Immediate effect of
advertisement

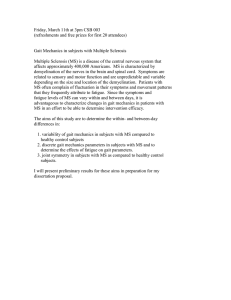
Immediate effect of percutaneous intramuscular stimulation during gait in children with cerebral palsy: a feasibility study Margo N Orlin* PT PhD PCS, Programs in Rehabilitation Sciences, Drexel University; Samuel R Pierce PT MS NCS; Carrie Laughton Stackhouse MS; Brian T Smith MS; Therese Johnston PT MS, Shriners Hospitals for Children; Patricia A Shewokis PhD, Programs in Rehabilitation Sciences, Drexel University; James J McCarthy MD, Shriners Hospitals for Children, Philadelphia, PA, USA. *Correspondence to first author at Drexel University, Programs in Rehabilitation Sciences, 245 North Broad Street, Philadelphia, PA 19102-1192, USA. E-mail: margo.n.orlin@drexel.edu The feasibility of percutaneous intramuscular functional electrical stimulation (P-FES) in children with cerebral palsy (CP) for immediate improvement of ankle kinematics during gait has not previously been reported. Eight children with CP (six with diplegia, two with hemiplegia; mean age 9 years 1 month [SD 1y 4mo; range 7y 11mo to 11y 10mo]) had percutaneous intramuscular electrodes implanted into the gastrocnemius (GA) and tibialis anterior (TA) muscles of their involved limbs. Stimulation was provided during appropriate phases of the gait cycle in three conditions (GA only, TA only, and GA/TA). Immediately after a week of practice for each stimulation condition, a gait analysis was performed with and without stimulation. A significant improvement in peak dorsiflexion in swing for the more affected extremity and dorsiflexion at initial contact for the less affected extremity were found in the GA/TA condition. Clinically meaningful trends were evident for improvements in dorsiflexion kinematics for the more and less affected extremities in the TA only and GA/TA conditions. The results suggest that P-FES might immediately improve ankle kinematics in children with CP. See end of paper for list of abbreviations. 684 Developmental Medicine & Child Neurology 2005, 47: 684–690 Gait deficits are common in children with cerebral palsy (CP) in comparison with children of typical development. Children with CP have decreased walking velocity and stride length compared with children of typical development (Norlin and Odenrick 1986, Sutherland et al. 1988, Abel and Damiano 1996). Winters et al. (1987) examined the gait of a heterogeneous sample of 46 children and adults with hemiplegia and found that decreased dorsiflexion in swing was a commonly seen deficit in ankle kinematics. Even small changes in ankle angle during stance phase or swing phase can significantly affect foot clearance (Winter 1992). Poor foot clearance contributes to the frequent tripping and falling reported by children with CP. In addition, children with CP often do not demonstrate a true heel strike at foot contact, thereby loading the triceps surae and creating a plantarflexion and knee extension coupling during initial stance. This increases absorption work by the triceps surae during initial stance, resulting in a more inefficient gait. In a comparative study, Olney et al. (1990) found that the ankle plantar flexors in children with spastic hemiplegic CP produced less positive work at push-off than those in children of typical development. Power generation by the plantarflexors during push-off contributes significantly to step length and walking velocity (Winter 1992). Interventions have been developed to improve the gait mechanics of children with CP. Ultimately, the goal of such intervention is to improve gait mechanics, reduce energy consumption, improve poor foot clearance, and, possibly, prevent secondary injuries due to abnormal loads placed on the musculoskeletal system. Functional electrical stimulation (FES) is the use of electrical current for activation of muscles through the stimulation of intact peripheral motor nerves to promote functional activities (American Physical Therapy Association 2000). FES has been investigated as a method of addressing abnormal gait mechanics in children with CP, typically by stimulation of the ankle plantarflexors, ankle dorsiflexors, and/or peroneal nerve. The primary focus of previous investigations has been on the carry-over effect of prolonged FES training on gait and function. Carmick (1993, 1995) reported improvements in gait, voluntary walking speed, and energy efficiency in multiple case studies of children with CP after prolonged FES training of several muscles including the gastrocnemius (GA). Comeaux et al. (1997) examined the use of FES of the GA and tibialis anterior (TA) in 14 children with CP and found that FES training improved ankle position at initial foot contact by about 4˚. The immediate effect of surface FES on gait kinematics, kinetics, and temporal–spatial parameters has not been well investigated. Naumann et al. (1985) reported immediate improvements in dorsiflexion at initial contact of about 10˚ in two adolescents with CP when they walked with FES applied to their dorsiflexors during swing. Step length and walking velocity also improved in one of the participants during FES application. Joint kinetics were not reported in this investigation. These studies of FES in children with CP have primarily involved stimulation applied by means of surface skin electrodes. Implanted intramuscular stimulation, applied using fine wire electrodes, may have potential advantages over surface stimulation. Difficulties associated with surface electrodes that might be addressed with intramuscular stimulation include obtaining repeatable stimulated motor responses, the inability to stimulate deeper muscles, and decreased skin tolerance with prolonged use (McNeal and Bowman 1985). The levels of discomfort associated with surface FES and percutaneous intramuscular FES (P-FES) have been compared in adults with hemiplegia due to stroke and it was found that the P-FES was perceived as significantly more comfortable (Chae and Hart 1998, Yu et al. 2001). These authors suggested that P-FES was more comfortable because it avoids the stimulation of cutaneous nociceptors. To our knowledge, the use of percutaneous electrodes with children with CP has been limited to several small studies conducted at our hospital. In one of the first, Bertoti et al. (1997) investigated the use of P-FES of the TA, GA, quadriceps, and gluteal muscles during gait and exercise in two children with CP. Gross motor function was not tested specifically, but improvements in unassisted ambulation, stopping, and starting while walking, and alteration of walking direction were reported. Range of motion of the lower extremity improved and increases in step length and base of support in one participant were reported after completion of the stimulation program. Our laboratory has also reported on the use of P-FES in tandem with soft tissue surgical procedures needed by children with CP (Johnston et al. 2004). There is a paucity of work investigating the immediate effect of P-FES on gait kinematics, kinetics, and temporal–spatial parameters in children. Recently we reported immediate Table I: Participant inclusion criteria Diagnosis of cerebral palsy, spastic diplegia, or spastic hemiplegia Level I or II in GMFCS Age between 7 and 12 years Migration Index less than 40% as measured on X-ray or hip dislocation Seizure-free or seizure-controlled Visuoperceptual skills and cognitive/communication skills sufficient to follow multiple step commands and to attend to tasks associated with data collection as determined by history and clinical observation Absence of severe tactile hypersensitivity in the lower extremities A minimum of 1 year after surgery to the lower extremities A minimum of 6 months after botulinum toxin injection to the lower extremities Passive range of lower-extremity joints: less than 10˚ contracture of hip in extension measured by the Thomas Test; at least 20˚ range in hip abduction; less than 5˚ knee flexion contracture, and popliteal angle less than 45˚; more than 0˚ ankle dorsiflexion with knee extended and foot in varus GMFCS, Gross Motor Function Classification System (Palisano et al. 1997). improvements in gait in two children with CP while walking with P-FES (Pierce et al. 2004). Both participants received percutaneous stimulation to the TA and GA muscles alone and to GA/TA simultaneously at appropriate times during the gait cycle. Improvements in peak dorsiflexion in swing, mean dorsiflexion in swing, ankle dorsiflexion angle at initial contact, and ankle work during early stance were noted for both children with TA and GA/TA stimulation. Both children showed improvements in ankle work during late stance in all stimulation conditions. It is important that the immediate effects of P-FES on gait be understood in order to establish the efficacy of the intervention before assessing its use in longer-term training studies. The purpose of this investigation was to determine the feasibility of using P-FES to produce immediate effects on ankle kinematics and kinetics in children with CP when applied to the GA and TA during the gait cycle. There were three aims of the study with the following hypotheses. (1) Stimulation to the TA while walking as compared with walking without stimulation will result in the following: (i) increased ankle dorsiflexion at initial contact; (ii) increased peak ankle dorsiflexion during swing; (iii) increased mean ankle dorsiflexion during swing phase; (iv) increased stride length; (v) increased walking velocity; and (vi) decreased power absorption by the ankle during loading response. (2) Stimulation to the GA while walking as compared with walking without stimulation will result in the following: (i) increased stride length; (ii) increased walking velocity; (iii) increased ankle moment at push off; and (iv) increased ankle power generation at push-off. (3) Stimulation to the TA and GA while walking as compared with walking without stimulation will result in the following: (i) increased ankle dorsiflexion at initial contact; (ii) increased peak dorsiflexion during swing; (iii) increased mean ankle dorsiflexion during swing phase; (iv) increased stride length; (v) increased walking velocity; (vi) decreased power absorption by the ankle during loading response; (vii) increased ankle power generation at push-off; and (viii) increased ankle moment at push off. Method PARTICIPANTS Participants were recruited through the CP clinic at Shriners Hospitals for Children in Philadelphia, Pennsylvania, USA. The Institutional Review Board of Temple University in Philadelphia approved the study. Informed consent was obtained from each child’s parent or guardian. A convenience sample was chosen consisting of eight children with CP with a mean age of 9 years 1 month (SD 1y 4mo). Inclusion criteria are Table II: Demographic information on all participants Participant 1 2 3 4 5 6 7 8 Age (y:m) Sex CP type More affected limb Height (cm) Weight (kg) GMFCS level 9:1 7:11 8:2 8:9 8:8 11:10 10:4 8:1 M M M F F M F F Diplegia Diplegia Hemiplegia Diplegia Diplegia Diplegia Hemiplegia Diplegia Right Right Right Left Right Left Right Right 123 120 121 115 127 149 134 134 26 19.6 23.3 20.6 32.3 65.9 23.6 45 II II I II II I I I GMFCS, Gross Motor Function Classification System (Palisano et al. 1997). Feasibility of P-FES in Children with CP Margo N Orlin et al. 685 listed in Table I. There were two participants with spastic hemiplegia and six with spastic diplegia. Four were classified in level I and four were classified in level II of the Gross Motor Function Classification System (GMFCS; Palisano et al. 1997). Table II lists the demographic information on all study participants. PROCEDURE Intramuscular electrodes (NeuroControl Corporation, Valley View, OH, USA) with a needle insertion procedure were used to deliver the stimulation. Memberg et al. (1994) provide details on electrode design but a brief description is provided here. The electrode leads are created from a double helix of cables composed of stainless steel filaments covered in FEP-Teflon (DuPont Company, Wilmington, DE, USA). The entire double helix is contained within medical-grade Silastic tubing (Dow Corning, Midland, MI, USA) to prevent the electrode from binding down to the tissue beneath the skin surface. The tip of the electrode has a polypropylene anchor with five barbs around a central core, which hold the electrode in place within the muscle tissue. After the electrode is implanted, the Silastic tubing exposed above the skin is stripped away and the Teflon coating at the skin interface is left in place to allow tissue growth around the lead to hold it in place. The leads are placed in a block for connection to the stimulator. Four channels for the children with diplegia and two channels for the children with hemiplegia of a research-grade electrical stimulator provided control of muscle stimulation through the percutaneous electrodes. The electrode leads exiting from the skin and contained in the connector block on the anterior thigh were placed underneath the clothing and attached to the stimulator worn by the individual in a waist pack. The stimulator used a charge-balanced asymmetrical stimulation waveform. Pulse durations and frequencies were individualized for patients based on strength of contraction and patient comfort. The stimulation patterns contained in the stimulator used during walking were unique to each child. The goal Figure 1: Illustration of coordination of dorsiflexors and plantarflexors for gait training by electrical stimulation. Stimulation pattern is shown in reference to the highlighted leg. Timing of electrical stimulation delivery was controlled through detection of initial contact, midstance, and terminal stance via the force-sensing resistor in the shoe. Stimulation was applied to gastrocnemius and tibialis anterior of both legs to children with spastic diplegia and to the involved leg for children with hemiplegia. Adapted from Fig. 7.11 in Sutherland et al. (1998), p 147, and reprinted with permission of Cambridge University Press. FS, foot-strike; OTO, opposite toe-off; OFS, opposite foot-strike; TO, toe-off. 686 FS OTO Developmental Medicine & Child Neurology 2005, 47: 684–690 of individualizing the stimulation parameters for the TA was to produce a contraction against gravity through the full range of motion while in the seated position. For the GA, the goal was to produce a maximal contraction to the child’s tolerance during the gait cycle. Using these goals, the pulse durations used ranged from 12 to 200 seconds and the frequencies from 20 to 50Hz. The amplitude was set at 20mA. The implant procedure was performed with the patient under general anesthesia. An intramuscular electrode was implanted in the TA near the fibular head of the participant’s right leg and at the motor end-point of the lateral head of the GA. The motor end point was used as the site at which an optimal stimulated response was obtained. Electrical stimulation to a 25-gauge insulated probe was initially used to identify the motor end point and confirmed with a larger blunt intramuscular probe. A cannula was placed over the probe. The probe was removed and the cannula was used as a guide to insert the percutaneous electrode. Electrode placement and responses were evaluated during the procedure to ensure that the best possible response was identified. This was carried out by visual inspection of muscle contraction elicited while the muscle was stimulated. The ankle motion elicited by TA stimulation was observed, to be certain that it was balanced without too much inversion due to an uneven pull of the TA. After electrode implantation, the electrode leads from GA and TA muscles were tunneled subcutaneously to a common exit site on the proximal anterior thigh. Gauze and a clear plastic bandage were used to cover the exit site to protect the electrodes. Children with spastic diplegia all had electrodes implanted in both limbs; children with hemiplegia had electrodes implanted on their affected side only. On postoperative day one, the electrodes were tested to determine that the stimulated contractions continued to be optimal. The electrodes were then crimped and placed into a block to connect into the stimulator box. Before implantation of the electrodes, the process for control of stimulation was initiated. Force-sensing resistors (FSRs; OFS TO FS Interlink Electronics, Camarillo, CA, USA), embedded in an insole worn in the shoes, were used to detect gait cycle events for the control and timing of stimulation for each individual while walking. The F-scan plantar pressure insole (TekScan Inc., Boston, MA, USA) was used to determine FSR placement. Before implantation of the electrodes, participants wore the F-scan insoles in each shoe while walking so that plantar pressures could be recorded over three to five steps. Specific areas of greatest plantar pressure at three gait events (initial contact, mid-stance, and terminal stance) were recorded and the insole with embedded FSRs was fabricated. The FSRs detected gait events and delivered stimulation to the appropriate muscles at the correct time during the gait cycle through an interface with a portable stimulator used by the child during walking practice. Participants walked with the insoles to determine the combination of FSR signals and the threshold pressure levels to be used to detect each gait event. Table III: Parameters used to determine Normalcy Index for each participant Percentage of gait cycle when foot-off occurs Step length Cadence Velocity Average pelvic tilt Pelvic obliquity range Average pelvic obliquity Pelvic rotation range Maximum hip extension Maximum hip flexion Knee flexion at initial contact Maximum knee flexion in swing Average knee flexion in stance Knee range of motion Dorsiflexion at initial contact Maximum dorsiflexion in stance Maximum plantar flexion in swing Maximum dorsiflexion in swing Foot progression angle Figure 1 shows the timing pattern of the stimulation delivered during walking. The FSRs have been shown to detect gait events accurately during stance in a sample of seven children with CP in 94.5% of 642 steps (Smith et al. 2002). After 1 week of recuperation at home, participants returned to begin walking practice. Participants practiced walking with the electrical stimulation under three randomly ordered conditions. The three conditions were GA stimulation on (GA), TA stimulation on (TA), and both GA and TA (GA/TA) stimulation on. Participants practiced for two 45-minute walking sessions per day for about 1 week under each condition. A therapist used a manual switch to turn the stimulation program on and off as needed. The stimulation program continued during walking, until the therapist stopped the program manually with another switch at the end of the practice session. Rests were given as needed during the sessions. Immediately after the practice week in each condition, a standard three-dimensional gait analysis was conducted in both stimulation on and stimulation off conditions using a six-camera Vicon motion-capture system (Vicon Motion Systems, Tustin, CA, USA) at the participant’s self-selected walking speed. Data collection took about 1 to 2 hours. Retroreflective markers were attached to the bilateral lower extremities with tape and secured with non-adhesive wrap on the following anatomical locations: sacrum, anterior superior iliac spine, lateral aspect of the mid-thigh, mid-calf, lateral malleolus, base of the heel, and the dorsal aspect of the foot between the second and third metatarsal bones (Davis et al. 1991). A static calibration trial was collected before the walking trials, with a triaxial marker set (knee alignment device; Motion Lab Systems, Inc., Baton Rouge, LA, USA) to define the knee flexion and extension axes. After the standing calibration, the knee alignment device was removed and a marker was placed on the lateral femoral condyle. Video data, collected at 60Hz, and ground reaction force data, collected at 1200Hz, were recorded simultaneously. Four force plates (Advanced Mechanical Technology, Inc., Watertown, MA, USA), embedded within the walkway, were used to collect kinetic data during the walking trials. During and immediately after each trial, force-plate contacts were Table IV: Data and results for statistical comparison – tibialis anterior condition only Variables More affected DF at IC,˚ Peak DF in swing,˚ Mean DF in swing,˚ Stride length, m Walking velocity, m/s Absorption work, W/kg Less affected DF at IC,˚ Peak DF in swing,˚ Mean DF in swing,˚ Stride length, m Walking velocity, m/s Absorption work, W/kg Stim. off Mean (SD) Stim. on Mean (SD) Mean (SD) Change 95% CI Uncorrected p –2.9 (5.6) 0.6 (6.5) –8.2 (7.6) 1.03 (0.1) 1.10 (0.1) –0.12 (0.04) 1.6 (5.7) 3.5 (5.6) –4.5 (7.7) 1.05 (0.1) 1.12 (0.1) –0.09 (0.03) 4.42 ↑ (3.19) 2.96 ↑ (2.25) 3.69 ↑ (3.45) 0.02 ↑ (0.03) 0.03 ↑ (0.06) 0.03 ↑ (0.03) 1.7 to 7.1 1.1 to 4.8 –0.8 to 6.6 –0.01 to 0.05 –0.03 to 0.07 0 to 0.06 0.012 0.014 0.038 >0.1 >0.1 0.082 –4.9 (3.3) –2.4 (3.7) –10.7 (6.1) 1.03 (0.1) 1.10 (0.1) –0.10 (0.03) .01 (3.3) 3.1 (4.7) –5.5 (7.0) 1.04 (0.1) 1.11 (0.1) –0.06 (0.02) 5.01 ↑ (3.21) 5.5 ↑ (3.67) 5.2 ↑ (4.82) 0.01 ↑ (0.04) 0.01 ↑ (0.07) 0.03 ↑ (0.03) 1.6 to 8.4 1.7 to 9.3 0.1 to 10.3 –0.03 to 0.04 –0.05 to 0.07 –0.02 to 0.09 0.024 0.028 0.092 >0.1 >0.1 >0.1 Stim. off, stimulation off; Stim. on, stimulation on; CI, confidence interval; DF, dorsiflexion; IC, initial contact; ↑, improvement. For kinematic values, positive is dorsiflexion and negative is plantarflexion. Feasibility of P-FES in Children with CP Margo N Orlin et al. 687 confirmed. The test continued until three force-plate contacts were collected bilaterally for both the stimulation on and stimulation off conditions. The two conditions (stimulation on and stimulation off) were initially alternated approximately after every second trial. When sufficient data were collected for one condition (i.e. three total foot strikes on the force plates), walking trials continued with the remaining condition only. Ankle joint kinematic, ankle kinetic, and temporal–spatial data were determined with Vicon Clinical Manager Software (Oxford Metrics, Vicon Motion Systems, Lake Forest, CA, USA) and custom-written software in Matlab (The MathWorks, Inc., Natick, MA, USA). DATA ANALYSIS For data analysis purposes, participants’ more affected and less affected legs were analyzed separately. This was done so that data from children with diplegia and hemiplegia could be grouped together. To distinguish the ‘more affected’ side, an index to determine the magnitude of the deviation from typical gait was calculated for three gait cycles on each leg and then averaged for each leg separately. The index was calculated by principal component analysis from the data of 36 children with typical development collected in the laboratory at Shriners Hospitals in Philadelphia. When the data from the individuals with atypical gait are compared with this normal database, an index score or a number representative of the amount of deviation from a typical gait pattern is determined. A larger number is indicative of a more atypical gait pattern. The limb with the greater value was determined to be the more affected side. Table III lists the gait parameters used to calculate this index. The parameters used include temporal–spatial and kinematic variables. Using principal component analysis, these variables differ slightly from the variables in previous literature, but the technique is the same (Novacheck et al. 2002, Schutte et al. 2000). The results of the calculated index were compared with the clinical determination provided by the physical therapist who examined each child. This determination was made after a detailed clinical examination and observation of videotapes of walking. In all cases except one, the calculated index and clinical determination agreed. For the one that disagreed, the clinical determination was accepted. Data were analyzed with the use of paired one-tailed t-tests with comparisons made between the on and off stimulation conditions. Each aim focused on one of the muscle stimulation protocols, namely the TA (aim 1), GA (aim 2) and GA/TA (aim 3). Within each aim, the more affected and less affected legs were tested separately. Each aim and side was considered to be a family of tests. To control for an inflated type I error rate, Bonferroni corrections were made for the number of tests in each family of aims. Thus, the significance criteria were 0.006, 0.0125, and 0.0055 respectively, for each family of aims. Results Descriptive data and results for all statistical comparisons for the three aims are given in Tables IV–VI. Uncorrected p values are reported in the Tables. Two significant differences were noted in the GA/TA condition: peak dorsiflexion in swing on the more affected side (t=4.99, p=0.004) and dorsiflexion at initial contact on the less affected side (t=0.004, p=0.004). The actual changes from stimulation off to stimulation on were 2.8˚ and 4.36˚ respectively. On the basis of the corrected p values, there was no significant difference in the TA only and GA only conditions, but several trends of clinical importance were noted. In the TA condition, on the more affected side there was a trend toward improvement in dorsiflexion at initial contact (t=3.91, p=0.012), peak dorsiflexion in swing (t=3.70, p=0.014), and mean dorsiflexion in swing ( t=3.02, p=0.038). For these variables, the increases in dorsiflexion were 4.42˚, 2.96˚, and 3.69˚ respectively. In the TA condition, on the less affected side, both dorsiflexion at initial contact (t=3.81, p=0.024) and peak dorsiflexion in swing (t=3.67, p=0.028) improved, by 5.01˚ and 5.5˚ respectively. Positive trends were also seen in the GA/TA condition. On the more affected side, dorsiflexion at initial contact increased by 4.84˚ (t=2.81, p=0.062). On the less affected side, peak dorsiflexion in swing increased by 2.97˚ (t=3.86, p=0.024) and mean dorsiflexion in swing increased by 3.98˚ (t=4.47, p=0.014). Discussion The purpose of our study was to determine the feasibility of implanting percutaneous electrodes in lower-extremity muscles in children with CP and to have these children walk with stimulation of the muscles applied at appropriate points in the gait cycle to affect immediate changes in gait. In feasibility studies the requirements for sample size determination are not as stringent as in randomized controlled trials. Feasibility Table V: Data and results for statistical comparison – gastrocnemius condition only Variables More affected Stride length, m Walking velocity, m/s Ankle positive work, W/kg Ankle moment, Nm/kg Less affected Stride length, m Walking velocity, m/s Ankle positive work, W/kg Ankle moment, Nm/kg Stim. off Mean (SD) Stim. on Mean (SD) Mean (SD) Change 95% CI Uncorrected p 1.02 (0.12) 1.10 (0.13) 0.11 (0.04) 0.64 (0.15) 1.04 (0.13) 1.14 (0.14) 0.12 (0.04) 0.61 (0.20) 0.02 ↑ (0.06) 0.04 ↑ (0.12) 0.01 ↑ (0.05) 0.03 ↓ (0.08) –0.03 to 0.07 –0.06 to 0.14 –0.04 to –0.04 –0.10 to 0.05 >0.1 >0.1 >0.1 >0.1 1.02 (0.13) 1.10 (0.15) 0.09 (0.02) 0.69 (0.14) 1.05 (0.13) 1.14 (0.14) 0.10 (0.03) 0.63 (0.21) 0.03 ↑ (0.04) 0.04 ↑ (0.12) 0.01 ↑ (0.03) 0.06 ↓ (0.10) 0.0 to 0.07 –0.05 to 0.15 –0.05 to 0.03 –0.18 to 0.06 >0.1 >0.1 >0.1 >0.1 Stim. off, stimulation off; Stim. on, stimulation on; CI, confidence interval; ↑, improvement; ↓, decline. For kinematic values, positive is dorsiflexion and negative is plantarflexion. 688 Developmental Medicine & Child Neurology 2005, 47: 684–690 studies are comparable to pilot studies in that the goal of the study is to determine the efficacy of the methodology and procedures, as well as to obtain an estimate of intraparticipant variability. We were able to measure the short-term application of P-FES on gait function for these children, resulting in estimates of intraparticipant variability on selected spatial–temporal, kinematic, and kinetic gait variables with and without stimulation. These estimates are important for establishing a baseline performance of the direct application of P-FES. Our focus in this study was on detecting gait function values comparable to previous gait studies that employed FES (Carmick 1993, 1995; Bertoti et al. 1997; Comeaux et al. 1997) for a longer duration. Importantly, we also controlled for type I errors for each aim of the study. The decision to correct for multiple comparisons was made to minimize the risk of type I error due to the invasive nature of the intervention. The number of potentially statistically significant comparisons in the TA only and GA/TA condition would have increased markedly from 3% to 33% of comparisons between the on and off conditions if we had not corrected for multiple comparisons in our data analysis. Two significant increases in DF angle during stimulation, peak dorsiflexion in swing on the more affected side, and dorsiflexion at initial contact on the less affected side were found in the GA/TA condition but not in the TA condition. It is important to note that the magnitude of change was very similar for each of these measures in the two conditions, even though in the TA condition (Table V) the differences were not statistically significant. The lack of difference in the TA condition may be due to the larger variability and wider confidence intervals in that condition for these two variables. This would suggest that whereas the GA/TA and TA conditions effected a positive change in the amount of ankle dorsiflexion, the change was less variable in the GA/TA condition. Presumably, the GA/TA condition provided coordinated muscle activation and sensory feedback by stimulating GA/TA muscles around the joint during appropriate times in the gait cycle. Consequently, stimulating GA/TA muscles may produce a more consistent outcome than stimulation of each muscle separately. We contend that a finding of this type merits further investigation. The improvement of about 4.5 to 5˚ of dorsiflexion at initial contact found in both the TA and GA/TA conditions is clinically meaningful because a 2.6˚ change in the angle of the stance limb ankle has been shown to affect swing-limb foot clearance (Winter 1992). These changes in ankle dorsiflexion angle could potentially improve foot clearance for children with CP who often have difficulty with tripping during walking. In the TA condition, both the peak and mean dorsiflexion angle in swing were improved relative to the off condition and were of comparable magnitudes to those in other studies (Carmick 1993, 1995; Comeaux et al. 1997). The magnitude of this improvement (2.96˚ and 3.69˚ respectively) is clinically significant because a joint angle change of 2.07˚ has been shown to alter foot clearance significantly (Winter 1992). Our hypothesis that stimulation would improve ankle kinetics and temporal–spatial gait parameters was not supported by the data. There was no change in any of these variables, indicating that the short-term application of P-FES was insufficient to modify them. Temporal–spatial gait characteristics are often difficult to change, particularly in children with diplegic CP (Abel and Damiano 1996), especially with shortterm applications, as in the 1 week in this study. Bertoti et al. (1997) reported a step length increase of 7.7cm in a child with CP after 7 months of gait training with P-FES with six lowerextremity muscles implanted. However, with 7 months of training and multiple muscles stimulated, this child was unable to affect a velocity change. Multiple factors have the potential to affect temporal–spatial variables, including the amount of motor impairment, pelvis, hip and knee function, range of motion, and balance. In this sample, the children were classified at Table VI: Data and results for statistical comparison – gastrocnemius/tibialis anterior conditions Variables More affected DF at IC,˚ Peak DF in swing,˚ Mean DF in swing,˚ Stride length, m Walking velocity, m/s Absorption work, W/kg Ankle positive work, W/kg Ankle moment, Nm/kg Less affected DF at IC,˚ Peak DF in swing,˚ Mean DF in swing,˚ Stride length, m Walking velocity, m/s Absorption work, W/kg Ankle positive work, W/kg Ankle moment, Nm/kg Stim. off Mean (SD) Stim. on Mean (SD) Mean (SD) Change 95% CI Uncorrected p –6.0 (7.2) –2.2 (7.0) –11.3 (9.3) 1.05 (0.14) 1.13 (0.14) –0.09 (0.04) 0.13 (0.04) 0.47 (0.22) –1.2 (6.4) 0.6 (7.3) –8.5 (10.3) 1.09 (0.12) 1.16 (0.12) –0.08 (0.04) 0.12 (0.04) 0.45 (0.30) 4.84 ↑ (4.55) 2.8 ↑ (1.51) 2.8 ↑ (3.0) 0.03 ↑ (0.02) 0.03 ↑ (0.09) 0.01 ↑ (0.04) 0.01 ↔ (0.01) 0.02 ↔ (0.10) 0.6 to 9.0 –4.2 to –1.4 –5.5 to 0.0 –0.08 to 0.01 –0.11 to 0.04 –0.05 to 0.03 –0.004 to 0.03 –0.09 to 0.12 0.062 0.004a 0.100 >0.1 >0.1 >0.1 >0.1 >0.1 –3.0 (6.9) 1.8 (5.4) –6.6 (4.3) 1.08 (0.15 1.14 (0.14) –0.08 (0.04) 0.12 (0.03) 0.53 (0.21) 1.4 (6.1) 4.8 (3.8) –2.7 (4.1) 1.07 (0.13) 1.12 (0.12) 0.08 (0.05) 0.11 (0.04) 0.48 (0.27) 4.36 ↑ (1.89) 2.97 ↑ (1.89) 3.98 ↑ (2.18) 0.005 ↔ (0.04) 0.02 ↔ (0.08) 2.3 ↑ (6.67) 0.007 ↔ (0.01) 0.05 ↓ (0.07) 2.4 to 6.3 1.0 to 5.0 1.7 to 6.3 –0.04 to 0.03 –0.09 to 0.04 –0.06 to 0.07 –0.02 to 0.01 –0.14 to 0.04 0.004a 0.024 0.014 >0.1 >0.1 >0.1 >0.1 >0.1 Stim.off, stimulation off; Stim.on, stimulation on; CI, confidence interval; DF, dorsiflexion; IC, initial contact; ↔, no change; ↑, improvement; ↓, decline. aSignificant p value correcting for multiple comparisons. For kinematic values, positive is dorsiflexion and negative is plantarflexion. Feasibility of P-FES in Children with CP Margo N Orlin et al. 689 GMFCS levels I and II with stride length and velocity values close to typical levels (Steinwender et al. 2000). There might, therefore, have been a ceiling effect, and additional improvement might have been even more difficult to achieve. The short-term application of P-FES might not be enough to modify these values, so a longer-term application with practice might be required to make this change. Because our investigation examined only the immediate effects of percutaneous stimulation on gait in children with CP, the long-term effects of training with percutaneous stimulation on gait and function are unknown. Additional controlled studies with a larger sample of children randomly assigned into control and stimulation groups, along with a more extended practice period, will be necessary to establish the efficacy of FES as a rehabilitation intervention. Future comparisons of surface and percutaneous stimulation are also necessary to determine the relative effectiveness of each modality. Conclusion This study provided evidence that P-FES applied to the TA and GA muscles together at appropriate times in the gait cycle is a feasible method of immediately improving ankle dorsiflexion in children with spastic diplegic or spastic hemiplegic CP. Trends also indicated that stimulation of the TA alone might also improve ankle dorsiflexion during gait. All of the improvements that were noted produced clinically meaningful change. Neither temporal–spatial or kinetic characteristics of gait changed with stimulation, suggesting that these attributes might be more difficult to modify, particularly with a short-term application of P-FES. Because this feasibility study used a short-term application of P-FES to produce only an immediate change, more study is needed to determine the long-term effects of P-FES with practice as a way of improving overall ambulatory function in children with spastic CP. DOI: 10.1017/S0012162205001398 Accepted for publication 17th November 2004. Acknowledgements This study was funded by Shriners Hospitals for Children, grant no. 8530. References Abel MF, Damiano DL. (1996) Strategies for increasing walking speed in diplegic cerebral palsy. J Pediatr Orthop 16: 753–758. American Physical Therapy Association. (2000) Electrotherapeutic Terminology in Physical Therapy. Section on Clinical Electrophysiology. Virginia, USA: American Physical Therapy Association. p 36. Bertoti DB, Stanger M, Betz RR, Akers J, Maynathon M, Mulcahey MJ. (1997) Percutaneous functional electrical stimulation as an intervention choice for children with cerebral palsy. Pediatr Phys Ther 9: 123–127. Carmick J. (1993) Clinical use of neuromuscular electrical stimulation for children with cerebral palsy, part I: lower extremity. Phys Ther 73: 505–513. Carmick J. (1995) Managing equinus in children with cerebral palsy: electrical stimulation to strengthen the triceps surae muscle. Dev Med Child Neurol 37: 965–975. Chae J, Hart R. (1998) Comparison of discomfort associated with surface and percutaneous electrical stimulation for persons with chronic hemiplegia. Am J Phys Med Rehabil 77: 516–522. Comeaux P, Patterson N, Rubin M, Meiner R. (1997) Effect of neuromuscular electrical stimulation during gait in children with cerebral palsy. Ped Phys Ther 9: 103–109. 690 Developmental Medicine & Child Neurology 2005, 47: 684–690 Davis RB, Ounpuu S, Tyisurski D, Gage JR. (1991) A gait analysis data collection and reduction technique. Hum Move Sci 20: 575–587. Johnston TE, Finson RL, McCarthy JJ, Smith BT, Betz RR, Mulcahey MJ. (2004) Use of functional electrical stimulation to augment traditional orthopaedic surgery in children with cerebral palsy. J Pediatr Ortho 24 (Suppl.3): 283–291. McNeal DR, Bowman BR. (1985) Peripheral nerve stimulation. In: Mykleburst JB, Cusick JF, Sances A, Larson SJ, editors. Neural Stimulation. Vol 2. Boca Raton, FL: CRC Press. p 95–118. Memberg WD, Peckham PH, Keith MW. (1994) A surgically-implanted intramuscular electrode for an implantable neuromuscular stimulation system. IEEE Trans Rehabil Eng 2: 80–91. Naumann S, Mifsud M, Cairns BJ, Milner M, Herbert MA. (1985) Dual-channel electrical stimulators for use by children with diplegic spastic cerebral palsy. Med Biol Eng Comput 23: 435–444. Norlin R, Odendrick P. (1986) Development of gait in spastic children with cerebral palsy. J Pediatr Orthop 4: 674–680. Novacheck TF, Trost JP, Schwartz MH. (2002) Intramuscular psoas lengthening improves dynamic hip function in children with cerebral palsy. J Ped Orthop 22: 158–164. Olney SJ, MacPhail HE, Heden DM, Boyce WF. (1990) Work and power in hemiplegic cerebral palsy gait. Phys Ther 70: 431–438. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi E. (1997) Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 39: 214–223. Peckham PH, Keith MW, Kilgore KL, Grill JH, Wuolle KS, Thrope GB, Gorman P, Hobby J, Mulcahey MJ, Carroll S, Hentz VR, Wiegner A, Implantable Neuroprosthesis Group. (2001) Efficacy of an implanted neuroprosthesis for restoring hand grasp in tetraplegia: a multicenter study. Arch Phys Med Rehabil 82: 1380–1388. Pierce SR, Orlin MN, Lauer RT, Johnston TE, Smith BT, McCarthy JJ. (2004) Comparison of percutaneous and surface functional electrical stimulation during gait in a child with hemiplegic cerebral palsy. Arch Phys Med Rehab 83: 798–805. Schutte LM, Narayanan U, Stout JL, Selber P, Gage JR, Schwartz MH. (2000) An index for quantifying deviations from normal gait. Gait Posture 11: 25–31. Smith BT, Coiro DJ, Finson R, Betz RR, McCarthy J. (2002) Evaluation of force-sensing resistors for gait event detection to trigger electrical stimulation to improve walking in the child with cerebral palsy. IEEE Trans Neural Syst Rehabil Eng 10: 22–29. Steinwender G, Saraph V, Scheiber S, Zwick EB, Uitz C, Hackl K. (2000) Intrasubject repeatability of gait analysis data in normal and spastic children. Clin Biomech 15: 134–139. Sutherland D, Olshen R, Biden E, Wyatt M. (1998) The Development of Mature Walking. Clinics in Developmental Medicine No. 104/105. London: Mac Keith Press. Winter DA. (1992) Foot trajectory in human gait: a precise and multifactorial motor control task. Phys Ther 72: 45–66. Winters TF, Gage JR, Hicks R. (1987) Gait patterns in spastic hemiplegia in children and young adults. J Bone Joint Surg Am 69 (Suppl. 3): 437–441. Yu DT, Chae J, Walker ME, Har RL, Petroski GF. (2001) Comparing stimulation-induced pain during percutaneous (intramuscular) and transcutaneous neuromuscular electric stimulation for treating shoulder subluxation in hemiplegia. Arch Phys Med Rehabil 82: 756–760. List of abbreviations FES FSR GA P-FES TA Functional electrical stimulation Force-sensing resistor Gastrocnemius Percutaneous intramuscular functional electrical stimulation Tibialis anterior