first contact through to discharge, the patient journey must be a positive experience. We strive to work with patients, users and their carers in identifying where patient experience has not been as good as it should have been and we will ensure that learning and changes to services occur as a result. We will make sure that quality includes equality and inclusion. Ensuring high quality care always takes into account a person’s age, disability, gender reassignment, marriage and civil partnership, race, religion or belief, sex and sexual orientation. This will help us to meet and go beyond the Care Quality Commissions standards of care and comply with today’s equality rules. The patient experience strategy we have produced is “a partnership between the people who use our services, the Milton Keynes community, clinical staff and service managers. The strategy comprises a series of ‘Campaigns’ designed to make real and lasting improvements in areas which matter to our service users”. 4 Quality Account We have used our Patient Experience Working Group and our Clinical Council to give initial feedback on this quality account and established a working group which members including senior clinicians, managers and Local Involvement Network (LINk) representatives, to pull the report together. This input, along with feedback from the National Staff Survey and the Care Quality Commission’s Quality Risk Profile, helped us to determine where we’ve done well and areas that need improvement. In using this approach we are assured that this report gives a true and accurate picture of Milton Keynes Community Health Services and the issues that are important to the local community and our staff. We are confident that the data and information contained within this report gives a true and accurate picture of our achievements in 20010/11 and areas for development in 2011/12. Our Quality Account, in its draft format, was discussed and approved by the Leadership Management Team, the Patient Experience Working Group, the Joint Negotiation & Consultative Committee and our Clinical Council. The draft document was also circulated to NHS Milton Keynes, the Health and Community Wellbeing Select Committee and Milton Keynes Local Involvement Network (LINk). Once feedback was received the report was finalised and then formally presented to our organisation’s Board (Provider Committee) before final publication. Within this Quality Account we have highlighted areas of importance to people who use our services; under Patient Safety we have included, falls, pressure ulcers, infection control, and safeguarding vulnerable people. The Clinical Effectiveness section gives assurance that we have a high quality workforce, we are taking forward the national ‘Productives ’ initiative ,improving safety, quality and reliability of services. Finally that we actively participate in audit at a local and national level, and use this to demonstrate how we make improvements and sustain them. Under Patient Experience we have included making improvements to communications with service users and their carers, 5 Quality Account transfer of care, nutrition and hydration as well as work to improve Patient Environment (PEAT), looking at patients’ access and patient safety and standards, as well as privacy and dignity. We hope you find the report interesting and that it gives you an understanding of how seriously we take quality – it’s at the heart of everything we do. Milton Keynes Community Health Services Leadership Team Left to right; Sheila Begley (Deputy Director of Nursing), Jenny Williams (Head of Business Development), Cathy Walker ( Managing Director and Operational Director of Adult and Older People’s Services), Ruth Weetman (Operational Director of Patient Safety and Standards and DIPC), Matthew Webb (Associate Director of Finance, Performance and Business Development), Jane McVey (Director of Human Resources), Dr. Nanda DeSilva (Medical Director), Anna Selby (Operational Director of Joint Mental Health Services) and Jill Wilkinson (Operational Director of Children’s Health and Secure Settings and Lead Nurse). 6 Quality Account SECTION TWO Priorities for 2011/12 2.1 Priorities for Improvement Our 2010 /11 quality account identified three areas as priorities for development within the coming year; these were Transfer of Care, Nutrition and Hydration, and Communication with the focus on improved information to service users and their cares. We will demonstrate how these were taken forward and achieved within section three of this document. We have identified the following areas as priorities for improvement in 2011/12: • Patient Safety – Pressure Ulcers • Clinical Effectiveness – Energizing for Excellence in Care (E4E) high impact actions for Nurses. • Patient Experience; which includes Medicines Management as one of the areas for focused work Patient Safety – Pressure Ulcers Pressure ulcers, also known as pressure sores, affect some of our most vulnerable service-users and are often preventable; they are of concern for everyone who provides care in Milton Keynes; in the community, in hospital and in residential and nursing homes. It is essential therefore, that we work with our partner organisations to achieve progress. Pressure Ulcers featured in our 2009/10 Quality Account (please see section 3), we plan to progress the initiatives in the coming year in partnership with the hospital and Local Authority. How do we achieve progress? We have developed a set of standards jointly with the hospital and the nursing team which provides support and training on this subject in nursing homes. The standards relate to; 7 Quality Account • Numbers of avoidable pressure ulcers measured against the baseline established this year. • Staff training on pressure ulcers • Peer review, by partner organisations, of each others pressure-ulcer investigations. How are we monitoring and measuring? These standards have been included in this year’s CQUIN (Commissioning for Quality and Innovation) scheme and we will be expected to present reports on a bi-monthly basis to our Commissioner, and to undertake peer review of investigations at the Serious Incident Review Group. We will also be carrying out regular audits of pressure-ulcer incidents. How will progress with this be reported? Reports will be presented • internally, to the Clinical Governance Committee and Patient Experience Strategy Group, • to the Commissioner at the Serious Incident Review Group and the quality monitoring forum. • to people who use our services via the Patient Experience Strategy Group and through the Quality Account. Clinical Effectiveness – Energize for Excellence Energise for Excellence in Care (E4E) provides a national framework for promoting quality in nursing and midwifery. The framework is structured under 5 key domains: 1. Get staffing right 2. Deliver care 3. Measure impact 4. Patient experience 5. Staff experience 8 Quality Account Energise for excellence aims to draw together many of the initiatives which have been designed to improve safety, quality and involvement in care under these 5 domains such as: • High impact actions • Productive care • Safety Express • Essence of care. Few of these initiatives are new to Milton Keynes Community Services, however energize for excellence draws together and provides a clear structure to understand the range of work aiming to deliver clinical service improvement, as shown in the diagram below. Energise for Excellence Work in Community Health Services How will we achieve progress? • Get staffing right - correct staffing levels and mix is critical to providing safe and effective care 9 Quality Account • Delivery of care - via re launched Essence of Care work so we can be accurately benchmarked nationally • Measure impact - The Department of Health has identified eight high impact actions to monitor the effective of nursing and clinical care practice. These will be adopted and monitored. How will we monitor and measure this? Milton Keynes Community Health Services has an active essence of care steering group which works to maintain momentum across clinical services in the use of essence of care benchmarking. This group will be used to monitor and measure progress. How will progress be reported? A range of tools and systems as shown in the diagram page 9 are used to measure the impact of clinical care across the organisation. However many of these tools are Acute Hospital based so we have adapted them for use within the community setting. e.g. Royal Collage of Nursing staffing level tool used rather than Acute based HURST tool. Most of this information is reported through performance reports to each service through the directorate meetings and through leadership team and board meetings. Patient Experience - Communication and Transforming Services Our priority during challenging financial times is to communicate well with our service users particularly where services are being transformed or reduced. This will ensure that service users have the information they need to enable them to understand the decisions made about their care and treatment. 10 Quality Account Our aim is to gain real insight into how it feels for our service users, to move away from traditional paper based surveys and to listen to our patients. How do we achieve progress? • Conducting interviews with service users where service’s are being transformed • Using ‘real time’ patient feedback systems allowing us to make any improvements much faster • Reviewing our complaints to look for trends • Creating an email address for service users to contact us on • Developing a Community Health Service Patient Panel who will offer advise on all aspects of patient care How are we monitoring and measuring? We will be using the information from both our ‘real time’ feedback and our interviews to give us a full picture of how well we are communicating. This information will be monitored by our Patient Panel and our Clinical Governance Committee, which consists of both staff and patients. How will progress be reported? Progress will be reported formally through our Patient Panel and our Clinical Governance Committee and also fed back to our patients using a variety of medias including our website. Patient Experience – Patient Experience Strategy Community Health Services has an active Patient Experience Strategy which includes five campaigns chosen annually to make measurable improvements to services and care experience. The campaigns are chosen based on both national initiatives and local information including patient feedback, incidents and complaints. Medicines Management will be one of the campaigns for 2011 and will include work with the Mental Health Pharmacy Team and the patients who attend the Clozapine Clinic. They will be focusing on what they do well and what can be improved. (Other campaigns are noted page 53 -59) 11 Quality Account How do we achieve progress? • Each of the campaigns will have a working group including patients who will assess current baseline information and set objectives for the coming year • Regular reporting will ensure that campaigns are progressing well and that any issues are dealt with promptly How are we monitoring and measuring? The Patient Experience Strategy will be monitored through the Patient Panel and the Patient Experience Strategy Steering group. Individual campaigns including Medicines Management will have their own working groups. How will progress be reported? The campaign groups will report quarterly to the Patient Panel and the Patient Experience Steering group. Progress made will also be reported back to the patients 2.2 Statements of assurance from the Board One of the aims of the Quality Account is to give information to the public which will be common across all Quality Accounts in the country. In order to do this our Quality Account has a number of statements that must be included. To quickly identify these compulsory sections we have printed them in a different coloured text (yellow) to the main body of the report. Performing to essential standards. Milton Keynes Community Health Services achieved ‘unconditional’ registration with our regulatory body, the Care Quality Commission (CQC). Our priority now is to make sure that we comply with the new CQC Essential Standards. 12 Quality Account To provide extra assurance, we have opted in to an assessment by the NHS Litigation Authority which will test all the policies we have in place to manage risk. Measuring clinical processes and performance MKCHS is a research-active organisation; we are able to participate in research and to support our clinicians in providing excellent, research evidence-based care (details can be found pages 24 – 27) We measure our delivery of high-quality care through a program of Clinical Audit; the audit plan includes audit linked to NICE and topics identified from national reports as well as local clinical concerns. Involvement in national projects and initiatives aimed at improving quality MKCHS participates in research projects arising from the Comprehensive Research Network (a national portfolio of projects) and the national clinical audits which apply locally. MKCHS takes account of any concerns arising from National Confidential Inquiries and reports (such as the Francis Report), to address any issues which might apply locally and to provide assurance that these are addressed. 2.3 Review services During 2010 /11 Milton Keynes Community Health Services provided and/or sub-contracted 36 NHS services. Milton Keynes Community Health Services has reviewed all the data available to them on the quality of care in 36 of these NHS services. The income generated by the NHS services reviewed in 2010 /11 represents 100% percent of the total income generated from the provision of NHS services by Milton Keynes Community Health Services for 2010 /11. 13 Quality Account 2.4 Participation in clinical audits During April 2010 to March 2011, 11 national audits and 1 confidential enquiry covered NHS services that Milton Keynes Community Health Services provides. During that period Milton Keynes Community Health Services participated in 4 (40%) national clinical audits and 100% national confidential enquiries of the national clinical audits and national confidential enquiries which it was eligible to participate in. The national clinical audits and national confidential enquiries that Milton Keynes Community Health Services was eligible to participate in during April 2010 to March 2011 are as follows: National Clinical Audits • Childhood Epilepsy • Chronic Pain • Parkinson’s Disease • Chronic Obstructive Pulmonary Disease • Stroke Care • Falls and Non-hip fractures • Depression and Anxiety Psychological Therapies) • Prescribing in Mental Health Services • Schizophrenia • National Patient Survey for Mental Health Services National Confidential Enquiries • Suicide and Homicide by People with Mental Illness 14 Quality Account 2.5 Measuring participation The national clinical audits and national confidential enquiries that Milton Keynes Community Health Services participated in, and for which data collection was completed during 2010/11, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. During the period April 2010 to March 2011, 10 (18.5%) of 54 national clinical audits were relevant to Milton Keynes Community Health Services. The table below details audits the organisation did or did not participation in and reasons for non-participation where applicable. National Clinic Audit MKCHS Reason for non-participation Participation Yes No Childhood Epilepsy × Chronic Pain × No reason given Parkinson’s Disease × A new post was created at the beginning of 2010 for a Specialist Parkinson’s Nurse so it was considered unsuitable to audit the service at such an embryonic stage. COPD × No reason given Stroke Care × A new Stroke Care service was established in 2010 so it was not considered suitable to audit performance until it was properly embedded. Falls and Non-hip × N/A × N/A fractures Depression and Anxiety (Psychological 15 Quality Account Therapies) Prescribing in Mental × N/A Health Services Schizophrenia × Unable to capture diagnosis info as implementation of new patient management system. National Patient Survey × N/A for Mental Health In the same period, Milton Keynes Community Health Services participated in all national confidential enquiries that were relevant to the services they provide. The table below details participation. National Confidential MKCHS Enquiry Participation Yes Suicide and Homicide Reason for Non-participation No × N/A by People with Mental Illness 2.6 Measuring Coverage/Recruitment National Clinical Audit Participation Yes % Cases Submitted No Childhood Epilepsy × N/A Chronic Pain × N/A Parkinson’s Disease × N/A COPD × N/A Stroke Care × N/A Falls and Non-hip fractures × 40 hip fracture 16 Quality Account 20 other fragility fractures (100% of requested sample) Depression and Anxiety × 38 service user surveys and (Psychological Therapies) 5 therapists survey were returned (unsure of numbers distributed or eligible cases) and 123 patients were submitted for a retrospective analysis of patients who ended their care between September and November 2010 Prescribing in Mental Health × 5 patients (unsure of Services number of eligible cases) Schizophrenia National Patient Survey for Mental × × Health 856 patients submitted (52% of eligible patients) 2.7 Reviewing Reports of National Clinical Audits The reports of the four national clinical audits relevant to our services were reviewed by the organisation in 2010/11 and MKCHS intends to take the actions described in the table below to improve the quality of healthcare provided. AUDIT Summary of Actions Falls and Non-hip fractures Results not yet available – no confirmed date for publication Depression and Anxiety Results due for publication October 2011 (Psychological Therapies) Prescribing in Mental Health Services Although results for Milton Keynes Community Health Services were good overall, it was considered suitable to 17 Quality Account design a pro-forma as a front sheet to records to act as a reminder to carry out required physical health checks for patients prescribed antipsychotic medication. This is currently underway and should be in place by Autumn 2011. National Patient Survey for Mental Overall the results of the 2010 patient Health survey were disappointing in several areas, and a comprehensive action plan has been applied to all areas identified as performing less well 2.8 Reviewing Reports of Local Clinical Audits The annual clinical audit plan reflects local and national priorities for service improvement and there is an expectation for all services to engage fully in the audit process to ensure continual review of current practice against specific objectives. All services are expected to complete an audit of their record keeping practice each year to demonstrate that adequate information is recorded for each patient to ensure safe and effective treatment and care. Health and Safety audits, Hand Hygiene and Infection Prevention audits are also carried out in all services annually and are of great value in terms of ensuring safety of patients and staff and minimising spread of infection. Consent audits are conducted for all services on a three year cycle and the purpose of these is to demonstrate that patients are suitably engaged in the consent process. Although some services include an assessment of whether consent has been sought in the care records audit, it was considered that qualitative audits should be conducted in order to assess the extent to which patients are involved in discussions and decisions about their care and whether the content of these discussions can demonstrate clear patient 18 Quality Account agreement to and understanding of their treatment and care prior to consent. In general, results have demonstrated good practice and continual improvement year on year. In addition to mandatory audit requirements, the annual audit plan is an integral part of the service improvement process for all services and topics relate clearly to service objectives against local and national priorities. Included in the plan are projects to identify level of compliance with national quality and best practice indicators such as the NICE guidelines and the Care Quality Commission’s Standards for Equality and Safety as well as locally applicable patient satisfaction surveys or audits pertaining to emergent themes in incidents or complaints. The reports of 163 local clinical audits were reviewed by the provider in 2010/11 and MKCHS intends to take the recommended actions to improve the quality of healthcare provided. Four case studies are given below as an illustration and details of the audits are available on request. The case studies below are examples of audits conducted within Milton Keynes Community Health Services during the past 12 months. Transfer of Care. Concerns had been raised about the quality of processes for transfer of care between clinical settings and for discharging people from healthcare settings into the community. A review of incidents relating to transfer of care was conducted to provide information to support improvements in processes and communication throughout the health and social care economy in Milton Keynes. The aim of the audit was to enable people who use our services to have a seamless experience, however many times they are transferred between clinical and/or social care settings. 19 Quality Account The study demonstrated that problems relating to transfer of care are wide ranging and impact upon services in all areas and in general relate to poor communication between services. These communication issues result in lack of public confidence in health and social care services. As a result of this audit, the following recommendations were made: • Staff are aware to report all incidents relating to transfer of care, however minor and copies of these should be provided to both MKCHS and MKFTH. • That all services have a designated Senior Manager with responsibility for leading transfer of care discussions relating to their service. • To establish a Senior Manager’s forum for Milton Keynes Hospital and Community Health Services to consider strategic issues such as care pathways, protocols and training. • The issue of transfer of care should be a standard agenda item at MKCHS Directorate meetings and the Commissioning Clinical Concerns Group. NICE. In November 2006, NICE published guidance on supporting people with Dementia and their carers in health and social care. Part of this guideline pertained to pharmacological interventions for the cognitive symptoms of Dementia, with three drugs recommended as suitable options in the management of patients with the disease. The guideline made the following recommendations: • That only specialists in the care of people with Dementia (psychologists, neurologists, physicians) should initiate treatment • That patients prescribed drugs for Dementia should be reviewed every 20 Quality Account six months. • That drug treatment should only continue while the patients ‘mini mental state examination’ (the MMSE is a test use to determine level of cognitive ability) remained above 10 points unless it is judged by significant impairments in functional ability and personal/social function that the patient likely has Dementia. • The drug treatment should only continue for as long as the patient’s global, functional and behavioural condition demonstrates the drug is effective. An audit was conducted to identify level of compliance with this guideline with good results and last year, a re-audit was carried out to ensure continued best practice. 25 patient cases were reviewed for this audit. Of these, 24% of patients had a mini mental state score of between 10 and 20 on commencement of treatment but 76% of those with a score above 20 displayed significant functional impairments to justify a clinical diagnosis of Dementia. 100% of patients receiving pharmacological intervention were reviewed six monthly. 22 of 25 patients’ MMSE score remained between 10 and 20 throughout the review period. 100% of patients whose score fell below 10 had medication discontinued. 19 patients with drug intervention displayed that the drug continued to be effective. Of those for whom it seemed ineffective, 2 patients had drug treatment discontinued and 3 continued with the same prescription. It is unclear from audit data whether their prescription was continued due to evidence of functional impairment. Overall this audit demonstrates good practice although further review of those 21 Quality Account patients prescribed medication with a MMSE score of below 10, not displaying significant functional impairment may be required to justify pharmacological intervention. Patient Satisfaction. Gaining information regarding patient experience of and satisfaction with treatment and care has been a high priority across all services provided by Milton Keynes Community Health Services over the past 12 months. Numerous projects have been conducted to attempt to adequately collect information to help us improve services and a Patient Experience Strategy Group has been established to ensure continued commitment to inclusion of patient and public perspective in planning and delivery of services. Many services have distributed service user questionnaires to assist in establishing a baseline of patient perception of services. One such questionnaire was distributed by Children and Adolescents Mental Health Services and collected feedback from children under the care of the service but also from the parents of those children. Parents and children were asked the same questions, ranging from whether or not they felt their therapist had listened to and had understood their problems and whether they felt confident that the therapist could help to whether the treatment was adequately explained, if their appointments times were suitable and if waiting room facilities were comfortable and inviting. Overall results were very positive with parents reporting overwhelming satisfaction with the service. They felt that the support offered by therapists extended to their own needs as well as their children’s, that issues were 22 Quality Account discussed sensitively and professionally and many felt that their children had enjoyed therapy sessions, despite them being difficult at times. Children felt that they were able to speak very openly and honestly with their therapists and many reported an increase in confidence and ability to express themselves positively. Most children felt that appointment times were suitable, not interfering with school or extra curricular commitments. One commented it was helpful to have appointments outside of school hours as the nature of appointments could create issues with peers. Some valuable points were made that could help to improve the service: • Parents and children commented that referral to the service was often slow and that children were possibly discharged too soon. • A few were concerned by lack of information provided regarding withdrawal of medication. Some felt medication was stopped too soon and others felt they were ready to stop medication long before their prescriptions were withdrawn. • Some mentioned that toys and reading materials provided in the waiting area were unsuitable for older children and were designed for very small children or adults only. Although overall, results demonstrate that parents and children are satisfied with the service, appointment referral times and communication regarding medication are both important issues to be addressed. 2.9 Research In order to ensure compliance with the Department of Health’s Research Governance Framework, all research active NHS organisations are expected to have a forum for monitoring all aspects of research governance and for promoting evidence based practice. Milton Keynes Primary Care Trust’s Research & Development Committee meets quarterly to fulfill this dual 23 Quality Account function and is made up of designated research leads from each service with relevant expertise to consider the impact of participation in research studies in terms of clinical, financial and resource Implications. Additional members include the organisation’s R&D Facilitator, Chief Knowledge Officer and key contacts from Milton Keynes Hospital Foundation Trust and Academia. Committee meetings consist of progress updates from all service members regarding studies being conducted by service staff or external studies the service are currently participating in; a summary of new or pending studies that have recently received or are awaiting organisational approval for participation and discussion of potential risks; presentations of research results by internal or external researchers and general research news and legislative updates. Over the past 12 months Milton Keynes Primary Care Trust has hosted approximately 55 local and national research projects, working in partnership with Trust staff, academia and commercial industry. Patient participation in local and national research provides a valuable contribution towards the advancement of medical knowledge overall but can also be of significant benefit in terms of identifying areas for improvement and refining service provision locally. Study Reference Details Number of Patients Recruited ASCEND Aspirin vs placebo and omega-3 vs 34 placebo for primary prevention of cardiovascular events in people with Diabetes. REAL Rehabilitation Effectiveness and 3 Activities for Life. Study of rehab services and efficacy of promoting activities for people with severe mental 24 Quality Account health problems. SNIFS Study A primary care trial of steam inhalation 5 and nasal irrigation for recurrent sinusitis SSEW Study of Suicide in England and Wales 3 BDR Donor Brains for Dementia: Recruitment of 1 Recruitment potential brain donors for longitudinal cognitive and memory assessment prior to donation 6605 Studies of psychiatric in-patients who 1 commit suicide in first week of admission and suicides within 2 weeks of discharge from psychiatric in-patient care PET1 Comparison of acute mental health in- 2 patient wards which use protected engagement time with other wards delivering standard care alone 7462 Cardiovascular outcomes in patients with Unknown Type 2 diabetes 9906 Nasopharangeal pneumococcal carriage 2 in pre-school children 9845 Nasopharangeal pneumococcal carriage 32 in older people 9422 Swine flu vaccine study 17 8976 Meningitidis vaccine study 33 8556 Canaglifozin vs placebo for treatment of Unknown older people with Type 2 Diabetes 8092 Pneumococcal vaccine study 11 7297 Meningoccal B vaccine study 15 7296 Meningoccal B vaccine study 16 6953 Meningoccal B vaccine study 5 5173 Staying well after depression Unknown 4609 Effects of meningococcal opa proteins on Unknown the immune system 25 Quality Account 9456 Work related illness survey 1 7844 Evidence in management decisions: 1 advancing knowledge utilisation in healthcare management 3C Cough complications study 160 7410 PRISM Primary care streptococcal management 5 study TOPIC Study of effectiveness of inter- 1 professional working for community dwelling older people 7467 Cough complications cohort study 104 The number of patients receiving NHS services provided or sub-contracted by Milton Keynes Community Health Services during April 2010 to March 2011 that were recruited into research approved by a research ethics committee was approximately 452. We are committed to supporting research in all areas of healthcare and to ensuring continued organisational and staff development. The table below gives an overview of research studies we have been involved with in the last 12 months in various categories. SPECIALITY NUMBER OF STUDIES Cardiovascular Disease 1 Neurodegenerative Disease 9 Stroke 3 Diabetes 5 Paediatrics/Child Development 10 Mental Health 21 Chronic Obstructive Pulmonary Disease 5 Cancer 6 Urgent Care 3 Pregnancy 1 26 Quality Account Organisational Development 4 Ear, Nose and Throat 9 Obesity 1 Epilepsy 1 Pharmacology 1 Vaccinations 14 Older People 3 Staff Development 3 Dentistry 1 Musculoskeletal Conditions 2 Miscellaneous 5 Additional Research and Development priorities over the last 12 months were to arrange a research shared learning event and to include service user perspective in identifying priorities for research by establishing the Service Improvement Patient Panel. Although slightly delayed, a shared learning event is planned for July 2011 and has been organised collaboratively with Milton Keynes Foundation Trust Hospital and the faculty of Health and Social Care at the Open University. This event will provide an opportunity for staff and students to present their research findings and to discuss applicability to local services and care, therefore potentially influencing changes in practice. We hope this event will prove a great success and will provide a platform for development of future collaborative events to promote research locally. The Service Improvement Patient Panel, a committee of public and patient representatives now meets quarterly to discuss improvement priorities and these are reflected in the organisations annual audit plan that includes studies conducted by staff as part of academic study. Panel members are actively involved throughout the project process and recruitment of members is an ongoing process and a priority for the year ahead. 27 Quality Account 2.10 Goals agreed with commissioners A proportion of Milton Keynes Community Health Services income in 2010 /11 was conditional on achieving quality improvement and innovation goals agreed between Milton Keynes Community Health Services and any person or body they entered into a contract, agreement or arrangement with for the provision of NHS services, through the Commissioning for Quality and Innovation payment framework. Further details of the agreed goals for 2010 /11 are summarised below. Full details and the CQUIN scheme for the following 12 month period are available electronically at [http://www.miltonkeynes.nhs.uk/default-ContentID-6202.htm] 28 Quality Account Outlined below are the 2010/11 CQUIN standards and a summary of our achievement against them: 2010/11 CQUIN STANDARDS COMMUNITY SERVICES (CS) & MENTAL HEALTH SERVICES (MH) Clinical Quality Indicator (CQUIN) 2009/10 Performance We have achieved our interim target for CS1 To achieve recommended levels of this CQIN which is 443 people aged 0-5 health visiting per health visitor. . The experience of patients using MK Community Health Services will be sought and analysed on a regular basis by service providers and the outcome CS2 shared with commissioners. All five ‘campaigns’ have resulted in In-year, there will be 5 patient service improvements. Details available experience strategy ‘campaigns’. (as from the Clinical Governance Team outlined in MKCHS Patient Experience Strategy 2010-13) These are designed to make measurable improvements to CQC priority topics and cover all service areas Pressure Ulcers. A year on year reduction across the MK health economy in newly acquired preventable CS3 pressure ulcers of no less than 25% against the baseline. (n.b. the CQUIN was revised mid-year Achieved; there have been significant improvements in patient assessment, training and management of people at risk of developing pressure ulcers this year. to reflect changes in requirements) 29 Quality Account End of Life Care. Use of the Liverpool Care Pathway to support people in the last stages of life. • CS4 anticipatory prescribing for key symptoms that may develop in the last days and hours of life. • compliance with completion of Achieved; the work has included the development of pathways used in acute trust, care homes and CHS. There has been an emphasis on training of staff this year. the LCP. Re – admission to hospital during the 90 CS5 days following discharge from Intermediate Care Services. Achieved; all readmissions were for conditions unconnected with the original admission Community Stroke Services. Access to stroke specialist supported On track for achievement by year-end. discharge Development of pathway is awaiting final Development of early improvement plan sign off. CS6 for whole of community stroke service At the last audit, 100% of patients had a All Stroke Patients being transferred comprehensive care plan and access to from hospital to community and/or social specialist staff services will have a comprehensive stroke care plan and access to specialist staff. (n.b. HONOS is a Health of the Nation indicator) The commissioner will expect quarterly MH1 audit reports that detail HONOS compliance, aggregate outcomes and Achieved The audit showed 97.5% compliance for HoNoS recommendations for improvement 30 Quality Account Achieved. The focus has been on 1. Medication and health review Using Care Program Approach to MH2 clinics improve engagement, health and well- 2. use of Advance directives being: MKCHS Mental Health providers 3. 7 day CPA follow-up will adhere fully to the new CPA 4. Number of adults in contact with guidance issued by the DH. secondary mental health services in settled accommodation and employment 5. Patient surveys . Achieved; highlights include 1. Service user involvement in the development of recovery pack, CPA and risk training for staff. User Involvement: Providers will work with service users and carers to develop MH4 a method that promotes full engagement 2. Service user involvement in training. 3. Development of local focus groups across the service. with service users and carer from . Minority Ethnic 4. Employment of service user/expert by Involvement of SU forum in service design Recovery Planning Tool: Providers will implement the Recovery Star as a recognised tool for recovery planning; Action plan in place leading to full roll out in March 2011. who have signed recovery plans 31 Quality Account 2.11 What others say about the Milton Keynes Community Health Services The Care Quality Commission Milton Keynes Community Health Services is required to register with the Care Quality Commission and its current registration status is ‘Unconditional Registration’ Milton Keynes Community Health Services has not participated in any special reviews or investigations by the CQC during the reporting period. During 2010 /11 the Care Quality Commission introduced a monthly Quality Risk Profile for all NHS Organisations. The Quality Risk Profiles (QRP) are used by the CQC to support monitoring of compliance with essential standards of quality and safety. The monitoring is carried out by using external data that is relevant to MKCHS e.g. National Staff Survey, Patient Environmental Action Team Assessments, National Mental Health Patient Survey. This data is then put together in a report and depending on what the data is indicating e.g. good / poor performance is given a risk rating. The QRP’s were introduced in September 2010 and since this time MKCHS have shown month on month that 88% of the data collected relevant to our organisation is ‘similar to’ or ‘much better than expected’ This is a good indicator that on the whole we are performing well. However there are a number of areas that we are already aware of where performance could be improved. These exceptions (areas for improvement) are monitored via monthly performance reports that go to our Provider Committee on a bi monthly basis. 32 Quality Account In 2011, we have continued to build upon our successes with the introduction of provider compliance assessments. These assessments relate specifically to the outcomes that service users should experience when receiving care and treatment and so are highly relevant tools for understanding our services and service user experiences. Services are demonstrating innovative approaches to embed CQC standards in practice and to complete the compliance assessments including full team involvement. This will help MKCHS be able to demonstrate compliance with CQC standards and also provide high quality care for all our service users. 2.12 Data Quality Relevance of Data Quality and actions to improve Data Quality: Milton Keynes Community Health Services will be taking the following actions to improve data quality. The quality and accuracy of data is a key factor in monitoring and improving performance across all services. MKCHS has made significant strides forward in improving both the completeness and validity of the data that is captured. Opportunities to further improve data quality are routinely identified and the Information Team & the Performance Team sets clear priorities every month for development and improvement. MKCHS has a comprehensive and systematic approach to the management of data quality held on its patient information systems, mainly RiO (River of Information) that is then used for reporting. The Information Team liaises with the end users and the RiO team on a regular basis to fix system issues & the data quality issues; the aim is to ensure substantial assurance ratings to our systems and processes. This should give everyone confidence that data reported in these accounts and routinely in our information and performance reports is reliable and of high quality. 33 Quality Account Our performance on data completeness is good but with room for improvement and the measures taken to rectify RiO during 2011/12 will enable us to make great strides towards the achievement of the target for the all the community services. During 2010/11, we made considerable progress to enable the internal and external reporting of performance data required as a result of increased contractual requirements. We achieved this through the implementation of RiO in Mental Health & Children and Young Peoples Directorates, various data collection tools in a number of services, the enhancement of established information databases and increasing the capacity and capability of staff within services with regard to data recording, reporting and analysis. For 2011/12 Milton Keynes Community Health Services are taking the following actions to improve data quality. We have set a key business objective of making sure that all services are in a position to record, report and analyse their activity and performance data to enable them to manage capacity and demand, ensure delivery of contractual requirements, increase quality of services and measure the outcomes from service improvement initiatives. We will build on the foundations established in 2010/2011 and develop the following areas to act as a tool for measuring our quality, efficiency, cost effectiveness and in some areas accessibility: Work has started to ensure good data correction processes are in place for the RiO national IT system that will continue to be implemented throughout the organisation along side regular weekly monitoring of quality at both initial data entry stage and post corrections. NHS number and general medical practice code validity: Milton Keynes Community Health Services submitted records during April 2010 to March 2011 to the Secondary Uses service for inclusion in the 34 Quality Account Hospital Episode Statistics which are included in the latest published data. Based on published data in the SUS data quality dashboard from the Information Centre for coverage between April 2010 to January 2011 (latest release at time of writing); the percentage of records which included the patient’s valid NHS number was: 99.7% for admitted care and 99.6% for out patient care. The percentage of records in the published data which included the patient’s valid General Medical Practice Code was 97.8% for admitted care and 99.6% for out patient care. On Information Governance Toolkit attainment levels: Milton Keynes Primary Care Trust (MKCHS & NHSMK) Information Governance Assessment Report score overall score for 2010/11was 60% and was graded ‘red’ This national tool kit is compulsory for all NHS organisations to complete. The data from this ‘tool kit’ gives a benchmark concerning how the organisation looks after information regarding our service users as well as information about services and the organisation it self. For the purpose of this submission MKCHS data is joined with that of NHS Milton Keynes which gives feed back as a Primary Care Trust (PCT) The above information in the compulsory section is combined for both organisations. Across the South Central Strategic Health Authority 1 out of the 9 Primary Care Trusts (PCT’s) was graded ‘green’ The average score was 60%, with 3 scoring above and 5 scoring below. We are aware of the key areas that will need improvement over the coming year and have in place a director led action plan to ensure a compliance by the time of the next annual review. On Clinical Coding Error Rate: Milton Keynes Community Health Services was not subject to the Payment by Results clinical coding audit during 2010/2011 by the Audit Commission. 35 Quality Account SECTION THREE Review of 2010/11 3.1 Review of Quality Performance 3.1.1Patient Safety Falls Why is this a priority? We are concerned about the number of falls in one of our in-patient units, which provides care for older people, many of whom have conditions which make falls more likely. It is recognised that if someone falls a subsequent fall is more likely, and that health and wellbeing can deteriorate very quickly after someone has fallen. In one quarter of this year there were 36 falls and in order to understand the causes we carried out an audit of the falls incident reports. For some of the falls, physical factors contributed to the incident; physical frailty was an underlying theme for all patients and it is included separately in this diagram only where it was the primary cause of the fall. Key; Slippers; ill-fitting or not worn Toilet; patient fell in the toilet or because of an urgent need to go Walking aid; two incidents related to patients not using walking aids correctly and the others related to patients not using equipment which had been provided. Did not ask; The patient did not call for assistance in walking Task; patient fell while doing something else (getting dressed, cleaning a sink) Not clear; the incident report included only brief information and contributory factors were not explained. 36 Quality Account The audit also looked at assessment of people’s risk of falling, the care environment, staffing levels, training and the transfer of care between one clinical setting and another, and made recommendations about all of these factors. What are the outcomes from the work developed? We have made a number of changes which aim to reduce the number of people who sustain falls; • The Community Health Service Inpatient Slips, Trips and Falls policy has been reviewed to ensure that it reflects the latest guidance from National Patient Safety Agency. • In-patient units have local procedures that reflect the organisations recommendations. • This particular in-patient unit has purchased stand-alone telecare devices which will alert when those at risk are moving from safe areas. • Training around falls awareness is available for all units and in May 2010 Windsor Intermediate Care Unit which has the most vulnerable services users in relation to falls arranged enhanced training for its staff. • We are working with our partner organisations to improve the quality and timeliness of information given when a patient moves from one service to another. This must include the person’s risk of falling Pressure Ulcers Why is this a priority? This was a priority in 2010/11 and the topic will be included in this year’s quality initiatives to ensure that improvements are sustained. Pressure ulcer prevention is a priority because there has been an increase in patients with pressure ulcers across the NHS; it is also understood that the majority of pressure ulcers are avoidable. n.b. Pressure ulcers are categorised according to severity; Grades one and two are superficial and grades three and four involve greater damage to 37 Quality Account tissues. Grade two ulcers are reported as ‘incidents’ and grades three and four are reported as Serious Incidents and are subject to a full investigation. The topic was included in the CQUIN scheme for the year; it included a measure of the number of avoidable pressure ulcers above category 2 against the baseline. The CQUIN also required at least 90% compliance with national guidance. Audit of MKCH staff undertaking pressure ulcer prevention training is also part of the CQUIN. The threshold for reporting pressure ulcers as Serious Incidents was reduced in 2010 so that now, all category 3 and 4 pressure ulcers must be reported. This resulted in an initial increase in reports, mainly because of increased awareness of the need to report, but is of benefit as it enables pressure ulcer incidents to be investigated thoroughly. What are the outcomes from the work developed? There has been considerable work progressed within the last year including: All category 3 and 4 ulcers now have Serious Incident Investigations carried out. Rolling programme of training in place across the health economy giving an integrated approach to prevention and treatment. Dedicated Pressure Ulcer Nurse working with community nursing staff and nursing homes to improve reporting and documentation Accurate reporting in place to measure prevalence Development of patient education Monitor documentation to ensure that nutritional and pressure risk assessments are in place- training to take place in risk assessments Register of pressure ulcer and risk assessment guide in place for staff 38 Quality Account Pressure ulcer figures for 2009/10 and 2010/11. This shows that there has been an increase in pressure ulcer reporting since last year; an investigation demonstrated that the increase relates to a greater awareness of the need to report ulcers. It is very positive to see that the number of grade three and four ulcers has fallen since 2009/10; we will continue to monitor these trends as one way of determining the effectiveness of improved training and management of pressure ulcers. Infection Prevention and Control Why is this a priority? Effective infection prevention and control standards and avoidance of healthcare associated infections (HCAI’s) are essential to ensuring the safety of patients in our care, wherever their care is provided. We know form speaking with patients and the public during the last year that good infection control and the cleanliness of all of our facilities is really important to them. We are proud of our infection control achievements, some of which are set out below. 39 Quality Account What are the outcomes from the work developed? Hand Hygiene: Studies show that infection rates can be reduced by 10-50% when healthcare staff regularly clean their hands. The introduction of alcohol hand rub has been instrumental in improving hand hygiene compliance in healthcare and is recommended for routine use where hands are not visibly soiled. Hand rubs at the point of care are critical to increasing the likelihood that staff will clean their hands at the appropriate times. Our hand hygiene strategy has included the availability of alcohol hand rub for all of our staff regardless of whether care is being provided in our in-patient settings, health centres or within the patients own home. We continue to embrace ‘bare below elbows’ for all our staff undertaking clinical duties. This requirement has been included in our uniform and dress code policy and all relevant infection prevention and control policies and procedures. Meticillin-resistant Staphylococcus aureus (MRSA) bacteraemia We have made a significant contribution to the reduction in the number of patients admitted to hospital with MRSA bacteraemia. South Central Strategic Health Authority set a standard of no more than 2 cases of MRSA bacteraemias across all community care within Milton Keynes.(MKCHS is one of many providers of health care outside the hospital) We met this target with only two patients diagnosed with an MRSA bacteraemia for 2010/11. Of these two cases, none were attributed to Milton Keynes Community Healthcare Services. Clostridium difficile Incidence of Clostridium difficile is also monitored very closely and reported as a key performance indicator on a monthly basis. A target of no more than 59 cases across community care was set. In total, 29 cases were reported and of these only 3 cases were attributed to Milton Keynes Community Healthcare in-patient services. There is clearly more work to be done to reduce this further, and the work undertaken this year is anticipated to form a 40 Quality Account solid foundation upon which to drive the incidence of Clostridium difficile infection down. Clean environments Improvement of infection prevention and control standards requires a multifaceted approach. It is widely recognised that environmental cleanliness is a key component in the provision of safe, clean care. To this end, in July 2010 the Domestic services integrated fully with the infection prevention and control team. This re-organisation of services has meant much closer working and shared goals, with patient safety and satisfaction at the heart of everything we do. Since July 2010, a key initiative that we have fully developed, is monthly Quality Control (QC) audits of standards of cleanliness in all of our in-patient facilities. Areas are audited against nationally recognised NHS standards and targets. A scoring system is used which gives a clear indication of compliance with the national targets. Whenever standards are found to be below this target, a report with recommendations is issued to the unit manager identifying where improvements are required. The Domestic team, together with the infection control team, the unit manager and clinical staff, work together to ensure that standards improve to an acceptable level by the following month. Integration of the Domestic team with the infection prevention and control team has made this process streamlined and efficient, ensuring that we are all working to one standard that is compliant with the Health and Social Care Act (2008). The graphs below show compliance with the national targets for standards of cleanliness for all of our in-patient areas from July 2010. 41 Quality Account Outcomes of all audits undertaken are formally reported to the Provider Committee on a bi-monthly basis. We are currently engaging with patients and visitors in all of our clinical areas to find out their perceptions of standards of cleanliness. We will use our findings to continually improve the way that we work and enhance and sustain levels of satisfaction for all of our service users. 42 Quality Account Prudent Antibiotic Prescribing One of the innovative pieces of work carried out by the antibiotic pharmacist and IPC team this year, has been the introduction of Guidelines on Diagnosing a Urinary Tract Infection (UTI) in an Older Person. This guideline was developed as it has been shown that older people, particularly within healthcare environments receive antibiotics for a suspected UTI when they do not need them. Older people often have bacteria in their urine with no accompanying infection, this is called asymptomatic bacteriuria, treatment of asymptomatic bacteriuria in older people is not good practice and can cause harm in one out of three people treated with antibiotics for it. In order to improve antibiotic prescribing within the care home environment and to reduce the risk of unnecessary harm, (including Clostridium difficile infection) associated with antibiotic overuse in older people, a guide was compiled from nationally recognised guidelines and translated into easy to understand English for use in the care home environment. This guideline was then adopted and rolled out across primary care including district nursing and MKCHS inpatient settings that look after older people. Comparison of antibiotic audit prescribing in these units Nov 09 to Nov 10 has shown a decrease in antibiotic prescribing of 28%. The antibiotic prescribing related to UTI symptoms has also fallen from 71 to 50%. Improvements were also seen in appropriateness of urine dipstick tests and compliance with PCT guidance on choice of antibiotic prescribed, dose and course length for urinary tract infections. 43 Quality Account This work has been presented verbally at the national Infection Prevention Society Conference September 2010 and as a poster at the North West Antibiotic Pharmacist Group Inaugural Conference in November 2010. At both conferences the work received first prize for best free paper and poster presentation respectively. Safeguarding Children Why is this a priority? Safeguarding Children has been in the national media over the last few years, flagging up devastating outcomes that can happen when systems to protect vulnerable children fail. Working Together to Safeguard Children (2010) is statutory guidance which sets out how organisations and individuals should work together to safeguard and promote the welfare of children and young people in accordance with the Children’s Act 1989 and Children Act 2004. What are the outcomes from the work developed? Milton Keynes Community Health Services has a small team of nurses and a doctor who are specially trained to offer advice, support and training to staff about safeguarding children. 44 Quality Account In the past year the Safeguarding Children Team has: • continued to increase the number of training sessions for staff to make sure they are all up-to-date with what they need to know about safeguarding children. • updated the policy for our staff to follow in line with national guidance • undertaken audits of practice and developed a better process for reviewing safeguarding children cases so we can learn lessons for improving practice. • developed a more robust governance structure within the organisation to monitor safeguarding activity • continued as an active partner in supporting the work of the Milton Keynes Safeguarding Children Board (MKSCB): a multi-agency Board set up as part of the Every Child Matters reforms, which requires all organisations that work with children to co-operate to keep children safe from harm. We continue to increase the number of training sessions for staff to make sure they are all up-to-date with what they need to know about safeguarding children including what to do if they have concerns about a child. 45 Quality Account We are confident that because of this ongoing work ensuring staff have the required skills and competencies it will enable them to identify and take appropriate action when there are safeguarding concerns. This therefore ensures staff are better able to safeguard and promote the welfare of vulnerable children within Milton Keynes. Safeguarding Adults. Why is this a priority? Safeguarding Adults has again been in the news over the last year. The Francis Report into Mid Staffordshire Hospital will now be reopened as a public enquiry, and the NHS Ombudsman reported in February on the care of older people, using ten case studies to highlight concerns. Again, these developments have lead to MKCHS using recommendations contained in these reviews to check and measure our own service provision, even though the cases cited took place in hospital surroundings. What are the outcomes from the work developed? The work of the Safeguarding Adults Board continues after its re launch last year, and MKCHS continues to play a leading part in the running of this and the four sub-groups which report on progress to the main Board. The four sub-groups are: • Policy and Procedure • Training • Quality Assurance and Serious Case Review • Communication and Stakeholder Engagement 46 Quality Account These continue to ensure high level involvement in developments which aim to protect people from abuse or to respond effectively to abuse which is suspected or reported. Last year’s Safeguarding Adults annual report showed a further increase in such cases. This increase is felt to be an indicator that more staff members are now aware of the policy through training and are responding appropriately to concerns. Training provision continues to increase, with the hospital declaring Safeguarding Adults to be a mandatory session for its staff. Three sessions a month are now running, including an induction session for all new staff. MKCHS attendance on these multi-agency half day courses continues to rise, and there have been several requests for targeted sessions where staff cannot be released otherwise. The Clinical Effectiveness Manager for Vulnerable Adults has also addressed volunteer and charity groups both locally and nationally, and has presented a paper on joint Safeguarding Adults work in Milton Keynes at a national conference. What do service users say? LINk MK has representation on the Safeguarding Adults Board and all of its sub-groups to ensure that service users are considered at all points. These developments are continuing to raise awareness of Safeguarding Adults both internally and externally, with the aim of improving the experience of service users. 3.1.2 Clinical Effectiveness High Quality Workforce Milton Keynes Community Health Services employs around 1000 staff, around two thirds of whom hold professional qualifications, either as doctors, nurses, therapists or other technical staff. Why is this area a priority? The key to providing excellent care to those who use our services is to ensure that we recruit and retain a skilled and competent workforce. Most of the 47 Quality Account healthcare budget is spent on staff. Therefore the quality of our staff, how motivated and committed they are to their jobs, can really affect the standard of care provided to patients and service users. It is important to ensure that staff are effectively trained, given opportunities for development and feel engaged in the work they are doing. What are the outcomes from the work developed? We have placed a great deal of emphasis this year on ensuring that our staff receive all the training defined as mandatory – this covers issues such as infection control, load and patient handling and safeguarding children. Currently over 75% of staff have undertaken the training and we continue to work towards increasing this. Our aim is for 87% of all staff to have completed their mandatory training. We have put in place robust monthly monitoring of mandatory training via the Leadership Management Team meeting and performance reports which go formally to the Provider Committee. High levels of Mandatory training is also a key objective for our Risk Committee and therefore this is also monitored on a directorate basis as we know this does impact on the overall ‘risk status’ of the organisation. Further steps being implemented is to hold managers and directors more robustly to account if areas fail to reach the targets set. The table below highlights some results from the national Staff Survey 2010, which benchmarks us to similar organisations. We are pleased to see that staff generally enjoy their work, are well trained and are able to contribute to making improvements at work. 48 Quality Account Issue % 2010 % 2009 % average Similar organisations Staff received health and 93% 86% 83% 75% 32% 47% Staff receiving appraisal 93% 71% 78% Quality of appraisal 46% 33% 38% Number of staff with 84% 62% 68% Staff job satisfaction 93% 86% 83% Able to contribute to 93% 71% 78% safety training Staff received equality and diversity training development plan improvements at work Although there are a few occasions when it s difficult to recruit staff, we have had no major recruitment issues this year, and our turnover rate is reducing. Due to improved planning and management of our services, we have been able to reduce the use of agency staff this year, which saves us money as well as ensuring a good quality service for patients. The rate of sickness absence amongst staff is also reducing overall, although there have been the normal winter ‘flu pressures. We have also reviewed our recruitment processes to ensure that staff are recruited safely and that all the underpinning checks are in place. All qualifications, registration details and permits to work are checked before an individual is allowed to start work. An online process for giving CRB clearance has also enabled us to speed up the process by several weeks, reducing the gap between one person leaving and another taking up post. 49 Quality Account The Productives Why is this a priority? The Productive Ward is a national initiative by the NHS Institute for Innovation and Improvement to remove waste from clinical area and release time to spend on direct patient care. The Program aims to: • Ensure every patient has a good experience • Improve patient safety and clinical outcomes • Offer a systematic way of measuring quality and patient outcomes • Equip frontline staff with known improvement methods • Develop staff capability for improvement and productivity • Address the NHS reforms and wellbeing agenda • Reduce variations in practice in core procedures What are the outcomes from the work developed? Milton Keynes Community Health services has been rolling out the productive ward program across four key in-patient areas over the past two years • Windsor Intermediate Care Unit. • The Older Peoples Mental Health Unit and • Hazel and Willow Wards of the Campbell Centre All units have made good progress with rolling out the modules of the program. The most obviously successful has been the well organized ward which produced demonstrable improvements in: • Clearing out sorting and organizing a range of working areas • Developing standardized procedures for tasks such as administration of medicines, cleaning patient equipment, • Producing minimum stock levels lists reducing time spent ordering and reducing the costs of over stocking. • Improving the working environment for staff reducing potential for stress. In addition the meals module for example has been completed by all wards supporting the work across the organisation on nutrition and hydration, the 50 Quality Account medicines module also has been completed by all wards improving medicines administration processes to improve patient safety and reduce errors and improve effectiveness of medication therapy. More recently the organisation has commenced roll out of ‘productive community ‘ which will use the same systematic approach to improvements. How patient feed back makes a difference During one of the regular weekly community meetings at The Older Peoples Assessment Service (TOPAS) which involves patients relatives and staff, there was a guest presentation and discussion about the nutritional needs of older people who are restless and agitated. One patient involved in this praised the unit for introducing a range of snacks and fruit which gave free access to the increased calories these patients needed, but the patient felt that this could be further improved. They suggested a greater range of health snacks such as fruit smoothies, cheese and biscuits and drinking yogurts. Following some discussion on how these foods could be stored it was agreed the unit would buy a small glass fronted fridge which would be kept in the dinning area. This would allow patients to see what was in the fridge and help them selves. The fridge is now a permanent fixture, is check and stocked on a daily basis and is well used by patients. By acting on patient feed back the unit has been able to further support good nutrition for patients. Clinical Audits Why is this a priority? Clinical Audit is considered by the CQC to be the ‘gold standard’ for determining whether clinical treatment and care is in-line with best practice and policies. People who use our services have been very keen to see the results of audits which have been discussed at our Clinical Audit Patient Panel and have helped to determine what should be in our Patient Experience Strategy Campaigns. MKCHS has a robust program of audits for all clinical 51 Quality Account services; audits of care records, safety and consent are mandatory and we also conduct audits where we know, from external reports and incidents or complaints, that there might be a risk. What are the outcomes from this work? Some of our audits were described in section two of this document and all are available on request. An example is given here to illustrate the link between patient safety incidents, clinical audit and the patient experience strategy. The audit reviewed all medication incidents during quarter 1 of 2010 from all clinical service areas; the study was conducted to provide information to support organisational learning and to facilitate improvements in processes and communication. The audit showed that Incidents were less frequent in areas with: • • • • • • Good support from pharmacy advisers (technicians and pharmacists). There was evidence of very good support in many settings, particularly mental health. An effective approach to the management of incidents; for example WICU reviews all incidents on a regular basis and develops action plans where necessary. This is effective in preventing recurrence. Prompt reporting and reflection; there were some excellent examples where this had minimised the impact of incidents e.g. in District Nursing and Oakhill where it had supported a staff-member’s learning. Training; there was evidence of good practice across many service-areas together with evidence which suggests lower numbers of incidents where training is in place. Clinical supervision of staff particularly when there has been an error. This needs to strike the right balance between supporting the staff member and performance management if necessary. Effective communication between prescribers and administrators of medication; this has been shown to reduce the likelihood of incidents. Communication breakdown was a feature in some incidents in the community where DNs and Local Authority staff have different working practices; it was also an issue at a service where roles and responsibilities of staff from different organisations are not always clear. There were several recommendations, one of which was to carry out further work on medicines, to understand the issues from the service-user perspective. 52 Quality Account 3.1.3 Patient Experience Patient Experience - Patient Information Why is this a priority? As an organisation it is vital that we ensure that service users, or those acting on their behalf, have sufficient information to enable them to make informed choices and decisions about the services they access and any treatment they receive. In order to ensure that this happens, and that MKCHS is compliant with CQC Essential Standards of Quality and Safety and the DH Information Standard, patient information was agreed as a priority campaign of work. A work group was established to develop a patient information strategy and guidelines for development of patient information that would result in: • The provision of good quality, timely information about services, care and support, in appropriate language and format. • A consistent approach to developing, distributing and reviewing service-user information • Partnership working with service users as well as other agencies in the development of service user information • Service users being engaged with and given timely, appropriate information before, during & after care What are the outcomes from the work developed? 1. A Patient Information strategy and action plan enabling work to commence on developing new guidelines for creating patient information. 2. Service users’ views influenced the direction of the strategy and action plan from the outset through: • active participation in the workgroup through 2 LINks MK representatives 53 Quality Account • feedback from public consultations • Workgroup representatives giving accounts of their service user views and needs (e.g. RNIB, Deaf Community, young people & children, older people). 3. New leaflet templates have been produced for services that are more ‘author-friendly’, addresses local issues such as alternative formats and also satisfies Equality & NHS Brand standards. 4. An audit and database of patient information leaflets in use by MKCHS Next Steps A New guideline for producing patient information is currently being developed. This guideline includes an agreement on the information that must be made available to service users and the requirement to proactively consult with service users and other stakeholders. An audit encompassing service user views will be conducted following implementation of the guidelines and the production of new patient information, Patient feed back from listening events For the deaf community, a large number will be unable to read letters or leaflets, either because they have limited literacy or because the way in which the deaf community structures sentences and use BSL (information obtained from consultation with deaf and visually impaired community re: council and health services) Many of the people at the event had perceived that they had received a poor service as a result of their blindness or partial sight. None had felt able to complain and questioned whether we produce our complaint information in different formats? (Information obtained from a LINk event which was held in conjunction with the RNIB) Need to involve other LINks members in evaluating forms and leaflets and have more communication with carers (focus group held with representatives including patient, Age Concern, MK Carers, and LINks re: End of Life Care) 54 Quality Account National NHS Community Mental Health Service Users Survey 2011 Detail from the 2011 results of the above survey has shown a marked improvement in the care and treatment of peoples with mental health problems locally. Our results compare more favourably than the national average for some aspects of our interventions, for example: • 70% of those surveyed had been seen in the last month in comparison to 60% of people surveyed nationally. • More people know who their care co-ordinator is. • More people report being able to express their views at care planning meetings and find their review helpful. The survey supports the need to focus further on medication and talking therapies. These are areas of development that we have already started work on by investing in staff training and development and the creation of more non medical prescribers. With this investment we should see more staff who can advise service users on all aspects of their medication, as well as give greater emphasis on the use of psychological interventions and talking treatments which will result in a better patient experience. This Year’s Patient Experience Strategy aimed to produce real, measurable improvements in topics which we know (from incident reports, complaints and reports from other organisations) can be a cause for concern. As described earlier, some of these topics will need further work in 2011 to ensure that improvements are sustained. Examples from the Patient Experience Strategy are given below. 55 Quality Account Patient Experience - Medicines Management The Mental Health Pharmacy Team has seen a number of developments this year targeted at improving medication safety and ensuring the best use of medicines. Why is this area a priority? The priority for our patients is to ensure that they have their medicines when they need them, in a safe way and that wherever possible they have information about the medicine being prescribed made available to them or those acting on their behalf. What are the outcomes from the work developed? In line with the national Medicines Reconciliation Initiative we strive to ensure that our patients are prescribed the right medication on admission to hospital. A six month study was conducted to assess our compliance with this and the results showed that in the majority of cases this took place. Over half of the patients were involved in this process, an example of excellent practice working with a challenging cohort of patients. Some excellent work has been conducted in response to the National Patient Safety Alerts related to the safe use of medicines. A new policy on Lithium and Mood Stabilisers have been developed and a booklet for patients newly prescribed lithium will shortly be made available. Patient Experience: Transfer of Care Why is this a priority? The Patient Experience Strategy identified Transfer of Care as one of its first priorities last year after an audit of transfers from the hospital to MKCHS. The audit was triggered by a rise in reported incidents which identified problems in transferring patients. 56 Quality Account What are the outcomes from the work developed? Part of the response to this audit within MKCHS was the commissioning of a new policy to underline a commitment to multi-agency working in transfers of care. This now nears completion in agreement with health and social care statutory agencies, and MKCHS is also developing its own internal policy to reflect the provisions of the wider document. Together, these policies will make clear the agreed components of any transfer of care, wherever it occurs and whichever services are involved. Key areas at this stage are felt to be improved inter-agency communication and forward planning, which have been the subjects of previous audits. Training sessions have been developed to share information to support joint planning and understanding of transfers of care. These will be open to all health and social care staff who are engaged in such transfers. It is hoped that these will be widely attended to share knowledge and good practice. What do service users say? Work carried out for the Patient Experience Strategy has underpinned these developments. Here, work is on-going to develop a format that will allow service users in all clinical areas to report on their experiences of transfers of care. Within MKCHS, these transfers will fall into one of three categories: • From MKCHS clinical services to another agency or vice versa (for example, from the Older Peoples Assessment Service (TOPAS) to a private nursing home); • Between MKCHS clinical services (for example, from the Windsor Intermediate Care Unit (WICU) to community nursing services); or • Between sections of one MKCHS clinical service (for example, from adult mental health services to older peoples mental health services). It is hoped that the interviews will be representative of all three of these categories and that enough respondents can be found amongst service users to provide important feedback on how transfers of care are experienced currently. 57 Quality Account Service user feedback and involvement is key, and a representative from LINk MK is being sought to act as a conduit for policy and other developments in this area. Without such involvement, work would not be able to be responsive to those who experience them. Nutrition & Hydration – better patient care better patient outcomes. Why is this a priority? Nutritional care is fundamental to patient dignity and human rights. The nutritional care of in patients is a top priority for us as it ensures our service users have better treatment outcomes if they have appropriate and sufficient food and drink when in our in patient units. What are the outcomes from this work? There has been considerable work undertaken over the last year in MKCHS. The nationally recognised Malnutrition Universal Screening Tool (MUST) has been rolled out across MKCHS across inpatient areas and for those patients, identified as at risk, in their own homes. Four community wards have been participating for the past 2 years in the Productive Ward program and all areas have completed the Meals Module. This has resulted in some innovative developments in the delivery of good nutritional support for patients. There is a protected mealtime’s policy in place across all inpatient units and implementation of this is audited on an annual basis. An annual nutrition audit is undertaken to ensure that the trust nutrition policy is being implemented consistently across in patient units, these are: • Windsor Intermediate Care Unit (WICU 20 beds) • The Older Peoples Assessment Service (TOPAS 20 beds) 58 Quality Account • The Campbell Centre (36 beds). • Oakwood (6 beds) The audit (completed February 2011) demonstrates significant improvement across all areas with 100% of patients having their nutritional status assessed following admission to the unit across the first three areas and 80% in Oakwood which is a Learning Disability Unit. This is the first year that Oakwood has been assessed and given the size of the unit (6 beds) the 20% relates to one patient who refused to be weighed on admission. While these audits are useful in demonstrating that specific aspects of the policy and good practice is being implemented, they do not reflect if patients are actually experiencing the care and support they want and need. As a consequence, a survey has been completed by in-patients to capture their actual experiences of nutritional care. What did patients users say? Patient’s responses showed that there was a high level of satisfaction with access to and quality of the food and beverages provided on all units. While all of the units provided 24/7 access to food and beverages one or two patients expressed that they were not aware of this or how to access it. A recommendation from the survey generally was that units need to make this clear to patients on admission and throughout their stay. Patient Environment Action Team (PEAT) Audits Why is this a priority? Every year all NHS Trusts in the UK are required to undertake an in-depth audit of all in-patient settings which have 10 beds or more. The PEAT audit programme is managed by the National Patient Safety Agency (NPSA) and as from 2011 the data submitted from these audits will be released to the public as an official statistic. PEAT data is also used as a highly valued performance 59 Quality Account tool by the Care Quality Commission, contributing to five outcomes on a Trusts ‘Quality Risk Profile’. Within Milton Keynes Community Health Services (MKCHS) three premises qualify for PEAT audit, the Campbell Centre, Windsor Intermediate Care Unit and TOPAS (The Older People’s Assessment Service). As PEAT is an audit focusing on the ‘patient perspective’ therefore MKCHS ensures patient representation on all audits. In addition the PEAT Lead has undertaken a training session on PEAT with the LINk MK and plans to make this an annual event. What are the outcomes from this work? Following a PEAT audit an action plan is developed, issued and followed up by the PEAT Lead. Any serious concerns that are flagged are dealt with as a matter of urgency on the day of the audit. Meetings are held with the relevant service managers to progress the action plans and updates are also supplied to the Infection Prevention & Control Committee (IPCC). As the PEAT audit programme takes place between January and March of each year, with scores being released in early spring, the 2011 data is not yet available to publish. Below is a table showing the data from 2006 to 2010. Table 1 – PEAT scores 2006-2010 2010 PEAT Section Campbell Centre TOPAS Windsor ICU Environment Good Good Good Food Good Good Good Excellent Good Excellent Campbell Centre TOPAS Windsor ICU Environment Excellent Excellent Good Food Excellent Good Good Privacy & Excellent Excellent Excellent Privacy & Dignity 2009 60 Quality Account Dignity 2008 2007 2006 Campbell Centre Ward 14 Windsor ICU Environment Good Acceptable Good Food Excellent Excellent Acceptable Campbell Centre Ward 14 BCH Environment Good Acceptable Acceptable Food Excellent Excellent Excellent Campbell Centre Ward 14 BCH Environment Poor Acceptable Acceptable Food Good Excellent Good Note: Prior to 2009-10 audit programme Privacy & Dignity score was incorporated into Environment section The new patient weighing and nutritional assessment sections which caused the ‘Food’ scores to drop in 2010 have significantly improved in 2011, with two of the three sites likely to return to ‘Excellent’. In addition the element which kept TOPAS from getting an ‘Excellent’ in ‘Privacy & Dignity’ in 2010 has been rectified. Overall ‘Environment’ scores are likely to remain the same despite improved section scores in two of the premises. As PEAT is a national tool it is useful to compare the 2010 data with the national averages for NHS trusts: Table 2 – PEAT 2010 data national comparison PEAT Campbell Section National Average Centre TOPAS Windsor ICU Environment Good (62%) Good Good Good Food Excellent (57%) Good Good Good Good (48%) Excellent Good Excellent Privacy & Dignity 61 Quality Account For more information on PEAT please contact: Lee.Peddle@mkpct.nhs.uk Or visit: http://www.npsa.nhs.uk/nrls/improvingpatientsafety/cleaning-andnutrition/peat/about-peat/?locale=en PEAT 2011 Although MKCHS has now had formal notification of the 2011 PEAT results we are unable to publish them within this Quality Account as they have not been formally released for general publication. However we can indicate that our position from the 2010 results has improved. What patient said during the PEAT Assessments for 2011: Windsor Intermediate Care Unit ‘The staff are very friendly, accommodating and take time to talk to you’ ‘You are made to feel at home’ ‘The food is good and drinks are available on request’ The Older Peoples Assessment Service (TOPAS) ‘I’ve no complaints the food is good’ ‘Very nice food!’ 62 Quality Account 3.2 Statements from Local Involvement Networks (LINks), Health and Community Wellbeing Select Committee and NHS Milton Keynes. NHS Milton Keynes ( Local commissioners of NHS care) NHS Milton Keynes has reviewed the MKCHS’ Quality Account. All of the nationally mandated elements of a Quality Account are covered and there is evidence that MKCHS has used both internal and external assurance mechanisms. NHS Milton Keynes is satisfied as to the accuracy of the data contained in the Account. The account identifies significant progress in relation to: 1. Low rates of MRSA and C Difficile / PEAT 2. Safeguarding Vulnerable Adults & Children 3. Antibiotic prescribing MKCHS have identified in their quality account a number of improvements linked to the experience of patients: 1. Use of clinical audits 2. Implementation of a Patient Experience Strategy 3. Implementation of the Productive Ward Initiative 4. Learning from falls and pressure ulcer incidents NHS Milton Keynes was pleased to note the achievement of all CQUIN schemes in 2010/11 and the impact that this will have on patient care. NHS Milton Keynes will continue to work closely with MK CHS and support their ambition to achieve excellence in the quality of care provided to patients, through quality monitoring, incentivising (through CQUIN Schemes), and performance management. We believe that this coming year will be even more challenging both clinically and financially but I am sure with the commitment the trust has built that we will see further improvements in quality. Health and Community Wellbeing Select Committee ( Milton Keynes Council) The Panel welcomed the document, which it believed was readable and easy to access by members of the public and as well as giving a fair and frank assessment of performance, included examples of the patient experience. The Panel noted that the Service had conducted / been part of a number of detailed audits and recognised where improvements needed to be made, although in places the document failed to detail the actual areas to be improved. Specific examples identified by the Panel of where improvements 63 Quality Account were being made were in communications, both between prescribers and administrators of medication and between different service providers. The Panel also welcomed the attention being given to the issues around prescribing antipsychotic medication and that a checklist was being introduced to ensure that physical checks were undertaken to quickly detect any harmful side-effects. The Panel recognised the apparent success in implementing the Productive Ward initiative and the success in achieving all of the CQUIN Standards. However, the Panel suggested that the 5 patient Experience Strategy Campaigns (CS2) could have been named for clarity and information. The Panel particularly welcomed the work being done to reduce the number of injuries caused by falls. The Panel would have liked to have seen greater emphasis being given to how engagement between different services was being taken forward to ensure that the transfer of care was handled smoothly. It was noted that the role of the GP in the transfer of care was not mentioned. With regard to the outsourcing of services the Panel would expected to see details of how service quality was monitored and maintained at a required standard. Also the Panel noted the concerns of users at apparent reductions in the podiatry service, which had seen not only a reduction in services available, but also longer waiting times. It was also believed that the changes to the service had been poorly communicated. The Panel believed that the document would be even more useful and informative if further contextual details were provide such as patient numbers, together with benchmarking information and trend data. On a more minor note the Panel found the use of the abbreviation N/A and thought that vas a general rule abbreviations should be avoided. Generally the Panel believed that, to help the public to understand and use Quality Accounts, it would be helpful if there was a standard template / format used by all health providers. Milton Keynes Local Involvement Network (LINks) We would like to acknowledge the efforts of Milton Keynes Community Health Service in producing a comprehensive, open and wide ranging report on Quality Accounts as well as take this opportunity to thank them for involving LINk:MK and its members in its work in the past year. LINk:MK enables the voice of the patients and the public to be heard and taken into account in the design and delivery of health and social care services. We are pleased to note that Patient Experience has been taken on as a priority and efforts are being ploughed into seeking feedback from service users to help make service improvements as well as maximise patient satisfaction. We are also pleased to note that access to health care services by the hearing impaired and the visually impaired have been classified as priorities to achieve 64 Quality Account real, measurable improvements in the coming year and we look forward to working together to achieve this. We would also like to acknowledge MKCHS achievements in Patients Safety in the areas of preventing Pressure Ulcers, Infection Prevention and Control as well as Prudent Antibiotic Prescribing. We also sincerely hope that the new commissioning policy on Transfer of Care that underlines a commitment to multi-agency working is completed successfully and the internal policy within MKCHS is developed at the earliest so as to provide clarity to the components of transfer of care encompassing all services. LINk:MK would also like to congratulate the commitment of MKCHS in successfully conducting the PEAT (Patient Environment Action Team) Audits that focuses on the ‘patient perspective’ on the quality of inpatient settings in premises and would also like to place our sincere thanks in involving LINk:MK members every year. LINk:MK is pleased to note the priorities for 2011/12 and would urge MKCHS to continue to focus and aim to make significant improvements in involving service users as well as in the communications with regard to services that are being transformed or reduced. It is in this context that LINk:MK is looking forward to work LINk:MK Responsewith MKCHS in the coming year and in particular with regard to the provision of Podiatry Services, which is an area of great concern to LINk:MK. MKCHS Quality Accounts shows dedication in involving patients and the public in the design, development and delivery of health and social care services including continuous efforts in making service improvements. We are equally committed in extending our help and support to MKCHS in the future to enable the citizens of Milton Keynes to participate and influence the commissioning and delivery pathways across all of their services. 65 Quality Account 3.3 How to Provide Feedback on the Account Your comments and feedback are always welcome and will help us to shape the future healthcare provision in Milton Keynes. If you wish to comment or provide feedback on any aspect of this document please contact the Communications and Engagement Team on Tel: 01908 278801 or email communications@mkpct.nhs.uk 66