CONGENITAL CARDIOLOGY TODAY
Timely News and Information for BC/BE Congenital/Structural Cardiologists and Surgeons
February 2016; Volume 14; Issue 2
North American Edition
IN THIS ISSUE
Surgical Outcomes in
Pediatric Patients, Who
Underwent Tetralogy of Fallot
Correction, Relative to
Different Techniques Used to
Relieve Right Ventricular
Outflow Obstruction
By Lorielyn G. Mandigma, MD
(Investigator); Ma. Bernadette A.
Azcueta, MD (Co-investigator);
Corazon A. Estevanez, MD
(Consultant Adviser); Mercilyn
Yap, MD (Consultant Adviser)
~Page 1
Tools to Stay Organized: Using
Software to Enhance
Efficiency
By Animesh (Aashoo) Tandon,
MD, MS
~Page 12
Medical News, Products &
Information
~Page 14
Upcoming Medical Meetings
PICS-CSI Asia 2016 - Catheter
Interventions in Congenital,
Structural and Valvular Heart Disease
Mar. 3-5, 2016; Dubai UAE
www.csi-congress.n2g06.com/l/
105882733/c/0-844d-7ouiro-11nt
The 13 th International Dead Sea
Symposium (IDSS) on Innovations in
Cardiac Arrhythmias and Device
Therapy
Mar. 6-9, 2016; Tel Aviv, Israel
http://idss-ep.com
Congenital and Paediatric
Echocardiography From Basics to
Advanced
Apr. 28-30, 2016; Toronto, On Canada
www.cvent.com/d/zfqjx4
CONGENITAL CARDIOLOGY TODAY
Editorial and Subscription Offices
16 Cove Rd, Ste. 200
Westerly, RI 02891 USA
www.CongenitalCardiologyToday.com
Official publication of the CHiP Network
© 2016 by Congenital Cardiology Today
Published monthly. All rights reserved.
Recruitment ads pages: 4, 7, 9, 14
Surgical Outcomes in Pediatric
Patients, Who Underwent Tetralogy
of Fallot Correction, Relative to
Different Techniques Used to Relieve
Right Ventricular Outflow Obstruction
By Lorielyn G. Mandigma, MD (Investigator);
Ma. Bernadette A. Azcueta, MD (Coinvestigator); Corazon A. Estevanez, MD
(Consultant Adviser); Mercilyn Yap, MD
(Consultant Adviser)
Introduction
Tetralogy of Fallot (TOF) is the most common
Cyanotic Congenital Heart Disease, with an
incidence of approximately 0.5/1000 live births
(5% to 7% of congenital heart lesions).1 Before
the advent of surgical intervention, about 50%
of patients with Tetralogy of Fallot died in the
first few years of life, and it was unusual for a
patient to survive more than 30 years.2 Most
patients died in childhood with a rate of survival
of 66% at 1 year of age, 40% at 3 years, 11% at
20 years and 3% at 40 years.1,2 Nowadays, with
the advent of surgical repair, which includes
closure of the Ventricular Septal Defect (VSD)
and relief of Right Ventricular Outflow Tract
(RVOT), the long-term survival of TOF patients
has been greatly improved.1
Nevertheless, a myriad of potential
complications have been reported in operated
TOF patients that underlie the importance of
follow-up after surgery, even if they remain
asymptomatic.1 These complications include
rhythm and conduction disorders such as:
sudden cardiac deaths, pulmonary regurgitation
(PR) with RV dilatation and dysfunction,
residual RVOT obstruction. These
complications may lead to subsequent
hospitalizations, repeat operations, arrhythmias,
and heart failure, as well as death following
initial corrective surgery.1
These relevant postoperative residues bring
about limitation in the right ventricular function
and, accordingly, the quality of life and life
expectancy.
Review of Related Literature
Reparative surgery for TOF should ideally result
in complete closure of the VSD, preservation of
right ventricular form and function, with an
unobstructed right ventricular outflow tract
incorporating a competent pulmonary valve.3
Successful repair through a right ventriculotomy
was first achieved by Lillehei and Varco, using
“controlled cross-circulation” in 1954.4 Kirklin et
al. was the first to use a pump oxygenator for
the repair of TOF 1 year later.5 Improvements in
cardiopulmonary bypass technology, as well as
in surgical technique and perioperative care
made early repair feasible with low morbidity
and mortality. 6 Transatrial/transpulmonary
repair of TOF, which was first reported in 1963
by Hudspeth et al., has been an important step
in the evolution of TOF surgery.7 It was reintroduced by Edmunds et al. in 1976, and
popularized in recent years. The benefits of the
transatrial/transpulmonary approach are
believed to derive from eliminating a right
CONGENITAL CARDIOLOGY TODAY
CALL FOR CASES AND OTHER ORIGINAL ARTICLES
Do you have interesting research results, observations, human interest stories,
reports of meetings, etc. to share?
Submit your manuscript to: RichardK@CCT.bz
We are committed to the
lifetime management of
congenital heart disease.
Transcatheter and Surgical
Heart Valves
RVOT Conduits
Ablation Technologies
ICDs
Oxygenators and Filters
Cannulae
InnovatIve
TeCHnOlOGIeS.
EvEry StEp
of the Way.
Pacemakers
Pulse Oximetry Monitoring
for CCHD Screening
3rd Generation PFO, ASD,
and PDA Occluders*
Cerebral/Somatic Monitoring
These products are not
available in the US.
*
Melody-tPV.com
Medtronic | Minneapolis, Mn 55432-5604
Toll-free: 1 (800) 328-2518
UC201601683 en ©2015 Medtronic.
All rights reserved. 08/2015
M e ..m m n .K
Further,Together
ventriculotomy, which may lead to late right ventricular (RV) dilatation
and dysfunction, as well as increased risk of ventricular ectopic
activity.8 At our center, Tetralogy of Fallot correction has been
performed since 1975 when the center became operational. Since
1980, a local study by Bote-Nunez et al., has shown that both
transannular patch and valve-sparing techniques are already being
performed, and have had excellent late survival with only three known
late deaths due to cardiac-related causes.9 Subjects included in the
study belong to functional Class I and II. Residual pulmonary stenosis
was also noted on 2D echocardiogram in 60% of the subjects.9
3.
A study by Murphy et al. on the long-term outcome in patients
undergoing surgical repair of Tetralogy of Fallot showed an overall
survival rate of 95% 5 years after operation, 92% after 10 years and 15
years, 91% after 20 years, 87% after 25 years and 86% after 32
years.10 According to age at the time of operation: 30-year survival was
90% for less than 5 years old, 93% for 5 to 7 years old, 91% for 8 to 11
years old, and 76% for more than 12-years-old.10 According to
patching of pulmonary annulus, 30-year survival was 87% for those
without pulmonary outflow patch, 85% for those who had patching
through the annulus, and 88% for those who had patching up to the
annulus.10
Alternative Hypothesis:
Despite the high number of favorable outcome as shown in several
studies, several potential complications have been identified and
warrant the need for long-term follow-up.
Study Setting and Period
In the study by Cardoso et al., restrictive RV physiology was seen on
follow-up of most patients.11 Incidence varied from 50%-70% in the
study by Gatzolius et al. Restrictive physiology increases the chance of
ventricular arrhythmia and sudden cardiac death.12
To determine the relationship of the surgical technique used in
RVOT repair relative to the determined outcome.
Hypothesis
Null Hypothesis:
The surgical technique used in relieving RVOT obstruction has no
association in the development of unfavorable outcomes in patients
who underwent Tetralogy of Fallot correction.
The surgical technique used in relieving RVOT obstruction has an
association in the development of unfavorable outcomes in patients
who underwent Tetralogy of Fallot correction.
Methodology
Study Design
Prospective Cohort
Recruitment of subjects for the study took place at the Philippine Heart
Center from November 2012 to October 2014.
Inclusion and Exclusion Criteria
Inclusion Criteria
Pulmonary regurgitation (PR) complicating surgical repair of TOF is
common in all patients, with over 80% having at least moderate-tosevere PR. PR has been shown to be related to the use of a
transannular patch during RVOT reconstruction and aggressive
infundibulectomy involving the pulmonary valve annulus. The adverse
effects of PR include: progressive dilatation of RV, reduced exercise
capacity, arrhythmia and sudden death.13
- Tetralogy of Fallot patients whose age at the time of surgery
was 3-18 years old
Exclusion criteria
- TOF with pulmonary valve atresia
- TOF patients with associated Complex Congenital Heart
Disease
- TOF patients with genetic abnormalities
- Tetralogy of Fallot patients who had clinical signs of rightsided failure (jaundice, hepatomegaly, pulmonary venous
congestion) prior to surgery.
- Tetralogy of Fallot patients who had echocardiographic
findings of RV dysfunction prior to surgery.
Impaired exercise capacity after complete repair of Tetralogy of Fallot
is directly related to the degree of residual pulmonary regurgitation.14
Significance of the Study
The aim of this study was to provide current data on the surgical
outcome of Tetralogy of Fallot patients who underwent repair at our
institution. It also aimed to help establish a guideline on post-operative
monitoring and follow-up.
General Objective
To determine the outcome of pediatric patients who underwent
Tetralogy of Fallot correction in relation to the surgical technique used
in relieving RVOT.
Specific Objectives
1.
2.
To determine the surgical techniques used in relieving right
ventricular outflow tract obstruction (RVOT).
To determine the outcome of patients who underwent Tetralogy of
Fallot correction in terms of:
• Presence and degree of pulmonary regurgitation
• Presence and degree of residual pulmonary stenosis
• Presence of right ventricular dilatation
• Presence of RV dysfunction
• Systolic
• Diastolic
• Functional capacity
Sample Size
The sample size computed is n = 45 based on 95% confidence level,
maximum tolerable error of 10%, assumed rate of RV diastolic
dysfunction of 72.5%,14 and assumed census of TOF correction.11
Identification of Variables
Definition of Terms
1.
2.
3.
Tetralogy of Fallot – comprises a constellation of cardiac
findings that share the following common anatomic
abnormalities: large malaligned VSD, overriding of the aorta
over the septal defect, right ventricular outflow obstruction,
and right ventricular hypertrophy.
Dyspnea – difficulty breathing, observed as an increase in
respiratory rate and the use of accessory muscles in
breathing.
RV Diastolic Dysfunction – shall be defined
echocardiographically as the presence of any of the following
signs of diastolic dysfunction: a.) presence of prolonged
isovolumic relaxation time, b.) E/A reversal, d) E/A ratio >1.5,
e.) E/Ea > 10, or f.) presence RV restrictive physiology which
CONGENITAL CARDIOLOGY TODAY t www.CongenitalCardiologyToday.com t February 2016
3
4.
5.
is the presence of laminar antegrade diastolic PA flow
throughout the respiratory cycle, which is coincident with
atrial systole on 2D echocardiography.
RV Systolic Dysfunction – shall be defined.
echocardiographically as an impairment in any of the
following parameters: TAPSE, TDI systolic velocity, or RVEF.
Functional Capacity – defined as the individual’s capacity to
perform submaximal activities as measured by the distance
walked in six minute exercise test and therefore the ability for
patients to perform day-to-day activities.
Study Maneuver
Seeking Medical Director, Pediatric Inpatient
Cardiology Services
Join a Leading Healthcare System in South Florida
After approval of the IERB, eligible subjects for the study were
recruited, informed consent was secured from parents/guardians of all
subjects; assent form was also secured for patients 7-18 years old.
The eligible subjects were further grouped depending on the surgical
technique used in relieving their RVOT obstruction (Group A – TOF
patients who underwent transannular patching, and Group B – TOF
patients who underwent valve-sparing procedure). The demographic
characteristics, pre-operative clinical data (hematocrit, oxygen
saturation, pulmonary arteries and pulmonary valve Z-score, previous
palliative procedure) were obtained. The presence and degree of
residual pulmonary stenosis, presence and degree of pulmonary
regurgitation, right ventricular dilatation, RV dysfunction (systolic and
diastolic) were determined by echocardiographic assessment prior to
hospital discharge of subject (at least one week, up to one month postoperation). Transthoracic 2-dimensional echocardiography was
performed and interpreted on the eligible subjects by three
echocardiographers to avoid bias. RV diastolic dysfunction was
determined by the presenceof any of the following signs of diastolic
dysfunction by 2D echocardiography:
a)
b)
c)
d)
e)
0'
Joe DiMaggio
Children’s Hospital
AT MEMORIAL
Presence of shortened isovolumic relaxation time,
E/A reversal,
E/A ratio >1.5,
E/Ea > 10, or
Presence RV restrictive physiology.
Determination was done by M-mode imaging of the right ventricular
cavity, followed by detailed pulsed Doppler echocardiography:
transtricuspid and characteristics at the level of the tips of the valve
leaflets in apical 4-chamber view. The antegrade diastolic PA flow, E:A
ratio, and right ventricular isovolumic relaxation time was measured.
Tissue Doppler imaging was used to measure RV diastolic
dysfunction. For RV systolic function determination, the parameters
that were determined were RV ejection fraction, and tricuspid annular
plane systolic excursion (TAPSE). Tricuspid annular plane excursion
was used to arrive at a quantitative measurement of RV systolic
function by directing the M-Mode cursor from the apex to the medial
tricuspid annulus during systole or when RV shortens from base to
apex. Tissue Doppler imaging was also used to measure RV systolic
dysfunction.
The Six-Minute Walk Test (6MWT) was used to predict the functional
capacity of the subjects. Functional status classification was done using
the Modified Ross classification for heart failure in children. The SixMinute Walk Test was done on OPD follow-up (at least two weeks postoperation). For subjects aged three to six years old, psychological
conditioning regarding Six-Minute Walk Test was done prior to hospital
Joe DiMaggio Children’s Hospital is seeking a leader to direct its
busy and dynamic pediatric inpatient cardiac services division. The
desired candidate must be board certified in pediatric cardiology,
and should have proven leadership experience. The Medical
Director will lead a successful team of cardiac specialists and will
collaborate with the existing pediatric cardiologists, in-house
physician teams, intensivists, hospitalists and neonatologists in the
care of a growing population of patients with heart disease.
Responsibilities will include all aspects of inpatient cardiac care,
requiring demonstrated experience in a vast array of pediatric
cardiology modalities. The position offers competitive benefits and
a compensation package that is commensurate with training and
experience. Professional malpractice and medical liability are
covered under sovereign immunity.
About Joe DiMaggio Children’s Hospital
Joe DiMaggio Children’s Hospital opened in 1992 and has grown
to be the leading children’s hospital in Broward and Palm Beach
counties. With 232 beds, an 84-bed Level II and III NICU, 30-bed
PICU and 12-bed intermediate care unit, Joe DiMaggio Children’s
Hospital combines leading-edge clinical excellence with a childand family-friendly environment that emphasizes the Power of
Play. Located in the heart of South Florida, a region whose quality
of life attracts new residents from all over the country and around
the world, Joe DiMaggio Children’s Hospital offers a
comprehensive range of healthcare services – delivered with
kindness, dedication and compassion.
About South Florida
South Florida offers a dynamic urban/suburban lifestyle with an
abundance of cultural and recreational amenities, miles of beautiful
beaches, top-rated golf courses, zoos and wildlife refuges, a vibrant
arts community, museums and world-class dining. South Florida’s
high quality of life – including year-round summer weather, exciting
multiculturalism and no state income tax – attracts new residents
from all over the country and around the world.
Contact: Pamela Spangenberg, Physician Relations Specialist
Physician Recruitment and Business Development Division
Memorial Healthcare System
4320 Sheridan St, Hollywood, FL 33021
Office: 954-265-0903 Fax: 954-989-7959
jdchdoctor@mhs.net
Archiving Working Group
International Society for Nomenclature of
Paediatric and Congenital Heart Disease
ipccc-awg.net
CONGENITAL CARDIOLOGY TODAY t www.CongenitalCardiologyToday.com t February 2016
4
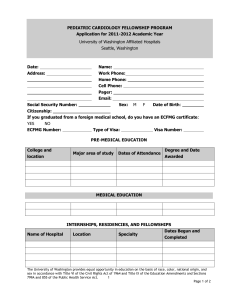
Table 1 – Pre-operative Clinical Data of Patients Who
Underwent TOF Correction
*Group A
**Group B
P value
N = 23 (%)
N = 40 (%)
Sex
1
Male
13 (56.5%)
23 (57.5%)
Female
10 (43.5%)
17 (42.5%)
Age (years + SD)
7.5 + 3.5
7.0 + 3.8
0.64
Weight (kg + SD)
22.5 + 10.64
19.5 + 9.89
0.27
Hematocrit
0.56 + 0.08
0.53 + .09
0.27
(SI unit + SD)
Oxygen saturation
77.7 + 7.0
77.6 + 7.4
0.94
(%+ SD)
Previous palliative
0.13
surgery
Yes
3 (13%)
1 (2%)
No
20 (87%)
39 (98%)
Z score
Right pulmonary
artery (z score + SD)
-0.95 + 0.93
0.79 + 0.86
0.49
Left pulmonary artery
(z score + SD)
-1.1 + 1
- 0.75 +0.78
0.17
Pulmonary valve
annulus (z score + SD)
- 2.5 + 1.7
- 2.1 + 1.1
0.27
* Group A – Transannular Patch Group
**Group B – Valve-sparing Group
discharge, and prior to the test on follow-up. If any of the subjects,
regardless of their age and reason, failed to finish the test, he/she was
rescheduled at another time within a month, until he/she was able to
complete the test. The data that were determined were: distance walked
in six minutes, oxygen saturation and heart rate during the six minutes and
during a three-minutes recovery period. The patient’s functional status was
assessed using the Modified Ross classification for heart failure in
children, which was done through patient and parent/guardian interview.
Plan for Analysis
Continuous variables were calculated as mean + standard deviation
or median and range. Significance was determined at a p value of
< 0.05. All p values are two-sided, and confidence intervals are 95%.
The two groups were compared by chi-square tests for dichotomous
variables and student’s t tests for continuous variables.
Ethical Considerations
The study was conducted in compliance with the ethical principles set
forth in the Declaration of Helsinki. Prior to the study initiation, a
review and approval of the study protocol and informed consent and
subsequent amendments by the Philippine Heart Center Institutional
Ethics Review Board (PHC IERB) was done.
Before a subject’s participation, a written informed consent was
obtained by the investigator after adequate explanation of the aims,
methods, anticipated benefits, and potential risks of the study. The
informed consent was signed and personally dated by the subject,
and the person who conducted the informed consent discussion. One
copy of the informed consent was given to the subject.
The investigator preserved the confidentiality of all subjects taking
part in the study. The investigator ensured that the subject’s
anonymity was maintained.
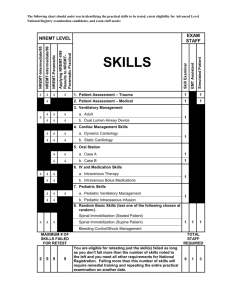
Table 2 – Post-Operative Outcome of Patients Who Underwent
TOF Correction
*Group A
**Group B
P value
N = 23 (%)
N = 40 (%)
Presence and degree of
0.798
pulmonary regurgitation
None
16 (69.6%)
26 (65%)
Mild
7 (30.4%)
11 (27.5%)
Moderate
0 (0%)
0 (0%)
Severe
0 (0%)
0 (0%)
Presence and degree of
0.229
residual pulmonary
stenosis
Mild
23 (100%)
20 (50%)
Moderate
0 (0%)
15 (37.5%)
Severe
0 (0%)
5 (12.5%)
Presence of right
1.0
ventricular dilatation
Yes
14 (60.9%)
24 (60%)
None
9 (39.1%)
16 (40%)
Presence of RV
0.6
dysfunction
Systolic
Yes
13 (56.5%)
19 (47.5%)
None
10 (43.5%)
21 (52.5%)
Diastolic
Yes
21 (91.3%)
None
2 (8.7%)
Distance travelled in six
297 + 71.3
minutes (meters + SD)
* Group A – Transannular Patch Group
**Group B – Valve-sparing Group
34 (85%)
6 (15%)
215.3 + 69.2
0.51
0.81
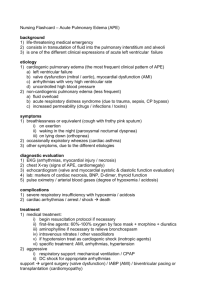
Table 3 – Functional Assessment by Modified Ross
Classification for Heart Failure in Children in Patients Who
Underwent TOF Correction
*Group A
**Group B
P value
N = 23 (%)
N = 40 (%)
Class I
0
0
1.0
Class II
22 (96.7%)
39 (97.5%)
Class III
1 (4.3%)
1 (2.5%)
Class IV
0
0
* Group A – Transannular Patch Group
**Group B – Valve-sparing Group
there was no significant difference between the two groups.
Table 2 shows the outcome of patients in the two groups during the
immediate post-operative period. Results showed that postoperatively, pulmonary regurgitation was more common among the
transannular patch group (Group A) at 30.4% compared to the valvesparing group (Group B) at 27.5%. All patients who had pulmonary
regurgitation in both groups have mild severity.
In terms of residual pulmonary stenosis, all patients in both groups
had residual pulmonary stenosis. Patients from the valve-sparing
group (Group B) had greater severity, with 15 having moderate
pulmonary stenosis, and 5 having severe pulmonary stenosis. This
finding, however, did not yield a statistical difference.
Results
Right ventricular dilatation was still present on most patients on both
groups, with Group A at 60.9% and Group B at 60%.
Table 1 shows the baseline characteristics of the two groups being
compared in this study. Results show that the subjects in Group A
were older and had a greater weight compared to Group B, although
RV systolic dysfunction was more common in Group A patients,
accounting for 56.5% of the group, while in Group B, it was present in 19
patients, accounting for 25% of the group.
CONGENITAL CARDIOLOGY TODAY t www.CongenitalCardiologyToday.com t February 2016
5
Proven
Performance.
Simply
DelivereD.
melody TPv
delays conduiT
rePlacemenT
98%
91%
Patients at 2 years
melody
®
Transcatheter Pulmonary valve Therapy
Data from US IDE Study
Patients at 5 years
Data from US IDE Study
melody-Tpv.com
medtronic | minneapolis, mn 55432-5604
Toll-free: 1 (800) 328-2518
uc201601525a en ©2015 medtronic.
all rights reserved 08/2015
Meottronic
Further,Together
Important Labeling Information for United States
Indications: The melody TPv is indicated for use as an adjunct to surgery
in the management of pediatric and adult patients with the following
clinical conditions:
• Existenceofafull(circumferential)RVOTconduitthatwasequaltoor
greater than 16 mm in diameter when originally implanted and
• DysfunctionalRVOTconduitswithaclinicalindicationforintervention,
and:
-regurgitation:≥moderateregurgitation,AND/OR
-stenosis:meanRVOTgradient≥35mmHg
Contraindications: none known.
Warnings/Precautions/Side Effects
• DONOTimplantintheaorticormitralposition.Preclinicalbenchtesting
oftheMelodyvalvesuggeststhatvalvefunctionanddurabilitywillbe
extremelylimitedwhenusedintheselocations.
• DONOTuseifpatient’sanatomyprecludesintroductionofthevalve,if
the venous anatomy cannot accommodate a 22-fr size introducer, or if
thereissignificantobstructionofthecentralveins.
• DONOTuseifthereareclinicalorbiologicalsignsofinfectionincluding
activeendocarditis.Standardmedicalandsurgicalcareshouldbe
strongly considered in these circumstances.
• Assessmentofthecoronaryarteryanatomyfortheriskofcoronary
arterycompressionshouldbeperformedinallpatientspriorto
deployment of the TPv.
• Tominimizetheriskofconduitrupture,donotuseaballoonwitha
diameter greater than 110% of the nominal diameter (original implant
size) of the conduit for pre-dilation of the intended site of deployment,
or for deployment of the TPv.
• Thepotentialforstentfractureshouldbeconsideredinallpatients
who undergo TPv placement. radiographic assessment of the stent
withchestradiographyorfluoroscopyshouldbeincludedintheroutine
postoperative evaluation of patients who receive a TPv.
• Ifastentfractureisdetected,continuedmonitoringofthestentshould
beperformedinconjunctionwithclinicallyappropriatehemodynamic
assessment.Inpatientswithstentfractureandsignificantassociated
RVOTobstructionorregurgitation,reinterventionshouldbeconsidered
in accordance with usual clinical practice.
Potential procedural complications that may result from implantation of
the melody device include the following: rupture of the rvoT conduit,
compressionofacoronaryartery,perforationofamajorbloodvessel,
embolizationormigrationofthedevice,perforationofaheartchamber,
arrhythmias,allergicreactiontocontrastmedia,cerebrovascular
events (Tia, cva), infection/sepsis, fever, hematoma, radiation-induced
erythema,blistering,orpeelingofskin,pain,swelling,orbruisingatthe
catheterization site.
Potential device-related adverse events that may occur following device
implantation include the following: stent fracture,* stent fracture resulting
inrecurrentobstruction,endocarditis,embolizationormigrationofthe
device, valvular dysfunction (stenosis or regurgitation), paravalvular leak,
valvularthrombosis,pulmonarythromboembolism,hemolysis.
*The term “stent fracture” refers to the fracturing of the Melody TPV.
However, in subjects with multiple stents in the RVOT it is difficult
to definitively attribute stent fractures to the Melody frame versus
another stent.
for additional information, please refer to the instructions for use
provided with the product.
CAUTION: Federallaw(USA)restrictsthisdevicetosalebyorontheorder
of a physician.
melody is a registered trademark of medtronic.
Medtronic
Further,Together
13- Medical City Children‘; Hospital‘
The City Just far Kids
Medical Director and Staff Level Pediatric
Cardiovascular Critical Care Physicians
General Pediatric Cardiologist
Pediatric Cardiac Interventionalist
Geneticist
Medical City Children’s Hospital has an unwavering focus on
patient care and offers world-renowned excellence in
comprehensive pediatric services. Since 1996, our specialists
haven’t let anything distract them from serving children. As a
result, we’ve helped thousands of children from more than 75
countries. We are a comprehensive children’s hospital with
specialists in virtually every pediatric subspecialty. Medical
City is the only facility in north Texas where fetal diagnosis,
maternal, neonatal and pediatric transport, high risk delivery
stabilization in the NICU, corrective surgery, state of the art
postoperative monitoring and care and long term follow-up of
patients with complex congenital heart disease can all be
delivered under one roof.
The Congenital Heart Surgery Unit (CHSU) accommodates
around 400 children annually who undergo heart operations
performed by Dr. Eric Mendeloff. 30% of our cases are
neonates and 58% are under the age of 2 years. Cases range
in complexity from palliation of hypoplastic left heart syndrome
to closure of atrial and ventricular septal defects. Highly
specialized care in the CHSU is provided by subspecialitytrained physicians and an excellent group of long term nurses
and respiratory therapists. This focus on pediatric cardiac
critical care has resulted in superlative patient outcomes that
exceed national norms. The heart program’s success has
attracted referrals from across the country. With the addition of
a second Congenital Heart Surgeon to our already robust
program, we anticipate growth that will require a sixth member
for our CICU team in addition to our need for a Medical
Director of the Unit. Preferred candidate for the director level
position will possess leadership attributes with evidenced
experience, along with a strong clinical skill set.
All candidates are preferred to be BC/BE in Pediatric
Cardiology and Pediatric Critical Care or boarded in one of
these with additional training in Pediatric Cardiac Critical Care.
Those with certification in one discipline and solid experience
in the alternate subspecialty should also apply. Positions are
employed and offer a competitive salary and excellent benefits
packet.
Our hospital has immense current capabilities and is
positioned to grow.
Kathy Kyer
National Director of Pediatric Subspecialty Recruitment
Kathleen.Kyer@HCAHealthcare.com
937.235.5890
RV diastolic dysfunction was present in 91.3% of Group A and 85% in
Group B. Specifically, Stage 3 diastolic dysfunction, which connotes
restrictive physiology, is present in 33% of the patients in Group A and
20% in Group B.
With regards to the distance travelled in 6 Minute Walk Test, Group A
has a longer distance travelled at a mean of 297 + 71.3m as compared
to Group B, at 215.3 + 69.2m.
Table 3 shows the functional classification of the patients who underwent
Tetralogy of Fallot correction. Most patients in Group A (96.7%) are in
functional Class II, while there was only 1 (4.3%) who was in functional
Class III. This patient had a prolonged hospital stay due to chylothorax
and right ventricle failure. This patient was subsequently diagnosed with
Absent Left-Pulmonary Artery on hemodynamic studies that were done
postoperatively. In Group B, 97.5% were in functional Class II while one
patient was in functional Class III. This patient had previous BlalockTaussig Shunt (BTS) surgery, which was patent, but was not able to be
taken down intraoperatively due to technical difficulties. This patient
subsequently had a reoperation after 8 months, and was subsequently
discharged; however, the patient apparently died after 4 months.
All the results that were gathered did not yield any statistical significance.
Discussion
Surgical repair by means of Ventricular Septal Defect (VSD) closure and
relief of right ventricular outflow obstruction is the definitive management
for Tetralogy of Fallot. Over the years, there has been consistent
progress in refining the surgical techniques in improving anesthetic and
critical care management to achieve this goal. This evolution has
provided better postoperative outcomes and has led to improvement in
the quality of life of repaired TOF patients as they reach adulthood.
Postoperative complications of pulmonary incompetence and right
ventricular dysfunction can be attributed to many factors, among which,
the surgical technique used to relieve right ventricular outflow tract
dysfunction has been implied as one of the many causes.
In our study, pulmonary incompetence was already seen among patients
in both groups, with the transannular group having a greater incidence at
30.4%, as compared to the pulmonary valve-sparing group at 27.5%.
Both groups had mild severity. Not long ago, pulmonary incompetence
was regarded as an inevitable, but unimportant late sequelae of repair.
Much emphasis was placed on the need for complete relief of
obstruction, often at the expense of a freely regurgitant and ever-dilating
outflow tract.3 These misguided assertions of investigators can be
understood when the time course of the effects of postoperative
pulmonary incompetence is considered. Problems from pulmonary
incompetence however occur decades after repair,3 and is due to
progressive RV dilatation and pressure overload.
Both groups had residual pulmonary stenosis. All patients in the
transannular group had mild severity. In the pulmonary valve sparing
group, 50% had mild, 7.5% had moderate, and 2.5% had severe
severity. In the past 20 years, a shift from the need for complete relief of
obstruction15 towards a policy to preserve the pulmonary valve, even at
the expense of a modest residual stenosis, has occurred.16 This shift
might keep adverse late effects of pulmonary incompetence to a
minimum, and retain the integrity of the outflow tract, avoiding late
aneurysmal dilation.3
Findings of both diastolic and systolic RV dysfunction were noted at the
early post-operative period, of which, there were more patients in the
transannular patching group who had diastolic dysfunction (91.3%),
compared to the valve-sparing group (85%). In the study of Cardoso and
Miyague,11 RV restrictive physiology, which connotes diastolic
dysfunction, was seen in 63.3% of their patients who underwent
Tetralogy of Fallot correction. In their particular study, most of their
subjects underwent transannular patching. Authors of previous
studies17,18,19 have found a correlation between this technique
(transannular patching) and the appearance of anterograde diastolic flow
in the pulmonary artery, which is seen in 2D echocardiography of
patients with restrictive physiology. Restrictive right ventricular
physiology can occur both early and late after repair. Norgard et al.
found in their study that the anatomical substrate requiring a
transannular patch repair is the most important determinant for early
restriction, and mid-term restriction is most likely to occur if early
restriction is present.17 Restrictive physiology may relate to a process of
endomyocardial fibrosis intrinsic to the disease itself, and intensify as
time goes by;20 to the ventriculotomy; and to the interposition of patches
in the interventricular septum and in the infundibulum.17 It also seems to
be influenced by immaturity of the right ventricle, which adapts to the
aggressions of extracorporeal circulation, cardioplegia, and hypothermia.21
In the study done by Cardoso and Miyague,11 they have concluded that
early postoperative restrictive right ventricular physiology (diastolic
dysfunction) may be a transient phenomenon of incomplete adaptation
of that ventricle to volume and pressure modifications.
RV systolic dysfunction was more common in the pulmonary valvesparing group at 52.5% compared to the transannular group at 43.5%.
These findings were contrary to the findings of Nair et al, wherein, RV
dysfunction was more common in patients who needed a transannular
patch. They also found that this remarkable decrease in systolic wall
motion velocity occurred despite the presence of volume overload in all
of their patients, because of the concomitant pulmonary regurgitation.22
This difference may be explained by the timing of follow-up. Findings in
our study were during the early post-operative period as compared to
the study of Nair et al, wherein, their findings were noted at least 10
years pos-op.
Almost all patients in both groups belong to functional Class II. This
finding is expected to improve after full recovery from surgery. There was
only one patient from both groups who was in functional Class III. This
patient from the transannular group had systolic and diastolic RV
dysfunction postoperatively, and suffered from RV failure. He needed
prolonged inotropic support and several failure medications to relieve his
symptoms. Subsequent cardiac catheterization data revealed that an
absent left pulmonary artery was the etiology of the patient’s RV failure.
In the pulmonary valve sparing group, the patient who was in functional
Class III was already 12-years-old, and had undergone previous
palliative surgery. Technical difficulties were encountered during her
surgery, and the patent shunt from the previous palliative surgery was
not removed. Postoperatively, she had RV systolic dysfunction, and was
noted to have a significant VSD leak causing volume overload and
pulmonary congestion.
Results of the Six-Minute Walk Test for both groups were sub-optimal at
a mean of 297 + 71.3m for Group A, and 215.3 + 69.2m for Group B as
compared to the normal value by age which is 470 + 57m.23. Like
functional class, these results are expected to improve after full recovery
from surgery.
The results of this study did not show statistical difference
between the two groups as compared to previously published
studies, but it has confirmed the presence of RV dysfunction in the
early postoperative period. The implications of these findings
suggest a well-catalogued and continuous follow-up of repaired
TOF patients. As shown in the study by Remotigue et al., both RV
systolic and diastolic dysfunction were present among repaired
TOF patients after one to two years of follow-up, and transannular
patching technique was associated with the occurrence of
restrictive physiology. These findings show that complications at
the early postoperative period, although they may be a transient
phenomenon, may still persist during the midterm follow-up.
Limitations of the Study
Most subjects of this study were preoperatively risk-stratified as low risk.
There were only 13 patients who had additional risk factors for surgery.
CONGENITAL CARDIOLOGY TODAY t www.CongenitalCardiologyToday.com t February 2016
8
Ten of which were adolescents, and 4 of which underwent previous
palliative surgery.
This variable may have affected the findings of this study, since the
results may not be a true reflection of the TOF patients undergoing
TOF correction.
Conclusion
Both RV systolic and diastolic dysfunction were present in both groups in
the early postoperative period. Diastolic dysfunction was more common
among patients who had transannular patching, while systolic dysfunction
was more common among patients who had pulmonary valve sparing.
Our study showed that the surgical technique used to relieve the
right ventricular outflow obstruction, is not, by itself, associated with
the development of right ventricular dysfunction.
Pulmonary incompetence was a more common finding among patients
who underwent transannular patching.
Most patients in both groups were in functional Class II, and had suboptimal distance travelled in Six-Minute Walk Test.
Recommendations
1.
2.
3.
Vigilant monitoring of those patients diagnosed to have right
ventricular dysfunction in order to address its impact on the
patient’s recovery.
Post-op Tetralogy of Fallot patients must continuously be
followed-up to check for the persistence of RV dysfunction and
the evolution of pulmonary incompetence.
A prospective study that would equally include TOF patients with
pre-operative moderate and high-risk stratification per group,
should be done in order to evaluate the true incidence of right
ventricular dysfunction among post-op Tetralogy of Fallot patients.
Appendix A
Modified Ross Heart Failure Classification for Children
Class I Asymptomatic
Class II Mild tachypnea or diaphoresis with
feeding in infants.
Dyspnea on exertion in older children.
Class III Marked tachypnea or diaphoresis
with feeding in infants.
Marked dyspnea on exertion.
Prolonged feeding times with
growth failure.
Class IV Symptoms such as: tachypnea,
retractions, grunting, or diaphoresis at rest.
References
1.
Ho K., Tan R., Wong K., Tan T., Shankar S. Late Complications
Following Tetralogy of Fallot Repair: The Need for Long-term
Cardiology
C2016
II
CHILDREN'S HOSPITAL
OPPORTUNITY IN
PEDIATRIC CARDIOLOGY - MRI
CORPUS CHRISTI, TEXAS
Driscoll Children’s Hospital is advancing a comprehensive
Heart Center to meet the healthcare needs of congenital
heart patients in South Texas. The Heart Center is
seeking a Pediatric Cardiologist with 6-12 months of
additional training in MRI congenital heart imaging. Subspecialty board eligible or board certification is required.
Driscoll Children’s Cardiac MRI program has completed
nearly 200 pediatric/congenital heart scans on a new 1.5
Tesla Phillips Magnet over the last 19 months. Scans are
supported by pediatric anesthesia. The successful candidate
will spend about 30% of his/her time in direct patient care.
Pediatric Cardiology has been an integral part of Driscoll
Children’s Hospital since 1962. The Hospital and the Heart
Center are committed to bringing state-of-the-art technology
and quality service to 31 counties in South Texas. The Heart
Center incorporates all cardiology subspecialties including
fetal, interventional catherization and surgical support.
Driscoll Children’s Hospital is associated with three pediatric
cardio-thoracic surgeons who deliver all aspects of surgical
service including hybrid procedures.
Corpus Christi and the Rio Grande Valley offer a relaxed
“island style” setting with miles of Gulf beaches and mild
weather perfect for outdoor activities. South Texas offers
world class hunting, fishing, sailing and wind surfing. Golf,
cycling and tennis are enjoyed year round. The cost of living
in south Texas is low, and there is no state income tax.
If you are interested in more information on this
excellent opportunity, please contact:
John Brownlee, MD
Cardiology Medical Director
John.Brownlee@dchstx.org
or
Annette Shook
Physician Recruiter
Driscoll Children’s Hospital
Annette.Shook@dchstx.org
19th Annual Update on Pediatric and Congenital Cardiovascular Disease
Feb. 24- 28, 2016
Loews Royal Pacific Resort at Universal Orlando®
6300 Hollywood Way, Orlando, FL 32819
www.chop.edu/events/cardiology-2016#.VnMHWzYR6yI
CONGENITAL CARDIOLOGY TODAY t www.CongenitalCardiologyToday.com t February 2016
9
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
Follow-up. Ann Acad Med Singapore
2007;36:947-53.
Bertranao EG, Blackstone EH, Hazelrig
JB, Turner ME, Kirklin JW. Life
expectancy without surgery in tetralogy of
Fallot. Am J Cardiol 1978;42:458-66.
Apitz C, Webb Gary, Redington A.
Tetralogy of Fallot. Lancet 2009; 374:
1462-71.
Lillehei CW, Coehn M, Warden HE, Red
RC, Aust JB, De Wall RA, Varco RL.
Direct vision intracardiac surgical
correction of the Tetralogy of Fallot,
Pentalogy of Fallot and pulmonary atresia
defects. Report of first 10 cases. Ann Surg
1955;142:418.
Kirklin JW, Du Share JW, Patrick RT,
Donald DE, Hetze PS, Harsh- barger HG,
Wood EH. Intracardiac surgery with the
aid of a mechan- ical pump-oxygenator
system (Gibbon type). Report of eight
cases. Mayo Clin Proc 1955;30:201.
Shumway NE. Total surgical correction of
tetralogy of Fallot. Arizona Med 1966;Feb:
106.
Hudspeth AS, Cordall AR, Johnston FR.
Transatrial approach to total correction of
Te t r a l o g y o f F a l l o t . C i r c u l a t i o n
1963;27:796–800.
Karl TR, Sano S, Pornviliwan S, Mee R.
Tetralogy of Fallot: favor- able outcome of
nonneanatal transatrial transpulmonary
repair. Ann Thorac Surg 1992;54:903–
907.
Bote-Nunez JR, Cantre T, Casas ML.
Long-term results after Total Repair of
Tetralogy of Fallot. PHC.R.053.01.
Murphy J., Gersh B., Mair D., Fuster V.,
McGoon M., Ilstrup D., McGoon D., Kirklin
J., Danielson G. Long-term outcome in
patients undergoing surgical repair of
Tetralogy of Fallot. N Engl J Med
993;329:593-9.
Cardoso SM, Miyague NI. Right
Ventricular Diastolic Dysfunction in
Postoperative Period of Tetralogy of Fallot.
Arq Bras Cardiol, volume 80 (no 2),
198-201, 2003.
Gatzoulius MA, Norgard G, Josen M,
Cullen S, Redington AN. Does Restrictive
right ventricular physiology in the early
postoperative period predict subsequent
right ventricular restriction after repair of
tetralogy of Fallot. Heart 1998;79:481-484.
Carvalho JS, Shinebourne EA, Busst C,
Rigby ML, Redington AN. Exercise
capacity after complete repair of tetralogy
of Fallot: deleterious effects of residual
CHI-‘ NETWORK
CONGENITAL HEART AND PEDIATRIC CARDIAC
PROFESSIONALS NETWORK
JOIN TODAY
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
pulmonary regurgitation. Br Heart J
1992;67:470-3.
Rathore KS., Agrawal SK., Kapoor A.
Restrictive Physiology in Tetralogy of
Fallot: Exercise and Arrhythmogenesis.
Asian Cardivascular & Thoracic Annals
2006, Vol. 14, No. 4.
Kirklin JW, Blackstone EH, Pacifico AD,
Kirklin JK, Bargeron LM Jr. Risk factors for
early and late failure after repair of
tetralogy of Fallot, and their neutralization.
Thorac Cardiovasc Surg 1984; 32: 208–
14.
Van Arsdell G, Yun TJ. An apology for
primary repair of tetralogy of Fallot. Semin
Thorac Cardiovasc Surg Pediatr Card
Surg Annu 2005: 128–31.
Norgård G, Gatzoulis MA, Moraes F,
Lincoln C, Shore DF, Shinebourne EA,
Redington AN. Relationship between type
of outflow tract repair and postoperative
right ventricular diastolic physiology in
tetralogy of Fallot: implication for long-term
outcome. Circulation 1996; 94: 3276-80.
Singh RS, Kalra R, Kumar RM, Rawal N,
Singh H, Das R. Assessment of right
ventricular function in post operative
patients of tetralogy of fallot and its
predictive factors. World Journal of
Cardiovascular Surgery, 014,4, 139-150.
Eroglu AG, Saraglu A, Saraglu T. Right
ventricular diastolic function after repair
of tetralogy of Fallot: Relationship to the
insertion of a “transanular” patch. Cardiol
Young 1999; 9: 384-91.
Hegarty A, Anderson RH, Deanfild JE.
Myocardial fibrosis in tetralogy of Fallot:
effect of surgery or part of natural
history? Br Heart J 1996; 59: 123.
Munkhammar P, Cullen S, Jogi P, de
Leval M, Elliot M, Norgard G. Early age
at repair prevents restrictive right
ventricular physiology after surgery for
tetralogy of fallot. J Am Coll Cardiol 1998;
32: 1083-7.
Nair KK, Ganapathi S, Sasidharan B,
Thajudeen A, Pillai HS, Tharakan J et al,.
Asymptomatic right ventricular
dysfunction in surgically repaired adult
tetralogy of fallot patients. Annals of
Pediatric Cardiology 2013 Vol 6 Issue 1.
Lammers AE, Hislop AA, Flynn Y,
Haworth S. The six-minute walk test:
Normal values for children of 4 -11 years
of age. Arch. Dis. Child. published online
3 Aug 2007.
Remotigue F. The Association of
P o s t o p e r a t i v e R i g h t Ve n t r i c u l a r
Restrictive Physiology with Right
Ventricular Systolic Dysfunction among
Pediatric Patients with Tetralogy of Fallot.
CCT
Corresponding Author
Lorielyn G. Mandigma, MD
Clinical Research Fellow
Section of Non-invasive Pediatric Cardiology
Philippine Heart Center
East Avenue
Quezon City, Philippines, 0850
Tel: +63 02 9252450
Fax: +63 02 9220551
ryliemd@yahoo.com
Ma. Bernadette A. Azcueta, MD
(Co-investigator)
Section Head
Pediatric Surgical Intensive Care Unit
Philippine Heart Center
Pediatric Cardiology
East Avenue
Quezon City, Philippines
docbernee@yahoo.com
25.
Corazon A. Estevanez, MD
Consultant, Non-invasive Pediatric
Cardiology
Philippine Heart Center
East Avenue
Quezon City, Philippines, 0850
Mercilyn C. Yap, MD
Pediatric Cardiologist
Philippine Heart Center
East Avenue
Quezon City, Philippines, 0850
mayap19@yahoo.com
The congenital heart professionals network exists to facilitate communications
between congenital heart professionals locally, regionally, and globally.
w w w. c h i p n e t w o r k . o r g
13
‘[
Cf:1L‘im1L1li
Ch|Id|'EIpfq
Funded by Cinclnnati Chi|dren'5 Hear! lnsliima
Ih;-.n1 J||\l(lulc
CONGENITAL CARDIOLOGY TODAY t www.CongenitalCardiologyToday.com t February 2016
10
Why the CHAMP App?
“ We had to come up with a
better solution that would
allow these infants to go
home safely between
surgeries, without placing an
enormous burden on parents
and caregivers.”
—Girish S. Shirali, MBBS,
FACC, FASE, Co-Director, the
Ward Family Heart Center
BEST
CHILDREN'S
HOSPITALS
CARDIOLOGY &
HEART SURGERY
,3
CONSTANT MONITORING. IMMEDIATE
INTERVENTION. THE COMFORT OF HOME.
Knowing children born with single-ventricle heart defects are markedly high-risk
patients, the heart team at Children’s Mercy worked to create a system that would
help parents with critical home monitoring. That resolve led to the ground-breaking
development of the Cardiac High Acuity Monitoring Program, better known as CHAMP.
This includes an interdisciplinary team available 24 hours a day, seven days a week for
the patient’s parents, as well as a one-of-a-kind home monitoring tablet app.
The CHAMP App was developed to allow real-time home monitoring of pediatric
cardiac patients for immediate response and intervention. From weight to oxygen
saturation, CHAMP gathers critical patient information and sends it directly to the
CHAMP team. This constant, consistent monitoring has already yielded results: since
its implementation at Children’s Mercy in April 2014 there has not been a single death
in this delicate population. Now this technology is being shared with other pediatric
hospitals across the country.
Advancing pediatric cardiology in real time. It’s not just an outcome we pursue
—it’s a transformation we lead.
.
Ward Family Heart Center
CHILDREN'S MERCY KANSAS CITY
Find out more about CHAMP at ChildrensMercy.org/CHAMP.
Tools to Stay Organized: Using Software to Enhance
Efficiency
By Animesh (Aashoo) Tandon, MD, MS
license. In addition, many manufacturers and academic libraries provide
online or in-person training for these programs, which could increase the
efficiency of use.
Keywords: Software, Mobile, Technology
Introduction
The digital age has brought significant changes to physicians’ lives, both
personally and professionally. The ways we interact with patients and
make clinical decisions have been strongly influenced by the vastly
increased amount and availability of information. Many physicians carry
a powerful computer in their hands in the form of a smartphone, which
allows nearly instant access to medical journals, textbooks, and
guidelines.1, 2 The ubiquity of social media has also required adaptations
of the way that physicians and patients interact.3 Smartphones are also
showing utility in replacing the pager as the preferred method of
communication in healthcare settings.4, 5
In addition to influencing patient care and communication, technology
can also be beneficial in staying organized and efficient; software tools
that can be used across devices and platforms are one such example. A
great time to experiment with these tools is during fellowship training, so
that each individual can find the combination of tools best suited for her
or his needs early on. The goal of this article is to outline three
categories of software programs that, individually and especially in
combination, can yield significant time savings for early career
physicians. These programs can especially be beneficial for clinicianscientists involved in research endeavors.
Reference Management Programs: Which Paper Had That Thing I
Read That One Time?
One key method of staying organized during research projects is the use
of a reference management program. Learning to use a reference
management program can increase the speed of all aspects of a
research project, including reviewing existing literature, composing
institutional review board documents, and drafting and revising abstracts
and manuscripts.6 Some commonly-used reference management
programs include: EndNote (Thomson Reuters, Philadelphia, PA, USA),
Mendeley (Elsevier Inc., New York, NY, USA), Zotero (Roy Rosenzweig
Center for History and New Media, Fairfax, VA, USA), and RefWorks
(Proquest LLC, Ann Arbor, MI, USA). Most of these programs are
available for free for end-users, either because they are open source, or
because many universities and medical schools have an institutional
Key skills to acquire for the use of reference managers include:
searching for references; importing references into the database;
tagging references for future ease of use; searching for references in
your database, especially searches based on keywords; and adding
citations to your document (IRB/abstract/manuscript). Each of the
above-mentioned reference management programs have their strengths
and weaknesses;7 choosing the program that will work best depends
heavily on your preferences. Specifically, three areas in which the
programs function differently include:
1. The workflow for importing documents into the database;
2. Methods available to query the reference database;
3. And whether the reference library is available and shareable
online and on mobile devices.
Many comparisons of these software offerings exist, both in publications,
7, 8 and on the internet.
Developing an efficient method of importing references into a reference
manager program will also help address what to do with all the papers
that fellows and attending physicians tend to send out over email. Once
added to the reference manager software, the papers will always be
easily accessible and searchable.
One of the prime uses of a reference management program is inserting
citations into text. Most of the reference manager programs have the
capability to insert citations into word processing software (such as
Microsoft Word (Microsoft, Redmond, WA, USA)) using journal-specific
styles and with automatically updating numbering. In comparison to
manually entering and updating citations, use of a reference
management program saves significant amounts of time when
documents are written, revised in response to reviewers, and
resubmitted to another journal.
Project Management Programs: What Was It I Was Supposed To Be
Doing Today?
Project management programs can be useful in both the personal and
professional realms. They are designed to help keep the various stages
of a project organized, and can specifically assist in the process of
The 7th
hy:
Phoenix Fetal Cardiology Symposium
May 3 7, 2016
-
.i»--'-\
To register, visit www.fetalcardio.com
CONGENITAL CARDIOLOGY TODAY t www.CongenitalCardiologyToday.com t February 2016
12
planning the project, keeping track of progress,
and adapting to changes in the project. Two
examples of project management programs
include: Evernote (Evernote Corp., Redwood
City, CA, USA) and Trello (Trello, Inc., New
York, NY, USA).
Evernote functions at its most basic level by
making notes, which can contain text,
checklists, and images. However, advanced
versions of Evernote also have the ability to
add and annotate PDFs, create notes with
handwriting, store websites, and more (for a
fee). Trello is based more on a whiteboardstyle organization scheme, with boards
representing projects and cards representing
tasks for each project. This allows for granular
task assignment to projects, and a different
method of visualizing tasks for a given project.
Both programs are accessible on most
common devices (PCs, Macintosh, iOS,
Android, etc.) and have slightly different
interfaces depending on which device is being
used. In addition, both programs allow sharing
of tasks and notes to different users, allowing
easy collaboration on projects.
The key functionality for any project
management program is the near-real-time
syncing capabilities across many devices. This
way, portions of projects can be performed any
time, in any place (with an internet connection),
on any device. An inspiring idea about a new
research project that occurs at the grocery
store can be added to a note or card
immediately, then later fleshed out, organized
into a to-do list, and acted upon at a desk or
remotely. This can minimize duplication of
work, and help identify the next step of a
project. Both of these programs can also be
integrated into a digital calendar or have popup reminders; e.g. one can set a reminder for a
month after paper submission to check on its
progress, or remember the abstract deadline
for the American College of Cardiology
Conference. So far, the use of these programs
in the medical setting has not been wellstudied, though some examples exist.9 There
are numerous online tutorials for these
programs, including some designed specifically
for physicians.
Online File Storage: Did I Update the Right
Version of That Draft?
Online file storage (otherwise known as “cloud
storage”) is a method of storing files that frees
the user from a specific computer or device.
Online file storage programs usually have an
automatic sync feature that continually updates
files. So, if a document (e.g. manuscript draft)
is edited on a work computer, and saved to the
synced folder, the changes will then be
reflected on the version of the file stored in the
cloud, and then pushed to all other connected
devices (e.g. smartphone, home computer).
This allows easier transition of work from one
computer to the next, allowing greater
efficiency and a lower likelihood of editing the
wrong version of a document. In addition,
online storage platforms can be used to share
files between collaborators, even at different
sites. Online storage does have potential
limitations, though: not all systems are HIPAAcompliant, and not all are allowed by hospital/
medical school IT departments. In addition,
free accounts often have limited storage, and
as with all computer systems, files can be
accidentally deleted or damaged, so always
back up important files.
Quick Hits: Bonus Efficiency Tips
In addition to the examples mentioned above,
there are numerous other software tools
designed to improve efficiency that could be
useful for individual fellows and attending
physicians, fellowship programs, and
departments. For instance, some email
services allow “snoozing” of emails, which
then disappear until the snoozed time,
decluttering the inbox. Some services provide
shared calendars that any member can see
and add events to, such as on call schedules
and reminders for abstract and grant
deadlines. Another example is voice
recognition: some voice recognition programs
can be integrated into electronic medical
records, making writing clinic notes easier for
those used to dictation.
Discussion
The utility of the approaches described above
has not been studied in depth, but limited
evidence suggests that health care
professionals find using software tools useful.10
The key is to find the set of tools that works
best for any given individual for staying
o r g a n i z e d a n d w o r k i n g e f f i c i e n t l y.
Experimenting with these tools may take time
up front, but could pay dividends later on;
therefore, fellowship is an ideal time to develop
a personal toolbox. As with any technology,
development of new software tools might
require a reevaluation of current preferences,
but the potential benefit of that innovation is
even more productivity.
Acknowledgement: The author would like to
thank Ritu Sachdeva, MBBS, MD, for her
insights on this manuscript.
Author Contributions: AT conceived of and
wrote the entire article.
References
1.
Ventola CL. Mobile devices and apps for
health care professionals: uses and
benefits. P T. 2014;39(5):356-64.
2. Seabrook HJ, Stromer JN, Shevkenek C,
Bharwani A, de Grood J, Ghali WA.
Medical applications: a database and
characterization of apps in Apple iOS and
Android platforms. BMC Res Notes.
2014;7:573.
3. Snipelisky D. Social media in medicine: a
podium without boundaries. J Am Coll
Cardiol. 2015;65(22):2459-61.
4. Ortega GR, Taksali S, Smart R,
Baumgaertner MR. Direct cellular vs.
indirect pager communication during
orthopaedic surgical procedures: a
prospective study. Technol Health Care.
2009;17(2):149-57.
5. Frizzell JD, Ahmed B. Text messaging
versus paging: new technology for the
next generation. J Am Coll Cardiol.
2014;64(24):2703-5.
6. Mahajan AK, Hogarth DK. Taking control
of your digital library: how modern citation
managers do more than just referencing.
Chest. 2013;144(6):1930-3.
7. Zhang Y. Comparison of select reference
management tools. Med Ref Serv Q.
2012;31(1):45-60.
8. Lorenzetti DL, Ghali WA. Reference
management software for systematic
reviews and meta-analyses: an
exploration of usage and usability. BMC
Med Res Methodol. 2013;13:141.
9. Sampognaro PJ, Mitchell SL, Weeks SR,
Khalifian S, Markman TM, Uebel LW, et al.
Medical student appraisal: electronic
resources for inpatient pre-rounding. Appl
Clin Inform. 2013;4(3):403-18.
10. Amgad M, AlFaar AS. Integrating web 2.0
in clinical research education in a
developing country. J Cancer Educ.
2014;29(3):536-40.
CCT
Conflict of Interest Statement: The author
has no conflicts of interest.
Funding: There was no funding for this article.
Biographical Sketch
Animesh (Aashoo) Tandon, MD, MS, FAAP,
FACC, is a junior faculty member at UT
Southwestern/Children’s Medical Center
Dallas who specializes in cardiac imaging. His
research interests include translational
applications of cardiac MRI and big data in
pediatric cardiac patients. He is also interested
in fellow education, and the use of technology
in clinical practice.
Animesh (Aashoo) Tandon, MD, MS
University of Texas Southwestern
Medical Center, Dallas, Texas, and
Children’s Medical Center Dallas,
Dallas, Texas
1935 Medical District Dr.
Dallas, TX 75235 USA
Tel: 214.456.8761
animesh.tandon@utsouthwestern.edu
CONGENITAL CARDIOLOGY TODAY t www.CongenitalCardiologyToday.com t February 2016
13
Compiled and Reviewed by Tony Carlson, Senior Editor
Personalized Heart Models for Surgical Planning - System Converts
MRI Scans into 3-D-Printed, Physical Models in a Few Hours
Researchers at MIT and Boston Children's Hospital have developed a
system that can take MRI scans of a patient's heart and, in a matter of
hours, convert them into a tangible, physical model that surgeons can
use to plan surgery.
The models could provide a more intuitive way for surgeons to assess
and prepare for the anatomical idiosyncrasies of individual patients.
"Our collaborators are convinced that this will make a difference," says
Polina Golland, a professor of Electrical Engineering and Computer
Science at MIT, who led the project. "The phrase I heard is that
'surgeons see with their hands,' that the perception is in the touch."
This fall, seven cardiac surgeons at Boston Children's Hospital will
participate in a study intended to evaluate the models' usefulness.
Golland and her colleagues will describe their new system at the
International Conference on Medical Image Computing and
Computer Assisted Intervention in October. Danielle Pace, an MIT
graduate student in Electrical Engineering and Computer Science, is
first author on the paper and spearheaded the development of the
software that analyzes the MRI scans. Medhi Moghari, a physicist at
Boston Children's Hospital, developed new procedures that increase
the precision of MRI scans tenfold, and Andrew Powell, a cardiologist
at the hospital, leads the project's clinical work.
The work was funded by both Boston Children's Hospital and by
Harvard Catalyst, a consortium aimed at rapidly moving scientific
innovation into the clinic.
MRI data consist of a series of cross sections of a three-dimensional
object. Like a black-and-white photograph, each cross section has
regions of dark and light, and the boundaries between those regions
may indicate the edges of anatomical structures. Then again, they may
not.
Determining the boundaries between distinct objects in an image is
one of the central problems in computer vision, known as "image
segmentation." But general-purpose image-segmentation algorithms
aren't reliable enough to produce the very precise models that surgical
planning requires.
Typically, the way to make an image-segmentation algorithm more
precise is to augment it with a generic model of the object to be
segmented. Human hearts, for instance, have chambers and blood
vessels that are usually in roughly the same places relative to each
other. That anatomical consistency could give a segmentation
algorithm a way to weed out improbable conclusions about object
boundaries.
#22‘
Medical News, Products &
Information
E
Canolinas HealthCare System
Interventional Pediatric Cardiologist
Levine Children’s Hospital
Sanger Heart & Vascular Institute
Charlotte, NC
The Congenital Heart Center at Levine Children’s Hospital (LCH)
and Sanger Heart & Vascular Institute (SHVI), seeks to add an
additional Pediatric Interventional Cardiologist to join their existing
faculty. Responsibilities for this position will include diagnostic and
interventional catheterization, as well as general cardiology outpatient
and inpatient care with shared night / weekend call.
• Candidates will have completed an ACGME accredited fellowship
in pediatric cardiology and be BC/BE by the American Board of
Pediatrics. A fourth year of additional training in interventional
cardiac catheterization is required.
• A Minimum of 5 years of independent experience is preferred.
The Congenital Heart Center, established in 2010, has been
ranked as one of the top-50 pediatric heart centers in the country by
U.S. News and World Report for the last two years. Our
comprehensive services include cardiac imaging, electrophysiology,
dedicated cardiovascular intensive care staff, and regional referral
programs in heart failure / transplantation, adult congenital heart
disease, and fetal echocardiography. Surgical and cardiac
catheterization volume has been growing at a rate of 15% per year
over the last five years. Because of our continued growth, a new state
of the art two lab cardiac catheterization and electrophysiology suite is
under construction, with a plan to open in the fall of 2016. The cardiac
catheterization program is active in industry sponsored clinical
research.
LCH and SHVI are both premier referral facilities within the Carolinas
HealthCare System (CHS), one of the nation’s leading and most
innovative healthcare systems. CHS operates nearly 2,500 systememployed physicians, more than 60,000 employees and more than
7,460 licensed beds across the Carolinas.
Levine Children’s Hospital (LCH), a state-of-the-art, 234 bed facility
is the largest and most comprehensive children’s hospital between
Washington, DC and Atlanta, GA. LCH has a robust inpatient service
with a 20-bed PICU/CVICU, 85-bed NICU, and an inpatient
rehabilitation facility.
Sanger Heart & Vascular Institute (SHVI) is one of the largest
cardiac and vascular programs in the Southeast, with more than 50
years of experience in providing world-class, comprehensive acute
and chronic cardiovascular services, including the region’s only heart
transplant center and pediatric heart surgery program.
.
To learn more or to submit your CV please contact:
Janisyn McLaurin, CHS Physician Recruiter at
Janisyn.mclaurin@carolinashealthacare.org
The problem with that approach is that many of the cardiac
patients at Boston Children's Hospital require surgery precisely
because the anatomy of their hearts is irregular. Inferences from a
generic model could obscure the very features that matter most to
the surgeon.
"They want to bring the kids in for scanning and spend probably a day or
two doing planning of how exactly they're going to operate," Golland says.
"If it takes another day just to process the images, it becomes unwieldy."
In the past, researchers have produced printable models of the heart
by manually indicating boundaries in MRI scans. But with the 200 or so
cross sections in one of Moghari's high-precision scans, that process
can take eight to 10 hours.
Pace and Golland's solution was to ask a human expert to identify
boundaries in a few of the cross sections and allow algorithms to take over
from there. Their strongest results came when they asked the expert to
segment only a small patch --one-ninth of the total area -- of each cross
section.
CONGENITAL CARDIOLOGY TODAY t www.CongenitalCardiologyToday.com t February 2016
14
Congenital and Paediatric Echocardiography:
From Basics to Advanced
Thursday, April 28 to Saturday, April 30, 2016
The Hospital for Sick Children (SickKids)
Daniels Hollywood Theatre, 1st Floor, Burton Wing
555 University Avenue, Toronto, Ontario M5G 1X8
Course Objectives
This course offers a unique introduction into
Paediatric Echocardiography and imaging of
Congenital Heart Disease. The main goal is
to improve the knowledge of physicians and
sonographers who perform and/or interpret
echocardiograms in newborn and paediatric patient
populations or perform echocardiographic studies
in adults with repaired congenital heart disease.
Specific course objectives are:
1. Introduce the specific technical aspects of
paediatric and congenital echocardiography:
image acquisition and representation.
2. Introduction to cardiac morphology and
how it relates to echocardiographic imaging.
3. Overview of pre—operative and post—operative
imaging of the most common congenital defects.
4. Echocardiographic assessment of more
complex congenital defects.
5. Introduction to assessment of systolic and diastolic
function in children with a special focus on novel
techniques for evaluating LV and RV function.
Currently, the algorithm examines patches of unsegmented cross
sections and looks for similar features in the nearest segmented cross
sections. But Golland believes that its performance might be improved
if it also examined patches that ran obliquely across several cross
sections. This and other variations on the algorithm are the subject of
ongoing research.
The clinical study in the fall will involve MRIs from 10 patients who
have already received treatment at Boston Children's Hospital. Each of
seven surgeons will be given data on all 10 patients -- some, probably,
more than once. That data will include the raw MRI scans and, on a
randomized basis, either a physical model or a computerized 3-D
model, based, again at random, on either human segmentations or
algorithmic segmentations.
Using that data, the surgeons will draw up surgical plans, which will be
compared with documentation of the interventions that were performed
on each of the patients. The hope is that the study will shed light on
whether 3-D-printed physical models can actually improve surgical
outcomes.
Guy Cloutier, also of the University of Montreal Hospital Research
Centre, holds the promise of not only effectively identifying leaks, but
also evaluating how the aneurysm is healing. And finally, the last word
in endovascular repair is the bioactive stent and injection of a gel
around the implant to prevent or stop leaks. These new biomaterials
are being developed in collaboration with Soulez and Cloutier’s
colleague Sophie Lerouge.
Source: University of Montreal Hospital Research Centre (CRCHUM)
@CRCHUMDr. Gilles Soulez is a radiologist with the University of
Montreal Hospital (CHUM), a researcher at the University of Montreal
Hospital Research Centre (CRCHUM), and a professor with the
university’s departments of Radiology, Radiation Oncology, and
Nuclear Medicine. The University of Montreal is officially known as
Université de Montréal.
CONGENITAL CARDIOLOGY TODAY
Physicians . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .$495
Fellows/Sonographers/Trainees . . . . . . . . . . . . . . . . . . . . . . . . . . . . .$375
© 2016 by Congenital Cardiology Today (ISSN 1554-7787-print; ISSN
1554-0499-online). Published monthly. All rights reserved.
www.CongenitalCardiologyToday.com
Registration
8100 Leaward Way, PO Box 444, Manzanita, OR 97130 USA
Tel: +1.301.279.2005; Fax: +1.240.465.0692
Early Bird Registration (Before March 1, 2016)
Physicians . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .$595
Fellows/Sonographers/Trainees . . . . . . . . . . . . . . . . . . . . . . . . . . . .$45O
Registration Fee Includes
--
Attendance to all lectures
Access to online course syllabus
Continental breakfast, lunch and refreshments
Accreditation
CME eligible
www.cvent.com/d/zfqjx4
"I think that if somebody told me that I could segment the whole heart
from eight slices out of 200, I would not have believed them," Golland
says. "It was a surprise to us."
Together, human segmentation of sample patches and the algorithmic
generation of a digital, 3-D heart model takes about an hour. The 3-Dprinting process takes a couple of hours more.
Publishing Management:
• Tony Carlson, Founder, President & Sr. Editor - TCarlsonmd@gmail.com
• Richard Koulbanis, Group Publisher & Editor-in-Chief RichardK@CCT.bz
• John W. Moore, MD, MPH, Group Medical Editor JMoore@RCHSD.org
• Allan Berthe, Contributing Editor-Special Projects
Editorial Board: Teiji Akagi, MD; Zohair Al Halees, MD; Mazeni Alwi, MD;
Felix Berger, MD; Fadi Bitar, MD; Jacek Bialkowski, MD; Mario Carminati,
MD; Anthony C. Chang, MD, MBA; John P. Cheatham, MD; Bharat Dalvi,
MD, MBBS, DM; Horacio Faella, MD; Yun-Ching Fu, MD; Felipe Heusser,
MD; Ziyad M. Hijazi, MD, MPH; Ralf Holzer, MD; Marshall Jacobs, MD; R.
Krishna Kumar, MD, DM, MBBS; John Lamberti, MD; Gerald Ross Marx,
MD; Tarek S. Momenah, MBBS, DCH; Toshio Nakanishi, MD, PhD; Carlos A.
C. Pedra, MD; Daniel Penny, MD, PhD; James C. Perry, MD; P.
Syamasundar Rao, MD; Shakeel A. Qureshi, MD; Andrew Redington, MD;
Carlos E. Ruiz, MD, PhD; Girish S. Shirali, MD; Horst Sievert, MD; Hideshi
Tomita, MD; Gil Wernovsky, MD; Zhuoming Xu, MD, PhD; William C. L. Yip,
MD; Carlos Zabal, MD
Free Subscription to Qualified Professionals: Send your name, title(s),
hospital or practice name, work address, phone and email to: sub@cct.bz.
Statements or opinions expressed in Congenital Cardiology Today reflect the
views of the authors and sponsors, and are not necessarily the views of
Congenital Cardiology Today.
CONGENITAL CARDIOLOGY TODAY t www.CongenitalCardiologyToday.com t February 2016
15
When Precise Sizing
is the Heart of the Matter
Tysha k N UCLEUSTMPTV Catheters
PTS-Xmsizing Balloon Catheters
Rx only
CV90l8
@2015
6/15
B. Braun Interventional Systems Inc.
Tyshak NuCLEUS’“ and PTS—X"" are registered trademarks of NuMED, Inc.
The Tyshak NuCLEUS'"' PTV Balloon Dilatation Catheters are recommen
A patient with isolated pulmonary stenosis. A patient with valvular pulm
The PTS—X"" Sizing Balloon Catheters are recommended for use in tho
select the appropriately sized occluder device. Refer to the lnstructi
Manufactured for:
B. Braun Interventional Systems Inc.
Bethlehem, PA 18018 I USA
Tel: 877—VENA CAV (836-2228) (USA) I Fax: 610-849-1334
824 Twelfth Avenue
www.bisusa.org
I
neous Transluminal Valvuloplasty (PTV) of the pulmonary valve in the following:
ith other minor congenital heart disease that does not require surgical intervention.
ardiovascular defects wherein accurate measurement of the defect is important to
elevant warnings, precautions, complications, and contraindications.
B I BRAUN
SHARING EXPERTISE
S""""‘
"N