ESTIMATION OF CARDIOVASCULAR PARAMETERS FROM NON-INVASIVE MEASUREMENTS
advertisement

ESTIMATION OF CARDIOVASCULAR PARAMETERS
FROM NON-INVASIVE MEASUREMENTS
by
Janice S. Tan
B.S. in Mechanical Engineering
University of Illinois @ Urbana Champaign, 2001
Submitted to the Department of Mechanical Engineering in Partial Fulfillment
of the Requirements for the Degree of
MASTER OF SCIENCE IN MECHANICAL ENGINEERING
at the
MASSACHUSSETTS INSTITUTE OF TECHNOLOGY
January 2003
MASSACHUSETTS
INSTIUTE
0F TECHNOLOGY
@ 2003 Janice S. Tan. All rights reserved.
JUL 0 8 2003
The author hereby grants to MIT permission to reproduc
and to distribute publicly paper and electronic copies
of this thesis document in whole or in part.
LIBRARIES
A uthor..........................................
Certified by.............................
A ccepted by..........................
......................................................
Department of Mechanical Engineering
January 2, 2003
...........................................................................
Roger D. Kamm
Professor of Mechanical Engineering
Thesis Supervisor
.................................................
Ain A. Sonin
Chairman, Departmental Committee on Graduate Studies
Department of Mechanical Engineering
BARKER
ESTIMATION OF CARDIOVASCULAR PARAMETERS FROM
NON-INVASIVE MEASUREMENTS
by
Janice S. Tan
Submitted to the Department of Mechanical Engineering on January 2, 2003
in Partial Fulfillment of the Requirements for the Degree of
Master of Science in Mechanical Engineering
Abstract
Parameters such as Cardiac Output (CO) and Systemic Vascular Resistance (SVR) provide
key information regarding the state of cardiovascular (CV) health; hence they are critical for the
management of patients with CV dysfunction. As current measurement methods are typically
invasive they are not routinely made. If these parameters could be determined non-invasively, it
could prove invaluable for patient monitoring in various clinical and non-clinical settings.
Thus, a computational model of the CV system was developed by Ozawa et al. to describe
blood flow in human arterial networks, allowing for the study of the relationship between
haemodynamic variables usually obtained invasively, such as left ventricular contractility (ELv),
end diastolic volume (EDV), SVR and CO, and the morphology of arterial pressure and flow
waveforms at various arterial locations. Coupled with a system identification algorithm, the model
allows for estimation of these parameters from the shape of measurable Radial Arterial (RA)
pressure tracings.
To validate this model, clinical studies were performed on 5 volunteer patients undergoing
Coronary Artery Bypass Graft (CABG) procedures at Massachusetts General Hospital (MGH).
Measurements of the electrocardiogram and Radial Arterial, Pulmonary Arterial and Central
Venous Pressures were recorded, along with CO and transesophageal echocardiographic (TEE)
images. Subsequent calculations and analyses revealed overall absolute percentage errors of 30.7%
for SVR and 19.9% for CO. Taking into account the inherent error within the thermodilution CO
measurements, this model can produce acceptable estimates for CO, following the guidelines
recommended by precision statistics tests such as Bland Altman and error-gram methods. Good
qualitative comparisons were also obtained between the reconstructed and measured input pressure
profiles. Due to the small sample size though, further testing is being planned to draw more
definite conclusions.
Thesis Supervisor: Roger D. Kamm, Ph.D.
Title: Professor of Mechanical Engineering, Associate Director, Center for Biomedical Engineering
2
Acknowledgements
How do I thank thee, let me count the ways...
To begin, I would like to thank my advisor, Prof. Kamm, for his guidance and trust in me, a wise
shepherd who gave me sufficient freedom to pursue this project and thesis, and yet gently guided
me back on the path when I was led astray. To another patient friend, Mohammad, who believed
in me enough to take me on this project in the first place, and who has been an endless source of
support and encouragement, both personal and professional. At the end of a long day, we can
still share philosophical discussions, and his lessons of tolerance and forbearance, I will strive to
emulate. This thesis would also not have been possible without the help of many others, notably
Edwin Ozawa, Grace Xiao, Marcos Vidal Melo and Ray Chan, and the team of anesthesiologists
and nurses in the Cardiac Anesthesia Unit at MGH. Their kindness and willingness to help a
green graduate student will always be appreciated and remembered.
When things were high, or low or blue, I'm glad I had my family to turn to. Despite the
many miles that separate us, it only seems to draw us closer in times of celebration and need. A
big thank you, especially to my mother, my all-time best friend and #1 cheerleader; and also to
Doris Moore, a mother away from home. Many thanks too, to Sephalie Patel, a friend with the
amazing ability to always make me laugh and see the sillier side of life.
I spent many hours in the Fluids Lab, and would like to thank some cheerful companions
as well, both in the Kamm group - Ana, Belinda, Ernie, Gina, Helene and Jan, and the greater
HML gang. We all know how important it is to have a great extended lab family; I only wish I
had had more time to get to know each and everyone of you better. Thanks be to Claire too, for
oiling the bureaucratic cogs, and making everything run smoothly.
Without a doubt, I've spent some of my happiest and most enriching times here. Apart
from work and classes, I have always to thank, the people at Ashdown House for making my
stay that much more meaningful. Especially to all my desi friends in the clan, dhanyawaad!And
to my other Singaporean friends, particularly HP, who saw me through thick and thin, from
Illinois to MIT, xie xie nil!
Last, but certainly not least, my deepest gratitude to the Lord Buddha, the Goddess of
Mercy and to Kong Chu Kong, for plentiful blessings, of which prayers will eternally be offered.
Saddhu, saddhu, saddhu.
Thank you, Terima Kasih, Merci beaucoup, Xie xie, Tegekkur Ederim, Danke, Dhanyawaad,Gracias,Grazie...
3
Table of Contents
Title Page ........................................................................................................................................
1
A bstract ..........................................................................................................................................
2
A cknow ledgem ents ........................................................................................................................
3
Table of C ontents ...........................................................................................................................
4
1.
2.
3.
Introduction
6
1.1
M otivation ......................................................................................................................
1.2
B ackground....................................................................................................................7
1.3
N on-invasive M easurem ent Techniques................................................................
11
1.4
V alidation .....................................................................................................................
12
Methods
2.1
Patient Screening.....................................................................................................
14
2.2
D ata A cquisition .....................................................................................................
16
2.3
Patient D ata Processing .........................................................................................
25
2.3.1
General Outline ...........................................................................................
25
2.3.2
Characteristic Length ....................................................................................
29
2.3.3
W avespeed D eterm ination ...........................................................................
31
2.3.4
SV R Calculation............................................................................................
39
Results and Analysis
3.1
Q uantitative Analysis..............................................................................................
41
Statistical Analysis .......................................................................................
41
3.1.1
3.2
A nalysis of Potential Sources of Error ..................................................................
49
General Profile Com parison.........................................................................
49
3.2.1
3.2.1.1
Mode of PEP determination: ePEP versus fPEP...........................
3.2.1.2
Objective Function as an accurate predictor of SVR and
3.2.1.3
50
CO % error ....................................................................................
53
Inter-patient variability..................................................................
54
4
3.2.1.4
3.3
4.
Inter-procedural variability............................................................
57
Sum m ary & Conclusion..............................................................................................60
Future Research ...................................................................................................................
61
Bibliography.................................................................................................................................65
Appendix 1: PatientConsent Form............................................................................................
68
Appendix 2: ProtocolSummary ................................................................................................
69
Appendix 3: Organizationof Detailed Protocol.......................................................................
71
Appendix 4: Application: Notification ofIRB Approval/Activation .........................................
74
Appendix 5: Qualitative Comparisonsof Input and Reconstructed RadialPressure
Profilesfor Five Analyzed Subjects .......................................................................
Appendix 6: Running the Code ...................................................................................................
5
83
88
1
INTRODUCTION
1.1
Motivation
Since 1900, cardiovascular disease (CVD) has been the leading cause of death in the United
States every year but 19181. In fact, CVD claims almost as many lives each year as the next 7
leading causes of death combined, including cancer and accidents. On an international level,
WHO estimates that 17 million people around the globe die of CVD each year36 , and in 1999, it
contributed to one-third of all global deaths.
It is no wonder then, that many parties are
involved in many diverse aspects of this field, be it from a fundamental understanding of the
pathology to preventative measures and treatment. Such wide expertise is needed since CVD
encompasses a broad spectrum of conditions that are immensely complex and inter-related,
preventing easy prophylaxis and prognosis, let alone a cure. The enormity and gravity of the
situation though, necessitates basic procedures such as adequate monitoring to warn of imminent
dangers. Parameters such as Cardiac Output (CO) and Systemic Vascular Resistance (SVR)
provide key information regarding the state of cardiovascular (CV) health; hence they are critical
for the management of patients with CV dysfunction. As current measurement methods are
typically invasive they are not routinely made. If these parameters could be determined noninvasively, it could prove invaluable for patient monitoring in a wide variety of settings such as
in the operating room, cardiac wards or even at home.
This motivation led to the development of a computational model that could noninvasively predict critical haemodynamic parameters, and hence the state of one's cardiovascular
health. Ozawa et al. 25 created a computational model of the CV system based on onedimensional equations of motion in a geometrically accurate distributed arterial system to
describe blood flow in human arterial networks. The model allows for study of the relationship
between haemodynamic variables usually obtained invasively, such as left ventricular
elastance (ELV), end diastolic volume (EDV), SVR and CO, and the morphology of arterial
pressure and flow waveforms at various arterial locations. Coupled with a system identification
technique, the model allows estimation of these parameters from the shape of measurable Radial
Arterial (RA) pressure tracings. The objective of this work then was to build upon past efforts by
validating the results of this model. Preliminary clinical trial results are reported and analyzed to
determine the accuracy of this model and provide a platform upon which to base future research.
6
1.2
Background
Before proceeding to actual clinical experiments and analysis, a brief survey of relevant
literature is undertaken in order to place this work in proper perspective. There are a few major
areas of research covered here, namely a model of the cardiovascular system, parameter
estimation/optimization techniques and non-invasive measurement techniques. In developing the
computational model, the specifics and technicalities of the first two areas have already been
documented in the theses of Ozawa 25 and Xiao 39. As such, they will not be covered here, but
instead, validation of complete non-invasive systems with the aim towards clinical or home
monitoring will be explored.
Various groups around the world have worked on computational models of the
cardiovascular system. Tadjfar et al. 34 at the Advanced Computing Center in Japan, Zacek and
Krause40 , collaborators from the Institute of Hydrodynamics at Prague and the Aerodynamics
Institute in Aachen, Germany and Sheng et al. 2 9 at the Technical University of Nova Scotia have
each used different algorithms to simulate blood flow in humans. Tadjfar used a parallel, timeaccurate flow solver, capable of dealing with moving boundaries and grids to handle complex
three dimensional vascular systems, whilst Zacek and Krause used the Runge Kutta method to
solve 32 non-linear ordinary differential equations resulting from a model composed of 15
elements connected in series. Each element consisted of a rigid connecting tube with an elastic
reservoir, representing a main part of the human cardiovascular system. Sheng's paper highlights
a model similar to the one used here by solving for blood flow, transmural pressure and blood
velocity at all vessel sites of a multi branch model for each time step. They also used the LaxWendroff difference method, which is similar to the MacCormack two-step predictor corrector
method used by Ozawa et al. They, however, use a hybrid method (characteristic method and
finite difference method) to solve for non-linear terms instead ofjust the finite difference method
as in Ozawa et al.'s model. These three groups have reported reasonable results, but thus far, all
validations have only been compared to numerical simulations or selected physiological data
from the literature.
Space research has also motivated work on cardiovascular models. The works of Heldt et
al.
and Mukkamala and Cohen21 are both based at MIT. Heldt developed a cardiovascular
model capable of simulating transient and steady state haemodynamic responses to head-up tilt
and lower body negative pressure, particularly upon astronauts' return to Earth. Though his
7
model is suitable for a global systemic response, which serves his objectives, the Heldt model is
based on a lumped parameter representation of the entire circulation. Furthermore, model
verification, though good, was performed in comparison with sets of population-averaged
haemodynamic data reported in the literature. Mukkamala and Cohen's main objective in
developing a computational model of the cardiovascular system was primarily to generate
realistic beat-to-beat variability (forward modeling) for analysis of beat-to-beat fluctuations in
non-invasive measured heart rate, arterial blood pressure and instantaneous lung volume. Their
model, which consists of three major components: a pulsatile heart and circulation, a short term
regulatory system (including an arterial and cardiopulmonary baroreflex)
and resting
physiological perturbations (such as respiratory activity and autoregulation of local vascular
beds) is again not suitable for studying subtle changes in the arterial pressure pulse due to
propagation and reflection within the distributed arterial network.
Olufsen et al.2 4 developed a numerical simulation of blood flow in arteries with
structured-tree outflow conditions that have shown excellent agreement with measured flows,
albeit only on one patient. One-dimensional Navier-Stokes equations for flow in compliant and
tapering vessels are solved with large arteries being modeled as a binary tree and small arteries
and arterioles as structured trees (binary asymmetric trees in which the radii of the daughter
vessels are scaled linearly with the radius of the parent vessel). The geometry of the large vessels
are determined from magnetic resonance measurements, while those of the structured tree are
based on general statistical relationships estimated from literature data. Though it has a limited
computational domain and is much more complicated than the windkessel model used in
Ozawa's model, the resulting pressure and flow profiles have shown correct characteristics and
are able to capture observed oscillations of the impedance due to wave propagation effects.
Of direct relevance to Ozawa's model is the work of Stettler and Niederer
32
and
Stergiopulos and Westerhof 31. Many of the equations used in the prediction of normal pulse
patterns were influenced by Stettler et al., who developed a distributed model of the arterial
system. Ozawa, however, solved the equations using finite difference, as opposed to using the
method of characteristics, and also included losses at bifurcations and a sophisticated ventricular
model. Stergiopulos et al.'s work aided in the derivation of the central aortic pressure (only
available invasively) from non-invasively determined peripheral pressure and flow velocity.
Their time domain method was based on the separation of carotid and brachial waves into their
8
forward and backward components, which could then be added again to reconstruct aortic
pressure accurately. In addition, this method could be applied to each patient individually.
The relative strength of the model used here (Ozawa et. al.) lies in its distributed nature,
based on a geometrically accurate 30-element arterial model. One-dimensional equations of
motion are solved for flow in this branching network, including energy losses at bifurcations, a
ventricular model incorporating specified time-dependent wall circulatory systems, damping
mechanisms and viscoelastic behavior of arterial walls. Lumped parameter venous and
pulmonary circulatory systems complete the cardiovascular model. As each pressure and velocity
profile is a global (CV) systemic outcome, given specific haemodynamic parameter values, the
numerical solutions of the distributed arterial model allow us to obtain estimates of blood
pressure, flow velocity and cross sectional area at each location in the arterial tree as a function
of time. The model is then used to generate a solution library of 2351 data points containing
physiologically feasible pressure and velocity profiles.
To validate the model, the inverse problem has to be solved. When a patient's pressure
and/or velocity profile is entered into the code, the parameter estimation scheme characterizes
each profile through a set of distinctive features, and matches these features to the profiles stored
in the library through a surrogate function interpolating between points in parameter space using
a local n-dimensional surface representation. A best fit is achieved when the differences between
the input and library profiles are minimized. Since we know the parameters that are used to
generate each library profile, the parameters corresponding to the best-fit (interpolated) library
profile are output as the estimated parameters. We then repeat the forward process, and run these
estimated parameters through the arterial model to reconstruct the patient's input profiles to
check the accuracy of the inverse procedure. Thus, in summary, when a patient's data (pressure
and/or velocity profile(s) and other corollary measurements) are input into the computational
model, we can estimate key haemodynamic parameters and reconstruct pressure and velocity
profiles at various locations throughout the body. This is the objective of a monitoring set-up, but
from a research point of view, success or validation of the model occurs when the reconstructed
profiles and estimated parameters match well with the corresponding (clinically) measured
quantities. A flowchart of the overall algorithm of the computational model is shown on the next
page, which highlights the different components of the entire system.
9
OVERALL ALGORITHM
..........................I....
.
. . . .
. .
..
. .
. . . .
. . . .
. . . .
. .
.
I
- - - -
- -
--
- - - -
- -
--
- -
--
- -
- - - -
--
I
- -
- - - -
- - - -
- - - -
- -
--
- -
-----------AA iLI
----------------------------------------------------------------------------------------------------------------
IJ
ELv = Left Ventricular Contractility, EDV = End Diastolic Volume, SVR = Systemic Vascular Resistance, CO = Cardiac Output
Figure 1: Overall algorithm of Ozawa et al.'s computational CV model
10
-
1.3
Non-invasive Measurement Techniques
Estimation of cardiovascular or haemodynamic parameters requires some form of input
from the patient. This is usually in the form of a knowledge of parameters such as the heart rate
(HR), pressure (pressure profile itself or systolic/diastolic values from various arterial sites;
Central Venous Pressure (CVP) as an indication of the preload), flow (wavespeeds of pulse or
blood flow, velocity profiles at various vascular sites, cardiac output (CO)) or volume (end
diastolic volume (EDV)). A combination of inputs is often required to extract different
parameters of interest.
Numerous non-invasive methods exist from which to gather these data, ranging from the
simplest, requiring no instrumentation whatsoever (the palpatory method for measuring HR) to
complex. Other simple methods include the electrocardiograph (EKG) for measuring HR, and
the
auscultatory
method
and
sphygmomanometer
for
measuring
blood
pressure.
Bioinstrumentation has undergone significant improvements, an example of which is the
Portapres, an advanced ambulatory noninvasive blood pressure monitor. A successor of
Finapres* (an acronym for FINger Arterial PRESsure), the Portapres measures arterial blood
pressure waveform continuously in the finger via an infrared photoplethysmograph. As arterial
pulsations fill the capillary bed of the fingertip, the changes in volume of the blood vessels
modify the IR absorption of an incident infrared light, enabling HR and pressure waveforms to
be measured. Another non-invasive method for recording pulse pressure wave contours is by
way of a pulse tonometer, a hand-held probe equipped with pressure sensors at the tip, described
by Xiao39.
Most of these methods involve measurements made at the radial or brachial arteries, since
external measurements can easily be made at the arm. For measurements closer to the heart,
Doppler ultrasound is the technique of choice. With this method, ultrasound is directed at the
moving blood and the change in frequency of the signal reflected off the red blood cells provides
a measure of blood velocity. The total flow can be obtained by integrating the signal over the
cross sectional area of the vessel. Doppler techniques are very convenient since they are noninvasive and the transducers may also be used in echocardiography to evaluate cardiac chamber
size, wall thickness, wall motion, valve configuration and motion. Also known as cardiac
ultrasonography, the term echocardiography arises from the reflected sound waves used, or,
'echoes'.
Finapreswas commercially available through the US company Ohmeda but is now no longer in production
11
Transthoracic impedance is another non-invasive way of measuring CO, and can be
measured across externally applied electrodes. Since impedance changes with the cardiac cycle
(change in blood volume), the rate of change of impedance is a reflection of CO.
Though non-invasive, most of these tools are still primarily used in a clinical setting. For
a home application of this cardiovascular model, forseeably, a patient could measure his or her
own HR and radial pressure profile by tonometry. Electrical probes would also provide a pseudo
EKG reading, from which wavespeed calculations could be made. Together with the patient's
height, these could then be input into a small processing unit equipped with software containing
this code, and have results displayed in approximately 10-15 minutes.
1.4
Validation
Despite the abundance and convenience of non-invasive measurement techniques,
invasive methods continue to be practiced as they provide greater accuracy. As such, though noninvasive measurements may suffice as input data in a monitoring system, for validation purposes,
invasive data must be used. Haemodynamic monitoring has traditionally relied on the
measurement of arterial or central venous pressures, and consequently fostered a pressure
oriented monitoring environment. Thus, the radial arterial pressure profile was selected as the
standard marker for comparison of actual and reconstructed waveforms. The radial artery was
chosen as measurements at this location can easily be obtained both invasively and noninvasively, thus validation results can easily be applied to future monitoring outcomes.
The next chapter on experimental methods highlights the various measurements made to
validate the radial arterial pressure profile as well as to calculate the necessary haemodynamic
parameters being estimated and other ancillary inputs. This builds upon previous clinical studies
conducted by Ozawa
and Xiao39 . Ozawa studied 6 patients at the Brigham & Women's
Hospital, comparing their estimated SVR values with actual non-invasive measurements
obtained before and after a vasodilator intervention. Relatively large errors ranging from 6% 162% were obtained, with a mean error of 77.22%. Though his study served mainly to provide a
framework with which to design the estimation scheme, he highlighted the need for wavespeed
determination as well as overall accurate clinical measurements.
12
Xiao 39 followed up on this suggestion and initiated work on wavespeed calculations.
After additional work on the model; she then ran simulations using computer generated brachial
pressure and velocity data, and obtained errors of < 10% for estimates of SVR, ELv and EDV.
Encouraged by these promising results, she also conducted clinical studies on 12 adult subjects
(9 healthy volunteers and 3 cardiac patients) at the Brigham & Women's Hospital. Carotid,
brachial and radial pressures were measured by tonometry and velocities at corresponding
locations were measured by ultrasound. Reasonable agreement was found between the measured
and reconstructed pressure and velocity curves. Multiple SVR and CO invasive measurements
were also obtained in 2 patients, giving rise to errors ranging from 8.1% - 28.4% for SVR and
0.71% - 5.8% for CO. Different accuracies arose, depending on when the measurements were
actually taken, though none of these measurements coincided with the pressure and velocity
measurements.
As such, it was imperative to obtain simultaneous measurements in ensuing
clinical studies. Xiao deemed her clinical results favourable, and used them to confirm the choice
of the feature set used in the parameter estimation scheme as well as the improvement introduced
by the new left-ventricle elasticity model by Senzaki et al.28
The lessons learnt from past clinical studies were taken into account and incorporated
into the current methodology, serving as guidelines and reminders for effective and efficient
experimental procedure.
13
2
METHODS
2.1
Patient Screening
To validate the computational models, estimated parameter values had to be compared to actual
patient measurements. Since measurements of the parameters of interest are routinely carried out
during heart surgery, studies were carried out on patients undergoing coronary artery bypass
grafting (CABG) or valve repair at the cardiac surgery unit at Massachussetts General Hospital
(MGH). Inclusion criteria included:
1. Male & female subjects between the ages of 18-90 years
2. Patients undergoing either first time or repeat coronary artery bypass surgery
3. Patients whose valvular dysfunction was being corrected surgically, to include valve
replacement or repair
4. Scheduled Transesophageal Echocardiography (TEE) deemed necessary for the clinical
management of this specific subject and for the calculation of Pre-Injection Period (PEP)
and End Diastolic Volume (EDV).
Conversely, patients with the following conditions were excluded from the study:
1. Aortic aneurysms
2. Prior history of peripheral bypass grafting
3. History of amputation of the lower and/or upper extremities
4. Hemodialysis arterial-venous fistulas
5. Valvular dysfunction, specifically aortic or mitral insufficiency which are classified as
greater than trace on pre-operative workup, or any degree of aortic or mitral stenosis in
patients not having these valvular problems corrected
6. Any degree of interventricular conduction delay or bundle branch block as seen on the
pre-operative electrocardiogram (EKG), unless the patient is having simultaneous
transduction of the aortic root pressure and the radial artery pressure intra-operatively
7. Any condition for which the intra-operative use of transesophageal echocardiography is
not indicated or is contraindicated
8. Participation in other research studies within the last thirty days
14
Upon confirmation of eligibility, patient consent (Appendix 1) was then obtained prior to surgery
and documented in the subject's medical record. A total of 16 patients were tested, with 5
patients admitted for CABG procedures, 9 for Aortic Valve Replacement (AVR), and 2 for
Aortic and Mitral Valve Replacement (AVR & MVR). A summary of patient demographics,
characteristics and haemodynamic variables is shown in Table 1. All studies were performed in
accordance with a protocol (Appendix 2,3,4) approved by the Human Research Committee
(Institutional Review Board) of MGH.
Table 1: PATIENT DEMOGRAPHICS AND HEMODYNAMIC DATA
Value
Parameter
No. of Patients
16
Age, yrs
42
-
88
Male/Female
4, 12
Procedure undergone (CABG/AVR/ AVR & MVR)
5,9,2
Haemodynamic Variables
RA, mmHg
37.2 - 188
CVP, mmHg
2.2
CO, 1/min
2.3
SVR, dyn-s/cm 5
17.5
-
7.0
735 - 2393
Definition of abbreviations:CABG = Coronary Artery Bypass Graft; AVR = Aortic Valve Replacement;
MVR = Mitral Valve Replacement; RA = Radial Arterial Pressure; CVP = Central Venous Pressure;
CO = Cardiac Output; SVR = Systemic Vascular Resistance.
15
2.2
Data Acquisition
Apart from standard demographic data (e.g. gender, age, height and weight) and a brief
patient history, three major forms of data were recorded, namely; pressure waveforms and
electrocardiogram (EKG) readings, cardiac output (CO) measurements and echo images.
The standard haemodynamic monitoring set-up of interest to this project begins at the
invasive lines, which, for cardiac surgery, typically consist of indwelling catheters placed in the
radial and pulmonary arteries and in the jugular vein. Analog signals from pressure transducers
within these catheters are then amplified and transferred to a data acquisition module (TRAM
450SL) before being filtered, and digitized by a GEMS-IT Solar 8000M processing unit. This
central brain further processes the data and performs the necessary analytical calculations before
being sent to a distribution box in analog format. This distribution box disseminates the
haemodynamic data to various equipment throughout the room, including to the TEE machine,
the balloon pumps, the heart and lung machine, as well as a video driver that subsequently
displays the information on two large ceiling monitors. These monitors, suspended from the
ceiling at the head of the patient, provide direct access and easy viewing of all the key data to the
entire cardiac team.
In a similar manner, EKG tracings are conveyed by leads placed at specific points on the
patients' bodies and broadcast on both ceiling monitors. The distribution tower connected to the
monitors in the Cardiac Operating Rooms (Gray 45-48, MGH) is further equipped with data
outlet BNC ports which provide ready access to the monitor data without interfering with the
routine monitoring set-up.
Four cables were connected between the distribution center and a National Instruments'
CA-1000 data acquisition black box to relay the haemodynamic data to our recording system.
The accompanying software (LabView 5.0) was installed onto an Apple Macintosh G3 laptop
and together, enabled analog to digital data conversion and real time recordings of the patient's
EKG and pressure waveforms from the Radial Artery, Pulmonary Artery and jugular vein
(Central Venous Pressure). These waveforms were sampled at 100 Hz, and collected four times
over the course of each surgery, i.e.:
1.
Before Induction of anesthesia (Pre-Induction)
2. Post-Induction
3. Post Bypass
4. Chest closure
16
To give a time perspective of the study on each patient, a single recording lasted on the
order of about one minute whilst each surgery lasted between 5 - 10 hours.
In addition, Cardiac Output measurements were obtained using the PA catheter by the
thermodilution technique. Whenever possible, an average of 2 to 3 readings was taken and at
least one of these C.O. measurements was taken simultaneously with the pressure waveform
recording to ensure temporal relevance.
It is important to note that the computer connections posed no additional risks to the
patient, and all the electronic equipment were inspected and certified by the Biomedical
Engineering Department at MGH. These safety precautions arise from the fact that background
or leaked 60Hz cycle electrical currents can easily disrupt the electrical signals of the heart that
form the basis of excitation contraction coupling (the pumping mechanism of the heart). The
open chest cavity of patients undergoing open heart surgery leave them particularly defenseless
against microshocks, and when added to their already precarious cardiac rhythm, can pose
serious risks.
Echo images were obtained via an HP Sonos 5500 transesophageal echocardiography
(TEE) machine utilizing pulsed/continuous ultrasound
@ 4-6
MHz. For better image quality,
digital images were saved on an optical disk and subsequently transferred onto CD-ROMs for
further processing (as opposed to taping sequences on an analog VHS cassette).
Since echo
images are routinely collected after induction and after bypass (to check the cardiac anatomy
before and after surgery), to avoid any additional procedures that might cause unnecessary
interference, TEE images were only collected twice for each patient. All post-induction and post
BP waveforms were recorded simultaneously with the Echo images, and immediately after the
computer recording of the waveforms began, the EKG plug was quickly disconnected and
reconnected to produce an instantaneous spike in the EKG tracing that would show up on both
the laptop and the optical disk. This then served as a time marker for that particular sequence of
echo images. Each echo taping was timed to include approximately eight cardiac cycles. After
the conclusion of the echo sequence, the laptop recording was continued until after the CO
reading was obtained and the CVP waveform had stabilized.
Many slices
through the heart may be
obtained using the two-dimensional
echocardiographic technique ". For best views, two approaches were selected from the
armormentarium of 2-D Echo examination techniques
17
20, 30, 36:
(i) the short axis (SAX) plane for
a view of the aortic valve, and (ii) the apical long axis (LAX) approach for a view of the left
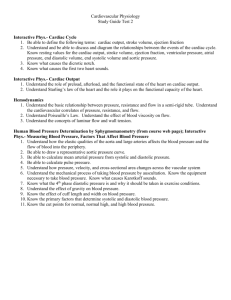
ventricle. A summary of some of the planes of interest is shown in Figures 2, 3 and 4 below.
http://www.echoincontext.com/begin/skillB_07.asp
Figure 2: Basic two-dimensional Echocardiographic Imaging Planes
18
http://info.mecLyale.edu/intmed/cardio/echoatlas/views/
Figure 3: View of the aortic valve through the SAX plane
http:/info.med.yale.edu/intmed/cardio/echoatlas/views/
Figure 4: View of the Left Heart through the apical LAX plane.
19
In all aspects of data recording, patient confidentiality was maintained and study codes
used to protect their individual identities. An outline of the entire setup is provided in Figures 5-8
overleaf, which provide a clearer picture of the operational surroundings and the complexity of
the equipment and teamwork that go into ensuring the ultimate safety and success of the patient.
An estimated timeline of the experimental procedure during a standard CABG operation is
presented in Table 2.
20
Ceilingmonitor,
TEE machine
Ceiling
Monitor
Distribution tower with the TRAM450SL Data Acquisition Module &
Patient'sBed
GEMS IT Solar 8000M Processing Unit embedded within (can't be seen here).
The yellow panel containsBCN portsfor additionalconnections, in this case to our DAQ system & laptop.
Figure 5: Photograph of an empty OR with the complete monitoring set up
21
Figure 6: One of the ceiling monitors with the haemodynamic parameters displayed. Two EKG
tracings (in green) are shown, but since they are primarily used as time markers, only one lead/tracing
was recorded for our purpose. Red = RA; Yellow = PA and Blue = CVP.
In consecutive order, the values at the bottom of the screen are displayed as Pmax , Pmin , and Pmean -
Figure 7: Real time recording of the
haemodynamic data displayed on the ceiling
monitors to the laptop via an NI CA-1000
Data Acquisition (DAQ) system and
LabView software.
22
Figure 8: The SONOS 5500 Transesophageal Echocardiography (TEE) Machine.
Echocardiography applies the principle of reflected ultrasound waves to discern the cardiac
topography. Unlike normal (transthoracic) echo machines, the probe is inserted into the patient's
esophagus, thus giving a clearer image of the cardiac anatomy (without obstruction by the sternum,
skin & chest muscles). Notice the image of the Left Ventricle on the screen. The green line at the
bottom of the screen shows the EKG tracing. Although TEE produces better images, the invasive
manner of this method is not without risk, and may be contra-indicated for critical patients. It is usually
used when greater visualization/assessment of cardiac function is called for, e.g. after a valve
replacement.
23
TABLE 2: Estimated Timeline of events for CABG with heart-lung bypass.
Note: Verbal consent must be obtainedfrom the patientprior to administrationof sedation/pre-medication.
TIMELINE
0:00 - 1:00
SURGERY
Patient arrives & prep.
begins (sedation &
placement of lines)
1:00
PRE - INDUCTION
v EKG, RA, PA, CVP
(- 1 min,)
Pressurewaveforms will
ANESTHESIA
Prepares equipment, places lines (IV,
arterial line, PA catheter). Pressure
monitors zeroed & connected to patient.
CO MEASUREMENT
(Thermodiluffon via PA catheter)
MD or anesthesia nurse takes several CO
measurements & an avg. is recorded. This
be recorded on a laptop
CO measurement MUST be done
connected to the display
v CO
simultaneously with the recordings, so
please give notice prior to measurement.
Induction dose of narcotics & paralytics.
STUDY
1:10
1:15
Endotracheal tube & TEE probe placed.
Surgery continues to
prep. & drape field.
POST - INDUCTION
v EKG, RA, PA, CVP
" CO
" TEE (Optical Disk)
CO MEASUREMENT (as above)
Sequence: (- 1- 4 mins)
For coordination of timing, the EKG (lead
"Laptop started
(haemodynamics
recordingstarted)
" CO + Echo
(as many cycles as
necessary to catch LV
features & PEP)
"EKG spike during Echo
"Laptop stopped
1:30 - 4:30
4:30
4:45
5:00
Incision & sternotomy
Surgery & Bypass.
Heart-lung bypass
terminated & heart
restarted. Patient
rewarmed.
POST - BYPASS
Surgeons remove
v EKG, RA, PA, CVP
cannulas, cauterize
bleeding & place chest , CO
tubes.
v TEE (Optical Disk)
CHEST CLOSED
Chest & Skin are
closed.
v EKG, RA, PA, CVP
vCO
24
All 3 measurements (haemodynamic, CO
& Echo) MUST be SIMULTANEOUS, so
again, please give prior notice.
1) will be detached/unplugged briefly @
the start of recording to produce an artifact,
which will be recorded by both the laptop
& on the Echo.
Things to note on Echo:
i) (Maximal) LONG AXIS VIEW,
LV End Systolic & End Diastolic Diam.
over a few cycles (to determine ESV,
EDV, EF). A 4-Ch view would be helpful
for recognition purposes.
ii) Colour Doppler/ clear shot of Ao valve
(to determine exact Ao valve opening
for calc. of Pre-Ejection Period - delay
btw Q wave on EKG & actual ejection)
(for calc. of wavespeed)
TEE continues.
Pacing & ventilation initiated. Anesthesia
renewed & coagulation reversed.
CO MEASUREMENT
CO MEASUREMENT
2.3
Patient Data Processing
2.3.1
General Outline
From each of the four recorded data sets from each patient, one characteristic cycle from
the RA channel was selected and entered as input to the parameter estimation scheme. The
values for Heart Rate (HR), standard length (L), and the arterial wall stiffness (E) were
additional inputs to the parameter identification algorithm. The estimated parameters were, in
turn, used as inputs to the reconstruction program to form the radial arterial pressure waveform,
which was subsequently compared to the corresponding waveform originally obtained during
surgery. An overview of the parameter estimation and reconstruction schemes, complete with the
actual parameter inputs and outputs, is presented in Figure 9.
INITIAL INPUT
PARAMETER
ESTIMATION
RECONSTRUCTION
.HR
* Pressure Waveform
eHR
9 Length
E e
*ELV
* ELV
*EDV
*SVR
*EDV
*SVR
* Obj. Fn.
* CO
Input & Output
Feature Values
e Pressure Waveform
ACTUAL & RECONSTRUCTED
WAVEFORM COMPARISON
FIGURE 9: Summary of all the input & output variables for each of the parameter
estimation and reconstruction schemes. See text for definition of the abbreviations and the
real (R) and standardized (S) data.
25
Through careful analysis of the closeness of fits between both curves and other statistical
methods, the accuracy and effectiveness of both models could then be ascertained and/or
validated. The validation algorithm is shown in the flow chart in Figure 10 on the following
page. Following that are sections describing in detail, the specific calculations (in chronological
order) conducted to determine each variable.
A seemingly trivial, but nonetheless important point to note is the issue of
standardization. Data was processed in two forms, termed either "real" or "standardized". "Real"
refers to the actual dimensional values for the particular subject, unprocessed. "Standardized"
refers to scaled values of pressure, velocity, etc., adjusted so that they relate to the calculations
used to create the solution library. As a consequence of the use of dimensionless variables in the
parameter reduction process, all calculations could be obtained for a single value of characteristic
length (Lo) and wavespeed (Co). That is, all dimensional variables were made dimensionless by
combination with LO, CO, and fluid density, p. In order to compare measurements made on
subjects with arbitrary LO and CO, therefore, it is necessary to rescale these measurements so that
they correspond to the dimensionless results. For convenience, the conventions used by Xiao
were maintained. That is, 'real values' are input into the parameter estimation scheme, which
outputs 'standard values'. The reconstruction program however, both receives and produces
'standard values'
(as denoted by R and S in the schematic overleaf). Therefore, the
reconstructed waveforms were 'realized' for consistent comparison with the original (actual)
waveform. (see Table 3 overleaf for the conversion factors that link real and standardized
values).
26
VALIDATION ALGORITHM
YES
Figure 10: Validation Algorithm Flow Chart
27
Parameter
Conversion/Multiplication Factor
Heart Rate (1/s)
HRR
=
HRs
C
HRR =LL
Hs)
Left Ventricular Elastance (dyn/cm 5 )
T)
EL
ELVR
End Diastolic Volume (ml)
3(C2
=
EDVR
Systemic Vascular Resistance (dyn-s/cm)
ELLVs
c)L
ED4
3
(LR2SC
5
SVRR = SVRSsG
Central Venous Pressure (mmHg)
C-
(C2
CVPR = CVPs
)
* R = Real; S = Standard;
* Block letters refer to library reference values.L =averageforearm length =22.9cm; C= reference
wavespeed at aortic root at 1 00mmHg = 462 cm/s
Table 3: Conversion factors for converting parameter values from 'standard' to 'real'
values ('realizing').
28
2.3.2
Characteristic Length
To reduce the number of variables, it was assumed that all vascular networks are
geometrically similar; that is, that each is defined by a single length scale, and that all linear
dimensions of the arterial networks scale in direct proportion to this length
25.
Namely, we
defined the length between distal points of the brachial and radial arteries as a characteristic
length marker and assumed that the rest of the arterial tree geometry corresponded linearly with
this length scale. According to Gray's Anatomy
12
the brachial artery ends about 1cm below the
bend of the elbow while the radial artery commences at the bifurcation of the brachial, just below
the end of the elbow, and passes along the radial side of the forearm to the wrist. Although the
radial artery also passes through various bones at the wrist into the hand, for practical purposes,
the characteristic length was assumed to run from 1cm below the (inner) crease of the elbow to
the crease at the base of the hand
23.
This notation made use of clear anatomical markers and
made clinical sense as quick pulse checks are usually made by sensing the pulse at the wrist.
A
side
trial
was
conducted
to
determine
an
average
ratio
between
the
characteristic/forearm length versus a person's height. Measurements were made on 25 female
and 25 male volunteers of a wide range of heights, ages and ethnicities and recorded as shown in
Table 4 overleaf. Since little (fourth decimal place) differences were found between the average
male and female ratios, as well as among other classifications, the entire population average was
taken and the ratio of a person's forearm length to their height was determined to be 0.13 ±
0.0074. This was done to avoid the additional hassle of measuring a patient's forearm length
during the study. Instead, each patient's characteristic length could be easily obtained by
knowing the patient's height, readily available on his/her medical chart.
29
No
Name
Height (cm)
1
JT
150.5
2
SP
162.5
3
4
5
6
7
8
9
10
11
HK
GK
YZ
FQ
KH
AP
CL
GK
SC
12
13
14
15
16
17
18
19
20
21
(cm)
Forearm/Height
Radial-Heart (cm)
Radial/Height
0.119601
0.128134
0.120482
0.124224
0.123457
0.122951
0.132258
0.130435
0.122699
0.128440
57
67
73
62
64
62
73
63
64
65
64
0.378738
179.5
166
161
162
183
155
161
163
163.5
18
21
23
20
20
20
22.5
20.5
21
20
21
0.406685
0.373494
0.397516
0.382716
0.398907
0.406452
0.397516
0.398773
0.391437
AG
175
25
0.142857
70
0.400000
ST
KD
KV
Al
CS
FK
A
GK
LC
161.5
147
161.5
163
160.5
165
151
162
164.5
20
19
21
22
21.5
21
20
24
21
0.123839
0.390093
0.130031
0.134969
0.133956
0.127273
0.132450
0.148148
0.127660
63
63
66
68
64
63
63
64
66
0.408669
0.417178
0.398754
0.381818
0.417219
0.395062
0.401216
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
TYC
JN
IM
AE
WMH
GD
MK
JHZ
SK
EO
HV
ZJ
AS
GH
PJ
AS
CF
SS
SK
TK
HD
EC
JH
JW
AC
VA
SZ
DM
163
178.5
157
168
168
167
173.5
179
169
172.5
173
178.5
179.5
182.5
167
170
178
165
177
168
168.5
180.5
189
194.5
200
166
160
185.5
22
25
22
22.5
22
19.5
22.5
22.5
24
20
25
22
23
22.5
21.5
22.5
22
23.5
25
23.5
22.5
24
23
26
26
22
21
24
0.134969
0.140056
0.140127
0.133929
0.130952
0.116766
0.129683
0.125698
0.142012
0.115942
0.144509
0.123249
0.128134
0.123288
0.128743
0.132353
0.123596
0.142424
0.141243
0.139881
0.133531
0.132964
0.121693
0.133676
0.130000
0.132530
0.131250
0.129380
65
73
64
70
67
66.5
70
68
69
71
70
70
69
70
66
71
70
68
70
65
68.5
74
76
79.5
84
68
65
74
0.398773
0.408964
0.407643
0.416667
0.398810
0.398204
0.403458
0.379888
0.408284
0.411594
0.404624
0.392157
0.384401
0.383562
0.395210
0.417647
0.393258
0.412121
0.395480
0.386905
0.406528
0.409972
0.402116
0.408740
0.420000
0.409639
0.406250
0.398922
50
PK
177
21.5
0.121469
68
IForearm
0.129231
0.129252
FEMALE AVG:
Std. Dev.
MALE AVG:
___
___
_____Std.
__
Dev.
-__TOTAL
AVERAGE:
0.412308
0.428571
0.384181
0.130457
0.400607
0.007132
0.013114
0.130199
0.400478
j
0.007777
________
0.011068
]
0.130328
________[
0.400542
0.007386
Std. Dev.
0.012010
Table 4: Forearm/Height and Radial/Height Ratio Determination
Sample Population: The first 25 measurements arefrom females and the last 25 arefrom males.
30
2.3.3
Wavespeed Determination
Definition
For a typical RA pressure waveform that shows dispersion due to the frequencydependent velocity of its components, the term group velocity might better describe this set of
waves. However, the conventional method of analysis has been to measure the time of travel of
the 'foot' of the wave (at the end of diastole, when the steep rise of the wavefront begins) over a
known distance 19. This is principally to determine a point of identity in the traveling wave and to
use its velocity as characteristic of the whole wave. Apart from being more easily recognizable,
this early part of the wave will also be less affected by reflections and can be considered to be
the most unadulterated portion of the propagated wave. The wavespeed used here has been
defined as how fast the wave propagates from the aortic valve at the start of systole to the distal
end of the radial artery. Later, it is shown how this relates to the reference wavespeed, Co. The
simplicity of the definition though, belies the complexity of the calculation. Much effort has
gone into the calculation of wavespeed and this exemplifies the difficulty in modeling a nonlinear biological system and the multitude of considerations that have to be undertaken.
Wave propagation distance
It is difficult to ascertain the exact position of the aortic valve at a cursory glance as there
are no clear external anatomical indicators. The aortic orifice is situated a little below the upper
angle of the third left stemocostal articulation; close to the articulation.
Figure 11: Front of thorax, showing surface relations of bones, lungs (purple), pleura (blue), and
heart (red outline). P. Pulmonary valve. A. Aortic valve. B. Bicuspid valve. T. Tricuspid valve
31
A simple way of determining the (aortic - radial) distance would be to use the distance between
the sternum and the wrist instead. This lack of precision is not detrimental as long as it is
consistent among all the patients. In a survey similar to that described in the previous section,
volunteers were asked to stand with their arms outstretched (human T), and the straight distance
between their sternums and wrists were measured. From Figure 11 above, it can be seen that this
straight distance closely approximates our intended measurement. The average ratio (over a
population of 50) of the aortic-radial length to a person's height was found to be 0.40 ± 0.0120.
This distance was then divided by the corresponding time interval (see below) to obtain the
patient wavespeed.
Time
The electrocardiograph (EKG) is a valuable instrument in monitoring the electrical
depolarization and repolarization of the heart as a function of time. An extensive literature
suggesting the use of Systolic Time Intervals (STI) as a measure of left ventricular performance
has been established 35. Here, use of these specific time intervals will be made to obtain the most
accurate wavespeeds possible.
The time interval of interest here, At, is the wave propagation time from the root of the
aorta (the aortic valve) to the distal radial artery at the wrist (signified by the beginning of the
upstroke on the Radial Arterial Pressure Waveform, as highlighted in the definition section
above). The EKG is the de facto clinical time marker. However, because the onset of the time
interval of interest is marked by the opening of the aortic valve (an occurrence dependent on the
achievement of necessary pressure gradients across the valve); the EKG, (dependent upon
electrical potentials) fails to distinctly present an accurate marker. The Wigger's Cycle (see
Figure 12) clearly demonstrates the difference between the onset of systole (Q wave on the
EKG) and the actual opening of the aortic valve.
32
1U
i
x
U
S
ca
'I15=
C
-~
1.
I.)
L.0
111"M
120100Pressure 80(mm Hg) 604020-
I
4 -
-----
4
- -i
I
Aortk
pressu re
aorfic vall
closes
aorti!
valve
opens
(.1...
(0l
b-
le yen kular
pressure
itral
ive
coses
mitral
valves
opens
%too
Heart
sounds
ow
1
4
e~IpI~I
1P
0
I
p!
2
L
r'at
esur
I
I
3
-
V
Venous
pulse
R
T
Electrocardiogram
lar.
0
I
aI
I.
0.1
I
3
I II
I
.
0.2 0.3 0.4 0.5 0.6 0.7 0.8
ime(s)
Source: http://www.mmi.mcgill.ca/Unit2/Shrier/lect3basiccardiacelectroPartl.htm
Figure 12: The Cardiac Cycle (Wiggers Diagram).
33
I
To overcome this, the Pre-Ejection Period (PEP) had to be determined. The PEP 3 is the interval
from the beginning of ventricular depolarization (Q wave) to the beginning of left ventricular
ejection (aortic valve opening), and signifies the delay in transmission of the pulse to actual
ejection of blood from the heart. The final determination of At then becomes the PEP subtracted
from the time interval between the
Q wave
on the EKG and the beginning of the upstroke on the
Radial Arterial Pressure Waveform.
I
Radial Arterial Pressure
V
R
Beginning of upstroke
T,
Time Interval, At =T - PEP
Figure 13: Determination of Time Interval, At
The time interval demarcated by T, is relatively easily obtained from the EKG and Radial
Arterial Pressure Waveform recordings. For best definition, the main characteristics of these
recordings should be clearly delineated, as follows: (1)
a clear initial depolarization force
departing acutely from a flat baseline on the EKG and (2) a clearly discernible rapid upstroke on
the radial arterial pulse tracing. These factors add to the selection criteria for an appropriate cycle
for data processing. PEP determination, however is less trivial and may be obtained by two
methods: (i) from Echo images, (11) by formula, as described below.
34
Echo PEP
This method involves scanning through the trans-esophageal echocardiography (TEE) sequences
to pinpoint the exact moment of the aortic valve opening, relative to the EKG
Q
wave. A
commercially available software, Fast Movie Processor v.1.41, was employed to view the
sequences frame by frame. Once the two frames containing the pulse at the
Q wave
and the
aortic valve opening had been ascertained, the time lapse was calculated as the number of frames
divided by the Frame Per Second (FPS) rate. Below is a sample calculation obtained by this
method:
Frame # 118: Q wave of EKG
Frame # 123: Opening of Aortic Valve
The coaptation of the three leaflets (full closure)
The leaflets part to allow blood flow into the
of the aortic valve is clearly seen as the left
aorta. Notice that the white cursor on the
ventricle undergoes diastolic filling
green EKG tracing below has moved
beyond the QRS complex.
File Info: FPS: 71.0
PEP Calculation:
PEP = # of frames / FPS
= (123 - 118) /71.0
= 0.0704 s = 70.4 ms.
Figure 14: Short Axis View of an Aortic Valve (JPEG Images)
35
By taking an average of a few cycles from each individual patient, the PEP for that patient can be
determined. Needless to say, the accuracy of this method is, to a large extent, limited by the
image quality as well as the fortuitous viewing of the opening of the aortic valve. It is not
uncommon for the initial opening view to be obscured due to the out of plane twisting of the
pumping heart.
FormulaPEP
In applying STI measurements, it is of utmost importance to define a normal range of variation
relative to heart rate. It has been found that in the range of heart rate from 40-110 bpm, the
durations of total electromechanical systole, Left Ventricular Ejection Time (LVET) and PEP are
related linearly to heart rate (HR). Linear regression analysis data from normal individuals yield
equations relating STI and heart rate as follows 35
Gender
Regression Equation (ms)
Standard Deviation (ms)
Male
PEP = -0.4 HR + 131
10
Female
PEP = -0.4 HR + 133
11
Abbreviations: HR = Heart Rate
These equations offer a convenient formula for studying intra- and inter-patient changes. It must
be noted though, that these indices are influenced by changes in posture, diurnal cycles, age etc.
Nonetheless, to a first order approximation, the general form of these regression equations is
sufficient.
36
Cm,,n versus Co
With the knowledge of both the aortic-distal radial length and time interval, the mean
wavespeed, Cme can easily be calculated as:
Cmean = Laortic - distal radial/
At
(2)
where At = T, - PEP. After obtaining Cmea, a relationship between Co (the reference wavespeed
at aortic root at 100 mmHg) and Cmean must be used to calculate Co. Following Xiao
39,
a
polynomial fit was generated for Co as a function of Cman and the radial diastolic pressure,
Pdias,rad.
(Xiao used
Pdias,bra
instead, which was not available in the present study). A
computational code in C was written to generate this relationship from the library points (where
Co = constant = 462 cm/s), and the following relationship was obtained:
Cmean
Co =
disrd2
-0.55
- 10'')
M100o)
+1.
"
44 5
(3)
'
(_'';t _
d
L(100 )
+0.8113
Cmean/462 vs P raddias/l 00
2
1 .8
1 .6
y = -0.559X2 +
1.4
1.4457 x + 0.8113
1 .2
C
E
0 0.8
0.6
0.4
0.2
0
0
0.2
0.4
0.6
0.8
1
1.2
1.4
1.6
Prad dics /100
Figure 15: Relationship between (Cme./ 462) and (Pdis,rd /100)
The banding seen in the plot above is due to finite time steps in the libraryprofiles carriedover by the
calculationsin the C code.
37
To test this formula, it was used to back-calculate the Co of all the library points. The mean
value of 462.19 cm/s ± 50.00 corresponded well with the known value of 462 cm/s, and the
standard deviation was comparable to Xiao's results (463.64 cm/s ± 33.73 cm/s).
Co for positive & limited normal range (cm/s)
700
Std Dev.: 5O.OO121867 crns
200
00
0
0
500
)00
1500
2000
2500
Number of pts
Figure 16: Calculated Co for library points.
Since there are two methods of calculating PEP, the corresponding values of both Cos were used
and the subsequent results compared.
A final point to note is the input of E, Young's modulus of elasticity of the artery walls,
instead of Co in the parameter estimation scheme. The two variables are linked by the previously
mentioned Moens-Korteweg equation, which has the form:
I E-h
where the reference wavespeed CO is a function of Young's modulus of elasticity, E, arterial
inner radius, R, fluid density, p, and wall thickness, h, at the aortic root. With a normalized E
curve and known values of R, p, and h accounted for in the computer models, the above relation
simplifies to:
Co =4E
or
38
E =C
2.3.4
SVR Calculation
Finally, the systemic vascular resistance, SVR, is calculated:
SVR
where
Pmean
=
P
ean
- CVP
CO
(4)
is the mean Radial Arterial Pressure, CVP is the Central Venous Pressure, and CO is
the Cardiac Output.
39
3
RESULTS & ANALYSIS
From the total number of patients studied, 5 cases were selected for full analysis. These
corresponded to patients undergoing only CABG procedures. Patients with AVR/MVR
procedures were excluded as some of their data (collected prior to the bypass procedure) showed
compromised haemodynamic behaviour due to valvular dysfunction; hence, were incompatible
with the model's assumptions of a normal valve function. Though 2 additional data points (at
Post BP & Chest Closure) could be obtained from each of the excluded patients, the focus was
aimed at these 5 'complete' patients (with acceptable data from all 4 time-points of data
measurement) to enable complete inter-patient and inter-procedural analysis, i.e. to assess the
effects of individual variability and surgical interventions on the model's results. From these 5
patients, 16 data points were obtained. Four runs did not converge, mainly because the
(standardized) heart rate was below the minimum parameter set point of 40bpm. It is important
to note that runs usually will not converge if any of the calculated input parameters fall outside
of the specified range used to construct the solution library, as highlighted in the table below.
Parameters
HR (bpm)
ELV (dynlcm 5 )
EDV (ml)
SVR (dyn-s/cm 5)
Range
40-160
300-15000
30-400
300-3500
Table 5: Ranges of four parameters (standardized values)
Two other parametersare kept constant: D = 0.57 and CVP =5.0 mmHg
Since two parameters were kept constant, and HR was input directly from the patient's
data, only 3 parameters were left to be estimated, i.e. ELV, EDV and SVR. Another output
variable that was not a parameter, but was also estimated was Cardiac Output, CO. Though Echo
images were captured to calculate EDV, certain issues arose due to the difficulty in ensuring
homogeneity amongst all the patients. This would require obtaining images from a fixed
anatomical reference point, which was extremely difficult due to surgical time constraints.
Furthermore, this would not necessarily guarantee a maximal long axis measurement, which is
crucial for accurate EDV calculations; not to mention the vicissitudes of image quality. ELv was
also impossible to quantify with the current set up in the OR, as it would require continuous
intraventricular pressure-volume measurements and a significant change in surgical equipment as
well as procedure. Given these constraints at hand, the current data were only verified for SVR
and CO, and measures for full verification are described in further detail in the section on future
research.
40
3.1
QUANTITATIVE ANALYSIS
3.1.1
Statistical Analysis
Two main statistical methods were utilized to determine the precision and accuracy of the
computational model within the sample population. Termed bias and precision statistics, they
have several advantages over conventional regression analysis. They are described below in the
following sections.
1) Bland Altman Analysis
The Bland Altman Analysis method is a common tool used to assess agreement between
two methods of clinical measurement 3. In this context, this analysis is used to determine
agreement between the estimated parameters and the measured values, and to conclude if the
computational results are sufficiently accurate so as to be interchangeable with or replace the
(invasive) measured values. Most other statistical methods, by testing for regression coefficients,
test for correlation between two sets of data. In their paper published in The Lancet in 1986, the
authors made a key distinction between agreement and correlation - that agreement implies a
high correlation, but the reverse is not necessarily true. This is easily understood when viewed
from a graphical perspective. When data points fall along any straight line, they exhibit
correlation, but only data points that fall along the line of equality, i.e. y = x show perfect
agreement. It is important to note that data which seem to be in poor agreement may actually
produce rather high correlations. They also point out that significance tests may show that two
methods are related, but the test of significance is irrelevant to the question of agreement since it
would be amazing if two methods designed to measure the same quantity were not related.
They proposed instead, to plot the difference between the methods against their mean for
a more informative display. The mean is used on the x-axis because assuming that the true value
of a measurement is unknown, the best estimate of it would be the average of the two methods
used. Assuming also, that the differences are normally distributed, 95% of these differences will
lie between the so-called limits of agreement [d 1 1.96s], where d is the bias or mean difference,
and s is the standard deviation. The key point is that provided differences within these limits are
not clinically important/significant,
then these 2 methods of measurement may be used
41
interchangeably. Figures 14-15 overleaf show plots of agreement and Bland Altman analysis for
SVR and CO data respectively.
Bland Altman analyses of CO data revealed a mean difference of -0.3 L/min and a
standard deviation of 1.14 L/min, with corresponding limits of agreement at (1.935, -2.54) L/min
respectively. These values were superior to those obtained by Espersen et al. in Denmark 10.
They conducted a study to compare various cardiac output measurement techniques
(Thermodilution, Doppler and CO 2 rebreathing) versus the direct Fick method, (the gold
standard), of healthy volunteers at various positions. For the comparison between thermodilution
and the direct Fick method in the supine position, they obtained a bias of 2.3 L/min and a
standard deviation of 2.1 L/min from 10 patients. If both the mean difference and standard
deviations of the thermodilution method are larger than those of the computational method, then
any inaccuracies that arise may be largely due to the measurement technique itself. Furthermore,
the thermodilution technique is not without fault. A significant overestimation, independent of
the absolute values has been shown before, compared to the direct Fick method 5,17,
27.
This
systematic error may be introduced by the co-existence of many factors such as lack of
temperature equilibration between the ice bath and the syringes, incorrect volume of the
syringes, loss of indicator (temperature) when handling the syringes and in the catheter,
differences in the rate of injection, errors in the computer performance especially when
calculating the downslope of the curves or the cyclic temperature changes in the pulmonary
artery during respiration
16,26
With that said, it is also important to note that the direct Fick method itself is prone to
error. Changes in gas tensions in the arterial blood during sampling as well as inaccuracies of
blood gas measurements contribute towards deviations. In short, our knowledge of CO through
measurements, are, at best, estimates as well. These are important factors to keep in mind when
comparing agreement (or differences) between estimated and measured values. With the data
presented here, it is clear that the estimates of CO have deviations less than those of the
thermodilution method itself. Thus if thermodilution is a widely used and accepted method, then
CO estimates obtained from this computational method should serve as well.
42
2500
2000
+
> 1500
-1000
500
-
0 4!<I-1500
1000
500
0
2500
2000
Actual SVR
65
0
04
2-
1
0
1
2
3
45
67
Actual CO
Figure 14: Plots of agreement between estimated and measured values of SVR and CO.
43
Bland Altman Analysis of SVR
1200
1018
1000
- - -
-
- -
_ - - - - -
- - - - - - - -
- -
Ma+.6
Mean+1.96s
- - - -
- - - - - - - -
800
600
Cu
400
3
cd)
200
16
cu
156.43
0
- - - - - - - - - - - - - - - - - - - - - - - - - - - - Mean
- - - - - - - -
1800
1600
1400
1200
1000
-200 -
2000
2200
- - - - -
Mean-1.96s
-400 -
-600
-705
- - - -
- - - - - - - - - - - - - -
- - - -
- - - - - - - -
-800
Average of SVR estimated and measured values (dyne-s/cmA5)
Bland Altman Analysis of CO
21.94 1.5
- - -
- -
-
- -
Mean + 1.96s
-- - - -
- - - - - - -
1
Ii
0.5
Se
00
0n
U)
C
-0.3 - - - - 2.5_
0.5
_
_
_
_
- - 3_5_
_
4
_
_ _
01
4
_ 0_ _
_
_
_
_
_
_
_ _
Mean
00
-1.5 -2
-2.5
-2.54
-3
-
- - - -
- - -
- - - - - - - - - -
- - - - - - - - - - -
- - - - - - -
Average of CO estimated and measured values (L/min)
Figure 15: Bland Altman Analysis of SVR and CO data.
44
Mean - 1.96s
As previously mentioned, SVR and CO are related by the same formula. Thus if all other
variables were kept constant, it was assumed that in the absence of data for comparison, CO
results could be extended to SVR as well. However, looking at the Bland Altman analysis for
SVR data, (bias: 156.43 dyne-s/cm 5 and std. dev.: 439.33 dyne-s/cm 5 ) and comparing it with the
normal range in which SVR falls in (800-1200 dyne-s/cm 5 ), it would seem that more work needs
to be done to improve these estimates since the standard deviation of the differences are larger
than the entire range in which normal values fall in.
2) Error-gram Method
The Bland-Altman method, though a significant improvement upon regression analysis,
is based on a linear relationship between errors and measurements. Unfortunately, CO
measurements, especially when collected over a large physiological range, have been shown to
have errors that show proportionality to the magnitude of the cardiac output
6. Thus,
Bland and
Altman's method does not compensate for relationships between the magnitude of CO
measurements and the size of the error.
To overcome this 'proportionality effect', Critchley and Critchley 9 proposed calculating
the percentage error for each set of data instead of the absolute error used by Bland and Altman.
The absolute percentage error for SVR and CO was calculated as such:
Absolute%error =
A Estimated - Actual
Actual
Ixl100
(5 )
Absolute values were also used to prevent the canceling out of positive and negative errors. For
16 data points, the average percentage error for SVR and CO was 30.7 and 19.9% respectively.
Table 5 overleaf shows all the calculated values for all data points.
45
ACTUAL
PARAMETERS
ESTIMATED PARAMETERS
(real values)
ABSOLUTE
% ERRORS:
INPUTS & FEATURES:
E
Obj.
No. File
SVR
CO
ELv
EDV
SVR
CO
Fn.
SVR
CO
HR
Std. HR Len
Co
(I0e6) Pdias
Psys
Pmean CVP
1
9.1
1074.175
5.4
732.7
275
1608.617
3.71
0.10
49.754
31.30
62.50
49.52
22.16
564.2
5.965
54.7
116.8
76.75
4.2
2
11.1
1130.949
4.7
2221
136
1731.544
3.66
0.01
53.105
21.32
58.25
51.61
23.85
543.1
5.528
57.8
107.1
83.21
17.5
3
20.1
1975.058
3.1
13948
112
1764.560
4.04
0.09
10.658
30.25
53.097
51.91
22.18
457.7
3.925
60.9
119.8
83.54
7.0
4
3.2
1438.775
4.5
531.6
281
1404.234
3.73
0.11
2.401
17.18
57.143
41.53
21.85
606.6
6.895
48.6
117.3
83.43
2.5
5
9.2
1692.345
3.6
1801
355
1497.093
4.22
0.02
11.537
17.31
61.22
61.33
22.16
446.2
3.730
59.5
112
78.02
1.9
6
11.2
1331.620
4.8
2230
116
2262.249
3.14
0.01
69.887
34.58
54.05
44.98
23.85
578.2
6.266
73.3
124.3
95.25
15.3
7
20.2
1001.377
4.7
14561
133
1158.614
4.84
0.05
15.702
4.17
55.55
57.82
22.18
429.9
3.464
53.4
101.9
68.21
10.0
8
3.4
1819.279
4.1
609.1
320
1231.727
4.32
0.18
32.296
5.32
80
58.06
21.85
607.4
6.913
48.4
116.3
96.11
2.9
9
9.3
735.497
6.0
1248
296
1490.735
3.62
0.17
102.684
39.67
85.71
82.02
22.16
467.1
4.088
51.5
98.2
64.46
9.3
10 13.3
1623.913
3.2
1204
235
1655.271
3.40
0
1.931
7.85
86.96
80.31
22.84 498.9
4.665
59.4
98.7
71.85
7.9
11 20.3
1184.324
5.7
16390
157
1414.880
5.74
0.24
19.467
1.63
81.081
88.69
22.18
409.1
3.136
62.5
127.3
87.65
4.0
12
3.5
1226.181
4.9
958.2
314
1290.730
5.37
0.26
5.264
9.49
80
60.26
21.85
585.2
6.418
54.4
133.5
78.11
3.0
13
9.4
782.513
5.8
1446
296
1481.287
3.70
0.14
89.299
36.28
86.96
83.78
22.16
463.9
4.034
52.6
98.4
65.17
8.4
14 11.5
1230.365
4.6
368.3
421
1274.042
4.60
0.03
3.550
0.05
85.71
68.53
23.85
601.8
6.788
64.2
120.1
81.62
10.9
13.4
2293.472
2.4
1927
180
1850.288
3.31
0.01
19.324
38.02
86.96
82.68
22.84 484.6
4.402
65.2
105.7
78.07
9.3
16 20.4
1740.958
4.7
23873
168
1667.766
5.80
0.31
4.204
23.37
78.947
92.00
22.18
384.0
2.763
77.2
150
105.29
3.0
15
J
30.691 19.86 72.133 65.940 122.51 1507.991 4.936 58.98 115.5 81.046 17.314
0.11
4.20
1548.977
5253 1 237
1392.5501 4.5
Notation:
5
SVR = Systemic Vascular Resistance (dyne-s/cm5); CO = Cardiac Output (L/min); ELy =Left Ventricular Elastance (dyn/cm ); EDV = End
2
Diastolic Volume (ml); Obj. Fn. = Objective Function; HR = Heart Rate (bpm); Co = wavespeed (cm/s); E = Young's Modulus (dyn/cm );
Pdias,Psys, Pmean = diastolic/systolic/meanRadial ArterialPressure (mmHg); CVP = Central Venous Pressure (mmHg)
]Avg:
Table 5: Measured, Calculated and Estimated Data for all patients
46
To account for the inherent error within the thermodilution measurement method
(estimated at 10-20% by Stetz et al. 33 ), Critchley proposed an error-gram method, constructed
from the percentage errors in the estimated and measured values to enable a graphic
determination of the limits of agreement between the two methods. The error-gram below
obtained from Critchley's paper matches the CO data here very well since our CO percentage
error is almost exactly equal to the sample value shown in this example.
Figure 16: Error gram enabling one to graphically determine the limits of agreement
between two techniques that measure cardiac output.
The x-axis refers to the limits of precision (±2 s.d.), or percentageerror, of the method being tested. The
isolines refer to the limits of precision, or percentage error, of the reference method, such as
thermodilution cardiac output. The left-hand axis shows the resultant absolute limits of agreement
between methods for a typical study with an overall mean CO of 5 L/min. The right-handaxis shows the
correspondingpercentage limits of agreement.An example is shown where the limits ofprecisionfor both
the test and reference methods are ±20% and predictedlimits of agreement are shown to be ±1.42L/min
or ±28.3%.
47
Assuming a thermodilution error of 20% and comparing it with our estimated CO
absolute percentage error of 19.86 ~ 20%, the combined limits of agreement from the error-gram
above are ±28.3% (from the right-hand axis) or ±1.42 L/min (from the left-hand axis). From the
meta-analysis of various CO measurement techniques that Critchley & Critchley conducted, they
recommend that limits of agreement between the new and reference technique of up to ±30% be
accepted. Consequently, the error-gram method echoes the Bland-Altman conclusion that the CO
estimates obtained from this computational model are acceptable.
As an afternote, the template error-gram above assumes a mean CO of 5 L/min, and
Critchley warns that allowances need to be made for variations from this mean value,
particularly if data from children are included. From Table 5, it can be seen that the mean
measured CO value is 4.5 L/min, which is approximately 5.0 L/min, thus no adjustments need be
made. One could even posit that the final value of the combined limits of agreement of ±28.3%
is an overestimate due to the actual lower value of the estimated CO absolute percentage error of
19.86% and the assumption that the CO measurement error is at its maximum value of 20%
33.
Both these factors tend to minimize the final result by shifting the lines toward the left and
downward. By virtue of proportionality, the lower mean CO measurement of 4.5 L/min could
also have led to lower absolute percentage error values.
If this method is extended to the analysis of estimated SVR data, for an absolute
percentage error of 30.7%, the combined limits of agreement would be approximately 37%,
which would be deemed unacceptable.
In summary, both the Bland Altman and error-gram methods give rise to the same
conclusion, i.e. that the CO estimates from the computational model are acceptable, but the SVR
values are not; CO error proportionality effect notwithstanding.
Note too, that the estimates of ELv and EDV have been included in Table 5. They span a
wide range (368-23,873 dyne-s/cm5 for ELv and 112-421ml for EDV) but are generally
consistent in magnitude from patient to patient. Patient 20 has comparatively much larger values
of ELV, but this might largely be due to the fact that this patient's data were collected by another
researcher. All also seem to show an increasing trend as the procedures proceed from start to
finish, which, reasonably, reflects an increase in cardiac capacity They do not however, seem to
relate to the SVR and/or CO percentage errors and objective functions. Some values fall outside
of the healthy/normal range reported by Xiao 39, but since these values have not been validated,
trends remain speculations.
48
3.2
ANALYSIS OF POTENTIAL SOURCES OF ERROR
3.2.1
General Profile Comparison
Apart from the quantitative analysis, comparisons were also made between the measured
and reconstructed profiles to gauge the visual goodness of fit. A representative comparison is
shown below in Fig. 17. In general, the results were promising, with measured curves well
approximated by the reconstructions. The general morphology of the curves was well preserved
with good correlations in terms of amplitude and temporal pattern. Most deviations, if any,
occurred either at the slope of the
2 d
half of the initial upstroke or at the diastolic portion. These
were manifested as slight shifts to the right (decreased dP/dt), or overestimations (similar shape,
but transposed higher). In a few cases, a small initial systolic hump was also observed before the
main upstroke of the pressure profile.
Figure 17: Representative plot of comparison between measured and reconstructed
profiles.
49
Given the good match between the reconstructed and measured profiles, it is actually
rather surprising that better quantitative results were not obtained. To further explore this, more
qualitative comparisons were made to better characterize and explain the results. The following
categories were defined for further study:
1.
Mode of PEP determination: ePEP versus fPEP
2. Objective Function as an accurate predictor of SVR and CO% error
3. Inter-patient variability
4. Inter-procedural variability
They are elaborated upon in the next section, and followed by possible reasons and redemptive
suggestions.
1.
Mode of PEP determination: ePEP versus fPEP
As mentioned previously in the Methods section, there are 2 ways of determining the Pre-
Ejection Period (PEP), namely from the echocardiographic images (ePEP) or by formulaic
calculations (fPEP). PEP determination is an intermediate step leading towards the calculation of
a key input parameter, i.e. the wavespeed, hence its accuracy is crucial, and the pros and cons of
each method have to be carefully weighed.
The first method is much more tedious since additional recording and processing of the
echo images have to be conducted, but it allows patient specificity since the patient's own echo
images are used. However, the accuracy is also dependent upon image quality and the ability of
the echoes to capture the valve opening. Frame rates differ depending on the particular sequence
taped, but the images processed here varied from 14-20 ms/frame. The second method provides
ease of use, though at the expense of specificity since it is based on population averages.
The PEP itself is on the order of about lOOms (range: 60-11 Oms) and can account for up
to 55% of the time window between the QRS complex on the EKG and the initial upstroke of the
RA Pressure waveform. As such, it cannot be neglected. Because of the time and length scales
involved here as well, a small difference in PEP can lead to large differences in the final
calculated wavespeed. For example, a 36ms PEP difference in one patient led to wavespeed
differences of more than 150cm/s.
Initially, the ePEP method was expected to give rise to better reconstructions, but a
comparison of both ePEP and fPEP plots in the first 4 patients universally revealed better fits for
50
the fPEP reconstructions! Subsequently, only the fPEP calculations were used for the 5 patient.
These comparisons can be seen in the four representative plots shown in Figure 18,
corresponding to comparisons between ePEP and fPEP reconstructions for 4 different patients at
4 different time intervals. The complete set of plots for each patient can be seen in Appendix 5.
There are a number of possible reasons to explain this occurrence. The formula tends to
give rise to larger PEP estimates, leading to larger wavespeeds, which are closer to physiologic
values. Other possible explanations include inaccurate ePEP estimates due to poor image quality.
Perhaps the formulae (culled from a sample population of 211 normal supine subjects) provide
global averages that better suit the assumptions used in the model, the keyword here being
'normal' or healthy. In any case, in anticipation of the usage of this computational model in a
non-clinical environment, the fPEP method conveniently provides a good solution and obviates
the need for more involved invasive or non-invasive echo measurements.
As an aside, in processing the data, it must be noted that the calculated wavespeeds for
patients after bypass and at chest closure were obtained from Cmean measurements at the postinduction stage. This was necessary due to the large amount of interference in the EKG signals at
post BP and chest closure from the pacemakers as well as from the cauterization procedure,
which made distinguishing key signal features tricky and risky. Results from preliminary runs of
post BP and chest closure data comparing between using their own Cmean and Cmean from the
post-induction stage confirmed that the latter was a better method. The wavespeed is not
expected to change from procedure to procedure, hence the suitability of interchanging the
Cmean from one procedure to another. To cover the possibility of inter-procedural differences,
post-induction Cmean was used over pre-induction Cmean as the patient's condition at post BP
and at chest closure were closer to those at post-induction.
Changing the mode of PEP determination has the effect of changing the input wavespeed,
and hence the arterial stiffness. Often, this results in profiles that are relatively similar, but
transposed further from the actual waveform; particularly in the peak and diastolic region; hence
it is not obviously reflected in the objective function (since no feature in the current feature set
characterizes the diastolic curve). It does however, lead to greater quantitative errors, hence, the
importance of the determination of an accurate wavespeed is emphasized again.
51
Figure 18: Representative plots for comparison between reconstructions using PEP
calculated by echocardiographic methods (ePEP) or by formula (fPEP) for 4 patients at 4
different time points.
52
2.
Objective Function as an accurate predictor of SVR and CO% error
Till now, not much has been mentioned about the objective function, except it being an
output of the parameter estimation scheme, as shown previously in Figure 9. The objective
function is defined as follows:
n
Objective Function =
-
2
(6)
where fe and fn are features of the estimated and measured profiles respectively. Clearly, it is a
least squares calculation; therefore a lower value corresponds to less error and vice versa.
Because it is based upon the relative error of the features that define the profiles, objective
function is a good predictor of the qualitative fits between the input (measured) and output
(reconstructed) pressure versus time curves. However, it may not necessarily be so for the
parameter estimates. It would be useful, though, if the objective function could be used to
identify which predictions might be reliable, particularly in predicting the magnitudes of SVR
and CO % errors.
To test the relationship between objective function and SVR and CO% errors, a plot of
these variables was generated, as shown in Figure 19 below. No clear relationship is evident,
however.
Relationship between Obj Fn and SVR, CO% error
120
100
,0
*
2
(D60
0
80
0
S
-
I
ISVR
- SVR
-.- CO
80
40
20 -.-
0
0.05
0.1
0.2
0.15
0.25
0.3
0.35
Objective Fn
Figure 19: Objective Function as a predictor of SVR and CO % errors
53
3.
Inter-patient variability
To compare the effects of an individual patient's physiological and medical conditions on
the model, a plot was made comparing the average values of objective functions and SVR and
CO % errors for each patient, as shown in Figure 20 overleaf. These averages were obtained
from all the runs of each patient that converged. In addition, the objective functions were
multiplied by 100 to enable them to fit on the same scale.
At first glance, there do not seem to be any singular factors that lead to the obtained
results. Age and gender do not seem to be strong markers as well, other than the fact that all
these individuals are elderly and predominantly male, which reflect the population demographics
of heart patients (our sample group) in general. Upon further scrutiny however, a slight trend
surfaces that may explain some of the observations here. Patients 3, 13 and 20, which seem to
show better overall results are patients with normal to good ejection fraction (EF) readings.
Ejection Fraction is the percentage of the total amount of blood in the left ventricle that is
pumped out for systemic circulation per heart beat. Thus, EF may be seen as an analog of flow the higher the EF, the higher, or more undisturbed the arterial flow due to valvular dysfunctions,
arterial stenosis or infracted areas. Patient 20 may have only a low normal EF reading, but
interestingly enough, has had an angioplastic procedure (a technique used to widen narrowing
arteries, most commonly done by inflating a small balloon positioned at the end of a catheter).
Patient 11 however, also shows a high EF of 64%, yet has a contradictorily high SVR % error.
One possible explanation for this is that this patient showed mitral regurgitation (MR), (a
condition in which disease or injury has caused the heart's mitral valve to become leaky,
allowing blood to flow backwards/regurgitate towards the left atrium, and subsequently into the
lungs), causing systemic blood flow to deviate from the norm. Patient 9, analogous to Patient 20,
has a lower EF value, but no prior angioplasty; hence has the highest SVR & CO % errors. The
vascular system does not act independently of the heart though, therefore a normal EF also
reflects normal left ventricular function, as documented in Patient 3's medical history.
54
Inter-Patient Comparison
80
82F, Angina, HTN,
HLip.; 3 vessel
70 + CAD; Nml LV
(EF: 65%);
73M, EF: 40-50%;
severe infarct areas &
ischemia. Multiple
occlusions in Cor. Art
elevated LVEDP
60
61M, HTN,
HCho;
History of CAD,
EF:64% w.
inferoposterior
dys. Trace MR.
77M, Redo CABG
Long history of
CAD. Severe
disease of native
vessels.
67M, Smoker,
-
High BP, Chol.;
EF: low normal;
3 vessel CAD.
Prior angioplasty
Fn (100x)
0
0
50
.00
,
40
0
.0
30
i
20 '
10
0-
-
3
9
11
13
20
Patient
EF: X% (the amount pumped out) of the total amount of blood in the ventricle per heart beat. (Nml > 55%)
Figure 20: Inter-patient comparison of Objective Functions, SVR & CO % errors and medical histories.
Key: M: male; F: female; HTN: Hypertension; HLip: Hyperlipidemia; CAD: Coronary Artery Disease; Nml LV: normal left ventricularfunction; EF: Ejection
Fraction; LVEDP: left ventricular end diastolic pressure; Cor. Art.: coronary arteries; HCho:Hypercholesterolimia;MR: mitral regurgitation; BP: blood
pressure;Chol.: cholesterol.
55
Looking back at Table 5 though, Patient 9 seems to contribute significantly to the large
overall percentage errors. A closer look at the patient's medical history does not show any
outstanding issues, other than the fact that this patient is the only one with severe infarcted areas
and ischemia. In the particular instance of Patient 9's post BP data, errors of 102.7% and 39.7%
were observed for SVR and CO respectively, the highest among all estimates for both
parameters. Perhaps Patient 9's pathophysiology was compounded by the occurrence of a high
CVP value of 9.3 mmHg, leading to particularly poor estimates.
The normal range of CVP lies between 0-8 mmHg, while a constant value of 5.0 mmHg
was used in the model. Ozawa found by a sensitivity analysis that CVP had a significant effect
on the various output parameters, yet it was held constant in producing the library since it was
assumed that its effects would not be significant in the calculation of SVR as its magnitude is
only on the order of 10% of Mean Arterial Pressure (MAP). A high CVP
2
usually reflects
volume overload on the heart or Congestive Heart Failure (CHF), an almost certain affliction in
our sample population as well as in patients requiring cardiac monitoring in general, therefore,
the use of a low, constant value might not be prudent. Certainly the highest SVR % errors mostly
arose from patients with higher CVP values, with SVR % errors of > 50% arising from cases
with CVP > 8 mmHg. (Range of patients' CVP: 1.9 - 17.5 mmHg). A correspondingly higher
number of higher CO % errors was also obtained with increasing CVP values. This can be seen
in an abbreviated form of Table 6 shown overleaf, where results are arranged in order of
increasing CVP value. From the data below, perhaps it can also be hypothesized that a
combination of high CVP and (standardized) HR lead to particularly poor estimates; the cause of
which, still remains to be seen
In short, it may be surmised that the patients whose measurements provided the best input
for accurate estimates and reconstructions were patients with normal left ventricular function and
undisturbed blood flow (i.e. normal to high EF, previous angioplasty (if applicable) and no
valvular dysfunction). These trends are not surprising considering that these assumptions
correspond best with the assumptions used in the model, and that patients with any mitral
regurgitation or aortic stenosis (AS) were to be excluded from the study. The model also tends to
give rise to poorer estimates for patients with infarcted areas or whom have ischemia and/or high
CVP values.
56
No
File
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
9.2
3.2
3.4
3.5
20.4
20.3
9.1
20.1
13.3
9.4
13.4
9.3
20.2
11.5
11.2
11.1
ABS. % ERRORS:
SVR
CO
11.537
17.31
2.401
17.18
5.32
5.264
9.49
4.204
23.37
19.467
1.63
10.658
1.931
7.85
19.324
15.702
4.17
Std. HR
61.33
41.53
58.06
60.26
92.00
88.69
49.52
51.91
80.31
83.78
82.68
82.02
57.82
68.53
44.98
51.61
Co(cm/s)
446.2
606.6
607.4
585.2
384.0
409.1
564.2
457.7
498.9
463.9
484.6
467.1
429.9
601.8
578.2
543.1
INPUTS:
E (10e6)
MAP(mmHg)
3.730
78.02
6.895
83.43
6.913
96.11
6.418
78.11
2.763
105.29
3.136
87.65
5.965
76.75
3.925
83.54
71.85
4.665
4.034
65.17
4.402
78.07
4.088
64.46
3.464
68.21
6.788
81.62
6.266
95.25
83.21
5.528
CVP(mmHg)
1.9
2.5
2.9
3.0
3.0
4.0
4.2
7.0
7.9
8.4
9.3
9.3
10.0
10.9
15.3
17.5
Table 6: Patient Data, arranged in ascending CVP order, with corresponding
SVR and CO % error
Increased% errors are highlighted: Light greyfor SVR % errors below 50%
Dark grey for SVR % errorsabove 50% and CO % errors above 30%
4.
Inter-procedural variability
To complete the analysis, 2 more plots were generated as shown in Figures 21 and 22
overleaf. They contrast the percentage errors of results from measurements taken at different
procedures. Figure 21 plots comparisons for each individual patient, hence it is patient
dependent, while Figure 22 shows data across patients. All values of Objective Function are also
multiplied by 100 to enable them to be compared on the same scale as the percentage errors. A
thorough study of the plots did not reveal any significant trends or patterns. The values obtained
appeared random, and even contradictory at times. Perhaps this highlights the difficulty in
modeling the human cardiovascular system - a non-linear dynamic system that is not only
complex and epistatic, but also subject to and dependent upon many sources of variability.
57
Patient 9
Patient 3
70
70
60
60
50
50-
40-
40-
30-
30-
20.
20
Post BP
0-
N Chest Closed
Chest Closed
Post BP
Post-Induction
0
Post Induction
SVR % error
U Post BP
10
Chest Closed
10-
O Pre-Induction
O Post-Induction
Obj. Fn.
CO % error
Pre-Induction
SVR %
error
CO %
error
Patient 20
Patient 13
Patient 11
701
701
701
60
601
601
50-
50-
50
40J
40
30-
30-
20-
20-
3020.
Chest Closed
10
Post-induction
0
Chest Closed
Post BP
Chest Closed10
0
Post Induction
Post-induction
Pre-Induction
CO % error
CO %error
Objective
SVR %
Function
error
Note: All values of Objective Function are multiplied by 100
Figure 21: Intra-patient inter-procedural comparison for 5 patients
58
. . ......
..
.....
Pre-Induction
CO % error
POST4NDU~fOTM
PRE-INDUCTION
70
60
50
50-
40
30-
20-
WPatient 20
10
Pant
11
Patient 9
CO %error
00%Uww
CHEST CLOSED
POST BYPASS
90
80
70]
60
50-
40-
30-
20.
13 20
rPotlent
Pdient
10
Pctlent9
Pc*Ient3
CO %
eror
Note: All values of Objective Function are multiplied by 100
Figure 22: Inter-patient inter-procedural sort for 5 patients
59
3.3
SUMMARY
Analysis of the available patient data has provided some preliminary conclusions, and
may provide some insight on the model itself as well as directives for future work. Overall, the
average absolute SVR and CO % errors stand at 30.7 and 19.9% respectively. From the Bland
Altman methods, the limits of agreement for SVR are (1018, -705) dynes-s/cm 5 , whilst for CO,
they are (1.94, -2.54) L/min. The error-gram method instead reveals a combined error of ±37%
and ±28.3% (or 1.42 L/min) respectively. Keeping in mind that the experimental error for the
thermodilution method of measuring Cardiac Output lies between 10-20%, and by comparing
these results with past work, both these precision statistics methods suggest that the CO
estimates are marginally acceptable, but not the SVR estimates. Better quantitative results were
observed from patients with normal left ventricular function (or normal EF) with no valvular
dysfunctions, infarcted areas and ischemia. This is to be expected as the computational model is
based on an assumption of normal valve function and a relatively normal CV system.
In terms of qualitative analysis, on the whole, the reconstructed pressure profiles fit well
with the measured inputs, matching the basic morphology, amplitude, temporal duration and
other characteristic features of the curves. Better curve fits are obtained when PEP is calculated
by formula, though this did not translate into better quantitative results. In addition, the Objective
Function is a good predictor of the accuracy of the qualitative fits, though not necessarily of
quantitative accuracy and a high CVP value tends to give rise to poorer estimates. No clear trend
was observed from inter-procedural comparisons. Finally, it should be noted that due to the small
sample size, it is premature to attempt to draw conclusion, either positive or negative. Clearly,
further testing is needed.
60
4
FUTURE RESEARCH
This thesis first set out to estimate cardiovascular parameters non-invasively by clinical
validation of results from the computational model and parameter estimation scheme developed
previously
4,
39.
In this work, an experimental procedure was developed to test the accuracy of
parameter estimation on patients using a comparison to parameters measured by invasive
methods. Analysis revealed some promising results as well as some unexplained trends. Apart
from inter-patient and inter-procedural variability, the small sample size might certainly have
been a factor. The inherent error in the thermodilution technique has also been discussed, which
includes both equipment as well as operator variability. Of course, one should not discount the
fact that measurements made during cardiac surgery are not representative of normal behaviour.
Apart from the physiological and mental stresses of surgery, patients are also bombarded with a
barrage of drugs that maintain the patient's vital signals at 'optimum' levels, hence do not
necessarily reflect natural responses.
Analysis of the computational model also revealed possible weaknesses. Understandably,
it is a tough task to try to strike a balance between precision and accuracy on one hand and
computational efficiency on the other. Though we understand and pay the price for
generalizations and assumptions, some of these simplifications might need to be revisited and
reassessed. A key example might be in the use of a constant CVP value. Considering its
influence on quantitative accuracy, CVP should probably be included as one of the parameters
varied in the library.
In some of the reconstructed waveforms, an extra systolic hump has been observed, as
shown in a representative library profile in Figure 23 below. This additional hump may result
from discrete reflection sites at aortic branches or from the shape of the ventricular elasticity
curve. In either case, it represents a deviation from what is typically observed and therefore is a
potential source of error.
Last but certainly not least, the errors contributed by the parameter estimation scheme are
considered. These are not expected to be major, otherwise the effects would have been observed
in the tests using computer-generated data. The main foreseeable weakness is the premature halt
at a local minimum of the Objective Function rather than at the global minimum, leading to suboptimal estimates. Apart from that, inadequate characterization of the input profile (in terms of
61
choice of features or feature sets) may also lead to insufficient knowledge or poor matching to
provide better estimates.
Netout1
80
70
Brachial
60
E
E
50
--
~40
Radial
Extra systolic hump
U
30
U-
20
8.6
8.8
9
9.2
9.4
9.6
9.8
10
10.2
10.4
10.6
time (s)
Figure 23: Extra systolic hump
After identifying the weaknesses at hand, the next step remains to suggest new solutions
to overcome these problems. Chronologically, work on the parameter estimation scheme must
proceed before any future clinical validation, though in this case, this might not be necessary
since its effectiveness has already been demonstrated though previous computer simulations.
Nevertheless, modifications to the parameter estimation scheme are already underway, and the
results of this new student's work will hopefully supplement and improve upon this model.
Though prior tests had been done to determine the present feature set used in the model, more
trials might also be conducted to include other features or feature combinations. Of particular
interest might be dP/dtdias, the descending slope of the input profile during diastole, which might
be a better indicator of SVR. A higher slope is expected to reflect a lower SVR, since less
resistance would allow greater deceleration of flow into the arteries.
62
If and when the parameter estimation scheme has been updated, more clinical trials
should be planned to increase the sample size for analysis. Biological systems are often highly
variable, thus the greater the sample size, the more chances are available to identify trends and
glean more meaningful data. Clinical data sampling is currently still in progress, though at a
much delayed pace. Some changes might also be proposed to improve upon the accuracy of the
information that might be extracted from them. These include clinical modifications such as
using Fick's Method of measuring Cardiac Output instead of thermodilution and using pressuretipped catheters (instead of the present fluid filled catheters) to record pressure profiles. Both
these methods aim to improve accuracy either by reducing experimental error or by reducing the
recording time lag (thus, better wavespeed inputs). Some clinicians have also suggested the use
of the femoral arterial (FA) waveform instead of the radial arterial waveform with the belief that
the FA line better approximates the waveforms seen in the aorta. While this may be useful during
surgery, it would be difficult to obtain the FA pressure waveform by non-invasive measurement.
It has also been proposed to pause patients' breathing during CO measurement to avoid
respiratory variations (which also affect HR and BP).
A major aspect of the clinical studies that has not been dealt with so far concerns the
validation of ELv and EDV. Some of the difficulties faced have already been highlighted in the
previous section. ELV could not be previously determined from this data set because it is requires
from a continuous Pressure-Volume
(PV) loop, whilst the data here were collected
instantaneously. Technologies exist though, to measure these quantities with relative ease. The
hurdles to acquisition of simultaneous continuous pressure and volume data have been greatly
overcome with conductance and manometric catheters. The conductance catheter technique is
based on measuring the time-varying electrical conductance of the blood in the ventricle
41.
This
time-varying electrical conductance is, to a first approximation, linearly proportional to the
actual volume of blood in the ventricle (based on Ohm's Law). Combination Pressure-Volume
Catheters combine pressure sensors and electrodes on the same instrument, enabling minimallyinvasive continuous intracardiac pressure-volume analysis. In order to automate and computerize
data acquisition and data analysis as well as to decrease subjectivity of human error in the
analysis of pressure-volume data, Cassidy and Teitel 7 developed LabViewTM applications that
could digitize and display data recorded from such indwelling combination catheters. These
applications could then separate data into cardiac cycles and process the data meaningfully to
63
graphically display PV loops and other important cardiac indices such as stroke work, stroke
volume, EF, HR, maximum and minimum derivatives of ventricular pressure, indices of
relaxation, peak filling rate and ventricular chamber stiffness. Such a tool would be immensely
useful for our experimental studies. While considering such alternatives, it is essential to keep in
mind that the priority of the hospital and/or cardiac team lies in the health and safety of their
patients. Implementation of new or different procedures such as the Fick method for CO
measurement, recording from the FA line or the simultaneous PV catheters must therefore be
considered carefully, taking all factors into consideration.
Another way of improving volume estimates from the echo images is by the use of
myocardial contrast echocardiography 8, 14,
1,
18, 22. This new technique basically enables better
delineation of the endocardium for volume calculations by using ultrasound contrast agents that
opacify the left heart chambers when stimulated by sound waves of particular frequencies
This as well as other changes might be considered in the future. Improvements are
certainly welcome, albeit within prudent and practical confines. Even in the absence of such
enhancements however, it will still be necessary to increase the current sample size and continue
to pursue other approaches to analyzing the data. Whatever the case may be, it is sincerely hoped
that this work will continue to be built upon to develop a system that in the near future, may
become commonplace and more importantly, beneficial for cardiac patients, both in the clinical
and non-clinical setting.
64
Bibliography
Publications:
1.
American Heart Association. 2002 Heart and Stroke Statistical Update. Dallas, Tex.: American Heart
Association; 2001.
2.
Berne RM, Levy MN. Physiology. 4t" ed., 1998. Mosby Inc, St. Louis, MO.
3.
Bland JM, Altman DG. The Lancet 1986; 1:307-3 10.
4.
Bottom KE. A Numerical Model of CardiovascularFluid MechanicsDuring External CardiacAssist.
1999. Master's Thesis, Massachusetts Institute of Technology.
5.
Branthwaite MA, Bradley RD. Measurement of cardiac output by thermal dilution in man. J Appl
Physiol 1968; 24:434-438.
6.
Broomhead CJ, Wright SJ, Kiff KM, Withington PS. Validation of thoracic electrical boimpedance
as a porcine research tool. Br J Anaesth 1997; 78:323-325.
7.
Cassidy SC, Teitel DF. Left Ventricular Pressureand Volume Data Acquisition and Analysis using
Labview m . Comput Biol Med 1997; 27:141-149.
8.
Cohen JL, Segar DS, Gottdiener JS. Improved Left Ventricular EndocardialBorder Delineationand
Opacificationwith OPTISON (FS069), a New EchocardiographicContrastAgent. Results of a Phase
IIIMulticenter Trial. JACC 1998; 32(3):746-752.
9.
Critchley LAH, Critchley JAJH. A meta-analysis of studies using bias and precision statistics to
compare cardiacoutput measurement techniques. J Clin Monit 1999; 15:85-91.
10. Espersen K et.al. Comparison of cardiac output measurement techniques. thermodilution, Doppler,
CO 2 - rebreathingand the direct Fick method. Acta Anesthesiol Scand. 1995; 39:245-251.
11. Feigenbaum H. Echocardiography.4h Ed. 1986. Lea & Febiger PA.
12. Gray H. Gray'sAnatomy of the Human Body.
3 0th
Ed. 1984. Lea & Febiger PA.
13. Heldt T, Shim EB, Kamm RD, Mark RG. Computational modeling of cardiovascularresponse to
orthostaticstress. J Appl Physiol. 2002 Mar; 92(3): 1239-54.
14. Kaul S. Myocardial Contrast Echocardiography: Basic Principles. Progress in Cardiovascular
Diseases 2001; 44(1):1-11.
15. Lafitte S et. al. Improved Reliabilityfor EchocardiographicMeasurement ofLeft Ventricular Volume
using Harmonic Power Imaging Mode Combined with ContrastAgent. Am J Cardiol 2000; 85:12341238.
16. Levett JM, Replogle RL. Thermodilution cardiac output: a critical analysis and review of the
literature.J Surg Res 1979; 27:392-404.
65
17. Mackenzie JD, Haites NE, Rawles JM. Method of assessing the reproducibility of blood flow
measurement. factors influencing the performance of thermodilution cardiac output computers. Br
Heart J 1986; 55:14-24.
18. Mayer S, Grayburn PA. Myocardial Contrast Agents: Recent Advances and Future Directions.
Progress in Cardiovascular Diseases 2001; 44(1):33-44.
19. McDonald DA. Blood Flow in Arteries. 2 "d Ed. 1974. The Williams & Wilkins Co. Baltimore.
20. Mercier JC et. al. Two-dimensional EchocardiographicAssessment of Left Ventricular Volumes and
Ejection Fraction in Children.Circulation 1982; 65(5): 962-969.
21. Mukkamala R, Cohen RJ. A forward model-based validation of cardiovascularsystem identification.
Am J Physiol Circ Physiol. 2001 Dec; 281(6):H2714-30.
22. Nahar T et. al. Comparison of Four EchocardiographicTechniques for MeasuringLeft Ventricular
Ejection Fraction.Am J Cardiol 2000; 86:1358-1362.
23. Netter FH. Atlas ofHuman Anatomy.
2nd
Ed. 1997. Icon Learning Systems.
24. Olufsen MS et al. Numerical simulation and experimental validation of blood flow in arteries with
structured-treeoutflow conditions. Ann Biomed Eng 2000; 28(11): 1281-1299.
25. Ozawa ET. A Numerical Model of the Cardiovascular System for Clinical Assessment of the
Haemodynamic State. 1996. PhD. Thesis, Massachusetts Institute of Technology.
26. Runciman WB, Ilsler AM, Roberts JG. An evaluation of thermodilution cardiac output measurement
using the Swan-Ganz catheter. Anesth Intensive Care 1981; 9:208-220.
27. Russell AE, Smith SA, West MJ. Automated non-invasive measurement of cardiac output by carbon
dioxide rebreathingmethod: comparisonswith dye dilution and thermodilution. Br Heart J. 1990; 55:
195-199.
28. Senzaki H, Chen C, Kass DA. Single-beat estimation of end-systolic pressure volume relation in
humans. Circulation 1996; 94(10): 2497-2506.
29. Sheng C, Sarwal SN, Watts KC, Marble AE. Computational simulation of blood flow in human
systemic circulationincorporatingan externalforce.Med Biol Eng Comput. 1995 Jan; 33(1):8-17.
30. Silverman Nil et. al. Determinationof Left Ventricular Volume in Children. Echocardiographicand
Angiographic Comparisons.Circulation 1980; 62(3):548-557.
31. Stergiopulos N, Westerhof B, Westerhof N. Physical basis of pressure transferfrom periphery to
aorta: a model-based study. Am J Physiol 1998; 274(2):H1386-H1392.
32. Stettler JC, Niederer P, Anliker M. Theoretical analysis of arterialhemodynamics including the
influence of bifurcations. Part I: mathematical models and prediction of normal pulse patterns.
Ann Biomed Eng. 1981; 9(2):145-64.
33. Stetz CW, Miller RG, Kelly GE, Raffin TA. Am Rev Respirat Dis 1982; 126:1001-1004.
66
34. Tadj far M, Himeno R. Time accurate,parallel, multi-zone, multi-block solver to study the human
cardiovascularsystem. Biorheology. 2002; 39(3-4):379-84.
35. Weissler AM. Noninvasive Cardiology. Grune & Stratton NY.
36. Weyman AE. Principlesand Practice ofEchocardiography.2 nd Ed. 1994. Lea & Febiger, PA.
37. World Health Organization. CardiovascularDiseases - Prevention and Control. WHO CVD Strategy.
2001/2002.
38. World Health Organization Web Site, www.who.int/ned/svd
39. Xiao, X. Noninvasive Assessment of CardiovascularHealth. 2000. Master's Thesis, Massachusetts
Institute of Technology.
40. Zacek M, Krause E. Numerical Simulation of the blood flow in the human cardiovascularsystem. J
Biomech. 1996 Jan; 29(1):13-20.
Online References:
41. http://www.cardiodynamics.nl/TheMethod.htm
42. http://www.mc.vanderbilt.edu/surgery/trauma/PDF/HemoParamReference.PDF
67
Appendix ]
CARDIAC ANESTHESIA - HEMODYNAMIC STUDY GROUP CONSENT
I enrolled this patient in our hemodynamic study. As required by the IRB, I informed the patient
that we would be digitally recording the hemodynamic data available through the OR monitoring
system using a laptop computer, and that also we would be obtaining digital copies of the TEE
study. I stated that the study would in no way affect the quality of care given, and that no
identifying information would be used in order to protect the anonymity of the subject. All
questions were answered. The patient gives verbal consent.
Edwin T. Ozawa M.D. Ph.D.
Pager # 36214
Dept. of Anesthesia & Critical Care
68
Appendix 2
PROTOCOL SUMMARY
(limit to 3 pages)
PRINCIPAL/OVERALL INVESTIGATOR
Marcos F. Vidalmelo M.D. Ph.D.
PROTOCOL TITLE
Measurement of Hemodynamics During Cardiac Surgery
FUNDING
Grant funds provided by Prof. Roger Kamm, Massachusetts Institute of Technology
SPECIFIC AIMS
We propose to collect data pertaining to the clinically relevant indices as well as arterial pressure
and flow tracings and transesophageal echocardiography data in order to validate a computer
generated hemodynamic parameter estimation scheme.
BACKGROUND AND SIGNIFICANCE
A numerical model of the cardiovascular system was developed in order to study the relationship
between hemodynamic parameters, such as left ventricular contractility, systemic vascular
resistance, and other indices of value to the practitioner, and the morphology of arterial pressure
and flow waves at various locations throughout the arterial system in large caliber vessels.
Furthermore, a parameter estimation scheme was developed, using the numerical cardiovascular
model as a reference, which has the potential to estimate clinical hemodynamic indices based on
the morphology of measureable arterial pressure and flow tracings. Thus, the parameter
estimation algorithm allows one to solve the "inverse" relationship which the original
cardiovascular model solves for. Parameter estimation schemes have been utilized widely in the
engineering field for the purposes of optimization of manufacturing processes, etc.
RECRUITMENT
We propose to recruit and consent patients immediately prior to surgery in the induction area, or
if premedication is to be given, the night prior to surgery.
RESEARCH DESIGN AND METHODS
The following cardiovascular indices need to be measured prior to and following a
pharmacological intervention which alters hemodynanics to a significant degree. The induction
of anesthesia qualifies as such an intervention. We propose to collect hemodynamic data which
includes the following:
1) Radial artery pressure waveforms
2) Central venous pressure waveforms
3) Right ventricular pressure waveforms, as obtained with an indwelling pulmonary artery (PA)
catheter
4) Electrocardiogram
5) Cardiac output, also obtained using the PA catheter by the hemodilution technique
BWH1 /DFCIMGH Human Subjects Research Application Form
Version 3: March 1998
69
Filename: Protosum.doc
Page 1 of 2
Appendix 2
Indices I though 4 will be obtained using an analog to digital data recording system that has been
installed onto a laptop computer. The monitors in the cardiac operating rooms are equipped with
data outlet BCN ports which provide ready access to the monitor data.
Patients undergoing cardiac surgery routinely are monitored using trans-esophageal
echocardiography, or TEE. From the TEE we hope to obtain an estimate of left ventricular (LV)
volumes from recorded videotape and hardcopy images. In some instances, the aortic root
pressure may be routinely transduced intra-operatively, and in that case we plan to record the
data in the same manner as the other pressure tracings (indices I through 3).
RISKS AND DISCOMFORTS
There are no additional risks or discomfort to the patient other than what is already routinely
experienced by patients undergoing routine cardiac surgery.
POTENTIAL BENEFITS
There are no direct benefits to the patients enrolled in the study. The long term benefits of the
study include validation and improvement of existing technology which may be used to assess
the cardiovascular function of patients.
BWH/DFCI/MGI Human Subjects Research Application Form
Version 3: March 1998
70
Filename: Protosui.doc
Page 2 of 2
Appendix 3
ORGANIZATION OF DETAILED PROTOCOL
I.
BACKGROUND AND SIGNIFICANCE
Computer models have been used for decades to study how the flow of blood may be affected by
drugs or mechanical devices, such as the intra-aortic balloon pump or the ventricular assist
device. Ozawa et al. [1][2] developed a computational model of the cardiovascular system based
on fluid mechanical equations that describe blood flow in arteries. The model allowed for the
study of the relationship between hemodynamic variables usually obtained invasively, such as left
ventricular end diastolic pressure, cardiac output, ejection fraction, and systemic vascular
resistance, and the morphology of arterial pressure and flow waves at various locations
throughout the arterial system in large caliber arteries. With use of a special computer technique
termed system identification, coupled with the numerical cardiovascular model, a method was
developed to estimate those hemodynamic variables from the shape of measurable arterial
pressure and flow tracings such as the radial artery pressure tracing.
So far, the model was evaluated with computer simulation of physiological data. Based on such
simulations, Xiao [3] has already shown that the system identification scheme is able to estimate
useful hemodynamic variables to a high level of precision. For instance, estimates to within 10%
were obtained for left ventricular end-diastolic volume and contractility, and 3% for systemic
vascular resistance. No validation of the method with use of clinical data has been attempted thus
far.
Measurements as cardiac output, ejection fraction, left ventricular contractility and systemic
vascular resistance provide valuable information for the management of patients with
cardiovascular dysfunction. However, due to the invasive nature of their measurement, they are
many times not obtained. The ability to assess such data non-invasively or less invasively could
be valuable in any setting involving the monitoring of patients with cardiovascular disease.
Examples are the operating room, cardiac wards and outpatient settings. Consequently, if the
method to be studied proves to deliver accurate estimates of variables obtained invasively, it
could be very useful as a hemodynamic monitoring system.
II.
SPECIFIC AIMS
We propose to validate a computer based system to estimate hemodynamic variables from radial
artery pressure tracings. The variables to be estimated are: left ventricular end diastolic pressure,
cardiac output, ejection fraction, and systemic vascular resistance.
III.
SUBJECT SELECTION
We propose to enroll up to 35 subjects undergoing coronary artery bypass grafting or valve repair
by the cardiac surgery service. We will assess the data from 23 completed subjects.
Inclusion criteria:
1) Patients undergoing either first time or redo coronary artery bypass surgery.
2) Patients whose valvular dysfunction is being corrected surgically, to include valve replacement
or repair.
3) Scheduled transesophageal echocardiography deemed necessary for the clinical management of
this specific subject.
4) Male and female subjects age 18- 90 will be eligible to participate.
Exclusion criteria:
Patients with the following conditions will be excluded from the study:
1) Aortic aneurysms;
2) Prior history of peripheral bypass grafting;
BWH/DFCI/MGH Human Subjects Research Application Form
Version 3: March 1998
Filename: Protocol.doc
Page 1 of 3
Appendix 3
3) History of amputation of the upper or lower extremities;
4) Hemodialysis arterial-venous fistulas;
5) Valvular dysfunction, specifically aortic or mitral insufficiency which are classified as greater
than trace on pre-operative workup, or any degree of aortic or mitral stenosis in patients not
having these valvular problems corrected;
6) Any degree of interventricular conduction delay or bundle branch block as seen on the preoperative electrocardiogram, unless the patient is having simultaneous transduction of the aortic
root pressure and the radial artery pressure intra-operatively.
7) Any condition for which the intra-operative use of trans-esophageal echocardiography is not
indicated or is contraindicated;
8) Participation in other research studies within the last thirty days.
Subjects will be identified only by their initials and date of birth.
IV.
SUBJECT ENROLMENT
Information about the study will be given to the potential subjects by a member of the study team
12 to 24 hours before the scheduled procedure. Informed consent will be obtained by an
investigator. Since this is a minimal risk study that only involves processing of normally captured
cardiovascular vital signs with a computer based system identification scheme, we will obtain oral
consent. The consent to participate will be documented in the subject's medical record. During
the consent process, the subjects will be told that this is a research study, that it involves only a
computer connection for assessment of vital signs in the operating room. Subjects will be told
that the study is voluntary, with little or no additional risk, and will be of no direct benefit to
them. They will also be told that all information that might describe them will be coded to protect
their privacy. They will understand that choosing not to participate will have no affect on their
care now or in the future. The routine procedures for cardiac surgery and anesthesia will be
unchanged for this study.
V.
STUDY PROCEDURES
Routine invasive lines for cardiac surgery comprise an arterial line, usually in the radial artery and
a pulmonary artery catheter. After placement of these lines, the following data will be collected:
1)Radial artery pressure waveforms via an indwelling radial artery catheter;
2)Pulmonary artery pressure waveforms, as obtained with an indwelling pulmonary artery (PA)
catheter ;
3)Pulmonary capillary wedge pressure, obtained using the PA catheter;
4)When available intra-operatively, aortic root pressure tracing;
5)Continuous 2 lead electrocardiogram (ECG);
6)Cardiac output, also obtained using the PA catheter by the thermodilution technique;
7)After induction and insertion of the TEE probe, images of the left and right ventricles.
In addition, demographic data, i.e., patient's sex, age, height, and weight and patient's armspan
measured with a tape measure will be obtained.
Cardiovascular data will be collected at the following points along the surgical procedure:
1) Induction of anesthesia;
2) Skin incision;
3) Sternotomy;
4) Aortic cannulation;
5) Post-bypass period;
6) Chest closure.
BWH/DFCI/MGH Human Subjects Research Application Form
Version 3: March 1998
Filename: Protocol.doc
Page 2 of 3
Appendix 3
Waveforms will be sampled at 200 Hz using an analog to digital data recording system that has
been installed onto a laptop computer (Apple Macintosh G3). The monitors in the cardiac
operating rooms of Blake 45 through 48 are equipped with data outlet BCN ports which provide
ready access to the monitor data without interfering with the routine monitoring set-up. The
digital TEE images will be saved on computer disk, with a study code to preserve confidentiality.
VI.
BIOSTATISTICAL ANALYSIS
Post processing analysis of the data will be performed by feeding the radial artery pressure wave
data into the system identification scheme installed on a computer at M.I.T. The system
identification scheme will then compute the hemodynamic variables of left ventricular end
diastolic pressure, cardiac output, ejection fraction, and systemic vascular resistance. The
computed hemodynamic variables will be compared with the actual measured hemodynamic
variables that were collected during the surgery at the time corresponding to the collection of the
radial artery pressure wave. Statistical analysis of the difference between measurements obtained
by the routine method involving the PA catheter and TEE, and the new method involving system
identification, will be perfromed. The method of data analysis for comparing two measurement
techniques is decribed by Bland and Altman [4]. This involves plotting the mean value between
the two meaurement techniques for each hemodynamic variable against the actual difference in
measurement. From this, a mean difference and an associated standard deviation of the difference
can be calculated. From the standard t-test distribution, a 95% confidence interval can then be
assigned. Data from 23 completed patients will be collected. This is based on the estimate of the
standard deviation of the studied variables with alpha error of 10% and accuracy of 0.25.
VII.
RISKS AND DISCOMFORTS
There are no additional risks or discomfort to the patient other than what is already routinely
experienced by patients undergoing routine cardiac surgery.
VIII.
POTENTIAL BENEFITS
There are no direct benefits to the patients enrolled in the study. The long term benefits of the
study include validation and improvement of existing technology which may be used to assess the
cardiovascular function of patients.
IX.
MONITORING AND QUALITY ASSURANCE
All data will be collected and assessed by an investigator and members of the Fluid Mechanics
Laboratory at Massachusetts Institue of Technology in Cambridge. Participating members of this
department are Roger Kamm, PhD., Professor of Mechanical Engineering, Mohammad R.
Kaazempur-Mofrad, PhD., Postdoctoral Fellow and Xinshu Xiao, graduate student. All subject
data will have been coded for confidentiality prior to assessment.
X.
REFERENCES
1. Ozawa, E.T. "A Numerical Model of the Cardiovascular System to Assess Strategies for
Clinical Intevention." Ph.D. Thesis, Massachusetts Institute of Technology, August 1996.
2. Ozawa, E.T., Bottom, K.E., and Kamm, R.D. "Numerical Simulation of Enhanced External
Counterpulsation." Annals of Biomedical Engineering, Apr 2001, vol 29, pp 284-297.
3. Xiao, X. "Noninvasive Assessment of Cardiovascular Health." M.S. Thesis, Department of
Mechanical Engineering, Massachusetts Institute of Technology, Cambridge, MA, 2000.
4. Bland, J.M. and Altman, D.G. "Statistical Methods for Assessing Agreement Between Two
Methods of Clinical Measurement." The Lancet, Feb 8 1986, pp 307-3 10.
BWH/DFCI/MGH Human Subjects Research Application Form
Version 3: March 1998
Filename: Protocol.doc
Page 3 of 3
Appendix 4
ummn ItseArch COmOMItt
Massachusetts General Hospital
Lawrence House
l0 Not1hGroveStreet
Boston, MA 02114
(617) 726-3494
Application: Notification of IRB Approval/Activation
Protocol #: 2001-P-001023/1; MGH
To:
Marcus Melo, MD
An sthesia
CLN
Tidle of Protocol:
Issue Date:
SponsorApproval Date:
Mathematical Modeling of the Cardiovascular System Using Radial Artcry
Pressure Waveforms
07/10/2001
Departmental Funds
07/10/2001
This certifies that the Application referenced above was reviewed by an appropriately authorized
Institutional Review Board (IRB) appointed to review research involving human subjects. The IRB
approved the Application. In their review, the IRB specifically considered (i) the risks and anticipated
benefits, if any, to subjects; (ii) the selection of subjects; (iii) the procedures for securing and documenting
infommed consent; (iv) the safety of subjects; and (v) the privacy of subjects and confidentiality of the data.
NOT
Protocol, Protocol Sunnary and Medical Records are approved.
INVESTIGATOP.., please note the following:
1.
2.
3.
4-
Use only IRB approved copies of the consent fonn(s), questionnaire(s), letter(s), advertisement(s),
etc. in your research. Do not use expired consent forms.
Any modifications or changes made to the study must be submitted to the IRB in writing for
review. The [RB must approve all changes before they can be initiated.
Any serious and/or unexpected adverse event in a study subject and/or death of a subject is to be
reported to the nRB within 24 hours followed by a written report within 10 working days of the
event.
The MGO assurance number is: M1331. Form FDA 1572 and NI grant submissions or follow-up
certifications for this protocol should reference the appropriate institution and/or institutional assurance
number
All administrative requirernents for the above referenced protocol have bei i met. This protocol is
activated for recruitment and enrollment of subjects.
The MGH is the IRB of record for this protocol. Direct any questions, correspondence and forms (e.g.,
continuing reviews, amendments, adverse events, safety reports) to Fred Syliien, MG,-I, (617) 726-3493
07/10/2002
Expiration Date of IRB Approval
Q8/l0//Q
Date
Fred Syllien
Protocol
mistr tor
cc- Sandra dcBronkart
SG!Sc"ALHOSI-
74
Appendix 4
BWH/DFCI/MGH HUMAN SUBJECTS RESEARCH APPLICATION
1. PRINCIPAL/OVERALL INVESTIGATOR (cannot be resident or
Name: Marcos F. Vidalmelo M.D. Ph.D.
research
fellow
except for hem/onc. studies)
First Name, Middle Initial, Last Name. Degree(s)
Institution:
E] BWH
E] DFCI
ZMGH
Dept/Service:.Anesthesia and Critical Care
Employee
ID#:.
Div/Unit: Cardiac Anesthesia
Address: CLN3-309, Massachusetts General Hospital
Telephone:.617-726-3030
FAX:.617-726-5985
Beeper:.35592
E-Mail: mvidalmelo@iipartners.org
2. STUDY TITLE
Measurement of Hemodynamics During Cardiac SurgerY
In our opinion, the protocol and safeguards described in the attached application are adequate to meet the standards
of the Brigham & Women's Hospital (BWH), the Dana Farber Cancer Institute (DFCI), the Massachusetts General
Hospital (MGH), the United States Department of Health and Human Services (DHHS), and the Food and Drug
Administration (FDA) in regard to investigations which use human subjects.
We consider specifically that the rights and welfare of the individual(s) involved, the appropriateness of the methods
used to secure informed consent, and the risks, if any, are so outweighed by the potential benefit to the subject
and/or the importance of the knowledge to be gained, as to warrant the Institutional Review Board's (IRB) decision
to permit subjects to accept these risks.
We the undersigned, accept responsibility for assuring adherence to the Department of Health and Human Services
and the Institute/Hospital's policies relative to the protection of the rights and welfare of patients/subjects used in
this study.
I certify that I am in full compliance with the Harvard University Faculty of Medicine policy on conflicts of interest.
PRINCIPAL/OVERALL INVESTIGATOR
(sgn and date above)
Non Hematology/Oncology Protocols must provide the Department Chair's Signature for each participating department:
CHAIR OF DEPARTMENT (sign & date above)
(type name & department above)
CHAIR OF DEPARTMENT (sign & date above)
(type name & department above)
CHAIR OF DEPARTMENT (sign & date above)
(type name & department above)
Hematology Oncology Protocols must provide the following signature and informationt
Hem/One Only PROGRAM LEADER or REPRESENTATIVE
(sign & date above)
(type name & department above)
This protocol is the property of the BWH/DFC/MGH; it may contain information that is confidential and proprietary to the I3WH/DFC[/MGHt
or the study sponsor. Its distribution is restricted in accordance with BWH/DFCI/MGil policy and approval by the BWH/DFCI/MGH is
required for outside distribution.
BWH/DFCI/MGH Human Subjects Research Application Form
filename: 3-form.doc
Page
Version 3: March 1998
75
1
Appendix 4
BWH/DFCI/MGH HUMAN SUBJECTS RESEARCH APPLICATION
A Site Responsible Investigator with staff privileges must be listed for each site where the research is being
conducted unless the principal investigator has staff privileges at each of the sites.
1. SITE RESPONSIBLE INVESTIGATOR (cannot be resident or research fellow except for hem/one studies)
Employee ID#:
Name: Marcos F. Vidalmelo M.D. Ph.D.
First Name, Middle Initial, Last Name, Degree(s)
fl BWH
Institution:
Dept/Service:
Address:
fl DFCI
Z NIGH
[]~_Other Explain:
Div/Unit:
Anesthesia and Critical Care
CLN3-309, Massachusetts General Hospital
Telephone:
617-726-3030
FAX:
Beeper: 35592
617-726-5985
E-Mail/Internet Address: mvidalmelo(apartners.org
2. STUDY TITLE
Measurement of Hemodynamics Durina Cardiac Surgery
In our opinion, the protocol and safeguards described in the attached application are adequate to meet the standards
of the Brigham & Women's Hospital (BWH), the Dana Farber Cancer Institute (DFCI), the Massachusetts General
Hospital (NIGH), the United States Department of Health and Human Services (DHHS), and the Food and Drug
Administration (FDA) in regard to investigations which use human subjects.
We consider specifically that the rights and welfare of the individual(s) involved, the appropriateness of the methods
used to secure informed consent, and the risks, if any, are so outweighed by the potential benefit to the subject
and/or the importance of the knowledge to be gained, as to warrant the Institutional Review Board's (IRB) decision
to permit subjects to accept these risks.
We the undersigned, accept responsibility for assuring adherence to the Department of Health and Human Services
and the Institute/Hospital's policies relative to the protection of the rights and welfare of patients/subjects used in
this study.
I certify that I am in full compliance with the Harvard University Faculty of Medicine policy on conflicts of interest:
(sign & date above)
SITE RESPONSIBLE INVESTIGATOR
Non ilematology/Oncology Protocols must provide the Department Chair's Signature for each participating department:
DEPARTMENT (sign & date above)
(type name & department above)
CHAIR OF DEPARTMENT (sign & date above)
(type name & department above)
CHAIR
CHAI
OF
OF DEPARTMENT
(type name & department above)
(sign & date above)
Hematology Oncology Protocols must provide the following
signature and
information:
Hein/One Only PROGRAM LEADER or REPRESENTATIVE
(type name & department above)
(sign & date above)
This protocol is the property of the [WVI/DFCI/MGH; it may contain information that is confidential and proprietary to the lIWHI/DFCI/MGI
or the study sponsor, Its distribution is restricted in accordance with 3WH/DPCI/MGII policy and approval by the BWH/DFCfMGH is
reqUired for outside distribution.
BWH/DFCI/MGH Human Subjects Research Application Form
Version 3: March 1998
76
filename: 3-form.doc
Page Ia
Appendix 4
3. CO-INVESTIGATORS:
(Copy this page as necessary for additional co-investigators)
I have reviewed this protocol and acknowledge my participation. I accept responsibility for assuring adherence to
the Department of Health and Human Services and Hospital/Institute policies relative to the protection of the rights
and welfare of patients/subjects enrolled in this study. I certify that I am in full compliance with the Harvard
University Faculty of Medicine policy on conflicts of interest.
Name: Edwin T. Ozawa M.D. Ph.D.
First Name, Middle Initial, Last Name, Degree(s)
f
Institution:
BWH
(]DFCI
Z MGH
Employee ID#: 3374937
Div/Unit:
Dept/Service: Anesthesia and Critical Care
Address: CLN3
Telephone:
FAX:
Beeper: 36214
617-726-3030
E-Mail: eozawa(qTalurn.mit.edu
Date:
Signature:
Name:
First Name, Middle Initial, Last Name, Degree(s)
Institution:
E BWH
[]DFCI
E] MGH
Employee ID#
Div/Unit:
Dept/Service:
Address:
FAX:
Beeper:
Telephone:
E-Mail:
Date:
Signature:
Name:
First Name, Middle Initial, Last Name. Degree(s)
Institution:
BWH
DFCI
Q MGH
Employee ID#:
Div/Unit:
Dept/Service:
Address:
Telephone:
FAX:
Beeper:
E-Mail:
Date:
Signature:
BWH/DFCI/MGH Human Subjects Research Application Form
Version 3: March 1998
77
filename: 3-form.doc
Page 2
Appendix 4
4. STUDY STAFF
Name:
First Name, Middle Initial, Last Name
Institution:
[
fl BWH
DFCI
[] MGH
Indicate role on project (check all that apply):
El Research Nurse L Research Coordinator
Employee ID#:
[
Other, Specify:
Div/Unit:
Dept/Service:
Address:
E-Mail Address:
Tel:
Name:
First Name. Middle Initial, Last Name
Institution:
Employee ID#:
MGH
E]DFCI
E] BWH
Indicate role on project (check all
[3
Research Nurse
[3
that apply):
Research Coordinator
[]
Other, Specify:,
Div/Unit:
Dept/Service:
Address:
E-Mail Address:
Tel:
Name:
First Name, Middle Initial, Last Name
Institution:
[]IBWH
[3DFCI
[MGH
Indicate role on project (check all that apply):
[] Research Nurse [3 Research Coordinator
Employee
ID#:
Other, Specify:
Div/Unit:
Dept/Service:
Address:
E-Mail Address:
Tel:
5. fF YOU WOULD LIKE TO HAVE SOMEONE (WITHIN PARTNERS) OTHERTLAN THE PRINCIPAL INVESTIGATOR
RECEIVE COPIES OF 1RB CORRESPOND ENCE REGARDING THIS PROTOCOL, COMPLETE SECTION BELOW:
Name:
First Name, Middle Initial, Last Name, Degree(s)
Employee ID#:
[1MGH
DFCI
[3BWH
Institution
D
Dept/Service:
Div/Unit:
Address:
Telephone:
FAX:
Beeper:
E-Mail Address:
BIWH/DFCI/MGH Human Subjects Research Application Form
Version 3: March 1998
78
filename:
3-orm.doc
Page 3
Appendix 4
If you have any questions or concerns about potential conflicts of interest, @BWH contact the Vice President for
Corporate Sponsored Research at 278-1088; @DFCI contact the Director for Research at 632-3488; and @MGH
contact the Assistant Director, Office of Corporate Sponsored Research at 726-1069.
6. SPONSOR: (complete separate sheet for each sponsor)
Sponsor Type:
L] Government [j Foundation Z Industry
If Sponsor Type 'Other', explain: MIT Fluid Mechanics Laboratory
Z Grant
Application Type:
If Application Type 'Other', explain:
E] Subcontract
Contract
[
[]Internal
Other
[
Other
Sponsor/Agency:
Sponsor Deadline (if applicable):
Grant No.
If known Hospital Grant No.
Title of Proposal (ifdifferent):
Applicant Institution:
Other
0 DFCI
BWH
MGH
[J1 OTHER
Institution:
Principal Investigator:
Marcos F. Vidalmelo
Who initiated study'?
Z
fl~
Sponsor
[] Cooperative Group
Q NCI
Investigator(s)
Will the sponsor provide funding?
0
Will sponsor provide free drug and/or device?
No
Yes
[] Yes
No
Indicate below who will cover patient/subject-related research costs (check all
0
Sponsor
[] Dept Funds
g
F
Third Party Payers
chat apply):
SubjeCLs
0
N/A
In general, all research-related patient/subject costs must be covered by the sponsor. Therefore, if patients or third
party payers will be charged for research-related costs, explain below what costs will be billed to the patient or
his/her insurer and why these costs are not being covered by the sponsor or departmental funds.
none
Sponsor Contact Person: Roger D. Kamm. M.I.T.
Sponsor Contact Tel: 617-253-5330
Will any data generated from this study be submitted to the FDA?
f
YES
Z NO
The principal/overall investigator's signature on the first page of this application form certifies s/he is in full
compliance with the Harvard University Faculty of Medicine policy on conflicts of interest.
BWH/DFCI/MGHl Human Subjects Research Application Form
Version 3: March 1998
79
filename: 3-form.doc
Page 4
Appendix 4
7. NUMBER OF SUBJECTS: (enroltment at this site and study-wide [total enrollment all sites)
ENROLLMENT AT THIS SITE (#): 20
(total enrolled from sites Indicated below, e.g., 8WH, DFCI, NIGH)
SUBJECTS WILL BE ENROLLED AT:
OTHER, explain:
8. TYPES OF SUBJECTS:
El
El
fl
(total enrolled at all sites, e.g., nationwide)
BWH
E] DFCI
Z
[E] OTHER
MGH
(check all that apply)
f
Normal Volunteers
Pregnant Women
Mentally Disabled
Students/HMS Students (must have HMS Dean's approval)
~] BWH/DFCI/MGH employees
[] Other, explain:
Fetuses
Newborns/Infants
Children (2-12)
Adolescents (13-17)
Adults (18-64)
Adults (65+)
9. SOURCE OF SUBJECTS:
[~
(check all that apply)
Primary Physician
Emergency Room
Outpatients/Clinics
~ Newspaper/Radio/Television Advertising
[~ Postings within Hospital(s)
E-Mail Announcements
Internet Sites
Registries (e.g. cancer registry) (Indicate registry):
E] Other, explain:
Inpatients
[
El
ENROLLMENT STUDY-WIDE (#): 20
Medical Records
Census/Public Records
Discarded Human Materials
NB: The text of all advertisements used to recruit subjects must be submitted for IRB approval.
10. SITE UTILIZATION: (check all that apply)
H Inpatient
BWH
H Outpatient
Clinical Research Center
E Clinical Trials Center
DFCI
] Outpatient
Z Inpatient
MGH
Outpatient
Other
[
11. STUDY
[~
H
H1
MRT Suite
Operating Room
Clinical Research Center
(explain):
TYPE:
(check all that apply)
[ Therapeutic
F1Diagnostic
If 'Other' study type, explain:
Z
Physiologic
E]Epidem iologic
Genetic
LJOther
12. KEYWORDS
Provide up to 6 keywords for your study (e.g., disease or condition being stildied, ctc.)
Cardiovascular monitoring
Cardiovascular disease
BWH/DFCI/MGII Human Subjects Research Application Form
Version 3: March 1998
80
filename: 3-form.doc
Page 5
Appendix 4
13. STUDY PROCEDURES Provide amplification of details in protocol for each section below.
13A. RECRUITMENT PROCEDURES: (check all that apply) (include copies with submission)
Z NO
Li YES Advertisements
Indicate how many different advertisements will be used:
Z NO
Li YES Letters
Indicate how many different letters will be used:
NO
Li YES Postcards
Indicate how many different postcards will be used:
NO
Li YES Telephone Calls
13B. CONSENT PROCEDURES: (check all that apply)
Z Written Consent Waived in Accordance with Federal Regulations
Li A patient advocate will be used to obtain consent
Consent to be Obtained:
Consent to be Obtained From:
Z
Z
Li
Li
E
Immediately prior to study
1-12 hours prior to study
12-24 hours prior to study
24+ hours prior to study
Consent to be Obtained By:
Li Principal Investigator
Z Co-investigator(s)
[ Research
Nurse/Assistant/Coordinator
Patient/Subject
[O Parent(s)
O Legally Authorized Representative
Residents/Fellows (not on protocol-Iem/onc studies only)
Staff Physicians (not on protocol-hem/onc studies only)
Other, explain:
13C. DURATION OF SUBJECT'S PARTICIPATION:
Active Participation (as defined by protocol):
If no active participation, indicate why: use of records only
Follow-up (long-term follow-up after study completion):
13D. PATIENT DIARIES:
( NO
fl YES
Include copies with submission.
13E. QUESTIONNAIRES OR PSYCHOLOGICAL INSTRUMENTS: (include copies
Z NO
fl YES
Indicate how many questionnaires/instruments will be used:
13F. REMUNERATION:
NO
[~1 YES
If YES, complete below:
f
O
]
Cash
Parking
Amount:
Amount:
E] Transportation
Other, explain:
with submission)
Amount:
Amount:
Vouchers
13G. RESEARCH-RELATED USE OF ANY OF THE FOLLOWING: (if YES, complete appropriate forms)
Drugs/Biologics Form (4_ drug.doc)
NO
YES Drug(s) or Biologic(s)
Medical Device Form (3-device.doc)
YES Medical Devices
NO
YES Lasers, MRI, Ultrasound
Nonionizing Radiation Form (6-nonion.doc)
NO
Radiation Exposure Form (7-X-rays.doc)
YES X-rays and/or Radioactive Drugs
NO
Human Materials Form (8-dishum.doc)
NO
YES Discarded Human Material
NO
YES Medical Records
Medical Records Form (9-inedrec.doc)
Contact A dministrator (732-7793)
YES Clinical Research Center (BWH)
NO
Contact Administrator (732-8100)
NO
YES Clinical Trials Center (BWH)
NO Q YES General Clinical Research Ctr (MGH) Contact Administrator (726-6886)
Complete Nursing Form (nursi .doc)
Z NO Li YES Nursing Services
13H. USE OF SPECIMENS: (Amplification of details required in protocol and consent form for any 'YES' answer)
[ NO E] YES Will genetic research be done on biologic samples?
NO
Z
NO
NO
NO
L
Li
Li
Li
(if YES, must follow Genetic Guidelines and include appropriate language in the protocol and consent form)
YES
Will permanent or immortal cell lines be developed?
YES
YES
Will samples be stored/banked for future use not detailed in this protocol?
Will samples be shared with other researchers, sponsors, etc. not associated with study?
YES
Will samples be used for research unrelated to this study?
(if YES, samples must be anonymized)
BVII/DFCI/MGI I Human Subjects Research Applicafion Form
filename: 3-form.doc
Page 6
Version 3: March 1998
81
Appendix 4
BWHDFCI/MGH HUMAN SUBJECTS RESEARCH APPLICATION
DEPARTMENT/DIVISION PEER REVIEW FORM
(for use of human subjects in research)
Principal/Overall
Investigator: Marcos Vidalmelo
Study Title: Measurement
of Hemodynamics During Cardiac Surgery
DEPARTMENT/DIVISION PEER REVIEW
1. Do you recommend any changes or modifications to the proposed protocol? If YES,
please list below and make sure they have been incorporated before submission to the
O
YES
S
YES
E
NO
IRB.
2.
3.
4.
5,
6.
7.
8.
9.
Do you recommend scientific and/or administrative review by any other
BWHIDFCI/MGH department or division? If YES, address in comments.
Does the protocol deviate from standard practice at BWI/DFCI/MGH or in the medical
community?
If there are deviations from standard practice, are these adequately addressed in the
protocol and consent form?
[ Not applicable
Is the rationale for this study supported by pre-existing data?
Are the methods proposed to perform this research adequate to answer the research
question?
Is the value of the investigation or the potential benefit to a subject sufficient to warrant
the discomfort, risk, and inconvenience for the subjects who consent?
Are the proposed recruitment approaches reasonable for the potential study subjects and
for the institution?
Are those who are conducting the research, collecting the data, and performing any
invasive or non-invasive procedures competent in these techniques?
5
5
NO
YES
L
NO
YES
YES
YES
L
5
S
NO
NO
NO
YES
5
NO
YES
NO
YES
NO
REVIEWER COMMENT(S)
DEPARTMENT/DIVISION REVIEWER
Name of Reviewer (type) (Can NOT be associated with protocol)
Signature of Reviewer
Date
13Wl/DFCI/MGH Human Subjects Research Application Form.
Version 3: March 1998
82
filename: 2-review.doc
Page 1
Appendix 5
QUALITATIVE COMPARISONS OF INPUT AND RECONSTRUCTED RADIAL
PRESSURE PROFILES FOR FIVE ANALYZED SUBJECTS
Patient 3
Height (cm)
167.64
Wei ht (Ibs)
160
Medical Condition
82F with angina, hypertension, hyperlipidemia. 3 vessel CAD [LAD: 80%
stenosis, RCA: 90%, LCX: 80%] Normal LV function (EF- 65%). No
evidence of MR. Elevated LVEDP.
CAD: Coronary Artery Disease, LAD: Left Anterior Descending Artery, RCA: Right Coronary Artery, LCX: Left
Circumflex Artery, LV: Left Ventricle, EF: Ejection Fraction, MR: Mitral Regurgitation, LVEDP: Left Ventricular
End Diastolic Pressure
83
Appendix 5
Patient 9
Height (cm)
Weight (ibs)
Medical Condition
170
175.5
73M with severe infarct areas and ischemia. EF: 40-50%. Multiple
occlusions in Coronary Arteries.
EF: Ejection Fraction
84
Appendix 5
Patient 11
Height (cm)
Medical Condition
Weight (lbs)
61M with history of CAD, hypertension, and hypercholesterolemia. EF:
64% with inferoposterior dysfunction. Trace MR and no AS.
CAD: Coronary Artery Disease, EF: Ejection Fraction, MR: Mitral Regurgitation, AS: Aortic Stenosis.
183
209
85
Appendix 5
Patient 13
Medical Condition
77M with long history of CAD. Severe disease of native vessels.
Occluded LAD, proximal RCA, mid CFX. Prior CABG (1982).
CAD: Coronary Artery Disease, LAD: Left Anterior Descending Artery, RCA: Right Coronary Artery,
CFX: Circumflex Artery, CABG: Coronary Artery Bypass Graft.
Height (cm)
175.26
Weight (ibs)
128
86
Appendix 5
Patient 20
Height (cm)
Medical Condition
Weight (ibs)
67M with high blood pressure & cholesterol, prior angioplasty and back
surgery. LAD: 60% stenosis, LM: 40%, LCX: 95%. EF: low normal.
Smoker.
LAD: Left Anterior Descending Artery, LM: Left Main Artery, LCX: Left Circumflex Artery, EF: Ejection Fraction
1
160
87
Appendix 6
RUNNING THE CODE
A. Data (Pre)-Processing
" Open the saved VI files in Excel. You should see 4 columns of data, corresponding to EKG,
RA, PA & CVP (if all went well during the measurement).
* Multiply all 4 columns' values by 100 to bring it to units of mmHg.
* Include an extra column for time (in increments of 0.01s)
* Plot
* Select a characteristic cycle, i.e.
o beginning from the minimum value at the initial upstroke of the RA waveform to the
minimum value at the beginning of the next cycle, and
o the beginning of the Q (or R) wave on the EKG line.
* From this cycle, calculate the HR. Also calculate the mean CVP and mean PA for that
corresponding cycle. You can now calculate the Systemic Vascular Resistance:
SVR =
P
-CVP
c
Co
x
1333.2 x
60
I0(1)
1000)
* From the patient's height, the std len & radial length can be calculated from the ratios in
Table 4 in the thesis.
* Knowing the HR, the PEP may be calculated from Weissler's formulae.
" delta t = time of upstroke of RA profile - time of Q wave on EKG - PEP
* Cmean = (Rad. Len/delta t)
" C0 can be calculated from Cmean using the relationship in Fig. 15 of the thesis.
" From the standardized, simplified Moens Korteweg equation, e x (106)= 4 x (Co / 462)2
You now have all the data needed to run the code. Please refer to Complete Wavespeed
Calculations.xls if more help is needed/to see an actual spreadsheet; located in
fluids20 /E : /Janice/research,and Entry 70 (Fri, 8/30/02) in my Research Logbook.
See also Entry 69 (8/26/02) and p.26 of the thesis for more clarification on 'standard' and 'real'
values.
B. Running the Code
Accessing fluids30
Login: jstan
Password: Janice7
Administrator's Password: cfdlove7
The general pathway is:
'/data2/users /j stan/cODES /programs' which contains the
subdirectories of outputs, inputs etc. The correct version of the CV model is:
networks . newrecon. c NOT networks . new. c
88
Appendix 6
Parameter Estimation Routine
You will need: 1) RA profile (store it in the outputs directory. It has to be in the same directory
as the par. est. routine to be able to be read by MatLab)
2) HR, (std) len, e
Open a new window. At the prompt:
>>tcsh
>>cdCVM
%stands for change disk to CardioVascular Model%
This will automatically lead you to the outputs sub-directory:
/data2/users/jstan/CODES/programs/outputs
>>mat lab
%launch MatLab%
>>genscrexp4 f
* Input the requested variables, i.e. Real HR, len, e and name of the file of the stored RA
profile
* Run the program. This takes 5-10 min.
* When done, record the estimated par. values, test2, fest2 and the objective
function.
o tes t2 contains all the feature values of the RA profile that was input.
o fest2 contains all the feature values of the matched library RA profile. The features
are: dP/dtmax ,Pmean, AP = max - min Pressure, Pmax
o The obj ective function should be ~ O.Ox. Anything larger than 0.3 is very large!!
Reconstruction
Change to programs directory, and open batchlistrecon . m and
reconstructlibbase2 .m in the text editor
* Enter values of e and the forearm length for ge and glen in batchlistrecon . m. Save.
*
Inreconstructlibbase2.m,
enter values in p2 =[(std) HR ELv EDV Q SVR CVP]. Save.
o ELv , EDV and SVR are the estimated parameter values from above
o Q and CVP are constants at 0.57 and 5.0 respectively
o Remember, std HR # real HR (which is input in the par. est. routine)!
* Run the program, i.e. >>batchlistrecon
Should run till cycle 11, with an eta value > 100; - 5-10 minutes also.
* 'Realize' the values and plot the reconstructed curve. Here is the command sequence:
>> load netout
c = (netout(:,l) - min(netout(:,1)))*462/22.9/c*l
rwav = [c(:,1), netout(:,116)*(c/462)^2]I
crop = [rwav(1,m:n)-p; rwav(2,m:n)]
%p = value of t at Col. m %
z=[crop(1,:),rwav(1,1:m-1)+ q + 0.01;crop(2,:),rwav(2,1:m-1)]
% q = time value at the last column of crop %
>> plot(z(1,: ), z(2,: ))
* Note that c, rwav, crop are variable names. See Entry 66 (8/11/02) and on Sat (9/7/02) in
the Research Log for more details.
>>
>>
>>
>>
89
Appendix 6
" Do NOT use the CO value from aortic file ( 1st column, last row), as this is less accurate.
Instead, back calculate it, as will be explained in the next section on Post Processing.
* All the runs conducted are numbered sequentially and their data values are contained in the
blue exam booklets titled: Model Codes (III - V): Patient Testing. Actual waveforms/plots
are also numbered as such (e.g. 21.fig), and are stored in the programs directory of fluids30.
(/data2/users/jstan/CODES/programs)
C. Post Processing
From the Reconstructed Waveform ...
(Remember, everything has now been realized (from the commands in the 9/7/02 entry))
* Calculate Pmean from the (real) values of the reconstructed curve. Knowing the estimated
SVR and (constant) CVP = 5.OmmHg, the estimated CO can be calculated as in Eqn. (1)
above.
* Calculate the absolute percentage errors using the formula below:
%error=
est - real
real x00
real
(2)
Further Analysis
* Perform Bland Altman analysis
" Use Critchley's Error-gram method
* Inter - patient Analysis
* Inter-procedural Analysis
* Note effect of CVP
* Qualitative analysis of reconstructed profiles with respect to input parameters, feature sets,
objective function etc.
* Validate ELv and EDV
90
Appendix 6
FLOWCHART OF DIRECTORIES ON FLUIDS30@MIT.EDU
/data2/users/jstan/CODES
libbackup
I
1-Processing
new-gui
programs
I
I
3D Plots
Plots
I
I
Results
I
Trash
Trials
I
I
gui
outputs
I
inputs
I
Everything
else
JT's Work
Janice's trials
Everything else
Notation:
1) Subdirectories/foldersin BOLD are containedon CD2. 'Everything else' refers to the numerous individualfiles not contained in a
separatefolder. If the files from CD2 are used, the new user should ensure that the relevantfiles are 'owned by the new user' and that they are
in the correct mode (rewritable/executable);namely the
in inputs and batchlistrecon in programs.
2)
a. out & testb* files in outputs, reconstructlibbase2 .m
>>chown username filename(s);
newgui and gui refer to the GraphicalUser Interface preparedby Xiao.
91
& 1* files
>>chmod a+rwx filename (s)
]