ISU– MEDICAL HISTORY
advertisement
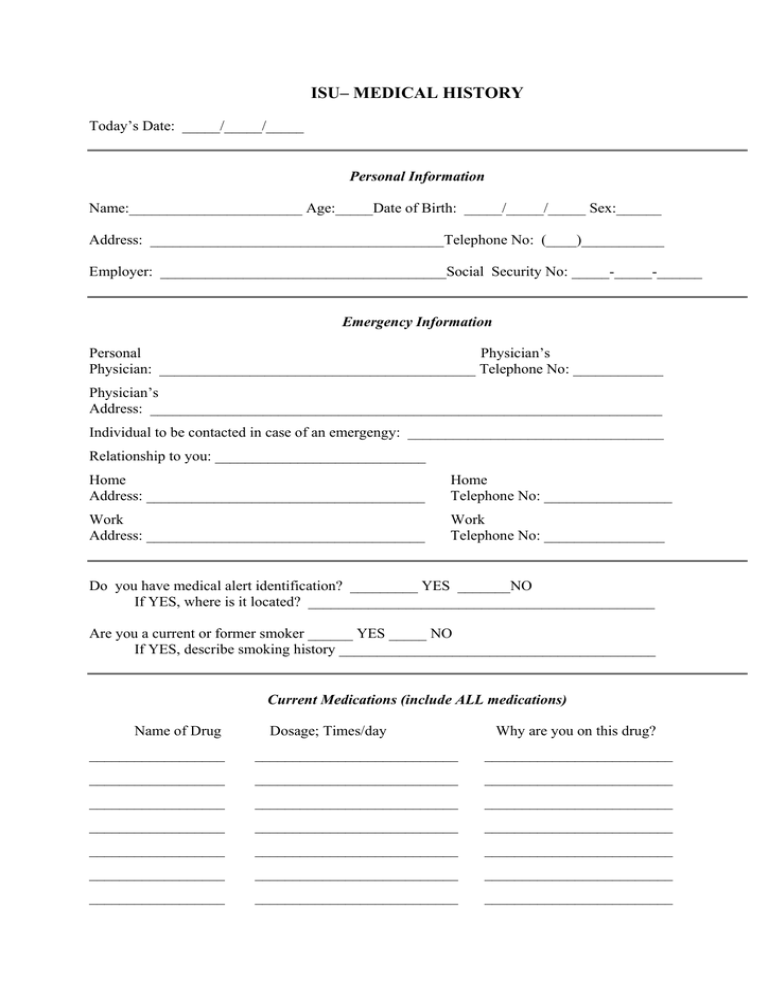
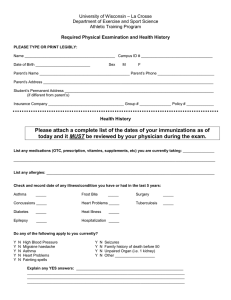
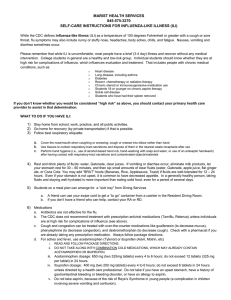
ISU– MEDICAL HISTORY Today’s Date: _____/_____/_____ Personal Information Name:_______________________ Age:_____Date of Birth: _____/_____/_____ Sex:______ Address: _______________________________________Telephone No: (____)___________ Employer: ______________________________________Social Security No: _____-_____-______ Emergency Information Personal Physician’s Physician: __________________________________________ Telephone No: ____________ Physician’s Address: ____________________________________________________________________ Individual to be contacted in case of an emergengy: __________________________________ Relationship to you: ____________________________ Home Address: _____________________________________ Home Telephone No: _________________ Work Address: _____________________________________ Work Telephone No: ________________ Do you have medical alert identification? _________ YES _______NO If YES, where is it located? ______________________________________________ Are you a current or former smoker ______ YES _____ NO If YES, describe smoking history __________________________________________ Current Medications (include ALL medications) Name of Drug Dosage; Times/day Why are you on this drug? __________________ ___________________________ _________________________ __________________ ___________________________ _________________________ __________________ ___________________________ _________________________ __________________ ___________________________ _________________________ __________________ ___________________________ _________________________ __________________ ___________________________ _________________________ __________________ ___________________________ _________________________ Hospitalizations Please list the last three (3) times you have been ill (sick) enough to see a physician, been hospitalized or had surgery. When? What was done (surgery, etc.)? Why was this done? ___________________ _____________________________ _____________________________________ ___________________ _____________________________ _____________________________________ ___________________ _____________________________ _____________________________________ Personal Medical History Do you have any known allergies? ______ YES ______NO If YES, please explain:_______________________ ___________________________________________________________________________________________ Please check the following disease conditions that you had or currently have: ____ High blood pressure ____ Aneurysm ____ High blood cholesterol ____ Anemia ____ High blood triglycerides ____ Diabetes ____ Angina pectoris ____ Jaundice ____ Heart attack ____ Hepatitis ____ Heart surgery (catheter, bypass) ____ Infectious mononucleosis ____ Heart failure ____ Phlebitis ____ Heart murmur ____ Gout ____ Stroke/transient ischemia attacks ____ Kidney stones ____ Rheumatic fever ____ Urinary tract infections ____ Arteriosclerosis ____ Emotional disorder (depression, etc.) ____ Abnormal chest X-ray ____ Asthma ____ Emphysema ____ Bronchitis ____ Thyroid problems ____ Hernia ____ Cancer ____ Epilepsy or seizures ____ Prostate problem ____ Osteoporosis ____ Eating disorder ____ Other Please provide dates and explanation to any of the above which you checked: _______________________ ______________________________________________________________________________________ Recent Illness Have you had any symptoms of illness within the last 3 weeks (such as runny nose, stuffy nose, sore throat, fever, aches, etc) ________ YES _______ NO If YES, please list the symptoms that you experienced: Have you taken any medication within the last 3 weeks for symptoms of illness or pain (aspirin, tylenol, ibuprofen, over the counter cold medications, etc) ________ YES _______ NO If YES, please describe: _______________________________________________________________________________________________ Prior Influenza Immunization Have you received an influenza immunization before? _________ YES ________ NO If yes, please circle the years that you received the vaccine 2002 2001 2000 1999 1998 Activity History Please list any physical or recreational activities that you currently do or have done on a regular basis. List each activity below (ACTIVITIES MAY INCLUDE: walking, hiking, swimming, jogging, water exercise class, calisthenic exercises, badminton, basketball, exercise bicycle, bicycle outdoors, dancing – please list type of dance, farm work – please describe, gardening, golf, horseback riding, skiing-downhill, skiing-cross country, tennis, racquetball, OR ANY OTHER ACTIVITY THAT MAKES YOU BREATHE HARDER) Activity Frequency (days/week) Time (min/session) How long (years) __________________ ______________________ ____________________ ____________________ __________________ ______________________ ____________________ ____________________ __________________ ______________________ ____________________ ____________________ __________________ ______________________ ____________________ ____________________ __________________ ______________________ _____________________ ____________________ Vitamin and Nutritional Supplement Intake Please list below all of the vitamins, minerals, and nutritional supplements you consume NAME AMOUNT HOW OFTEN? ____________________________ ______________ _______________________ ____________________________ ______________ _______________________ ____________________________ ______________ _______________________ ____________________________ ______________ _______________________ ____________________________ ______________ _______________________ ____________________________ ______________ _______________________ ____________________________ ______________ _______________________ THANK YOU FOR YOUR COOPERATION! If you have any questions or concerns please call: Dr. Marian Kohut, Ph.D., 294-8364 SOCIAL ACTIVITY QUESTIONNAIRE NAME _________________________________ Social Activities Please list any social activities that you currently do or have done on a regular basis. Report those activities that you do at least once every 2 months. (Examples of activities: attending classes, playing cards, bowling club, gardening club, member of religious or non-religious social group, church visits, visiting family members, visiting friends, OR ANY OTHER ACTIVITIES THAT INVOLVE SOCIAL INTERACTION WITH OTHER PEOPLE) Activity Frequency (days/week) Time (min/session) How long (years) __________________ ______________________ ____________________ ____________________ __________________ ______________________ ____________________ ____________________ __________________ ______________________ ____________________ ____________________ __________________ ______________________ ____________________ ____________________ __________________ ______________________ ____________________ ____________________ __________________ ______________________ ____________________ ____________________ __________________ ______________________ ____________________ ____________________ THANK YOU FOR YOUR PARTICIPATION IN THE RESEARCH STUDY PLEASE RETURN TO THE ________________________________________ ON ___________________________ AT _______________________________ We will collect a small blood sample from you on this day. SIDE EFFECTS FOLLOWING THE FLU SHOT If you experience any side effects from the flu shot please describe below: ON THE DAY YOU RETURN FOR YOUR BLOOD SAMPLE: Please bring all forms back with you (medical history, diet analysis, consent form). We will ask you to complete a short questionnaire about your attitudes and stress in your daily life. We will also serve a light breakfast. APPROXIMATELY ONE MONTH AFTER THE BLOOD DRAW, OUR REGISTERED DIETITIAN WILL CALL YOU WITH THE RESULTS OF YOUR DIET ANALYSIS. THANK YOU FOR YOUR PARTICIPATION. PLACE A CHECK BELOW IF YOU WOULD LIKE TO SEE A COPY OF THE RESULTS FROM THIS STUDY. ______ Please mail me a copy of the results ______ Please call me with information about the results