The Doctors’ Challenge 2013 LTCIF New Orleans, LA

The Doctors’ Challenge
2013 LTCIF
New Orleans, LA
Today’s Panel
• Dr. Stephen Holland
Chief Medical Officer, Univita Health
• Dr. Bruce Margolis
Medical Director, Genworth Financial
• Dr. Bryan Yanaga
Medical Director, Bankers Life and Casualty
Session Format
• 6 cases will be reviewed
• Case details shared for each case
• Discussion lead by one panelist with input from others
• Questions/comments from the audience are welcome
• Chance for you to ask about your tough cases
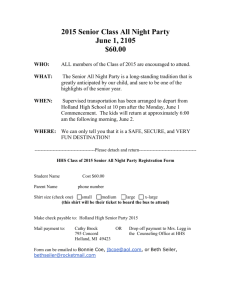
Case # 1 – UW
(Dr. Holland)
All too typical LTCI applicant
58 years old male, applying for a 6-year LTC policy, 90 day EP, $300/day, spouse disc
History of hypertension on metoprolol 25 mg daily and HCTZ 25 mg. daily
Sedentary, no regular exercise, non-smoker, 1 glass a wine daily
Family history: Father deceased age 79 d/t MI, Mother alive with Alzheimer’s age
84
APS
– 3-4 visits per year for health maintenance, dietary counseling
– BPs average 134/90, normal physical exam, BMI 32
– Labs: Normal electrolytes, Creat/BUN normal, CBC normal, FBS 123mg%
– Lipids: Cholesterol 240 mg/dl, HDL 32 mg/dl, LDL 132 mg/dl, Triglycerides 220 mg/dl
– EKG: Normal
– Chest x-ray: Normal
– Colonoscopy: Normal
Case # 1 – UW
(Dr. Holland)
Underwriting Questions:
– Is this gentleman insurable?
– At a Standard Rating?
– For the policy requested?
Case # 2 – UW
(Dr. Margolis)
What’s the LTC Risk?
– 55 yo male; applying $235/day, 5 years, 90 day EP
– Build: 5’10”/250lbs (BMI 36)
– Notes HTN on Micardis® and metoprolol; non-smoker
– Has a PCP and a cardiologist
– Works as a civil engineer
– Father deceased age 70 - CVA
– Prescription drug report – consistent with application
– Medical records:
• HTN, hyperlipidemia, OSA on CPAP
• FBS 122mg%; BUN/Cr 14/1.0; cholesterol141mg/dl; triglycerides 192 mg/dl; HDL 39 mg/dl; cholesterol/HDL ratio 3.6
• Nuclear stress test 4/12 - negative
• Carotid doppler 4/12 - mild plaque right ICA; no stenosis
• Echocardiogram 3/12 – mild LVH, no VHD, mild dilation aortic root
• CT chest 3/12 – stable 4cm ascending aortic aneurysm unchanged from
11/07; calcification left coronary artery
Case # 2 – UW
(Dr. Margolis)
Underwriting Questions:
– What’s the overriding diagnosis?
– Is the ascending aortic aneurysm of concern? Risk of rupture?
– What’s his cardiovascular risk?
– Is he insurable?
Case # 3 – UW
(Dr. Yanaga)
A Common Presentation
– 63-year old woman, $150/day, 3 years, 30 day EP
– Said to be physically active and in excellent health
– HTN, hyperlipidemia
– Hyzaar, Crestor
– Lap band surgery 9 months ago. Lost a total of 70 lbs
• 5’5”, 210 lbs (APP), BMI = 34.9
• 5’5”, 230 lbs (APS), BMI = 38.3
– At her most recent PCP visit she complained of a 4-6 week history of right ankle pain that began after walking her grandchildren to school
(0 to 3 out of 10 at rest. 3 to 6 out of 10 with ambulation.) She was referred to PT by her podiatrist, but never attended. No diagnostic testing has been performed.
Case # 3 – UW
(Dr. Yanaga)
Underwriting Questions:
– How will you rate for Build?
– How will you rate for Build in the face of recent weight loss?
– How will you rate for Pain?
Case # 4 – CL
(Dr. Holland)
A Case of Too Much Holiday Cheer – Part 1
78 years old male found at home at Christmas, disoriented and confused
TQ LTCI Policy Effective Date: 7/1/1996, 5 year, 90 day EP, $300/day, spouse disc
Hospitalized for delirium, creatinine 8.2 mg/dl, BUN 100, glucose: 532 mg%, BAC
0.15%
Diagnosis: Diabetic nephropathy, ETOH, chronic renal failure, dementia; dialysis begun
Discharged to nursing home after 21 day hospital stay in a debilitated state
MDS: Renal failure, diabetes, dementia, 4 of 6 ADL dependent, poor decision making
Medical Records were obtained
– Diagnoses of diabetes, chronic renal failure on hemodialysis (twice weekly), dementia
– Rx: insulin, low protein diet, beta blocker
Working with Care Manager, discharged to ALF after 45 day nursing home stay
Attending MD sends in Carrier’s Chronically Ill Statement stating 4/6 ADL + Cognitive
Eligibility approved, benefits begin
When and how would you reassess this claimant?
Case # 4 – CL
(Dr. Holland)
A Case of Too Much Holiday Cheer – Part 2
Reassessment at 90 days
- ALF records reviewed, ongoing assistance with 2 of 6 ADLs, poor decision making,
- Dialysis once a week
- Chronically Ill Statement sent in from attending MD
Medical Records obtained
– Diagnoses of diabetes, chronic renal failure on hemodialysis (weekly), dementia
– Rx: insulin, low protein diet, beta blocker
– Note in medical record that patient adjusting to ALF, home has been sold
Approved for ongoing benefits
When and how would you reassess this claimant?
Case # 4 – CL
(Dr. Holland)
A case of too much Holiday Cheer – Part 3
Reassessment at 45 days
ALF records received: ongoing assistance with 2 of 6 ADLs, poor decision making,
No mention of dialysis, “resident adjusting well to surroundings”
At family’s request, Chronically Ill Statement once again sent in from attending
MD stating 4 of 6 ADL dependencies and ongoing cognitive impairment
Invoices reviewed
– Room and Board only, several over night trips billed to claimant
When and how would you proceed?
In-person assessment and review of actual ALF care notes
Results of assessment and investigation
In-person assessment showed completely ADL independent, self-administers medications, no dialysis, no ongoing personal care other than IADLs in medical record, leaves facility often without an escort (bingo and horse races) – CLAIM
CLOSED
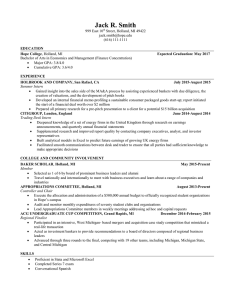
Case # 5 – CL
(Dr. Margolis)
A Claim or Not a Claim – That is the Question
– 60 yo female calls in to open a claim
– TQ Policy, Effective Date: 1/17/2006, 3 year, 90 day EP, $150/day
– Insured states has lost parents and spouse past 18 months
– Feels depressed and has developed problems with word finding and concentration; trouble getting out of bed; getting lost
– PCP declines to submit information; refers us to insured’s psychologist and psychologist
– Psychologist submits letter sent for SSDI determination in 11/12
• Several year history of MDD with three psychiatric hospitalizations
• Notes decline in memory and concentration; easily overwhelmed; confused at times; disorganized; forgets medication and bathing; purchased car she could not afford
• Dx: MDD with psychotic features, fibromyalgia; GAF 35
Case # 5 – CL
(Dr. Margolis)
A Claim or Not a Claim – That is the Question (cont.)
– In-home assessment
• Lives alone in own home
• Needs reminders for bathing and dressing; partially dependent for most
IADLs
• MMSE 29/30
• On anti-depressant and anti-anxiety medication
• Can spend days in her pajamas
• Two accidents while driving – cut corners too closely and blew out tires
Claim Questions:
– Is insured cognitively impaired?
– Could there be an associated dementia?
– Does the insured meet HIPAA definition of (severe) cognitive impairment?
– Any other work up necessary?
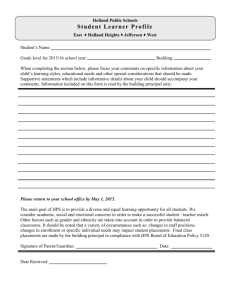
Case # 6 – UW
(Dr. Yanaga)
A TIA By Any Other Name…
– 74-year old man, $150/day, 3 years, 30 day EP
– Type 2 Diabetes (HbA1c=6.2), hyperlipidemia
– Metformin, Lipitor
– Smokes 1-2 cigarettes per day for 10 years
– 12-months ago he presented one day following an episode of mental confusion and right-sided weakness. Witnessed by his wife.
Symptoms resolved after 2 hours.
– 5’8”, 180 lbs (APP), BMI = 27.4
– Neurological exam: Negative
– MRI of the brain without contrast: Minimal age-related atrophy
– MRA of the head: Normal intracranial circulation and circle of Willis
– Recently received a letter from primary care physician: “He did not have a TIA. His symptoms were due to the use of Daliresp”.
Case # 6 – UW
(Dr. Yanaga)
Underwriting Questions:
– Will you rate for history of TIA?
– What value do you place on the information provided by the primary care physician?