“ This was our first experience of the Hospice. We... care, support and commitment provided by all staff and
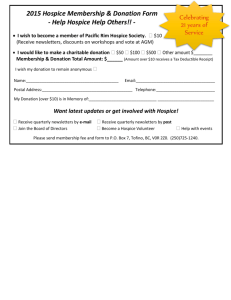
advertisement

“This was our first experience of the Hospice. We found the care, support and commitment provided by all staff and volunteers to be of the highest quality. You gave our dad, husband, brother, dignity and respect at a difficult time in his life and we cannot thank you enough for that.” 1 Statement from the Chief Executive Page 3 Our vision, purpose and values Page 4 Summary of Services Page 5 Priorities for Improvement 2014/15 Page 6 Other Improvements in 2014/15 Page 9 Clinical audit, Hospice Activity and Complaints Page 12 Accidents and Incidents, Key Quality Indicators Page 13 Patient and Family Experience Page 14 Priorities for Improvement 2015/16 Page 14 Statements from the Care Quality Commission Page 15 2 The care The Hospice of St Francis provides is very special. Our dedicated staff team work tirelessly to ensure we provide a secure, safe and welcoming environment at the Hospice to look after those with life-limiting illnesses and are active in improving end of life care for all in our community. The Inpatient unit is always busy and occupancy of our 14 beds is at 88% with the number of non-cancer patients continuing to rise. Our clinical team receives continuous training and education to ensure they are able to advise on, and implement, latest developments in palliative care. This is vital as we are seeing more patients with complex physical, psychological and social requirements and need to provide appropriate support. This year, we have working even more closely than ever before with GPs, district nurses and our local hospitals to share best practice and work collaboratively to ensure that everyone in our catchment across Hertfordshire and Buckinghamshire has access to good end of life care. We remain committed to maintaining our high standards and rigorous quality control in order to continue to deliver our exceptional care in all areas of Hospice life. Charles G Toner Chairman of the Board of Trustees. I became CEO at the Hospice of St Francis in March 2015 and witnessed at first hand the outstanding compassionate care that the team of professionals and clinicians give to our patients and their families. I am very proud of the commitment of all our staff to constantly improve the way we care for patients with life limiting conditions, their families and friends. Our staff, volunteers and Trustees have developed our values which are fundamental to everything we do. We now use these to underpin the recruitment and selection criteria for all our new staff and volunteers. Our values are listed later in the report and they reflect the quality of care you will see in this document. We are in the process of implementing new governance structures through my new Executive Team who are responsible for the senior management and leadership of the Hospice. I believe that we demonstrate through this report our performance for last year and our plans for the next 12 months. This has been endorsed by our Board of Trustees and is, to the best of my knowledge, an accurate description of the quality of care at The Hospice of St Francis. Steve Jamieson, CEO 3 The Hospice of St Francis Quality Account provides an opportunity for all stakeholders to monitor and openly scrutinise the process by which we seek, year on year, to improve the quality of the services we provide. Our Quality Account is an annual report of – An introduction to the Hospice of St Francis Clinical Governance, our services and our commitment to quality Our progress on last year’s priorities Looking forward and setting our priorities for the coming year 2015/16 Development of our quality priorities 2015/16 Improving quality is a high priority for the Hospice of St Francis and it is important that we are able to develop meaningful quality indicators that we will identify for future development so that they can be monitored, reported and scrutinised by all. Quality Account Governance Arrangements The Director of Care and Clinical Development has the responsibility for the content of the Quality Account and this is overseen by the Chief Executive and the Board of Trustees. The Hospice data quality is assured through audit processes both internal and external. Our vision is of a community where people live well until the end of their life and where nobody dies afraid or in pain. Our mission is to transform the experience of illness and death, through care, education, innovation and engagement with our community. Be at the heart of communities Respond to personal preferences and needs Deliver high quality and holistic accessible care Be effective and use resources efficiently Influence the quality of care through education Collaborate with other health and social care providers Enhance the capacity and resilience of communities through volunteering 4 Following consultation with our staff and volunteers the Hospice Values were developed and shaped and are now embedded into every aspect of hospice life. Respectful Relationships We create a caring and compassionate environment: demonstrating appreciation and respect in all our interactions, and taking account of individuals’ needs and circumstances. Constructive Communication We encourage open, clear and honest communication, where everyone can be heard. Excellence through Innovation We strive for excellence in everything we do; encouraging innovation, maximising opportunities and exploring fresh ideas in order to see continuous improvement. Integrity and Trust We act with integrity, building trust by demonstrating our loyalty to the Hospice, its people, aims and vision. Encouraging Learning We educate and develop to enhance knowledge and skills, improve performance and help people reach their potential. Sustainable Service We aim to provide a professional and sustainable service, which is fair, efficient and co-ordinated. Community Engagement We involve and engage with our community, building mutually supportive relationships which maximise our contribution. Inpatient care (14 beds) – which provides 24 hour care and support by a team of specialist staff The Spring Centre – this provides wellbeing and rehabilitation services to patients with stable and advancing illness, their carers, family and friends Outpatient service – consultations with a doctor, clinical nurse specialist or therapist Community services – which provide specialist support and advice in a patient’s home or in a care home Education – to promote excellent hospice care within other settings Bereavement Care, including support for children. Doctors including medical consultants Nurses and healthcare assistants Therapies to support independence and promote comfort including o Physiotherapy o Occupational therapy o Complementary therapy o Creative arts therapists Social workers provide specialist support and counselling Spiritual care services supporting patients and their families Bereavement services for adults Children’s support team to provide pre- and post-bereavement support 5 In 2014/15, the Hospice planned to address the following key priorities for improvement in each of the quality indicators. 1. Patient safety In 2014/15 we said we would improve some of the processes around patients’ nutrition and improve infection control. The following steps have been taken to address this: Nutrition The Nutrition Matters Group was formed with clinical staff and kitchen staff to discuss nutritional issues regarding patients’ needs. This group discussed the need for protected mealtimes for patients, and for a better internal system, with help from the kitchen volunteers to record patients’ preferences and food intake. A Macmillan Dietician was appointed in 2014 to complete a 9-month scoping project to assess dietetic needs across both Peace Hospice Care and The Hospice of St Francis. Six months into this development the project has highlighted assessment and education as the priorities for clinical staff. An Expression of Interest proposal for Part 2 of the Dietetic Pilot Project has been made to Macmillan for approval. Infection Control The Hospice has signed a new contract with a different cleaning company starting in April 2014. A rigorous training and supervision programme has been regularly provided, with clear documentation and an auditable trail to demonstrate that the Hospice is a clean and safe environment. 2. Clinical effectiveness In 2014/15 we said we would develop a service for patients with prostate cancer, we would develop a Hospice Champions Project in Watford General Hospital and introduce Healthcare Assistants into the community team. The following steps have been taken: Prostate Cancer Specialist Nurse In February 2014 a prostate cancer specialist nurse was appointed; this has helped us in our aim of reaching more patients at an earlier stage in their illness, and providing them with tools to understand and manage their condition more effectively. The prostate cancer nurse has set up self-management clinics and support groups in collaboration with Peace Hospice Care which is a neighbouring hospice. This was initially funded by Prostate Cancer UK and is now a substantive post at The Hospice of St Francis. Prostate Cancer UK created a video with the Hospice and patients and this was showcased nationally as an innovative way of reaching more men with prostate cancer. Hospice Champions Project This project was a year long collaboration with Peace Hospice Care and West Hertfordshire Hospitals Trust and aimed to train and support hospice champions on selected wards to affect change at a local ward level and promote excellent end of life care. During the year, the post holder trained over 500 staff and was able to initiate the Rose Project within the Trust. This aimed to promote dignity, respect and commpassion at the end of life through the use of an end of life care symbol, which for the Trust was a pink rose. 6 Healthcare Assistants in the Community Team A business proposal was accepted by our Board of Trustees which supported the introduction of Palliative Care Healthcare Assistants to provide hands-on care and emotional support to patients and their families who are at home. This type of care is particularly important at end of life or in a crisis. The Healthcare Assistants have proved to be an invaluable part of the team enabling the community specialist nurses to focus on more complex problems and for families to feel more supported at home. 3. Patient experience In 2014 we said we would develop new ways for patients and their families to feed back their experience of care. As a result we are now conducting Real Time Reporting surveys and the Fifteen Steps Challenge. Real Time Surveys ‘Real time” surveys are a short list of easy-to-answer questions to help patients, carers, families and others who use the services of the Hospice to tell us what they think of the care they receive. We are doing this: To receive feedback on the quality of our care from those who use the Hospice. To help us understand how well we are meeting the needs of all our service users. To enable us to respond quickly to concerns to improve our care. To help us demonstrate the quality of the services we provide. We carry out this survey using trained volunteers who: Can help to complete the form or answer any questions raised. Can record answers on paper or an iPad. Safeguard anonymity of response, ensuring that there is no obligation on the patient or carer to take part. Feed back survey results to the Hospice staff for evaluation and review. The Fifteen Steps Challenge The purpose of this tool is a series of questions and prompts to guide you through first impressions of the Inpatient Unit. The challenge helps gain an understanding of how patients feel about the care provided and how high levels of confidence can be built. The tool helps organisations understand and identify the key components of quality care that are important to patients and carers on their first contact to the Ward. The purpose of the Fifteen Steps Challenge is to – Help staff, patients and other to work together to identify improvements that can be made to enhance the patients’ experience. Provide a way of understanding patients’ first impressions more clearly. Provide a method for creating positive improvements in the quality of care through identifying what is working well and what can be improved. Associate Members (an identified group of committed volunteers who are advocates for the Hospice) were trained to complete the Fifteen Step Challenge alongside the Head of Quality and Patient Experience and the Clinical Audit Nurse Specialist Lead and a Fifteen Step Challenge action plan was devised and presented to the Clinical Leadership Team. Actions include reviewing the signage to the Hospice in the roads approaching the building and also internal signage for patients and families within the Hospice. This challenge will be repeated on a yearly basis. 7 8 This report is based around our 3 main quality indicators: Patient Safety Clinical Effectiveness Patient and Family Experience 1. Patient Safety a) Incident Reporting The Hospice has now streamlined the way that all incidents, accidents and near miss events are reported with a new Incident Reporting Policy. This enables the Hospice to have an improved method of rating each incident in line with the National Patient Safety Agency matrix. This ensures that team leaders can review the incidents to reduce recurrance and other associated risks and thereby improve safety. This new process also ensures that there are mechanisms to report incidents to the right internal groups (and external agencies) and thereby disceminating lessons learnt throughout the whole organisation including the Board of Trustees. b) Mattresses Following a pressure ulcer review we identified a need to purchase brand new mattresses for the Inpatient Unit. This was part of a programme to replace all the mattresses, which was completed in March 2015. We sought advice from the Tissue Viability Nurse team prior to purchase. 2. Clinical Effectiveness Care Planning and Documentation Review During 2014/15 we reviewed the way we document care plans and decided to have a mix of electronic and paper to ensure ease of access for the clinical team while they are caring for patients. The paper copies also provide an opportunity to discuss individual care plans with patients as well as support the prevention of falls and pressure ulcers. Increased access to wellness and palliative rehabilitiation for patients and families. The Spring Centre had a successful second year in operation. This has been a joint project with Peace Hospice Care, supported by Macmillan Cancer Support which seeks to support more patients earlier in the palliative trajectory, promoting wellness and self management. It aims to enable patients and families to have greater resilience in the face of a serious illness and to enable future planning and better understanding of hospice service for their potential future use. 2013/14 Average number of patients using any service/ month = 113 2014/15 Number of patients using any service/ month = 152 The numbers of patients using our services have steadily risen since opening in 2013 although appears now to have plateaued in line with our capacity and our vision to expand our services to reach more people, both by facilitating patients to travel to the Spring Centre, and by working with partners so that our staff can reach patients in different settings. Partnership working with Carers in Herts, YMCA and Macmillan CAB enables us to offer opportunities to patients and carers whom we would otherwise not be able to sustain and we continue to consider further partnerships to enable sustainability and development. 9 Hospice Pharmacist The Hospice of St Francis appointed a Speciality Pharmacist who has completed a prescribing course to become an Independent Prescriber. This allows her to prescribe and advise our clinical team on medicine management which has contributed significantly in patient safety regarding complex medicines and saving costs to the Hospice budget. The Pharmacist sees outpatients in the Spring Centre, taking their drug history and monitoring them for any side effects and any drug interactions. The Pharmacist advises GPs and the Community Palliative Care Team in the care of patients in their home focusing on patient medication and compliance. Herts Neighbours Project This is a collaborative project led by the Peace Hospice, including Hertfordshire Community Trust, Hertfordshire Social Services and The Hospice of St Francis following a successful bid for funding from the Cabinet Office from their End of Life Social Action fund. It is a year long, research based project, which is being evaluated by Lancaster University. The project aims to recruit and train 60 volunteers who will be matched with people who may be in the last year of life who require practical assistance or emotional support. Workforce resilience Schwartz Center Rounds® In 2014 we held 5 of these Rounds where clinical staff and volunteers were encouraged to attend. These case reflections are targeted to discuss and explore how the clinical care scenario made the staff member feel and act. On average 50 internal and external participants attended each time. Subjects have included: - Whose bed is it anyway? - The dilemma of wanting to make things perfect in an imperfect world - He who shouts the loudest - When death is all around - When it’s the small things said or done that have the most impact. Evidence has shown that Schwartz Center Rounds® result in greater cohesion of teams, along with increased empathy, staff resilience, and mutual understanding of professional roles. They also provide protected time for staff to continue their own professional development on the Unit. Clinical Supervision Clinical supervision is offered to all of our registered nurses and HCAs (including Bank Staff) using a group supervision model. Students at the Hospice We have increased our student intake from the University of Hertfordshire following the appointment of our Director of Education and Research in spring 2015. We have also introduced a rota of medical students allocated to the Medical Director and the team including two Social Work Students on placement. 10 An Audit, Survey & Research Register is maintained and regularly updated, detailing the work that staff at the Hospice have initiated or are involved in, both internally and externally. All audits are led by the Hospice’s Audit Clinical Nurse Specialist and are discussed at the Hospice’s Clinical Leadership Team meetings and results are reported to all relevant staff with action plans in place where necessary. For the year 1st April 2014 to 31st March 2015, 27 new projects were registered. Audits included: Infection Control Health and Safety Medications Nutrition Safeguarding Pain and bowel management Inpatient admission documentation Review of patient discharge from Inpatient Unit REVIEW OF HOSPICE ACTIVITY DATA Overall Service – Patient Care Referrals to Inpatient Unit, Community and Spring Centre % of non cancer diagnosis (new referrals) Inpatient Unit Number of admissions Average length of stay (days) Spring Centre Total Attendances Clinical Nurse Specialist outpatient appointments. Medical outpatient appointments. Allied Health Care Professional outpatient appointments. Community Community Nurse Specialist domicillary assessments Medical domicillary assessments. Allied Health Care Professional domicillary asssessments Clinical Support Services Adult bereavement service contacts Children’s bereavement service contact Complementary Therapy Contacts 2013/14 2014/15 673 24 700 28 298 13 341 11 1765 270 117 511 2980 454 142 803 2325 49 416 2342 35 813 1238 730 319 1283 630 385 The Hospice received two formal complaints during this year and both were concluded in line with the Hospice Complaints Policy. In both cases, the complainants did not want to take the matter further. Hospice staff have diseminated the learning from these complaints and, as a result of one of them, invested in extra equipment. 11 All accidents, serious incidents, significant events, safety incidents and concerns/constructive comments are reported using the new Incident Reporting Policy. They are all then graded, registered on a Hospice database and investigated. Action plans are written for those that are rated Amber or Red, using the National Patient Safety Agency matrix. Reports are discussed at the Health & Safety Group, Clinical Leadership Team and the Clinical Care Committee and the Board of Trustees. There were 237 completed forms relating to patients, staff, volunteers and families during 1st April 2014 – 31st March 2015. Documentation on Crosscare was checked and assessed in all clinical cases and family and carers were made aware of any incident. There were no Serious Incidents to report during 1st April 2014 – 31st March 2015. KEY QUALITY INDICATOR (KQI) Number of patients who expressed a preference about their preferred place of death Complaints Total number of complaints Patient Safety Internal drug incidents/near misses* Number of slips, trips and falls* Number of patients with a documented Grade 2 pressure ulcer either on admission or developed whilst in the Hospice * Number of patients developing a Grade 3 pressure ulcer within the Hospice Number of patients admitted with MRSA Number of patients who developed MRSA during admission Number of patients admitted with Clostridium Difficile Number of inpatient who developed Clostridium Difficile 2013/14 94% 2014/15 93% 2 2 18 36 29 21 48 44 0 0 0 1 0 1 0 0 0 0 *The reporting of all clinical incidents has changed from 2014, including falls, medication incidents and pressure ulcers. The increase in figures during 2014/15, in part, is due to better data collection. Patient Experience There is nothing I could add to the treatment I received. Your staff brought me back to the 'land of the living' and I go on to fight for more days. I have only the highest praise for all staff involved in my case. I have met a whole team with so much patience. I can't have been easy. 12 Carer Experience The exemplary dignified care given to us all came not only from the medical staff but from everyone - the cleaners, volunteers, social staff and Chaplain. The medical staff (doctors and nurses) were amazing - we all knew what was happening and the course of action from the moment we arrived. We never felt there was a time limit when we were talking to anyone and everyone had time to talk and discuss anything and everything at any time. The inside and outside spaces are fantastically maintained and helped to make a bad situation as pleasant as possible. Patient Experience Staff are so proactive, reassuring and with a ready smile. The caring attitude of staff - and that includes volunteers - cannot be "taught" and is a big indication that the right staff are employed (paid or not!). 13 For 2015/2016 the Hospice has agreed the following priorities: PRIORITY 1 Patient Safety The Hospice plans to upgrade the current call bell system within the Inpatient Unit and the Spring Centre. This system will ensure that patients get a prompt response when they call for assistance. It will also incorporate new sensor pads which will alert clinical staff when a patient who has been identified as high risk of falls, is likely to fall. Hospice clinical staff will review past data about falls and the current Falls Assessment Tool. This will be in place by December 2015. PRIORITY 2 Clinical Effectiveness One of our key aims for 2015/16 is to reach more patients and families. To do this we: Plan to invest in community services as part of more collaborative work with local specialist palliative care providers to promote equality of access to palliative care services in our area. Continue to work on identifying gaps in community provision so we can direct wellbeing and rehabilitation resources to reach more people in the community. Develop links with Higher Education Institutions to become research active and improve the evidence base for our care Introduce the national palliative care outcome measures (Outcome Assessment and Complexity Collaborative OACC) PRIORITY 3 Patient and Family Experience During 2015/16 the Hospice plans to: Implement the Real Time Reporting that is currently happening in the Inpatient Unit, to those patients who are seen within the Spring Centre Introduce ‘patient panels’ which will be a forum for patients and family members to contribute to service development Work with the CCG and other specialist palliative care providers to design ways to better co-ordinate community care and access to the IPU beds across Peace Hospice Care and The Hospice of St Francis. 14 Care Quality Commission Gives Hospice Top Marks The Hospice of St Francis received an excellent report from the Care Quality Commission following the most recent inspection in February 2014. The Care Quality Commission, which independently checks whether hospices, hospitals, care homes and other care services are meeting essential standards, concluded that The Hospice of St Francis met all criteria in its inspection across care and welfare, cleanliness and infection control, staffing, complaints and meeting nutritional needs. The report’s overall conclusion was that the Hospice staff were ‘just so caring’. It highlighted that staff and doctors communicated with people very well, keeping them informed of any changes in their health and wellbeing and that all staff, from the chef and nurses to the volunteers and doctors, were ‘willing to help’. The Inspector praised the ‘excellent’ level of care planning at the Hospice, always involving the multidisciplinary team, the patient and those close to them. This was confirmed by relatives who were interviewed, who stated that they “never had to explain things twice” to the Hospice team. The report also noted that the Hospice, which cares for people living with life-shortening illnesses in Herts and Bucks and supports their families and carers, had comprehensive infection control procedures in place, carrying out regular checks to ensure everyone was protected against risk of infection. It also emphasised that the Hospice had enough qualified, skilled and experienced staff, who all underwent regular competency assessments in key areas of clinical care, to meet people’s needs. 15 Healthwatch Hertfordshire’s response to St Francis Quality Account 2014-2015 Healthwatch Hertfordshire is a pleased to submit a response to the Hospice of St Francis Quality Account. The Account is admirably concise and accessible, setting the context for the document through an emphasis on the Hospice’s values. We are pleased to note progress in relation to Priorities for 2014-15, including further approaches to ensure the cleanliness of the environment and we welcome changes to approaches to food and mealtimes which allow a greater opportunity to take account of patient preferences. The Hospice collaboration with the Peace Hospice and West Herts Hospitals Trust to make changes at a ward level and promote excellent end of life care is an excellent development. The adoption of the 15 steps challenge is a useful approach to identifying practical changes that can be made. The data in the report shows increasing levels of activity for almost all the Hospice’s activities. Of particular interest is the number of domiciliary assessments made by allied Health Care Professional assessments which shows the importance of these posts as part of the team. The increase in numbers of slips trips and falls is noted and that this is in part due to better data collection, but welcome the Hospice plans to review falls as part of its priorities for 2015-16. We also are pleased to see a focus on introducing patient panels as a priority for the coming year and look forward to seeing how this approach develops. Michael Downing, Chair Healthwatch Hertfordshire, July 2015 16 17