Document 10446249
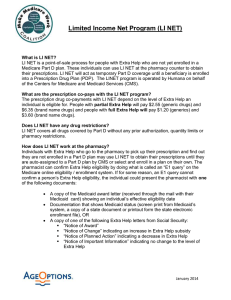
advertisement

MAX LIBRARIES - DEWEY Digitized by the Internet Archive in 2011 with funding from Boston Library Consortium IVIember Libraries http://www.archive.org/details/savingbabieseffiOOcurr Dewey HB31 .M415 '0 ^ , working paper department of economics SAVING BABIES: THE EFFICACY AND COST OF RECENT EXPANSIONS OF MEDICAID ELIGIBILITY FOR PREGNANT WOMEN Janet Currie Jonathan Gruber 94-11 Dec. 1993 massachusetts institute of technology 50 memorial drive Cambridge, mass. 02139 SAVING BABIES: THE EFFICACY AND COST OF RECENT EXPANSIONS OF MEDICAID ELIGIBILITY FOR PREGNANT WOMEN Janet Currie Jonathan Gruber 94-11 Dec. 1993 MTtUBRSBiES JUL 1 2 1994 RECEIVED Saving Babies: The Efficacy and Cost of Recent Expansions of Medicaid Eligibility for Pregnant Women Janet Currie UCLA and NfBER Jonathan Gruber MIT and NBER December, 1993 We Diamond, Sarah Feldman, Guido Imbens, Alan Knieger, Jim Poterba, Jon Stem, Duncan Thomas, Aaron Yeiowitz, and to seminar participants at Cornell, UVA, and the NBER for helpful discussions, to Sharieff Mansour and Nancy Cole for excellent research assistance, and to Marilyn Ellwood, Michael Fischer, Ian Hill, and Aaron Yeiowitz for providing information on Medicaid policies. Janet Currie gratefully acknowledges support from the National Science Foundation (SES-9 122640) and the Alfred P. Sloan Foundation. The views expressed are solely the authors' and should not be attributed to either organization. are grateful to Peter Skinner, Doug Staiger, Steve Abstract A key question for health care reform in the U.S. is whether expanded health insurance improvenwnts in health outconoes. We address this question in the context of dramatic expansions in the Medicaid eligibility for pregnant women that took place during the 1980s. We build a detailed simulation model of each state's Medicaid policy during the 1979-1990 period, and use this model to estimate 1) the effea of changes in the rules on the eligibility of pregnant women for Medicaid, and 2) the effect of Medicaid eligibility changes on birth outcomes in aggregate eligibility will lead to Viial Siaiisncs data. We eligibility have three main findings. First, the of pregnant women, but did so expansions did dramatically increase the Medicaid at quite differential rates expansions lowered the incidence of infant mortality and low birthweight; percentage point increase in infant mortality of in eligibility 7%. Third, among 15-44 year earlier, targeted old changes relaxations of the family structure requirements from the on birth levels. outcomes than broader expansions of eligibility We women was in Medicaid AFDC to all who became eligible we estimate that the 20 associated with a decrease eligibility, compared much lower takeup of Medicaid under the broader expansions. to conventional estimates We of the value of a life. making insurance policy effective. find that the life We insurance expansions can improve health, but that translating eligibility to coverage link in effects with somewhat higher income targeted expansions, which raised Medicaid expenditures by $1.7 million per infant fairly cost effective such as through program, had much larger women suggest that the source of this difference was the coverage by individuals Second, the across the states. saved, were conclude that may be the key Will the extension of health insurance to the uninsured improve their health? question underlying the current debate over health care reform. be a necessary precondition for improvements eligibility for may insurance insurance coverage. improvements It is This is a key Although insurance coverage may in the utilization of medical care, expansions in not translate into increased utilization of care, or even mto increases in possible that also increased utilization of care will not result in in health. This paper sheds light on these issues by investigating the relationship between the health of newborns and recent expansions of the insurance coverage provided Medicaid program. With 10 infant deaths per 1000 births, the to pregnant women U.S. infant mortality rate exceeds that of 20 other industrialized nations (U.S. House of Representatives, 1992). This high rate to reflect large numbers of unhealthy newborns. improves neonatal health, there is Hence, scope for a decrease under the to the extent that in this rate is thought adequate prenatal care through the promotion of prenatal care (Institute of Medicine, 1985). In an effort to increase die use of prenatal care, the past decade has seen a rapid expansion in the eligibility of pregnant women for Medicaid, a federal-state matching entitlement provides health insurance for the poor. receipt of cash welfare eligibility Medicaid had traditionally been eligibility to was extended to a very low income number of women in single additional groups of pregnant women This experience provides a case study of whether expanding health insurance actually improve infant health, or whether poor beyond the reach of government insurance during the eligibility can infant health in the U.S. simply reflects other factors policy. study the effert of this government intervention, changes occurred tied to the parent households. 1980s. To that payments under the Aid for Families with Dependent Children (AFDC) program. This generally limited However, Eligibility for program at different rates across the states in we exploit the faa that the eligibility order to identify their effects on birth outcomes, birth inputs, Medicaid coverage, and Medicaid expenditures. analysis is a detailed simulation model of each state's Medicaid eligibility rules for pregnant We over the 1979-90 period. in women apply this model to data from the Current Population Surveys (CPS) order to quantify the effects of changes We The baclcbone of our in the rules on eligibility and on actual Medicaid coverage. then use aggregate Vital Statistics data to examine the effea of the expansions on two widely used indicators of infant health: the incidence of low birthweight, and infant mortality. Using these estimates in conjunction with data on Medicaid expenditures from the Health Care Financing Administration (HCFA), we then examine the costliness of Medicaid expansions. information on the use of medical services by pregnant women from the fraction of increase of changes women major fmdings. 140%. This increase occurred a lower incidence of was stronger than the effect in Medicaid and a decrease on low birthweight. eligibility who had been Third, program, and expansions of Medicaid ineligible for AFDC extensions of Medicaid coverage to of the federal poverty Medicaid all level). women on eligibility two categories. infant changes "Targeted in eligibility criteria for eligibility to for reasons of family structure. all were associated with in infant mortality; the effect In particular, the changes can be divided into AFDC 34%, an to across the states, causing dramatic expansions' were narrowly targeted changes which included changes welfare under the inputs. of pregnancy from 14.2 at quite different rates births use estimate that the expansions of the 1980s increased Second, increases generosity. low birthweight are not created equal. we eligible for public insurance in the event in relative state mortality First, we the National Longitudinal Survey of Youth (NLSY) to ask how the policy changes affected the use of birth We have three Finally, cash demographic groups "Broad expansions" were with incomes less than specified levels (e.g. 185% These two types of policy changes affected quite different populations, suggesting the potential for heterogeneity in their effects. In fact, we outcomes, while the broad expansions had is little in the differential effects that these policies much lower takeup featured had sizeable and significant effects on birth find that the targeted expansions rates, We effect. suggest that the source of this difference had on Medicaid coverage; the broader expansions even among otherwise uninsured mothers. The targeted expansions were associated with a Medicaid expenditure increase of $1.7 million per infant saved. This figure is fairly low compared to recent estimates of the value of a high relative to clinical estimates of the costs of saving a life. However, through improved prenatal care. life are unable to resolve whether this reflects a failure of prenatal care to deliver its life it is We promised savings, or a failure of mothers to obtain such care once they were eligible for Medicaid. The rest of the paper is about our measures of newborn health. effects on eligibility. Part In Part laid out as follows: In Part II, we I, we provide background information discuss the Medicaid expansions, and their investigates the effect of these expansions III on birth outcomes. Part IV discusses the differential effects of the targeted and broad expansions on Medicaid coverage. V investigates the cost-effectiveness of the targeted expansions using information expenditures and individual use of prenatal care. Part Part on Medicaid VI concludes with a discussion of the policy implications of our findings. I. The infant nwrtality rate and the incidence of examined indicators of 1980s. less Background oo Birth Outcomes infant health. The incidence of low in the U.S. low birthweight are two of the most frequently Figures la and lb plot the trends in these measures over the birthweight, defined as the number of live births per 1000 weighing than 2500 grams (approximately 5.5 pounds), declined from 68.7 in 1979 to 66.6 then rose to 69.4 by 1990. in 1984, but In contrast, infant mortality declined throughout the decade, although it declined at a slower rate between 1984 and 1989 than underscore the fact that although they are related, had it earlier. These differing trends low birthweight and infant mortality measure different aspects of birth outcomes. Low birthweight of low birthweight are is at a key indicator of the underlying health of the fetus. Horbar et al. who among normal (1993) found that between 601 and 1300 grams at birth, a decrease of approximately 10% birthweight infants (Office of Technology Assessment, in a sample of very low birthweight children weighing each increase in the probability in birthweight of 100 grams was associated with of death, other things being equal. In contrast, infant mortality rates reflect not only the health of the fetus as measured by New birthweight, but also the effect of any interventions that occur during or shortly after birth. technologies have had dramatic effects on the survival rate of low birthweight infants. al. are high risk of neonatal mortality and experience post-neonatal mortality rates 10 to 15 times those found 1987a). Children Buehler (1985) report that improvements in birthweight-specific mortality rates accounted for 91% et of the overall decline in neonatal mortality between 1960 and 1980.' These interventions, however, are often very expensive. although babies weighing less than 25(X) grams account for only they account for 57% of the cost of neonatal hospital care. 9% Schwartz (1989) reports that of neonatal hospital caseloads, The average cost of caring for a surviving low birthweight baby was $9,712 compared to $678 for an infant weighing more than 2,500 grams. These costs rise as birthweight falls; in birthweight below 1000 grams was $118,000 ' More recently, Horbar (OTA, 1987b). Moreover, survivors et al. (1993) report that as mortality reported between 1989 and 1990 1984, the cost of saving an infant with nwy much as half of the decline are at high risk m national infant be attributable to the introduction of a new therapy replacing an essential substance in the lung (pulmonary surfactant) that is not manufactured by the fetus in significant quantities until the 33rd week. This therapy was introduced for artificially in October 1989. ^ of handicaps such as cerebral paJsy of significant degree, major seizure disorders, blindness, (McCormick deafness, and learning disorders ei al., OTA, 1992; 1987b, Chaikind and Corman, 1990). The high cost of caring for low birthweight infants and their uncertain future should they survive, have led policy makers to emphasize the prevention of low birthweight through the There are a number of ways promotion of appropriate prenatal care. improve For example, approximately two-thirds of fetal health. term, and Creasy et al. (1980) found that over inexpensive ($10 to $20) screenings 60% all that early prenatal care can low-birthweight births are pre- of these cases could have been identified using in the first prenatal care visit. Several clinical studies cited in the Institute of Medicine's influential 1985 report suggest that providing appropriate prenatal care to women identified by these screenings a cost of between $400. and $500. per (at reduce the incidence of low birthweight of more than 20%. saving a life through improved prenatal care As has been noted by outcomes among most $142,000 per number of economists, however, a women who do is at and do not receive prenatal care are Compared see Harris (1982) for an extensive discussion. This figure cost $20,000. is calculated as follows. One would Of these, Prenatal care for these 28 of low birthweight by much that the cost of saved. studies based likely to on differences based on survey smaller effects of prenatal care on screen 1(XX) pregnancies at a cost of $20 each would To 20%, or 47 will women six babies. in be biased by selection; expect 70 of these pregnancies to result in low birthweight births absence of any intervention. screening. life to clinical studies, studies data that attempt to control for this selection typically find ' These figures imply woman) could be pre-term, and 28 (60%) will then cost Using the Vual will be caught in the by this $14,000, and will reduce the incidence Statistics data below, we estimate that a decrease of one low birthweight baby per 1000 births lowers the infant mortality rate by 0.04 deaths per 1000 births. Thus, the $34,000 spent to reduce low birthweight births by six babies will save 0.24 lives, for a cost of $141,667 per benefits of prenatal care, since some of life saved. the babies higher birthweight, will be less impaired later who in life. an understatement of the would not have died, but who are now of This figure is birthweight (Rosenzweig and Schultz, 1982, 1983, 1988; Frank etaL, 1991; Grossman and Joyce, studies focus These differences 1990). on the gains that could be attained die impact of prenatal care as it is under practiced in the field. all pregnant In women, summary, For example, women the cost of saving an infant life et al., 1987; also reflect the fact that clinical ideal circumstances, reduce pre-term delivery were delivered not only to the but to may in results Gorman if whereas surveys reflea prenatal care designed to identified as high risk would rise to by screenings, over $1.3 million.' the available clinical evidence suggests that while both reduaions in the incidence of low birthweight and high-tech neonatal care can reduce infant mortality rates, the former is the more cost effeaive policy. the use of prenatal care coverage of pregnant was woman in Decreasing the incidence of low birthweight through increases faa the primary motivation The Medicaid Expansions Background* Historically, in Medicaid that took place during the 1980s. II. a) for the expansions in the in AFDC. Medicaid This linkage with the existence of the eligibility for AFDC restricted access to the AFDC-Unemployed which the primary earner is women and children has been closely tied program in three ways. to participation First, despite Parents program which provides benefits to households unemployed, AFDC in benefits are generally restricted to female-headed 'That is, there would be $500,000 spent in delivering prenatal care to all 1000 women in the sample, and 9.4 pre-term low birthweight births would be prevented (since 100% of these cases would now be caught). This implies a cost per life saved of 1.33 million. which Federal matching funds were available. States can cover additional groups under Medicaid, but only if they pay the full cost of coverage. We do not have mformation about these "state-only" policies. In addition, we only There were also expansions of the Medicaid discuss policies that applied to pregnant women. * The policies discussed in this section are those for coverage provided to children in this era; see Yelowitz (1993) for details. households.* Second, income cutoffs for cash welfare vary across states, and can be very low. example. In Texas, the cutoff for a family of 4 the stigma of applying for cash welfare in 24% 1979 was only of the poverty programs may have prevented line. Third, from families eligible For receiving Medicaid benefits (Moffitt, 1992). However, from the inception of the Medicaid program, extending Medicaid benefits to some groups of pregnant options expanded rapidly during 1980s, in a manner that eligibility changes can be divided into two types. defmed groups who had not women whose income was somewhat above Also included Medicaid in this category are changes eligibility. Because these in first AFDC. AFDC. This included AFDC AfTX) income These In brief, these type expanded coverage to narrowly diese cutoffs but eligibility not on detailed in the Appendix. and two parent families whose income was below individuals in traditionally qualified for have had the option of women who were is The states first time pregnant cutoffs, and "Medically Needy" who had large medical expenses. limits, which carry with them changes changes are narrowly targeted, we label them "targeted expansions". Beginning States were income first in April 1987, the income requirements for Medicaid were also greatly liberalized. given the option and then required to provide Medicaid coverage to levels that greatly exceeded the AFDC uniform minimum threshold had been established with incomes up to incomes up to 185% of income requirements * Not every 133% of state - all limits in states most states. were required to By the poverty line. In what follows, we with April 1990, a cover pregnant the poverty line, and stales had the option of covering women women with will denote these relaxations of the as "broad expansions". AFDC-UP program over our sample period, and eligibility requirements of 1990 only 5% of the AFDC caseload qualified under this program (U.S. had an strirt. As a result, as House of Representatives, 1992). are income women b) Effects on EUgibiUty In order to estimate the effects of these eligibility expansions, we have built a detailed simulation of Medicaid policy in 49 states and the Distria of Columbia, over the 1979-1990 period.* The construaion of 12 years of CPS simulation this is described in detail from 14.2% In this seaion, Medicaid coverage to recession years, 34% of this in women in eligibility criteria figure indicates that population between 1979 and 1990. became sample when moderate increase eligible because they The percent However, the stricter in the early is restricted to fell into for that the eligible rose eligibility increases During the poverty, so eligibility increased years of the Reagan adnunistration. women with incomes below twice the poverty to the AFDC in eligibility associated program in the early most dramatic changes '80s. line. fell Both figures show a with increases in the coverage of unborn children and two- earner families mandated in the Deficit Reduction Act of 1984 *We is have been business cycle effects are controlled for in this way, eligibility 1982 as a result of cutbacks show The CPS CPS who would in the each year had they become pregnant. many women became In Figure 2b, the The use demographic and income information of the early 80s show that these estimates are sensitive to business cycle effects. even as we this simulation. Figure 2a shows the fraaion of 15 to 44 year old eligible for Appendix. data to simulate the effea of the expansions on Medicaid eligibility. the largest available annual data source with the requisite undertaking in the in the number of exclude Arizona from the analysis because program. 8 (DEFRA eligibles it '84). But the figures clearly were associated with the relaxation does not have a conventional Medicaid of income restrictions 80s in the late -- eligibility The aggregate time trends shown growth of On Ohio saw steady On between 1988 and 1990. 1988, but large jumps in the This variation women eligible for we examine eligibility. states, is rises in eligibility show two from 1979 explored further in variability in the with very different patterns: to 1988, and a relatively small jump little change in eligibility until each in Table state, in 1. Here, we show the fraaion of 15-44 year old each of the years 1979, 1986, and 1990. For 1990, under the targeted and broad expansions separately, as well as overall eligibility The growth from 1979 a reduction in states such as is states 1990.' two years of the sample. to 1986 under the targeted expansions such as Colorado, Minnesota, and Virginia, while there but there mask considerable the other hand, Florida experienced last Medicaid Figures 2a and 2b Figures 3a and 3b eligibility across states. the one hand, in 100% between 1987 and increased almost New is little The growth from 1986 Jersey. to also substantial variation; eligibility growth in Mississippi is very dramatic growth in 1990 positive for is is some in Delaware and even all states, over three times that of New Jersey.* It is this substantial for our study. change within If states are and over time that provides the identifying variation ranked by the frartion of the 15-44 year old female population that eligible, the correlation between rank experienced a change ranking of in states in 1990 and rank at least 10 positions: in 1979 is Illinois fell only 0.33. Twenty-seven is states from the 8th most generous state ^Within the set of targeted expansions, the policies that had the biggest effect were those that covered first-time pregnant women. The faa that these changes, and not the coverage of two-parent families, had the largest impact reflects the fact that few married couples were poor enough to qualify for the Medicaid program under the AFDC income cutoffs. changes were "expansions"; half of the states increased eligibility from 1986-1990, and half of them reduced it. On the other hand, almost every state shows a sizeable increase in eligibility under the broad expansions. • Clearly, not all of the targeted eligibility to the 38th most generous, while Mississippi rose from the 44th most generous state to the state that makes c) the highest fraaion of Targeted vs. population eligible. Broad Expansions Throughout expansions. its Our this we paper, will rationale for doing so is distinguish between the effects of the early and broad presented in Table 2, which highlights the heterogeneity of the populations affected by these two types of expansions. covered under the targeted expansions, while the third looks under the targeted expansions, but were are based eligible at individuals column shows the the set of individuals who would not have been under the broad expansions. All columns on data from the 1990 CPS. While individuals covered by relative to the fiill somewhat either the targeted or broad expansions appear disadvantaged sample, the broad group appears to be nx>re similar to the sample average than to the targeted group. is first The second column examines characteristics of the entire eligible sample. eligible The Compared wealthier, more to the targeted group, the likely to Furthermore, the broad-expansion group group covered by the broad expansions be white and married, and slightly older on average. is much more likely to be working, and less likely to be receiving any form of public assistance than the group covered by the targeted expansions; in fact, the group covered by the broad expansions average 15-44 year old female. is less likely to While the two groups are equally composition of insurance coverage differs substantially. expansion group 7% is be receiving public assistance than the covered by Medicaid, while only group does. 10 be uninsured, the Thirty-eight percent of the targeted- 13% of the broad-expansion group of the targeted group has employer-provided health insurance die broad likely to in their own name, is; and only while 25% of This population heterogeneity suggests that the two types of expansions may have had very different effects on birth outcomes. We will allow for such a differential effea in the estimation below. III. Eligibility a) and Birth Outcomes Methodology We from examine the Vital Statistics, effect of the eligibility expansions the that two measures of 1979-1990 period. The is, we outcomes using aggregate data birth which reports the incidence of low birthweight infant mortality in each state this data to on and year for the eligibility first is among full sample of births 15-44 year old all the actual percentage of use the data presented in Table 1 than 2500 grams) and (less in that state/year.' women women made for each of these years, in each state eligible matched We match and year over under expansions; to the birth outcomes data for that state/year. A may potential drawback to this strategy, however, is that the CPS fraaion-eligible measures incorporate business cycle effects, or other shocks specific to states and years. showed, for example, that the recession of 1982 was associated with increases despite the adoption of stricter eligibility criteria. in Medicaid To ' eligibility Similarly, the fact that in 1990 Mississippi had the highest fraction eligible of any state reflects both the generosity of the state relative poverty Figure 2a program and the of Mississippians. the extent that relevant state and year specific characteristics are not captured by state and explored the effea of the expansions on low birthweight in the NLSY While the findings were supportive of our conclusions using aggregate data, In an earlier draft, data discussed below. the confidence intervals we were too large to draw any unable to investigate infant mortality with the NLSY II useful conclusions. due to small sample Furthermore, sizes. we were year dummies, coefficient on the a state recession frartion eligible will be biased between Medicaid In order to We first source of variation this Suppose, for example, that overcome this fraaion of this same sample of By using in eligibility could induce a spurious positive correlation and low birthweight. '° eligibility problem, took a 1-in-lO sample of our that year. by omitted variables. associated both with increases in eligibility and with a higher incidence of low is Then birthweight. they are not constant within a state, or across states within a year), the (i.e. CPS we have created a measure of "simulated eligibility". women cohort of women who would have for each year. in Furthermore, we derives from having relatively small cells for These models some evidence which suggests states in the Medicaid policy as exogenous treat state that this assumption is not true. were more and outreach programs. likely to In the '°A similar bias could arise level find for example in to birth indicates that Simulated women is in much our estimate that in Gold is year dummies included in fact et al. (1993) report that states women who delayed obtaining if adverse trends will include state fixed effects eligibility is will control outcomes are correlated with the absolute largest impact where the population is poorest. in birth much fiaiter, which indicates better than those in other states. flatter which On of women that fell sharply on average, young the other hand, the increase in than the increase in actual eligibility in Mississippi, which Mississippi were poorer than a nationally representative group of eligibility will still we independent of other outcomes; there that in Connecticut, actual eligibility for this cohort Conneaicut fared simulated eligibility in the models below, we Simulated in the mid-to-late-80s. women state in adopt optional expansions and to set up complementary advertising of poverty, since expansions may have their "We each CPS. with high proportions of low birthweight births and high fractions of prenatal care is reduce the sampling variability some in each state simulation, obtain an estimate of the fraaion eligible that depends only on state rules, and characteristics of states." then calculated the been eligible for Medicaid same group of approximately 1000 women the We vary with aggregate cyclical conditions, but this variation in the regression. 12 is women. absorbed for such spurious correlation between time invariant state characteristics and Medicaid policy. b) Overall Results Table 3 presents the basic regression All regressions include a full set of year results. effects, to control for the strong trends in infant mortality They la and lb. across states that is identified may be correlated with both Medicaid policy and birth outcomes. by the deviation of Medicaid When we birthweight, but illustrated in Figures also include a full set of state effects, to control for time invariant differences The top panel of Table 3 models 1980s. and low birthweight eligibility is we fraaion eligible, and becomes significant lead to a redurtion of in eligibility 2% in the rate state-specific find a negative effect The estimate not statistically significant. percentage point increase its mean. the overall effects of changes in Medicaid eligibility in the use the actual fraction eligible, it from at the 5% level. rises The on the incidence of low when we use the other hand, there is 7% We of low birthweight. conclude that there eligibility eligibility is is some evidence relatively small. a sizeable and significant effect of expanding Medicaid eligibility eligibility used. The estimate from the simulated regression indicates that a 20 percentage point rise in eligibility under Medicaid led to a decline in the infant mortality rate. mortality 20 (roughly the magnitude of the expansions of the 1980s) would on infant mortality, regardless of the measure of eligibility the simulated coefficient suggests that a of an effect of these expansions on the incidence of low birthweight, but the effect On Thus, the model In the final two colunuis, we regress on the incidence of low birthweight and on our on mortality is eligibility the mcidence of infant measure. The strong effect of apparent even after conditioning on the positive correlation between changes and birthweight improvements. Thus, there is evidence that eligibility for health 13 insurance improves health, as measured by birth outcomes. terms of their stated goal of reducing infant mortality, the expansions of the In 1980s were a success.'^ We examine the heterogeneous will explore the cost of this success below. effects of the different types of eligibility First, however, we policies pursued over this period. c) Differential Effeas of Targeted and Broad Expansions The bottom panel of Table mortality rate in each state and year 3 regresses the incidence of low birthweight and the infant on estimates of the percentage of under the targeted and broad expansions constructed from the CPS. over the full set of years (1979-1990), while the broad regression years that the broad expansions were in place. women The is eligible for Medicaid targeted regression is run run over only 1987-1990, the All the regressions include a full set of year and state dummies. Table 3 shows that the targeted expansions have much stronger effects on both measures of infant health than the broad expansions. This result eligible, despite the fact that the estimates was associated with a highly strongest on percent regressions. Using the simulated fraaion eligible, eligibility is significant we 4.5% when we use the simulated fraction eligible are equally precise across the find that a two 20 percentage point increase in decline in the incidence of low birthweight under the targeted expansions, but with only an insignificant 0.4% decline under the broad expansions. Similarly, a 20 percentage point eligibility rise was associated with a 7.3% decline in '^Our finding of stronger effects on infant mortality than on the incidence of low birthweight is who examined the introduction of National Health Insurance consistent with that of Hanratty (1992), Canada, and found significant effects on mortality but mixed effects on birthweight. It does contrast widi the fmding of Fischer (1992), who also studied the effects of the Medicaid expansions from 1984 onwards. He found strong effects on the incidence of low birthweight for blacks, but no in effects on mortality for either race. 14 infant mortality under the targeted expansions, but with only a 0.6% decline under the broad The expansions. findings for infant mortality persist when we condition on the incidence of low birthweight.'^ IV. Explaining the Heterogeneous Effects: The is birth outcome results presented The Role of Medicaid above provide a mixed message. On strong evidence that insurance eligibility can improve birth outcomes. nature of the policy appears to be key. Why is it that the targeted successful than the broad expansions in improving birth outcomes? lie in a number of researchers have emphasized, programs does not automatically translate into coverage. only about two-thirds of women eligible for fmd a similar takeup rate for effea on fetal health We suggest that the answer unemployment insurance. individuals if by pregnant women. eligibility for social insurance and welfare For example. Blank and Ruggles fmd that Eligibility can not be expected to have an they were covered by Medicaid at any point in the under the targeted expansions Unemployed Parent program, and those eligible only the "other targeted expansions" had a birthweight. may take up their benefits, and Blank and Card (1991) also attempted finer divisions of the data. fraction eligible the other hand, the unless individuals takeup their newly available Medicaid benefits. The March CPS asks "We have AFDC the one hand, there expansions were so much more the differential takeup of these different types of eligibility changes As On Takeup For example, we have tried separating the under AFDC or the AFDC- into those eligible under any other targeted expansion. statistically significant effect We fmd that on the incidence of low the standard errors are large, and in the estimates using the simulated cannot rejert the hypothesis that both types of targeted expansions had similar However fractions eligible, we For infant mortality we find using simulated eligibility that both types of targeted expansions had quite similar effects, although once again the standard errors are large. effects. 15 1 previous year.'* We women made every 100 Of women coverage? period, so that about By the year.'^ 1 eligible for 15 to old, .5% of women women. This 6.5% had in the relevant is how many in the entire We who became an undercount of those is, women for report some at point during population would represent full only a lower bound, however, since some of the Medicaid changes (those associated with the adoption of the is additional age range were pregnant takeup rate of 0.115 figure of these expansions; that a child in any given year during our sample AFDC-UP program, Hence, the number of covered not only pregnancy but also other conditions. pregnant elasticity coverage of pregnancy, 44 years this calculation, a takeup by pregnant eligibility can therefore estimate the "takeup" eligible for coverage under example) for women who became changes. all eligibility examine the relationship between Medicaid coverage and state/year average eligibility using linear probability models that control for other observable characteristics, including race, marital status, employment status, and income. CXir data set consists of All regressions include a full set of state and year dummies.'' a 12 year period. In the first column of Table 4, we include an indicator equal to We under either the targeted or the broad expansions. '* 455,774 observations over Unfortunately, prior to March 1988, find that there is 1 if a woman was an increase health insurance coverage in the eligible in the probability CPS was assigned according to whether one received coverage under the policy held by the head of the household. Thus, those dependents deriving coverage from outside the household were counted as uninsured. After March 1988, each family member was asked about health insurance coverage from any source. its largest effect on children below the age of 15, so that it should not our results; furthermore, the inclusion of year dummies will capture overall changes This questionnaire change had significantly bias in the '^ nature of responses. All women who In addition, give birth in a year, must have been pregnant between 2/3 and 3/4 of the next year. '*We use a women whose Hence, the percent pregnant linear probability model in in and for computational ease with our large sample is at least (1 facilitate the size. 16 some time during pregnancies begin in one any year order to at + that year. year will give birth in .67)*6.5, or 11.5%. use of instrumental variables below, 10% of coverage of 2.4% for every in rise This estimate appears relatively high eligibility. cximpared to the calculations given above. The other covariates have the expected effects; Medicaid coverage is less likely if individuals are white, married, working, or high income, and the probability of coverage increases with the number of children. In the we second and third columns, disaggregate the eligibility measure into eligibility for a targeted expansion (over the 1979-1990 period) and eligibility for a broad expansion (over the 1987-1990 period). We 10% the broad expansions; a by 2.7%, while a 10% find that the targeted expansions rise in the eligibility had much larger effects on coverage than under the targeted expansions increased coverage under the broad expansions rise in eligibility is actually estimated to decrease coverage. Why did the targeted expansions have a bigger effea the results are subjea to omitted variables bias: there on coverage? One may be AFDC more are both likely to is that omitted characteristics that are correlated both with coverage and with eligibility. Suppose for example, that were on possibility women whose be eligible (because they are poor), and more mother's likely to be covered (because they are familiar with the system). The bias associated with oniitting the family's history of welfare dependency is likely to be nwre important in the case of the targeted expansions, because they applied to a lower income portion of the population. In order to address this issue, of Medicaid coverage in we each state in and year; columns in (4) columns use the simulated measure.'' we present instrumental variables estimates of the probability through (7) of Table (4) and (S) we dummies burdensome. (it is The instrument In both cases, the targeted expansions is the fraaion eligible have much larger effects similar to instrunoenting using the full set of equally consistent but less efficient), but Actual eligibility remains potentially problematic 17 is use the actual value, and in columns (6) and (7) ''Using actual eligibility in each state and year state*year 4. is much in this less computationally context, since state/year than the broad expansions; in neither case When we 1 % is the coefficient for the broad expansions significant. we use our preferred simulated instruments, for every 10% rise in targeted eligibility. This elasticity appears more reasonable calculations discussed above, and suggests that takeup for the targeted expansions, but We this was high fairly low among the population among eligible for the in light the population eligible broad expansions." broad expansions was First, the population eligible for the group had higher incomes and better access of need, the broader expansions Second, given a level difficult to bring women who (1987) report that for Medicaid many low-income even if to needy; as Table 2 less employer provided health insurance. may have been less effeaive. have never received any sort of social assistance program, either because they do not know about women AFDC benefits. It unaware into the easier for illustrated in These two explanations clearly have differing welfare implications; the first need it; was fairly benign since the the second suggests that women who women who Medicaid program expansions because these had more frequent mteraaions with the government assistance system, as difference in takeup rates be that they can qualify may have been eligible for the targeted may It Rymer and Adler or because of stigma effects. it families and their physicians are they do not receive administrators to find and notify likely to of the can think of two other possible explanations for lower takeup rates under the broad expansions. shows, estimate that coverage increased by roughly women Table 2. suggests that the did not take up coverage were less needed the program were not aware of it. recessions will increase both Medicaid eligibility and coverage. '*As discussed above, the targeted expansions are at least partially comprised of AFDC eligibility changes, which should have more lasting effects on coverage than pregnancy only expansions, while the broad expansions consist of pregnancy coverage only. It seems unlikely that this factor can explain a difference in coefficients of the magnitude of those in Table 4; the majority of the total growth in eligibility under the targeted expansions was accounted for by changes coverage. 18 in pregnancy-only In an effort to differentiate between these two hypotheses, models using the subsample of We Medicaid. women The without sources of health insurance coverage other than results are estimates are similar to those for the full shown in the final two columns of Table sample, and show that even because they were not effeaively translated the broad expansions did eligibility failed to affect birth into increases in The 4. among otherwise uninsured on coverage while the targeted expansions had significant effects This suggests, therefore, that the broad expansions of not. reran the instrumental variables present the results using the simulated instrument; the relative findings using the actual instrument are similar. women, we coverage, even outcomes among needy women. V. Exploring the Cost-EfTectiveness of the Expansions a) Medicaid Payments per Infant Saved While the Medicaid expansions of birth data outcomes, this improvement came on Medicaid expenditures States report their a cost to the Medicaid program. to assess the cost effeaiveness We and outpatient hospital costs for examine all total (ic. "We are grateful to Killard in we use to the Health Care Financing to the class of expenditures on physicians, clinics, and non-disabled children and non-disabled/non-elderly pregnant wonoen and infants). 15-44 year old female population improving of the expansions. Unfortunately, these data are not available by type of service population type in In this section, These reports break down expenditures according provider, and the category of recipient. adults. have been successful payments made under the Medicaid program Administration each year." inpatient at the 1980s appear to We that year. Adamache of Health these data. 19 (ie. childbirth) or by detailed normalize the expenditures using the All figures are in 1986 dollars; we state's deflate Services Research, Inc. for providing us with expenditures on hospital inpatient and outpatient expenditures by the Consumer hospital services, and expenditures for physician and clinic services by the services. Once of Medicaid The again, we eligibility, Price Index for CPI for physician's regress this measure of expenditures on the actual and simulated measures and disaggregate by the type of expansion (targeted versus broad). results are reported in Table 5. As would be expected, the expansions significantly increased Medicaid expenditures; regressions using the simulated eligibility measure indicate that an additional eligible woman was associated with an increase in expenditures of $232 per year. Expenditures on the targeted expansions were much larger, amounting to $449 per eligible woman. In contrast, although the coefficient on eligibility under the broad expansions is sizeable, it is not statistically significant. These data can be used woman who became percentage point rise rough estimate of the cost-effeaiveness of the targeted Using the simulated measure, Medicaid expansions. by $449 per to provide a eligible births. Taken estimate that Medicaid spending increased under the targeted expansions. in (simulated) targeted eligibility 0.04 deaths per 1000 we We also fmd that a one decreases the incidence of infant mortality by together, these fmdings imply that the cost of saving a life through the targeted expansions was $1.73 million." What does this imply for the efficiency of Medicaid policy? This figure appears high "This figure is calculated as follows. To generate 1000 births, given the average fenility rate of 0.065 in our sample, would require 15,385 mothers. A one percentage point increase in eligibility in this sample would therefore cost $69,079 ($449 for each of 153.85 women). This would reduce the number of infant deaths by 0.04. So, to reduce the number of infant deaths by one would cost $1 .73 million. Note that to the extent that the newly eligible women (under either type of expansion) were getting treated for free when they were uninsured, the net cost to society of the Medicaid expansions is lower than the costs to the Medicaid program. Saywell et al. (1989) show that the average cost of uncompensated care for pregnancy and childbirth in 1986 in Indiana was $2668. Subtracting this from the cost per birth of the targeted expansions lowers the cost to society per saved to $1.66 million. 20 life compared to the cost of saving a low birthweight infant through technological intervention; as discussed above, the Office of Technological Assessment found that the average cost of saving an infant with birthweight less than 1000 grams was $135,000.^' However, this figure understates the effeaive cost of high-tech interventions, for two reasons. First, over 30% we comparing the only have information on expenditures per infant that lived. In of these infants died, and OTA figure to ours, the cost per lived saved should be inflated to account for babies that used resources, but were not saved. Second, described in Part I, serious handicaps. we have no there is Hence, infant mortality through information on the quality of life a distinct possibility that surviving to the extent that the improvements of infants who low birthweight infants will suffer Medicaid expansions were effective in fetal health, their costs (per life As are kept aJive. in reducing of a given level of health) will be overstated relative to high-tech interventions. Moreover, $1.73 million a life. Manning et al. is at the low end of the recent range of estimates for the value of (1989) use data from studies of willingness to pay for a small change probability of survival to estimate that the value of a life is $1 .66 million. in the Cropper and Oates (1992) report that studies based on compensating differentials for risk of death on the job yield a value of life of between $1.6 and $9.0 million; Viscusi (1992) presents a broader range, with a preferred estimate of $12.1 million.^ have spent, at nx)st, as ^'This and all much Judged by to this yardstick, the targeted Medicaid expansions appear keep an infant alive as that person would have been willing subsequent figures are expressed in 1986 dollars. Where deflation is to to pay necessary, expenditure figures. it is done using the Medical care component of the CPI, for comparison to our The correa deflator for this exercise is not obvious, but using different deflators would not substantially alter our conclusions. ^ Furthermore, compensating wage differentials understate the amount than an average person would pay to reduce the risk of death, because the least risk-averse persons tend to take the riskiest jobs. 21 ^ to be kept alive. Alternatively, we can compare the cost of saving a life through the Medicaid expansions to the cost of keeping individuals alive through other public policy interventions. Graham and Vaupel (1980) report the cost of saving a life-year through 57 different public policy interventions, ranging from mandatory (the seat belts or air bags to reduced emissions. Using a U.S. average for 1986), 38 of their 57 interventions cost However, the other 19 interventions cost $30 million.^ Cropper per consumer producer life government life et al. much more, and in life less than some expectancy of 74.8 years $1.7 million per cases, the costs were life saved. as high as (1992) estimate that regulations on the use of pesticides cost $60,000 saved, but that regulations on the production of pesticides cost $35 million per saved. Thus, while the targeted Medicaid expansions were not the most cost effective life-saving intervention, they were much more efficient than some of the policies currently being pursued. b) Evidence from Individual-Level The effective results above suggest means of saving relative to the Data that the targeted Medicaid expansions may have been a cost Nevertheless, the cost of doing so appears to be quite high infant lives. promised cost savings from prenatal care discussed explanations for this high cost estimate. The first is that women "Relative to these other studies, our findings are subjert to our estimates are likely to be too low, since studies are valuing saving the lives of we in Part failed to at least are valuing saving a two I. There are two possible make use of (offsetting) biases. life at birth, workers or survey respondents. cost-effective First, whereas the other Second, our estimates may be too high, since the infants kept alive by medical interventions may be of worse health later in life, as described above. "Furthermore, mandatory air do not consider the cost of the intervention to the consumer; the government, but do increase the societal cost of saving a life. their calculations bags have no cost to 22 prenaial care come care when they were covered by Medicaid; thai the infant lives that is, primarily through expensive hospital interventions." The second targeted. These alternative views obviously have very different implication Evidence from case studies of Medicaid expansions suggest for the high cost of saving an infant expansion of eligibility in Tennessee to would not allow we Longitudinal Survey of Youth (NLSY) We to "Women may Medicaid The is die explanation increased Medicaid enrollments, but that Enrollment failed to take effects of eligibility first is the first trimester of pregnancy. have eligibility, former such a at late do so using individual-level data from the National examine the expansions on two indices of prenatal care use. doaor during for future policy design. (1990) found that a 1985 et al. days prior to delivery. thirty not appropriately is attempt to distinguish between these views by examining the effect of the expansions on the use of prenatal care.^ a that the it for the effeaive use of prenatal care. In this seaion, saw women married most of the increase took place within the date For example. Piper life. praaice, prenatal that, in is not as cost effeaive as clinical studies suggest, perhaps because is were saved may have under the targeted an indicator equal to one Early initiation of prenatal care if the is woman important advantage of prenatal care because they were unaware of or because available providers were unwilling to accept Medicaid coverage. Neither of these problems would deter the use of expensive hospital care because hospitals that participate in Medicare are prohibited from refusing already in labor (OTA, 1987b). Furthermore, uncompensated care, accounting for make every effort to enroll eligible uninsured (Gold aL, 1993). Once et is enrolled, al. women may women receive in al. services than their (1990) find that uninsured patients receive less intensive hospital treatment than insured patients along a much et Medicaid for the costs of childbirth much more expensive (1991) and Wenneker et ''The expenditure data do not offer women component of hospital al., 1989). As a result, the largest single 17.4% of these expenditures (Saywell hospitals uninsured counterparts; Hadley et or from transferring, any to treat, childbirth number of margins. Both physician and hospital insight into this question. draw further inferences from the relative changes in these categories, since the distinction between them is not clear; for instance, the physician category will include the costs of deliveries done by outside doctors, but perhaps not the costs of deliveries done by resident interns. expenditures rose significantly under the targeted expansions. 23 It is difficult to both for conducting screenings, and for establishing a base-line for the monitoring of initial development (OTA, 1987b). The second measure sonogram during months of the pregnancy. ultrasound itself the first six has any effea on the fetus, of delivery as a sign that a physician The Since 1983, NLSY women birth, including began in is we view an indicator equal to one While there is if no evidence woman had a that the use of the receipt of an ultrasound before the point monitoring the pregnancy. is 1979 with a sample of 6,283 women between the ages of 14 and 21. have been asked bi-annual questions about the prenatal care when the fetal that preceded each they initiated prenatal care and questions about sonogram use. Retrospective information has also been collected for births before 1983. NLSY The also contains enough information about income, family structure, and state of residence to allow us to determine whether the woman was eligible for Medicaid coverage using the same simulation program we applied to the After the exclusion of missing values, occurred between 1979 and 1990." sample of U.S. mothers poor were over-sampled. bom to 78% are We do so data. left with 4759 observations on births that NLSY is not a representative age range because African- Americans, Hispanics, and the Almost half of the of the African-American infants, we CPS important to note that the It is in the relevant of the pregnancy. in the first trimester infants are African-American or Hispanic, and of the Hispanic infants, and 32% 73% of the other infants were mothers from the supplemental "poverty" sample. The data indicate that throughout coverage of their pregnancies are poorer, most of our sample period, less educated, and more women likely to eligible for be African-American or Hispanic relative to the sample as a whole, and even relative to the subsample of " One shortcoming of these data and birth outcomes took place is Medicaid women with that the last available survey that asked about prenatal care in the spring of 1990. must await the release of the 1992 survey. 24 Information about births in the rest of 1990 incomes below the poverty line." They also have much lower scores on the Armed Forces QuaJiflcation Test (AFQT), Medicaid-eligible eligible women women are a standardized test of ability.^ 32% more sonogram in the first These comparisons highlight the eligibility not surprising that is it likely to delay obtaining prenatal care: 20% delay care compared to eligible received a Hence, in the entire sample. 6 months compared to possibility that estimates Similarly, 48% 27% of Medicaid- 43% of Medicaid- of non-eligible women. of the effects of individual Medicaid on the usage of prenatal care may be biased towards zero by omitted variables correlated with both eligibility and propensity to seek care. problem, we instrument In order to address this individual eligibility using first both the actual and the simulated fraaion eligible measures CPS, calculated for this cohort of young women.'" expansions because the post-1987 sample size expansions affected Medicaid coverage, ^* it is We examine only the impaa of Also, quite small. seems reasonable to assume from the the targeted since only the targeted that the broad expansions had random measurement error and minimize the amount of missing data, we use the average income in the two years preceding the birth as our measure of income. If the woman was living with her parents then we use the parents' income less the need standard for a family of that size (following the procedure use by the AFDC program to impute family resources to minors living at home). Otherwise, we use the sum of the woman's own income, the spouse or partner's income, and "other" income. The use of this measure also avoids the In order to attenuate the effects of imputation of eligibility for prenatal care on the basis of temporary income losses suffered after the birth. " Since the AFQT was administered normalized using the mother's age. to all the Some readers measure of background and education, rather than ''^e problem that individual eligibility outcomes has been noted in the may women may as a at the same point prefer to regard the measure of native wider social insurance literature. were summary ability. For example, unemployment may confound of those benefits on unemployment durations (Meyer, 1989). interpretation of the effect In that context, control for the wage, or nonlinear functions of the wage, directly. it may be Since Medicaid complicated function of a large number of individual characteristics, 25 as a be correlated with unobserved determinants of insurance benefits are a fiinaion of lagged wages, and this variables strategy. in time, scores AFQT we easiest to eligibility is a prefer the instrumental little impact on the use of prenatal care. We estimate logits models which include exogenous characteristics of the mother and child, in addition to a full set dummies. As discussed above, characteristics of states that state fixed effects state (California), We of year dummies." demand also estimate models with and without a set of state the inclusion of state fixed effects controls for time invariant may be correlated with state Medicaid policy. a lot of our data 9 states represented in -- However, models with although there are over 600 observations for the largest our sample have fewer than 15 observations. We do not include fixed effects for these 9 states, so together they form the omitted "state". The instrumental effects, we find variables results are presented in Table 6. some evidence In the models without state expansions led to increased use of early prenatal that the targeted Using the simulated instrument, our estimates imply that eligibility for Medicaid under the targeted expansions decreased the probability that the initiation of prenatal care was delayed beyond care. the first trimester by first six 13%. There months; the coefficient is is no statistically significant effect wrong-signed. Once on the use of sonograms state effects are included in the in the model, none of the results are significant, although the sonogram result for the simulated instrument becomes right-signed (eligibility raises the probability of a state effects themselves are not jointly the targeted expansions were successful sonogram in the first six statistically significant. in increasing early contacts months). However, the Thus, the evidence on whether with physicians is mixed. These data are unable to definitively resolve whether prenatal care did or did not rise under the targeted expansions. VI. DiscussioD "We use the predicted and Conclusions value of eligibility from the first stage linear probability model (individual regressed on state/year eligibility) directly in the second stage logit. This procedure consistent but not efficient, and our standard errors are somewhat under-stated as a result. eligibility 26 is A key question for health reform improvements in health. While healthy, whether covering the uninsured will actually lead number of a studies have surmount the problem health, they are generally unable to less is in the Medicaid eligibility of pregnant that the uninsured are in that the uninsured Our approach independent of insurance status." exogenous changes shown women to in the worse may be fundamentally problem this to 1980s. to is examine Judged by the most frequently used indicator of birth outcomes, the Medicaid expansions were a great success; infant mortality women was reduced by 7% for every eligible for Medicaid. relative to the value of a life limited, along low income at the effects little clinical sojdies of women life to obtain such care, or studies suggest. A have been reasonable, broad expansions of Medicaid We lives. eligibility to ail among needy were unable to resolve whether prenatal care fruitful direction for future research is women. (otherwise uninsured) under the targeted expansions was much higher than of prenatal care. 44 year old effea, primarily because they were not effectively translated into increased Medicaid coverage, even by to to of the Medicaid expansions suggests that their success First, the later appear to have had Second, the cost of saving a fraaion of 15 Moreover, the cost of the policy seems two dimensions. women rise in the or the cost of other government policies designed to save However, a closer look was 20 percentage point whether this that suggested was due to the failure simply not as cost effective as clinical would be to investigate more carefully, perhaps through additional case studies of targeted expansions, the utilization of different types of prenatal and hospital care in response to the increased availability of public insurance. Thus, our research offers two insights for the design of insurance policy. First, increased insurance eligibility can improve health outcomes, and the cost of doing so appears to be lower than '^ne study which does surmount this problem is that of Lurie et al. (1984), which finds that individuals (exogenously) terminated from Medicaid due to California budget cutbacks saw reductions in their self-reported health. 27 many estimates of the value of a effective is to ensure that the qualified for government newly Second, the crucial is moving making insurance policy Groups who have not previously programs may be particularly hard to to reach. Fortunately, address this problem (National Governor's Association, Several states have adopted public relations campaigns with themes such as Baby" (Utah) or "Baby Love" (North Carolina) In fact, in contrast to the findings et al. step in initial eligible takeup their benefits. social insurance public policy at the state level 1992). life. accompany expansions to from case study of Tennessee that in "Baby Your Medicaid eligibility. were discussed above, Buescher (1991) find that the North Carolina program had significant positive effects on the utilization of prenatal care and on birth outcomes. To the extent that informational problems are to blame, national health insurance of the type proposed by President Clinton takeup problem since there would be no question of would presumably surmount this eligibility. Another question which our research does not resolve effective in improving the health of other populations. is whether insurance policy Birth outcomes may will be be a particularly responsive margin to health interventions, relative to other medical problems later in life. It would be useful to extend the methodology developed here to explore the effect of exogenous changes insurance coverage on health at other points in the 28 life cycle. in Table ST 1: Eligibility by State over Time 1979 1986 Any Exp. Any Exp. Any Exp. Targeted Broad AL .146 .214 .342 .148 .194 AK .058 .187 .243 .216 .026 AR .123 .151 .307 .137 .169 CA .189 .252 .423 .271 .151 CO .095 .192 .236 107 .128 CT .154 .165 .253 .161 .091 DE .114 .114 .243 .092 .150 DC .286 .215 .454 .308 .145 FL .094 .133 .361 .170 .190 GA .090 .178 .280 .200 .079 HI .202 .179 .389 .522 .167 ID .095 .168 .300 .159 .141 IL .171 .186 .268 .181 .086 IN .081 .137 .300 .140 .159 lA .103 .165 .380 .136 .243 KS .117 .157 .293 .131 .161 KY .119 .154 .396 .210 .186 LA .164 .225 .391 .77.6 .164 ME .141 .200 .420 .222 .198 MD .137 .167 .350 .156 .194 MA .156 .165 .352 .209 .142 MI .173 .225 .390 .228 .161 MN .099 .209 .375 .184 .191 MS .111 .233 .567 .233 .334 MO .092 .155 .273 .109 .164 MT .165 .137 .334 .177 .157 NfE .133 .153 .233 .114 .118 NV .095 .088 .254 .123 .131 NH .096 .072 .184 .128 .055 1990 29 ST 1979 1986 Any Exp. Any Exp. Any Exp. Targeted Broad NJ .157 .149 .232 .157 .074 NM .110 .147 .347 .137 .210 NY .238 .242 .411 .257 .153 NC .106 .150 .364 .202 .162 ND .110 .134 .279 .146 .133 OH .131 .187 .278 .172 .105 OK .139 .162 .314 .198 .116 OR .161 .155 .264 .145 .119 PA .138 .164 .293 .182 .111 RI .197 .152 .352 .187 .164 SC .150 .228 .401 .160 .241 SD .110 .149 .277 .131 .146 TN .104 .162 .361 .216 .145 TX .079 .143 .318 .141 .176 UT .132 .255 .243 .140 .102 VT .228 .234 .396 .239 .157 VA .129 .245 .271 .136 .135 .170 .242 .262 .165 .097 .105 .215 .408 .206 .201 WI .126 .232 .271 .175 .096 WY .068 .140 .245 .127 .118 WA WV Notes: Figures are fractioo of 15-44 year old (columns 1,2, and 3), targeted 1990 womeo ID each state/year eligil)le for Medicaid under expansions only (column 4), and broad expansions only (column March 1980, 1987, and 1991 CPS. 30 5). ai Tabulated from Table Population Covered Under "Targeted" and "Broad" Expansions, CPS Data 2: Characteristics of the Characteristic Sample Targeted Expansions Expansions 38,403 18,775 22,164 (29,768) (27,676) (22,232) 24.9% 99.1% 38.5% Full Family Income Poor Number of Kids Broad 1.26 1.34 1.31 (1.26) (1.41) (1.39) 839.% 71.7% 80.9% 29.9 25.8 28.4 (8.35) (7.54) (7.67) Married 51.8% 12.7% 38.0% Working 74.7% 52.6% 72.4% 6.1% 26.2% 5.08% Uninsured 16.4% 30.1% 31.7% Employer-Provided HI 33.2% 6.91% 25.4% Medicaid 10.1% 37.6% 12.8% White Age Received Public Assistance N9t?§: Data from 1990 previous year; poor is saimple of CPS. Working is defined as working at least family income below poverty line for that family size. 31 Table 3: OLS Regressions of Low Birthweight and Infant Mortality on Eligibility Using VUai Suidstics Low DaU Each State and Year Tor Birthweight Infant Mortality Actual Simul. Actual Simul. Actual Simul Elig. Elig Elig Elig. Elig. Elig. Models Using Fraction Eligible Under Any Expansion Fraction ^.211 -7.431 -2.093 -3.458 -1.926 -3.171 Eligible (2.886) (3.848) (0.819) (1.090) (0.813) (1.085) Low Birthweight Intercept Adjusted R' 0.040 0.039 (0.012) (0.012) 74.29 75.25 9.162 9.571 6.206 6.662 (1.145) (1.371 (0.325) (0.388) (0.957) (0.990) .969 .969 .906 .906 .907 .908 Models Using Fraction Eligible Under Targeted Expansions Fraction -7.749 -15.37 -1.752 -3.989 -1.439 -3.391 Ehgible (4.123) (5.920) (1.176) (1.689) (1.170) (1.685) Low Birthweight Intercept Adjusted R^ 0.040 0.039 (0.012) (0.012) 74.13 75.49 8.814 9.201 5.821 6.267 (0.983) (1.226) (0.280) (0.350) (0.945) (0.984) .969 .969 .905 .906 .907 .907 Models Using Fraction Eligible Under Broad Expansions Fraction Eligible Low Adjusted R' : -1.451 -0.108 -0.336 -0.067 -0.232 (2.458) (6.178) (0.699) (1.757) (0.679) (1.706) Birthweight Intercept Notes -0.565 All regressions 0.072 0.072 (0.023) (0.023) 74.35 74.35 8.440 8.447 3.081 3.089 (1.406) (1.397) (0.400) (0.397) (1.743) (1.742) .981 .981 .910 .yi\j .910 .»iu .916 mcluded state expansion and targeted expansions; and N = y« iS^ Standard errors in parenth(leses. 2(X) for broad expansions. 32 .916 N = 600 for any a. ^-K £^1 O O o d C/5 ^^ ^-S O O d d O 9 d <^ 00 o 9 2, 00 - O d d « 2:1 i/3 o d O "5 5^ o 90 9 o o d O 9 o "1 </^ a 3 ? o £ 5" o 9d 90 90 9o o <::> d^ 9o ^ ^ U fa* u s o ^1 > 2, 3 — O 00 S3 S li od d d CD d 2— gSS 92, "1 f^ — o 90 — ^<N ""M — §g 2g z§ 2g 2 90 90 90 dd 9d £!fN 50 W-1 ? 3 -3 o u o 9 O S 9 d 9S 5i u e u w m O <N O £ >3 002- 8S So 98 2g =8 38 d d ^2°2' *'8- ^S ^S ^S '2- 5 — s. IT) O t .^1 1 ro (N u — u .SF — S8 O d d s a 2 o p>i d d 2-9 2- <N S? fn 98 S8 98 90 9 d 9 d vr — in r— t- 9 d d 9 o o d d ° 8 9 d ''^ iO . •Q ii •3 & 3 E "Sc^ ^=3 n f^ of- 98 00 9d dd 2 >-^ .,^^ i* H - !2 <^ ^ <^ •? o 98 28 = 8 9292- ''S- 9 d >»^ -..^ ^.ir 3 -3 :$ 2 II i u ^? •a 3 ^ s 9v QO t< d d 2 o _ 58 ^§ 88 o i Sid 9d 9d 9d 9 2, J58 <^ 8 o d d = § s 9 d _ V — * — o_ S8 S8 -8 S8 -8 98 08 do 9d 9d 9d ? 9- 2- 9 2 If— 31 d d "^S" fs -> p^i 3 — > a V s IT) p~ I i g 3 o 1 ^E 5 .2? |.S |S < b- ca 2* a- ._ ^ < V < O u 1 ! a ao E a ^ 2 ^ u. 2 * « •• u > 3 S 3 z Z ? Table 5: Medicaid Eligibility and Medicaid Payments: Evidence from HCFA Data Measure of Fraction Elig: Overall Eligibility Targeted Expansions Broad Expansions Actual Simulated .206 .232 (.077) (.102) .357 .449 (.110) (.156) .137 .262 (.154) (.187) Notes This table shows the coefficient on various Medicaid eligibility variables from regressions including year and state dummies. For example, the coefficient under "actual" in the targeted expansions row refers to the coefficient on the actual fraction made eligible under the targeted expansions. Standard errors in parentheses. Dependent variable is payments in thousands of : 1986 dollars per 15-44 year old woman. 34 \ i i "3 O r4 so r^ r^ CM — — O O — o <N — O O — O vn O in u 3 •J < p~ On SO rj in \0 in Pv| r^t r-1 r-i CM — O O z V 1 3 3 B« ^ 0\ (N ro 00 O O r- O — m — — o o •* o 1^ — u-i <N ro 00 CN oO m o 00 o irl > — o o NO fN 00 — o 00 — r-1 vO so m 00 — m vo <t — *"" SO — <N 00 rM CTv f<) ^ 5 OS 00 eN OO — •* (^ 00 — o On cm OS — r-i a s •s « § s *g 3 ZV e e _2 3 E m >n CM On <N <N ' SO 00 ss ^*^ ^"^ ^"^ f^ ss 1 '^-^ i a C ,^^ C^ >. "sS r~ •— 2 «N /— ^nm^ \0 00 S^ 00 ro <N 1/^ -^ < ^ 8 t« 1 E 3 — ,^_^ o oo in 00 •* so OS vn 00 m 1 NO r^ 00 Q — .^M^ r^ S^ r- :::S — * yrt O ^ oo 00 —* SO •* On iO 00 is 5 2S »n •la OS •^ "^ SO <s 00 <N oo m — 00 o NO (N 00 <N <N SO 00 m — — ^.^ V5 o ^ I ow o in t3 O r*> O oo OO — —O tr. u ^ (X </9 ka e 1> E 5 a 4J s C/3 fl w 4) E eted M £? :^ W H ca «J k> u <i ?3 e 25 ^ U iZ 1/1 c "3 o is ii o 19 it s< a. 1/1 o & u. < rO —o — — — 00 o vO «0 00 4> a> 00 iri o c V5 VO e o >n r- so 00 — O — vO — r— o o —_ oo o m 00 VO C « 2 -s o 00 in >/^ rvi "O CM fM IT) S 4) 2 E .£ W) 00 so 3 o =s ^2 O^ 30 — — 00 2 (N oo 3 00 o W-> = s l| o .£ 00 o m t/5 s« g-a Ov 00 s — o ON S — O "8 Hi o 00 r~ 00 2o c VO 4> E o (?v 00 — 2 i' o 00 — 25w <»• 00 r— O IT) ^ 1 IT) vO «^ w' ' s Se to r- S r- 00 SO >> VO 5 '•5 00 <o IT) <N 00 — r-, oo O O ^ 00 — p = P <N < r» 00 — •^ oo pp 946 3813 U 3 S,s 00 9> 00 •<« c 4> Income e 4> s s ^ 1 E S o 8 Tf R 1 > o a. lember Du Du Age unple rban Poverty 2 §^ = 2 S * I >» » o 1s « -S 00 o tI 8^ 1 o E >> c i2 •= 00 1 Q o ;;o 3 ear ?3 s > ate ca o— 00 .-5 21 (N 4> III 4> E E 3 3 zz wj 4> <3 U ^ 4) 113 ^ .3 u] 1985 year Figure ID: Low Birthweignt in the 1980s 35 9 1 u S J 3 i - 1 -T T 25 / - / / / 2 / - 15 ^ 1 ^^-"^ 979 Figure 1982 2a: 1985 year 1988 1990 Medicaid EligiDility Trends c "T in 6 - 10 u .5 - 4 - 1979 Figure 2a: Medicaid EligiDility Trends for <2>^Poverrv References Alan Guttmacher Institute. The Financing of Matemitv Care in the United States . New York: AGI, 1987. American Public Welfare Association. "Voluntary Contributions and Provider-Specific Taxes: Survey Results". Washington, D.C.: APWA, 1991. Buehler, J.W., J. Kleinman, and C. Hogue. "Birth Weight-Specific Infant Mortality, U.S., 1960 and 102 #2, 1985, 3564-3567. 1980," Public Health Reports Buescher, et al. Outcomes . "An Evaluation of in the Impaa of Maternity Care Coordination on Medicaid Birth North Carolina," American Journal of Public Health Blank, Rebecca and David Card. "Recent Trends of Eligibility Is There an November 1991, 1157-1190. "When Do Women Use vs. Participation," 81, 1991, 1625-1629. Insured and Uninsured Unemployment: in Explanation?," Quarterly Journal of Economics 106, Blank, Rebecca and Patricia Ruggles. . AFDC & Food Stamps? The Dynamics mimeo, July 1993. Braveman, Paula, et al. "Adverse Outcomes and Lack of Health Insurance Among Newborns in an EightCounty Area of California, 1982 to 1986," The New England Journal of Medicine 321 #8, August 24, 1989.508-513. . Buehler, J.W., J. Kleinman, C. Hogue. "Birth Weight-Specific Infant Mortality, United States, 1960 and 1980," Public Health Reports 102 Kl, 1985, 3564-3567. Chaikind, Stephen and Hope Corman. "The Special Education Costs of Low Birthweight, " NBER Working Paper #3461, October 1990. Children's Defense Fund. The Deficit Reduaion Act of 1984 . Washington, D.C.: Children's Defense Fund. 1984. Creasy, R.K., B.A. Gummer, and G.C. Obstetrics and Gynecology . Liggins, "System in Predicting Spontaneous Preterm Birth," 6, 1980, 692ff. Corman. Hope, Theodore Joyce, and Michael Grossman. United States', Journal of Human Resources 22, . "Birth Summer Outcome Produaion functions in the 1987, 339-360. "Environmental Economics: Cropper, Maureen L., and Wallace E. Oates. 675-740. Economic Literature 30, June 1992, A Survey," Journal of . Cropper, Maureen L. et al. . "The Determinant of Pesticide Regulation: Decision-Making," Journal of Political Economy . Statistical Nancy Cole. "Welfare and Child Health: The Link Between AFDC Weight," The American Economic Review 283 #3, September 1993. Currie, Janet and Birth A . 37 Analysis of EPA 100, 1992, 175-197. Participation and . "Weighing the Evidence: An Empirical Analysis of the Expansions of Medicaid Coverage for Pregnant Women, 1984-1990". Thesis, Harvard College, 1992. Fischer, Michael. Donna Frank, Richard, Storbino, David Salkever, Catherine Jackson. "Updated Estimates of the Impact of Prenatal Care on Birthweight Outcomes by Race," NBER Working Paper #3624, February 1991 Gold, Rachel, Susheela Singh and Jennifer Frost. "The Medicaid Eligibility Expansions for Pregnant Women: Evaluating the Strength of State Implementation Efforts", Familv Planning Perspeaives 25 M5, September/October 1993, 196-207. . Government Accounting Medicaid Expansions: Coverage Improves but State Fiscal Problems Washington, D.C.: GAO, June 1991. Office. Jeopardize Continued Progress . Graham, John D., and James W. Vaupel. Analvsis 1 . "Value of a Life: What Difference Does Make?," Risk it #1, 1981,89-95. Grossman, Michael, and Steven Jacobowitz. "Variations In Infant Mortality Rates Among Counties of the United States: The Roles of Public Policies and Programs," Demography 18, November 1981, . 695-713. Grossman, Michael and Theodore Joyce. "Unobservables, Pregnancy Resolutions and Birth Weight Production Functions in New York City," Journal of Political Economy 98 #5, October 1990, 983. 1007. Gruber, Jonathan. "The Effect of Price Shopping in Medical Markets: Hospital Responses "Canadian National Health Insurance and Infant Health". Hanratty, Maria. to PPOs in Economics California," forthcoming. Journal of Health Mimeo, Cornell University, 1992. Harris, Jeffrey. of Health "Prenatal Medical Care and Infant Mortality," in Victor Fuchs, ed.. . Chicago: University of Chicago Press, 1982. Health Care Financing Administration. D.C.: HCFA, Analvsis of ,< ?taTt Mg^i?"d Program Characteristics Hill, Ian. fft at Hill, Ian. . . Washington, 1982, 1983, 1984. Health Insurance Association of America. The Cost of Maternity Care and Childb irth 1989 Economic Aspects in the United States. Washington, D.C.: HIAA, 1990. Medicaid Eligibilitv: ? P?';P"Pfft1^ A Descriptive Report of OBRA. TEFRA. and DEFRA Provisions, and Washington, D.C.: National Governors Association, 1985. Broadening Medicaid Coverage of Pregnant Women and Children: State Policy Responses. Washington, D.C.: National Governors Association, 1987. Horbar, Jeffrey, Elizabeth Wright, Lynn Onstad et al., 38 "Decreasing Mortality Associated with the Introduction of Surfactant Therapy: Grams Hutchens, at Birth," Pediatrics . tfl, An Observational Study of Neonates Weighing 601 to 1300 August 1993, 191-196. "AFDC and the Birthweight . Washington D.C.: National Academy George Jakubson, and Saul Schwartz (1989). Robert, Subfamilies," Journal of Institute 92 Human of Medicine, Preventing Low Formation of Resources 24, 1989, 599-628. . Press, 1985. "Major Changes in State Medicaid and Indigent Care Programs ". Washington, D.C.: The George Washington University, various years. Intergovernmental Health Policy Projea. Eds. Debra J. Lipson et al. Manning, Williard G. et al. "The Taxes of Sin: Do Smokers and Drinkers Pay Their Way?," Journal of the American Medical Association 261 #11, March 17, 1989, 1604-1609. . McCormick, Barbara, at "The Health and Developmental Status of Very-Low-Birthweight Children School Age," Journal of the American Medical Association 267, 1992. et al., . "A Quasi-Experimental Approach Working Paper #3159, 1989. Meyer, Bruce. "Incentive Effects of the U.S. Robert. Moffitt, Literature . 30, March 1992, to die Effects of Welfare System: A NBER Review," Journal of Economic 1-61. Piper, J.M. et al. "Effects of Medicaid Eligibility Expansion in Unemployment Insurance," on Prenatal Care and Pregnancy Outcomes Tennessee," Journal of the American Medical Association . 264, 1990, 2219-2223. Rosenzweig. Mark and T. Paul Schultz. "The Behavior of Mothers as Inputs to Child Health: The Determinants of Birth Weight, Gestation, and Rate of Fetal Growth," in Economic Aspects of Health . Victor Fuchs (ed). University of Chicago Press: Chicago, 1982. Rosenzweig, Mark and T. Paul Schultz. "Estimating a Household Production Function: Heterogeneity, the Demand for Health Inputs, and Their Effects on Birth Weight," Journal of Political Economy . 91, October 1983, 723-746. Rosenzweig, Mark and T. Replication," Paul Schultz. "The Stability The Journal of Human Resources . Produaion Technology, of Household A 23, Fall 1988, 535-549. Rymer, Marilyn and Gerald Adler. "Children and Medicaid: The Experience Financing Review 9#1, Fall 1987, 1-20. in Four States," Health Care . Saywell, et al. "Hospital and Patient Characteristics Implications," Journal of Health Politics. Policv. and of Uncompensated Uw . Hospital Care: Policy 14, 1989, 287-307. Schwartz, Rachel. "What Price Prematurity," Familv Planning Perspectives 21, July/August 1989, 170. 174. 39 U.S. Department of Health and to Familiea U.S. Human Services (various years). With Dependent Children . Washington, D.C.: Characteristics of State Plans for Aid US DHHS. House of Representatives, Green Book 1992: Background Mate rial on Programs Under Jurisdiction of the Committee on Wavs and Means Washington D.C.: GPO, 1992 the . U.S. Office of Technology Assessment. Washington, D.C.: GPO, 1987a. Healthv Children: Investing in the Funire . OTA-H-344, U.S. Office of Technology Assessment. Neonatal Intensive Care for Low Birthweight Infants: Costs and Effectiveness . OTA-HCS-38, Washington, D.C.: GPO, 1987b. Viscusi, Kip. Weitz, Judith. FrltH l T^? '\ ^^^} New York: Oxford University Press, 1992. Testimony before House of Representatives on DEFRA (PL 98-369), 1983. Yelowitz, Aaron. "The Medicaid Notch, Labor Supply and Welfare Participation: Evidence from Eligibility Expansions," MIT mimeo, July 1993. 40 Appendix: Eligibility Simuiatioas During the entire period studied, 1979-90, the fundamental basis for eligibility for Medicaid was AFDC. The core of our eligibility calculation was therefore a simulation of eligibility for welfare receipt. In order to qualify for AFDC, a family must pass three tests: their gross income must be below a multiple of the state's needs standard (this test was applied from 1982 onwards only);" their gross income less certain disregards for work expenses and child care must be below the state's needs standard; and their gross income less certain disregards less a portion of their earnings must be below the state's payment standard. receipt of The exaa definition of a family unit is the first source of difficulty in making this calculation. If minor (which we define as less than age 19) is living with her parents, then a ponion of the parents' a income is deemed to that individual in making the eligibility calculation. This fraction is calculated by subtracting from family income the needs standard for a family of that size. If the individual is age 19 or above, then the treatment of family resources is less clear, and varies across states; see Hutchens et al. (1989) for a description of these differing treatments. We assume, following the praaice of the majority of the states, that the parent's resources are ignored Before OBRA Before OBRA if the individual is not a minor. was no standardized allowance for work and child care expenses under AFDC. Beginning in October 1981, the allowance was standardized to be $75 per month for work expenses, and a maximum of $160 per child for child care costs. This was not changed until the Family Support Act of 1988, which raised the allowances to $90 for work expenses and $175 per child for child care, effective October, 1989. For years before 1982, we assume that states allowed the same level of disregards as was designated under OBRA. '81, there '81 , there was a work incentive feature of AFDC known as "30 and one-third" . This $30 of earned income, and one third of die remainder, while Since individuals must qualify for an AFDC payment in order to receive Medicaid, this meant that the individual's income, less disregards, and less $30 and onethird, was compared to the payment standard for the third test described above. From 1982 to 1984, this incentive was limited to the first four nwnths that individuals were on AFEKD. In order to model this, we assume that for our sample it is their first full year on AFDC, so that they get $120 and 1/9 of their earnings for the year. From 1985 onwards, individuals who would have lost Medicaid due to the end of the $30 and 1/3 rule after 4 months were allowed to remain on Medicaid for an additional 9 to 15 months (the length was at state discretion). We modelled this as amounting to a fiill 30 and 1/3 exclusion after 1984, parallel to the pre-1982 rules. Our objea was to consistently nnodel die maximum amount that an incentive allowed families to keep the first the other two-thirds led to reduced AFDC individual could have received under F'mally, a key restriction benefits. AFDC. on the receipt of AFDC is family structure. In all states, single women one child are eligible. In addition, in some states, married women with an unemployed spouse Eligibility for AFDC-UP conditions on both current are eligible under the "AFDC-UP" program. employment status and work history. Lacking longitudinal data on work histories, we assume that families are eligible if the state has a program and the spouse had worked less dian 40 weeks in die previous year. with at least "From 1982 to 1984, this multiple was 1.5; ft-om 41 1985 onwards, die multiple was 1.85. Since families eligible for AFDC-UP malce up only a small fraction of the overall AFDC population, this should not greatly affea our estimates For most Medicaid recipients, AFDC receipt summarizes the necessary conditions for Medicaid However, from the inception of the program, there have been a number of special options, to be used at state discretion, which allow further means of eligibility for certain populations, and, in eligibility. particular, for pregnant The who first women. mothers who are pregnant for the first time, Before 1982, a number of states had first-time pregnancy programs, which covered women from some point in their pregnancy even if of these are state programs are therefore not yet eligible for options under their ATOC they had no other children. although some states the first trimester. most women were covered ftx)m the point of medical verification, later point; we only counted those states that covered women during Generally, covered them In to cover single AFDC. at a states, the states counted only the nwther in the family unit size (i.e. the size of the family was one), although a few states counted the future child as well. The states which had these programs are identified in U.S. Department of Health and Human Services (various years). After OBRA '81, states with these programs were no longer allowed to cover women before the month of pregnancy. However, states were offered the option of deeming first-time pregnant women eligible for Medicaid from the moment of verification, even though AFDC payments had not yet begun to flow. As with most Medicaid-only options, information about which states took up this c^nion is spotty and often contradictory. Based on information in Health Care Fmancing Administration (1982,1983,1984), Weitz (1983), and Hill (1985, 1987), we came up mAi a list of states which appeared to have taken up this option in each year. We also assumed that, under this program, states did not count the unborn child in sixth determining the size of the assistance unit. Under DEFRA which was effective from 1985 onwards, states were required to cover "a eligible for Aid to Families with Dependent Children ... as if her child had bom was living with been and her ..., [ifl such pregnancy has been medically verified' (P.L. 98-369, Sec. 2361, Subtitle B). Thus, first-time pregnant women are covered in all states frx>m 1985 onwards, and the effective family size for AFDC receipt is increased by one for all pregnant women. pregnant '84, woman who would Another unportant would qualify for AFDC structure (ie. children in of such children (ie. be state Medicaid option is coverage of 'Ribicoff children", under income considerations alone, but poor two-parent families). Before 1981, only those In institutions, only those in who would states could who are children who not qualify due to family cover selected categories two-parent families, etc.), or all categories, up to age 21 From 1982 onwards, they were also offered the option of restricting die coverage of children between 18 and 21 years of age. Thus, for teens in our sample in states with comprehensive Ribicoff children programs, we ignored tbe family structure requirements of AFDC and only screened on . income.** which took up die Ribicoff option to cover poor children in two-parent families. However, the data on this program are spotty, and this category is never presented. Thus, we only included those states which were listed as having programs that The data on this program are from HCFA covered all categories of Ribicoff children. **In theory, we should do this for any state 42 Furthermore, although OBRA '81 restricted the AFDC coverage of unborn children, states were given the option of covering unborn children under their Ribicoff children programs. This amounted to covering pregnant women whose income qualified them for AFDC, regardless of family structure. We HCFA gathered information on this Ribicoff option from modelled it as being in place (1982,1983, 1984) and from Weitz (1983), and from 1982 onwards. Medicaid program, states have had the option of covering them for AFbc but who were not single mothers. This little In addition, since the inception of the all women whose income pregnant ioiown option is only discussed qualified Weitz (1983), Children's Defense Fund (1984), and in Hill (1987); the last of these sources gives the dates of the inception of these programs. Each of the three options restrictions for pregnant women) just listed (Ribicoff teens, Ribicoff unborn, and no family structure apply only to the pregnant women herself, or only to her unborn child, would be one. However, we assumed that had more than one of these programs, the family unit size was increased by the future child. so the family unit size (for example) for a fu"st time pregnancy when states Needy program, which is designed to cover individuals who meet the family structure requirements for AFDC and whose gross resources are above AFDC levels, but whose high medical expenditures bring their net resources below some certain minimal level. States who take up this option may establish Medically Needy thresholds that are no more than 133% of the state's AFDC needs standard. Individuals can then 'spend down' to these thresholds by subtracting their medical expenditures from their gross income; if they do, Medicaid will pay the remainder The fmal state option of importance is the Medically of their expenditures." While this program may be whose income is somewhat above option First, is we quite useful for covering the birth expenditures of a pregnant the it is We unclear how important the Medically Needy therefore model this program in two ways. is, this program women whose gross incomes are between the AFDC threshold Second, we subtraa from gross income the expected global fee for pay for the medical costs of and the Medically Needy threshold. an obstetrician, itom Alan Guttmacher pregnant mother for their global fee qualify for the Medically former cutoff, simply compare the woman's net income to the Medically Needy threshold; that will help to bill to AFDC for covering her prenatal care expenditures. woman Institute (1987).^ The notion here at the first prenatal care visit, Needy program. Since is that, if obstetricians bill the then the mother will be able to use this the measures were very similar, we only used the in the analysis. Beginning with DEFRA '84, the Federal government began a series of mandates which extended (1982,1983,1984) and Hill (1987). "The model time frame over which such spend-down occurs varies across the states, and we do not it. **The global fee natal care. is the bill for all obstetric services, including pre-natal care, delivery, and post- This fee averaged $830 in 1986, and physician's services component of the Consumer is deflated (and inflated) to other years using the Price Index. 43 DEFRA '84 txKiuded two features: mandatory coverage of above), and mandatory coverage of pregnant women in AFDCwomen under AFbC (described type families, even if the state did not have an AFDC-UP program. COBRA '85 then mandated that the Medicaid covenfe of prefnant women. pregnant UP women who met the AFDC resource standards were eligible regardless of family structure (similar This law was effective in July, 1986. Since we are focusing to the state programs described above). pregnant primarily on the effect of Medicaid on early prenatal care, we model this law as being effective from 1987 onwards. Beginning with OBRA '86, states were given the option, and then mandated regardless of family structure. OBRA '86 gave flrst to, increase the income thresholds for Medicaid eligibility, states the option women up to 100% of the poverty threshold, beginning in April, 1987. OBRA '87 increased that optional level to 185% of poverty. Under the Medicare Catastrophic Care Act states were of covering pregnant mandated to cover pregnant required to cover women up women up to 133% to 75% Then under OBRA '89, they were 1990. Using data from Government Accounting of poverty by July of poverty by April, 1. Office (1991), Fischer (1992), and Intergovernmental Health Policy Project (various years), we modelled women was covered as being covered if their income was below the average percentage of poverty during the year. 44 that k dS6 5 7 MIT LIBRARIES 3 ^DflD D0a4bS^3 T Date Due ^t. 1 WW MAY Lib-26-67