THE MFT PRACTICUM AND CLINICAL SERVICES CENTER MANUAL
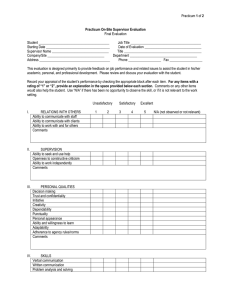
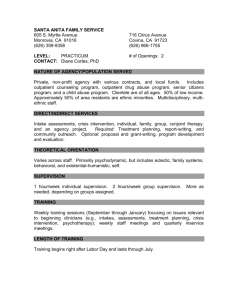
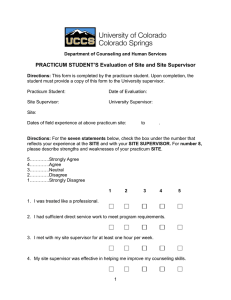
advertisement

THE MFT PRACTICUM AND CLINICAL SERVICES CENTER MANUAL UW-Stout Marriage and Family Therapy Masters Program University of Wisconsin-Stout Menomonie, WI 54751 (Students should STUDY this manual at the beginning of practicum. Doing so will answer most questions and will improve the overall clinical experience.) CONTENTS TOPIC PAGE INTRODUCTION……………………………………………………………… 1 PRACTICUM…………………………………………………………………… 1 Grading………………………………………………………………….. 1 Practicum Attendance……………………………………………………. 2 Staff Meetings…………………………………………………………… 2 Transitioning to Seeing Clients …………………………………………. 3 On-Campus Supervision…………………………………………………. 3 Definition of Supervision………………………………………………... 4 Required Contact Hours…………………………………………………. 4 Co-Therapy………………………………………………………………. 4 Observing from Behind the Mirror……………………………………… 5 A Note On Team Hours ………………………………………………… 5 Practicum Semester Schedule …………………………………………… 6 Appropriate Therapeutic Modalities……………………………………… 6 Emphasis on Conducting Relational Sessions……………………………. 6 Off-Campus Practicum Expectations……………………………………. 7 Participating in the Sreening of New Applicants to the MFT Program … 8 THE CLINICAL SERVICES CENTER…………………………………………. 8 Mission……………………………………………………………………. 8 Clinical Services Center (CSC)…………………………………………... 8 Clinic Manager……………………………………………………………. 8 CSC Orientation: Staff & Student Therapists‟ Responsibilities…………. 9 Ethics and Non-Discrimination ………………………………………… 9 Emergencies, and Duties to Warn and Report……………………………. 9 Contact with Clients Outside of a Clinical Site…………………………... 10 Physical Space and Confidentiality………………………………………. 10 Client Intakes and Scheduling……………………………………………. 11 Session Reminder Phone Calls…………………………………………… 11 Billing and Cancellations…………………………………………………. 11 Record Keeping and Transportation, Storage and Transmission of Confidential Material ..……………………………………………… 12 Records…………………………………………………………………. 12 Case Staffing ………..…………………………………………………. 13 Student Work Desk and Computer and Constructing Client Records ..… 13 Room Maintenance……………………………………………………… 14 End Sessions On Time…………………………………………………... 14 Telephone Use…………………………………………………………… 14 Office Security/Locking Up…………………………………………….. 15 I.D. Card Access…………………………………………………………. 15 Pick-Up Drawers………………………………………………………. 15 Child-Subsystem Therapy Room (Clinic Room 241)……………………. 15 Systemic Dynamics Among Classmates…………………………………. 16 APPENDICES……………………………………………………………………. 16 RECORDING CLIENT CONTACT AND SUPERVISION HOURS……. 16 Required Client-Contact and Supervision Hours…………………. 16 Weekly and End-of-Term (Semester) Hour Recording Forms……. 16 Weekly Off-Campus Form………………………………… 17 Weekly On-Campus Form…………………………………. 18 Semester Cumulative Client/Supervision Form……………. 19 Instructions for Completing the Hours Forms……………….…….. 20 Evaluative Process and Criteria …………………………………... 21 Co-Evaluation Competance Form…………………………………. 22 INTRODUCTION Most students experience a mixed bag of emotions as they advance into practicum. The excitement of being able to participate in an actual therapy session in order to apply the clinical concepts learned in the classroom is tempered by the fear of demonstrating complete and total incompetence in full view of classmates, supervisors and clients! However, students soon realize that all of these people -- including the clients -- are tremendous supporters of their professional development. Everyone involved is wonderfully patient and supportive as student therapists become increasingly skilled at conducting therapy. While there will be some “difficult” clinical situations along the way, these are often the best learning experiences, and someone will always be present to provide support and consultation, including supervisors, co-therapists, clinical team members, and the clinic manager. The purpose of practicum is to allow students the time and opportunity to transform the conceptual material learned in the classroom into tangible techniques and procedures that can be applied in actual clinical practice. By the end of practicum, students should be able to demonstrate clinical competencies expected of an entry level Marriage and Family Therapist. (It is not realistic to expect more thorough mastery of the competencies until a therapist has had two or more years of post-graduate clinical experience and supervision. This is built into the state licensing process as described in the MFT Program Manual distributed at the beginning of the MFT program.) The entire practicum process has been continuously fine-tuned over the decades to result in an optimum learning experience. This manual describes the practicum structure as well as the policies and procedures of the Clinical Services Center. It also delineates the clinical competencies and evaluative criteria used to guide and assess the student‟s development. While student therapists may not believe it at the beginning of their clinical year, by the time they graduate each will be able to manage a wide range of clinical scenarios and procedures without the need for intensive outside support/supervision. PRACTICUM Practicum is much more than direct client contact. It is a class in the full sense. When not working face-to-face with clients students are involved in other activities such as case staffing, paperwork, treatment planning, working as a team member behind the mirror, phone calls to clients and networking with other agencies/treatment providers, and individual and group supervision. Practicum also involves advanced reading and case videotape study. There should be little “down time” in practicum. Practicum involves actual MFT practice with actual clients. Much of it will occur on campus on Mondays and Tuesdays from 1 p.m. to 9 p.m. at the Clinical Services Center (CSC). The CSC functions as an outpatient mental health clinic. The student is expected to adhere to the standard rules of professional decorum, ethics and legalities as taught in this program. For a review of professional ethics students should go to http://www.aamft.org and for the most up-to-date information on state statutes and rules related to MFT practice go to http://drl.wi.gov/profession.asp?profid=24&locid=0. Grading. Throughout the “Practicum” portion of this document, much emphasis is placed on grading. While at times this might appear threatening, it should be pointed out that major grading deductions or disciplinary actions seldom occur. These only result when there has been a major breech of practice protocol. Everything discussed in this section of the document, as well as that covered in the “Clinical Services Center” section, will be considered when figuring the end of 1 semester practicum grades. Students should also review the “Evaluative Process and Criteria,” and “Trainee Practicum Evaluation Form” sections included in this document that identifies the Student Learning Outcomes and evaluative process that will be used to rate each student‟s performance at the end of each semester. (See “Evaluative Process and Criteria” in appendix section.) Practicum Attendance. Attendance and punctuality is regarded seriously by the faculty and will definitely constitute a major consideration in the assignment of grades. Reference is made to attendance throughout this section of the manual. Faculty regard attendance as a sign of professionalism and responsibility. It is a concrete way for students to demonstrate their level of commitment to clients, the program, their peers, the faculty, and the profession. It is recognized and appreciated that each student will be responding to a variety of family and work expectations, but the faculty trust that as professionals students will manage these elements in a fashion that promotes their being in attendance on the days at the Clinical Services Center (Mondays and Tuesdays) and times (1:00 to 9:00 p.m.) required for this course. (Summer practicum is Monday only, from 1:00 to 9:00 p.m.) A minimum of one additional day each week is also expected at an off-campus placement (discussed below), although most students do more. Practicum is the primary experiential learning component of the program. A student cannot learn if they are not present. Therefore, attendance or punctuation related problems, regardless of the reason, are factors that can culminate in lower grades or dismissal from the program. It is expected that students will not miss any part of clinical practicum. However, if for any reason a student must be absent for any part of the day, s/he must immediately inform the Clinic Services Center (715-232-2404) as well as make arrangements with classmates/co-therapists to cover her/his clients. There may be short periods of time when the client caseload at the Clinical Services Center is low. This sometimes occurs early in the fall semester. As mentioned, this should never be idle time. These are excellent times for students to work on a team from behind the mirror in order to build clinical skill/familiarity and to help the clinical process (for more on team hours, see “RECORDING CLIENT CONTACT AND SUPERVISION HOURS” in this document). When not conducting sessions, it is expected that students will be observing other sessions and sharing their observations with classmates. In those rare circumstances when a student is not seeing a client, doing paperwork, working on a team, attending supervision, reading clinical books/articles or reviewing a video, s/he may use this time to leave the clinic to do something constructive such as go to the Stout library, go for a short walk on campus, meditate, do yoga, etc. This should be limited in both frequency and in time. The student should let someone know where s/he is in case needed. (This does NOT include running personal errands off-campus.) Staff Meetings. On-campus staff meetings occur from 1:00-2:00 p.m. on Mondays unless otherwise designated by the supervisor responsible for the clinic that week. These supervised meetings are used to do client status updates, case reviews, and to overview common clinical policies and procedures. This includes treatment planning, discussion of diagnosis and issues of imminent harm, mandated reporting, and needs for referral. This time is also used to determine the case schedule for the coming week, assign intakes and other such procedures. This is a vital element of clinical practice and should be regarded as such, as evidenced by one's attendance, punctuality and participation. As mentioned, inordinate absence, or tardiness, for whatever the reasons, can result in grade reduction or dismissal from the program. 2 Transitioning to Seeing Clients. Building the first case load is an anxious time for new student therapists. This is especially true the first semester of practicum. A number of structures are in place to support you in this. (1) Supervision, Staffing and Processing. (2) Co-therapy. (3) Team Behind the Mirror. All are described in this document. On-Campus Supervision. Each practicum student will be assigned to one of the campus based clinical supervisors for their primary supervision. Prior to the start of each practicum term students are asked to indicate which supervisor they prefer to work with. At this time there is not data that conclusively documents that one treatment orientation is uniformly superior to others. Thus, this program does not focus on just one specific systemic-relational treatment orientation. The program supervisors are proponents of different systemic-relational orientations and believe these differences provide important variety and choice for student learning. Students will have become familiar with each supervisor‟s preferred style of therapy (mostly through classroom exposure) prior to starting practicum. This will help them make a reasoned choice. As often as possible the supervisors try to honor student requests. Supervision consists of both individual (1-2 supervisees with a supervisor) and group (3-14 supervisees with a supervisor). Fall/Spring individual supervision is required a minimum three out of four weeks (although weekly is recommended), and group occurs weekly. Due to shortened clinic hours, summer requires individual supervision every other week and weekly group. Individual Supervision: Each student is responsible to schedule and attend supervision, usually on a Monday or Tuesday at the Clinical Services Center or in the supervisor‟s office. Each individual student is expected to be prepared to discuss, as cogently as possible, their ongoing cases. Each should bring all of their active client files with them. Each MFT supervisor will routinely check and evaluate the clinical charts of their supervisees. It is also strongly encouraged that student therapists record every session at the CSC and also have it available for supervision. When not being used, all recordings are to be kept in the locked file cabinet at the CSC for confidentiality. Be aware that at least 100 hours of total supervision is required, with minimally 50 of these hours being either live or video/audio assisted. (Please refer to “RECORDING OFF AND ON CAMPUS CLIENT CONTACT AND SUPERVISION” in this manual for a description of supervision and the student‟s responsibility for keeping records in this regard.) Group supervision runs promptly from 8:00-9:00 p.m. on the evening the CSC supervisor is present. Everyone is expected to end their cases by 7:50 p.m. in order to be ready to participate. The purpose is to process sessions that were observed, and to bring a sense of closure to the clinical day. Students who receive feedback on cases the supervisor observed live can count this as direct group supervision, other students count it as case review. Therapists who have had a particularly difficult session may need to de-brief as well as receive support/reassurance and new ideas. It is amazing how student therapists, by combining each other‟s strengths and knowledge, are able to generate a thorough systemicrelational understanding of each case and an appropriate treatment intervention/plan. All student therapists benefit as a result of this supervision. Supervisors refer to this as the “Wise Group Mind” (analogous to Bateson‟s idea of “Mind and Nature” and the emergent properties of systems). This processing also occurs on the night the floating supervisor is not present, but it is not counted as supervision. As always, attendance and participation is required. Finally, each student will be expected to keep current in assigned readings or other “homework” that they may receive from their supervisor. The supervisor will look for the student to apply insights from supervision to their current caseloads. For example, over the years, there has been a definite positive correlation observed between the level of therapeutic competence developed during the second year of the program and amount of clinical reading completed. 3 Definition of Supervision. For program and COAMFTE accreditation purposes, students must keep a record of the amount and type of supervision received during the clinical component of the program. Standard forms are provided for this use later in this manual. Each student therapist will use them to record supervision that is received both on and off campus. The types of supervision are: A. Individual Supervision One-to-one meeting with supervisor to discuss cases or view recording of session. Meeting with supervisor and co-therapist (no more than one other supervisee and yourself). When observed from behind a mirror by a supervisor, and you receive individual feedback on that session with no more than one other student present (otherwise it is group). B. Group Supervision Meeting with a supervisor and three to fourteen supervisees to discuss active cases, view recordings and/or discuss therapeutic application of various constructs and techniques. Students behind the one-way mirror may receive credit for group supervision provided: 1) at least one supervisor is present behind the mirror, 2) there are no more than fourteen students present (including the therapists), and 3) the supervisory experience involves an interactional process between the student therapists, the observing students, and the supervisor. Required Contact Hours. Each student therapist must accumulate 500 hours of face-to-face client contact time during their practicum year in order to graduate. Of the 500 total hours, at least 150 hours must be working with people in on-going relationships, the most obvious being couples or families. Up to 75 of the total 500 hours of client contact can be gained by working as part of a therapeutic “team” (defined later in this document). Each student must also have 100 hours of supervision, with at least 50 of them being live, video or audio (audio is allowable but less preferred). All of this is described in great detail in the “RECORDING CLIENT CONTACT AND SUPERVISION HOURS” section of this manual. Co-Therapy. Co-therapy is encouraged at the CSC. It allows developing therapists the chance to support one another both during and between sessions -- an opportunity that will be rare after graduation. It also allows greater intervention flexibility in sessions. For example, therapists can demonstrate to clients how to communicate effectively, how to cross-reference perceptions with one another and model various interpersonal processes within the session itself. The following procedures are an important part of the co-therapy process: A. Pre-session: Work together to anticipate what the family may present and formulate possible session plans. While this helps the student to prepare for the family, it also helps the 4 student to become familiar with their co-therapist's therapeutic style. This pre-session coordination is essential. It should include agreeing on a single theoretical approach, or at the very least coordinate how different approaches will be used without contradicting one another. B. Within-session: co-therapists can work effectively by learning to read one another, taking mid-session breaks (highly recommended) to consult with one another and the team or supervisor, cooperatively changing strategies, and using their interaction to model changes for the family during sessions. Co-therapists should try to balance their interaction, such as taking turns as the lead therapist both when doing treatment planning and when in the room with the clients. C. Post-session: follow-up is useful for reviewing progress in the session, sharing inferences concerning family structure, formulating possible strategies to cope with changes, and deciding what information belongs in the progress notes. It is often advantageous to view the case recording together at some point before the next session. This can occur in or out of supervision. Observing from Behind the Mirror. As is evident, high priority is placed on teamwork. This includes every student being behind one of the mirrors observing/assisting classmates when not busy attending to one of their own cases. The job of the student team behind the mirror is to support the student therapists in the room by generating ideas about therapeutic processes and potential interventions, and sharing these with the lead therapists at the appropriate time. The method by which ideas are shared with the primary therapists is determined by the therapists. They might welcome an occasional “call in” from the team using the room phone. Most seem to prefer to take a short mid-session break in order to consult with the observers in another room. Some student therapists may value having a “reflecting team” visit with them and the clients in the therapy room (participants should be well schooled on how to conduct a reflecting team). Finally, some therapists might not want any interruptions and prefer consults only before and after a session. This usually occurs in a student‟s last semester of practicum when they are more confident. Whatever the method of consultation employed, the therapist(s) in the room always have the final say on how to proceed with their clients because they know what they are most capable of and they have the most direct relationship (and therefore, responsibility) to their clients. Observers should not take it personally if their intervention/idea is not used. Finally, remember that the clinic supervisors always have the option of intervening at any time in any clinical process that occurs in the CSC. It should be noted that clients sometimes refuse to allow observation. This is rare and we urge student therapists not to give in easily to this request. Acknowledge the client concern, and reassure them of the purpose (i.e.: to provide the best services to them) and confidentiality that goes with observation. Encourage them to try it for a session or two and then revisit their decision. If they still adamantly refuse, they must at the very least allow recording of every session and observation by a supervisor. Because this is a training facility clients cannot be seen without a supervisor having total access. If the client(s) refuse supervision (this almost never happens), they cannot be seen at the CSC and will need to be referred to another clinic. A Note On Team Hours. Up to 75 hours of the required 500 client contact hours can be acquired by regular, live participation on a therapy team. It is recommended that therapists acquire many of these early in their practicum experience before building a high caseload as a way of easing the transition into working face-to-face with clients. Team hours also allow therapists to practice collaborative teamwork and refine treatment planning skills. Not all observation counts as 5 “team.” To qualify, the following conditions must be met: 1. pre-approval from the lead therapist(s) in the room and a supervisor; 2. monitoring of the case from intake to termination, only direct observation counts as client contact; 3. assist the primary therapist(s) in case preparation and debriefing, including the construction of hypotheses and interventions -- but know that the therapists in the room are the “team leaders.” They and the supervisor(s) have the final say with regard to the resulting treatment plan; 4. respect the therapist(s) and clients (e.g., Be on time. Do not interrupt or disturb the actual therapy session unless prearranged with the therapist(s) and clients); and, 5. record client contact hours gained through live team participation separate from those gained through regular face-to-face client contact (use the "Team" row on client contact forms to designate these hours (see “RECORDING CLIENT CONTACT AND SUPERVISION HOURS” in this document.) Practicum Semester Schedule. The summer, fall and spring term practicums start one week before the regular term classes begin and go one week beyond when courses normally end. This is to reduce the amount of time clients go without therapy. Fall and Spring is M & T 1-9 pm; Summer is M only, 1-9 pm. The academic year schedule is always available through the UW-Stout homepage http://www.uwstout.edu . This practicum schedule typically leaves two-three weeks between terms when sessions are not scheduled. Vacations must be planned accordingly. The clinic remains open between semesters, however. Therefore, while sessions are not normally scheduled during this brief interim period, students may schedule cases during this time if there is value or need. Be sure to consult with the Clinic Manager (Tiffany Hayden; see “Specific Ground Rules…” section in this manual) at the CSC to insure which rooms and times are available. Appropriate Therapeutic Modalities. WI statutes state that, “a supervisor may not permit a supervisee to engage in any practice that the supervisor cannot competently perform” (from DRL Training License Application form). The MFT program is designed to train students in the use of systemic-relational therapies. This includes such therapies as studied in the primary MFT classes. Intergenerational, experiential, structural, strategic, solution-focused, narrative, cognitivebehavioral and systems-relational based eclectic approaches (such as emotion-focused or internal family systems) make up the bulk of appropriate approaches. All four supervisors recognize and appreciate that other useful approaches exist. Yet, unless the student AND one of the supervisors is appropriately trained in a specific approach, it cannot be performed at the CSC. There may also be times when a supervisor does have the training but an approach is not used at the CSC because it is not what the program is designed for. In the past this has included such things as animal assisted therapy, religion-based therapy, and drug treatment (see also the conditions for doing Play Therapy discussed next). Any question about the appropriateness of an approach should be directed to a supervisor. Emphasis on Conducting Relational Sessions. Many MFT approaches are designed to include as many people who are involved in the relational system as possible. This is the preference in the MFT program. Many clients (and many non-MFT therapists) are socialized to think in individual terms. Thus, they sometimes assume that only one member of a system (the “identified patient”) can or should attend sessions. It is strongly recommended that student therapists discuss during the initial phone contact with clients the importance of having other members of the involved system attend the sessions, at least early on. Later sessions might result in other arrangements. While such 6 separate subsystem assessment can help with systemic-relational level treatment planning, separate subsystem sessions should be conducted only as needed based on the student therapist‟s clinical judgment. Clients should be reminded of the “No Secrets” component of “Informed Consent” before proceeding to subsystem sessions. It is further recommended that systemic-relational sessions be resumed as soon as subsystem meetings are no longer necessary. At the CSC, it is encouraged that the same therapist or co-therapy team work with the different subsystems themselves rather than disperse family members among different therapists. This decreases (1) the need for clients to establish yet another therapeutic relationship with a new therapist, (2) the likelihood of miscommunication or competing agendas occurring between therapists, or (3) the likelihood of therapists or clients becoming triangulated between subsystems. Systemic therapists are expected to be able to work at the levels of individual, couple and family systems. From a systemic perspective, so long as the therapist has the skills for working with the problems being presented, referring subsystems to other therapists is not only unnecessary, but in many instances counter-therapeutic. This being said, sometimes it makes sense to have some separate meetings with various subsystems of a family, such as having some individual meetings with members of a couple, or separate meetings with children and parents. In certain circumstances people might find it easier to “open up” with the therapist if other members of the family system are not present in the same room. However, it is usually best for members of the system to agree to this arrangement in advance, together. Yet, sometimes making this agreement jointly is not clinically sound practice. Such may be the case where the therapist suspects that a person is abused, threatened or intimidated by a family member or is unsure how to bridge a “loaded” subject with a family member. Here the therapist is wise to assume responsibility for initiating meetings with separate subsystems. (Notes: (a) Student therapists should not be conducting “Play Therapy” sessions unless they have appropriate Play Therapy training. However, they may conduct separate sessions with the child subsystem working from a systemic perspective as a part of assessing/treating the larger family system. In these instances, child-subsystem sessions are usually intermingled with therapy sessions that include the primary caregiver(s). (b) Cases involving the threat of abuse or other harm should be staffed with a supervisor regarding how to proceed and whether it is safe to hold couple/family meetings.) Off-Campus Practicum Expectations. The same expectations for supervision, client-contact, demonstration of MFT competencies and attendance policies apply to off-campus practicum sites (as indicated in the attached “Scope of Work” document). Furthermore, it should be noted that it is not wise to change a site once clients have been seen there. This is not good for the clients or the site, and is likely to cost the student client contact hours due to lost momentum. It could also cause ill-will between the site, the student and the MFT program. The student could end up with a lower grade, an “incomplete” for the course, or (worst case scenario) dismissal from practicum/program. Any problems with an off-campus site should be discussed with the MFT Program Director before the student takes any action. Also, each student must remember that s/he is a guest at the offcampus site. Be gracious and respectful. The goal is NOT for a student to make it her/his responsibility to change the way a site operates. A student might not agree with everything that is done (or not done), but unless it is illegal or unethical, the student‟s job is not to overhaul the system, but simply learn from it. 7 Participating in the Screening of New Applicants to the MFT Program. Every February, approximately 24 applicants to the MFT program will visit the campus for a memorable () oneday interview/screening process. Twelve will visit on a Monday and twelve on Tuesday. In the morning they meet with members of the MFT Admissions Committee and one MFT student representative (usually the Graduate Assistant) for the verbal interview. In the early to mid afternoon they meet with the second year MFT students in two shifts of six applicants to take turns playing the therapist in the role-play in CSC room 239. (On these two days, regular CSC activities (i.e.: clients, staffing, supervision) should not be scheduled until after the screening is completed, usually around five p.m.) Consequently, in mid January, second year students are asked to design a clinical scenario in which four play a family seeking services at the CSC. The family should be slightly challenging but not overwhelming (applicants are already very nervous). The remaining students will be behind the mirror with a screening instrument recording their impression of the applicants‟ performance. (Students‟ ratings are compared with the morning interview ratings to get a sense of overall performance of applicants.) Time is allowed at the end for applicants to process the role-play experience amongst themselves, which is also used as part of the screening. Finally, some time should be allowed for applicants to question second year students about their experience of the MFT program. More details will be provided by the Clinic Manager (Tiffany Hayden) and the MFT Program Director & Clinic Director (Bruce Kuehl) as the interview date nears. THE CLINICAL SERVICES CENTER Mission. The UW-Stout Clinical Services Center (CSC) provides a practice setting for welltrained and supervised Marriage and Family Therapy and School Psychology graduate students. It does this by providing affordable individual, couple, family and group therapy services and educational assessment services to the general public. Clinical Services Center (CSC). The on-campus facility where clients are seen is known to the MFT students as the “Clinical Services Center” (CSC). It is actually a multifaceted lab facility that serves numerous other programs and courses on campus, such as the School Psychology, School Counseling and Mental Health Counseling programs. Because it is space that is shared, there are specific days, times and rooms that are available to MFT students, as will become clear later in this document. Scheduling has to do with (a) coordinating the use of the facility and (b) maintaining client confidentiality. All CSC scheduling goes through the Clinic Manager. Clinic Manager. With regard to the MFT program, the role of the Clinic Manager is to attend to the outside-of-session, non-clinical aspects of the CSC as described below. (By contrast, all intherapy, clinical questions are to be directed to one of the MFT supervisors.) For example, the clinic manager is responsible for recording the CSC budget, answering the phone during daytime hours, forwarding messages to students, forwarding new intakes to the practicum supervisor, overseeing the filing system including tracking the paperwork and billing status of active clients, monitoring the scheduling of clients and use of the CSC rooms, overseeing the reception area, stocking office materials, and supervising clinic staff such as graduate assistants, among other things. Student therapists should always let the Clinic Manager know when they are going to be around in case she has messages for them. The Clinic Manager (and the Work Study student and Graduate Assistant under her supervision) have the right to remind practicum students when they are not following established procedures concerning scheduling, billing, paperwork/files. Clinic Manager hours: Monday, Tuesday, 8:30 a.m. – 4:30 p.m. and Thursday, 8:30 a.m. – 3:30 8 p.m. These hours have been flexible and may vary at times. If she is not working and a student has important time-sensitive questions/concerns, they can call her at home - 962 -2113. Graduate Assistants will be staffing the desk and phone on Wednesdays and Fridays; days which pertain primarily to School Psychology students. CSC Orientation: Staff & Student Therapists’ Responsibilities. The Clinic Manager along with the MFT Program Director and Clinic Director will orient students and support staff (graduate assistants) to the CSC procedures at the beginning of their practicum or work experience. After this, it is each person‟s responsibility to follow the procedures as outlined. If a student or staff member does not understand a procedure, s/he should ask for directions. Students/Staff must quickly master such things as how to schedule clients using the room schedule book, handling of records (including filling out the appropriate paperwork and keeping records current), properly filling out billing forms, being prompt and professional toward clients and peers, and calling in on those rare occasions when s/he will be absent or late (see “Attendance” in “PRACTICUM” section), etc. They must also be well versed in the importance of maintaining confidentiality and securing records. The ability to master these procedures will be reflected in the practicum grades or employment performance evaluations. Because these procedures are highly important, the Clinic Manager or Clinic Director will point out to a student/staff when s/he is not following them. The Clinic Manager will also inform the Program Director and/or the student‟s immediate MFT supervisor. Expedient remediation on the part of the student/staff is expected. If the problem is serious or persists, a request can be made to the MFT Program Director/Clinic Director for a joint meeting of the involved parties. Ethics and Non-Discrimination. As discussed in the course “MFT 755: Professional Issues in MFT,” all students must adhere to the Ethical Code of the AAMFT. Breach of this ethical code may result in disciplinary action, including dismissal from practicum or the program. (For the most current code of ethics visit: http://www.aamft.org) Furthermore, the same student nondiscrimination policy described in the MFT Orientation and Academic Advisement Manual applies to clients as well. The Clinical Services Center strives to create a safe and supportive clinical experience for all clients. The Center provides a context in which diversity and non-discrimination are addressed, practiced and valued. “It is the policy of UW Stoout to provide equal opportunity to all persons regardless of race, color, sex, creed, age, ancestry, national origin, sexual orientation, gender identity/expression, political affiliation, marital status, disability or arrest or conviction record in its education programs, activities and employment practices. Racist and other discriminatory conduct will not be tolerated within UW Stout,” (http://www.uwstout.edu/affirm). The UW-Stout Clinical Services Center seeks to enhance the lives of clients that are diverse in these many ways, including religious affiliation, ethnicity, family composition, educational and socioeconomic background not addressed in the UW Stout policy. Emergencies, and Duties to Warn and Report. All cases of suspected child abuse encountered by a therapist must be immediately reported by that therapist to the appropriate authorities, such as Child Protective Services or the Sheriff‟s office (if CPS is closed). Also, all cases of imminent harm posed by a client either to his/herself or another requires that the therapist take reasonable protective steps (i.e.: suicidal persons who will not agree to a reasonable safety plan are sent to the hospital, by police escort if necessary. If there is a real threat of interpersonal violence, the student therapist must call the potential victim AND call the police). Every student therapist must know how to assess the level of risk for harm, as covered in her/his training. This procedure must be reviewed with a supervisor until the therapist-in-training is confident that s/he can conduct such an 9 assessment in actual practice. Any client cases containing issues of the above nature should be brought to the attention of a supervisor for staffing within a reasonable time period. If a student therapist needs immediate guidance and a supervisor is not physically present, their phone numbers are on display by the clinic phone as well as listed in the Practicum syllabus. In case of clinical emergencies, seek the supervisor most readily available. This includes both on and off campus cases and supervisors. Clients who call with an emergency when the CSC is closed will be told by voice message to call the Dunn County Human Resource Clinic at 232-1116 or if life threatening call 911. These lines are answered 24 hours per day. Student therapists or staff should not give their home phone numbers (or those of the supervisors) to clients. This is a personal boundary issue that can sometimes lead to intractable problems. (Have you seen the movie “What about Bob”? ). If a client has an urgent need to talk with a student therapist or supervisor outside of a session they should call the CSC. If the therapist/supervisor is not present at the CSC, a staff member will phone her/him to pass along the client‟s message. The therapist/supervisor can then contact the client as the situation warrants. If a client calls with a life/death emergency, who ever first becomes aware of this must proceed as discussed above in reference to “Emergencies…”. Contact with Clients Outside of a Clinical Site. Student therapists must be aware that sex with clients is against the law and against the AAMFT Code of Ethics (including ex-clients). Furthermore, other kinds of multiple relationships with active clients are to be avoided. These same expectations apply to staff. While rare, student therapists may sometimes run into a client in public. Student therapists are required by ethics and HIPAA to maintain client confidentiality in these situations. If a client initiates a greeting or conversation, the student therapist can acknowledge her/him but should not lead the conversation beyond what the client is volunteering, especially not to “therapy talk.” In most instances, it is best to keep the conversation brief and focused on “social talk.” Save “therapy talk” for in the sessions. Violations in this area are subject to serious consequences depending on the infraction, possibly including reporting to the legal authorities, the ethics board and dismissal from the program. Physical Space and Confidentiality. All personnel with access to the CSC will maintain confidentiality of case material, both within the Clinical Services Center and away from it. This includes all student therapists and staff. It is not appropriate for students to congregate in the reception area of the Clinical Services Center on "clinic days" nor is it appropriate to discuss case material over coffee in the Student Union or other places where conversation may be overheard. The violation of this rule could result in immediate expulsion from the program. In this regard, when waiting for clients, student therapists are to use the processing room in the back of the CSC as a place to gather. To congregate in the reception area can create an uncomfortable sense of "being on display" for the clients gathered there. Therapists should move to the reception area only at the appointed time to greet their clients. Sometimes a student might know someone from the university or community who is seeking therapy at the CSC. When this is the case, respect the right to confidentiality by not observing their sessions or being involved in the related group processing. Special Guests: No one is allowed in the CSC without proper authorization. Mutual cooperation is solicited during times when special guests are brought into the clinic for things such as first year student observations, a clinical workshop/demonstration, a clinic tour, screening student applicants, or COAMFTE accreditation visits. Friends and family are definitely not allowed into the clinic. 10 Client Intakes and Scheduling. After being assigned an Intake/Client, the therapist must write her/his name, the co-therapist‟s name, and the therapists‟ individual supervisors‟ names next to "Clinician" on the pink intake form. Write legibly – ALWAYS – on all forms, otherwise you will be asked to rewrite it (a mass storage device (e.g.: flash drive) is useful in this regard). S/he must make a copy of the intake form and put it in the designated drawer at right side of the Clinic Manager‟s desk. The original “pink form” goes in the client‟s file. A Client/Intake file must be made immediately regardless of whether the client was able to be contacted. Blank files are located on top of the file cabinet above the MFT active drawers (see “Record Keeping” below). The Clinic Manager must be able to locate the Intake Form in case the client calls again, and all forms should be kept in the Active File section of the locked cabinets. Extra blank forms for the files are located on the right side of the student work desk. Please make sure to let the Clinic Manager know when running low on any of these forms. The student therapist should try to contact the clients by telephone to briefly introduce her/him self and schedule a session as soon as possible. It may take more than one attempt to reach them. Always be pleasant and professional in order to begin establishing a therapeutic relationship. Whomever is scheduling the client should consult with their co-therapist beforehand to know their availability. (Do not double-book.) Whenever possible, intake sessions are scheduled for 2 hours but billed at the same price as a regular 1 hour session (however, regular sessions may also be longer in length if warranted). If unable to make contact by phone within one week, please send the client(s) a letter. After about one week more, if they have not initiated contact, please fill out the Closing Summary saying the clients was unable to be contacted and never seen, and let the Clinic Manager know that the file should be put in the Inactive Files. NEVER PUT FILES IN THE INACTIVE FILES DRAWER FOR TIFFANY. There are other items she has to include in the file prior to filing. Once a client is scheduled, write the designated appointment time in the appointment book kept at the student work desk. (Do not remove the schedule book from this area of the room.) Please enter the client's full name and the therapist(s) last name(s) in the appropriate day, room and time slot of the schedule book. Also, if clients do not know where the CSC is located, please give verbal directions and send them a map (maps are kept at the work desk). When a client arrives before 4:00 p.m. and they are driving a vehicle, MAKE SURE THEY KNOW TO PARK IN LOT #27 (South of the General Services bldg.) AND ASSIGN THEM A PARKING PERMIT FOR THE DAY THEY WILL BE HERE. The student therapist may mail the permit in advance, or give it to them at the time of the session (if the latter, ask them to arrive early). Session Reminder Phone Calls. You will notice that some clients are inconsistent in attending meetings. A few clients may benefit from a session reminder phone call a few days before their session. A list should be constructed on Tuesday evening before students leave and placed in the MFT folder locked in the file cabinet. An office staff member will make the reminder calls on Friday. Reminder calls are especially important when there has been a long break between sessions, such as between semesters. Billing and Cancellations. Once an appointment is listed in the appointment book, the Clinic Manager will make a receipt for services rendered to use after the clients‟ session. This is referred to as a “Superbill.” The client's name, date of appointment and previous balance will be entered on the superbill. After the session, check what type of service was provided under the “Services Rendered” section and the amount of time. There is a space for both the therapist and client to 11 sign. Always list the total charges: $10.00 (for an MFT intake or regular session regardless of session length; $3.00 only if they have a Medicaid card or other assistance. Make a copy of the card for their records) or $100.00 (for a psychometric assessment that requires specialized interpretation, such as the MMPI). It is policy that clients pay every time, but that does not always happen. Therefore, indicate if the client has paid or charged. Never reduce a fee without prior approval of a supervisor because billing can have therapeutic implications that go beyond the apparent fiscal need of the client. Keep in mind that if there was a previous balance to add that to the current day's charge. Give the client the YELLOW copy of the superbill. Retain the pink copy as it is essential for bookkeeping. When done - put the superbill and money received in the deposit box. Remember – the CSC is not able to make change - exact amount only. Whenever a client cancels a session, tell the Clinic Manager (or at the very least, leave her a note) and place a large “C” over their names in the appointment book as soon as possible so that she does not make an unnecessary superbill. This also lets other therapists know that the room is available for use. NEVER THROW A SUPERBILL AWAY!!! Record Keeping and Transportation, Storage and Transmission of Confidential Material . All client files should have the same basic information in them. There are blank files made out for use with each client. Each contains the needed forms. The blank files are located in the top far right storage file, above the “Active MFT” client files. Please make sure that all information is filled out in a timely manner. Make sure all client's files are kept in the lockable filing cabinet. NEVER take any part of the files out of the CSC or supervision areas. Students do not want to be responsible for lost/missing/stolen files. A breech of confidentiality along these lines is a serious offence that could result in disciplinary action toward the student. Each student should become very familiar with the "paperwork" that goes in each client file. While the amount of paperwork can be irritating, it is absolutely essential. The forms used in the CSC reflect the standard of the field and therefore are characteristic of what is utilized in any clinical setting. Each MFT supervisor will routinely check and evaluate the clinical charts. The federal Health Insurance Portability and Accountability Act (HIPAA) requires that clients are informed of the privacy of their records. This includes spoken, written and electronic health information. Behavioral health (i.e.: psychotherapy) records qualify. Thus, as mentioned above, unless being used in the Clinical Services Center, all records are to be kept in the locked file at all times. Under no circumstances are client files to be removed from the clinic or supervision areas. As with client files, all recordings of sessions should be treated with the utmost confidentiality and kept in the locked cabinet. No confidential client data is to be stored or transmitted in electronic fashion (i.e.: on computers). All case notes typed on a computer must be printed and securely stored, and deleted from the computer. Storage devices may be used (e.g.: flash drive) but must be secured in the locked cabinet where files are kept. Furthermore, no cases shall be discussed outside of secure supervision and group processing contexts. Poor discretion or judgment in the maintenance of confidentiality of this information could constitute reason for immediate discharge from the MFT program or from employment. Records. Before beginning therapy, it is the student therapist‟s job to see that all clients 16 years of age and older understand and sign the clinic‟s Informed Consent and Client Rights Form. There is also a general Client Information form and a Fee Agreement form that must be completed. Included in every file is a Release of Information form with which each student should be familiar in case they need to use it. Whenever a student is going to request information 12 from other people or agencies that have been involved with the client, the client must first give permission by signing a release form. Likewise, information cannot be released to anyone outside of the CSC, verbally or otherwise, without the client first providing written authorization via a signed release form. This form is also to be kept in the client‟s file. An Initial Assessment form is to be filled out by the therapists after the first session. Among other things, it includes space for session notes, 5 Axis DSM and systemic diagnoses, and treatment planning. Starting with session two, Progress Notes are to be made by the student therapist following each subsequent session. These notes are used to maintain treatment consistency from one session to the next. They should provide an objective, non-opinionated representation of the key content of each meeting. Progress notes are also viewed as an indicator of the quality of treatment being provided. Thus, treatment records serve as primary data when a therapist‟s course of action is questioned, such as during a malpractice or ethics investigation. Records not only assist in client care, they are a therapist‟s best defense, so be sure the records are an accurate description of the services provided. Finally, students must know that the records they construct may very well end up in the hands of future treatment providers or be reviewed by attorneys (this is frequently true in cases of contested child custody). When writing case notes, the student therapist must always keep in mind that other professionals could use her/his records to formulate a treatment plan, make a legal decision, or judge the therapist‟s work. S/he should make every effort to be fair, succinct and professional when writing them. Finally, clients have access to their records. Write accordingly. Always be respectful in your descriptions of clients‟ lives. At the termination of treatment, each file must have a Closing Summary form included. This form must be completed and placed in the client's file as soon as the case is closed, or if closure is ambiguous, placed in the file within at least three weeks of the last session. This is to be completed regardless of the reason for termination of treatment. Each student is encouraged to keep track of their personal performance using the CSC Exit Questionnaire. This form asks clients to rate the quality of services they received and to judge their effectiveness. The completed form is to be kept in each client system's file for later analysis. The purpose of the exit questionnaire is professional development. The results help students know where to focus their effort as they continue to evolve as therapists. This form is not used for grading purposes. Furthermore, major payers (public and private) are demanding improved accountability from mental health providers. Having a performance profile is useful in seeking and maintaining employment in an increasingly competitive market. Conducting a selfassessment as part of the practicum experience is good preparation for future practice. Case Staffing. All Initial Assessments are to be staffed with an individual supervisor within a week of the first session. All imminent harm should be staffed at least weekly. Thereafter, all cases are to be staffed with a supervisor regularly as specified on the green sheet regardless of the number of sessions held in that time. Staffing includes a review of the paperwork, including assessment/diagnosis, treatment plan and goals, and progress toward goals. Each staffing shall be recorded on the green sheet attached to each case file. Student Work Desk, Computers and Constructing Client Records. Students should try as much as possible to use the student work desk when making phone calls or scheduling clients. Students may use the Clinic Manager‟s desk in the evening after she has left, but only when the 13 student desk is already occupied. The Clinic Manager‟s computer is off limits. It is extremely important to her job and the operation of the clinic. Therefore, it should not be used by anyone else. There are computers for student use kept in rooms VR 242 and 344. These computers contain the Initial Assessment, Progress Note and Closing Summary forms. It is highly recommended that students type these records. The completed forms should then be printed and kept in the client‟s “hard” records. In keeping with HIPAA regulations, no client material is to be stored on these computers or transmitted over the internet because it is not secure. Again, use a portable storage device and secure it in the locked cabinet. The computers in 242 are also heavily used by School Psychology students. The educational and psychometric testing programs loaded on these machines are not for use by MFT students. Do not load or delete any programs on any of the computers without first consulting with either the Clinic Manager or Clinic Director. Room Maintenance. The CSC facility will be readily accessible to MFT students. All students who use the facility are responsible for keeping it in form for optimum utilization by others. Any initiative regarding the development and maintenance of this area is encouraged and appreciated. Each individual is expected to assume responsibility for preparation of rooms available for therapy sessions. “If you make a mess, clean it up!” The child-subsystem therapy room especially needs to be put back in order after each use. The therapist should either have the child help or go back after the session to clean up. Nobody else is responsible to clean the room. (Therapists should not sit on the child-sized furniture because it will break.) Other maintenance includes the refrigerator and microwave in the lobby. Please do not abandon anything in the refrigerator & keep both appliances clean. Clean the microwave after each use. If something spills in the refrigerator, clean it up. When eating at the clinic, waste must be placed in the appropriate bins. Students should please be respectful of others, including the custodial staff. Don‟t leave garbage or crumbs for them to clean up. They can quickly forbid the use of any food items in the clinic. End Sessions On Time. Therapy rooms should be vacated by the end of the scheduled session (ten minutes before the hour, with the exception of emergencies). This is standard therapeutic practice and common courtesy. Clinic rooms are heavily used and student therapists need time to transition clients in and out of sessions. Therapists-in-training must cooperate with one another and the respective room schedules. Telephone Use. The telephones are for CSC related calls. The telephone on the student work desk is for student therapist use. There is also a phone in room 242 that can be used for extended conversations or when more confidentiality is needed. The Clinic Manager‟s phone is for back-up purposes only. For all local calls - Menomonie (235), Elk Mound (879), Colfax (962), Downsville (664), Knapp (665), Boyceville (643), Wheeler (632), dial 9 then the full number. If you are not sure if it is a local call, please ask the client or somebody else before dialing. Do NOT dial long distance with 9. For long distance calls - dial 8 then 1. Remember - the area code must be used at all times now. Do NOT dial local calls with 8. The UW-Stout phones are not for personal calls other than the rare call home in the case of a personal emergency, or to announce a change of schedule due to bad weather or some unforeseen CSC event. If a staff member is not at the Clinic Manager‟s desk, student therapists should answer the CSC telephone. This is especially important after she has left for the day. Say "Clinical Services Center" and your name when answering. Make sure to write down messages thoroughly, date it, and put your name on it in case anybody has a question later. The voice mail may also be 14 checked for messages, especially at night when clients are calling for student therapists. There is a note on the phone to get voicemail started, then simply follow the directions through the voice mail system. Again, be sure to write the messages correctly and get them to the person they are for. When needing to transfer a call to another number, press the flash button (you will get a dial tone) then punch in the transfer phone number, when they answer, press the flash button again, and all three of you are on the line, and you may then say "go ahead". If the number you are trying to transfer is busy or does not answer, press the flash button two times, and you will be back with the original party. Press the hold button to put the party on hold while checking on something, but you cannot transfer while on hold. Office Security/Locking Up. The front desk must be staffed at all times. This becomes the student therapists‟ responsibility if a staff member is not present. Responsibility for securing the CSC area and VR 342/344 (upstairs) is assigned to pairs of students on a rotating basis throughout the year (no individual should remain alone at the CSC). The schedule will be established by the clinic supervisor at the start of each term. Please be sure to check all of the following before leaving. Always straighten up both the office and reception area before leaving. Also, please refer to the list above the student work desk for details on rooms and hallways. Responsibilities include: *Be sure front desk is staffed at all times CSC is open *Coffee Pot - turn off/unplug *Lights in all rooms-turn off *Monitors and head phones – turn off *Lock all file cabinets in office * Turn off the copy machine *Lock all doors *Turn off the computers in 242 and 344 *Be sure upstairs MFT Lobby & Resource Area (VR 342) hallway door is locked *Place “session reminder” call sheet in MFT folder in locked cabinet. I.D. Card Access. Practicum students will have access to the West Entrance of the Voc. Rehab. Bldg., the hallway corridor by the CSC, and the back of the CSC using their UW-Stout ID card. This will be de-activated when the student no longer needs access to the Clinic. Pick-Up Drawers. Each student (first and second year) will have a pick up drawer in the reception area of the CSC. These should be checked frequently as they might hold an important message. Any and all messages will be put there, including messages from clients, the clinic manager, supervisors and classmates. If a message also concerns a classmate or co-therapist, be sure to pass the information along. Child-Subsystem Therapy Room (Clinic Room 241). Room 241 is the primary room for MFT students to use when meeting with children. A child-subsystem may be seen as a part of family therapy as discussed in the “Emphasis on Conducting Relational Sessions” section above. By contrast, the “Play Therapy Room” is located across the hall from the CPL rooms and is only for students enrolled in the Play Therapy class. MFT students can use this room as a “last resort” and only if it is not being used by the Play Therapy students. You must check their class schedule before assuming you may use it, and clean it when finished. 15 Systemic Dynamics Among Classmates. As mentioned in the “MFT Program Manual,” differences of opinion will emerge as classmates debate theory, technique and life in general. Choosing partners for co-therapy, negotiating treatment plans and giving/receiving feedback will sometimes intensify things to the point where dissension comes to the forefront. The MFT supervisors have found that this interpersonal rub or “crucible” personalizes education. Properly attended to it has the potential to facilitate tremendous growth in students in the area of self-ofthe-therapist. Practicum students should re-read this section of the “MFT Program Manual.” APPENDICES RECORDING CLIENT CONTACT AND SUPERVISION HOURS Required Client-Contact and Supervision Hours. By the time a student completes all three practicum courses, s/he is expected to accumulate a minimum of 500 hours of total face-to-face client contact at both the Clinical Services Center and at an approved off-campus site that meets the requirements defined in the off-campus „Affiliation Agreement‟ form. Of the 500 total, 150 hours must include therapy with couples and families. The student must also accumulate a minimum of 100 hours of combined face-to-face supervision at both the on and off-campus sites. This results in a combined ratio of 1 hour of supervision for every 5 hours of client contact. It must include 50 hours of direct (live or recorded session) supervision. In addition to off-campus supervision, on-campus supervision consists of individual sessions three out of four weeks during the fall and spring semesters, and once every other week during the summer. (In the rare event a student‟s individual supervisor is not available, s/he should meet with one of the other supervisors.) It also includes one hour of weekly group supervision. Non-compliance can result in a lower grade, incompletion for the course, or dismissal from the program. Up to 75 of the 500 total client contact hours may be accomplished by participating on a clinical team. This requires the team member to be present behind the mirror and contribute to the treatment process from intake through case closing as defined in the Practicum and CSC Manual. Team hours ease the transition to working face-to-face with clients and are best accumulated in the beginning of practicum before the student therapist develops a full case load. Client contact and supervision is further defined on the attached “Instructions for Completing the Client Contact and Supervision Hour Form.” Finally, each student‟s caseload at the CSC will be adjusted slightly up or down according to their off-campus hour production. However, every student must see clients at the CSC through all three practicum semesters, and every student is expected to receive weekly supervision with an on campus supervisor, including discussing their off-campus caseload. A student cannot graduate until these hours are documented and approved by the program director. Weekly and End-Of-Term (Semester) Hour Recording Forms. The forms on the following pages have been constructed to help students record their hours. The hard copy “Weekly” off and on campus forms should be used throughout the semester to record weekly hours, while an excel document has been constructed for students to use to record their end of semester totals. The Excel document automatically tallies the appropriate rows and columns. Copies of these forms will be placed in the student‟s file for progress review each semester. The forms are also necessary to document compliance with program requirements as specified by COAMFTE accreditation standards. Students‟ records will be reviewed when COAMFTE makes its periodic site visit to the program. Therefore, it is important that every student‟s records be accurate. Students should look these forms over closely. All forms have instructions for how to fill them out. All of these forms are made available to the student in electronic fashion. Students should not hesitate to direct any questions regarding the recording of hours to the program director. 16 OFF CAMPUS WEEKLY MFT SUPERVISORY AND CLIENT CONTACT RECORD Insert Semester Date _________ First column to report type & hours of client contact, second column under each date to record type of supervision received that week. *F = Family C = Couple I = Individual In the supervision column specify: **I C = Individual Case Report G C = Group Case Report G = Group T = Team (Group & Team specify I, C, F) I D = Individual Direct (specify live, audio or video) G D = Group Direct (specify live, audio or video) Student and supervisor initial document. Week 1 Client Contact Hrs______ *F_ ___ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 4 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 7 Client Contact Hrs______ *F______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 10 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 13 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 16 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 19 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_____ Week 2 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 5 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 8 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 11 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 14 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 17 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 20 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ 17 Week 3 Client Contact Hrs____ *F_______ **I C______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 6 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 9 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 12 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 15 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 18 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 21 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ ON CAMPUS WEEKLY MFT SUPERVISORY AND CLIENT CONTACT RECORD Insert Semester Date _________ First column to report type & hours of client contact, second column under each date to record type of supervision received that week. *F = Family C = Couple I = Individual G = Group T = Team (Group & Team specify I, C, F) In the supervision column specify: **I C = Individual Case Report G C = Group Case Report I D = Individual Direct (specify live, audio or video) G D = Group Direct (specify live, audio or video) Student and supervisor initial document. Week 1 Client Contact Hrs______ *F_ ___ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 2 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 3 Client Contact Hrs____ *F_______ **I C______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 4 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 5 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 6 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 7 Client Contact Hrs______ *F______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 8 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 9 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 10 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 11 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 12 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 13 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 14 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 15 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 16 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 17 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 18 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 19 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 20 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ Week 21 Client Contact Hrs______ *F_______ **I C_______ C_______ I D_______ I_______ G C_______ G_______ G D_______ T_______ 18 SAMPLE CLIENT/SUPERVISION CONTACT FORM Student Name: ___________________ ___________________________________ Off campus placement setting: ___________________________________ On campus supervisor: ________________ ______________________________________ Off campus supervisor: _____________________________________ SEMESTER ________ Date entered program: (Mo/Yr): _____________________________ Date Left program: (Mo/Yr): _____________________________ CLIENT CONTACT HOURS Site Name & Type Modality (check one) _____________ G On G Off G Internship Indivi Couple Family (relational) (relational) Relational (add couple & family hours) 150 hrs YEAR________ Student's Year in program: _____________________________________ SUPERVISION HOURS Total Client Hours Case Report Live Video (raw Audio (raw (raw data) data) data) 500 hrs (I+C+F) Direct Raw Data (add audio, video & live) 500 hrs Total Superv. Hours 100 hrs IND TEAM xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx xxx GRP TEAM _____________ G On G Off G Internship IND TEAM GRP TEAM _____________ G On G Off G Internship IND TEAM GRP TEAM CUMULATIVE TOTALS (add hours earned at all sites aa CUMULATIVE TOTAL TO THIS POINT IN PROGRAM aa RATIO OF SUPERVISION TO CLIENT CONTACT (1:5) = BB/AA = __________ (SHOULD EQUAL .20 OR GREATER) (RECOGNIZE THE MAXIMUM FOR THE CUMULATIVE AA IS 500 REGARDLESS OF WHAT NUMBER MAY BE.) (This semester) Cumulative supervision to client contact ratio (all semesters) = all bb/all aa = ______ (should equal .20 or greater) Student signature _________________________________ Date: __________ Supervisor signature ______________________________ Date: __________ CLIENTSU.TBL(AAMFT 19 bb bb INSTRUCTIONS FOR COMPLETING THE CLIENT CONTACT AND SUPERVISION HOUR REPORTING FORM SITE NAME AND TYPE: List the name of the site and then indicate the type of site by checking the appropriate box. ON . . . . . . . . . . . . . . . . . . . . On-site practicum placement OFF . . . . . . . . . . . . . . . . . . . Off-site practicum placement MODALITY: This indicates the mode in which client contact and supervision hours were earned. IND . . . . . . . . . . . . . . . . . . . Individual mode for client contact occurs when the student sees one individual, one couple, or one family in the therapy room. (Individual mode for supervision occurs when 1-2 students work with the supervisor.) GRP . . . . . . . . . . . . . . . . . . . Group mode for client contact occurs when the student sees a group of individuals, a group of couples, or a group of families in the therapy room. (Group mode for supervision occurs when 3-14 students work with the supervisor.) TEAM………………………………… Individual or relational client contact hours that are earned as a result of meeting the conditions for working on a team. (Supervision of TEAM client hours is recorded in the IND or GRP rows based on the number of students present with the supervisor as defined elsewhere on this page.) CLIENT CONTACT HOURS: List the number of face-to-face client contact hours earned by each student in each category, and in each modality. INDIV . . . . . . . . . . . . . . . . . When a student sees one individual in the therapy room. This time should be logged in the IND row when a student sees one individual, and in the GRP row when a student sees a group of individuals. COUPLE . . . . . . . . . . . . . . . When a student sees a couple in the therapy room. This time should be logged in the IND row when a student sees one couple, and in the GRP row when a student sees a group of couples. FAMILY . . . . . . . . . . . . . . . When a student sees a family in the therapy room. This time should be logged in the IND row when a student sees one family, and in the GRP row when a student sees a group of families. RELATIONAL . . . . . . . . . . . Add the COUPLE and FAMILY columns together (numbers in the INDIV GRP cell should not be counted as relational client contact). TOTAL CLIENT HRS . . . . . . Add the INDIV and RELATIONAL columns. SUPERVISION HOURS: List the number of supervision hours earned by each student in each category and modality. INDIV VS. GROUP……………. Indiv = 1-2 students with a supervisor; Group = 3-14 students with supervisor. CASE RPT . . . . . . . . . . . . . . All forms of supervision not based on raw data. See definition of raw data below. LIVE . . . . . . . . . . . . . . . . . . The supervisor live observes a student conducting therapy through a one-way mirror, TV monitor, or other observation device. VIDEO . . . . . . . . . . . . . . . . . The supervisor observed a videotape of the student conducting therapy. AUDIO . . . . . . . . . . . . . . . . . The supervisor listened to an audiotape of the student conducting therapy. DIRECT RAW DATA . . . . . . . Add the LIVE, VIDEO, and AUDIO columns. This should be figured as the total number of raw data hours earned. It does not include CASE RPT hours. TOTAL SUPERV HRS . . . . . . Add the CASE RPT and DIRECT RAW DATA columns. CUMULATIVE TOTALS: Total each student‟s client contact and supervision hours in each column, adding all hours earned at different sites together. One row reflects only the semester total; the other reflects the total of all semesters added together up to this point in the program. RATIO OF SUPERVISION TO CLIENT CONTACT (1:5): Divide the number in cell “bb” by the number in cell “aa” (total number of supervision hours divided by the total number of client hours). Place the decimal number in the space provided. It must be at least .20. 20 EVALUATIVE PROCESS AND CRITERIA FOR MFT PRACTICUM All students will be receiving weekly feedback from their supervisors regarding their work in the group and individual supervisory sessions. This feedback will focus on the student‟s progress toward mastering the MFT practicum competencies. These are specified in the evaluation tool that follows. In addition to this, each student will have an end-of-semester feedback session with the supervisors as a group. This evaluation process is intended primarily to promote the student‟s growth as a therapist and will culminate in a grade given formally at the end-of-semester meeting with the supervisors. Each student‟s grade will represent the subjective consensus of the supervisors as all their observations are molded together. Two grades are given per fall and spring semester representing the two sections each student has registered for. Summer practicum has only one section. In keeping with UW-Stout policy, grades may be any combination of A, A-, B+, B, B-, C, D or F. Any student who might be in "danger" of getting less than a B in these practicums will be given early warning of this so that remedial action may be taken. If the supervisors find this to be true of a particular student, a session including the student and clinical faculty will be organized to determine future plans. Worst case scenario, it may be determined that the student is not prepared at this time in his/her life to learn and practice couple and family therapy. This is extremely rare. Since expectations for practicum performance are high to begin with, B grades represent an acceptable standard of performance and are not to be equated with some notion of "failure." Grades above the B level represent varying shades of superior or exceptional performance. In the final analysis, grades are a necessary nuisance. It is the constructive feedback from one‟s supervisors (and peers) that is most important. The criteria listed on the following evaluation tool represent a distillation of the collective thinking of the AAMFT as to what is considered core clinical competencies. It is used at the end of each semester to facilitate the evaluation process. It follows that some students will attain a higher level of performance on some criteria than on others, and different students will display different strengths and weaknesses. Finally, your practicum is not considered complete until all client contact and supervision hours forms (described above) are accurate, complete and turned in to the Program Director. This paperwork is essential. A grade of incomplete may be assigned, a reduced grade may ultimately be assigned, or failure to graduate could occur. 21 CO-EVALUATION OF CLINICAL COMPETENCE UNIVERSITY OF WISCONSIN-STOUT MARRIAGE & FAMILY THERAPY PROGRAM This document serves as an important tool in the authentic assessment of therapeutic competence. Trainees should complete this form in consultation with their on-campus supervisor, and then distribute one copy of this completed form to each of the on-campus supervisors. Trainee’s Name (print, sign, date): ________________________________________________________ Supervisor (sign, date): _________________________________________________________________ Practicum (circle): 1st Semester Semester (circle): Summer Fall 2nd Semester 3rd Semester 3rd Semester plus (specify)___________ Spring PRACTICUM COMPETENCIES Please use the following choices to rate the course competencies listed below: (3) Trainee can apply this competency primarily under self-direction. Supervisors, co-therapists and colleagues used mostly for validation. (Most trainees will merit this rating at the end of their last semester of practicum.) (2) Trainee can apply this competency with moderate support from supervisors, co-therapists and colleagues. (Most trainees will merit this rating by the end of their second semester of practicum.) (1) Trainee can apply this competency with considerable support from supervisors, co-therapists and colleagues. (Most trainees will merit this rating by the end of their first semester of practicum.) (0) Trainee is not able to apply this competency at this time (N/A) Trainee has not yet had the opportunity to apply this competency (first semester option only). _____ 1. Establish client contact, scheduling, fees, and determination of who should attend initial session. ____ 2. Explain client rights, billing process, and obtain informed consent for treatment. ____ 3. Establish and maintain productive therapeutic alliance. ____ 4. Establish DSM and systemic/relational assessment/diagnosis; include client strengths. ____ 5. Utilize genogram and psychometric tools to assist assessment as needed. ____ 6. Develop collaborative treatment plan appropriate to client(s) clinical issue(s), goal(s), and individual/couple/family development. ____ 7. Continually evaluate progress toward goals. Modify treatment plan accordingly. ____ 8. Manage risks, crises and emergencies. Establish safety plans. Report/protect as warranted. ____ 9. Develop termination and aftercare plans. ____ 10. Complete all required case documentation in a timely manner. ____ 11. Maintain professional relations with all personnel at on and off-campus clinical sites. Network with involved stakeholders as appropriate (extended family; other professionals, etc.) ____ 12. Utilize required supervision and collegial consultation at on and off-campus clinical sites. Support colleagues/observe behind the mirror. ____ 13. Attend to personal issues that affect the therapist‟s ability to conduct ethical, effective therapy. 22 ____ ____ ____ ____ _____ 14. Attend to dynamics of power, privilege and difference in client lives. 15. Utilize systemic/relational theory, technique and psychoeducation in a culturally sensitive manner. 16. Practice according to AAMFT Code of Ethics, WI law and professional standards of practice. 17. Work with supervisors and program director to document required client contact and supervision hours, and clinical competence. Total Score _____ Average Score (total divided by 17) Expected Progress: An average score of 0.5 is necessary to advance to second semester of practicum. An average score of 1.5 is necessary to advance to third semester of practicum. An average score of 2.5 is necessary to complete practicum (in combination with adequate client contact and supervision hours). NOTE: Please explain any score of “N/A” or “0” assigned to an individual competency, or any “Average Score” that falls short of expected progress as listed above. This will be used to help you and your supervisor create an individualized learning plan to support the development of increased competency: Required: Additional Comments (Such as reflection on personal/professional growth as an MFT; goals for next semester (or post-graduation)): 23