Advances in robot-assisted gait training at UD
advertisement

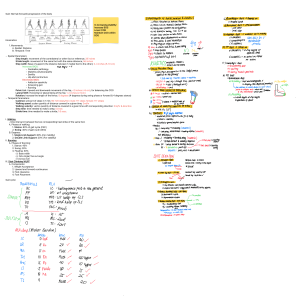
Advances in robot-assisted gait training at UD Stroke is the leading cause of adult disability in the United States with a yearly incidence greater than 750,000, and stroke survivors typically have walking impairments that not only limit function but increase the risk of falls and associated morbidities. Therefore, the development of novel approaches to better improve walking is important. This ongoing preliminary study reports the results of an initial test of a robotic-assisted gait training (RAGT) procedure with healthy individuals, as well as the results of a preliminary training experiment with one patient two years post left CVA. The purpose of the first experiment was to determine whether the principles underlying our application of RAGT could be supported initially in non-neurologically impaired individuals. We sought to determine if healthy subjects could adapt their normal sagittal plane foot trajectory to a scaled-down version and to determine if this adaptation could be retained for a period of time after training, including following periods of over ground walking. Two groups of ten subjects were trained in six 10-min blocks in one experimental session. Subjects in both groups received continuous visual feedback about their foot trajectory and the prescribed trajectory, which they tried to match. Ten subjects in the experimental group walked with soft elastic constraints (virtual tunnel) applied to constrain the foot trajectory, which resisted large deviations from the prescribed foot path. The width of the path and elasticity of the virtual walls were adjusted across training sessions. Treadmill walking performance during unconstrained walking without visual feedback was evaluated between each training block, immediately after training, after 10-min of additional over ground walking and two hours later. Results of the study with healthy subjects revealed adaptation of their foot trajectory to the scaled-down trajectory, whether receiving constraints or not. However, subjects practicing with the additional foot constraints performed better post-training. Subjects retained the altered pattern for short periods of time even after intervening periods over ground walking, although the trajectory began to approximate their normal pattern by 2 hours post-training, as expected. Changes in joint motion seemed to be better maintained. The results suggested a similar paradigm applied over more extended periods of training might help people with gait disorders improve their gait pattern. Thus, we initiated a preliminary study of gait training using a similar paradigm with one patient with right hemiparesis due to a stroke. This patient was trained for five days in eight five-minute bouts of walking on each day. The patient initially received continuous visual feedback about his foot path as well as a specified foot path template based on a healthy subject with similar leg lengths. The magnitude of the foot constraint was varied across blocks of training. Visual feedback was eliminated for periods during the latter days of training to facilitate better self evaluation. The patient showed improvements in over ground gait speed, TUG score and Dynamic Gait Index following the five days of training. Further evaluation of gait changes is currently underway. The results support the potential of this approach to gait re-training after stoke even in patients several years post-CVA.