Exposure Control Plan for Bloodborne
advertisement

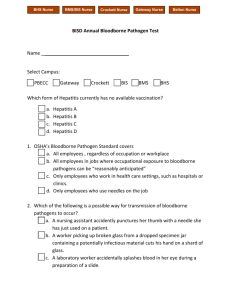
Ohio Northern University Exposure Control Plan for Bloodborne Pathogens 9/23/2014 9:36:37 AM 1 THE OSHA BLOODBORNE PATHOGENS STANDARD: SUMMARY The OSHA "Occupational Exposure to Bloodborne Pathogens" (29 CFR Part1910.1030) is applicable to employees with exposures to blood and other potentially infectious materials. The standard defines an "occupational exposure" as reasonably anticipated skin, eye, mucous membrane, or parenteral contact with blood or other potentially infectious materials that may result from the performance of an employee's duties. "Other potentially infectious materials"* include semen, vaginal secretions, cerebrospinal fluid, pleural fluid, pericardial fluid, peritoneal fluid, amniotic fluid, saliva, any body fluid that is visibly contaminated with blood, unfixed human tissue or organs, and cell cultures containing HIV or HBV. A summary of the OSHA standard, found in the Code of Federal Regulations (29CFR) 1910.1030, is appended to this plan but summarized below. Employers must write an Exposure Control Plan designed to eliminate or minimize employee exposures and must provide a copy to covered employees. Employers must identify job classifications in which employees have occupational exposures. Standard Precautions are to be utilized in the handling of blood or other potential infectious materials. Engineering and work practice controls and personal protective equipment are to be used to eliminate or minimize employee exposures. Hepatitis B vaccine is to be offered to all employees with occupational exposures. Post-exposure medical evaluation and follow-up is to be provided for employees with occupational exposures; Annual training must be provided for all employees with occupational exposures. *CDC and OSHA do not list the following body fluids as HIV/Hepatitis B transmission sources unless they contain blood: urine, feces, vomit, tears, sputum, sweat, or nasal secretions. Other materials may be sources: any unfixed tissue or organ, other than intact skin from a human, living or dead; HIV/Hepatitis B containing cell or tissue cultures, organ cultures and culture media; blood, organs or other tissues from experimental animals infected with HIV, Hepatitis B, or other bloodborne pathogen. 9/23/2014 9:36:37 AM 2 I. Purpose and Scope This Exposure Control Plan is established by Ohio Northern University (ONU) to document the procedures intended to eliminate or minimize, and to prevent, when possible, the exposure of ONU employees and students to disease-causing pathogens that may be transmitted through human blood and certain body fluids, in accordance with the Occupational Safety and Health Administration’s Bloodborne Pathogens Standard, 29 CFR 1910.1030. The exposure control plan is a key document to assist the University in implementing and ensuring compliance with the OSHA bloodborne pathogen (BBP) standard, thereby underscoring the University’s commitment to providing a safe and healthful work environment for all personnel. The purpose of the Bloodborne Pathogens Standard is to reduce the potential of occupational transmission of potentially infectious body fluids caused by microorganisms sometimes found in human blood and certain other potentially infectious body fluids and/or tissues. The OSHA Standard, found in the Code of Federal Regulations (29CFR) 1910.1030, is appended to this plan. This plan covers all ONU employees and students who may be exposed to blood and other potentially infectious materials (OPIM) during the performance of their job duties and/or during school-associated activities. It is expected that all elements of this plan will be adhered to by all employees and students of the University. This ECP includes: Determination of exposure Implementation of methods of exposure control, including: o Standard precautions o Engineering and work practice controls o Personal protective equipment o Housekeeping Hepatitis B vaccination Post-exposure and follow-up Communication of hazards to employees and students, and training Recordkeeping Procedures for evaluating circumstances surrounding exposure incidents Implementation of this standard is discussed in the subsequent pages of this ECP. 9/23/2014 9:36:37 AM 3 II. Glossary of Terms and Abbreviations 1. AIDS – acquired immunodeficiency syndrome. 2. Blood - human blood, human blood components, and products made from human blood. 3. Bloodborne Pathogens (BBP) – pathogenic micro-organisms that are present in human blood and can cause disease in humans. These pathogens include, but are not limited to, Hepatitis B (HBV) and Human Immunodeficiency Virus (HIV). 4. BPS – Bloodborne pathogen standard. 5. BSC – Biosafety Committee 6. CDC – Centers for Disease Control 7. CLS – Clinical Laboratory Science 8. Contaminated – the presence or the reasonably anticipated presence of blood or other potentially infectious materials on an item or surface. 9. Decontamination – the use of physical or chemical means to remove, inactivate or destroy bloodborne pathogens on a surface or item to the point where they are no longer capable of transmitting infectious particles and the surface or item is rendered safe for handling, use or disposal. 10. ECP – Exposure control plan 11. Engineering Controls – methods, equipment, and/ or procedures that isolate or remove the bloodborne pathogens hazard from the workplace. 12. Exposure Incident - a specific eye, mouth, other mucous membrane, non-intact skin, or parenteral contact with blood or other potentially infectious materials that results from the performance of an employee's duties. 13. HBV – Hepatitis B Virus 14. HCV – Hepatitis C Virus 15. HIV – Human Immunodeficiency Virus 16. IRB – Institutional Review Board 17. Licensed Healthcare Professional - a person whose legally permitted scope of practice allows him or her to independently perform the activities required by paragraph (f) Hepatitis B Vaccination and Post-exposure Evaluation and Follow-up. 18. NIOSH – National Institute for Occupational Safety and Health 19. Occupational Exposure - reasonably anticipated skin, eye, mucous membrane, or parenteral contact with blood or other potentially infectious materials that may result from the performance of an employee's duties. 20. Other Potentially Infectious Materials (OPIM) - (1) The following human body fluids: semen, vaginal secretions, cerebrospinal fluid, synovial fluid, pleural fluid, pericardial fluid, peritoneal fluid, amniotic fluid, saliva in dental procedures, any body fluid that is visibly contaminated with blood, and all body fluids in situations where it is difficult or impossible to differentiate between body fluids; (2) Any unfixed tissue or organ (other than intact skin) from a human (living or dead); and (3) HIV-containing cell or tissue cultures, organ cultures, and HIV- or HBV-containing culture medium or other solutions; and blood, organs, or other tissues from experimental animals infected with HIV or HBV. 21. OSHA – Occupational Safety and Health Administration 22. Parenteral – piercing mucous membranes or the skin barrier through such events as needlesticks, human bites, cuts and abrasions. 9/23/2014 9:36:37 AM 4 23. PHS – Public Health Service 24. Personal Protective Equipment - specialized clothing and/ or equipment worn by an employee for protection against a hazard. General work clothes (e.g., uniforms, pants, shirts or blouses) not intended to function as protection against a hazard and are not considered to be personal protective equipment. 25. Regulated Waste - liquids or semi-solid blood or other potentially infectious material; or contaminated items that would release blood or other potentially infectious material in a liquid or semi-liquid state if compressed; or items that are caked with dried blood or other potentially infectious material and are capable of leaking this material during handling. 26. Sharps – any contaminated object that can penetrate the skin, including but not limited to needles, scalpels, scissors, blades, broken glass, and broken capillary tubes. 27. Source Individual - any individual, living or dead, whose blood or other potentially infectious materials may be a source of occupational exposure to the employee. Examples include, but are not limited to, hospital and clinic patients; clients in institutions for the developmentally disabled; trauma victims; clients of drug and alcohol treatment facilities; residents of hospices and nursing homes; human remains; and individuals who donate or sell blood or blood components. 28. Standard Precautions – an approach to infection control in which all human blood and certain human body fluids are treated as if known to be infectious for HIV, Hepatitis B and other bloodborne pathogens. 29. Work Practice Controls – methods or procedures that reduce the likelihood of exposure by altering the manner in which a task is performed, i.e., wearing gloves, eye wear, etc. 9/23/2014 9:36:37 AM 5 III. Program Management Institutional Biosafety Committee Certain activities within the University have the potential for employee and student exposure to human blood and body fluids which may be sources of harmful and potentially lethal diseases. To provide oversight for work and school-related activities in these areas, the University has established an Institutional Biosafety Committee (IBC), a standing subcommittee of the University Safety Committee. The biosafety committee is comprised of the following individuals, appointed by the VP of Academic Affairs: A. Exposure Control Coordinator/Biosafety Committee Chair (Biosafety Officer); Human Resources Director or designee; Institutional Review Board Chairman; Representative(s) of Biological & Allied Health Sciences Representative of Student Affairs; Representative of the College of Pharmacy; Representative of University Security; and Representative of Physical Plant. Community Member Community Member The committee is charged with the following responsibilities: 1. Recommend policies to university administration that promote a healthful and safe work environment; and 2. Serve as a resource and advise the university safety committee and the institutional review board (IRB) regarding biosafety issues. B. The ECP will be reviewed and/ or updated: (a) annually, (b) whenever new or modified tasks and procedures are implemented which affect employee exposure, (c) whenever changes in technology eliminate or reduce employee exposure to bloodborne pathogens, and (d) whenever employees’ jobs are revised to include new tasks in which exposure may occur. The reviews are performed by the BSC. C. The annual review is intended to ensure that the ECP accurately reflects current federal and state regulations, and applicable CDC and PHS and guidelines. 9/23/2014 9:36:37 AM 6 Plan Coordinator A. The coordinator is charged with the following responsibilities: 1. Implementing the ECP; 2. Providing ECP training for all employees determined to have occupational exposure to blood or OPIM as follows: a. b. c. d. e. f. g. h. i. Initial training provided within two (2) weeks of employment or reassignment to a job having potential exposure; Annual training for all employees whose job position places them at risk of potential exposure; Documenting training, providing the human resources office with training documentation, and making the written ECP available for distribution to the university, OSHA and NIOSH representatives, and others as may be required to comply with the standard; Working with employees to develop and administer appropriate training of students whose campus activities places them at risk of potential BBP exposure; Working with the biosafety committee, university administration, employees, and other agencies to develop and administer any additional policies and practices related to bloodborne pathogens, including those specified by the Needlestick and Prevention Act; Maintaining and updating the ECP at least annually and as required by the BCP; Representing the University during inspections and campus events requiring input regarding biosafety; Conducting periodic facility audits to identify the need for changes in engineering and work practice controls and to maintain an up-to-date ECP. Reviewing the circumstances of all exposure incidents and maintaining a log of injuries resulting from occupational exposures to bloodborne pathogens, including sharps incidents. Human Resources A. The Human Resources Director or designee is responsible for: 1. Ensuring that all medical actions and training required by the standard are performed and that appropriate employee health and training records are maintained; 2. Distributing the ECP to University Administration, Services, Employees (full-time, part-time, temporary, contract, per diem, and appointed), and Academic Departments as required by the ECP; 3. Scheduling training required by the ECP with the Plan Coordinator; 4. Notifying employees of scheduled training. 9/23/2014 9:36:37 AM 7 University Administration, Directors, Managers, Supervisors, Division and Department Chairs A. University Administration, Directors, Managers, Supervisors, Division and Department Chairs are responsible for: 1. Implementing established policies and procedures regarding exposure control in their respective areas. They work directly with employees to ensure that proper exposure control procedures are followed. 2. Ensuring that all new employees receive education and/or training with respect to the requirements of the ECP. 3. Annually sending a list of all employees who need training to the Office of Human Resources. Employees A. Individual employees are key to successful implementation of the ECP. All employees who are determined to have occupational exposure to blood and OPIM are to comply with the procedures and work practices in the ECP. This includes but is not limited to: 1. Identifying which job tasks have potential for occupational exposure to blood, body fluids or tissues; 2. Attending initial and annual training; 3. Routinely and consistently following safe work practices as defined by the ECP to prevent exposure; 4. Practicing good personal hygiene habits without exception; 5. Immediately reporting all exposure incidents and sharp injuries to their supervisor to assure documentation and treatment; 6. Discussing all concerns regarding the ECP with their supervisor. 7. Participating in opportunities to identify and select safer devices to use as defined by the Needlestick and Prevention Act. IV. Exposure Determination A. All job categories where it is reasonable to anticipate that an employee may have mucous membrane or parenteral contact with blood or other body fluids (those listed below), are included in this ECP. Exposure determination is made without regard to the use of PPE. Blood and Blood Products (e.g., plasma, serum, red cells, white cells, and platelets) Cerebrospinal Fluid Serous Fluid (Pleural, Pericardial, and/ or Peritoneal) Synovial Fluid Amniotic Fluid 9/23/2014 9:36:37 AM 8 Semen Saliva Vaginal Secretions Any body fluid visibly contaminated with blood Other potentially infectious materials as defined by CDC B. OSHA standard 1910.1030 refers only to employees; however, the ONU ECP by design includes students who are at risk of exposure due to their campus activities including studies. These individuals are to receive appropriate instruction through the academic department supervising their educational programs or work. All other employees, with the exception of those listed below, have no expectation of occupational exposure to blood or other potentially infectious body fluids. 1. The following is a list of all job classifications at ONU in which employees (Fulltime, part-time, contract, and appointed) have anticipated occupational exposure. a. b. c. d. Physician Nurse Phlebotomist First aid responders who are: 1) 2) 3) 4) Security Officers Athletic Trainers Life Guards Safety Officers e. Faculty and staff who are involved in academic programs in clinical laboratory sciences, forensic science, nursing, pharmacy, and pre-professional areas. 2. The following is a list of job classifications in which some employees have possible occupational exposure. Job classification Tasks with occupational exposure Faculty/Non-faculty staff collecting blood samples or OPIM, processing unfixed tissues and blood specimens, antibody screening of blood specimens, separation of blood components, performing analytical tests on human blood and/ or blood components, and unfixed tissues, resolution of emergency/injury or illness incident 9/23/2014 9:36:37 AM 9 Lab or animal technician handling HBV and/ or HIV infected specimens and/ or animals, collecting blood samples or OPIM, processing unfixed tissues and blood specimens, separation of blood components, setting up labs in which human blood and/ or blood components, and unfixed tissues are tested, resolution of emergency/injury or illness incident Laboratory manager handles unfixed tissues and blood specimens, resolution of emergency/injury or illness incident Coach student athlete instruction, resolution of emergency/injury or illness incident Plumber Job classification repairing plumbing/ drains across campus, resolution of emergency/injury or illness incident Tasks with occupational exposure Groundskeeper resolving personal injury/illness incident Carpenter repairing facility structures across campus, resolution of emergency/injury or illness incident General Maintenance Worker making repairs and performing duties across campus, resolution of emergency/injury or illness incident Housekeeper cleaning restrooms, collecting and transporting sharps and medical waste containers, resolution of emergency/injury or illness incident Secretary or Mail Clerk delivering blood/tissue-containing packages, resolution of emergency/injury or illness incident Resident Assistant resolution of emergency/injury or illness incident V. Methods of Implementation and Exposure Control ONU has an exposure control plan and employees covered by the bloodborne pathogens standard receive an explanation of the ECP during their initial training. It is also reviewed in their annual refresher training. All employees can review this plan at any time during their work by contacting the Human Resources Office or the ECP coordinator. 9/23/2014 9:36:37 AM 10 A. Standard Precautions CDC isolation guidelines defines standard precautions as an approach to infection control in which all human blood specimens, blood contaminated body fluids, or materials are treated as if known to be infectious for HIV, HBV, and other bloodborne pathogens. Standard Precautions may include the following practices: Wear gloves, masks and protective eyewear Wear protective suits, gowns or aprons Wash hands and other skin surfaces Disinfect all contaminated surfaces Use proper disposal Use protective resuscitation masks for CPR Use safety devices to prevent occupational exposure via sharps (needles, blades, etc.) B. Standard precautions are to be observed by all employees to prevent contact with blood and/ or OPIM. Under circumstances in which differentiation between body fluids types is difficult or impossible, all body fluids shall be considered potentially infectious materials. C. Standard precautions are intended to prevent exposure to human blood and/or OPIM. The routes of transmission for occupational exposure are: 1. puncture of the skin with contaminated sharp objects 2. contact with broken skin 3. splash to mucous membranes of the eye, nose and/or mouth D. Specific precautions are described below. Engineering and Work Practice Controls – are used to eliminate or minimize employee exposure to bloodborne pathogens. Sharps and biohazard waste containers are inspected, maintained, or replaced as needed by primary users to prevent overfilling. Containers are available by contacting the manager of the university warehouse (extension 2580). Specific engineering controls and work practices used are listed below: 1. Hand washing - hands and any other contaminated skin are to be washed with soap and water, and mucous membranes flushed with water immediately following contact of such body areas with blood or OPIM. Employees shall familiarize themselves with the nearest hand washing facilities for the buildings in which they work. Because most ONU buildings are public access, they will have available hand washing facilities in public restrooms and custodial / janitorial closets. (If hand washing facilities are not available, housekeeping will provide either an antiseptic cleanser in conjunction with clean cloth/paper towels or antiseptic towelettes. If these 9/23/2014 9:36:37 AM 11 alternatives are used, then the hands are to be washed with soap and water as soon as feasible.) 2. Use of waste disposal containers: contaminated sharps e.g., (needles, lancets, and scalpels etc.) are not to be bent, broken, or re-capped. Sharps are to be disposed of in puncture resistant, leak-proof containers displaying a BIOHAZARD label. Contaminated PPE and OPIM are to be placed in biohazard-labeled cardboard containers lined with red bag liners. a. Warning labels must be affixed to containers of regulated waste, refrigerators and freezers containing blood or OPIM, and other containers used to store, transport or ship blood or other potentially infectious materials. Labels must include the biohazard symbol, and be fluorescent orange or orange-red with lettering or symbols in a contrasting color. Red bags or red containers may be used in lieu of labels. b. Equipment contaminated with blood or OPIM must be examined prior to servicing or shipping, and decontaminated as necessary. Portions of the equipment not feasible for decontamination are to be tagged with a BIOHAZARD label and the information communicated verbally and/or in written form to service personnel. 3. Eating, drinking, smoking, applying cosmetics or lip balm, and handling contact lenses in any area where there is reasonable likelihood of occupational exposure is strictly prohibited. Storage of food and drink is prohibited in refrigerators, freezers, shelves, cabinets or on countertops or bench tops where blood or OPIM are present. 4. Mouth pipetting is strictly prohibited. 5. Splash, spills, contaminated broken glass, fluid/tissue manipulation - All procedures involving blood or OPIM must be performed in such a manner as to minimize splashing, spraying, spattering, and generation of droplets of these substances. Broken glass that is contaminated is to be cleaned up using mechanical means, i.e., dust pan and broom or brush. 6. In accordance with the Needlestick Safety and Prevention Act, single-use needles with hinged or sliding sheaths and tube holders with needle guards are used to prevent needle stick injury. 7. ONU identifies the need for changes in engineering controls and work practices through its Biosafety committee activities and based on the recommendation of the employees who may have new information provided by a supplier, through specialized training, or following a review of the literature and OSHA updates. Both employees and management personnel are involved in the process while the ECP program coordinator is responsible for ensuring that these recommendations are implemented. 9/23/2014 9:36:37 AM 12 VI. Personal Protective Equipment (PPE) Personal protective equipment is provided to employees by ONU at no cost to them and, when used correctly by employees, will provide protection from exposure to potentially infectious or contaminated materials by creating an impervious barrier. Personal protective equipment includes, but is not limited to: Disposable latex or hypoallergenic gloves; Laboratory coats or gowns; Face shields; Face masks; Eye protection (e.g., goggles); Pocket cardiopulmonary resuscitation (CPR) masks with a one-way valve. PPE is located in work areas for easy access and supplies are available by contacting the manager of the university warehouse. A. All employees are to wear personal protective equipment when performing procedures in which potential exposure to the skin, eyes, mouth, nose or broken areas of the skin may reasonably be anticipated. Those wearing PPE must observe the following procedures: 1. Wash hands immediately or as soon as feasible after removing gloves or other PPE. Disposable gloves are not to be washed or decontaminated for reuse! Replace disposable gloves as soon as practical after contamination, or if they are torn, punctured or otherwise lose their ability to function as a protective barrier. 2. Remove and appropriately discard PPE after it becomes contaminated and before leaving the work area. 3. Remove immediately any garment contaminated by blood or OPIM in a manner to avoid contact with the outer surface. 4. Place used/and or contaminated disposable PPE in appropriately labeled biohazard waste containers. Non-disposable but contaminated PPE is decontaminated before reuse or prior to storage. a. Utility gloves may be decontaminated for reuse if their integrity is not compromised; these gloves are to be discarded if they show signs of tearing, puncturing, cracking, peeling, or deterioration. b. Decontaminate face shields, reusable eye protection, and resuscitation equipment by soaking for no less than 10 minutes in a freshly-prepared solution of household bleach mixed with water in a 1:10 solution (1/4 cup bleach in 1 gallon water). Rinse well with clean water and dry thoroughly before reuse and/ or placement in storage. 5. Wear appropriate face and eye protection when splashes, sprays, spatters, or droplets of blood or OPIM pose a hazard to the eye, nose, or mouth. 9/23/2014 9:36:37 AM 13 VII. Housekeeping Regulated waste is placed in containers which are closable, constructed to contain all contents and prevent leakage, appropriately labeled or color-coded (see the following section “Labels”), and closed prior to removal to prevent spillage or protrusion of contents during handling. A. Contaminated sharps are discarded immediately or as soon as possible in containers that are closable, puncture-resistant, leak proof on sides and bottoms, and appropriately labeled or color-coded. Sharps disposal containers are available in work areas and classrooms, readily accessible to prevent exposure to blood borne pathogens. Broken glassware that may be contaminated is only picked up using mechanical means, such as a brush and dustpan. B. The amount of regulated waste generated at ONU is expected to vary. C. Regulated waste is disposed of in the following manner: 1. Collect all regulated waste in a closing, leak-proof, Red Bag. 2. Dispose of all regulated waste in the Biohazard Waste Container, in accordance with applicable Federal, State and local regulations. 3. If the bag is contaminated with blood or OPIM double-bag it prior to handling, storing and or transporting the bag. 4. Place disposable syringes, needles, blades, broken glass and other sharp items in the puncture-resistant Sharps Container for disposal. Employees WILL NOT pick up sharp objects directly with their hands. Reusable containers will not be opened, emptied or cleaned manually or in any other manner which will expose employees to the risk of percutaneous injury. Employees WILL NOT reach by hand into a container of reusable contaminated sharp objects. 5. Sealed containers of regulated biohazard waste are picked-up by housekeeping and delivered to the ONU warehouse. For pick-up, call the physical plant. The waste is stored at the warehouse until pick-up and disposal. D. Laundry - Personnel will wear disposable lab coats or aprons, gloves and other applicable PPE when responding to an accident or when performing routine cleaning of guest rooms where blood or OPIM are present. Laundering of contaminated articles will be performed following these requirements: Contaminated laundry will be handled as little as possible, with minimal agitation. Wet contaminated laundry is placed in a leak-proof, labeled or colorcoded container for transport. Laundering will be performed by: Weekdays 8 – 5:30 p.m., contact physical plant for more information. After hours, and on holidays, contact Security at 2222 or the University operator (dial ‘0’) to arrange for contact with the supervisor on call. 9/23/2014 9:36:37 AM 14 VIII. Labels and Signage A. Any device or bag that contains a potential biological hazard will be marked with the following: Warning labels stating Biohazard Biohazard Symbol B. Warning labels will be firmly attached to containers of regulated waste, refrigerators and freezers containing blood or other potentially infectious material, and any other containers used to store, transport or ship blood or other potentially infectious material. C. Employees are responsible for ensuring that warning labels are affixed or that red bags are used as required if regulated waste or contaminated equipment is brought into the facility. Employees are to notify housekeeping/physical plant if they discover regulated waste containers, refrigerators containing blood or OPIM, contaminated equipment, etc., without proper labels. IX. Hepatitis B Vaccination Employees whose jobs may reasonably be anticipated to involve direct contact with blood or OPIM will be offered the Hepatitis B vaccination series after initial employee training and within 10 days of initial assignment to all employees identified in the exposure determination section of this plan. Vaccination is encouraged unless: 1) documentation exists that the employee has previously received the series; 2) antibody testing reveals that the employee is immune; or 3) medical evaluation shows that vaccination is contraindicated. A. Employees are strongly urged to follow the vaccination series through to completion as recommended in the U.S. Public Health guidelines on HBV prophylaxis. B. If an eligible employee chooses not to receive the Hepatitis B vaccination, the employee must sign a Hepatitis B Declination Statement which is filed in the Office of Human Resources. Employees who decline may request and obtain the vaccination at a later date at no cost. C. Vaccination will be given according to standard medical practice under the supervision of a licensed physician or another licensed healthcare professional. 1. Following a medication evaluation by a licensed physician or other qualified healthcare provider, a written copy of the evaluation will be obtained and provided to the employee within 15 days of completion of the evaluation. It will be limited to whether the employee requires the hepatitis vaccine and whether the vaccine was administered. 2. If a routine booster dose of Hepatitis B vaccine is recommended by the U. S. Public Health Service at a future date, the booster dose will be made available at no cost to eligible employees by ONU. 9/23/2014 9:36:37 AM 15 D. All laboratory tests will be conducted by an accredited laboratory at no cost to the employee. E. The ECP coordinator will provide training to employees on hepatitis B vaccinations, addressing safety, benefits, efficacy, methods of administration, and availability. X. Post-Exposure Incident Evaluation and Follow-up The ECP program coordinator is the person responsible for reviewing and documenting in the exposure injury log the circumstances of all exposure incidents to determine: Engineering controls in use at the time Work practices followed A description of the device being used (including type and brand) Protective equipment or clothing that was used at the time of the exposure Location of the incident Procedure performed when the incident occurred Employee’s training Following an exposure incident, employees have the opportunity to receive at no cost, at a reasonable time and place, a confidential medical evaluation performed by or under the direct supervision of a licensed physician. All associated testing will be performed by an accredited laboratory. Students and others should contact their own health practitioner because: He or she may need to be tested for Hepatitis B and HIV in the manner recommended by the CDC as soon as possible after the incident, including the opportunity for repeat testing at six weeks, twelve weeks, and six months post exposure. He or she may need to receive post exposure gamma-globulin, Hepatitis B immunoglobulin, and/or Hepatitis B Vaccination series or booster when medically indicated. A. In the event of an occupational exposure, employees are to, following initial first aid (e.g., clean the wound, flush eyes or other mucous membrane, etc.), immediately contact their supervisor, then the ECP program coordinator or his/her designee, and within twenty-four hours of the incident, contact the Human Resources office. A student is to notify the faculty of record who will report the incident to the ECP coordinator. B. An Exposure incident form, available from the employee’s department/unit main office or the human resources office, with directions for completion will be provided to the employee or student at the time of exposure. The route of exposure, the status of the source (unless the employer can establish that identification is infeasible or prohibited by state or local law), and the circumstances of the exposure will be documented on the form. The completed form and associated records will be sent to the ECP program coordinator for review before being forwarded to the Human Resources Office. An attempt will be made to contact the source patient to collect and test their blood for the presence of Hepatitis B and 9/23/2014 9:36:37 AM 16 HIV (not needed if the source individual is already known to be HIV, HCV, and/or HBV positive). Additionally, the exposed employee will be offered the opportunity to: Complete a confidential medical history at a local health facility; To be tested for Hepatitis B and HIV in the manner recommended by CDC as soon as possible after the incident, including the opportunity for repeat testing at 6 weeks, 12 weeks and 6 months post exposure; and To receive post-exposure gamma globulin or Hepatitis B immune globulin and/or the Hepatitis B vaccination series or booster, when medically indicated, at ONU’s expense. If an employee does not give consent for HIV serological testing during collection of blood for baseline testing, the sample is to be held for 90 days; if the employee elects to have the baseline sample tested during this waiting period, the testing is to be performed as soon as feasible. C. Follow-up care of the exposed worker will include counseling, medical evaluation of any acute febrile illness that occurs within 12 weeks post exposure, and the use of safe and effective post exposure measures according to standard medical practice. D. The treating health care facility will send the Human Resources Director a statement that: the employee has been informed in writing of the results of the evaluation the employee has been informed in writing of any medical conditions subsequent to exposure to blood or other potentially infectious materials that require further evaluation or treatment. E. All other health findings are to remain confidential and not included in the healthcare facility’s written report to the employer. F. The ECP program coordinator is to: Provide the healthcare professional(s) responsible for the employee’s hepatitis B vaccination and post-exposure evaluation and follow-up a copy of OSHA’s bloodborne pathogen standard. Ensure that the health care professional evaluating an employee after an exposure incident receives a description of the employee’s duties relevant to the incident, route(s) of exposure, circumstances of exposure, if possible a copy of the source individual’s blood tests, other relevant information on the health and vaccination status of the employee 9/23/2014 9:36:37 AM 17 XI. Recordkeeping For Employees, the Office of Human Resources is responsible for keeping all records pertaining to the ECP. Additionally the University biosafety committee chair must have access to all training records for staff, faculty, volunteers, and students. Training records for OSHA BBP and bioafety must also be kept on site. (In labs etc.) For students, it’s the Department Office of record. These records include: Name of employee/ or student Employee/Student ID number The Employee’s/Student’s Hepatitis B vaccination status Copies of the results of examinations, medical testing and follow-up procedures that took place as a result of the occupational exposure. A. Document Retention - the Office of Human Resources will document any exposure incident in accordance with the Access to Employee Exposure and Medical Records as found in the Code of Federal Regulations 1910.20. Records will be maintained in confidence by the Office of Human Resources for at least the duration of employment plus 30 years. B.Sharps Injury Log - will be maintained to record all percutaneous injuries from contaminated sharps. The information will be recorded in such a way as to protect the confidentiality of the injured employee. The log will contain: (a) the type and brand of device involved in the incident; (b) the Department or work area where the exposure incident occurred; and (c) an explanation of how the incident occurred. C. Exposure Record - all records are kept confidentially as part of the employee's records, and no information will be disclosed or reported without the employee's written consent, except as may be required by law. Any exposure incident will be documented on the exposure incident form maintained in the employee's confidential file kept by the Office of Human Resource. D. Training Records - while generated by the ECP coordinator, the records will be maintained by the Office of Human Resources for three (3) years from the date of training, including the date of training, contents or summary of training topics, names and qualifications of persons conducting the training, and the names and job titles of all employees attending the training. EXCEPTION – student training records will be maintained by the department of record, but made available upon request from the Human Resources Office and/ or the ECP coordinator. XII. Employee and Student ECP Education A well-informed, properly trained employee is crucial to the successful implementation and effectiveness of ONU’s ECP activities. Education of employees regarding the ECP is accomplished by means of initial training and repeated annually, and upon employment for new employees. Additionally, training will be provided to students who, though not expected to respond to situations involving potential exposure, may be at risk for exposure due to their studies and campus activities. 9/23/2014 9:36:37 AM 18 A. Presentation - training that is tailored to the educational level and language of employee or student will include an opportunity to ask questions and have them answered by a knowledgeable trainer. The ONU Office of Human Resources and the ECP program coordinator are responsible for scheduling and documenting the training. B. Topics covered during training will include, but not be limited to: Explanation and location of the Exposure Control Plan and the Bloodborne Pathogens Standard as found in the Code of Federal Regulations 1910.1030; The epidemiology, modes of transmission and symptoms of diseases transmitted via the human blood; Procedures and job tasks that may expose employees to blood and/ or OPIM; Engineering and work practice controls used at ONU; Limitations and basis for selection of personal protective equipment, including the types available, proper use, location within the facility, removal, handling, decontamination and disposal; Visual warnings of biohazards, including labels, signs and color-coded Red containers; Information on the Hepatitis B program, including the benefits and safety of vaccination, a test of protective titer, and that the vaccine will be offered free of charge; Information on procedures to use in an emergency that may involve an exposure incident; Explanation of post-exposure evaluation and follow-up procedures; How to inspect equipment for contamination; and How to decontaminate equipment. C. Education Methods - ONU will utilize appropriate training methods that achieve these objectives: (a) encourage trainee involvement with the topic; (b) utilize appropriate audiovisual aids; (c) build upon the participants’ current knowledge base of the subject; (d) allow opportunity for interactive questions and answers with the person conducting the training session; (e) offer handouts or other methods to obtain further information. 9/23/2014 9:36:37 AM 19 Authorized Signatures 9/23/2014 9:36:37 AM 20 ADDENDUM Hepatitis Declination Form Exposure Incident Form The exposed individual must complete and submit this form to the ECP coordinator within 24 hours following an occupational exposure to human blood. Sharps Injury Log Source Individual’s Consent or Refusal for Infectivity Testing Form The individual whose blood was involved in the occupational exposure (not the exposed individual) must complete and sign this form before submitting to testing. Refusal of Post-Exposure Medical Evaluation Form The exposed individual must complete this form only if refusing post-exposure medical evaluation by a health care professional. OSHA Standard 1910.1030 (on-line at https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS &p_id=10051 Summary of Key Provisions OSHA Standard 1910.1030 9/23/2014 9:36:37 AM 21 Ohio Northern University HEPATITIS VACCINATION DECLINATION FORM Hepatitis B Vaccination Declination Statement I understand that due to my occupational exposure to blood or other potentially infectious materials, I may be at risk of acquiring Hepatitis B Virus infection. I have been given the opportunity to be vaccinated with Hepatitis B vaccine at no charge to myself. However, I decline this vaccine. I understand that I continue to be at risk of acquiring Hepatitis B, a serious disease. If in the future I continue to have occupational exposure to blood or other potentially infectious materials and I want to be vaccinated with hepatitis B vaccine, I can receive the vaccination series at no charge to myself. ____________________________________________ Employee Name (PRINT) Date ___________________ ____________________________________________ Employee Signature ID No. __________________ Reason for Declination (please check one): At this time, I do not choose to receive the Hepatitis B vaccine. I have previously completed the 3 dose series of the Hepatitis B vaccine. Documentation of this is attached. I have been exposed to Hepatitis B and blood tests reveal that I have developed antibodies. Documentation of this fact is attached. Other (please briefly explain: ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ Filed to employee’s record 9/23/2014 9:36:37 AM _____________________________________________ Date 22 Ohio Northern University Sharps Injury Log Year______ Date Case/Report No. Type of Device (e.g. syringe, suture needle) Brand Name of Device Work Area where injury occurred (e.g. geriatrics lab) Brief description of how incident occurred (i.e. procedure being done, action being performed) 29 CFR 1910.1030, OSHA’s Bloodborne Pathogens Standard, in paragraph (h)(5), requires an employer to establish and maintain a Sharps Injury Log for recording all percutaneous injuries in a facility occurring from contaminated sharps. The purpose of the Log is to aid in the evaluation of devices being used in healthcare and other facilities and to identify problem devices or procedures requiring additional attention or review. This log must be kept in addition to the injury and illness log required by 29 CFR 1904. The Sharps Injury Log should include all sharps injuries occurring in a calendar year. The log must be retained for five years following the end of the year to which it relates. The Log must be kept in a manner that preserves the confidentiality of the affected employee. 9/23/2014 9:36:37 AM 23 Ohio Northern University Exposure Incident Report (Routes, Circumstances, & Follow-up of Exposure Incident) Date Completed ________________________________________________________ Name ______________________________________ SSN/ID Number _______________ Home Phone Birth Date ___________________________ Work Phone __________________ ________________________ Job Title ______________________________ Vaccination Status YES Current with HEP B: EXPLANATIONS: NO UNKNOWN ________________________________________________________ ________________________________________________________________________ Date of Exposure __________ Time of Exposure __________ _____a.m. _____ p.m. Location of Exposure (be very specific): ________________________________________ ________________________________________________________________________ Nature of Exposure (e.g., work-related trauma, school-related activity, etc. – be very specific) ________________________________________________________________________ ________________________________________________________________________ Describe what task(s) you were performing when the exposure occurred (be very specific): ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ Were you wearing PPE when the exposure occurred? YES Did the PPE fail? YES NO NO If yes, please explain. ______________________ ________________________________________________________________________ ________________________________________________________________________ What fluids or OPIM were you exposed to? ______________________________________ What type of exposure? (check all that apply) Mucous membranes (e.g., eyes, nose, mouth) Skin puncture, tissue wound 9/23/2014 9:36:37 AM Spill on Clothing and/ or Intact Skin Other (explain) _______________________________ 24 Ohio Northern University Exposure Incident Report Page 2 Did you receive medical attention? YES NO If yes, where? _____________________________________________________________ When? __________________________________________________________________ By whom? _______________________________________________________________ ID Source individual (what or who was the source of blood/fluid exposure) _____________ ________________________________________________________________________ ________________________________________________________________________ Please provide any additional information regarding this exposure incident. Blood Testing Offered? NO YES Explain ______________________ ________________________________________________________________________ ________________________________________________________________________ Vaccination Offered/Recommended? NO YES Explain ____________ ________________________________________________________________________ ________________________________________________________________________ Counseling Offered? NO YES Explain ______________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ Injured Person advised of need for further evaluation and medical attention? NO YES Explain ____________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________ __________________ Injured Person Signature Date Reviewed by: _____________________________________________________________ Filed: ___________________________________________________________________ 9/23/2014 9:36:37 AM 25 Ohio Northern University Source Individual’s Consent or Refusal Form Infectivity Testing *This person’s blood or body fluids provided the source of this exposure. NOTE: Print this form and distribute copies of this form to: □ Health Care Professional □ ONU Human Resources, BioSafety Committee Exposed Individual's Information Name (Please Print):_____________________________________________ Department or Program:__________________________________________ Telephone Number: ______________Exposure Date:___________________ Source Individual's Statement of Understanding I understand that employers are required by law to attempt to obtain consent for HIV, HBV, and HCV infectivity testing each time an employee is exposed to the blood or bodily fluids of any individual. I understand that an ONU employee or student intern has been accidentally exposed to my blood or bodily fluids and that testing for HIV, HBV, and HCV infectivity is requested. I am not required to give my consent, but if I do, my blood will be tested for these viruses at no expense to me. I have been informed that the test to detect whether or not I have HIV antibodies is not completely reliable. This test can produce a false positive result when an HIV antibody is not present and that follow-up tests may be required. I understand that the results of these tests will be kept confidential and will only be released to medical personnel directly responsible for my care and treatment, to the exposed healthcare worker for his or her medical benefit only and to others only as required by law. Consent or Refusal & Signature I hereby consent to: □ HIV Testing □ HBV Testing □ HCV Testing I hereby refuse consent to: □ HIV Testing □ HBV Testing □ HCV Testing Source Individual Identification Source individual's printed name and signature:____________________________ Date Signed:___________________________ Relationship (If signed by someone other than the source Individual): ________________________________ 9/23/2014 9:36:37 AM 26 Ohio Northern University Refusal of Post-Exposure Medical Evaluation Form for Bloodborne Pathogen Exposure Supervisor or Clinical Instructor: Complete this form only if the exposed individual refuses postexposure medical evaluation by a health care professional. Send this completed form to ONU Human Resources, Biosafety Committee Chair Exposed Individual Information Name:_____________________________________________________________ Department or Program:_______________________________________________ Exposure Date: ________________ Social Security Number:__________________ Exposure Information Facility & Department where the incident occurred:___________________________ Type of protection equipment used (gloves, eye protection, etc.):________________ Describe how you were exposed:________________________________________ __________________________________________________________________ Tell how this type of exposure can be prevented:____________________________ __________________________________________________________________ Statement of Understanding I have been fully trained in ONU's Exposure Control Plan, and I understand I may have contracted an infectious disease such as HIV, HCV or HBV. I also understand the implications of contracting these diseases. I have been offered follow-up medical testing free of charge by my employer to determine whether or not I have contracted an infectious Disease such as HIV, HCV, or HBV. I have also been offered follow-up medical care in the form of counseling and medical evaluation of any acute febrile illness (new illness accompanied by fever) that occurs within twelve weeks post-exposure. Despite all the information I have received, for personal reasons, I freely decline this postexposure evaluation and follow-up care. Exposed Individual’s Signature:_________________________ Date: ______________ Witness Name (Please Print):____________________________________________ Witness Signature: ________________________ Witness Date: __________________ 9/23/2014 9:36:37 AM 27 KEY PROVISIONS OF OSHA BLOODBORNE PATHOGEN STANDARD U.S. Department of Labor Program Highlight Fact Sheet No. OSHA 92-46 PURPOSE: Limits occupational exposure to blood and other potentially infectious materials since any exposure could result in transmission of bloodborne pathogens which could lead to disease or death. SCOPE: Covers all employees who could be "reasonably anticipated" as the result of performing their job duties to face contact with blood and other potentially infectious materials. OSHA has not attempted to list all occupations where exposures could occur. "Good Samaritan" acts such as assisting a co-worker with a nosebleed would not be considered occupational exposure. Infectious materials include semen, vaginal secretions, cerebrospinal fluid, synovial fluid, pleural fluid, pericardial fluid, peritoneal fluid, amniotic fluid, saliva in dental procedures, any body fluid visibly contaminated with blood and all body fluids in situations where it is difficult or impossible to differentiate between body fluids. They also include any unfixed tissue or organ other than intact skin from a human (living or dead), human immunodeficiency virus (HIV)- containing cell or tissue cultures, organ cultures and HIV or hepatitis B (HBV)containing culture medium or other solutions as well as blood, organs or other tissues from experimental animals infected with HIV or HBV. EXPOSURE CONTROL PLAN: Requires employers to identify, in writing, tasks and procedures as well as job classifications where occupational exposure to blood occurs-without regard to personal protective clothing and equipment. It must also set forth the schedule for implementing other provisions of the standard and specify the procedure for evaluating circumstances surrounding exposure incidents. The plan must be accessible to employees and available to OSHA. Employers must review and update it at least annually-more often if necessary to accommodate workplace changes. METHODS OF COMPLIANCE: Mandates universal precautions, (treating body fluids/materials as if infectious) emphasizing engineering and work practice controls. The standard stresses handwashing and requires employers to provide facilities and ensure that employees use them following exposure to blood. It sets forth procedures to minimize needlesticks, minimize splashing and spraying of blood, ensure appropriate packaging of specimens and regulated wastes and decontaminate equipment or label it as contaminated before shipping to servicing facilities. Employers must provide, at no cost, and require employees to use appropriate personal protective equipment such as gloves, gowns, masks, mouthpieces and resuscitation bags and must clean, repair and replace these when necessary. Gloves are not necessarily 9/23/2014 9:36:37 AM 28 required for routine phlebotomies in volunteer blood donation centers but must be made available to employees who want them. The standard requires a written schedule for cleaning, identifying the method of decontamination to be used, in addition to cleaning following contact with blood or other potentially infectious materials. It specifies methods for disposing of contaminated sharps and sets forth standards for containers for these items and other regulated waste. Further, the standard includes provisions for handling contaminated laundry to minimize exposures. HIV AND HBV RESEARCH LABORATORIES AND PRODUCTION FACILITIES: Calls for these facilities to follow standard microbiological practices and specifies additional practices intended to minimize exposures of employees working with concentrated viruses and reduce the risk of accidental exposure for other employees at the facility. These facilities must include required containment equipment and an autoclave for decontamination of regulated waste and must be constructed to limit risks and enable easy clean up. Additional training and experience requirements apply to workers in these facilities. HEPATITIS B VACCINATION: Requires vaccinations to be made available to all employees who have occupational exposure to blood within 10 working days of assignment, at no cost, at a reasonable time and place, under the supervision of licensed physician/licensed healthcare professional and according to the latest recommendations of the U.S. Public Health Service (USPHS). Prescreening may not be required as a condition of receiving the vaccine. Employees must sign a declination form if they choose not to be vaccinated, but may later opt to receive the vaccine at no cost to the employee. Should booster doses later be recommended by the USPHS, employees must be offered them. POST-EXPOSURE EVALUATION AND FOLLOW-UP: Specifies procedures to be made available to all employees who have had an exposure incident plus any laboratory tests must be conducted by an accredited laboratory at no cost to the employee. Follow-up must include a confidential medical evaluation documenting the circumstances of exposure, identifying and testing the source individual if feasible, testing the exposed employee's blood if he/she consents, post-exposure prophylaxis, counseling and evaluation of reported illnesses. Healthcare professionals must be provided specified information to facilitate the evaluation and their written opinion on the need for hepatitis B vaccination following the exposure. Information such as the employee's ability to receive the hepatitis B vaccine must be supplied to the employer. All diagnoses must remain confidential. HAZARD COMMUNICATION: Requires warning labels including the orange or orange-red biohazard symbol affixed to containers of regulated waste, refrigerators and freezers and other containers which are used to store or transport blood or other potentially infectious materials. Red bags or containers may be used instead of labeling. When a facility uses universal precautions in its handling of all specimens, labeling is not required within the facility. Likewise, when all laundry is handled with universal precautions, the laundry need not be labelled. Blood which has been tested and found free of HIV or HBV and released for clinical use, and regulated waste which has been decontaminated, need not be labeled. 9/23/2014 9:36:37 AM 29 Signs must be used to identify restricted areas in HIV and HBV research laboratories and production facilities. INFORMATION AND TRAINING: Mandates training within 90 days of effective date, initially upon assignment and annually - employees who have received appropriate training within the past year need only receive additional training in items not previously covered. Training must include making accessible a copy of the regulatory text of the standard and explanation of its contents, general discussion on bloodborne diseases and their transmission, exposure control plan, engineering and work practice controls, personal protective equipment, hepatitis B vaccine, response to emergencies involving blood, how to handle exposure incidents, the post-exposure evaluation and follow-up program, signs/labels/color-coding. There must be opportunity for questions and answers, and the trainer must be knowledgeable in the subject matter. Laboratory and production facility workers must receive additional specialized initial training. RECORDKEEPING: Calls for medical records to be kept for each employee with occupational exposure for the duration of employment plus 30 years, must be confidential and must include name and social security number; hepatitis B vaccination status (including dates); results of any examinations, medical testing and follow-up procedures; a copy of the healthcare professional's written opinion; and a copy of information provided to the healthcare professional. Training records must be maintained for three years and must include dates, contents of the training program or a summary, trainer's name and qualifications, names and job titles of all persons attending the sessions. Medical records must be made available to the subject employee, anyone with written consent of the employee, OSHA and NIOSH--they are not available to the employer. Disposal of records must be in accord with OSHA's standard covering access to records. 9/23/2014 9:36:37 AM 30