Jennifer L. Stinn Cartilage
advertisement

Inhibition of Metalloproteinases in Articular
Cartilage
by
Jennifer L. Stinn
Submitted to the Department of Electrical Engineering and
Computer Science
in partial fulfillment of the requirements for the degree of
Master of Science in Electrical Engineering
at the
MASSACHUSETTS INSTITUTE OF TECHNOLOGY
May 1995
@ Massachusetts Institute of Technology 1995. All rights reserved.
Author
Department o
lectrica Engineering and Computer Science
May 19, 1995
Certified by.........~:' .
"1" d
Al"....an J.'Grodzinsky
Professor of Electrical Engineering and Computer Science
Thesis Supervisor
(~\
Accepted by..........
~u1\AI
. I)
qp~-"
hA
.rl·'·
\KJ
Chairman, Dep rtmental
....................
Frederic R. Morgenthaler
ommittee on Graduate Students
IASSAGHUSE"TTS INST'ITU'rT
OF TECHNOLOGY
JUL 1 71995
LIBRARIES
Inhibition of Metalloproteinases in Articular Cartilage
by
Jennifer L. Stinn
Submitted to the Department of Electrical Engineering and Computer Science
on May 19, 1995, in partial fulfillment of the
requirements for the degree of
Master of Science in Electrical Engineering
Abstract
Osteoarthritic cartilage is characterized by an excess of matrix metalloproteinases
capable of degrading the tissue. Inhibition of articular cartilage degradation using
exogenously added natural and synthetic matrix metalloproteinase inhibitors was investigated. 4-aminophenylmercuric acetate (APMA) was used to activate latent metalloproteinases within articular cartilage explants and the degradation was assessed
by measuring the tissue's biochemical and physical properties. In addition, cartilage
treated with stromelysin was fitted to a layered poroelastic model to verify that in
cases where the inhomogeneity of cartilage is increased, the tissue is better described
by layers of homogeneous tissue than as a uniform sample.
Electromechanical measurements of explants treated with 4 p.g/ml of the natural
inhibitor, tissue inhibitor of metalloproteinase-1 (TIMP-1), show that this inhibitor
is capable of preventing the degradation induced by APMA. Streaming potentials
and dynamic stiffness were significantly greater in the samples which received TIMP.
Histology sections of TIMP and APMA treated explants suggest that TIMP is unable
to inhibit losses from the center of the explants. Doxycycline, a member of the tetracycline family, did not inhibit glycosaminoglycan (GAG) loss from explants treated
with APMA. The APMA did not induce measurable collagen loss so measurements
of collagenase inhibition by doxycycline were inconclusive. GAG loss from APMA
treated explants was inhibited in a dose dependent manner by an N-carboxylalkyl
compound, MC 354, with 2.0 pg/ml being sufficient to completely inhibit GAG loss
from explants treated with 1mM APMA for 3 days.
Progressive GAG loss from explants treated with SLN for 3 days results in an
increasingly nonhomogeneous tissue. Streaming potential and dynamic stiffness properties of SLN degraded explants can be modeled using the layered poroelastic theory.
This gives potentially better estimates of the hydraulic permeability, equilibrium modulus, and kinetic coupling coefficient for these samples than the estimates obtained
using the linear poroelastic model predictions.
Thesis Supervisor: Alan J. Grodzinsky
Title: Professor of Electrical Engineering and Computer Science
Acknowledgments
My list of 'acknowledgees' is long but the first one is easy. Many, many thanks to
Alan Grodzinsky. He is a wonderful teacher and patient advisor who also makes great
lab breakfasts. He was always enthusiastic and encouraging, even when the APMA
didn't do anything for the fourth experiment in a row! Thank you for making my
time in the lab rewarding and enjoyable.
Larry Bonassar and Eliot Frank were essential to the completion of these experiments and the understanding of how everything went together. Larry has been a
source of knowledge and advice on cartilage, the Dynastat, and how to crunch all
that data most efficiently. His patience and assistance are very much appreciated.
Without Eliot, I really wouldn't have had a fourth chapter in my thesis. Along with
his hell) on many of the technical aspects of the lab, he wrote the layered model
software which I used and was extremely patient when I wanted a different output or
input.
Thanks to Jane Murray and Claribel Paguio for their help in teaching me how
to do all those assays. An extra big thank you to Jane for many hours of help in
pipeting an(d those long days with explosive chemicals would have been disastrous
without your help!
Thanks to Dr. Mike Lark and Dr. Vern Moore from MERCKI
research laboratories
for providing us with the TIMP-1, proSLN, synthetic inhibitors and rhSLN antibody.
Dr. Ken Brandt supplied the doxycycline.
There are so many people in the lab who have all been great at helping out with
my experiments and in making the lab a casual, fun place to work. Thanks to Smruti
Parikh and Elaine Lee for running the SDS-PAGE gel to test the APMA, and helping
to show that it was the cows, not the experimenter that wasn't working! Steve Treppo
was a great consultant on how to layer up the degraded cartilage and although getting
the computer to do the fitting for me didn't work out that well, your enthusiasm was
infectious and made the model fitting much more fun. Tom Quinn makes the office
a much more interesting place to work and in between the jokes is always willing to
answer a serious 'cartilage' question. Thank you to Scott, Michelle, Paula and John
for operating 'Jen's answering service'. You have been great office-mates. Thanks to
Arthur, Greg, Colleen and Minerva for answering all those questions (How do you use
the scanner?) and offering encouragement when things were getting hectic. Many
thanks to Ann Black for always having an available pair of bent-tip tweezers and
making up all the DMB dye solution and to Linda for making sure we aren't too
serious. A final big thank you to everyone else in the lab for making this a great year
and a half.
Anybody reading this list will note the one 'lab member' that is conspicuously
absent. Dave, your friendship, caring, and sense of humor are invaluable. Because of
you, I've done a lot more with my time at MIT (like working with the GSC!), and
have had a lot more fun. Thanks for listening to my complaints (again and again)
and for all your help with my research, homework and everything.
Thank you to Thalia and Audrey for helping me to balance my life at MIT and
not get too stressed when things started to get really busy. I could always count on
one of you to take a "quick Tosci's break' when it was needed. To quote Sherry, you
are "really great friends".
Finally, thank you to my parents for getting me this far and for all your love,
confidence and support. Thanks also to my sisters, Sherry and Mandy, for listening
and for the glimpses of life in the 'real world'.
This research was funded by grants from MERCK and NIH.
Contents
1 Introduction
1.1
Background .
1.2
Electrokinetic Model ......
1.2.1
2
Layered Model.....
1.3
Matrix Metalloproteinases .
1.4
MMP Inhibitors .........
Methods
2.1
Materials
2.2
Cartilage Explant ........
2.3
APMA and Inhibitor Treatment
2.3.1
2.4
3
..........
............
APMA Efficacy .....
Biochemical Assays .......
2.4.1
Hydration Assay
2.4.2
Collagen Assay .....
2.4.3
GAG Assay
.
.......
2.5
Physical Property Tests
2.6
Histology
2.7
Statistics .
.
.
.
.
...........
............
Experimental Results
3.1
Synthetic Inhibitors .
3.2
Doxycycline ................................
.
.
.
.
.
.
. . . .
3.3
4
3.2.1
GAG Loss .....
. . . .
34
3.2.2
Collagen Damage .
. . . .
37
3.2.3
Hydration .....
. . . .
37
... .
37
37
TIMP
.
.
.
.
.
.
.
.
.
.
.
3.3.1
GAG Loss .....
. . . .
3.3.2
Physical Properties
. . . . 41
3.3.3
Histology
. . . .
. . . . .
41
Modeling the Response of Degraded Articular Cartilage
4.1
Theoretical Model Description ......................
4.2
Application of the Layered Model ....................
4.2.1
Initial Parameter Estimation ...................
4.2.2
Linearized GAG Loss Profile ...................
5 Discussion
63
5.1
Metalloproteinase Inhibitor Experiments
5.2
Layered Model
.
.........
. ...............
. . . . . . . . . .
63
.
. . . . ..
A Charged Inhibitors
67
A.1 Introduction ...................
A.2 Methods ...........
A.3 Results and Discussion .
65
.............
....
67
.................
. . . . . . . . . .
67
. . . . ..
68
List of Figures
1-1
A schematic representation of articular cartilage. The sparse population of chondrocytes are interspersed between the type II collagen
fibrillar network and the proteoglycans. Adapted from [1].
......
.
14
1-2
Schematic representation of the proteoglycan monomer. Adapted from [4]. 15
2-1
Activation of proSLN by APMA: SDS-PAGE of proSLN in DMEM
(column 1), in DMEM + APMA (column 2), with plasmin (column 3)
and with trypsin (column 4). The 57kDa proenzyme band is darkest
in the media column but still present in the plasmin column. All the
columns show both forms of the active enzyme but the APMA column
shows almost, complete activation to the 28 kDa form, with virtually
no proenzyme remaining. ...................
2-2
......
26
Cartilage explant samples cultured in DIMEM or 1 mMh APMA. The
three different APIMA curves are from three different animals. ....
2-3
Schematic of test chamber geometry for uniaxial confined compression
physical property measurements . ..................
3-1
227
..
30
Normalized GAG loss versus time in culture for calf cartilage explants
treated with APMA. with 2.0, 0.2. 0.02, 0.002, and 0.0002 pg/ml
MC 354 metalloproteinase inhibitor. ....................
3-2
33
Swelling Response versus time for calf cartilage explants treated DMEM,
DMEhM + 1mM APMA. and DMEM + 1 mM, APMA + MC 354 at
doses of 2.0. 0.2. 0.02, 0.002, and 0.0002 pg/ml. . ............
35
3-3
Normalized GAG content versus time in cartilage explants treated with
1 mM APMA and 1 mM APMA + 30 pjM doxycycline. . ........
3-4
36
Normalized tissue collagen content versus time in cartilage explants
treated with 1 mM APMA and 1 mM APMA + 30 pjM doxycycline. .
3-5
38
Swelled (0.01M saline) Weight/Unswelled Weight versus time in cartilage explants treated with 1 mM APMA and 1 mM APMA + 30 pM
doxycycline . . . . . . . . . . . . . . . . . .
3-6
. . . . . . . . . . . . . .
Normalized GAG loss versus time for 3mm cartilage explants treated
with 1 mM APMA with and without 4 pM TIMP for up to 72 hours.
3-7
39
40
Normalized equilibrium modulus for cartilage explants treated in 1
mM APMA with and without 4pM TIMP for 72 hours, expressed as
a percentage of the equilibrium modulus in the APMA with TIMP
sam ples. . . . . . . . . .
3-8
. .
.. . .
. . . . . . . . . . .
42
Comparison of A: hydraulic permeability and B: dynamic stiffness for
cartilage explants treated in 1mM APMA with and without 4pM TIMP
for 72 hours, expressed as a percentage of the hydraulic permeability
in the APMA and TIMP samples. .....
3-9
...............
. . .
43
Electromechanical property measurements for cartilage explants treated
in 1mM APMA with and without 4pM TIMP for 72 hours, expressed
as a percentage of the streaming potential for the APMA and TIMP
samples at each time point. A: Streaming Potential. B: Electrokinetic
Coupling Coefficient. .......
..........
.......
.
44
3-10 Histology samples for cartilage explants in DMEM (A), treated with 1
mM APMA for 72 hours (B) and treated with 1 mM APMA + 4 pM
TIMP for 72 hours (C). The stained regions represent areas of high
GAG content, while GAG has been removed from the unstained areas.
46
4-1
Light micrographs of cartilage disks incubated in DMEM alone for 72
hours (top) and DMEM with 100 jig/ml SLN for 24 hours (bottom),
represented at 100X. SLN treatment resulted in an apparent front of
enzymatic degradation moving inward from all exposed specimen surfaces, shown by the absence of toluidine blue stain for GAG. Adapted
53
from [2] .................................
4-2
Normalized GAG loss from cartilage disks incubated in DMEM with
and in DMEM with 100 pg/ml recombinant human stromelysin-1 (SLN)
Data are mean ± SD (n=4), reported as GAG remaining in the tissue normalized to total GAG (tissue + media GAG) at each time
point. Solid lines are best fit singles exponential decay curves of the
form le-t/T. The best fit decay time for 100 pjg/ml SLN is 7=26, and
7=1019 hr for DMEM alone. Adapted from [2].
4-3
.
. ..........
54
Layered model streaming potential magnitude and phase for completely degraded and undegraded layers. Data from 100pjg/ml SLN
treated cartilage is shown in the background (squares 0 hours of treatment, circles = 24 hours, stars = 48 hours, and triangles = 72 hours
of treatment)..............
4-4
...
56
............
Layered model dynamic stiffness magnitude and phase for completely
degraded and undegraded layers. Data from 100pg/ml SLN treated
cartilage is shown in the background (squares 0 hours of treatment,
circles = 24 hours, stars = 48 hours, and triangles = 72 hours of treat-
ment) ...................
4-5
5
.................
GAG content versus depth into tissue for trypsin treated cartilage cores
(mean ± SEM). For clarity, curves are plotted only until the depth at
which GAG content approxiamtely equals normal levels.
. .......
58
4-6
Layered model dynamic stiffness magnitude and phase for gradually
degraded cartilage using the optimal model parameters. The measured
response for cartilage treated with 100 pg/ml SLN is shown in the
background (squares = 0 hours of SLN treatment, circles = 24 hours,
stars = 48 hours and triangles = 72 hours of SLN treatment) .....
4-7
61
Layered model streaming potential magnitude and phase for gradually
degraded cartilage using the parameters from Table 2. The measured
response for cartilage treated with 100 pg/ml SLN is shown in the
background (squares = 0 hours of SLN treatment, circles = 24 hours,
stars = 48 hours and triangles = 72 hours of SLN treatment) .....
62
A-1 Normalized GAG loss for cartilage explants incubated in DMEM, DMEM
+ 1 mM APMA, DMEM + APMA + 2.0 ptg/ml MC068 (+), DMEM
+ APMA + 2.0 pg/ml MC044 (0), and DMEM + APMA + 2.0 pg/ml
MC069 (-). Data are mean±SD and n=4.
. ............
...
69
List of Tables
4.1
Layer thickness for the initial layered model parameters. Layers 1 and
3 were modeled as completely degraded with HA = 0.089, k = 16.2,
and ke = 3. Layer 2 was modeled as undegraded with HA = 0.89, k =
1.08, and ke = 4.
4.2
.
.
........ .........
....
...
..
.
55
Optimal layered model parameters to fit streaming potential and dynamic stiffness data from cartilage explants treated with 100 ug/ml
SLN for 24, 48 and 72 hours. . . ..............
.....
.
59
Chapter 1
Introduction
Osteoarthritis (OA) is an extremely common joint disorder affecting bone and cartilage in articulating joints. Symptoms are almost universal in the elderly, though it is
fairly uncommon in people under 40 years old [12]. The exact causes of OA are unclear
but heredity, aging, and metabolic and mechanical factors can promote the onset of
the disease [12, 21]. Clinically, initial superficial fissures in cartilage eventually give
rise to deep erosions, and finally loss of tissue. At the same time, the bone remodels,
leading to microfractures, thickening and hardening of subchondral bone and formation of bone cysts [21]. Although the disease mechanisms at, the cellular and tissue
level are unknown. research has shown that early changes in mechanical, chemical,
and metabolic properties are seen before macroscopic or radiological changes [25].
These early changes include increased hydration and swelling of the tissue as well as
a decreased fixed charged density and are the result of enzymatic degradation of the
extracellular matrix (ECM) constituents. The degradation of the matrix is thought to
be due to an excess of certain families of enzymes including matrix metalloproteinases
(MMPs) [28. 31, 5], serine proteinases [23], and "aggrecanase" [33].
This chapter contains an overview of the molecular structure and physical properties of articular cartilage, a description of the breakdown of the ECNM and the effect
of this on physical properties, and a summary of the model of the electromechanical
lbehavior of articular cartilage. Chapter 2 lists the materials and methods for the
physical testing and biochemical experiments. such as the mechanical testing pro-
cedure and the assay for glycosaminoglycan content. The results from the natural
and synthetic MMP inhibitor experiments are presented in Chapter 3, and Chapter 4
describes an extension of the electrokinetic model for non-homogeneous cartilage samples and shows how this model can be used to fit physical property parameters to
stromelysin treated cartilage explants. Finally, the results of the experiments and the
model are discussed in Chapter 5.
1.1
Background
Many books and review articles have been written about the structure and function
of the cartilage matrix. For example, see Maroudas [26], Hardingham [20], and Eyre
[10]. Cartilage physical properties are described in [18] and [19] and an electrokinetic
model of cartilage behavior is developed in [15] and [16].
Articular cartilage is a weight bearing material covering the ends of bones in synovial joints which reduces friction and distributes the loads in the joint. It is a highly
hydrated tissue (70-80% water) composed of collagen, proteoglycans, glycoproteins,
lipids and a sparse population of cells or chondrocytes. Figure 1-1 shows a simplified
schematic of the tissue structure.
Chondrocytes make up about 2-3% of the volume of adult cartilage (up to 10%,
in newborns) and are responsible for sustaining normal repair and turnover of proteins and other matrix constituents. They respond to mechanical, nutritional, and
hormonal stimuli [26] to produce the extracellular matrix components as well as proenzymes such as neutral metalloproteinases which are capable of degrading the matrix.
Adult cartilage is aneural and avascular, so the cells obtain nutrients by diffusion
from the synovial fluid.
Collagen makes up approximately 65-75 percent of cartilage dry weight and the
amount varies with depth in the tissue. The fibrils form a coarse network within
cartilage which provides for most of the tensile strength of the tissue. The network
consists of mostly type II fibrils, but also contains types IX and XI. The type II fibrils
are stabilized by extensive covalent cross-linking between type II and type IX collagen
GAG chain
I
Chondrocy
Figure 1-1: A schematic representation of articular cartilage. The sparse population
of chondrocytes are interspersed between the type II collagen fibrillar network and
the proteoglycans. Adapted from [1].
14
14
Chondroitin Sulfate
Figure 1-2: Schematic representation of the proteoglycan monomer. Adapted from [4].
molecules. At physiological pH, collagen is essentially neutral (slightly positive), so
its main functions are to provide the tensile strength of cartilage to resist swelling
and to provide bulk stiffness for the tissue.
Proteoglycans (PGs) form about 15 percent of the dry weight of cartilage and
are largely responsible for its electromechanical behavior. PGs are composed of large
macromolecules known as glycosaminoglycans (GAGs) which are unbranched linear
polymers of repeating disaccharide units. The most abundant PG is aggrecan which
consists of a long protein core to which are attached many chondroitin sulfate (CS)
and keratan sulfate (KS) side chains giving the molecule a 'bottle brush' appearance.
As shown in Figure 1-2, the N-terminus of aggrecan consists of two globular regions
(G1 and G2) separated by a 21 nm interglobular domain. Another globular domain
(G3) is at the C-terminal, after the extended CS and KS side chains. After secretion
from the chondrocyte, the N-terminus of these PG monomers binds to hyaluronic
acid (HA) to form large macromolecular aggregates. The bond with HA is stabilized
by a link protein. The size of these aggregates varies from 2-5 PGs to 400-800 PGs,
depending on the availability of PG monomers and the length of the hyaluronic acid.
At physiological pH, the carboxylic acid and sulfate groups on the GAGs dissociate
giving aggrecan a high negative fixed-charge density. To maintain electroneutrality,
there is an excess of positively charged mobile ions in the ECM creating a high osmotic
pressure and a tendency for the tissue to swell. The loss of PGs is one of the early
indicators of osteoarthritic changes and occurs when proteolytic enzymes, such as
stromelysin or aggrecanase, cleave aggrecan within the interglobular domain freeing
the negatively charged portion of the molecule to diffuse out the tissue.
Articular cartilage is subjected to a wide range of mechanical loads. Its ability to
withstand the resulting compressive, tensile and shear forces depends on the structure,
composition and integrity of the ECM. The collagen network provides the bulk of the
tensile strength of cartilage while the proteoglycans are responsible for the majority
of the compressive stiffness due to their bulk stiffness and electrostatic repulsion.
Electrostatic repulsion, at the molecular level, is the result of the interaction between
double layers around adjacent GAG chains.
The repulsive force is the combined
result of repulsion between negatively charged GAG chains and the repulsion by
the surrounding positive ions for each double layer. The electrostatic repulsion is
dependent oni the fixed charge density of the ECM and the pH of the surrounding
media.
When cartilage is compressed, interstitial fluid flow tends to separate the fixed
negative charges in the proteoglycan (PG) molecules from the positive counterions
in the fluid, creating an electric field pointing in the direction of the fluid flow. This
streaming potential field is proportional to the fluid velocity and the fixed charge
density. Conversely, if cartilage is exposed to an applied current density and held
at a fixed thickness, a current-generated stress can be measured which is the result
of electrophoretic force of the PG network towards the positive electrode and the
electro-osmotic flow of positive ions towards the negative electrode.
A controlled
reduction of the fixed-charge density using stromelysin and other enzymes to cleave
the proteoglycan molecule and allow the fixed charge portion to migrate out of the
tissue causes a significant reduction in the measured streaming potential [2]. This
signal (-an be used as an early indicator of PG degradation in cartilage.
1.2
Electrokinetic Model
A continuum model of cartilage electrokinetics has been developed by Frank and
Grodzinsky [15]. The results are summarized here for uniaxial compression. For a
complete description and derivation of the model as well as its experimental verification, please see [13].
The total area-averaged relative fluid velocity, U(z) and current density, J(z) are
linearly proportion to the gradients in fluid pressure Pf(z) and electrical potential,
V(z) (when the potentials and pressures are small enough),
U(z)
-ki
J(z)
k21
k12
Pf(z)
-k 22
V(z)
Adding a constitutive law for total stress in a homogeneous, isotropic tissue for
small strains, the relation between uniaxial compressive strain and tissue displacement
u(z), and continuity, conservation of momentum and conservation of current laws gives
seven equations in seven unknowns.
a = HAE + P1
E=
aU
-=
OJ
Oz
Ou(z)
Oz)
0&.
(1.2)
(1.3)
S= -
(1.4)
0
(1.5)
=0
(1.6)
HA is the equilibrium confined compression modulus, a is the compressive stress
and E is the compressive strain, defined to be positive in compression. J is the current
and u(z) is the tissue displacement in uniaxial confined compression. For an imposed
sinusoidal displacement of amplitude u0 , these equations can be solved [13] to give
open circuit cartilage stiffness, open circuit stress, and streaming potential:
Aoc -
= HA-yJ coth y6
(1.7)
6
A,HAy6 coth -y
oc = A + HASoth
[uo/] = A(uo/6)
(1.8)
F[ AHA'Y6 tanh 2-1 uO
oc = ke
[A + HAy
6 coth
(1.9)
2
y6J 6
where iu = u(z = 0) is the imposed displacement at the top of the plug, 6 is the
thickness of the cartilage plug, y2 = jw/HAk, k = kil - (k
12
k 2 1 /k
22
), ke = k21/k22,
and As is the effective platen spring stiffness. The imposed displacement u0 will not
all appear at the top of the plug because some of the displacement is taken up by the
porous platen, ie. u0 : u0.
1.2.1
Layered Model
Enzymatic degradation of cartilage and normal breakdown in osteoarthritis leads to
variations in fixed-charge density, water content, PG concentration, hydraulic permeability and other properties with depth in the tissue [26]. Frank and Grodzinsky
[19, 13] also developed a layered model to account for such spatial variations. In this
model, the cartilage sample is divided into many different homogeneous layers each
having different mechanical and electromechanical properties. The streaming potential and mechanical stiffness for each layer can by computed using the above linearized
poroelastic model. First, if steady state sinusoidal displacements u0 and u0 are applied to the top and bottom surfaces of the layer, the swelling stresses p,-P = HAE
are given by
p
p
1[
coth-y6
(-1/ sinh-y6)
(1.10)
u3
- coth y6
(1/ sinh-y)
This can be rewritten to give a transfer function relating the parameters for the
top and bottom surfaces
[Lu J=
(sinh76/HAy)
cosh y6
u
(1.11)
For an n-layer tissue sample, there will be n+1 tissue interfaces with the displacement and swelling forces at the bottom of the ith layer being equal to the forces at
the top of the (i+l)st layer. Multiplying the matrices for all the layers gives
[oi=1
PO
II
cosh 7J
HATY sinh76)
cosh
(sinh 76/HAy)
y6
pn
ithlaer
(1.12)
where po and uO are the swelling stress and displacements at z = 0 and u" = 0
since the bottom surface of the plug is fixed. The resulting open-circuit mechanical
stiffness is given by
Ao
where
-•l.
and
11n,
c
=
11
1121
(1.13)
are terms from the product matrix and 6 is still the total plug
thickness.
The streaming potential and current-generated stress can be found by solving
the matrix for the displacements and substituting these values back in the original
equations to find the potential and stress for each layer, then summing the results for
all the layers. The theoretical basis for the layered model is described more fully at
the beginning of Chapter 4.
1.3
Matrix Metalloproteinases
Matrix metalloproteinases (MMPs) are proteolytic enzymes capable of degrading the
ECM. In healthy tissue, they are synthesized and secreted to maintain normal matrix
turnover. In the disease state, the amount of MMPs present in cartilage increases
greatly [9, 25]. Three experimental models which mimic increased ECM degradation in vitro when added to tissue cultures are: interleukin-1 (IL-1), retinoic acid
(RA), and p-aminophenyl mercuric acetate (APMA). IL-1 is known to stimulate increased production of MMPs by chondrocytes; however, the aggrecan cleavage cite is
not that typically associated with MMPs but, rather, that due to an activity called
"aggrecanase". RA also stimulates increased degradation of PGs, again showing the
aggrecanase cleavage site. APMA activates the endogenous MMPs in the tissue.
MMPs are active at neutral pH, have zinc at their active sites and require Ca++
to be active. They are synthesized and secreted in a proenzyme form. Based on their
primary action, three of the 13 or more MMPs of interest to the present study are
[27]:
tissue collagenase (IMMP-I)
Cleaves collagen types I. II, III, VII, X
gelatinase (MMP-2) Cleaves collagen types IV, V,. VII and gelatins
stromelysin (MMP-3) Cleaves proteoglycans, collagen types IV, IX, laminin and
activates collagenase.
Activation of stromelysin (SLN) is key since it can activate procollagenase as well
as degrade most of the molecules in the ECM [29]. ProSLN is synthesized and secreted by connective tissue cells and can be activated by endopeptidases including
trypsin, chymotrypsin, plasmin, plasma kallikrein, neutrophil elastase, thermolysin
and cathepsin G as well as by mercurial compounds like APMA [29, 27]. The activation sequence occurs in two steps with the 57 kDa proenzyme being cleaved by
proteases and then being auto-cleaved. There are two active forms of SLN: a 45 kDa
form and a 28 kDa form with identical substrate specificities and specific activities
[27]. Interleukin-1 (IL-1) and tumor necrosis factor alpha are capable of increasing
the transcription and translation of proSLN mRNA [29, 24].
1.4
MMP Inhibitors
In addition to being secreted in an inactive form, MMP activity is limited by natural
inhibitors like tissue inhibitor of metalloproteinases (TIMP) which is also synthesized
and secreted by the chondrocytes [24]. TIMP-1, used in these experiments is a 23
000 kDa glycoprotein which inhibits MMPs on a 1:1 basis by forming a high-affinity
complex [31].
TIMP-2 shares approximately 40% sequence identity with TIMP-1
but is not glycosylated and has a molecular weight of 22 000 kDa [38]. Reduction
and alkylation of TIMP prevent its inhibitory action, suggesting that its activity is
dependent on its tertiary structure [24]. Normally, there is a molar excess of TIMP in
cartilage with a ratio of SLN concentration : TIMP concentration of approximately
0.5 [25]. In OA, both TIMP and MMP secretion increase but the TIMP:SLN ratio
increases to from 1.6 to 5.3 leading to excess ECM degradation [25, 9]. The local
induction of TIMP to synovial lesions has been suggested as a possible method of
treatment [38] but due to TIMP's large molecular weight, it is questionable whether
it. will be able to effectively diffuse into the ECM [30].
Several smaller, synthetic MMP inhibitors and antibiotics which are able to freely
diffuse into the tissue are being investigated as potential treatments for osteoarthritis.
Doxycycline (of the tetracycline family), hydroxamate-based peptides [8, 34], and Ncarboxyalkyl peptides [6] are all inhibitors of metalloproteinase activity with potential
clinical use. All these synthetic inhibitors work by chelating the Zn + + ion.
The inhibitory effects of tetracycline, doxycycline and minocycline on collagenase
and gelatinase activity have been confirmed by several investigators through in vitro
and in vivo studies [38, 17].
In addition, chemically modified tetracycline (CMT)
compounds have been synthesized which have no antibacterial activity but are still
capable of inhibiting collagenase activity [38]. However, animal model studies and
clinical trials to determine the effects in vivo have not produced conclusive evidence
of improvement of OA symptoms [17, 35] even when MMP activity was reduced.
Similarly, hydroxamate-based peptides and N-carboxyalkyl peptides have been
shown to greatly reduce the level of MMP activity in vitro and in vivo [34, 6] but
have not been approved for clinical testing so their ability to prevent or even slow the
progress of osteoarthritis is not proven.
Chapter 2
Methods
2.1
Materials
Dulbecco's phosphate buffered saline (PBS), penicillin/streptomycin, non-essential
amino acid solution, and Dulbecco's modified Eagle's medium (DMEM) were purchased from Gibco. Grand Island, NY. L-proline, p-aminophenyl mercuric acetate
(APMA), L-cysteine, sodium phosphate monobasic anhydrous, sodium phosphate
dlibasic anhydrous. twice crystallized papain, shark chondroitin sulfate, chloramine T.
p-diaminobenzaldehyde, sodium azide, hydrochloric acid and ethvlenediaminetetraacetic acid (Na 2 EDTA) were purchased from Sigma, St.
Louis, MO. Dimethyl-
methylene blue and gluteraldehyde were from Polysciences, Warrington, PA. Citric
acid monohydrate, glacial acetic acid, perchloric acid, dimethyl sulfoxide (DMSO)
and sodium chloride were from Mallinckrodt, Paris, KY. Proteinase K was from
Boehringer Mannheim, Indianapolis, IN. Glycine was from Aldrich Chemical Co..
Milwaukee, WI. Sodium acetate trihvdrate was from EM Science, Cherry Hill. NJ
and sodium cacodylate was from Bio-Rad, Cambridge, MA. 24-well tissue culture
dishes were from Costar, Cambridge, MA and acrylic cuvets were from Centar West,
Sparks, NV.
Tissue inhibitor of metalloproteinases (TIMP-1), human recombinant prostromelysin
(proSLN), and rhSLN antibody for SDS-PAGE were prepared courtesy of Dr. Michael
Lark and associates. MERCK Research Laboratories. Rahway, NJ. Doxvcycline was
provided courtesy of Dr. Ken Brandt, Indiana.
2.2
Cartilage Explant
Calf articular cartilage was harvested from the femopatellar groove of 1-2 week old
calves as previously described in [32]. All animals were purchased from J. Larusso,
Research 87, Revere, MA. Full thickness, 9mm diameter cartilage plugs with approximately 1cm of bone attached were drilled from the lateral and medial facets of the
femopatellar groove. The exposed cartilage surface was frequently washed with sterile PBS containing 100 U/ml penicillin and 100 pg/ml-streptomycin. Approximately
100,um was removed from the top surface of each plug with a sledge microtome (American Optical, Buffalo, NY) to create a level surface, then two 1mm thick disks were
sliced from the core. Four 3mm diameter plugs were punched from each slice using a
stainless steel dermal punch (Miltex Instruments, Lake Success, NY) and each group
of four plugs was placed in 1 ml of media and incubated for approximately 12-16 hours
at 37 0 C. 5% CO2: 957 air. The media consisted of DMEM with 1 g/L glucose and
10 mM HEPES supplemented with 100 U/ml penicillin and 100 pg/ml streptomycin.
2.3
APMA and Inhibitor Treatment
The control media for all the experiments was DMEM with 1g/L glucose, 0.1 mM nonessential amino acids and 10 mM HEPES. Aliquots of control media supplemented
with 1 rnM APMA were pH-equilibrated by incubating them in loosely capped tissue
culture vials at 370 C, 5% CO2: 95% air for approximately 16 hours. Additional
inhibitors (TIMP, doxycycline or MERCK compounds) were added to APMA and
control media solutions immediately before aliquoting media samples into culture
dishes and adding the cartilage plugs. In general, the four plugs from each disk were
matched across conditions and across time to minimize the effects of variations in
tissue based on original location within the joint. The cartilage plugs were incubated
at 370 C, 5% CO 2 : 95% air in their media and continuously mixed using an orbital
shaker (Lab Line Orbit Shaker) for 24, 48 or 72 hours, then assayed for hydration,
mechanical properties, GAG and collagen content.
2.3.1
APMA Efficacy
The degree of degradation which occurred due to the activation of endogenous metalloproteinases by APMA varied significantly between animals and between experiments. This could be due to variations in proenzyme levels in the tissue or precipitation of APMA. We ran sodium dodecyl sulfate-polyacrylamide gel electrophoresis
(SDS-PAGE)' of media with prostromelysin, and media with prostromelysin and
APMA to test the effectiveness of the APMA. Samples were boiled in sample buffer
(1.0 M Tris-HC1 pH 6.8, 60% glycerol, 2-mercaptoethanol, 5% bromophenol blue)
for 2 minutes, then stacked in 4.5% polyacrylamide gel (0.125 M Tris-HC1, pH 6.8,
0.1% SDS, 0.5 mg/ml ammonium persulfate) for 10 minutes at 175 V, and resolved
(-10%
polyacrylamide, 0.375 M Tris-HCl pH 8.8, 0.1% SDS, 0.5 mg/ml ammonium
persulfate) for 50 minutes at 200 V. After electrophoresis, the proteins were analyzed
by Western blotting: the proteins were blotted onto a sheet and treated with rhSLN
antibody (a bovine SLN antibody was not available), the sheet was rinsed with a
radioactively labeled antibody specific for the SLN antibody, and the sheet was overlayed with x-ray film, exposed and developed. As shown in Figure 2-1, the APMA
did activate the prostromelysin by cleaving a portion of the molecule producing the
lower molecular weight stromelysin molecule.
Therefore, the variations is GAG loss with APMA treatment as shown in figure 22 are most likely the result of variations in proenzyme level within the cartilage
explants.
1
SDS-PAGE is a method of separating proteins in a sample based on their molecular weight.
Proteins are coated with a charged material (SDS) to give an equal surface charge density to all
proteins, and aliquots of the media are placed at the top of a gel column. An applied voltage causes
the proteins to migrate down the column with smaller molecules migrating more quickly because
they are not as impeded by the gel. The separated proteins are then transferred to a membrane and
stained so a dark band will appear in the presence of any proteins. Control proteins or markers of
known molecular weight are run simultaneously so comparing the bands can give an approximate
molecular weight of the proteins [37].
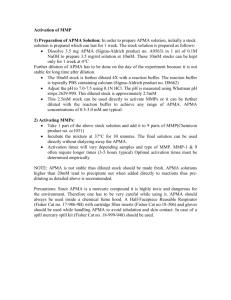
Figure 2-1: Activation of proSLN by APMA: SDS-PAGE of proSLN in DMEM (column 1), in DMEM + APMA (column 2), with plasmin (column 3) and with trypsin
(column 4). The 57kDa proenzyme band is darkest in the media column but still
present in the plasmin column. All the columns show both forms of the active enzyme but the APMA column shows almost complete activation to the 28 kDa form,
with virtually no proenzyme remaining.
26
Endogenous MMP Variability
10.8-
ii
_L
0
03
Ct
_L
<cn 0.6Cn
w
0.4-
~
m DMEM
* APMA (1)
A
z2s
0.2-
L
APMA (2)
* APMA (3)
r
048
24
72
TIME, hr
N=4 + SD
Figure 2-2: Cartilage explant samples cultured in DMEM or 1 mM APMA. The three
different APMA curves are from three different animals.
For future experiments, it would be useful to have an assay for the total amount
of proenzyme available in each tissue sample.
2.4
2.4.1
Biochemical Assays
Hydration Assay
As the collagen network is responsible for the tensile strength of the cartilage ECM,
damage or removal of collagen may result in tissue that is less able to resist swelling.
Based on the method of Maroudas [26], we indirectly assessed collagen network integrity using hydration measurements. We removed the samples from culture which
contained 0.15 M saline and measured the wet weights of the plugs assuming this to
be indicative of water content in physiological saline. We then placed each plug in 2
ml of hypotonic saline (0.01 M NaC1l) for 2 hours and remeasured the wet weights. We
calculated a swelling ratio as the hypotonic saline weight/physiologic saline weight.
2.4.2
Collagen Assay
For the doxycycline treated cartilage samples, we used the hydroxyproline assay described in [36] to measure the collagen content of the samples. Collagen is approximately 1/10 hydroxyproline, by weight. After taking dry weights of the cartilage
explants. we digested the samples with papain, and dehydrated aliquots in an oven.
We then added NaOH to alkaline hydrolize the tissue, neutralized the samples with
citric acid, oxidized the hydroxyproline with chloramine T, and stopped the reaction
with perchloric acid to prevent over-oxidation. Finally, we added dimethylbenzaldehyde (DMBA) to form a chromaphore, incubated the samples to accelerate the reaction, and read the absorbance on the spectrophotometer (Perkins-Elmer UV/VIS
spectrophotometer).
Hydroxyproline content was determined from hydroxyproline
standards and the total collagen was estimated as 10 times the hydroxyproline.
2.4.3
GAG Assay
'We assayed for the total GAG content in the samples and the media using the
metachromatic DMB dye-binding assay described in [11]. Each plug was digested with
papain (125 pg/ml of buffer containing 0.06 M NaH 2PO 4 -H2 0, 0.04 M Na 2 HPO 4 -7H2 0
and 5 mM Na 2 EDTA, pH 6.5) or proteinase K (0.5 mg/ml in same buffer as for papain
digestion) for 16 hours at 600 C. 20 ~Il of sample and 2 ml of dimethylmethylene blue
(DMB) dye solution were placed in a polystyrene cuvet and the absorbance read using a Perkins-Elmer UV/VIS spectrophotometer. GAG concentration was determined
from shark chondroitin sulfate standards. The percent GAG loss for each condition
was defined as the amount of GAG in the media divided by the total amount of GAG
in all four plugs plus the media.
2.5
Physical Property Tests
We used the confined compression geometry described in [14] and shown in Figure 23. Each 3mm cartilage disk was placed in the well, sandwiched between a Ag/AgC1l
electrode (Annex Research, Costa Mesa, CA) and a porous polyethylene platen. The
platen allowed free fluid flow at the top surface of the sample during testing; no fluid
flow occurred at the remaining disk surfaces. The well was filled with PBS suppleinented with penicillin/streptomycin and a second electrode placed in the solution to
obtain the streaming potential response. A 20% static strain was applied at the u=0
boundary, and the plug was allowed to recover for approximately 20 minutes, with
stress relaxation assumed to be complete when the measured load was approximately
constant. A 1% sinusoidal displacement was superimposed on the static strain at
frequencies from 0.01-1.0 Hz using a frequency generator (Rockland Systems, West
Nyack, NY). The load response was sensed by a mechanical spectrometer (Dynastat, IMASS, Hingham, MA) and the streaming potential, displacement, and load
response signals were recorded on a chart recorder (Gould Brush 2200, Cleveland,
OH) and on a microcomputer. In order to calculate the equilibrium modulus, the
static strain was increased to 21%, the plug was allowed to relax. and the response
To Load Cell
I
Ag/AgCI eli
Recirculation Port
ous Platen
tilage Sample
AgCI Reference Electrode
Jator mount
Figure 2-3: Schematic of test chamber geometry for uniaxial confined compression
physical property measurements
to a 1.0 Hz signal was recorded. Finally, the static strain was decreased to 19%, and
the 1.0 Hz signal response was measured after stress relaxation. The testing sequence
lasted about 1 hour/plug and the plugs were tested consecutively over approximately
8 hours for each time point (24, 48 and 72 hours). Using the model developed by
Frank and Grodzinsky [14], the dynamic stiffness, equilibrium modulus, and hydraulic
permeability of the samples was calculated from the recorded data.
2.6
Histology
APMA and APMA with TIMP treated cartilage explants were stained and sectioned
to show the spatial localization of degradation due to transport characteristics of
the APMA and TIMP molecules. Based on previous work by Hunziker et. al. [22],
samples were stained with dimethylmethylene blue (DMB), a cationic dye which
forms stable proteoglycan-dye complexes and aldehyde fixation conditions. The disks
were fixed for 48 hours in a solution containing 2% gluteraldehyde, 50 mM sodium
cacodylate, and 0.2% (w/v) DMB, pH 7.4. Samples were then rinsed three times over
1.5 h in 1 ml of sodium cacodylate buffer, at room temperature, pH 7.4. Samples
were stored in 1 ml of 70% ethanol (v/v) at 4VC then shipped to Pathology Services,
Cambridge, MA to be embedded in parafin, transverse sectioned and mounted on glass
microscope slides. The slides were viewed with a light microscope (Nikon DiaphotTMD, Tokyo, Japan) and selected tissue sections were photographed.
2.7
Statistics
All data are reported as mean +/- SEM, unless otherwise stated. Statistical significance of the data was calculated using the two-tailed t-test with p-values less than
0.05 considered to be significant.
Chapter 3
Experimental Results
This chapter describes the results from the synthetic inhibitor studies, the biochemical
assay results from doxycycline treatment, and the physical property measurements
from explants treated with APMA and TIMP.
3.1
Synthetic Inhibitors
Chapman et. al. [6] have demonstrated that n-carboxyalkyl compounds, such as
MC 354, are capable of inhibiting the activity of neutral metalloproteinases like SLN
in vitro and in vivo with exogenously added enzyme and inhibitor. We tested the
ability of these compounds to inhibit endogenous metalloproteinases, activated with
APMA.
We treated calf cartilage explants with 1 mM APMA in DMEM and 2.0, 0.2, 0.02,
0.002, and 0.0002 pg/ml MC 354 for up to 72 hours and assayed for swelling response
and GAG loss. Figure 3-1 shows that at 2.0 pg/ml, the inhibitor was capable of
completely preventing GAG loss from the tissue. The degree of inhibition decreased
with decreasing inhibitor concentration and by 0.002 and 0.0002 pg/ml MC 354,
the GAG loss was not significantly different than that loss without any inhibitor.
An additional condition in this test was the addition of 0.1% bovine serum albumin
(BSA) to the 2.0 pg/ml MC 354 condition. The inhibitor was thought to bind to
the BSA, reducing the amount available to diffuse into the tissue because BSA is
GAG Loss for MC354 and APMA Treatment
1-
0.8C)
Cn
I-
0.6N
-J
0.4-
Z
2e
0.2 •
0O- 1 ·
V
1
24
48
72
TIME, hr
N=4 + SEM
Figure 3-1: Normalized GAG loss versus time in culture for calf cartilage explants
treated with APMA, with 2.0. 0.2. 0.02, 0.002, and 0.0002 pg/ml MC 354 metalloproteinase inhibitor.
sterically limited in its ability to diffuse into normal cartilage ECM. Since any drug
administered as a treatment for OA will have to diffuse into cartilage from synovial
fluid, binding effects could play an important role in determining the effectiveness of
a drug. A small non-statistically significant effect of decreased inhibition is visible
by 72 hours but further experiments are necessary before conclusions can be made
about this effect.
The hydration measurements for these cartilage samples, in Figure 3-2, showed no
swelling for any of the conditions indicating that either there was no damage to the
collagen network or that the measurements were insensitive to the degree of collagen
damage present.
3.2
Doxycycline
Several researchers [38, 17] have found that drugs in the tetracycline family are capable of inhibiting collagen damage in cartilage. Conflicting reports of the ability of
tetracycline and its derivatives, such as doxycycline, to inhibit the release of proteoglycans is shown in the references. Burris et al [3] showed that doxycycline did not
prevent PG loss from human metacarpal cartilage explants. In contrast, Cole et al [7]
found that doxycycline, as well as several chemically modified tetracycline derivatives
did prevent proteoglycan release in chick tibial explants. We tested doxycycline as a
metalloproteinase inhibitor in the APMA system.
3.2.1
GAG Loss
As shown in Figure 3-3, 30pM doxycycline does not inhibit the metalloproteinases
activated by APMA, nor does it have any effect on control samples, incubated in
media alone. There was a large variation in the amount of GAG in each plug, leading
to a the large standard deviations in the normalized GAG content for the doxycycline
and doxycycline + APMA cartilage disks.
MC354 and APMA Treatment
Swelling Response
c 1.04 a)
.1.02 -
z0
D 0.002gg/ml MC354
o 0.0002pg/mi MC354
* 2.0pg/mi MC354 + 0.1% BSA
•0.980
48
24
72
TIME, hr
N=4 + SEM
Figure 3-2: Swelling Response versus time for calf cartilage explants treated DMEM,
DMEM + 1mM APMA, and DMEM + 1 mM APMA + MC 354 at doses of 2.0, 0.2,
0.02, 0.002, and 0.0002 pg/ml.
Doxycycline and APMA Treatment
GAG loss
C,
W
Cn
0.8-
w
za
0.6-
cc
...
r<
0 0.4-
O._
Z
0.2 -^§-%ml
nVm$B
T
tRU ILLw,•nnv
mO
VIy
0-24
48
72
TIME, hr
N=4 + SEM
Figure 3-3: Normalized GAG content versus time in cartilage explants treated with
1 mM APMA and 1 mM APMA + 30 pM doxycycline.
3.2.2
Collagen Damage
Based on the results in Figure 3-4, the APMA system did not induce any collagen loss
from the cartilage explants in the 72 hours of treatment, or the hydroxyproline assay
was not sensitive enough to detect the amount lost from the explants. Although the
hydroxyproline assay is the most common assay for collagen degradation, it is not an
easy assay to perform and there is a significant amount of variation within duplicates
in the assay. If we cultured the explants for a longer period of time, the collagenase
activated by the APMA would remove more collagen from the matrix but there would
likely be more proteoglycan and collagen loss from the control samples as well.
3.2.3
Hydration
The swelling results for the doxycycline treated cartilage explants, in Figure 3-5, are
consistent with the collagen loss results. Since the collagen loss from the explants
was minimal, the amount of swelling was expected to be minimal as well.
3.3
TIMP
TIMP is a highly potent natural inhibitor of metalloproteinases produced by the
chondrocytes. When administered in high enough doses to cartilage explants treated
with APMA, it is capable of completely blocking GAG loss from the tissue [30]. We
mechanically tested the APMA and APMA+TIMP treated cartilage disks to verify
that the tissue's physical properties were also maintained when TIMP was present.
3.3.1
GAG Loss
The results of the assay for GAG content showed that after 72 hours of treatment with
APMA, 75% of the GAGs had been removed from the tissue. However, the cartilage
plugs which also had TIMP in the media lost less than 15% of their GAGs and did
not differ significantly from control (DMEM only) plugs, as shown in Figure 3-6.
Doxycycline and APMA Treatment
Collagen Loss
Z
.. I
O
0
1-
iu.I
M1
U
.I
Výý
I
FII
OU
N
P_
m
-
-
i
LT
0.80
A
DMEM
APMA
@30 gM Doxy
0
* APMA + 30 ,gM Doxy
0.624
48
72
TIME, hr
N=4 + SEM
Figure 3-4: Normalized tissue collagen content versus time in cartilage explants
treated with 1 mM APMA and 1 mM APMA + 30 pM doxycycline.
Doxycycline and APMA Treatment
Swelling Response
C)
S1.05
C) 0.95
d
U,
S0.95
C)
0
48
24
72
TIME, hr
N=4 ± SEM
Figure 3-5: Swelled (0.01MN saline) Weight/Unswelled Weight versus time in cartilage
explants treated with 1 mM APMA and 1 mM APMA + 30 pM doxycycline.
GAG Loss for APMA and TIMP Treatment
C(3
DMEM
1-
4 gM TIMP +
1 mM APMA
Ui
LI.
U)
C,) 0.8-
0I-
N
-J
0.61 mM APMA
0.4-
a:
0 0.2Z
0
24
48
72
TIME, hr
N=4 ± SE
Figure 3-6: Normalized GAG loss versus time for 3mm cartilage explants treated with
1 mM APMA with and without 4 pM TIMP for up to 72 hours.
3.3.2
Physical Properties
Using the procedure described in Chapter 2, four plugs treated with 1 mM APMA
and four plugs treated with 1mM APMA + 100 pg/ml TIMP were tested in the
Dynastat at each time point: 24, 48 and 72 hours. The mechanical integrity of the
tissue samples was determined by comparing inhibited and uninhibited values for
permeability, dynamic stiffness and equilibrium modulus. The equilibrium modulus
for the APMA treated plugs decreased to approximately 65% of the modulus of plugs
treated with APMA and 4pM TIMP after 24 hours and remained at that level until
72 hours, as shown in Figure 3-7.
Hydraulic permeability and dynamic stiffness data are shown in Figure 3-8. Without TIMP, the hydraulic permeability increased significantly by 24 hours of APMA
treatment, and continued to increase to 48 hours. Dynamic stiffness decreased over
the 72 hours of treatment with APMA and no inhibitor.
Streaming potential and electrokinetic coupling coefficient measurements were
made to determine the electromechanical properties of the degraded and undegraded
tissue. The streaming potential of the APMA treated explants decreased with time
in culture, as shown in Figure 3-9. After 24 hours, the APMA streaming potential
was 5C3 7 , of the APMA and TIMP value and by 48 hours, it had decreased to 33%
of the streaming potential of the APMA and TIMP treated samples. Similarly, the
electrokinetic coupling coefficient of the APMA treated samples decreased with time
in culture.
These results suggests that both mechanical and electromechanical properties of
the cartilage explants were maintained by using 4pM TIMP to inhibit the 1mM
APMA in the explant media.
3.3.3
Histology
APMA is a very small molecule (MW = 351.8 g/mol) and is able to diffuse into
the cartilage ECM very rapidly, while TIMP is sterically excluded from the matrix
and diffuses into the tissue much more slowly. We stained and sectioned cartilage
APMA and TIMP: Equilibrium Modulus
C,,
1.5D 4 gM TIMP + 1 mM APMA
m1 mM APMA
C12
n-
1-
D
rn
5
w
0 0.5w
N
cc
0
Z
I --II
S-
24
48
72
TIME, hr
N=4 + SE
x p < 0.05
Figure 3-7: Normalized equilibrium modulus for cartilage explants treated in 1 mM
APMA with and without 4pMA TIMP for 72 hours, expressed as a percentage of the
equilibrium modulus in the APMA with TIMP samples.
APMA and TIMP Mechanical Properties
Hydraulic Permeability
60
50
4 gM TIMP + 1mM APMA
E
1 mM APMA
*
p < 0.05
{
40
E
c,
E
30
H
T
20
F-48
72
Dynamic Stiffness @ 1Hz
1.2 cn
1
0.8
c)
U)
E
0.60.4
0.200
24
48
72
TIME, hr
N=4 ± SE
Figure 3-8: Comparison of A: hydraulic permeability and B: dynamic stiffness for
cartilage explants treated in 1mM APMA with and without 4tpM TIMP for 72 hours,
expressed as a percentage of the hydraulic permeability in the APMA and TIMP
samples.
APMA and TIMP: Electromechanical Properties
1.5
Streaming Potential @ 1Hz
D 4 iM TIMP + 1 mM API
S1 mM APMA
*
1
0.5
-F
24
48
72
Electrokinetic Coupling Coefficient
1.2T
108
u.u-i
0.6
0.4
0.2
0
24
48
TIME, hr
72
N=4 ± SE
* p<0.05
Figure 3-9: Electromechanical property measurements for cartilage explants treated
in 1mM APMA with and without 4pM TIMP for 72 hours, expressed as a percentage
of the streaming potential for the APMA and TIMP samples at each time point. A:
Streaming Potential. B: Electrokinetic Coupling Coefficient.
explants with DMB to show the spatial distribution of GAG content and the effect
of transport on degradation. Slides for 72 hours of APMA treatment and 72 hours of
APMA+TIMP are shown in Figure 3-10.
Unfortunately, due to problems with the histology protocol, there is some staining
around the edges of the APMA treated samples which are theoretically free from
GAG. This may be due to thicker tissue at the edges of the sample because of the
slicing technique or some unbound GAG chains which were not washed out of the
sample.
A
B
C
Figure 3-10: Histology samples for cartilage explants in DMEM (A), treated with 1
mM APMA for 72 hours (B) and treated with 1 mM APMA + 4 [pM TIMP for 72
hours (C). The stained regions represent areas of high GAG content, while GAG has
been removed from the unstained areas.
Chapter 4
Modeling the Response of
Degraded Articular Cartilage
Fixed-charge density, water content, PG concentration, hydraulic permeability and
other articular cartilage properties vary with depth in the tissue and location across
a joint [26]. In normal cartilage, these variations are sufficiently small over the dimensions of our experimental samples that a homogeneous model can be used to
predict the response of the tissue to an applied sinusoidal displacement or current
[15]. However, enzymatic degradation can increase the inhomogeneity of the samples:
large molecular weight enzymes which are sterically excluded from the extracellular
matrix will degrade the exposed surface of the tissue more rapidly and to a greater
extent than tissue at the core of the sample. As the GAG chains are cleaved and
diffuse out of the matrix, the intermolecular spacing is increased and the enzyme
can diffuse deeper into the tissue. A 'layered' model has been proposed [19, 13] to
better represent the properties of degraded tissue. It divides the sample into distinct
homogeneous layers with different mechanical and electromechanical properties. The
response of each layer can be calculated from the linearized poroelastic model and
the overall response determined by applying continuous displacement and swelling
stresses at the laver boundaries.
4.1
Theoretical Model Description
This is a summary taken from Frank and Grodzinsky, 1987 [13] of the theoretical
basis for the layered model program. The response of each layer is modeled using
the linearized poroelastic model from Chapter 1. Therefore, we first combine equations 1.1-1.6 to obtain an equation of motion for the uniaxial confined compression
geometry depicted in Figure 2-3.
Substituting equations 1.2 and 1.3 into equation 1.5 gives
Pf
az
=
Oz
HA
02 u(z)4.
082
(4.1)
Solving equation 1.1a for V(z) gives
OV
az1= ke
aP,
J
9Z
k22
(4.2)
and substituting back into equation 1.1b,
U=
+ kJ)
k
(4.3)
where k = kil - (kl 2 k 21/k 22 ), kX= k 21/k 22 , and k = k 12 /k2 2 . Integrating equation 1.4
gives
U = -
Ou +
U
(4.4)
with U0 as the constant of integration representing divergence free fluid flow through
the sample. Finally, combining equations 4.1, 4.3, and 4.4 gives the equation of
motion
Ou
-=
at
02 u
HAk- 2
(9
+
kjJ + Uo
(4.5)
For sinusoidal steady state, displacement can be written as
f
u(z, t) = Re{(i(z,
w)e
w t}
(4.6)
and the equation of motion becomes
(4.7)
jWuiH
= HAk z 2 + kiJ + lJo
in the complex frequency domain. Dropping the '^' notation, for convenience, a
general solution to the equation of motion is
(z) =
where nu
(u= - uj)sinhy(6 - z) + (u' - uj)sinhyz
+ Uj
nh
sinhyd
(4.8)
= u(z = 0) and u0 = u(z = 6) are the top and bottom displacements,
respectively and 9y2 = jW/HAk and uj = (kiJ + Uo)/jw .
With the displacement in equation 4.8, the matrix swelling stress is
-H
uj)coshy(6 - z) - (uO - uj)coshyz
(() =
p(z) = HAsinh
sinhlyb
(4.9)
Writing the pressures at the top and bottom surfaces of each layer results in the
relation
P1
p
= HA Y
cothy6
(-1/sinh.76)
(1/sinhy6)
-cothy6
'U -Zuj
(4.10)
U - Uj
This can be rewritten to give a transfer function relating the parameters for the
top and bottom surfaces
coshy6
HAysinh'y6
(sinhy),/HAyT)
cosh'y6
1
-HAsinhy6
+[
1 - coshy6
Ij
(4.11)
For an n-layer tissue sample, there will be n+1 tissue interfaces with the displacement and swelling forces at the bottom of the ith layer being equal to the forces at
the top of the (i+l)st layer. Thus, for the ith layer
pi-1
U.
Ai'
P
.1
- A']
0
'U
JJ
(4.12)
As the swelling stress and displacement are continuous at the layer boundaries, the
overall relationship for displacement and stress between the top and bottom surface
can be found by multiplying the matrices for all the layers
[
I
n + E [Ii1 -
i]
U
i=1
e
(4.13)
i
where
ni = H
Aj
(4.14)
j=O
and
1 o0 = Ao = I.
(4.15)
In uniaxial confined compression, shown in Figure 2-3, the impermeable electrode
at the bottom of the sample allows no displacement and no fluid flow at this boundary
so uO = u(z = 6) = Un = 0 and Uo = 0. The porous platen at the top of the
sample allows fluid to flow freely so Pf = 0 above the sample. With these boundary
conditions, the total stress from equation 4.13 is
=
o21
1-2)-
12
2
1170
n0
1
(4.16)
- I2)
-I~ (
I21
i=1
The potential drop across each layer can be found by integrating equation 1.1b,
AV = -k•H
u"- - U - UJ
1+ 2Kz,1
KI
tanh
'
7
(4.17)
where k, is defined in equation 4.3 and
KJ =
12 k2 1
-k
-y6kk 22
tanh
7
2
.
(4.18)
For n layers, the total voltage drop is the sum of the voltage drops across each
individual laver
iot = -
"o
"•
.
kH'' i-i
=1
_
-
1 + 2IK]
- Uj1 +2
J
i
tanh 6
2
(4.19)
with the individual ui obtained from equations 4.13 and 4.16.
Under open circuit conditions, with an applied displacement Uapplied, J = 0 so
uj = 0 for each layer and equation 4.16 becomes
a = Acuo
where Ac =
(4.20)
nr
21
However, some of the applied displacement is taken up by the porous platen so the
displacement at the surface of the cartilage is not the same as the applied displacement
(Uapplied
u"3 ). Effectively, the platen acts as a spring in parallel with the cartilage.
The measured stress is therefore
= Acu
\As + Ac
(4.21)
Uapplied
The displacements at each layer can be obtained from equation 4.13:
(i n1
- 1n=1)
UuO
=
i 0pO
(4.22)
which can be simplified to
'a = fi-iuo
-_ ipO
(4.23)
since
(1I-i2-
nII
2
11) = detl
detAi' = 1.
=
(4.24)
j=0
Substituting equation 4.23 into 4.19 and using equation 4.21 to write uO in terms
of Uapplied, we obtain the open circuit streaming potential
As
OC
=-
=H1ae
ke
r i,
Ac + As Uapplied [I
i S -\
6
j
l
-I-
- AC 1-21 +
111)]
tanIh21---1
(4.25)
4.2
Application of the Layered Model
As shown in Figure 4-1, histology of cartilage explants treated with stromelysin (SLN)
shows a 'moving front' of degradation which progresses deeper into the tissue with
time [2], suggesting that these samples could be approximately modeled as layered
rather than uniform.
4.2.1
Initial Parameter Estimation
Based on the histology, we first estimated the model parameters by assuming that
the negatively charged GAG chains were almost completely removed from the outermost layers but that no degradation occurred at the core of the plug. Although
degradation would occur from the entire surface of the sample, and not just from
the top and bottom, we assumed the effect of the side degradation on the stiffness
and streaming potential would be minimal. Therefore, we modeled the samples as
consisting of three layers: completely degraded on the top and bottom but undegraded in the center. The equilibrium confined compression modulus, permeability,
and electrokinetic coupling coefficient values calculated from the streaming potential
and stiffness measurements for untreated and completely degraded (72 hours of 100
pjg/ml SLN treatment) samples using the linearized poroelastic model were used for
the core and degraded layers, respectively.
We determined the thickness of each degraded layer from a combination of histology and GAG loss measurements. After 24 hours of treatment with 100 pg/ml SLN,
GAG was removed from the outer 0.16 mm of the sample, as shown by the unstained
region in Figure 4-1. Assuming an equal degree of degradation at all sides of the
sample, this would correspond to loss of about 45% of the total GAG in the sample.
This agrees with similarly treated samples analyzed for GAG content by DMB assay
(see Methods) which lost an average of 50% of total GAG. In addition, the GAG
loss curve in Figure 4-2 can be approximated as an exponential decay with a time
constant of 26 hours. Equating the percent volume of the undegraded layer with the
•
...
~..........
Figure 4-1: Light micrographs of cartilage disks incubated in DMEM alone for 72
hours (top) and DMEM with 100 fg/ml SLN for 24 hours (bottom), represented at
100X. SLN treatment resulted in an apparent front of enzymatic degradation moving
inward from all exposed specimen surfaces, shown by the absence of toluidine blue
stain for GAG. Adapted from [2].
Stromelysin Induced GAG Loss
a)
0
1-
,DMEM
0 0.8U) 0.6-
0.4N
0.2-
U-
100 SLN
E
L0
Z 00
TIME, h 48
24 TIME,
72
Figure 4-2: Normalized GAG loss from cartilage disks incubated in DMEM with and
in DMEM with 100 pg/ml recombinant human stromelysin-1 (SLN) Data are mean +
SD (n=4), reported as GAG remaining in the tissue normalized to total GAG (tissue
+ media GAG) at each time point. Solid lines are best fit singles exponential decay
curves of the form le - t /'. The best fit decay time for 100 pg/ml SLN is 7=26, and
7=1019 hr for DMEM alone. Adapted from [2].
Time (hrs) Layer 1 (mm)
24
0.225
48
0.36
72
0.44
Layer 2 (mm)
0.55
0.28
0.12
Layer 3 (mm)
0.225
0.36
0.44
Table 4.1: Layer thickness for the initial layered model parameters. Layers 1 and 3
were modeled as completely degraded with HA = 0.089, k = 16.2, and ke = 3. Layer
2 was modeled as undegraded with HA = 0.89, k = 1.08, and ke = 4.
percent GAG remaining in each sample
7r(r
- x)2(t- 2x) = et/'irr2
(4.26)
where r = radius of sample = 1.5mm, t = thickness of sample = 1mm, and x=depth
of degradation, we obtained degraded layer thicknesses of 0.2mm at 24 hours, 0.35mm
at 48 hours, and 0.45mm at 72 hours. Since the GAG loss thickness estimates were
similar to the histology based estimates but were available for all three time points,
we used the GAG loss thickness estimates for the initial layer thicknesses. Table 4.1
summarizes the model parameters used to produce the primary layered model streaming potential and dynamic stiffness responses for a 1% displacement, shown in Figures 4-3 and 4-4. These theoretical estimates show poor agreement with the measured
responses.
4.2.2
Linearized GAG Loss Profile
Although the histological data for these explants showed a 'moving front' of degradation which progressed with increasing exposure to the stromelysin, analysis of the
variation in GAG content with depth in tissue for trypsin digested cartilage as shown
in Figure 4-5 suggests that the dye used for histological staining is subject to a threshold effect and the degradation is in fact much more gradual [1].
Assuming that the GAG loss for SLN treated samples is also gradual, we increased
the number of layers for the model and gradually increased the degree of degradation
from the outermost to innermost layers. We assumed similar layer thicknesses for
Streaming Potential: Measured vs 3-layer model
0.35
0.28
0.21
0.14
0.07
0
0.O
~AA
I UU
-
r-
75
,
I-
_
_
50
u.
_,
a,
25
-24
0)
0
CLI
=
w
1o
a.
zcn
0.
-25
24
-50
~ ...
,
"
i
.....
--
i
...
.. ...
.
I
_79
0.0 01
0.01
0.1
SFREQUENCY, Hz
Figure 4-3: Layered model streaming potential magnitude and phase for completely
degraded and undegraded layers. Data from 100pg/ml SLN treated cartilage is shown
in the background (squares 0 hours of treatment, circles = 24 hours, stars = 48 hours,
and triangles = 72 hours of treatment).
Eng Stiffness: Measured vs 3-layer model
12.5
-
i
10
.r
7.5
-•7
-I
5
'IP
2.5
48, 72-hours
24 hours
A
0.0 01
0.01
0.1
50
40
30
20
10
0
0.001
0.01
0.1
FREQUENCY, Hz
Figure 4-4: Layered model dynamic stiffness magnitude and phase for completely
degraded and undegraded layers. Data from 100pg/ml SLN treated cartilage is
shown in the background (squares 0 hours of treatment, circles = 24 hours, stars
48 hours, and triangles = 72 hours of treatment).
57
5
B
4
C)
2
0
O
O
0
1
2
3
Depth into Tissue (mm)
Figure 4-5: GAG content versus depth into tissue for trypsin treated cartilage cores
(mean + SEM). For clarity, curves are plotted only until the depth at which GAG
content approxiamtely equals normal levels.
Layer
1
2
3
4
5
A. 24 hours
Thickness (mm) HA
0.1
0.75
0.1
0.80
0.6
1.00
0.1
0.80
0.1
0.75
Layer
1
2
3
4
5
6
7
Thickness (mm)
0.1
0.1
0.15
0.3
0.15
0.1
0.1
Layer
1
2
3
4
5
6
7
Thickness (mm)
0.1
0.1
0.15
0.3
0.15
0.1
0.1
k
1.50
1.25
1.00
1.25
1.50
ke
2.0
3.0
4.0
3.0
2.0
k
15.0
10.0
5.0
1.0
5.0
10.0
15.0
ke
2.0
2.5
3.0
4.0
3.0
2.5
2.0
k
15.0
10.0
7.0
5.0
7.0
10.0
15.0
ke
B. 48 hours
HA
0.10
0.20
0.50
1.00
0.50
0.20
0.10
C. 72 hours
HA
0.10
0.20
0.40
0.50
0.40
0.2
0.1
2.0
2.5
3.0
3.0
3.0
2.5
2.0
Table 4.2: Optimal layered model parameters to fit streaming potential and dynamic
stiffness data from cartilage explants treated with 100 pg/ml SLN for 24, 48 and 72
hours.
the penetration depth of the SLN but reduced the amount of degradation for each
layer. In addition, we assumed that the loss of GAG and subsequent softening of the
superficial cartilage increased the amount of interdigitation between the upper layer
of cartilage and the porous platen, effectively decreasing the interfacial stiffness for
the model. The optimal model parameters are given in Table 4.2 and the resulting
dynamic stiffness response is shown in Figure 4-6 and the streaming potential curves
are in Figure 4-7.
After 48 hours of SLN treatment, we assumed that the degradation had increased
in the outermost layers and that deeper layers of tissue had also started to be de-
graded. However, as the linearized poroelastic model estimates of the modulus, permeability and electrokinetic coupling coefficient for 72 hours of SLN treatment were
still averages for nonhomogeneous tissue, we assumed that the amount of degradation in the outermost layers was actually more than that suggested by the 72 hour
estimates, thus we used a higher value for the permeability and lower values for the
modulus and coupling coefficient. We decreased the interfacial stiffness in proportion ( 90% to 1 MPa) to the percent decrease in modulus and percent increase in
permeability.
Finally, after 72 hours of treatment, we assumed that the SLN had at least partially
degraded the entire plug. The outermost layers were not degraded further from the
loss after 48 hours but some GAG was removed from the innermost layers. As the
streaming potential and dynamic stiffness measurements are mainly sensitive to the
GAG content in the outermost layers of the sample, the curves were largely unchanged
from the levels at 48 hours.
As the data shows, the agreement between measured stiffness magnitude and the
theoretical estimate is very good. Qualitatively, the predicted phase also agrees with
the measured values, though the model values are somewhat lower than expected.
The model output for both the 48 hour and 72 hour streaming potential curves
is lower than the measured signals for frequencies below 0.01 Hz. However, these
measurements are noisy, with large variations in phase, so they may not be extremely
reliable. For frequencies higher than 0.01 Hz, were the phase signal is much less noisy,
both magnitude and phase are in good agreement with the measured values.
Eng Stiffness: Measured vs Layered Model
12.5
10
7.5
5
2.5
n
0.001
0.1
1
0.01
0.1
FREQUENCY, Hz
1
0.01
40
30
20
10
n
0.001
Figure 4-6: Layered model dynamic stiffness magnitude and phase for gradually degraded cartilage using the optimal model parameters. The measured response for
cartilage treated with 100 pg/ml SLN is shown in the background (squares = 0 hours
of SLN treatment, circles = 24 hours, stars = 48 hours and triangles = 72 hours of
SLN treatment).
61
Streaming Potential: Measured vs Layered Model
0.35
0.28
0.21
0.14
0.07
0
0001
100
75
50
25
0
-25
-50
-75
0.001
0.01
0.1
.. FREQUENCY, Hz`
1
Figure 4-7: Layered model streaming potential magnitude and phase for gradually
degraded cartilage using the parameters from Table 2. The measured response for
cartilage treated with 100 pg/ml SLN is shown in the background (squares = 0 hours
of SLN treatment, circles = 24 hours, stars = 48 hours and triangles = 72 hours of
SLN treatment).
62
Chapter 5
Discussion
5.1
Metalloproteinase Inhibitor Experiments
Chapter 3 describes the results from a series of experiments on the ability of three
types of metalloproteinase inhibitors to prevent or block the degradation of cartilage
induced by APMA-activation of endogenous enzymes. The presence of large quantities of inactive metalloproteinases in normal cartilage suggests that chondrocytes
play a key role in the balance of ECM degradation and synthesis by controlling the
amounts of inactive enzymes and natural inhibitors. A shift in this balance towards
increased active metalloproteinases would lead to excess metalloproteinase degradation and could result in significant tissue degradation like that in OA. Addition of
exogenous metalloproteinase inhibitors has been suggested as a potential method of
preventing additional ECM degradation in patients with OA [38].
Previous studies [2] have shown that addition of 4pM exogenous TIMP-1 to the
culture media of 1 mM APMA treated cartilage explants is capable of fully preventing
GAG loss from the tissue. The results in Chapter 3 show that addition of TIMP-1 also
prevents the decrease in streaming potential and dynamic stiffness seen with 1 mM
APMA treatment. These results suggest that exogenously added TIMP-1 is capable of
inhibiting the change in physical properties induced in cartilage explants treated with
APMA, and maintaining a physically viable tissue which can perform its mechanical
function.
In addition, the physical property measurements for 1mM APMA and
1mM APMA with 4 piM TIMP-1 show very little variation with frequency. This
is consistent with the histology sections and theoretical predictions of homogeneous
degradation with 1mM APMA and only a small amount of degradation in the center
of the 1mM APMA and 4 pM TIMP explants since the streaming potential and
stiffness measurements are most sensitive to surface degradation, especially at lower
frequencies. If the physical property measurements varied greatly with frequency, it
would suggest that the tissue GAG content also varied significantly with depth. It
would be useful to redo the histology samples of APMA and APMA with TIMP1 treated explants to eliminate the edge effects and verify the predicted GAG loss
patterns of almost complete GAG loss in the samples with APMA (very pale samples),
and GAG loss only in the center of TIMP treated explants (dark around the edges
and light in the center).
Doxycycline and other members of the tetracycline family have been shown to
inhibit collagenase in vitro but their effect in long term clinical trials has not been
significant.
Furthermore, their ability to inhibit other metalloproteinases, such as
stromelysin, is not well documented, with conflicting examples in the literature [3, 7].
As these drugs are FDA approved for patient use as antibiotics, some patients are
already receiving tetracycline type drugs as treatment for their OA [38]. Therefore,
it is important to determine if these drugs are capable of preventing cartilage degradation in vivo and if so, what levels of the drug are needed in the tissue, and how
the drug should be administered. As shown in Section 3.2, 30 pM doxycycline did
not prevent proteoglycan loss from the cartilage explants with endogenous metalloproteinases activated by 1 mM APMA. The collagen assays (hydroxyproline and
swelling) did not show any significant loss in collagen from control (APMA alone)
samples, so no change was expected with additional doxycycline. In the near future,
it would be useful to try another doxycycline experiment with higher concentrations
to see if there is any GAG loss inhibition and to continue the treatment for 6 or 8
days to allow control samples to lose significant collagen and to see if the doxycycline
inhibited the collagen loss. In particular, it would be useful to determine the effects
of doxycycline in the APMA system because APMA blocks the biosynthetic activity
of the cells so the non-cell mediated effects can be determined. It would also be useful
to measure the effectiveness of tetracycline derivatives in the IL-10 and retinoic acid
systems in which the cells are active.
We tested the ability of n-carboxyalkyl compounds, such as MC 354, to inhibit
cartilage degradation in the APMA system. These compounds are much smaller
than natural inhibitors like TIMP-1 and should be able to freely diffuse into the
tissue. Therefore, they may be as effective as TIMP at similar doses, despite their
reduced potency. As with other n-carboxyalkyl compounds [2], MC 354 inhibited
GAG loss from cartilage explants in a dose dependent manner, with 2.0 Jpg/ml being
sufficient to completely inhibit GAG loss from explants treated with 1mM APMA
for 3 days.
Thus, these types of drugs are potentially important alternatives for
slowing or preventing metalloproteinase induced cartilage degradation in patients
with OA. In addition to the VDIPEN fragments (corresponding to the SLN cleavage
site) identified in synovial fluid of patients with OA, additional NITEGE fragments
which correspond to an as yet unidentified proteinase termed 'aggrecanase' are also
present. Since some of the physiological metalloproteinase inhibitors, such as TIMP1, are also effective at blocking the degradation of cartilage, it is possible that the
proteinase which cleaves aggrecan at 373-374 (producing NITEGE) fragments is also a
metalloproteinase (or can be activated by an MMP). Therefore, 'aggrecanase' activity
may also be affected in part by these compounds. This suggests that the most effective
metalloproteinase inhibitor for preventing overall ECM degradation may be a more
general inhibitor, rather than one that is 'tuned' to inhibit a specific metalloproteinase
such as stromelysin. The validity of such an hypothesis could be tested using the
biochemical and biophysical methods described here.
5.2
Layered Model
The linear poroelastic model can be used to estimate the hydraulic permeability,
equilibrium modulus, and kinetic coupling coefficient from streaming potential and
dynamic stiffness measurements. However, histology of explants treated with trypsin
and stromelysin suggests that these degraded tissues are significantly nonhomogeneous and may be better modeled by separating them into layers. Initial simple
estimates based on almost complete degradation in exposed tissue and virtually no
degradation in the core of the samples did not appear to accurately represent the
physical properties of the tissue. However, further analysis of the GAG content of
trypsin treated samples showed that despite the moving front appearance of the histology of these explants, the GAG loss appears to be a more continuous function of
depth and the misleading image of the histology may be due to a threshold effect
of the stain. Based on this data, we used a model with a more gradual change in
tissue parameters and more layers which was much more representative of the tissue
properties and function.
Since the GAG analysis was done with trypsin treated plugs but there was no
physical property assessment of these explants, we used the SLN treatment measurements for the modeling. In the future, it would be useful to test the layered model
by treating plugs with SLN and doing a similar GAG analysis with depth as well as
physical property measurements and use this data as the basis for the layered model
parameters.
Ultimately, it may be possible to predict the extent of GAG loss from full thickness
tissue samples based on the best layered fit of the physical parameters to streaming
potential and dynamic stiffness measurements. Furthermore, layered model predictions for the overall tissue electrokinetic coupling coefficient, equilibrium modulus
and hydraulic permeability may be more accurate for certain tissue treatments, and
even untreated cartilage samples, than the linear poroelastic model predictions. It
is important to determine when a layered model approach is necessary and when a
homogeneous tissue approximation would be sufficient to describe the tissue parameters.
Appendix A
Charged Inhibitors
A.1
Introduction
Cartilage ECM has a highly negative fixed charge density which is partly responsible for the ability of the tissue to resist compression. Many of the n-carboxylalkyl
inhibitors are also charged which may increase or decrease the ability of these compounds to enter the tissue. We tested the effectiveness of three different inhibitors
with approximately the same efficacy in vitro in inhibiting stromelysin and collagenase but with neutral, positive and negative charges. We hypothesized that the
negatively charged molecule might be partially excluded from the tissue by the negatively charged PGs and that the postively charged inhibitor would have an increased
concentration inside the ECM.
A.2
Methods
As with the other inhibitor studies, cartilage explants were incubated in DMEM with
1 mM APMA to activate and the endogenous metalloproteases with and without
the three inhibitors at 2 pg/ml 1. Plugs were removed at 24, 48 and 72 hours and
hydration and GAG assays were performed on them, as described in Chapter 2.
1The positively charged inhibitor was dissolved in DMSO so the media for this condition also
contained 0.01% DMSO.
A.3
Results and Discussion
Figure A-1 shows the relative levels of GAG loss for each condition. None of the
inhibitors had significantly different results. The trends suggest that both positively
and negatively charged inhibitors are better able to enter the cartilage ECM; however,
the stromelysin Ki values for both charged species are slightly lower than the Ki for
the neutral inhibitor, so the results seem to be affected more by the slight variations
in the efficacy of the inhibitors than in their charge. A more conclusive study might
use inhibitors which had closer Kis.
Charged Inhibitors GAG Loss
<
1
i
D 0.8
Cl)
0.6
N
0.4
nz 0.2
0
I IMl,
nr
N=4 ± SD
Figure A-1: Normalized GAG loss for cartilage explants incubated in DMEM, DMEM
+ 1 mM APMA. DMEM + APMA + 2.0 pg/ml MC068 (+), DMEM + APMA +
2.0 pg/ml MC044 (0), and DMEM + APMA + 2.0 pg/ml MC069 (-). Data are
mean±SD and n=4.
Bibliography
[1] S I Berkenblit.
Nondestructive Detection of Cartilage Degeneration Using
ElectromechanicalSpectroscopy. PhD thesis, MIT, 1995.
[2] L J Bonassar, E H Frank, J C Murray, C G Paguio, V L Moore, M W Lark, J D
Sandy, J-J Wu, D R Eyre, and A J Grodzinsky. Changes in cartilage composition
and physical properties due to stromelysin degradation. Arth and Rheum, page
in print, 1995.
[3] T S Burris, K Huch, M VOrth, K E Kuettner, and A A Cole. The effects of doxycycline on gelatinase a and b in human cartilage explant culture of metatarsals.
Transactions of the ORS, 20, 1995.
[4] D J Buttle, C J Handley, M Ilic, J Saklatvala, and A J Barrett. Inhibition of
cartliage proteoglycan release by a specific inactivator of cathepsin B and an
inhibitor of matrix metalloproteinases. Evidence for two converging pathways
of chondrocyte-mediated proteoglycan degradation. Arth Rheum, 36:1709-1717,
1993.
[5] S L Carney, M E J Billingham, H Muir, and J D Sandy. Structure of newly
synthesised ( 5s)-proteoglycans and (35s)-proteoglycan turnover products of cartilage explant cultures from dogs with experimental osteoarthritis. J Orthopaedic
Research, 3:140-147, 1985.
[6] K T Chapman, I E Kopka, P L Durette, C K Esser, T J Lanza, M IzquierdoMartin. L Niedzwiecki. B Chang, R K Harrison, D W Kuo, T-Y Lin, R L Stein,
and W K Hagmann. Inhibition of matrix metalloproteinases by n-carboxyalkyl
peptides. J Medicinal Chemistry, 36:4293-4301, 1993.
[7] A A Cole, X-W Xi, K E Kuettner, L M Golub, and R A Greenwald. The effect
of chemically modified tetracyclines on cartilage degradation in chicken tibial
explants. Trans Orth Res Soc, 20, 1995.
[8] B Davies, P D Brown, N East, M J Crimmin, and F R Balkwill. A synthetic
matrix metalloproteinase inhibitor decreases tumo burden and prolongs survival
of mice bearing human ovarian carcinoma xenografts. CancerRes, 53:2087-2091,
1993.
[9] D D Dean, J Martel-Pelletier, J-P Pelletier, D S Howell, and F Woessner. Evidence for metalloproteinase and metalloproteinase inhibitor imbalence in human
osteoarthritic cartilage. J Clin Invest, 84:678-685, 1989.
[10] D R Eyre, C A McDevitt, M E J Billingham, and H Muir. Biosynthesis of collagen
and other matrix proteins by articular cartilage in experimental osteoarthritis.
Biochem. J, 188:823-837, 1980.
[11] R W Farndale, D J Buttle, and A J Barrett. Improved quantitation and discrimination of sulphated glycosaminoglycans by use of dimethylmethylene blue.
Biochim Biophys Acta, 883:173-177, 1986.
[12] D T Felson. Osteoarthritis. Rheum Dis Clin N Amer, 16(3):499-512, 1990.
[13] E H Frank. Electromechanics of Normal and Degenerated Cartilage: Poroelastic
Behavior and Electrokinetic Mechanisms. PhD thesis, MIT, 1987.
[14] E H Frank and A J Grodzinsky. Cartilage electromechanics I: Electrokinetic
transduction and the effects of electrolyte pH and ionic strength. J Biomechanics,
20:615-627, 1987.
[15] E H Frank and A J Grodzinsky. Cartilage electromechanics II: A continuum
model of cartilage electrokinetics. J Biomechanics, 20:629-639, 1987.
[16] E H Frank, A J Grodzinsky, S L Phillips, and P E Grimshaw. Physicochemical
and Bioelectrical Determinants of Cartilage Material Properties, pages 261-282.
Springer-Verlag New York Inc, 1990.
[17] R A Greenwald, S A Moak, N S Ramamurthy, and L M Golub. Tetracyclines
suppress matrix metalloproteinase activity in adjuvant arthritis and in combination with flurbiprofen ameliorate bone damage. J Rheumatology, 19:927-938,
1992.
[18] A J Grodzinsky. Electromechanical and physicochemical properties of connective
tissues. CRC Crit Rev Biomed Eng, 9:133-199, 1983.
[19] A J Grodzinsky and E H Frank. Electromechanical and physicochemical regulation of cartilage strength and metabolism. In D Hukins, editor, Connective
Tissue Matrix II, pages 91-126. MacMillan, London, 1990.
[20] T E Hardingham, A J Fosang, and J Dudhia. Aggrecan, the chondroitin/keratan
sulfate proteoglycan from cartilage, pages 5-20. Raven Press Ltd., New York,
NY, 1992.
[21] D S Howell. Pathogenesis of osteoarthritis. Am J Med, 80:24-28, 1986.
[22] E B Hunziker, A Ludi, and W Herrmann.
Preservation of cartilage matrix
proteoglycans using cationic dyes chemically related to ruthenium hexaammine
trichloride. J Histochemistry and Cytochemistry, 40:909-917, 1992.
[23] G E Kempson, M A Tuke, J T Dingle, A J Barrett, and P H Horsfield. The effects
of proteolytic enzymes on the mechanical properties of adult human articular
cartilage. Biochim Biophys Acta, 428:741-760, 1976.
[24] M W Lark, L A Walakovits, T K Shah, J VanMiddlesworth, P M Cameron, and
T Y Lin. Production and purification of prostromelysin and procollagenase from
il-1 beta stimulated human gingival fibroblasts. Conn Tiss Res, 1990.
125] L S Lohmander, L A Hoerrner, and M W Lark. Metalloproteinasees, tissue inhibitor, and proteoglycan fragments in knee synovial fluid in human osteoarthritis. Arthritis Rheum, 36(2):181-189, 1993.
[26] A Maroudas. Physicochemical properties of articular cartilage. In M A R Freeman, editor, Adult Articular Cartilage, pages 215-290. Pitman Medical, Kent,
England, 1979.
[27] H Nagase, J J Enghild, K Suzuki, and G Salvesen. Stepwise activation mechansims of the precursor of matrix metalloproteinase 3 (stromelysin) by proteinases
and (4-aminophenyl)mercuric acetate. Biochem, 29(24):5783-5789, 1990.
[28] Q Nguyen, G Murphy, P J Roughy, and J S Mort. Degradation of proteoglycan
aggregate by a cartilage metalloprotease. Biochem J, 259:61-67, 1989.
[29] Y Okada, N Takeuchi, K Tomita, I Nakanishi, and H Nagase. Immunolocalisation
of matrix metalloproteinase 3 (stromelysin) in rheumatoid synovioblasts (b cells):
correlation with rheumatoid arthritis. Annal Rheum Dis, 48:645-653, 1989.
[30] C G Paguio. Effects of endogenous and exogenous metalloproteases on articular
cartilage explants: Relevance to osteoarthritis. Master's thesis, Massachusetts
Insititute of Technology, EECS, 1993.
[31] J-P Pelletier, F Mineau, M-P Faure, and J Martel-Pelletier. Imbalance between
the mechanisms of activation and inhibition of metalloprteases in the early lesions
of experimental osteoarthritis. Arthritis Rheum, 10:1466-1476, 1990.
[32] R L Sah, Y J Kim, J Y H Doong, A J Grodzinsky, A H K Plaas, and J D Sandy.
Biosynthetic response of cartilage explant to dynamic compression. J Orthopaedic
Research, 7:619-636, 1989.
[33] J D Sandy, C R Flannery, P J Neame, and L S Lohmander. The structure of
aggrecan fragments in human synovial fluid. J Clin Invest, 89:1512-1516, 1992.
[34] M P Seed, S Ismaiel, C Y Cheung, T A Thomson, C R Gardner, R M Atkins,
and C J Elson. Inhibition of interleukin-1 beta induced rat and human cartilage
degradation in vitro by the metalloproteinase inhibitor u27391. Ann Rheum Dis,
52:37-43, 1993.
[35] M Skinner, E S Cathcart, J A Mills, and R S Pinals. Tetracycline in the treatment
of rheumatoid arthritis: a double blind controlled study. Arth Rheum, 14:727732, 1971.
[36] H Stegemann and K Stalder. Determination of hydroxyproline. Clinica Chimica
Acta, 18:267-273, 1967.
[37] L Stryer. Biochemistry. Freeman and Company, New York, 1988.
[38] M P Vincenti, I M Clark, and C E Brinckerhoff. Using inhibitors of metalloproteinases to treat arthritis. Arth Rheumr, 37(8):1115-1126, 1994.