Document 10804707
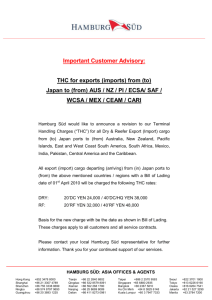
advertisement

J unn ( l , l A t h l c r i cT r a i nin g 2 0 0 2 .3 1 ( 3 ) :2 5 6 _ 2 6 1
O by t h e N a r i o n aA
l r h l e r iCT r a in e r Asso
s'
cia r io nln. c
u u u . j o u r n a lfoi r r hI e ti c t r ai nin g .o r g
IntraraterReliabilityof Functional
PerformanceTestsfor subjects with
Patellofemoral
PainSyndrome
Janice K. Loudon*;Doug wiesnerf; HeatherL. Goist-Foley*;cari Asjesf;
KarenL. Loudon*
*University
of Kansas, Overland Park, KS; fSports Rehabilitationand physical Therapy, overland park,
KS
Janice K' Loudon,PhD, ATc, PT, contributedto conceptionand design; acquisitionand
analysisand interpretationof thedata,
and draftingand criticalrevisionand final approvat
article.ooulg iviesner,ATC, Heather Goist-Fotey,MSpT, cari Asjes,
.of
.tite
PT, and KarenLoudon,ATC, M)MT, PT, contribuledto conceptionind design; acquisition
and anatysisandinterpretation
of
the data; and draftingand finat approva!of the afticte.
Address correspondenceto Janice K. Loudon, PhD, ATC, PT, t)niversityof KansasMedical
center, g,4g outtook, overlano
Park, KS 66207.Address e-mail to jloudon@kumc.edu.
Objective: Patellofemoralpain syndrome (pFpS) is a com_
mon clinicalentity seen by the sports medicine specialist.The
ultimategoal of rehabilitationis to returnthe patientto the hioh_
est functionallevel in the most efficientmanner. Therefore,ii is
necessaryto assess the progress of patientswith pFpS using
reliablefunctionalperformancetests. Our purposewas to eval_
uate the intraraterreliabilityof S functionalperformancetests in
patientswith PFPS.
Design and Setting: We used a test-retest reliabilitydesign
in a c linicse tting .
Subjects: Two groups of sublects were studied: those with
PFPS (n : 29) and those with no known knee condition(n =
11). Th e PFPS g rou p inc luded 19 wom en and . 10m en w i t h a
mean a ge o f 2 7.6 + 5 . 3 y ear s , height of 169. g0 * 10 . 5 c m ,
and weig ht of 6 9.5 9 + 15. 8 k g. The nor m al gr oup inc l u d e d7
women and 4 men with a mean age of 30.3 + 5.2 years, height
of 169.5 5 * 9 .9 cm, a nd weight 69. 42 * 14. 6 k g.
Measuremenfs: The reliabilityof 5 functional performance
tests (anteromediallunge, step-down,single-legpress, bilateral
squat, balance and reach) was assessed in 15 subiects with
PFPS. Secondly, the relationshipof the 5 functionaltests to
parnwas assessed in 29 PFpS subjectsusing pearson product
moment correlations.The limb symmetry index (LSl) was cal_
culated in the 29 PFPS subjects and compared with the group
of 11 normal subjects.
Resu/fs.' The 5 functional tests proved to have fair to high
intrarater reliability.Intrarater reliabilitycoefficients(lCC 3,1)
ranged from .79 to .94. For the pFpS subiects, a statistical
differenceexisted between limbs for the anieromediallunge,
step-down,single-legpress, and balance and reach. All func_
tional tests correlatedsignificanflywith pain except for the bi_
lateral squat; values ranged from .39 to .73. The average LSI
for the PFPS group was B5%, while the average LSI for the
normal subjectswas g7?o.
Conclusions: The 5 functional tests proved to have good
intraraterreliabilityand were relatedto changes in pain. Future
researchis needed to examine interraterreliability,validity,and
sensitivityof these clinicaltests.
Key Words: step-down,squat, limb symmetry, Knee
atcllot'cmoralpain syndrome (PFpS) is a cornrnon clinical entity uscd to describea varicty ofpathologic conditions associatedwith the articulation betwcen the unclersurfaceof thc patclla and thc femoral condylcs. patcllofcmoral pain syndrontccan be causedby a variciy of factors, including quadriccpswcakncss,increasede anglc, faulty lower
cxtren-ritymechanics,ovcrusc, and lateral retinaculum tisht_
ness.l.2Thc rnajor complaints of patients with pFpS ur..-diffusc kncc pain, patellar crepitus and locking, knec joint stiffncss, and dccrcasedactivity levels.s-7Onsct of symptoms is
usually insidious and may occur bilaterally. Activities such as
prolongcd sitting, stair desccnt,and squattingoften exaccrbate
t he pa in.E
The ultimate goal of rehabilitation for patients with pFpS
rs return to thc highest functional level in the most cfficient
rnanner.'/Accompanying this goal is the need for a testing
rnethodthat is objective,rcliablc, and sensitivcto the changin!
statusof PFPS. Comrnon objective measuresof knee function
include pain asscssmcnt,goniomctry, girth rlcasurcnlent,man_
ual musclc testing, and isokinetic evaluation. Howcver, thesc
tcsts have bcen shown to be poor prcdictors 6f funs1j6n.6.l{)
Functional testing is an attempt to evaluatc thc knec joint
under conditions that mimic realistic functional dernands.per_
fomrance on functional tests depcnds on many variablcs,in_
cluding pain, swelling, crcpitus, ncurornuscularcoordination,
muscular strength, and joint stability.ll The tests should bc
time efflcient and simple to pcrforrn with minirnal instruction;
they should requirc minirnal staff training and be conductecl
within a clinical setting. Scveral functional knce tests arc described in the literature and include thc shuttle run, stair-runnlng test, verticaljump test, and hop 19515.10-12
Thesetcstsare
useful after ligamentous knee injuries or othcr sport-related
injuries, such as muscle strains or meniscus injuries, and arc
not specific to the patellofemoraljoint.
Functional performance tests that arc specific for pFpS
s h o u l d b e c h o s e n b a s e d o n c l i n i c a l c v i d e n c l a n d t h e c ase o f
256
Volume 37 o Number 3 o September 2002
replication among clinics and facilities. Pain is a factor associated with PFPS and is commonly used as a measurementto
determine functional improvement. Chesworth et all3 evaluatcd the visual analog scale (a measure of pain) in patients
with PFPS, finding poor day-to-day rcliability but good sensitivity to clinical changes.In addition to measuring pain dircctly, performance of a functional test may add infom.ration
rcgarding muscle strength,endurance,proprioception,and balFunctional tests specific to PFPS should include wcightbearing stresswith various knee-flexion angles becausethese
are common aggravatingpositions and require dynamic nruscular control. Post and Fulkerson8found that 86''/"of patients
with patcllofernoralpain havc pain during stair climbing and
85% havc pain with squatting.The increascin pain with thcsc
joint
activitics is correlatedwith an increasein patcllofen.roral
rcaction forcc,3.'1'8'i4
At prcscnt, no functional tcsts specificto
thc patcllofcnroraljoint havc bccn reported in thc litcraturc.
Wc cvaluatedthc following functional pcrfonrance tcsts in
this study: anteromcdiallunge, step-down,single-legpress,bilatcral squat, ancl balance and reach. Thc antcrornediallunge
is a multiplanar rnovement designed to challenge the latcral
patcllofemoralarticulationwith thc valgus stressplaccd on the
kncc cluring thc ntancuvcrl5 Thcorctically, as an individual
lunges and thc ccntcr of gravity rnovcs fbrward and acrossthc
body, thc pull of the quadriccps rnuscle causescomprcssive
loading of thc lateral patellofcrnoralarticulation, a cotlrrron
site of patcllofemoral syrnptonrs.The step-down nrirnics the
function of stair dcsccnt, a cornnton aggravating factor. Thc
loacl of thc patcllof'crnoraljoint with stair dcsccnt has bccn
lcportcd to bc 3.5 tirncs body weight.rb A singlc-lcg prcss tcst
was chosen to strcss thc patellof'entoral joint in a partial
wcight-bcaring nrocic.This tcst can bc aclministcrcdearly in
rchabilitation whcn a full squat nray bc too aggravating.To
fufthcr challcngc thc patcllofcrroral .joint, a sccond tcst is a
full wcight-bcaringbilatcral squat. Thc joint rcaction forcc of
a squat to 90' is approxirnatcly 7.5 tinrcs body wcight.3 Thc
balancc-ancl-rcach
tcst, dcscribcd by Gray,ls spccifically challcn gcs sin glc-lcg b alanc c .
Thc primary purposc of our study was to detcminc thc
intraratcr rcliability of 5 functional pcrlbrrtrancctests on paticnts with PFPS. Sccondarypurposcswcrc to detcrntinelimb
syrnlnctry indcx (t-SI) dif-fercnccsfor involvcd and uninvolved
linrbs and to asscssthe rclationshirlbctwecn thc 5 functional
tcsts and pain ratings.
METHODS
Subjects
Two groupsof subjccts
wcrc includcdin this study,onc
group with PFPS (n : 29) and a secondgroup with no known
kncc condition (n : ll). The PFPS group included l9 wonren
and l0 men with a mcan age of 2'7.6 'r 5.3 years, height of
169 .U0 | 1 0.5 cm, and weight of 69. 59 | 15. 8 k g. D a t a f r o m
I 5 of these 29 subjects were used for the reliability tcsting.
Inclusion critcria for the subjects in the PFPS group wcrc 2
of the following on initial assessment:pain on direct compression of the patella against the femoral condylcs with the
knee in full cxtension,tendernesson palpation of the lateral
surfacc of the patella,pain on resistedknec cxtension,or pain
with isometric quadricepscontractionagainstsuprapatellarresistancewith the knee in slight flexion. These subjects'symp-
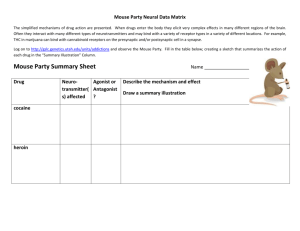
Figure'1. Anteromediallungetest.
toms wcrc consistentwith the cxccssive latcral prcssurcsyndrome as describedby Wilk et al.l7 Exclusion critcria for both
groups included a history of patcllar trauma; subluxation;dislocation; confirmcd ligamcntous,meniscal,or fat-paddarnagc,
evidcnce of tcndinitis, bursitis, or effusion; cvidcnce of rcferred pain from thc back or hip; osteochondralor chondral
fiacturcs; or uppcr or lower motor neuron lssl6n.l8.leThc duration of patellofenroral pain averaged 5.2 rnonths for thc
PFPS group. Thc normal group included 7 womcn and 4 nrcn
w i t h a m c a n a g c o f 3 0 . 3 + 5 . 2 y c a r s , h c i g h t o f 1 6 9 .5 5 t 9 .9
cm, and wcight of 69.42 -r 14.6 kg. Thc norrnal subjcctswcrc
used to compare the LSIs.
Experimental
measurements
Anteromedial lunge, left and right, For thc antcromcdral
lungc, thc subject is lincd up bchind a starl linc. Thc tcst is
pcrfbrrncd by having thc subject lungc forward with thc uninvolvcd limb so that thc front lcg is bcnt to 90' and crosscs
thc midlinc. The subjcct rtrust maintain good balancc ancl an
ercct trunk posturc. Distancc is recordcd from thc start line to
thc hcel of thc leacl limb during the lungc-out position. Thc
r.naximaldistancc of 3 trials is recordcd and markcd. Eighty
pcrcent of the maximal distancc is calculatedand n.rarkcdwith
a piccc of tape as a targct fbr thc scrics of timcd lungcs. Thc
subjcct is then asked to complete as many lunges as possiblc
in 30 scconds;lungcs lcss than thc 80% mark are not recordcd.
If thc subject deviatcs from thc path of motion or takcs an
extra stcp, the lunge is not included in the count. Thc involvcd
limb is thcn tested,using the 80% rnark fiom the uninvolvcd
limb (Figurc l).
Step-down, left and right. The step-down is a unilateral
test perfonned frorn a platforrn 8 inches(20.32 cm) high. Subjects step forward and down toward the floor. Thc down lirnb
only brushes the floor with the heel and thcn rctums to full
knee extension.This counts as one repetition. Each repetition
must bc cornpletedsuch that the step limb is not used to accelerateback onto the step. The number of repetitionsthe subject performs in 30 secondsis recorded.Both limbs arc tcsted
(Figure 2).
Single-leg press. Subjectsare positioned on the Total Cyrn
(FitnessQuest Inc, Canton, OH) at level 7, which is considcred
to be 50% of the subject's body weight. Subjectsbegin with
the test kncc in full extension. One repetition consists of a
complete cycle of full knee extension to 90' of knee flexion
Journal of AthleticTrainino
257
r
extreme right represents severe pain. The marked value was
measured with a standard ruler and then converted to a pain
score. The VAS has been previouslv validated in the literal u r e 2 {)a n d u s c d i n p a t i e n t sw i t h P F P S . l l
Procedure
The University of Kansas Medical Ccnter's InternalReview
Board approved the study. Bcfore participating,subjcctswcre
screencd with questions rcgarding previous lowcr extrentity
injuries. After being selectedto participate,each subjectcompleted an informcd consent form followed by the VAS. Aftcr
F igur e 2 , S t e p - d o w n t e st.
completing the VAS, thc subject was instructedin the propcr
technique for cach of thc functional performancc tests. Thc
subjectperformed each ofthe functional testsin random order,
and both lower extremitics were tcstcd. The beginningtest lcg
was randomly assigncd for thc single-lcg press and thc stcpdown test. Each tcst was perfon.nedonce, without the usc of
tapc or a brace. Pain lcvel during the test was ntonitorcd,and
subjectswere instructcd that thcy could stop duc to pain, but
prin lcvcl wts not a slopping critcrron.
Each subjcct bcgan thc assessmcntsessionwith a warnt-up
pcriod that consisted of low-resistance,lowcr cxtrcrnrty cycling. Thc task-spccific wantl-up includcd practicc fbr cach
F igur e 3 . S i n g l e - l e g p r e ss te st.
functional pcrfornrancctcst (3 to 5 rcpctitions with a 30-sccond rcst bcfbrc thc actual tcsting). A writtcn dcscription of
each tcst was rcad to thc subjcct, fbllowcd by a dcnronstration
of thc test by thc tcstcr (Appcndix). Participantsrcccivcclno
vcrbal encouragcmcntduring actual tcsting. Subjcctswcrc allowcd a l-minutc rcst bctwccn functional pcrforrrance tcsts.
Reliability. For intraratcrrcliability, l5 subjcctswith PFPS
wcrc tcstcd on 2 occasions,48 to 72 hours apart.Thc randorn
ordcr of functional tcsting was nratchcd bctwcen day I and
day 2. Visual analog scalc scorcshad to match within 0.5 fi'om
test clay I to test day 2 (cg, a subjcct who scorcd (r.5 on clay
Figure4. Balance-and-reach
test.
I had to score bctwccn (r.0 ancl 7.0 on clay 2). Pain has nrotivational, affcctivc, cognitivc, bchavioral,and scnsorydirncnand rcturn to full knec cxtcnsion. 'fhc numbcr of unilatcral sions,2land thcsc factorscan hindcr a tcst-rctcstdcsign.Thcrcsquats con.rplctcdin 30 scconds is rccordcd. Both limbs arc forc, for rcliability tcsting, subjcctshad to scorc within 0.5 on
thc VAS fiorn tcst day I to tcst day 2 to prcvcnt confounding
tcstcd (Figu rc 3 ).
Bilateral squat. Sub.jcctsstart this tcst standing with the of the pain variable.
C o r r e l a t i o n . T h e s c o r c s o n d a y I o f t h c l 5 r e l i a b i l i ty su b knccs in full extcnsion,shouldcr-widthapart,and wcight cvenly distributcd on both lirnbs. Subjccts lower thcir bodies to a jccts werc addcd to the scores of l4 othcr individuals with
kncc position of 90" and thcn rcturn to full extcnsion. One unilatcral PFPS who had complctcd thc VAS and 5 functional
rcpctition consistsof a corrrpletccycle of straight standing to tcsts. This infbm.rationwas uscd to establish a rclationshin
90" ofknee flcxion and rcturn to straightstanding.The number bctwcen the VAS and functional tcst scorcs. All sublcct.s
scorcdwithin this range except for 2. Both subjcctswcrc askcd
of bilatcral squatscompletcd in 30 scconds is recordcd.
Balance and reach. The subjectstartsthe test behind a start to return within 48 hours and repcat the VAS. Upon rcturn, I
line. The subjcct rcachesstraight forward with one leg so that of thc 2 subjectsscorcd within thc acccptableVAS rangc; the
thc hcel touchcs thc flooq with rnost of the body weight re- other did not and was dropped from thc study.
Limb Symmetry Index. The PFPS limb scoreswere cornn.rainingon thc back (tcst) leg. The uninvolvcd limb is tested
first. Distancc is recordedfrom the start linc to the heel of the p a r e d a n d a n L S I w a s c s t a b l i s h e d . r l T h c g r o u p o f l l su b j ccts
lcad limb. The rnaximal distance of 3 trials is recorded and with norn.ralknees also pcrformed thc 5 functional tests to
markcd. E,ightypcrcent of the maximal distanceis calculated deterrninethc LSI.
and rnarked with a piece of tape. During the 30-secondtest
period, thc subjectperforms as many balance-and-reach
lunges
DataAnalyses
as possiblc. Only lunges in which the subject's heel touchcs
beyonclthc 80% mark are recorded.The involved limb is thcn
We con.rpileddescriptivecharacteristicsfor each subjcctand
tested using the 80% mark from the uninvolved limb (Figurc all perfonnance scores in a Microsoft Excel (Microsoft Inc,
4).
vcrsion 2000, Redrnond,WA) spreadsheet.
Data frorn thc VAS
Visual Analog Scale (VAS). A l0-cm horizontal line was were recorded as a single score to one decimal placc. Data
uscd to assesspatellofcmoralknee pain over the 24 hours be- from each of the functional pcrformance tests were rccorded
tbre the testing pcriod. The far left is "pain free," and the as numbcr of repetitions. We recorded repetitions for right and
258
V olum e 37 r N u mb e r 3 o S e o te m b e r2 0 0 2
Table1. IntraraterReliabilityEstimatesfor FunctionalTests
Test
Anteromedial unge
Step down
Sin g l e - l e gp r e s s
Bil a t e r a ls q u a t
Ba l a n c e a n d r e a c h
In tr a cla ssCo r r e la tio n Sta n d ard E rror of
Co e fficie n t( 3 ,1 )
th e Mean
82
94
3B
6l
30
79
B3
47
68
RESULTS
Reliability
Intraclass correlation coefficients and SEMs for thc intratester mean scores are summarized in Table l. Intraclasscorrelation coefficientsranged from .79 to .94, and SEMs rangcd
from .38 to .68. The highest ICC was found with the stepdown test and the lowest ICC with the bilateral souat test.
Correlation
Table2. PearsonCorrelationCoefficients
F u n c t i o n a lT e s t
r Va lu e with Visu a l An al og S cal e
730-
An t e r o m e d i a l u n g e
Step down
S in g l e - l e gp r e s s
Bil a t e r a ls q u a t
Ba l a n c e a n d r e a c h
q-7n+
s031
386
461.
.Significant
at .05level.
at .01 level.
f Significant
Thc correlation matrix from the Pearson correlation cocfficicnt analysesis found in Table 2. Corrclation valuesbctwccn
thc VAS and thc functional tests ranged from .386 to .730.
Only the bilateral-squattcst did not corrclatcsignificantlywith
the VAS.
Limb Symmetry
Index
Lirnb difference in thc PFPS group was statisticallysignif'icant (P < .013) for all unilatcral functional tcsts. Limb dif-f-erenccin the normal subjccts was not statisticallysignificant
for any ofthc unilatcral functional tcsts.The LSI rangcd front
lcll anterornediallunge, right and lcft stcp-down,right and lefl 95.lVo to l00.6oh in thc normal group and 80.0% to 89.11%in
lcg prcss, bilatcral squat, and right and lcft balancc and rcach. thc PFPS group.
SPSS fb r Wind ows ( v c r s ion 10, SPSS I nc , Ch i c a g o , I L )
When comparing thc right lirnb of norrnal subjcctswith thc
statistical soflware was uscd to analyzc thc data. Statistical involved limb of thc PFPS group, thc norntal group scorcd
significanccwas sct at P < .05. Subjcct charactcristics(age, rnorc rcpctitions on thc stcp-down, lcg prcss, and bilatcral
hcight, and weight) werc compared betwecn thc groups using squat. Tcst scores bctwccn groups wcre statisticallydiffcrcnt
a 2-sarnplcI tcst.
for the stcp-down tcst (P < .013).
Reliability. We used thc intraclass corrclation cocfficicnt
(lCC) to cvaluatcintraratcrrcliability (lCC 3,I ). Standardcrror
of thc mcan (SEM) was calculatcd to dcscribc the prccision D I S C U S S I O N
of thc rncasurcmcnt.
Functional outcomc rncasurcsshould bc simplc to adrninCorrelation. Corrclation analyscs bctwccn the VAS and istcr, incxpcnsive, rcliablc, and valid. Most of thc functional
functional tcsts wcrc cvaluatcd using thc Pcarsoncorrelation tests prcviously reported in thc litcraturc are targetcd to pacocfficicnt.
ticnts after anterior cruciatc ligamcnt injury.22Thc purposcof
Limb Symmetry Index. Statistical diffcrcncc bctwccn in- our invcstigation was to dctcrmine the intraraterrcliability of
cliviclualsubjccts' lirnbs for thc unilatcral functional tcsts was 5 functional pcrfornrancc tcsts. In addition, thc rclationship
clctcrn-rincd
using a paircd I tcst. Bonfcrroni corrcction was bctween pain and functional tcst scoreswas asscsscd.
applicd to thcsc 4 tcsts, sctting thc alpha lcvel to .0514 :
Intraratcr rcliability nrcasurcs the consistency of a tcst's
0.013. The statisticaldillercnce between subjccts with PFPS scorc with respectto tin.rcancl thc evaluator.If a changc docs
and nomral subjectson functional tcst scorcs was detcrmined occur in the measure, onc can attribute the change to truc
with indcpcndent/ tests. Bonf-erronicorrection was applied to changc and not chance. In this study, intraraterreliability was
thc sc 4 tcsts, sctting t he alpha lev el t o . 0514: 0. 01 3 . L i m b
fair to high with a rangc frorn 0.79 to 0.94. The SEMs for all
syrnrnctry indcx was calculatcd with thc fomrula (involvcd/ testswerc lcss than one rcpetition, indicating high prccision.2l
uninvolved) x 100 fbr each group.
Pain is a common svmDtom of individuals with PFPS.
Table 3. Group Data*
NormalSubjects
Test
Anteromedial unge
Step down
S in g l e - l e gp r e s s
Bil a t e r a ls q u a t
Ba l a n c e a n d r e a c h
Rig h t L im b
M e a n ( SEM )
I 1. 60( 0. 54)
17. 80( 1. 02)
13. 80( 1. 25)
19, 6( 0. 91)
16. 4( 1. 46)
LeftLimb
M ean( SE M )
12. 2( 0. 7 0 )
17. 7 ( 1. 44 )
14.5(1.26)
NA
16.9(1.47)
P atel l ofemoralP ai n S ubi ects
LimbSymmetry
I n d e x( %)
l nvol ved Li mb
Mean (S E M)
Y3.Z
11.72(0.57)I
13e3 (1.02)t+
136e (0.87)t
NA
970
16.51 (1 .34)
17.93 (1.03)t
95.1
10 0 . 6
U ni nvol vedLi mb
Mean (S E M)
1 3 . 5 6( 0 , 4 8 )
1 7 . 3 1( 0 . 9 9 )
1 6 . 0 0( 0 . 8 4 )
NA
1 9 . 9 0( 1 . 0 4 )
Li mb S y mmel ry
Index (% )
8 5 .9
800
843
NA
8 9 .8
'SE M i n d i c a t e ss t a n da r d e r r o r o f th e m e a n ; NA, n o t a p p licabl e.
f S i g n i f i c a n td i f f e r e n ceb e twe e n lim b s a t P < .0 1 3 .
f S i g n i f i c a n t d i f f e r e n ceb e lwe e n g r o u p s a t P < .0 1 3 .
Journal of Athletic Traininq
259
Therefore, a functional test for this population should correlate
somewhat with a pain measure. All unilateral functional tests
correlated significantly with the VAS. This finding indicates
that these 4 functional tests were sensitiveto changesin pain
level. As pain level decreased,the number of rcpetitionsperfonned increased.The bilateral squat correlatcd the lcast with
the VAS and resulted in the lowest reliability. This rcsult is
probably due to the bilateral nature of the tcst. Bccause weight
distribution was not monitored, subjectscould shift weight to
the uninvolvcd limb to avoid overloading the involvcd side.
The 5 functionaltestswere tcstcd on subjectswith unilateral
PFPS and, therefore,we hypothcsizedthat there would be a
difference in performancebetwecn thc 2 limbs. For all tests,
thc uninvolvcd limb scored higher. Results from the paired t
tests reached significance for thc antcror.nediallunge (P <
. 013),step -do wn(P < . 013) , leg pr es s( P < 013) , and b a l a n c e
and re ach (P < .0 l3 ) .
Wc also cornparcdthe involved limbs of thc PFPS group
and thc right limbs of thc nomral group. Surprisingly,thc stcpdown was the only test that was significantlydifferent betwccn
the PFPS group and the normal group (P < .013). The normal
subjccts scorcd more repetitions on the step-down and lcg
press but not on the anteromediallungc or balanceand rcach.
Both thc anteromcdial lunge and balance-and-reachtcsts rcquirc sornework from both linrbs, and this may interfcrc with
a dif-fcrcntialscorc.
Sincc only thc stcp-down tcst was significantly different bctwccn groups, pcrhaps the LSI is a bcttcr indicator of PFPS
cliscrinrination.Thc LSI has bccn dcscribed in thc litcraturcas
a rcturn-to-sportcriterion. Barbcr ct alrl suggestedan LSI of
85'% as a satisfactory lcvel for dctcrmining norntalcy in thc
paticnt. For thc 5
antcrior cruciatc ligan'rcnt-reconstructcd
PFI'}Sfirnctionaltcsts,the LSI rangcd frorn 80.0'Zoin thc stcpdown to U9.tt% in thc balancc and reach. Thc nonr.ralgroup
avcragcd95% fbr thc unilatcral tcsts. Bccausc PFPS is so variablc ancl function dcpcnds on thc prcscncc of pain, a highcr
LSI of 93 to 95u/ofor cach functional tcst Inay bc a bcttcr
prcclictorof norrnalcy in this patient population.
Becausconly intraratcrrcliability was statisticallytested in
this study, thc rcsultscannot bc gencralizcdto othcr clinicians.
Furthcr work is undcrway to determincthc intcrratcrreliability
and scnsitivity of thcse 5 functional tcsts bctbre and aflcr rchabilitation.Clinically, wc have notcd that subjcctswith PFPS
irnprovc on all the functional tcst scorcsand incrcasctheir LSI
as thcy progrcssthrough rehabilitation.
C O NCLUSIONS
Thc purposc of our study was to investigatethe intrarater
rcliability of 5 functional performancetests.The intraraterreliability proved to be fair to high, with the highest reliability
occurring with thc step-down test and the lowest with thc bilateral squat. The unilatcral functional tests correlatedsignificantly with the visual analog scale and differentiatedbetween
the involved and uninvolved extren.rities.Howeveq the limb
symmetry index is probably a better discrirninatorof patcllof'en.roralpain syndrornethan the absolute number of repctitions
obtained on cach test. The key to the reliability of thc tests is
that the clinician follow standardprotocol. Further reliability
testing among clinicians needs to be investigated.
The functional tests are designedto be uscd independently
or together. Each test has a particular, unique contribution to
the total functional picture. For patients who are unable to
260
2002
Volume37 . Number3 . September
tolerate a single-leg squat, the single-legpress can bc used to
assessquadriceps function. As patients progress, the following
3 tests can be used: (l) the step-down requires balance and
eccentriccontrol of the quadriceps,(2) the anteromediallungc
requires a greater range of knee flexion, and (3) the balance
and rcach requires single-leg balance,lirnb stability, and proprioception. Before discharge, a patient with patellofemoral
dysfunctionshould be able to complete the unilateraltestswith
the involved limb and score within l0o/o of the uninvolved
limb.
ACKNOWLEDGMENTS
This study was funded by thc American PhysicalTherapyAssociationSportsPhysicalTherapyScction'sSmallGrantProgram.
REFERENCES
l. MarianiPP,Caruso
I. An electronryographic
investigzrtion
ofsubluxation
ofthc patel l a.J l l ona.Joi ntS urgB r. 1979;61:169l 7l .
l C , Worrel lTW. A ntcri orkneepai nsyndromc:
rol eof t hc v as tus
2. Wcstl al D
mcdi afi sobl i que.J S portl l chubi l . 1992:'l :311325.
syndrome.In:
3. Ficat RP Latcral lascia releascand latcral hypcrpressure
Pickett JC, Radin IlL, ctls. Chondronutlut'iaol tha Putellu. Baltimore,
MD : Wrl l i ams& Wi l ki nsl l 98l :95 l l 2.
4. Grcenfi cl dMA , S cottWN . A rthroscopi cval
c
uati onand trcatmc ntol ' thc
patcllolcnroraljoint. Orthop CIin North lm. 1992,23:587600.
patcl l ai n the adol escent.
In: K c nnc dy
5. JamesS L. fl hondrorral aciof'thc
a
JC, cd. Thc IniuraclrldolasccntKncc. Baltimore,MD: Williams & Wilki nsl 1979:205251.
6. KannusP, Nittymaki S. Which firckrrspredictoutcornein thc nonopcrativc treatmcntol'patellol'cmoralpain syndrorne'lA prospcctivclirllow-up
study. Mad Sci Sports Excrc. 11994:'26:289
296.
l acxi st'/In: P i ckel tJC , R adi nt]L,
7. R adi n[rL. D oeschondrornal acipatcl
a
gJs.Chondrontuluciu
o/ tha Putallu.IJtrltintotc,MD: Williarns& Wilkins;
1983:6882.
8. P ostMD , Ful kcl sonMD . K nce pai n di agrams:conel ati onw i th phy s i c al
cxaminationfindings in patientswith arrlcriorkncc pain. Arlhnt.scttp.v.
1994:l 0:618 623.
pai n syndrorncs:
9. Mal ck MM, Mangi ncl l l i . P atcl l ofcrnoral
a comprc l rc nsivc and conservativeapproach..l Orlhop Sport.sPh.vslhcr. l98l;2:108
I 16.
nt of l l ncti onal tcstsafl cr antc ri or
10. I{i sbcrgMA , U kel andA . A sscssme
217.
cruciatcligamcntsurgery.,l Orthr4tSport"-Phys Thar. 1994:'19:'212
l l . B arberS D , N oycs FR , Mrngi nc R l l , McC l oskcyJW, H artmanW . Quantitativc asscssmcnt
of lirnctionallrmitationin nonnal zrndantcriorcruciatc
214.
ligarrcnt-dcficicntknees.C/in Orrhop. 1990;255.2.01
12. B ol gl a LA , K eskul aD Il .. ttcl i abi l i tyof l ow er extremi tyf uncti onalpc rlrrnrance tests.J Orthop Sports PhysI-hcr. t991,26:138 142.
13. C hesw orthtsM, C ul ham E G, Tata GE , P cat M. V al i dati onof oul c onre
rneasLrres
in patientswith patellofernoralsyndnrnre.
,l Oilfu4t SportsPhvs
Il cr 1989:10:302
308.
mus c l e
14. R ei l l y D T, MartensM. E xpcri mcntalanal ysi sof the quadri c c ps
joint reactionforce lbr variousactivities.,'lcla
force and patellol-emoral
Orthop Scund. 1972 43:126 131.
15. Gray GW. Lower ExtremityFunttional Pro/tla. Adrian,MI: Wynn Marketi ngInc; 1995.
l ae.C un A thl 7'hcrA ,ssrsc./.
l 9 [t2;8:13
16. R ei d D C . C hondromal acipatel
a
20.
als orders :
17. Wi l k K E , D avi esGJ, Mangi neR E , Mal oneTR . P atel l ofemordi
lisystemand cl i nrcalgui del i nesfor nonoperati vrehabi
e
a cl assi fi cati on
tation. -/ Orthop Sports Phys Thcr. 1998,28:307 322.
l ae:r pros pec ti v e
a
18. Insal l J, Fal vo K A , Wi se D W C hondromal acipatel
study..l B one.l oi rttS urg,4rr. 1976;58:l 8.
l ae:
a surveyconduc ted
19. R obi nsonA R , D arracottJ. C hondromal acipatel
a
at the Anny Medical RehabilitatronUnit, Chester.lnn Phys Mad. 19101'
I 0:286-290.
B . The val i dati onof v i s ual
20. P ri ceD D , McGrathP A , R afi i A , B ucki ngharn
analoguescalesas ratio scalemeasuresfor chronicand experimental
pain.
Pain. 1983:l'7:45-56.
21 . M e l z a c kR . P a i n :an o ve r vie w.Acta An a e sth e sioSca
l n d .1999:43;880884.
22. LephartSM, PerrinDH, Fu FH, Minger K. Functionalperfonnancetests
for the anteriorcruciateligamentinsuflicicnt athlete.Athl Train J Natl
A r h l h n i n A s s o c .19 9 l:2 6 :4 45 0 .
23. PorrneyLG, WatkinsMP.FoundatknsoJ Clinital Resaurch.-Applicattuns
lo Pre('ticc.Norwalk, CT: Appleton and Lange; 1993,
APPENDIX
Instructionfor FunctionalPerformanceTests
l. Anteromedial lunge: "You will stand behind a staft line
and pcrform 3 lunges with the uninvolvcd lirnb. The maxir.nunrdistanceachievcd will be used to calculatethe 80%
targct distance.Thc targct distancewill bc marked on thc
floor with tape and recorded on the data form. Then, you
will stand with your feet straddling thc rniddle line. Your
toes must stay behind the central linc. Thcn, you will step
out with your - leg so that your hccl passesthe rnarked
distancc (tester will demonstrate).You will continue thc
lunges for 30 scconds.Do you havc any questions'/"
Criteria: Only lunges in which thc subjcct'shecl touchcs
bcyond thc 80% lnark will bc rccorded.
2. Step-down: "You will stand on this S-inch stcp with both
lcgs. Whcn I say go, you will lower your - lcg so that
your hccl touches thc ground. You will thcn rcturn this
lcg to the platforrn and touch the top of thc platform. You
will continuc this scqucncc until I say stop. Thc test is
run for 30 scconds. Do not push off thc ground as you
lowcr your hccl. Do you havc any qucstions?"
Criteria: Hccl must make contact with a slight hcsitation
both at the down phase and the start phase. Do not allow
the subjects to vault up with their touch leg.
3. Single-leg press: "You will start with your back against
the sled and your knees fully extended. Place your feet
hip-width apaft on the standing platform. When I say go,
you will bend your - knee and lower your body on the
sled to approximately 90o of knee flexion. I will tell you
when you achieved the appropriateknce bend. You will
continue performing the knee bends for 30 seconds.Do
you have any questions?"
Criteria: Foot must remain flat on the Total Gym platfomr, no vaulting. Full 90" must be achieved(slcd must
touch platforrn).
Bilateral squat: "You will stand with your f'ccthip-width
apart and squat down so that your knees bend to 90" like
this (tester dcmonstratcs).Your scat will touch this chair.
Do not rest on the chair. You will rcturn to the start position and repeatthis activity for 30 seconds.Do you havc
any questions?"
Criteria: Buttock must touch scat.Subjectrnustrcach full
s t a n d i n gw i t h f u l l k n c c c x t c n s i o n .
B a l a n c e a n d r e a c h : " Y o u w i l l s t a n d b e h i n d a sta r t l i n c
and pcrform 3 lungcs with thc uninvolved lirnb. The maximum distanccachieved will be used to calculatcthe tl0,%
targct distancc.Thc target distancewill be markcd on thc
floor with tapc and rccorded on thc data form. Stand with
your feet straddling thc middle linc. Your tocs must stay
bchind thc central linc. You will stcp out with your _ lcg
so that your hecl passesthe markcd distancc(tcstcr will
dcmonstrate).Do not rest your foot down whcn you reach
the targct distance.You will continuc thc reachestbr 30
scconds.Do you havc any qucstions?"
Criteria: Only rcachcsin which thc subjcct'shccl touchcs
beyond the 80% mark will bc rccordcd.
Journal of A thl eti cTrai ni nq
261