Effects of Salt Sensitivity on Neural Cardiovascular Regulation in Essential Hypertension
advertisement

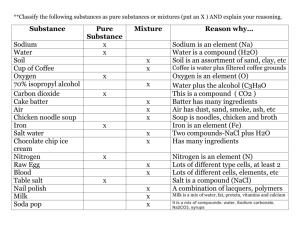
Effects of Salt Sensitivity on Neural Cardiovascular Regulation in Essential Hypertension Paolo Coruzzi, Gianfranco Parati, Lorenzo Brambilla, Valerio Brambilla, Massimo Gualerzi, Almerico Novarini, Paolo Castiglioni, Marco Di Rienzo Abstract—Salt-sensitive hypertensive subjects, as defined by conventional categorical classification, exhibit alterations of autonomic cardiovascular control. The aim of our study was to explore whether, in hypertensive subjects, the degree of autonomic dysfunction and the level of salt sensitivity are correlated even when the latter is only mildly elevated and displays under-threshold values. Salt sensitivity of 34 essential hypertensive subjects was assessed on a continuous basis by the salt sensitivity index after low- and high-sodium diet. Beat-by-beat finger blood pressure was recorded after each diet period. Autonomic cardiovascular control was evaluated by spectral analysis of blood pressure and pulse interval and by assessment of spontaneous baroreflex sensitivity (sequence technique). Salt sensitivity and baroreflex sensitivity showed a negative relationship during low and high sodium intake, starting from low values of the salt sensitivity index. All spectral indexes of pulse interval, except the ratio between low- and high-frequency powers, were inversely related to salt sensitivity index after high sodium intake. In subjects with lower salt sensitivity, baroreflex sensitivity and pulse interval power in the high-frequency band were higher after high sodium intake than after low sodium intake. In contrast, subjects with a higher salt sensitivity index showed lower values of baroreflex sensitivity and pulse interval power in the high-frequency band, uninfluenced by salt intake. Our results provide the first demonstration of an impairment of parasympathetic cardiac control in parallel with the increase in the degree of salt sensitivity, also in subjects who were not ranked as salt-sensitive by the conventional categorical classification. (Hypertension. 2005;46:1-6.) Key Words: autonomic nervous system 䡲 heart rate 䡲 baroreflex 䡲 blood pressure 䡲 sodium, dietary T he higher rate of cardiovascular events occurring in salt-sensitive subjects, either normotensive or hypertensive, has led to the suggestion that a salt sensitivity condition might represent an independent cardiovascular risk factor.1,2 An enhanced sympathetic cardiovascular drive has been suggested to play a role in determining the increased cardiovascular risk associated with salt sensitivity. In fact, an impaired sympathetic inhibition has been described during high sodium intake in salt-sensitive hypertensive humans,3 and a deranged reflex cardiovascular control has been proposed as one of the responsible mechanisms.4,5 Usually, salt sensitivity is considered a categorical parameter, with salt-sensitive individuals being defined as those with a difference in mean arterial pressure (MAP) between low- and high-sodium diet ⬎10%, and salt-resistant subjects those in whom MAP does not increase or shows an increase ⬍5% under sodium loading.6 – 8 However, adoption of this categorical approach does not allow exploring whether an impairment of cardiovascular autonomic regulation may occur also in subjects with salt-related blood pressure (BP) changes smaller than those defining salt sensitivity. In the present study, we specifically addressed the above open issue by investigating whether signs of an autonomic dysfunction are detectable in mild hypertensive subjects with under-threshold salt sensitivity values. To this aim, we explored the transition between salt resistance and frank salt sensitivity in a continuous fashion, making use of a relatively new index, proposed by Kimura and Brenner9 and previously used by Coruzzi et al10 for quantification of salt sensitivity. This index, called salt sensitivity index (SSI), relates the changes in BP induced by sodium loading with the concomitant changes in urinary sodium output without any arbitrary definition of threshold levels. Methods Subjects The study included 34 outpatients (21 men and 13 women) with a never- treated mild or moderate uncomplicated essential hypertension, and with repeated office auscultatory diastolic BP (DBP) measurements, in the seated position, between 95 and 109 mm Hg. The patients had neither a history nor physical or laboratory evidence of cardiovascular disease. They were free from target organ damage Received May 16, 2005; first decision June 2, 2005; revision accepted August 23, 2005. From the Department of Clinical Sciences (P.C., A.N.), University of Parma, Italy, and Fondazione Don C. Gnocchi ONLUS, Parma, Italy; Prevention and Rehabilitation Unit (L.B., V.B., M.G.,), Fondazione Don C. Gnocchi ONLUS, Parma, Italy; Department of Clinical Medicine, Prevention, and Applied Biotechnologies (G.P.), University of Milano-Bicocca and S. Luca Hospital, IRCCS, Istituto Auxologico Italiano, Milan, Italy; and Centro di Bioingegneria (P.C., M.D.), Fondazione Don C. Gnocchi ONLUS, Milan, Italy. Correspondence to Marco Di Rienzo, Centro di Bioingegneria, Fondazione Don C. Gnocchi, via Capecelatro 66, I-20148 Milano, Italy. E-mail mdirienzo@cbi.dongnocchi.it © 2005 American Heart Association, Inc. Hypertension is available at http://www.hypertensionaha.org DOI: 10.116110.1161/01.HYP.0000189183.50301.5c 1 2 Hypertension December 2005 at the heart level as assessed by echocardiography. Renal disease was excluded by normal urinalysis and creatinine clearance. Subjects under concomitant treatment with estrogens or nonsteroidal antiinflammatory agents, or with drugs known to influence salt, potassium, calcium, water, hemodynamic, or neural regulation, were excluded. Subjects were nonsmokers with body mass index of 24.8⫾3 kg/m2, 45⫾7 years of age, sedentary lifestyle, and no history of excessive alcohol consumption. Measurements Before starting the controlled sodium diets, we determined serum and urinary sodium and creatinine concentrations (Technicon analyzer). The 24-hour ambulatory BP was monitored by an oscillometric automated device (Spacelabs model 90207) to quantify baseline 24-hour systolic BP (SBP), DBP, MAP, and heart rate (HR) average values and SDs. The inflatable cuff was wrapped around the nondominant arm after excluding between-arm differences in BP ⬎5 mm Hg. The accuracy of the oscillometric device was assessed in each patient by comparison with 3 auscultatory readings simultaneously taken from the same arm with a Y-tube connection between the Spacelabs device pump and a mercury column. Salt Sensitivity Assessment According to a method described previously,11 after the baseline assessment, the 34 hypertensive patients followed either a highsodium (200 mmol NaCl per day) and a low-sodium (30 mmol NaCl per day) diet for 1 week in a randomized sequential order. The 24-hour urinary sodium excretion was quantified on the last day of each diet week. This measure was also used to verify the patients’ compliance with the dietary regimen. Compliance with caloric intake was controlled through repeated phone calls aimed at ensuring that patients were following a diet with the prescribed caloric content. The degree of salt sensitivity was estimated as follows: after overnight fasting, at 7:30 AM on days 7 and 14 (ie, at the end of each diet period), patients came to our laboratory, where they remained quietly seated for 150 minutes. After a 30-minute period of familiarization with the environment, SBP, DBP, MAP, and HR were measured at 15-minute intervals over the following 2 hours, from 8:00 to 10:00 AM, by the Spacelabs automated device. Simultaneously, continuous finger BP and HR were monitored by a Portapres model-2 device (Finapres Medical Systems), the finger cuffs of which were wrapped around the mid- and the ring fingers of the hand contralateral to the arm carrying the Spacelabs cuff and were always kept at heart level throughout the recording time. During the recording, subjects were asked to avoid sudden changes in respiratory rate, which remained ⬇12 to 15 breaths per minute. The SSI was calculated as the ratio of the change in brachial oscillometric MAP (⌬MAP), expressed in mm Hg, between the high- and the low-sodium diet periods, with the corresponding change in urinary sodium excretion rate (⌬UNaV) expressed in mmol/L per day, multiplied by a factor of 1000 to facilitate readability of results, namely: SSI⫽(⌬MAP/⌬UNaV)⫻1000 [mm Hg/(mol/L per day)]. The experimental protocol was approved by the ethical committee of our institution, and the patients gave their written informed consent after having received a detailed explanation of the study procedures and purposes. Analysis of Continuous BP Recordings Beat-by-beat SBP, DBP, and MAP values were identified from the 2-hour finger arterial BP recordings performed at the end of each dietary regimen. The heart interval was computed as pulse interval (PI; ie, the time interval between consecutive systolic peaks, after their parabolic interpolation to increase the accuracy of the estimate). After removal of artifacts and ectopic beats, mean values and SDs of SBP, DBP, MAP, and PI were calculated from each recording. Spontaneous arterial baroreflex sensitivity (BRS) was estimated by the sequence technique.12,13 SBP and PI beat-by-beat series were scanned searching for sequences of ⱖ3 consecutive heart beats in which a progressive increase in SBP values was followed, with lags ranging from 0 to 2 beats, by a progressive PI lengthening or, vice versa, in which a progressive SBP decrease was followed by a progressive PI shortening. The slope of the regression line between SBP and PI values included in each sequence was taken as an estimate of BRS. The baroreflex effectiveness index (BEI) was computed as the ratio between the number of SBP–PI sequences and the total number of SBP progressive changes14 to quantify how often the baroreflex takes the control of the sinus node in response to BP transients. SBP and PI beat-by-beat series were interpolated and resampled at 10 Hz for the spectral analysis. Fast Fourier transform power spectra were computed over consecutive, 50% overlapped, 300-s Hann data windows. For each subject, a final spectrum was estimated by averaging the spectra computed over the whole recording. Each spectrum was integrated over low-frequency (LF; 0.04 to 0.15 Hz) and high-frequency (HF; 0.15 to 0.40 Hz) bands. The PI HF power is an indirect measure of vagal cardiac modulation,4 whereas the LF/HF ratio of PI powers is taken as a measure of the sympatho-vagal balance.15 The LF power of SBP variability can be considered an indirect index of sympathetic control of peripheral resistance.16 Statistical Analysis The strength of the association between SSI and each cardiovascular variable was assessed by the nonparametric Kendall’s correlation coefficient. Positive coefficients mean that greater values of SSI are associated with higher values of the analyzed variable whereas they are associated to lower values in case of negative . We also evaluated how the sodium depletion/repletion maneuver influenced BRS and parameters of PI and BP variability associated with autonomic cardiovascular control as a function of SSI by the following procedure. First, the patient population was subdivided into quartiles of SSI distribution. Then, the statistical significance of the effect of the sodium depletion/repletion maneuver was assessed by repeated-measures ANOVA. When the effect of the maneuver was significant, mean values during sodium depletion and during sodium repletion were compared in each SSI quartile by the Fisher’s least significant difference test (Statistica 6.0; Statsoft Inc.). All variables were preliminarily tested for gaussianity; LF powers, HF powers, and the LF/HF power ratio had to be log-transformed to obtain normal distributions.17,18 The level of statistical significance was set at P⬍0.05. Results Baseline Data Over the group of 34 subjects, 24-hour ambulatory SBP, DBP, and HR (mean⫾SD) were 138⫾11 mm Hg, 89⫾9 mm Hg, and 70⫾8 bpm, respectively; SSI was 33.8⫾7.2 mm Hg/(mol/L per day) ranging between ⫺44 and ⫹146. The degree of salt sensitivity was not associated with age (⫽0.02; P⫽0.84), body mass index (⫽0.03; P⫽0.80), or with the baseline levels of 24-hour SBP (⫽0.19; P⫽0.11), DBP (⫽0.12; P⫽0.33), and HR (⫽0.19; P⫽0.11). Effects of Sodium Intake Figure 1 shows the frequency histogram of percent changes in MAP in response to sodium loading (⌬MAP) and the relationship between ⌬MAP percent changes and SSI. The modal value of ⌬MAP distribution fell below the 10% value commonly used to define salt sensitivity according to the traditional classification. The relationship between ⌬MAP and SSI was not linear, and a good fit was obtained by the parabola SSI⫽0.178⫻⌬MAP2⫹5.294⫻⌬MAP⫺0.631. This means that ongoing toward high levels of salt sensitivity the SSI score is progressively more amplified with respect to the ⌬MAP score. Coruzzi et al Salt Intake and Autonomic Cardiovascular Control 3 Figure 2. Individual values of 2-hour average SBP (top panels) and of spontaneous BRS (bottom panels) at the end of the lowsodium (left) and high-sodium (right) diets, plotted vs SSI in our 34 patients. BRS values being associated with lower SSI values. This trend characterized both dietary conditions but appeared more pronounced after the high sodium intake diet (right panel). Figure 1. a, Histogram refers to the distribution of percent changes of MAP (⌬MAP%) in response to sodium loading in our 34 hypertensive subjects; the arrow shows the threshold for identification of salt sensitivity by the conventional dichotomous approach.7 b, Relationship between SSI and ⌬MAP%. Subjects with above-threshold salt sensitivity are shown by squares. Dashed curve is the parabolic least-square regression line. TABLE 2. Correlations (Kendall’s and significance P ) Between SSI and Cardiovascular Parameters Derived From Beat-by-Beat Recordings at the End of Sodium Depletion and Repletion Periods Low Sodium Table 1 reports BP values measured during the last day of each week of sodium diet and sodium excretion values at the end of each diet week (mean of the last 2 days). All these parameters significantly increased at the end of the high sodium intake period. Individual values of SBP and BRS at the end of highsodium and low-sodium diets are plotted versus SSI in Figure 2. This figure shows a positive relationship between SBP and SSI at the end of the high-sodium intake diet (right panel), which disappears after the low-sodium diet (left panel). A negative association was found between BRS and SSI, higher TABLE 1. BP and Urinary Sodium Excretion After Low-Sodium and High-Sodium Diets (meanⴞSD) Quantity Low Sodium High Sodium P SBP 129⫾11 (mm Hg) 138⫾13 (mm Hg) ⬍10⫺4 DBP 88⫾8 (mm Hg) 91⫾9 (mm Hg) ⬍10⫺2 MAP 102⫾9 (mm Hg) 107⫾10 (mm Hg) ⬍10⫺3 221⫾69 (mmol/L per day) ⬍10⫺15 UNaV 44⫾15 (mmol/L per day) BP data refer to average values of 2-hour arm cuff oscillometric recordings; P indicates statistical significance; UNaV, urinary excretion rate of sodium. Cardiovascular Parameters High Sodium P P BP SBP mean 0.09 NS (0.43) 0.28 ⬍0.02 DBP mean 0.09 NS (0.47) 0.19 NS (0.12) MAP mean 0.08 NS (0.48) 0.22 NS (0.07) SBP SD ⫺0.07 NS (0.56) 0.05 NS (0.67) DBP SD ⫺0.07 NS (0.56) 0.03 NS (0.80) MAP SD ⫺0.06 NS (0.60) 0.04 NS (0.73) SBP LF 0.08 NS (0.50) 0.19 NS (0.12) SBP HF 0.02 NS (0.87) 0.08 NS (0.48) Baroreflex function BRS ⫺0.30 ⬍0.02 ⫺0.43 ⬍0.0004 BEI ⫺0.13 NS (0.29) ⫺0.14 NS (0.24) PI mean ⫺0.18 NS (0.13) ⫺0.29 ⬍0.02 PI SD ⫺0.24 ⬍0.05 ⫺0.44 ⬍0.0003 PI LF ⫺0.22 NS (0.07) ⫺0.36 ⬍0.003 PI HF ⫺0.23 NS (0.06) ⫺0.44 ⬍0.0003 LF/HF 0.16 NS (0.23) 0.19 NS (0.11) HR 4 Hypertension December 2005 Figure 3. BRS (meansⴞSEM) in the 4 quartiles of SSI at the end of low-sodium intake (䡬) and high-sodium intake (●) diets; significant differences between diets are shown by the asterisk (P⬍0.05). The quantification of the coupling between SSI and each cardiovascular variable through the Kendall’s correlation coefficient is reported in Table 2. Concerning the BP parameters, at the end of the high-sodium diet, a significant positive correlation with SSI was found for average SBP; also, MAP and DBP displayed a positive relationship with SSI that fell short of statistical significance. In contrast, no relationship was found between SSI and mean values of SBP, MAP, and DBP at the end of the low-sodium diet or between SSI and overall BP variability (quantified by the SD). As to SBP spectral powers, SSI showed a tendency to be directly related with LF powers only at the end of the high-sodium diet, although this trend did not reach the level of statistical significance. Concerning the baroreflex control of HR, a significant negative relationship was found between SSI and BRS in the low-sodium and high-sodium conditions, whereas BEI was not related to the degree of salt sensitivity. All indexes of PI variability showed a significant negative correlation with SSI at the end of the high-sodium diet, with the exception of the LF/HF powers ratio, which showed a tendency to increase with SSI (⫽0.19; P⫽0.11). After the low-sodium diet, only PI overall variability, quantified by PI SD, was significantly and inversely related to SSI. We also investigated in a deeper detail how the sodium depletion/repletion maneuver affected BRS, and BP and PI variability parameters known to be related to autonomic cardiovascular regulation (SBP LF power, PI LF and HF powers, and LF/HF powers ratio), as a function of the levels of salt sensitivity. To this aim, and to evaluate the statistical significance of differences between SSI levels, we considered levels of SSI defined by subdivision into quartiles, which, in our patients, were: SSIⱕ0 (first quartile); 0⬍SSIⱕ27.5 (second quartile); 27.5⬍SSIⱕ56 (third quartile); and SSI⬎56 (fourth quartile). It is worth noting that all patients conventionally classified as salt sensitive fell in the fourth quartile of SSI distribution. A post hoc analysis was performed on the variables in which ANOVA displayed significant differences between the 2 diets, namely BRS (⫹20% at the end of the high-sodium diet; P⬍0.002), PI HF power (⫹55%; P⬍0.005) and the LF/HF powers ratio of PI (⫺22%; P⬍0.002). The effects of sodium diets on SBP LF (⫺14%; P⫽0.12) and on PI LF (⫹12%; P⫽0.18) did not reach the statistical significance. Figure 3 shows that BRS was significantly lower at the end of the low-sodium diet in the first 3 SSI quartiles. In contrast, subjects within the highest SSI class showed the same low values of BRS independently of the administered diet. In line with Table 2, BRS clearly decreased from the first to the last SSI quartile, in the low- and high-sodium diet groups. Figure 4 shows the relationship of PI powers and of LF/HF PI powers ratio with SSI. Also, HF power was lower at the end of the low-sodium diet in the first 3 SSI quartiles, whereas subjects in the fourth quartile showed similarly low HF powers, independently of the amount of sodium intake. The LF/HF powers ratio was always higher at the end of the low-sodium diet, the difference being significant in the first 2 SSI quartiles. Figure 4. LF and HF PI powers and LF/HF powers ratio (meansⴞSEM) in the 4 quartiles of SSI at the end of low-sodium (䡬) and highsodium (●) diets. significant differences between diets are shown by *(P⬍0.05) and **(P⬍0.01). Coruzzi et al Discussion Our study offers novel information on the relationship between salt sensitivity and reflex cardiovascular regulation by exploring such a relationship on a continuous basis through use of the SSI9,10 and by focusing mainly on subjects with MAP changes in response to sodium loading below the conventional threshold used to define sodium sensitivity, according to the classical dichotomous approach. The important new finding is that spontaneous BRS, in spite of being already reduced because of the high BP condition,19,20 was progressively further impaired as a direct function of the degree of salt sensitivity. In particular, this impairment also occurred in hypertensive patients ranked as not salt sensitive according to the conventional classification. Furthermore, the reduction in BRS was paralleled by a reduction in HR variability, as quantified by its overall variance and, more specifically, by its HF power. Given the evidence that BRS and HR variability are largely markers of vagal cardiac modulation,21,22 our results provide evidence of a progressive impairment in parasympathetic cardiac control in parallel with the increase in salt sensitivity on top of the alterations already induced by the hypertensive state.13,23 Because of the reciprocal changes that usually characterize modifications in sympathetic and parasympathetic control of the heart, these data appear to be in line with previous reports on the occurrence of sympathetic activation in salt-sensitive subjects.24 Because autonomic dysfunction is a well-identified predictor of cardiovascular morbidity and mortality,25,26,27 our results may thus suggest that salt sensitivity could also have a role in this setting, being itself a reliable predictor of an impaired reflex autonomic control of the heart. A second important result of our study is that in subjects with a lower salt sensitivity, a high-sodium diet was characterized by higher BRS and HR variability values than a low-sodium diet. This may depend on the fact that when the reflex cardiovascular regulation is preserved, high sodium intake may activate cardiopulmonary receptors through an increase in plasma volume, leading to a reflex reduction in sympathetic efferent activity,28 whereas the opposite may occur under low sodium intake.29 This modulation was not observed in subjects displaying the highest degree of salt sensitivity, in whom no changes in their impaired autonomic cardiovascular control resulted from manipulation of sodium intake. Based on our data, the salt-dependent BP increase in hypertensive subjects with the higher degree of SSI might thus be attributable, at least in part, either to an impaired baseline arterial baroreflex function or to the inability to increase BRS in response to the increase in plasma volume determined by the sodium loading. The observed lack of correlation between the degree of salt sensitivity (evaluated by SSI) and either baseline 24-hour BP and HR, age, or body mass index supports the interpretation that the impaired autonomic control of circulation observed in our study as a function of SSI was actually related to the increasing SSI levels and not to the influence of other confounding factors. Finally, some implications of the methodology for sodium sensitivity assessment in our study deserve to be discussed. It should be emphasized that use of SSI, in addition to providing a continuous assessment of the degree of salt sensitivity, allowed us to explore the effects of diet sodium manipulation in a more Salt Intake and Autonomic Cardiovascular Control 5 accurate fashion with respect to the traditional approach. Indeed, SSI supplies a measure of salt sensitivity on the basis of the sodium output without requiring information on the actual sodium intake.9 Thus, at variance from the traditional approach, accuracy of SSI does not rely on patients’ full compliance with the dietary regimen. In conclusion, the results of our study indicate that an impairment of autonomic control can also be observed in hypertensive subjects with under-threshold scores of salt sensitivity, as measured by SSI. This approach might thus represent a more sensitive way to explore the relationship between neural autonomic regulation and sodium sensitivity in hypertensive patients, in whom an increased salt sensitivity carries a higher risk of cardiovascular complications. Perspectives Our study demonstrates an impaired autonomic control of circulation in hypertensive subjects with under-threshold salt sensitivity levels, providing additional information on mechanisms involved in the continuous link between sodium sensitivity and cardiovascular risk in hypertension. Additional studies of larger size, and possibly with a longitudinal design, would now be required to explore the possibility of a causal link between salt sensitivity and alterations in neural cardiovascular control. It would also deserve to be investigated whether a relationship between changes in SSI and differences in autonomic cardiovascular regulation might characterize not only hypertensive patients (as demonstrated in our article) but also normotensive subjects with and without family history of hypertension. References 1. Morimoto A, Uzu T, Fuji T, Nishimura M, Kumodo S, Nakamura S, Inenaga T, Kimura G. Sodium sensitivity and cardiovascular events in patients with essential hypertension. Lancet. 1997;350:1734 –1737. 2. Weinberger MH, Fineberg NS, Fineberg SE, Weinberger M. Salt sensitivity, pulse pressure, and death in normal and hypertensive humans. Hypertension. 2001;37:429 – 432. 3. Campese VM. Salt sensitivity in hypertension: renal and cardiovascular implications. Hypertension. 1994;23:531–550. 4. Piccirillo G, Bucca C, Durante M, Santagada E, Munizzi MR, Cacciafesta M, Marigliano V. Heart rate and blood pressure variabilities in saltsensitive hypertension. Hypertension. 1996;28:944 –952. 5. Trimarco B, Lembo G, Ricciardelli B, De Luca N, Rendina V, Condorelli G, Volpe M. Salt-induced plasticity in cardiopulmonary baroreceptor reflexes in salt-resistant hypertensive patients. Hypertension. 1991;18: 483– 493. 6. Kawasaki T, Delca CS, Bartter FC, Smith H. The effect of high-sodium and low-sodium intakes on blood pressure and other related variables in human subjects with idiopathic hypertension. Am J Med. 1998;64: 193–198. 7. Weinberger MH. Salt sensitivity of blood pressure in humans. Hypertension. 1996;27:481– 490. 8. Sullivan JM. Salt-sensitivity. Definition, conception, methodology, and long-term issues. Hypertension. 1991;17:I61–I68. 9. Kimura G, Brenner BM. Implications of the linear pressure-natriuresis relationship and importance of sodium sensitivity in hypertension. J Hypertens. 1997;15:1055–1061. 10. Coruzzi P, Brambilla L, Brambilla V, Gualerzi M, Rossi M, Parati G, Di Rienzo M, Tadonio J, Novarini A. Potassium depletion and saltsensitivity in essential hypertension. J Clin Endocrinol Metab. 2001;86: 2857–2862. 11. Coruzzi P, Musiari L, Mossini GL, Ceriati R, Novarini A. Water immersion and salt-sensitivity in essential hypertension. Scand J Clin Lab Invest. 1993;53:593–599. 6 Hypertension December 2005 12. Di Rienzo M, Bertinieri G, Mancia G, Pedotti A. A new method for evaluating the baroreflex role by a joint pattern analysis of pulse interval and systolic blood pressure series. Med Biol Eng Comput. 1985;23: 313–314. 13. Parati G, Di Rienzo M, Bertinieri G, Pomidossi G, Casadei R, Groppelli A, Pedotti A, Zanchetti A, Mancia G. Evaluation of the baroreceptor-heart rate reflex by 24-hour intra-arterial blood pressure monitoring in humans. Hypertension. 1988;12:214 –222. 14. Di Rienzo M, Parati G, Castiglioni P, Tordi R, Mancia G, Pedotti A. Baroreflex effectiveness index: an additional measure of baroreflex control of heart rate in daily life. Am J Physiol Regul Integr Comp Physiol. 2001;280:R744 –R751. 15. Parati G, Saul JP, Di Rienzo M, Mancia G. Spectral analysis of blood pressure and heart rate variability in evaluating cardiovascular regulation. A critical appraisal. Hypertension. 1995;25:1276 –1286. 16. Task force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Hearth rate variability. Standards of measurement, physiological interpretation, and clinical use. Circulation. 1996;93:1043–1065. 17. Castiglioni P, Parati G, Omboni S, Mancia G, Imholz BP, Wesseling KH, Di Rienzo M. Broad-band spectral analysis of 24 h continuous finger blood pressure: comparison with intra-arterial recordings. Clin Sci. 1999; 2:129 –139. 18. Jenkins GM, Watts DG. Spectral Analysis and Its Applications. San Francisco, Calif: Holden-Day; 1968. 19. Mancia G, Grassi G, Parati G, Zanchetti A. The sympathetic nervous system in human hypertension. Acta Physiol Scand. 1997;640:117–121. 20. Mancia G, Parati G, Pomidossi G, Casadei R, Di Rienzo M, Zanchetti A. Arterial baroreflexes and blood pressure and heart rate variabilities in humans. Hypertension. 1986;8:147–153. 21. Parlow J, Viale JP, Annat G, Hughson R, Quintin L. Spontaneous cardiac baroreflex in humans: comparison with drug-induced responses. Hypertension. 1995;25:1058 –1068. 22. Eckberg D, Drabinski M, Braunwald E. Defective cardiac parasympathetic control in patients with heart disease. N Engl J Med. 1971;285:877–883. 23. Pagani M, Somers V, Furlan R, Dell’Orto S, Conway J, Baselli G, Cerutti S, Sleight P, Malliani A. Changes in autonomic regulation induced by physical training in mild hypertension. Hypertension. 1988;12:600 – 610. 24. Campese VM, Romoff MS, Levitan D, Saglikes Y, Friedler RM, Massry SG. Abnormal relationship between sodium intake and sympathetic nervous system activity in salt-sensitive patients with essential hypertension. Kidney Int. 1982;21:371–378. 25. Berntson GG, Bigger JT Jr, Eckberg DL, Grossman P, Kaufmann PG, Malik M, Nagaraja HN, Porges SW, Saul JP, Stone PH, van der Molen MW. Heart rate variability: origins, methods, and interpretive caveats. Psychophysiology. 1997;34:623– 648. 26. La Rovere MT, Bigger TJ, Marcus FI, Mortara A, Schwartz PJ. Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. ATRAMI (Autonomic Tone and Reflexes After Myocardial Infarction) Investigators. Lancet. 1998; 351:478 – 484. 27. Osterziel KJ, Hanlein D, Willenbrock R, Eichhorn C, Luft F, Dietz R. Baroreflex sensitivity and cardiovascular mortality in patients with mild to moderate heart failure. Br Heart J. 1995;73:517–522. 28. Mark AL, Mancia G. Cardiopulmonary baroreflexes in humans. In: Shepherd JT, Abboud FM, eds. Handbook of Physiology. The Cardiovascular System. Bethesda, Md: American Physiological Society; 1983:795–813. 29. Grassi G, Dell’Oro R, Seravalle G, Foglia G, Quarti Trevano F, Mancia G. Short-and long- term neuroadrenergic effects of moderate dietary sodium restriction in essential hypertension. Circulation. 2002;106: 1957–1961.