[ ]
advertisement
![[ ]](http://s2.studylib.net/store/data/010804802_1-6f6884844a41635dde93759650ce89fb-768x994.png)
[
CLINICAL COMMENTARY
]
WHITNEY MEIER, DPT, OCS1HO7DC?PD;H"PhD, MPT2HE8?DC7H9KI"PT, PhD, OCS3
B;;:?88B;"PT, PhD, ATC39>H?IJEF>;HF;J;HI"MD4F7KB9$B7IJ7OE"PT, PhD, CHT5
Total Knee Arthroplasty: Muscle
Impairments, Functional Limitations, and
Recommended Rehabilitation Approaches
otal knee arthroplasty (TKA) is a commonly performed surgical
procedure designed to alleviate knee pain and improve function
in individuals with knee osteoarthritis (OA) or rheumatoid
arthritis. More than 450 000 TKAs are performed each year
in the United States and this number is expected to nearly double
by 2020.2,69 Despite the high incidence of knee replacement and the
availability of postoperative rehabilitative approaches, the resultant
T
muscle impairments are not well defined and are an understudied area of
postoperative care.1 Of particular interest to rehabilitation professionals is the
acute profound postoperative deficit in
quadriceps muscle strength5,42,52,55,67,70,79,85
TIODEFI?I0 The number of total knee arthroplasty (TKA) surgeries performed each year is predicted to steadily increase. Following TKA surgery,
self-reported pain and function improve, though
individuals are often plagued with quadriceps
muscle impairments and functional limitations.
Postoperative rehabilitation approaches either are
not incorporated or incompletely address the muscular and functional deficits that persist following
surgery. While the reason for quadriceps weakness
is not well understood in this patient population, it
has been suggested that a combination of muscle
atrophy and neuromuscular activation deficits contribute to residual strength impairments. Failure
to adequately address the chronic muscle impairments has the potential to limit the long-term functional gains that may be possible following TKA.
(J78B;') that fails to completely resolve
even years after surgery5,6,29,71,72,85 (J78B;
2). Hamstring strength deficits have also
been reported after TKA surgery5,29,42,51,72;
however, the focus on the quadriceps is
due to the association of the quadriceps
Postoperative rehabilitation addressing quadriceps
strength should mitigate these impairments and
ultimately result in improved functional outcomes.
The purpose of this paper is to describe these
quadriceps muscle impairments and to discuss
how these impairments can contribute to the
related functional limitations following TKA. We
will also describe the current concepts in TKA
rehabilitation and provide recommendations and
clinical guidelines based on the current available
evidence.
TB;L;BE<;L?:;D9;0 Therapy, level 5.
J Orthop Sports Phys Ther 2008;38(5):246-256.
doi:10.2519/jospt.2008.2715
TA;OMEH:I0 electrical stimulation, rehabilitation, quadriceps strength, total knee arthroplasty,
TKA
to normal functional activities such as
walking and stair climbing.5,29,42 Therefore, quadriceps weakness will be the focus of this clinical commentary.
While the reason for quadriceps weakness is not well understood in this patient
population, it has been suggested that a
combination of muscle atrophy and neuromuscular activation deficits contribute
to residual strength impairments.54 Failure to adequately address the chronic
muscle impairments is potentially limiting the long-term functional gains that
may be possible following TKA.
Despite the ubiquitous muscle impairments following TKA, long-term
functional outcomes are depicted by
both favorable and nonfavorable results.
In general, self-report functional questionnaires, like the Western Ontario and
McMaster Universities Osteoarthritis
Index (WOMAC) and Medical Outcome
Study 36-Item Short Form Health Survey (SF-36), show large improvements
following TKA.21,26,33,35,43,45,61,64 Despite
quite dramatic improvements in pain
and perceived function, people who have
had TKA for advanced knee arthritis
have lower scores compared to individuals without knee problems.18,59 In contrast
to self-reported outcomes, functional
performance measures, such as a timed
1
Clinical Faculty (Instructor), Department of Physical Therapy, University of Utah, Salt Lake City, UT; Physical Therapist, Department of Orthopedics, University of Utah, Salt Lake
City, UT. 2 Assistant Professor, Department of Physical Therapy, Eastern Washington University, Cheney, WA. 3 Associate Professor (Clinical), Department of Physical Therapy,
University of Utah, Salt Lake City, UT; Physical Therapist, Department of Orthopedics, University of Utah, Salt Lake City, UT. 4 Associate Professor, Department of Orthopedics,
University of Utah, Salt Lake City, UT. 5 Associate Professor, Department of Physical Therapy, University of Utah, Salt Lake City, UT; Adjunct Associate Professor, Department
of Exercise and Sport Sciences, University of Utah, Salt Lake City, UT; Adjunct Associate Professor, Department of Orthopedics, University of Utah, Salt Lake City, UT. Address
correspondence to Dr Paul C. LaStayo, Department of Physical Therapy, University of Utah, 520 Wakara Way, Salt Lake City, UT 84108. E-mail: paul.lastayo@health.utah.edu
246 | may 2008 | volume 38 | number 5 | journal of orthopaedic & sports physical therapy
Quadriceps Strength Deficits Compared to Uninvolved Side up to
6 Months Following Total Knee Arthroplasty
J78B;'
H[\[h[dY[
5
Berman (n = 68)
C[Wd7][
63
J_c[
Preoperative
J[ijCeZ[
?dlebl[ZDc
Kd_dlebl[ZDc
Isokinetic 60°/s
35.5
59.9
41
39.1
67.0
42
3-6 mo postoperative
Lorentzen42 (n = 60)
74
Preoperative
Isokinetic 30°/s
3 mo postoperative
6 mo postoperative
Rodgers (n = 20)
68
79.0
15
29
3 mo postoperative
39.0
52.0
25
6 mo postoperative
42.0
53.0
21
Preoperative
Isokinetic 60°/s
Preoperative
Isometric 75°
3 mo postoperative
6 mo postoperative
Mizner52 (n = 40)
64
15
29
52.0
3 mo postoperative
74
67.0
78.0
67.0
Isokinetic 120°/s
1.5 mo postoperative
Lorentzen42 (n = 60)
57.0
55.0
37.0
Preoperative
67
:_÷[h[dY[
74.6
102.4
27
56.9
101.7
44
29
73.9
103.4
66.0
87.0
24
55.0
92.0
40
29
65.0
92.0
183.7
225.6
19
1 mo postoperative
70.7
222.8
68
2 mo postoperative
95.7
228.1
58
3 mo postoperative
148.8
231.7
36
6 mo postoperative
179.9
228.9
21
Preoperative
Isometric 75°
* Percent difference calculated: [(uninvolved – TKA)/uninvolved] 100.
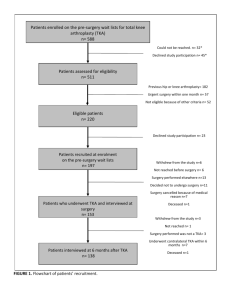
stair-climbing or walking test, depict only
modest improvements following TKA,56,81
and substantial residual deficits persist
when compared to age- and sex-matched
healthy comparison groups. These functional performance findings are consistent in those with chronic quadriceps
muscle weakness.59,80,85 At times, the deficits in functional performance are quite
pronounced. For example, approximately
three quarters of patients with a knee replacement report difficulty negotiating
stairs59 and the average stair-climbing
speed is only half as fast compared to
healthy counterparts.85 Furthermore,
following a peak in functional recovery 2
to 3 years after TKA, there is an accelerated decline in function relative to typical
age-related decrements.66 Physical therapy countermeasures seem ideally suited
to mitigate the muscle impairments and
functional limitations following TKA.
Recent descriptions of postoperative rehabilitation programs with intensive exercise following TKA have reported greater
restoration of quadriceps strength, im-
proved functional ability, and an earlier
return to activity compared to historical
TKA outcomes.52,58,62,72
The purpose of this clinical commentary is 4-fold: (1) to describe the quadriceps strength impairments related to
TKA and the associated muscle activation deficits and muscle atrophy; (2) to
explore how these impairments contribute to functional limitations; (3) to describe how the current concepts in TKA
rehabilitation are attempting to address
these impairments; and (4) to outline
recommendations and clinical guidelines
for rehabilitation based on the best available evidence and therapeutic exercise
principles.
GK7:H?9;FIM;7AD;II
<EBBEM?D=JA7
Q
uadriceps weakness has been
implicated in the development
and progression of knee OA9,74
and is related to a decline in physical function.15,20,27,32,73 People with knee
OA-induced quadriceps weakness consistently exhibit about a 20% strength
deficit compared to healthy age- and sexmatched cohorts.73 Strength deficits are
ubiquitous in people with advanced knee
OA who are considering a TKA. Muscle
strength assessments in patients with
TKA are performed with isometric or
slow isokinetic testing speeds. A compilation of these quadriceps strength results
before and after (short- and long-term
follow-up) TKA is provided in J78B;I '
and 2. The most common surgical approach during a TKA procedure involves
an incision through the extensor mechanism. This surgical approach apparently
compounds preoperative strength deficits
as patients produce less than half of their
preoperative torque values at 1 month
after TKA.52,54,57,79 While quadriceps
strength increases steadily thereafter, significant changes in strength start tapering off 6 to 12 months following surgery
(J78B;I' and 2). Hence, while isometric
quadriceps strength improves 10% to
20% from preoperative levels following
journal of orthopaedic & sports physical therapy | volume 38 | number 5 | may 2008 | 247
[
CLINICAL COMMENTARY
]
Quadriceps Strength Deficits From 6 Months to 13 Years Following
Total Knee Arthroplasty: Comparison to the Uninvolved Side or an
Age-Matched Healthy Group*
J78B;(
:_÷[h[dY[
:_÷[h[dY[
H[\[h[dY[
J_c[
J[ijCeZ[
JA7Dc
Kd_dlebl[ZDc
>[Wbj^oDc
Kd_dlebl[Z
>[Wbj^o
Berman5,†
7-12 mo
50.5
71.0
29
13-23 mo
Isokinetic, 60°/s
55.9
69.2
13
l24 mo
57.0
68.2
Huang29,‡
6-13 y
Isokinetic, 120°/s
48.4
Isokinetic, 180°/s
36.3
Walsh85,§
1.7 y
Isokinetic, 90°/s
57.0
64.5
Isokinetic, 120°/s
54.5
63.0
Silva72,??
2.8 y
Isometric, 75° of knee flexion
94.7
Berth6,¶
Preoperative
Isometric, 90° of knee flexion
66.3
81.9
84.8
79.4
Postoperative (2.8 y)
16
60.7
20
49.9
27
88.0
12
35
82.0
13
34
136.8
31
105.0
19
37
–7
19
* Percent difference calculated: ([healthy – TKA]/healthy) 100.
†
mean age, 63; n = 68.
‡
TKA, n = 36 (mean age, 68); age-match, n = 9 (mean age, 63).
§
TKA, n = 16 (mean age, 65); age-match, n = 10 (mean age, 62).
??
TKA, n = 31 (mean age, 64); age-match, n = 40 (mean age, 63).
¶
TKA, n = 50 (mean age, 66); age-match, n = 23 (mean age, 63).
TKA (85-95 Nm),6,72 strength rarely ever
reaches the value of age-matched healthy
individuals (105-137 Nm)6,72 or the potential isometric or isokinetic strength
levels of the nonoperative knee extensor
muscles (87-232 Nm).5,6,42,52,85 At times,
the amount of residual weakness in individuals following TKA is substantial in
that a general strength deficit of 20% or
more is common (J78B;().
Some caution must be exerted when
interpreting results that use the uninvolved limb as a comparator. Approximately 40% of patients with unilateral
TKA progress to a TKA in their nonoperative lower extremity by 10 years48,65;
hence, the uninvolved knee should probably not be considered a typically healthy
or unimpaired joint. Consequently, these
estimates of weakness are conservative.23 Accordingly, when comparing the
long-term strength outcomes of TKA
to healthy age-matched groups,40 the
strength deficit grows to between 30%
and 48%.23,52,53,85 In summary, the quadriceps strength deficits prior to surgery are
greatly compounded early after surgery
and slowly recover to levels only slightly
better than preoperative values. Thus,
pre-existing quadriceps weakness is not
resolved solely by TKA and strength values post surgery are far from age-matched
normative values.
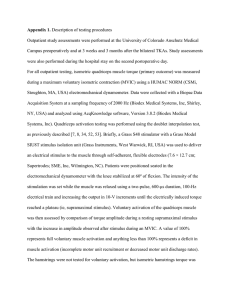
GkWZh_Y[fiCkiYb[7Yj_lWj_ed
<W_bkh[<ebbem_d]JA7
Quadriceps muscle weakness in patients
with OA of the knee is attributed in part
to failure of voluntary muscle activation
(ie, muscle inhibition).79 The failure of
voluntary activation of skeletal muscle
is defined as the inability to produce all
available force of a muscle despite maximal voluntary effort.36,75,76 There are 2
common techniques for equating failure of voluntary activation: twitch interpolation and burst superimposition.
The twitch interpolation procedure is
performed by superimposing a single or
multiple pulses on various intensities of
muscle contractions from 0% (resting)
to 100% maximal voluntary contraction
(MVC). Failure of voluntary activation is
computed as 1 – (superimposed twitch
at MVC/superimposed twitch at rest). A
burst superimposition technique is more
commonly used to determine the levels
of voluntary activation54,57,78 by super-
248 | may 2008 | volume 38 | number 5 | journal of orthopaedic & sports physical therapy
imposing a train of high-voltage pulses
with rapid frequency on a MVC. Failure
of voluntary activation of the quadriceps
using burst superimposition is frequently
reported as an index called the central
activation ratio (CAR).36 The CAR is derived by dividing the maximal voluntary
force by the total force achieved via a voluntary effort plus potential electrically
elicited force (<?=KH;). A CAR of 1.0 denotes complete activation of the muscle.36
Healthy older adults (66 to 83 years of
age) with no known knee pathology have
been reported to have a range of CAR values (0.87-1.00), with an average CAR of
0.96.40,49,77 When interpreting the studies
using superimposed electric stimulation
techniques, it is important to consider
the relationship between the CAR and
voluntary effort.49,76 The calculated CAR
may be lower than the true CAR, and the
failure of voluntary activation may be
overestimated.
Failure of voluntary muscle activation plays a substantial role in the weakness that is present both before and after
TKA surgery.6,7,23,57,79 Prior to TKA the
average failure of voluntary activation
is more than twice that of healthy older
[
CLINICAL COMMENTARY
]
Quadriceps Strength Deficits From 6 Months to 13 Years Following
Total Knee Arthroplasty: Comparison to the Uninvolved Side or an
Age-Matched Healthy Group*
TABLE 2
Reference
Time
Berman5,†
7-12 mo
Test Mode
Isokinetic, 60°/s
TKA (Nm)
Uninvolved (Nm)
Healthy (Nm)
Difference
Difference
Uninvolved (%)
Healthy (%)
50.5
71.0
29
13-23 mo
55.9
69.2
13
l24 mo
57.0
68.2
Huang29,‡
6-13 y
Isokinetic, 120°/s
48.4
Isokinetic, 180°/s
36.3
Walsh85,§
1.7 y
Isokinetic, 90°/s
57.0
64.5
Isokinetic, 120°/s
54.5
63.0
Silva72,??
2.8 y
Isometric, 75° of knee flexion
94.7
Berth6,¶
Preoperative
Isometric, 90° of knee flexion
66.3
81.9
84.8
79.4
Postoperative (2.8 y)
16
60.7
20
49.9
27
88.0
12
35
82.0
13
34
136.8
31
105.0
19
37
–7
19
* Percent difference calculated: ([healthy – TKA]/healthy) 100.
†
n = 68 (mean age, 63).
‡
TKA, n = 36 (mean age, 68); age-match, n = 9 (mean age, 63).
§
TKA, n = 16 (mean age, 65); age-match, n = 10 (mean age, 62).
??
TKA, n = 31 (mean age, 64); age-match, n = 40 (mean age, 63).
¶
TKA, n = 50 (mean age, 66); age-match, n = 23 (mean age, 63).
TKA (85-95 Nm),6,72 strength rarely ever
reaches the value of age-matched healthy
individuals (105-137 Nm)6,72 or the potential isometric or isokinetic strength
levels of the nonoperative knee extensor
muscles (87-232 Nm).5,6,42,52,85 At times,
the amount of residual weakness in individuals following TKA is substantial in
that a general strength deficit of 20% or
more is common (TABLE 2).
Some caution must be exerted when
interpreting results that use the uninvolved limb as a comparator. Approximately 40% of patients with unilateral
TKA progress to a TKA in their nonoperative lower extremity by 10 years48,65;
hence, the uninvolved knee should probably not be considered a typically healthy
or unimpaired joint. Consequently, these
estimates of weakness are conservative.23 Accordingly, when comparing the
long-term strength outcomes of TKA
to healthy age-matched groups,40 the
strength deficit grows to between 30%
and 48%.23,52,53,85 In summary, the quadriceps strength deficits prior to surgery are
greatly compounded early after surgery
and slowly recover to levels only slightly
better than preoperative values. Thus,
pre-existing quadriceps weakness is not
resolved solely by TKA and strength values post surgery are far from age-matched
normative values.
Quadriceps Muscle Activation
Failure Following TKA
Quadriceps muscle weakness in patients
with OA of the knee is attributed in part
to failure of voluntary muscle activation
(ie, muscle inhibition).79 The failure of
voluntary activation of skeletal muscle
is defined as the inability to produce all
available force of a muscle despite maximal voluntary effort.36,75,76 There are 2
common techniques for equating failure of voluntary activation: twitch interpolation and burst superimposition.
The twitch interpolation procedure is
performed by superimposing a single or
multiple pulses on various intensities of
muscle contractions from 0% (resting)
to 100% maximal voluntary contraction
(MVC). Failure of voluntary activation is
computed as 1 – (superimposed twitch
at MVC/superimposed twitch at rest). A
burst superimposition technique is more
commonly used to determine the levels
of voluntary activation54,57,78 by super-
248 | may 2008 | volume 38 | number 5 | journal of orthopaedic & sports physical therapy
imposing a train of high-voltage pulses
with rapid frequency on a MVC. Failure
of voluntary activation of the quadriceps
using burst superimposition is frequently
reported as an index called the central
activation ratio (CAR).36 The CAR is derived by dividing the maximal voluntary
force by the total force achieved via a voluntary effort plus potential electrically
elicited force (FIGURE). A CAR of 1.0 denotes complete activation of the muscle.36
Healthy older adults (66 to 83 years of
age) with no known knee pathology have
been reported to have a range of CAR values (0.87-1.00), with an average CAR of
0.96.40,49,77 When interpreting the studies
using superimposed electric stimulation
techniques, it is important to consider
the relationship between the CAR and
voluntary effort.49,76 The calculated CAR
may be lower than the true CAR, and the
failure of voluntary activation may be
overestimated.
Failure of voluntary muscle activation plays a substantial role in the weakness that is present both before and after
TKA surgery.6,7,23,57,79 Prior to TKA the
average failure of voluntary activation
is more than twice that of healthy older
MVIC + E
MVIC
Force (N)
300
CAR =
250
MVIC
212 N
= 0.86
=
MVIC + E 246 N
200
150
100
1
2
3
4
5
Time (s)
<?=KH;$A schematic representation of a quadriceps
force tracing from a maximal voluntary isometric
contraction (MVIC) with an electrically elicited force
during a burst superimposition (MVIC + E). The
central activation ratio (CAR) is derived by dividing
the maximal voluntary force by the total force
achieved during a combined voluntary effort plus any
additional electrically elicited force.
adults.54,63,79 One month following TKA,
the quadriceps activation deficits are
twice from preoperative levels and the average CAR of people with TKA is roughly
0.75.54,57,79 This level of quadriceps muscle
activation failure is unusually large. As a
reference, those with patellar contusions
have a CAR of 0.8644 and individuals with
acute (6 weeks) anterior cruciate ligament
tears average 0.92.10 As previously stated,
the acute loss of quadriceps strength is
dramatic and the reduction in voluntary
muscle activation accounts for 65% of
the variance in this loss of strength.57,79 In
fact, voluntary quadriceps activation failure contributes almost twice as much to
the acute decrease in quadriceps strength
as compared to the amount of quadriceps
muscle atrophy.57,79 Large activation deficits are of particular concern to physical
therapists, as these patients typically experience only modest strength gains with
exercise interventions.30
It appears that voluntary activation
failure can continue for an extended
period of time after surgery for a subset
of TKA recipients. Gapeyeva and colleagues23 reported average quadriceps activation levels did not improve in female
TKA recipients from the preoperative
time point until the sixth postoperative
month. Even with upwards of 8 days of
formal rehabilitation, activation levels
remained lower than those of healthy
subjects.23 A similar lack of activation
improvement up to 6 months following
TKA was also reported by Berth et al.7
Twenty patients who were scheduled for
bilateral TKAs had each knee randomly
assigned to receive either a subvastus or
midvastus surgical approach. Quadriceps
voluntary activation was assessed before
surgery, and at 3 months and 6 months
following surgery. All patients underwent
10 days of inpatient rehabilitation and an
additional 4 weeks of outpatient therapy
(though not described in the report).
There was no main effect of time or surgical approach, and quadriceps voluntary
activation levels were well below normal
at all test points. Some others, however,
report some limited activation improvements over time6,78; however, even years
after TKA, activation of the quadriceps
muscle is still significantly lower than for
age-matched healthy controls.6
Poor quadriceps activation is a rehabilitation concern because it may blunt
the potential effectiveness of voluntary exercise that relates to improving
physical function. Quadriceps activation
failure appears to act as a moderator between quadriceps strength and physical
function in patients with knee OA. That
is, physical function may be more limited
in those people with quadriceps weakness and a higher degree of activation
failure.21
GkWZh_Y[fi7jhef^o<ebbem_d]WJA7
Sarcopenia, the progressive loss of muscle mass with aging, is a fundamental
contributor to disability in the elderly
population.83 The quadriceps muscle activation failure present in patients with OA
may be contributing to muscle atrophy,
as neuromuscular inhibition prevents full
muscle activation and potentially blunts
the stimulus necessary to maintain muscle
mass.31 Clinicians sense both activation
failure and atrophy occur in those with
TKA, though there are very few reports
which have assessed muscle size changes
prior to or following TKA. Quadriceps atrophy of 5% to 20% has been reported in
the first month after surgery compared to
preoperative values.54,62,67 A recent report
utilizing magnetic resonance imaging
(MRI) assessments on patients who are
awaiting surgery describes a mean quadriceps cross-sectional area (CSA) that is
quite small at 42.3 cm2. Additionally, a
10% decrease in muscle size 1 month following TKA (38.2 cm2), compared to the
preoperative values, has been reported.54
When including quadriceps atrophy into
the regression model with activation
failure 85% of the change in quadriceps
strength in the first month after surgery
is explained, though the contribution of
the voluntary activation was nearly twice
the relative contribution of the maximal
cross-sectional area in the regression
equation.54 The atrophy associated with
TKA may be a conservative estimate of
muscle loss, considering the comparisons
that have been made to the uninvolved
or the preoperative values. As noted earlier, the assumption that the uninvolved
extremity is “normal” may not be a valid
comparison in individuals with a history
of OA. The maximal quadriceps CSA
of patients between the ages of 41 to 75
years with a history of OA is 46.1 to 49.5
cm2.24,25 This is considerably less than a
comparative group between the ages of
65 and 81 years, with a maximal CSA of
63.5 to 68.1 cm2.17,22 In summary, most individuals with a TKA exhibit small quadriceps CSA values that are consistent with
long-term OA-induced weakness. As well,
it is still unclear whether muscle strength
and atrophy can return to age-matched
normal values with postoperative rehabilitation interventions.
CkiYb[ ?cfW_hc[dji WdZ j^[ H[bWj[Z
<kdYj_edWbB_c_jWj_edi<ebbem_d]JA7
Quadriceps muscle impairments and
lower extremity OA are associated with
functional limitations and slower mobility performance in older adults.41 The primary goals of a TKA are to decrease pain,
improve functional mobility, such as walking and stair climbing, and to promote
return to physical activity. TKA has been
shown to be very effective in reducing the
knee pain associated with arthritis1,34,46;
but 30% of patients report dissatisfac-
journal of orthopaedic & sports physical therapy | volume 38 | number 5 | may 2005 | 249
[
CLINICAL COMMENTARY
tion in their physical function 1 year after surgery.13 Functional outcome scores
reported via questionnaires indicate an
improvement in quality of life following
surgery, but actual physical performance
measures and the individual’s perception
of functional ability remain worse than
the age-matched healthy population.18,59
Individuals 1 year after a TKA surgery
perceived their functional ability to be
approximately 80% of a group of similar age. In another self-report study only
50% of the TKA recipients considered
their knee function normal compared
to their healthy peers.59 Likewise, quadriceps weakness does not correlate well
with patient perceptions of function.52
Self-report scores of physical function
in this population tend to correspond
to what patients experience (like pain
or perceived exertion) when performing
activities, rather than their actual ability
to complete an activity.81,84 Improvement
in self-report physical function is often
most strongly associated with improvements in pain.81
While quadriceps weakness may have
a limited association with perceived
functional ability, it tends to have a
strong relationship with performance.52
Quadriceps weakness in older adults
has been associated with an increased
fall risk,73 decreased gait speed,5,37,55,60,85
and impaired stair-climbing ability.85
Like with other elderly patient cohorts,
strength is an important predictor of
functional abilities32,39 in patients who
have TKA.53 Once more, bodily pain
scores do not seem to limit functional
performance from 1 month to 6 months
after surgery.52 Even though knee range
of motion (ROM) is also considered to
be important in early phases of therapy
for enhancing functional performance,
there is little evidence that function is
related to knee ROM.50,52 Rehabilitation
following a TKA should still be directed
towards pain control and improving knee
ROM, but a focus on exercises to address
quadriceps muscle impairments appears
necessary to achieve the best functional
abilities.8,52,79
H;>78?B?J7J?ED
<EBBEM?D=JA7
T
he loss of quadriceps muscle
strength seems to be an inevitable
consequence for people who have
TKA surgery; hence, some have suggested the need for a more aggressive
and long-term postoperative rehabilitation approach.5,72 Quadriceps muscle impairments and corresponding functional
limitations have been addressed in physical therapy regimens, but the outcomes
to date have generally been suboptimal
and individuals with TKA continue to
perform below age- and gender-matched
controls.18,85 The reports of both preoperative and postoperative TKA rehabilitation
outcomes suggest further modifications to
the physical interventions that are needed
to maximize muscle structure and functional response post surgery. However,
further research, specifically randomized
controlled trials, is warranted to investigate the effectiveness of strengthening
exercises and manual physical therapy in
individuals after a TKA.
Fh[ef[hWj_l[?dj[hl[dj_edi
Physical countermeasures have been successful in improving knee pain, strength,
and joint stability in those with knee
OA who were not yet planning to have
a TKA.11,12,20 For those who go on to a
TKA, preoperative quadriceps strength
is a strong predictor of functional performance 1 year after surgery.53 Furthermore,
individuals with more extensive signs of
OA have more quadriceps weakness.73 If
quadriceps weakness could be addressed
prior to TKA surgery, then perhaps patients might experience a better overall
functional level.
Unfortunately, there is little documented success in improving the preoperative status in those planning a
TKA.19,20,82 Physical therapy interventions prior to TKA have focused on
strengthening, aerobic conditioning,
and educational programs. D’Lima et
al14 compared the effects of preoperative upper and lower extremity strength
250 | may 2008 | volume 38 | number 5 | journal of orthopaedic & sports physical therapy
]
training, general cardiovascular conditioning exercises, and no intervention
(control group) in individuals before
and after TKA (10 subjects per group).
No significant differences were observed
in the 3 groups at any of the postoperative evaluations. In another study conducted by Rodgers et al,67 10 patients
who underwent 6 weeks of preoperative
physical therapy showed no significant
change in Hospital for Special Surgery
Knee Rating (HSS) scores, knee ROM,
isokinetic knee extension strength, and
walking speed prior to surgery.67 Beaupre
et al4 addressed the combined effect of
preoperative strengthening exercise and
education in 131 subjects scheduled for
TKA. The outcome measures included
gait training with an assistive device, bed
mobility, and transfer training for functional recovery, and the Health-Related
Quality of Life (HRQOL) questionnaire.
The authors reported no significant differences in ROM, quadriceps and hamstring strength, function, or HRQOL
score when compared to a control group
1 year after TKA. Finally, Rooks et al68
found no significant improvements in
self-reported function or performance
measures in those who underwent preoperative exercise training compared to
those who did not (22 patients assigned
per group). Considering these findings,
it may be that quadriceps weakness
and functional limitations are recalcitrant in those about to receive a knee
replacement; however, starting quadriceps strengthening earlier (ie, in the
beginning stages of OA) may be the best
approach.53
Feijef[hWj_l[?dj[hl[dj_edi
There is a dearth of available evidence for
determining the best possible postoperative rehabilitation intervention, though
a limited number of reports suggest that
improvements in ROM and strength, a
lowered pain level, and improvements
in independence with activities of daily
living have resulted from such interventions. The authors of a recent randomized controlled trial comparing a
J78B;)
A Comparison of Therapeutic Exercise
Rehabilitation Approaches Following TKA
7lhWc_Z_i)
C_pd[hWdZIj[l[di52,78
Ce÷[j58
Start of therapy
1 d postoperative
3.5 wk postoperative
8 wk postoperative
Frequency
2 times/d
3 times/wk
1-2 times/wk
Number of visits (duration)
16 (8 d)
18 (6 wk)
12 (8 wk)
NMES*
Yes (6 wk)
Yes*
No
Bike
5-10 min
10-15 min
5-20 min
Core exercises
Quadriceps sets
X
Hamstring sets
X
Straight-leg raise
X
X
X
X
X
X
Hip abduction
X
X
Standing terminal extension
X
X
Step-ups/-downs
X
X
X
X
AROM/AAROM
X
Seated knee extension
X
Wall squats/standing squats
X
X
Standing hamstring curl
X
X
Lunges
X
Walking
X
Non–weight-bearing ROM
X
X
X
X
Ankle pumps
X
Sit-to-stand
X
Walking backward, marching, side step
X
Abbreviations: AAROM, active assistive range of motion; AROM, active range of motion; NMES, neuromuscular electrical stimulation; ROM, range of motion; TKA, total knee arthroplasty.
* NMES parameters: 2500-Hz triangular-wave alternating current (AC), 12-s on-time, 80-s off-time,
2- to 3-s ramp-up time, knee flexed to 60°, 10 isometric contractions, dose set to maximally tolerated
by the patient, large (7.6 12.7 cm) self-adhesive electrodes placed on motor points of the quadriceps
femoris muscle.
supervised home rehabilitation exercise
program to standard-care control group
reported that individuals with TKA who
received 12 supervised rehabilitation
treatment sessions starting 2 months after surgery walked longer distances at 1
year after surgery compared to the control group, and the distance walked in 6
minutes was within 1 standard deviation
of a group of healthy, age-matched individuals.58 The treatment group showed
an accelerated symptom recovery with
less pain, stiffness, and difficulty performing daily activities compared to the
standard-care group, as reported on the
WOMAC and SF-36 at 6 months after
surgery; but no significant differences
were noted at 1 year postsurgery. A description and comparison of published
postoperative therapy protocols is provided in J78B;).
A longitudinal study with a more progressive and intense rehabilitation program instituted earlier after TKA (3-4
weeks postoperatively) and designed
specifically to address the functional
impairments following a TKA has been
repeatedly reported by Mizner and colleagues at the University of Delaware.52,78
Their protocol consisted of 3 days of inpatient physical therapy, followed by 2 to
3 weeks of home physical therapy visits.
At approximately 4 weeks after surgery,
the patients with TKA began 6 weeks (2
to 3 times per week) of outpatient rehabilitation. Progressive, high-intensity
volitional exercises were used to increase
lower musculature extremity strength
and improve functional ability in 40 individuals who completed this protocol
(J78B; )). At 1 month postsurgery, before treatment was initiated, knee ROM,
quadriceps strength, and performance
on the timed up and go (TUG) and stair
climb test (SCT) were lower than they
were at presurgery. The TKA recipients’
quadriceps strength decreased 62% from
the preoperative value at the first month
postsurgery. Following 6 weeks of rehabilitation, quadriceps strength improved
significantly at each following assessment
(2, 3, and 6 months postsurgery). There
was also a 21% improvement in the TUG
and a 40% improvement in the SCT from
the preoperative test to 6 months after
surgery. Finally, quadriceps strength was
correlated with functional performance
measures at all testing sessions and, as
quadriceps strength improved, there was
an enhancement in functional performance. This study clearly demonstrates
that the muscle impairments and functional limitations can be reversed following a TKA.52
There is also some evidence that the
addition of neuromuscular electrical
stimulation (NMES) to a physical therapy protocol could enhance the speed
and ultimate recovery of quadriceps
strength after TKA. In 2 case report series from the same group, the addition of
high-intensity NMES to the quadriceps
muscle produced strength gains that exceeded previously published outcomes40,78
(NMES specifications described in J78B;
)). The data were also suggestive of a
positive dose-response relationship for
NMES. Those patients who achieved a
higher percentage of their knee extension
maximal voluntary isometric contraction torque with NMES contractions had
greater gains in strength.78 These results
suggest that NMES early after TKA may
help resolve quadriceps activation failure
and mitigate quadriceps muscle weakness. When considering the low quadriceps activation in this patient population
early after surgery, the addition of NMES
to augment volitional strengthening exercises could be a useful adjunct to reha-
journal of orthopaedic & sports physical therapy | volume 38 | number 5 | may 2005 | 251
[
CLINICAL COMMENTARY
bilitation, especially for those people who
are very weak.
The addition of NMES even earlier
than 4 weeks may also be beneficial. A
randomized control study by Avramidis
et al3 investigated the effect of 4 hours
per day of NMES (40 Hz, 300 μs) to the
vastus medialis, commencing on postoperative day 2 and continuing for 6 weeks
following surgery. This resulted in improved walking speed, though no changes
were noted in the HSS or in an index of
physiological cost.3 A recent case report
also describes the use of NMES, initiated
on postoperative day 2 for a 6-week period, and reported strength gains in the
first month after surgery compared to
preoperative values.51 In summary, outpatient rehabilitation after a TKA seems
to be superior to no intervention at all.
These studies suggest that muscle impairments and functional limitations can be
reversed following a TKA. But additional
research is necessary to determine the
optimal mode, intensity, and duration of
physical therapy needed to mitigate the
muscle impairments and related functional limitations following a TKA.
H;9ECC;D:7J?EDI7D:JA7
9B?D?97B=K?:;B?D;I
T
he recommendations and clinical guidelines described below are
derived from the best available
evidence, but additional research, specifically randomized controlled trials, is
needed to optimize short- and long-term
outcomes for individuals after a TKA.
Nevertheless, recipients of TKA should
respond favorably to similar therapeutic
exercise guidelines as suggested by the
American College of Sports Medicine
(ACSM) for older individuals.47 That is,
progressive resistive training of major
muscle groups (especially of the lower
extremities) should be performed 2 to
3 times per week and aerobic training 3
times per week for 30 to 40 minutes.38
The aerobic training for those with a
TKA, however, should include walking
on flat ground initially, adding hills, and
J78B;*
]
1999 Knee Society Survey 28
H[Yecc[dZ[Z7Yj_l_j_[i<ebbem_d]JejWbAd[[7hj^hefbWijo
Aerobics (low impact)
Square dancing
Bicycling (stationary)
Walking
Bowling
Golf
Croquet
Horseshoes
Ballroom dancing
Shooting
Jazz dancing
Shuffleboard
Swimming
Horseback riding
7Yj_l_j_[iH[Yecc[dZ[ZM_j^Fh[l_eki;nf[h_[dY[
Bicycling (road)
Skiing (cross country)
Canoeing
Skiing (stationary)
Hiking
Tennis (doubles)
Rowing
Weight machines
Speed walking
7Yj_l_j_[iDejH[Yecc[dZ[Z
Racquetball
Football
Squash
Gymnastics
Rock climbing
Lacrosse
Soccer
Hockey
Singles tennis
Basketball
Volleyball
Jogging
Handball
De9edYbki_ed
Fencing
Downhill skiing
Roller blade/inline skating
Weight lifting
negotiating stairs. Higher-level aerobic
exercises that minimize impact to the
knee, such as swimming, cycling, water
aerobics, and power walking, are also recommended. Recreational activities with
high joint loads, such as skiing, tennis,
and hiking, should be performed with
caution and only occasionally. TKA recipients are strongly cautioned to avoid even
the lowest-level impact recreational and
athletic activities until their quadriceps
and hamstring muscles are rehabilitated
sufficiently.28 Specific recommendations
derived from the 1999 Knee Society Survey28 have been used to develop a consensus recommendation for athletics
and sports participation for those with a
TKA (J78B;*). Despite these guidelines,
many TKA recipients still experience
significant difficulty in performing activities that require higher-level mobility
skills commensurate with recreational
activities.18,59
252 | may 2008 | volume 38 | number 5 | journal of orthopaedic & sports physical therapy
Therapeutic exercise guidelines following a TKA are traditionally focused
on the control of pain and swelling, while
improving ROM and functional mobility.
More progressive, high-intensity exercises may be necessary to address lower
extremity muscle size, activation and
strength deficits, along with functional
mobility early following surgery. The use
of NMES along with an exercise program
has demonstrated improved quadriceps
strength and activation and is recommended early in a rehabilitation program.
Resistance training (60% of the 1-repetition maximum) has been demonstrated
to induce increases in strength in the
elderly.16 Therefore, it may be necessary
to increase the lower extremity strength
training to at least that level of intensity
for 1 to 3 sets of 10 to 20 repetitions to
overcome the recalcitrant muscle impairments which may be present 6 months
to 1 year following TKA. The 7FF;D:?N
provides specific guidelines relative to
a progressive rehabilitative program for
those following a TKA. These recommendations are used to address the pertinent
muscle impairments in addition to enhancing mobility.
The protocols mentioned by Moffet
and colleagues58 and the investigations
from Snyder-Mackler’s laboratory at the
University of Delaware40,55,78 are combined
with the ACSM guidelines into 4 phases
and the timelines are a guide for progression into the next phase. Modifications to
this program are instituted immediately
if adverse knee joint reactions (eg, pain,
swelling) occur. Decreasing the intensity,
frequency, and duration of the resistance
exercise typically resolves any adverse
knee response. In phase I following a
TKA, patients receive home health or outpatient physical therapy 2 to 3 times per
week for 2 to 3 weeks after inpatient discharge. The emphasis of physical therapy
in this phase is on edema management,
improving ROM, starting a strengthening
program, and improving functional independence. At approximately 3 to 4 weeks
postsurgery, or when goals are met, the
patients start phase II, which consists of
outpatient physical therapy 2 to 3 times
per week for 4 to 6 weeks. Augmentation
of the quadriceps muscle’s activation following TKA should be emphasized early
in this rehabilitation phase to help restore quadriceps muscle strength. Physical therapy treatments should employ the
concepts of progressive high-intensity volitional exercises with NMES to increase
strength and quadriceps muscle activation.52,58,78 At 10 to 12 weeks postoperative or when the criteria for progression
are met, such as ROM from 5° or less to
110° or greater, minimal pain and edema,
and voluntary quadriceps muscle control,
patients progress to phase III of the rehabilitation program. Phase III includes
a semi-independent period of 4 to 8 inclinic visits over 3 to 4 weeks, with a goal
to improve strength and progress to an
independent phase (phase IV), with clinical follow-up visits for another 8 weeks.
In addition to a warm-up and functional
endurance exercises, this program places
an emphasis on strengthening resistance
exercises for the lower extremity. In an
attempt to mitigate the muscle impairments, progressive, moderately highresistance exercises are used. Most often
individuals with TKA can increase the
intensity of exercise after 3 sets of 10 repetitions are completed correctly without
undue fatigue.
IKCC7HO
.$
/$
'&$
M
uscle impairments that exist following a TKA may persist
for years. Improving quadriceps
strength may mitigate these impairments and result in improved functional
outcomes. An emphasis on muscle weakness countermeasures, like resistance
exercises and NMES, is needed. Further
research is required to determine the optimal exercise prescription that can safely
augment the return to near-normal levels of activity and function for individuals
who had TKA surgery. T
''$
'($
')$
H;<;H;D9;I
'$ NIH Consensus Statement on total knee replacement December 8-10, 2003. J Bone Joint
Surg Am. 2004;86-A:1328-1335.
($ American Academy of Orthopaedic Surgeons.
Arthroplasty and Total Joint Replacement Procedures: 2003. Available at: http//www.aaos.
org/wordhtml/research/stats/arthroplasty_recent.htm. Accessed 2003.
)$ Avramidis K, Strike PW, Taylor PN, Swain ID. Effectiveness of electric stimulation of the vastus
medialis muscle in the rehabilitation of patients
after total knee arthroplasty. Arch Phys Med
Rehabil. 2003;84:1850-1853.
*$ Beaupre LA, Lier D, Davies DM, Johnston DB.
The effect of a preoperative exercise and education program on functional recovery, health
related quality of life, and health service utilization following primary total knee arthroplasty. J
Rheumatol. 2004;31:1166-1173.
+$ Berman AT, Bosacco SJ, Israelite C. Evaluation
of total knee arthroplasty using isokinetic testing. Clin Orthop Relat Res. 1991;106-113.
,$ Berth A, Urbach D, Awiszus F. Improvement of
voluntary quadriceps muscle activation after
total knee arthroplasty. Arch Phys Med Rehabil.
2002;83:1432-1436.
-$ Berth A, Urbach D, Neumann W, Awiszus F.
'*$
'+$
',$
'-$
'.$
'/$
(&$
('$
Strength and voluntary activation of quadriceps femoris muscle in total knee arthroplasty
with midvastus and subvastus approaches.
J Arthroplasty. 2007;22:83-88. http://dx.doi.
org/10.1016/j.arth.2006.02.161
Brander VA, Mullarkey CF, Stulberg SD. Rehabilitation After Total Joint Replacement for
Osteoarthritis: An Evidence-Based Approach.
Philadelphia, PA: Hanley & Belfus, Inc; 2001.
Brandt KD, Heilman DK, Slemenda C, et al. A
comparison of lower extremity muscle strength,
obesity, and depression scores in elderly
subjects with knee pain with and without radiographic evidence of knee osteoarthritis. J
Rheumatol. 2000;27:1937-1946.
Chmielewski TL, Stackhouse S, Axe MJ, SnyderMackler L. A prospective analysis of incidence
and severity of quadriceps inhibition in a consecutive sample of 100 patients with complete
acute anterior cruciate ligament rupture. J
Orthop Res. 2004;22:925-930. http://dx.doi.
org/10.1016/j.orthres.2004.01.007
Deyle GD, Allison SC, Matekel RL, et al. Physical
therapy treatment effectiveness for osteoarthritis of the knee: a randomized comparison of
supervised clinical exercise and manual therapy
procedures versus a home exercise program.
Phys Ther. 2005;85:1301-1317.
Deyle GD, Henderson NE, Matekel RL, Ryder
MG, Garber MB, Allison SC. Effectiveness
of manual physical therapy and exercise in
osteoarthritis of the knee. A randomized, controlled trial. Ann Intern Med. 2000;132:173-181.
Dickstein R, Heffes Y, Shabtai EI, Markowitz E.
Total knee arthroplasty in the elderly: patients’
self-appraisal 6 and 12 months postoperatively.
Gerontology. 1998;44:204-210.
D’Lima DD, Colwell CW, Jr., Morris BA, Hardwick
ME, Kozin F. The effect of preoperative exercise
on total knee replacement outcomes. Clin Orthop Relat Res. 1996;174-182.
Ettinger WH, Jr., Afable RF. Physical disability
from knee osteoarthritis: the role of exercise
as an intervention. Med Sci Sports Exerc.
1994;26:1435-1440.
Evans WJ. Exercise training guidelines for the
elderly. Med Sci Sports Exerc. 1999;31:12-17.
Ferri A, Scaglioni G, Pousson M, Capodaglio P,
Van Hoecke J, Narici MV. Strength and power
changes of the human plantar flexors and knee
extensors in response to resistance training in
old age. Acta Physiol Scand. 2003;177:69-78.
Finch E, Walsh M, Thomas SG, Woodhouse LJ.
Functional ability perceived by individuals following total knee arthroplasty compared to agematched individuals without knee disability. J
Orthop Sport Phys Ther. 1998;27:255-263.
Fitzgerald GK. Therapeutic exercise for
knee osteoarthritis: considering factors that
may influence outcome. Eura Medicophys.
2005;41:163-171.
Fitzgerald GK, Oatis C. Role of physical therapy
in management of knee osteoarthritis. Curr
Opin Rheumatol. 2004;16:143-147.
Fitzgerald JD, Orav EJ, Lee TH, et al. Patient
journal of orthopaedic & sports physical therapy | volume 38 | number 5 | may 2005 | 253
[
(($
()$
(*$
(+$
(,$
(-$
(.$
(/$
)&$
)'$
)($
))$
)*$
quality of life during the 12 months following
joint replacement surgery. Arthritis Rheum.
2004;51:100-109. http://dx.doi.org/10.1002/
art.20090
Frontera WR, Hughes VA, Fielding RA, Fiatarone
MA, Evans WJ, Roubenoff R. Aging of skeletal
muscle: a 12-yr longitudinal study. J Appl
Physiol. 2000;88:1321-1326.
Gapeyeva H, Buht N, Peterson K, Ereline J,
Haviko T, Paasuke M. Quadriceps femoris muscle voluntary isometric force production and
relaxation characteristics before and 6 months
after unilateral total knee arthroplasty in
women. Knee Surg Sports Traumatol Arthrosc.
2007;15:202-211. http://dx.doi.org/10.1007/
s00167-006-0166-y
Gur H, Cakin N, Akova B, Okay E, Kucukoglu
S. Concentric versus combined concentriceccentric isokinetic training: effects on functional capacity and symptoms in patients with
osteoarthrosis of the knee. Arch Phys Med
Rehabil. 2002;83:308-316.
Gur H, Cakin N. Muscle mass, isokinetic torque,
and functional capacity in women with osteoarthritis of the knee. Arch Phys Med Rehabil.
2003;84:1534-1541.
Hartley RC, Barton-Hanson NG, Finley R,
Parkinson RW. Early patient outcomes after
primary and revision total knee arthroplasty.
A prospective study. J Bone Joint Surg Br.
2002;84:994-999.
Hassan BS, Mockett S, Doherty M. Static
postural sway, proprioception, and maximal
voluntary quadriceps contraction in patients
with knee osteoarthritis and normal control
subjects. Ann Rheum Dis. 2001;60:612-618.
Healy WL, Iorio R, Lemos MJ. Athletic activity
after total knee arthroplasty. Clin Orthop Relat
Res. 2000;65-71.
Huang CH, Cheng CK, Lee YT, Lee KS. Muscle
strength after successful total knee replacement: a 6- to 13-year followup. Clin Orthop
Relat Res. 1996;147-154.
Hurley MV, Jones DW, Newham DJ. Arthrogenic
quadriceps inhibition and rehabilitation of
patients with extensive traumatic knee injuries.
Clin Sci (Lond). 1994;86:305-310.
Hurley MV, Newham DJ. The influence of arthrogenous muscle inhibition on quadriceps
rehabilitation of patients with early, unilateral osteoarthritic knees. Br J Rheumatol.
1993;32:127-131.
Hurley MV, Scott DL. Improvements in quadriceps sensorimotor function and disability
of patients with knee osteoarthritis following
a clinically practicable exercise regime. Br J
Rheumatol. 1998;37:1181-1187.
Jones CA, Voaklander DC, Johnston DW,
Suarez-Almazor ME. Health related quality of
life outcomes after total hip and knee arthroplasties in a community based population. J
Rheumatol. 2000;27:1745-1752.
Jones DL, Westby MD, Greidanus N, et al. Update on hip and knee arthroplasty: current state
of evidence. Arthritis Rheum. 2005;53:772-780.
CLINICAL COMMENTARY
http://dx.doi.org/10.1002/art.21465
)+$ Kane RL, Saleh KJ, Wilt TJ, Bershadsky B. The
functional outcomes of total knee arthroplasty.
J Bone Joint Surg Am. 2005;87:1719-1724.
http://dx.doi.org/10.2106/JBJS.D.02714
),$ Kent-Braun JA, Le Blanc R. Quantitation of
central activation failure during maximal voluntary contractions in humans. Muscle Nerve.
1996;19:861-869. http://dx.doi.org/10.1002/
(SICI)1097-4598(199607)19:7&lt;861::AIDMUS8&gt;3.0.CO;2-7
)-$ Kroll MA, Otis JC, Sculco TP, et al. The relationship of stride characteristics to pain before and
after total knee arthroplasty. Clin Orthop Relat
Res. 1989;191-195.
).$ Kuster MS. Exercise recommendations after
total joint replacement: a review of the current
literature and proposal of scientifically based
guidelines. Sports Med. 2002;32:433-445.
)/$ Landers KA, Hunter GR, Wetzstein CJ, Bamman
MM, Weinsier RL. The interrelationship among
muscle mass, strength, and the ability to perform physical tasks of daily living in younger
and older women. J Gerontol A Biol Sci Med
Sci. 2001;56:B443-448.
*&$ Lewek M, Stevens J, Snyder-Mackler L. The use
of electrical stimulation to increase quadriceps
femoris muscle force in an elderly patient
following a total knee arthroplasty. Phys Ther.
2001;81:1565-1571.
*'$ Ling SM, Xue QL, Simonsick EM, et al. Transitions to mobility difficulty associated with lower
extremity osteoarthritis in high functioning
older women: longitudinal data from the Women’s Health and Aging Study II. Arthritis Rheum.
2006;55:256-263. http://dx.doi.org/10.1002/
art.21858
*($ Lorentzen JS, Petersen MM, Brot C, Madsen
OR. Early changes in muscle strength after total
knee arthroplasty. A 6-month follow-up of 30
knees. Acta Orthop Scand. 1999;70:176-179.
*)$ Mahomed NN, Liang MH, Cook EF, et al. The
importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29:1273-1279.
**$ Manal TJ, Snyder-Mackler L. Failure of voluntary
activation of the quadriceps femoris muscle
after patellar contusion. J Orthop Sports Phys
Ther. 2000;30:655-660; discussion 661-653.
*+$ March LM, Cross MJ, Lapsley H, et al. Outcomes after hip or knee replacement surgery
for osteoarthritis. A prospective cohort study
comparing patients’ quality of life before and
after surgery with age-related population
norms. Med J Aust. 1999;171:235-238.
*,$ Martin SD, Scott RD, Thornhill TS. Current
concepts of total knee arthroplasty. J Orthop
Sports Phys Ther. 1998;28:252-261.
*-$ Mazzeo RS, Cavanagh P, Evans WJ, et al. American College of Sports Medicine Position Stand.
Exercise and physical activity for older adults.
Med Sci Sports Exerc. 1998;30:992-1008.
*.$ McMahon M, Block JA. The risk of contralateral total knee arthroplasty after knee
replacement for osteoarthritis. J Rheumatol.
254 | may 2008 | volume 38 | number 5 | journal of orthopaedic & sports physical therapy
]
2003;30:1822-1824.
*/$ Miller M, Flansbjer UB, Downham D, Lexell J.
Superimposed electrical stimulation: assessment of voluntary activation and perceived
discomfort in healthy, moderately active older
and younger women and men. Am J Phys
Med Rehabil. 2006;85:945-950. http://dx.doi.
org/10.1097/01.phm.0000247648.62957.19
+&$ Miner AL, Lingard EA, Wright EA, Sledge CB,
Katz JN. Knee range of motion after total
knee arthroplasty: how important is this
as an outcome measure? J Arthroplasty.
2003;18:286-294. http://dx.doi.org/10.1054/
arth.2003.50046
+'$ Mintken PE, Carpenter KJ, Eckhoff D, Kohrt
WM, Stevens JE. Early neuromuscular electrical stimulation to optimize quadriceps muscle
function following total knee arthroplasty:
a case report. J Orthop Sports Phys Ther.
2007;37:364-371. http://dx.doi.org/10.2519/
jospt.2007.2541
+($ Mizner RL, Petterson SC, Snyder-Mackler
L. Quadriceps strength and the time course
of functional recovery after total knee
arthroplasty. J Orthop Sports Phys Ther.
2005;35:424-436.
+)$ Mizner RL, Petterson SC, Stevens JE, Axe MJ,
Snyder-Mackler L. Preoperative quadriceps
strength predicts functional ability one year
after total knee arthroplasty. J Rheumatol.
2005;32:1533-1539.
+*$ Mizner RL, Petterson SC, Stevens JE, Vandenborne K, Snyder-Mackler L. Early quadriceps
strength loss after total knee arthroplasty. The
contributions of muscle atrophy and failure
of voluntary muscle activation. J Bone Joint
Surg Am. 2005;87:1047-1053. http://dx.doi.
org/10.2106/JBJS.D.01992
++$ Mizner RL, Snyder-Mackler L. Altered loading
during walking and sit-to-stand is affected
by quadriceps weakness after total knee arthroplasty. J Orthop Res. 2005;23:1083-1090.
http://dx.doi.org/10.1016/j.orthres.2005.01.021
+,$ Mizner RL, Snyder-Mackler L. Patients perceptions do not match functional performance or
clinical presentation after total knee arthroplasty. 10th World Congress on Osteoarthritis.
Prague, Czech Republic: 2006.
+-$ Mizner RL, Stevens JE, Snyder-Mackler L.
Voluntary activation and decreased force
production of the quadriceps femoris muscle
after total knee arthroplasty. Phys Ther.
2003;83:359-365.
+.$ Moffet H, Collet JP, Shapiro SH, Paradis G, Marquis F, Roy L. Effectiveness of intensive rehabilitation on functional ability and quality of life
after first total knee arthroplasty: A single-blind
randomized controlled trial. Arch Phys Med
Rehabil. 2004;85:546-556.
+/$ Noble PC, Gordon MJ, Weiss JM, Reddix RN,
Conditt MA, Mathis KB. Does total knee replacement restore normal knee function? Clin
Orthop Relat Res. 2005;157-165.
,&$ Ouellet D, Moffet H. Locomotor deficits before
and two months after knee arthroplasty. Ar-
,'$
,($
,)$
,*$
,+$
,,$
,-$
,.$
,/$
-&$
thritis Rheum. 2002;47:484-493. http://dx.doi.
org/10.1002/art.10652
Parent E, Moffet H. Comparative responsiveness
of locomotor tests and questionnaires used to
follow early recovery after total knee arthroplasty. Arch Phys Med Rehabil. 2002;83:70-80.
Perhonen M, Komi P, Hakkinen K, von Bonsdorff
H, Partio E. Strength training and neuromuscular function in elderly people with total knee
endoprosthesis. Scand J Med Sci Sports.
1992;2:234-243.
Peterson SC, Mizner RL, Snyder-Mackler L.
Quadriceps Femoris Muscle Recovery After
Total Knee Arthroplasty. 9th World Congress on
Osteoarthritis. Chicago, IL: 2004.
Ritter MA, Albohm MJ, Keating EM, Faris PM,
Meding JB. Comparative outcomes of total joint
arthroplasty. J Arthroplasty. 1995;10:737-741.
Ritter MA, Carr KD, Keating EM, Faris PM. Longterm outcomes of contralateral knees after unilateral total knee arthroplasty for osteoarthritis.
J Arthroplasty. 1994;9:347-349.
Ritter MA, Thong AE, Davis KE, Berend ME,
Meding JB, Faris PM. Long-term deterioration
of joint evaluation scores. J Bone Joint Surg Br.
2004;86:438-442.
Rodgers JA, Garvin KL, Walker CW, Morford
D, Urban J, Bedard J. Preoperative physical
therapy in primary total knee arthroplasty. J
Arthroplasty. 1998;13:414-421.
Rooks DS, Huang J, Bierbaum BE, et al. Effect
of preoperative exercise on measures of functional status in men and women undergoing total hip and knee arthroplasty. Arthritis Rheum.
2006;55:700-708. http://dx.doi.org/10.1002/
art.22223
Roos EM, Toksvig-Larsen S. Knee injury
and Osteoarthritis Outcome Score (KOOS)
- validation and comparison to the WOMAC
in total knee replacement. Health Qual
Life Outcomes. 2003;1:17. http://dx.doi.
org/10.1186/1477-7525-1-17
Rossi MD, Brown LE, Whitehurst M. Early
strength response of the knee extensors
-'$
-($
-)$
-*$
-+$
-,$
--$
-.$
during eight weeks of resistive training after
unilateral total knee arthroplasty. J Strength
Cond Res. 2005;19:944-949. http://dx.doi.
org/10.1519/R-14333.1
Rossi MD, Brown LE, Whitehurst M. Knee extensor and flexor torque characteristics before
and after unilateral total knee arthroplasty. Am
J Phys Med Rehabil. 2006;85:737-746. http://
dx.doi.org/10.1097/01.phm.0000233178.22621.
a5
Silva M, Shepherd EF, Jackson WO, Pratt JA,
McClung CD, Schmalzried TP. Knee strength
after total knee arthroplasty. J Arthroplasty.
2003;18:605-611.
Slemenda C, Brandt KD, Heilman DK, et al.
Quadriceps weakness and osteoarthritis of the
knee. Ann Intern Med. 1997;127:97-104.
Slemenda C, Heilman DK, Brandt KD, et al.
Reduced quadriceps strength relative to body
weight: a risk factor for knee osteoarthritis in
women? Arthritis Rheum. 1998;41:1951-1959.
http://dx.doi.org/10.1002/15290131(199811)41:11<1951::AID-ART9>3.0.CO;2-9
Snyder-Mackler L, De Luca PF, Williams
PR, Eastlack ME, Bartolozzi AR, 3rd. Reflex
inhibition of the quadriceps femoris muscle
after injury or reconstruction of the anterior
cruciate ligament. J Bone Joint Surg Am.
1994;76:555-560.
Stackhouse SK, Dean JC, Lee SC, BinderMacLeod SA. Measurement of central activation
failure of the quadriceps femoris in healthy
adults. Muscle Nerve. 2000;23:1706-1712.
http://dx.doi.org/10.1002/10974598(200011)23:11<1706::AIDMUS6>3.0.CO;2-B
Stackhouse SK, Stevens JE, Lee SC, Pearce KM,
Snyder-Mackler L, Binder-Macleod SA. Maximum voluntary activation in nonfatigued and
fatigued muscle of young and elderly individuals. Phys Ther. 2001;81:1102-1109.
Stevens JE, Mizner RL, Snyder-Mackler L.
Neuromuscular electrical stimulation for
quadriceps muscle strengthening after bilateral
-/$
.&$
.'$
.($
.)$
.*$
.+$
total knee arthroplasty: a case series. J Orthop
Sports Phys Ther. 2004;34:21-29.
Stevens JE, Mizner RL, Snyder-Mackler L. Quadriceps strength and volitional activation before
and after total knee arthroplasty for osteoarthritis. J Orthop Res. 2003;21:775-779. http://
dx.doi.org/10.1016/S0736-0266(03)00052-4
Stickles B, Phillips L, Brox WT, Owens B,
Lanzer WL. Defining the relationship between
obesity and total joint arthroplasty. Obes Res.
2001;9:219-223.
Stratford PW, Kennedy DM. Performance measures were necessary to obtain a complete picture of osteoarthritic patients. J Clin Epidemiol.
2006;59:160-167. http://dx.doi.org/10.1016/j.
jclinepi.2005.07.012
van Baar ME, Assendelft WJ, Dekker J,
Oostendorp RA, Bijlsma JW. Effectiveness
of exercise therapy in patients with osteoarthritis of the hip or knee: a systematic
review of randomized clinical trials. Arthritis
Rheum. 1999;42:1361-1369. http://dx.doi.
org/10.1002/1529-0131(199907)42:7<1361::AIDANR9>3.0.CO;2-9
Volpi E, Nazemi R, Fujita S. Muscle tissue
changes with aging. Curr Opin Clin Nutr Metab
Care. 2004;7:405-410.
Walker DJ, Heslop PS, Chandler C, Pinder IM.
Measured ambulation and self-reported health
status following total joint replacement for the
osteoarthritic knee. Rheumatology (Oxford).
2002;41:755-758.
Walsh M, Woodhouse LJ, Thomas SG, Finch E.
Physical impairments and functional limitations: a comparison of individuals 1 year after
total knee arthroplasty with control subjects.
Phys Ther. 1998;78:248-258.
@
CEH;?D<EHC7J?ED
WWW.JOSPT.ORG
7FF;D:?N
H;>78?B?J7J?ED=K?:;B?D;I<EBBEM?D=7JEJ7BAD;;7HJ>HEFB7IJO
F^Wi[?0>ec[^[Wbj^ehekjfWj_[djf^oi_YWbj^[hWfo(#)j_c[if[hma"(#)ma
Goals:
1. Increase range of motion (ROM)
2. Decrease edema and pain
3. Gait training
4. Independence with activities of daily living (ADLs)
Exercises:
1. Seated or supine knee active range of motion (AROM)
2. Alternated ankle dorsiflexion and plantar flexion
3. Quadriceps sets
4. Straight-leg raise
5. Hamstring sets
6. Standing leg curls
7. Seated knee extension
8. Supported single standing for balance
9. Repeated sit-to-stand transfer training
10. Ambulating with appropriate assistive device
Modalities:
1. Ice 2-3 times per d, with lower extremity elevated for 20-30 min
journal of orthopaedic & sports physical therapy | volume 38 | number 5 | may 2008 | 255
[
CLINICAL COMMENTARY
]
7FF;D:?N9EDJ?DK;:
Criteria for progression to exclusively outpatient physical therapy:
a. AROM approaching 90° of knee flexion
b. Minimal pain/swelling
c. Independence in mobility in and out of the home
F^Wi[??0EkjfWj_[djf^oi_YWbj^[hWfo(#)j_c[if[hma"*#,ma
Warm-up (15-20 min):
1. Exercise bike (10-15 min), start with forward and backward pedaling with no
resistance until there’s enough knee ROM for a full revolution. Seat height may
be lowered for progression of ROM
Exercise progression:
a. Exercises are to be progressed once the patient can complete 3 sets of 10
reps of the exercise correctly and feels maximally fatigued
b. Add 0.2- to 1.5-kg weights to the exercises
c. Increase step height if showing good concentric/eccentric control
d. Increase wall slides to 60° and to 90°
F^Wi[???0I[c_#_dZ[f[dZ[djf^Wi['j_c[f[hmaehX_m[[abo"*#,m[[ai
Exercises:
1. Continue all exercises in phase I as a home exercise program or a gym
membership
2. Seated or supine knee AROM (flexion and extension)
3. Alternated ankle dorsiflexion and plantar flexion
4. Passive knee extension stretch
5. Patellar and knee mobilizations
Specific strengthening (10-15 min), 1-3 sets of 10 repetitions:
1. Neuromuscular electrical stimulation (NMES) to augment quadriceps muscle
activation. NMES parameters: 2500-Hz triangular-wave alternating current,
12-s on-time, 80-s off-time, 2- to 3-s ramp-up time, knee flexed to 60°, 10
isometric contractions, dose set to maximally tolerated by the patient, large
(7.6 12.7 cm) self-adhesive electrodes placed on the motor points of the
quadriceps femoris muscle
2. Quadriceps sets
3. Straight-leg raises (assistance as needed, goal to perform without a knee
extension lag)
4. Hip abduction (side lying)
5. Standing leg curls
6. Seated knee extension
7. Standing terminal knee extension from 45° to 0°
Functional exercises (10-15 min):
1. Step-ups, 5-15 cm, or climbing a flight of stairs
2. 45° wall slides or sit-to-stands
3. Walking backward, side step, march, or crossover steps
4. Walking through an obstacle course
5. Gait training emphasis on heel strike and push-off at toe-off
Endurance exercises (5-20 min):
1. Walking
2. Stationary cycle
Cool-down (10 min):
1. Ice and compression as needed
2. Gentle stretching and ROM
Criteria for progression:
a. Voluntary quadriceps muscle control or 0° knee extension lag
b. AROM 0° to greater than 105° of knee flexion
c. Minimal to no pain and swelling
Warm-up (15-20 min):
1. Seated or supine knee AROM (flexion and extension)
2. Alternated ankle dorsiflexion and plantar flexion
3. Passive knee extension and hamstring stretch
4. Exercise bike or treadmill walking (perceived exertion should be light)
Strengthening (20 -30 min, 1-3 sets of 10-20 reps of any of the following):
1. Leg press varying working ROM*
2. Leg extension: ROM, 90°-0° or 90°-30° for extension*
3. Standing or sitting leg curls*
4. Standing heel raises*
5. 4-way hip machine or (rubber band or ankle weights for resisted hip ROM)*
6. Sit-to-stand free weights in hands
7. Weight-bearing exercises with emphasis on eccentric control
8. Upper extremity strength training optional
*Use a 5- or 10-repetition maximum to determine 60%-70% resistance of 1-repetition maximum
*Machine weights
Functional exercises (10-15 min):
1. Step-ups 5-15 cm or climbing a flight of stairs
2. 45° to 90° wall slides or sit-to-stands, hold 5-10 s
3. Walking backward, side step, march, or crossover steps
Endurance exercises (5-20 min, alternate between walking and biking):
1. Walking, change speed and incline
2. Biking
Criteria for progression:
Exercises are to be progressed once the patient can complete 3 sets of 10 reps
of the exercise correctly and feels maximally fatigued
Exercise progression:
a. Reassess 65%-70% of maximal effort biweekly to determine progression of
resistance
b. Increase step height if showing good concentric/eccentric control
c. Increase wall slides to 60° and to 90°
F^Wi[?L0?dZ[f[dZ[djf^Wi[l_i_jiiY^[Zkb[Z'j_c[%maehX_m[[abo\eh.ma"ehWi
d[[Z[Z"jeh[Wii[iiijh[d]j^"HEC"WdZ\kdYj_ed"WdZjefhe]h[ii[n[hY_i[i
Exercises (continue all exercises, 1-3 sets at 10-20 reps, as a home program or
a gym membership 2-3 times/wk)
256 | may 2008 | volume 38 | number 5 | journal of orthopaedic & sports physical therapy