Randomized Clinical Trial of Balance-Based
advertisement

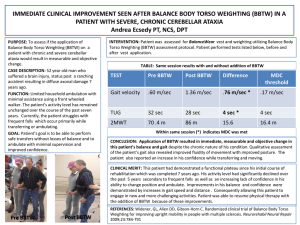
Randomized Clinical Trial of Balance-Based Torso Weighting for Improving Upright Mobility in People with Multiple Sclerosis Neurorehabilitation and Neural Repair Volume 23 Number 8 October 2009 784-791 © 2009 The Author(s) 10.1177/1545968309336146 http://nnr.sagepub.com Gail L. Widener, PhD, PT, Diane D. Allen, PhD, PT, and Cynthia Gibson-Horn, PT Background. Torso weighting has sometimes been effective for improving upright mobility in people with multiple sclerosis, but parameters for weighting have been inconsistent. Objective. To determine whether balance-based torso weighting (BBTW) has immediate effects on upright mobility in people with multiple sclerosis. Methods. This was a 2-phase randomized clinical trial. In phase 1, 36 participants were randomly assigned to experimental and control groups. In phase 2, the control group was subsequently randomized into 2 groups with alternate weight-placement. Tests of upright mobility included: timed up and go (TUG), sharpened Romberg, 360-degree turns, 25-foot walk, and computerized platform posturography. Participants were tested at baseline and again with weights placed according to group membership. In both phases, a physical therapist assessed balance for the BBTW group and then placed weights to decrease balance loss. In phase 1, the control group had no weights placed. In phase 2, the alternate treatment group received standard weight placement of 1.5% body weight. Results. People with BBTW showed a significant improvement in the 25-foot walk (P = .01) over those with no weight, and the TUG (P = .01) over those with standard weight placement. BBTW participants received an average of 0.5 kg, less than 1.5% of any participant’s body weight. Conclusion. BBTW can have immediate advantages over a nonweighted condition for gait velocity and over a standardized weighted condition for a functional activity in people with multiple sclerosis (MS) who are ambulatory but have balance and mobility abnormalities. Keywords: Multiple sclerosis; Physical therapy; Balance; Movement outcomes I n a recent sample of 354 middle-aged and older adults with multiple sclerosis (MS), 93.7% indicated that they had problems with balance and mobility.1 Balance or postural control requires sensory input (somatosensory, visual, and vestibular), central integration of sensory information, and selection and execution of timely motor responses to control head and body positions for mobility against gravity. Demyelination of various central nervous system connections in people with MS can affect any of these components of postural control. Cerebellar ataxia, alone, is a significant cause of balance and gait problems and is present in up to one third of people with MS.2 Weakness, fatigue, tremors, and spasticity, among other factors, were significantly different between 569 fallers and 520 nonfallers in a sample of people with MS. The fallers reported at least 1 fall in the prior 6 months.3 Physical therapy frequently has a role in helping people compensate for MS-related impairments and losses in postural control that result in decreased mobility.4-8 In previous studies and in clinical practice we have seen improved mobility and postural control with the strategic placement of small amounts of weight on the torso of people with MS.9,10 The strategy for this weight placement is called balance-based torso weighting (BBTW). With BBTW, a clinician places the weights to decrease any balance deviations observed while a patient stands quietly, reacts to perturbations at the trunk, walks, and performs transitional movements like sit to stand. With the weights appropriately placed, patients seem to have an easier time resisting perturbations and remaining vertical during gait. In a case report,9 results showed that strategic application of 0.9 kg (2% of the participant’s body weight) via the BBTW method resulted in increased gait speed, decreased ataxic movement of the trunk, and less difficulty turning. A preliminary study of 16 ambulatory participants with MS showed differences between baseline and BBTW conditions in one or more of the measures of balance and function.10 The purpose of the current study was to test whether the BBTW system of weight placement affected function when participants were randomized to groups, and whether a standardized weight placement worked just as well. Other clinicians have occasionally applied weights to patients’ trunk, limbs, or assistive devices to help control disordered movement,11-13 but few other researchers have described the methodical use of weights and their effect on mobility. Hewer et al14 described the use of 0.2 to 2.0 kg of weight to control upper extremity intention tremor in people with cerebellar disease. Morgan15 noted that light weights (1 kg) placed on the lower extremities and (1-2 kg) at the waist improved gait coordination in people with ataxia (some with From the Department of Physical Therapy, Samuel Merritt University, Oakland, California (GLW, CGH), and the Graduate Program in Physical Therapy, UCSF/SFSU, San Francisco, California (DDA). Address correspondence to Diane D. Allen, PhD, PT, 2955 Ramona Street, Palo Alto, CA 94306. E-mail: allendianed@gmail.com. 784 Downloaded from nnr.sagepub.com at UNIV OF DELAWARE LIB on January 8, 2015 Widener et al / Balance-Based Torso Weighting in People with Multiple Sclerosis 785 MS) while larger weights increased ataxic movements. Gillen16 added weight as a stabilizing force for an individual with ataxia from MS to improve upper extremity function. Clopton et al17 placed 10% of participants’ body weight at the shoulders or waists to investigate effects on ataxic gait. The BBTW method incorporates only the amount of weight required to improve responses of the patients, often less than 2% of body weight, which is quite different from the protocols described. The mechanism behind the therapeutic effects of weighting is unknown. Some have justified it as a means of joint compression to facilitate muscle cocontraction and increased stability.12,13,17,18 Others see weight placement as a means for changing the location of the center of mass and thus the moment of inertia for a body segment, thereby changing the biomechanics of a movement.13,15 Patients with ataxia have difficulty controlling body movements. The weighting may increase control by increasing the afferent input available regarding changes in biomechanical relationships between body segments. However, the increase in afferent input may have more than a biomechanical effect. It may also be a means of improving awareness of the weighted body segment so that the person can concentrate on controlling it.19 Each of these proposed mechanisms for the benefit of weighting in helping to control movement implies that added weights must be substantial and sufficient to compress joints, change the perception of the moment of inertia, increase afferent input, or increase awareness of a body segment. On the other hand, too much weight seems to result in loss of control for people with strength or endurance losses.15 The dramatic effects of the very small amount of weight placement in the BBTW method, described by Gibson-Horn9 imply that even subtle changes may be enough to improve performance. It may be that axial weighting affects an individual’s perception of body position. Studies have shown that humans can perceive a change in trunk rotation as small as 0.9 degrees20 and lateral flexion of less than 3 degrees.21 Some individuals may be able to adjust their control of upright positioning based on a new concept of self in space. However, participants with BBTW have said that they forget they have the weights on so increased awareness of body parts is unlikely as the mechanism for the effectiveness of weighting.10 The BBTW methods used in this study, if effective, will support theories of improved mobility based on subtle changes in sensory input or perception but not the concept that joint compression or awareness plays a role in the effectiveness of weighting. The specific location of weights seems to change the direction of balance loss, which implies that strategic placement of weights may optimize the effect on mobility. Lucy and Hayes18 reported a specific improvement in lateral postural sway with standardized placement of 1.36 kg on each shoulder of participants with ataxia from various diagnoses including MS. Anterior-posterior sway remained unchanged in the majority of their participants. It would have been interesting to see if anterior-posterior weight placement had an opposite effect, or if people with particular problems with increased sway in one direction could show greater change if weight placement focused on the direction of postural instability. Clopton et al17 reported that 2 of their 5 participants showed gait improvement when weights were placed at the shoulders, and 2 showed improvement when weights were placed at the waist. One participant improved with either location of weight placement. Again, a protocol like BBTW that specifically adjusts weight placement higher or lower according to patient need may have a more consistent effect on upright mobility. This 2-phase randomized clinical trial was designed to test the BBTW method in people with MS and upright mobility problems. Our aims were to examine the immediate effects of BBTW on postural control and upright mobility compared with an unweighted control group and to compare the effect of BBTW on postural control and upright mobility with the effect of standard weight placement of 1.5% body weight divided in 2 and equally distributed laterally at the waist. The null hypotheses were that no postural control or upright mobility measures would show a difference with weighting, and that no differences in postural control or upright mobility would be noted between people with weight placed according to the BBTW method compared to those with no weight or to those with standard weight placement (SWP). Our alternative hypothesis was that BBTW would prove beneficial over the unweighted condition and that it would differ from the SWP condition in improving performance on the dependent variables. Methods Participants were recruited through newsletter ads sent by a chapter of the National Multiple Sclerosis Society. The following inclusion criteria for acceptance into this study were: (1) able to walk 30 feet, (2) difficulty with walking, and (3) afraid of falling. Exclusion criteria were as follows: (1) unwilling to have balance challenged by a researcher, and (2) timed up and go (TUG)22 results of less than 8 seconds. The cut-off for the TUG was chosen to exclude people who had minor difficulty with walking and thus limit a possible ceiling effect. Figure 1 depicts the group assignment process. Randomization was stratified based on performance on the TUG. People who performed the TUG in 8 to 12 seconds were considered high functioning and people who performed the TUG in more than 12 seconds were considered low functioning. Once identified as high or low functioning, participants drew an opaque envelope from the high or low functioning pool of envelopes containing the information regarding group assignment. The content of envelopes was revealed to neither the participants nor the tester. All participants signed informed consent as directed by the Institutional Review Board of Samuel Merritt University. All participants answered demographic questions regarding type of MS, time since diagnosis, number of falls in the past 6 months, and experience with MS-related fatigue. A fall was defined as losing balance and unexpectedly landing on the floor. All participants were also measured for strength,23 range of motion (ROM), and muscle tone24 for flexion and extension at the knees and Downloaded from nnr.sagepub.com at UNIV OF DELAWARE LIB on January 8, 2015 786 Neurorehabilitation and Neural Repair Figure 1 Research Design With Sequence for Participant Recruitment and Assignment 100 Contacted us 56 Ineligible or Could not commit 44 Enrolled 3 No shows 3 TUG scores < 8 sec. 38 Subjects Phase I Randomized 1 had unrelated emotional breakdown 19 Control Phase II 1 TUG score < 8 sec. at BL3 1 unable to follow directions 19 BBTW Randomized 10 SWP 8 BBTW 2 TUG scores < 8 sec. at BL3 Abbreviations: TUG, timed up and go; BBTW, balance-based torso weighting; SWP, standardized weight placement; BL3, score at baseline for phase 2. dorsiflexion and plantarflexion at the ankles to ascertain group equivalency in these basic measures. The dependent variables included the following: the TUG22; the sharpened Romberg25 with time summed across 4 trials in which participants held the position for a maximum of 30 seconds each with right foot then left foot behind, eyes open (SREO) and eyes closed (SREC); the timed 360-degree turn summed across turns to the left and to the right; the 25-foot walk; and average body sway (in centimeters per second) during 10 seconds of standing with eyes open and then eyes closed for computerized platform posturography (CPP). The TUG, sharpened Romberg, 25-foot walk, and CPP were chosen because they were variables used in preliminary testing of the BBTW in people with MS.10 The 360-degree turn was chosen because turning had shown change in a case report with BBTW methods.9 The turn was performed as directed for the turning item in the Berg Balance Scale (BBS),26 but scored in the seconds it took to complete a turn, once to the left and once to the right. All data were collected in the same laboratory space. CPP was performed using a Basic Balance Master (NeuroCom International, Clackamas, OR). The researcher (GLW) administering all tests was blinded to test condition. Body weighting for the BBTW condition followed the procedure established by Gibson-Horn.9 Assessment of balance included observation of relative amount and direction of sway during Romberg testing with eyes open and eyes closed. One researcher (CGH) perturbed (and guarded) the participant with anterior, posterior, and lateral nudges to the shoulders and pelvis to identify response latency, amount, and direction of balance loss. Balance loss was defined as tilt or lean of the trunk requiring opposing parachute reaction, stepping response, or manual contact by the researcher to regain center of mass over the base of support. The researcher applied rotational force through the shoulders and or pelvis to determine asymmetry in resistance. Small weights were applied to the torso on a specially constructed vest-like garment that allowed Velcro application of weights to front, back, or sides of the torso between the shoulders and waist. The first application of weights was in a direction to counter the direction of balance loss and asymmetry of resistance. Balance was reassessed with the weights in place to determine if greater stability or decreased response latency was demonstrated. Weights were adjusted until stability improved with reassessment. The balance assessment took between 10 and 30 minutes (usually less than 20 minutes) depending on the number of balance-related errors found. The garment was removed for rest periods, and redonned for BBTW testing on the dependent variables. Body weighting for the standard weight placement was predetermined at 1.5% of the participant’s body weight and placed at the bottom of the vest, laterally, with half of the Downloaded from nnr.sagepub.com at UNIV OF DELAWARE LIB on January 8, 2015 Widener et al / Balance-Based Torso Weighting in People with Multiple Sclerosis 787 weight on either side of the waist. The garment was removed for rest periods, and redonned for SWP testing on the dependent variables. Procedure For phase 1, both groups were tested for a baseline (BL1) on all dependent variables. The experimental group had a 15-minute rest and then underwent the BBTW assessment to determine weight placement on the garment. After another 30-minute rest (in case the BBTW procedure was fatiguing), the experimental group was retested on all dependent variables. The control group also had a 30-minute rest between the baseline (BL1) and second testing (BL2). Because some people having BBTW may have carry-over effects, phase 2 only examined participants from the first control group. For phase 2, participants from the control group from phase 1 returned on another day and were tested on the dependent variables for another baseline (BL3). Phase 2 participants were then randomly assigned to 1 of 2 alternate condition groups. Only participants in the BBTW group received balance assessment. After 30 minutes of rest, one group received BBTW, and the other group received SWP. Participants were then tested again on all dependent variables. Blinding of the tester in both phases for test condition on all dependent variables was accomplished by having participants don an oversized black t-shirt to hide the presence or absence of the BBTW or SWP garment. Participants in phase 2 were unaware of the test condition, whether BBTW or SWP. Data analyses were performed with SPSS version 15.0 (SPSS Inc, Chicago, IL). Analyses to determine the significance of the differences between groups at baseline (with α = 0.05) included the following: 1. t tests for differences in mean age or years with the diagnosis of MS; 2. the Mann-Whitney U test for differences in the median Expanded Disability Status Scale27 (EDSS) score; and 3. χ2 tests for differences in frequency of people claiming falls or fatigue, or between numbers of females, numbers of people with different types of MS, numbers of people designated as high functioning, and numbers of people with strength, range of motion, and tone impairments. The data from the dependent variables were expected to have an abnormal distribution because of the sample size and expected movement dysfunction, so data analyses were performed with nonparametric statistics. The Wilcoxon signed ranks test was used to test the paired differences between baseline and second testing for each group in each phase. The Mann-Whitney U test was used to test differences in the average change in performance between groups in each phase. The family-wise α was set at 0.10 for each group of tests. Bonferroni’s correction thus resulted in α = 0.02 for each of the dependent variables in each group. The alpha was set liberally because advocating a potentially ineffective but low risk treatment (a type 1 error) is less of a problem to the clinical community than missing a potentially useful treatment when few treatments have documented effectiveness in this population. All paired differences and the group differences between the BBTW and control groups in phase 1 were assessed using 1-tailed tests because the intervention was expected to make a positive change in these dependent variables. For phase 2, group differences were assessed using 2-tailed tests because BBTW and SWP were alternative interventions and the direction of the difference was not proposed. Results Groups were similar with respect to age, years with the diagnosis of MS, EDSS scores, number of participants claiming one or more falls in the past 6 months, number claiming MS-related fatigue, and gender (Table 1). Chi-square tests revealed no significant difference (P > .05) between groups in numbers of participants with the different types of MS (secondary progressive, primary progressive, or relapsing-remitting), impairment of knee extension or ankle dorsiflexion ROM, or at least mild hypertonicity in one of the knee or ankle directions of movement (Table 2). The number of people designated as high functioning tended to be higher in the experimental group than in the control group in phase 1 (P < .06), but the number of people who had less than 4 on a manual muscle test of any knee or ankle muscle group also tended to be higher in the experimental group (P = .05). The average weight applied for the BBTW condition was 0.5 kg. The average weight applied for the SWP condition was 1 kg. Test-retest reliability estimates were calculated from the control group data from BL1 to BL2 (both performed on the same day). The TUG and 25-foot walk were single scores, so the intraclass correlation coefficients (ICCs) were performed as model 3, type 1. The ICCs were 0.98 and 0.96 for the TUG and the 25-foot walk, respectively. The other variables were combined scores across trials (eg, right, left, eyes open or closed), so the ICCs were performed as model 3, type k. The sharpened Romberg ICC was 0.73, the 360-degree turn was 0.96, and the CPP was 0.80. There were no statistically significant differences between day 1 and day 2 in mean baseline performances. ICCs ranged from 0.86 to 0.97 for the 5 variables when comparing BL2 and BL3. In phase 1 (Table 3), participants with the BBTW showed significant improvement over baseline in the TUG (P < .001), 25-foot walk (P < .001), sharpened Romberg (p < .02), and the 360-degree turns (P < .004). Participants in the control group showed no significant difference between BL1 and BL2 on any variable. The 25-foot walk revealed a statistical difference in change scores between the experimental and control groups (P = .01) with an average 8.5% improvement for the BBTW group versus no improvement for the control group (Figure 2). In phase 2, examination of baseline scores (BL3) revealed 3 additional participants who had TUG test scores of less than Downloaded from nnr.sagepub.com at UNIV OF DELAWARE LIB on January 8, 2015 788 Neurorehabilitation and Neural Repair Table 1 Participant Characteristics for Randomly Assigned Groups Phase 1 Control (n = 18) Age in years, mean (SD) Years with diagnosis, mean (SD) EDSS, median (range) Number (%) claiming falls in past 6 months Number (%) claiming MS-related fatigue Number (%) female Phase 2 BBTW (n = 18) P Value SWP (n = 9) BBTW (n = 6) P Value 55.7 (7.5) 13.2 (10.1) 4.5 (2-5) 14 (77.8) 16 (88.9) 16 (88.9) .40 .96 .41 .66 .23 .23 53.2 (10.9) 12.0 (7.5) 4.5 (2-5) 6 (60) 6 (60) 7 (70) 53.3 (8.8) 15.0 (16.0) 5.0 (3-5) 8 (100) 6 (75) 5 (62.5) .99 .61 .41 .09 .64 1.00 53.2 (9.7) 13.3 (11.7) 5.0 (2-5) 16 (88.9) 12 (66.7) 12 (66.7) Abbreviations: BBTW, balance-based torso weighting; SWP, standardized weight placement; EDSS, expanded disability status scale. Table 2 Number with Type of Multiple Sclerosis or Specified Impairments for Randomly Assigned Groups Phase 1 Phase 2 Control BBTW (n = 18) (n = 18) SWP BBTW (n = 9) (n = 6) Secondary progressive MS Primary progressive MS Relapsing remitting MS Unknown type of MS Number high functioning: 8-12 seconds on TUG Number with <4/5 strength for any knee flexion or extension or ankle dorsiflexion muscle group Number with knee extension less than full range Number with ankle dorsiflexion less than neutral Number with at least mild hypertonicity at knee or ankle 2 2 10 4 9 4 4 10 0 13 1 1 5 3 3 1 1 5 1 3 10 13 4 5 8 8 5 2 7 8 4 3 17 17 9 5 Abbreviations: MS, multiple sclerosis; BBTW, balance-based torso weighting; SWP, standardized weight placement; TUG, timed up and go. 8 seconds. Elimination of these participants in our analyses (consistent with initial exclusion criteria) resulted in 9 participants in the SWP group and 6 participants in the BBTW group. Participants with BBTW improved over BL3 in the TUG (P = .01). Participants with SWP improved over BL3 in the 25-foot walk (P = .004). The TUG test revealed a statistical difference in change scores between the 2 groups (P = .01) with an average 9% improvement for the BBTW group versus 1.5% improvement for the SWP group (Figure 3). Discussion The null hypotheses could be rejected. The BBTW groups showed changes in the weighted conditions and showed greater change than the unweighted control and SWP groups in a measure of mobility. The lack of difference between groups across more variables in phase 1 may reflect the relatively high standard deviation in the performance of unweighted control participants at baseline and second testing in the TUG, turns, and CPP (see Table 3); however, the mean across these control participants showed no significant improvement with second testing on any variable. When these same control participants were provided with alternative weight placements in phase 2, the improvement in mobility variables by both the SWP and BBTW groups indicate that weighting can be effective even when not placed in a patient-specific manner. The SWP group did not show better change in performance, however, on any variable compared to the BBTW group. The advantage for the BBTW group may have been both the patient-specific location of the weight and the relatively smaller amount of weight perhaps resulting in less fatigue, a common problem for people with MS. In this study, sharpened Romberg performance proved to be highly variable, with a test-retest ICC of 0.73 in our control group. In reliability testing of participants with MS who were unable to hold a single-leg stance, Fry and Pfalzer28 found that tandem stance had an ICC of 0.63, with a confidence interval that crossed zero, indicating even higher variability in this test. In contrast, Frzovic et al29 reported Spearman rho values of 0.86 and 0.93 for same day test-retest reliability of right and left legged tandem stance respectively in people with MS. Compounding the high variability on this test, many participants in our study could not perform the sharpened Romberg with eyes closed. The sharpened Romberg was included because it showed change with the BBTW in a previous study, but the previous sample included people with TUG scores below 8 seconds and thus higher functioning.10 Future testing of ambulatory people with MS and lower function might eliminate the sharpened Romberg testing, at least in the eyes closed condition and possibly also in the eyes open condition. In contrast, the average CPP tests showed minimal response to weighted conditions in this study. One reason for this lack might be that the average CPP for the experimental group in phase 1 was 0.5 cm/second, which is the cut-off designated by the manufacturer for “normal sway.” The other groups also had averages close to this number. The lack of change might be evidence of a ceiling effect. Downloaded from nnr.sagepub.com at UNIV OF DELAWARE LIB on January 8, 2015 Widener et al / Balance-Based Torso Weighting in People with Multiple Sclerosis 789 Table 3 Mean (Standard Deviation) Value on Dependent Variables for Control and Experimental Groups in Phase 1 and Standard Weight Placement and Balance-Based Torso Weighting Groups in Phase 2 Phase 1 Control (n = 18) TUG (seconds) 25-foot walk (seconds) Sharpened Romberg (seconds held) 360-degree turn (seconds) CPP (cm/second) Phase 2 Experimental (n = 18) SWP (n = 9) BBTW (n = 6) BL1 BL2 BL1 BBTW1 BL3 SWP 12.4 (3.6) 7.4 (2.2) 14.4 (21.2) 10.1 (4.3) 0.8 (0.4) 12.1 (3.6) 7.4 (2.2) 13.8 (18.8) 9.5 (4.1) 0.7 (0.3) 11.0 (2.7) 7.0 (2.0) 26.7 (26.6) 7.8 (2.8) 0.5 (0.2) 10.4a (2.4) 6.4a,b (1.6) 33.2a (28.0) 6.8a (2.4) 0.5 (0.2) 13.0 (3.8) 7.8 (1.8) 15.7 (26.2) 9.5 (4.0) 0.7 (0.3) 12.8 (4.0) 7.2a (1.8) 16.6 (26.8) 9.2 (4.4) 0.6 (0.2) BL3 13.6 (3.4) 7.9 (2.3) 17.6 (26.3) 11.4 (5.4) 0.8 (0.3) BBTW2 12.4a,b (3.0) 7.7 (2.0) 18.4 (21.3) 10.6 (5.7) 0.8 (0.4) Abbreviations: BL1, baseline of Phase 1; BL2, second testing of control group in Phase 1; BL3, baseline of Phase 2; BBTW1, experimental group with balancebased torso weighting applied, Phase 1; BBTW2, group with balance-based torso weighting applied, Phase 2; SWP, group with standard weight placement applied, Phase 2; TUG, timed up and go; CPP, computerized platform posturography. a Testing in weighted condition showed a significant improvement over baseline. b Testing in BBTW condition showed significantly different improvement over alternative condition in that phase of testing. Figure 2 Phase 1, the 25-Foot Walk: Results of 18 Control Participants (Designated 1-18) at Baseline (BL1) and Time 2 (BL2), and 18 Experimental Participants (Designated 19-36) at Baseline and With the BBTW Revealed a Statistical Difference in Change Scores Between the Groups (P < .01) 14 12 Seconds 10 8 6 4 2 0 1 4 7 10 13 16 19 22 25 28 31 34 Subjects BL1 BL2 BBTW Abbreviation: BBTW, balance-based torso weighting. The 25-foot walk is one of the standard timed walk tests used in research for people with MS. The results of our study suggest that weighting may have a positive effect on gait velocity. We observed an 8.5% improvement in the experimental group. The TUG test, while not a standard MS test, is used by many rehabilitation specialists because it contains sit to stand transfers, gait, and turns, many of the daily activities a person with MS might encounter. We found a significant difference between the alternate weighting groups in this functional variable, with a 9% improvement for the BBTW group. Downloaded from nnr.sagepub.com at UNIV OF DELAWARE LIB on January 8, 2015 790 Neurorehabilitation and Neural Repair Figure 3 Phase 2, TUG: Results of 9 Control Participants (Designated 1-9) at Baseline (BL3) and With SWP and 6 Experimental Participants (Designated 10-15) at Baseline and With BBTW Revealed a Statistical Difference in Change Scores Between the Groups in Favor of BBTW (P = .01) 25 20 Seconds 15 10 5 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Subjects BL3 SWP BBTW Abbreviations: TUG, timed up and go; SWP, standardized weight placement; BBTW, balance-based torso weighting. The improvements in upright mobility scores, as an immediate effect of BBTW, compare favorably with improvements noted in other reports of balance interventions in MS. For example, Wiles et al6 reported an 8% improvement in walking speed after 2 sessions of physiotherapy a week for 8 weeks. It would be interesting to see if use of weighting along with active intervention would increase this effect in a shorter time. Few studies have used other sensory input as a method of modifying postural control and function in people with MS. Schulfried et al30 compared a single bout of whole body vibration (WBV) with a placebo of transcutaneous electrical nerve stimulation (TENS) in people with MS and walking difficulties. They found no significant differences between groups immediately after WBV in functional reach, TUG, or sensory organization testing. The 0.6 second improvement in TUG scores for the 6 people in the WBV group, although it did not reach statistical significance, compares with the 0.6 second improvement in TUG scores with BBTW in phase 1 of the current study but is less than the 0.9 second improvement in phase 2. Neither study included other rehabilitation techniques along with the sensory input. This study design controlled for some learning effects possible with repeated testing, a possible source of improvement. Participants in the phase 1 control group performed the activities required by the dependent variables at baseline and second testing, and again for a second day baseline and intervention testing with weight placement according to group designation. No significant differences were noted in any variables between the baseline and second testing in phase 1, or between baseline for phase 1 and baseline for phase 2. Learning did not have a significant effect on performance over the 4 repetitions of testing in this study. Limitations This was a relatively small pilot study in a sample of participants with MS and acknowledged balance deficits. The results cannot be generalized to the function of all people with MS. On the other hand, it is possible that people with balance and mobility abnormalities resulting from pathologies other than MS may also benefit from this technique. Only one of the variables in each phase of the study showed a significant difference between groups. The significant improvements between BL1 and BBTW in phase 1 and trends in some variables across groups also seemed to favor BBTW, however. Further research might investigate the characteristics of people with MS or other pathologies who benefit most from weighting with the BBTW system when Downloaded from nnr.sagepub.com at UNIV OF DELAWARE LIB on January 8, 2015 Widener et al / Balance-Based Torso Weighting in People with Multiple Sclerosis 791 assessed across a more focused set of variables. Future studies will need to assess the repeatability of the balance assessment for weight placement; this was not needed in this study since only 1 person performed all balance assessments. Only immediate effects were examined in this study. Longterm effects of weighting or any carry-over after weighting is removed were not evaluated. Further research might investigate carry-over effects, or determine whether weighting is an orthosis that improves function only while applied or an intervention that changes function because people can practice or exercise differently during the application period. Such differentiation could enhance our understanding of the mechanism behind any changes in mobility noted with weighting. Assessment for BBTW could take up to 30 minutes and seemed to be fatiguing for participants, possibly affecting performance even after a 30-minute total rest time. In addition, the activities and perturbation required during balance assessment could have had positive effects. Future research might need to incorporate the balance assessment portion of the protocol for all groups, whether or not participants are assigned to get weight application. Although group assignment was randomized and no differences were noted in EDSS scores, strength, ROM, or tone between control and BBTW groups at baseline, the BBTW group in phase 1 may have had higher functioning. A total of 13 out of 18 participants in the BBTW group performed the TUG in less than 12 seconds, compared to 9 out of 18 in the control group, meaning that perhaps an over-all ceiling effect limited the ability of participants in the BBTW group to show change compared to the control group. Conclusion Weighting the torso can produce an immediate change in upright mobility, with some advantage noted by participants who had torso weighting applied with the BBTW system. People with MS who are ambulatory but have balance or mobility abnormalities may benefit from this intervention. Acknowledgment This study was funded by the National Multiple Sclerosis Society, grant PP1052. References 1.Peterson EW, Cho CC, von Koch L, et al. Injurious falls among middle aged and older adults with multiple sclerosis. Arch Phys Med Rehabil. 2008;89:1031-1037. 2.Weinshenker BG, Issa M, Baskerville J. Long-term and short-term outcome of multiple sclerosis: A 3-year follow-up study. Arch Neurol. 1996;53:353-358. 3.Finlayson ML, Peterson EW, Cho CC. Risk factors for falling among people aged 45 to 90 years with multiple sclerosis. Arch Phys Med Rehabil. 2006;87:1274-1279. 4.Lord SE, Wade DT, Halligan PW. A comparison of two physiotherapy treatment approaches to improve walking in multiple sclerosis: a pilot randomized controlled study. Clin Rehabil. 1998;12:477-486. 5.Rodgers MM, Mulcare JA, King DL, et al. Gait characteristics of individuals with multiple sclerosis before and after a 6-month aerobic training program. J Rehabil Res Dev. 1999;36:183-188. 6.Wiles CM, Newcombe RG, Fuller KJ, et al. Controlled randomised crossover trial of the effects of phsiotherapy on mobility in chronic multiple sclerosis. J Neurol Neurosurg Psychiatry. 2001;70:174-179. 7.Gutierrez GM, Chow JW, Tillman MD, et al. Resistance training improves gait kinematics in persons with multiple sclerosis. Arch Phys Med Rehabil. 2005;86:1824-1829. 8.Smedal T, Lygren H, Kjell-Morten M, et al. Balance and gait improved in patients with ms after physiotherapy based on the Bobath concept. Physiother Res Int. 2006;11:104-116. 9.Gibson-Horn C. Balance-based torso-weighting in a patient with ataxia and multiple sclerosis: A case report. J Neurol Phys Ther. 2008;32:139-146. 10.Widener GL, Allen DD, Gibson-Horn C. Balance-based torso weighting may enhance balance in persons with multiple sclerosis: Preliminary evidence. Arch Phys Med Rehabil. 2009;90:602-609. 11.O’Sullivan SB. Multiple sclerosis. In: O’Sullivan SB, Schmitz TJ, eds. Physical Rehabilitation. 5th ed. Philadelphia, PA: F. A. Davis Company; 2007:777-818. 12.Stockmeyer SA. An interpretation of the approach of rood to the treatment of neuromuscular dysfunction. Am J Phys Med. 1967;46:900-956. 13.Goff B. The application of recent advances in neurophysiology to miss rood’s concept of neuromuscular facilitation. Physiother. 1972;58:409-415. 14.Hewer RL, Cooper R, Morgan MH. An investigation into the value of treating intention tremor by weighting the affected limb. Brain. 1972;95:570-590. 15.Morgan MH. Ataxia and weights. Physiother. 1975;61:332-334. 16.Gillen G. Improving activities of daily living performance in an adult with ataxia. Am J Occup Ther. 2000;54:89-96. 17.Clopton N, Schultz D, Boren C, et al. Effects of axial loading on gait for subjects with cerebellar ataxia: preliminary findings. Neurol Report. 2003;27:15-21. 18.Lucy SD, Hayes KC. Postural sway profiles: normal subjects and subjects with cerebellar ataxia. Physiother Can. 1985;37:140-148. 19.Holmes G. The cerebellum of man. Brain. 1939;62:1-30. 20.Taylor JL, McCloskey DI. Proprioceptive sensation in rotation of the trunk. Exp Brain Res. 1990;81:413-416. 21.Jakobs T, Miller JA, Schultz AB. Trunk position sense in the frontal plane. Exp Neurol. 1985;90:129-138. 22.Podsiadlo D, Richardson S. The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142-148. 23.Kendall FP, McCreary EK, Provance PG. Muscles: Testing and Function. 4th ed. Baltimore, MD: Williams & Wilkins; 1993. 24.Bohannon R, Smith M. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67:206-208. 25.Lanska DJ, Goetz CG. Romberg’s sign: development, adoption, and adaptation in the 19th century. Neurol. 2000;55:1201-1206. 26.Berg K, Wood-Dauphinee S, Williams JI. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41:304. 27.Kurtzke J. Rating neurological impairment in multiple sclerosis: an expanded disability status scale (edss). Neurol. 1983:1444-1452. 28.Fry DK, Pfalzer LA. Reliability of four functional tests and rating of perceived exertion in persons with multiple sclerosis. Physiother Can. 2006;58:212-220. 29.Frzovic D, Morris ME, Vowels L. Clinical tests of standing balance: performance of persons with multiple sclerosis. Arch Phys Med Rehabil. 2000;81:215-221. 30.Schulfried O, Mittermaier C, Jovanovic T, et al. Effects of whole-body vibration in patients with multiple sclerosis: a pilot study. Clin Rehabil. 2005;19:834-842. For reprints and permission queries, please visit SAGE’s Web site at http://www.sagepub.com/journalsPermissions.nav Downloaded from nnr.sagepub.com at UNIV OF DELAWARE LIB on January 8, 2015