Document 10398006
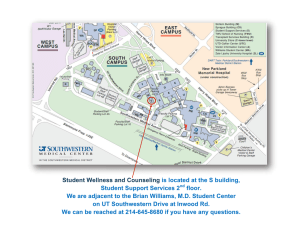
advertisement

C O N T E N T S 2 TEN THOUSAND & COUNTING Numbered among UTSW’s more than 10,000 medical school graduates are some of the world’s foremost scientists, distinguished physicians, and honored educators. TEAM TLC 12 Helping multiple sclerosis patients adjust to the disease can be just as important as providing the cutting-edge medical care for which UT Southwestern Medical Center is known. UNLOCKING THE MYSTERIES OF STEM CELLS 18 Groundbreaking scientific discoveries are revolutionizing the way we understand how stem cells exist at the interface of regenerative medicine and the biological basis of disease. ELECTRIFYING MEDICINE 28 Whether it’s telemedicine, state-of-the-art electronic medical records, or robotic surgery, UTSW continues to stay ahead of the technology curve to improve the quality of patient care. TEAMWORK OFFERS NEW LIFE TO TRANSPLANT PATIENTS 36 Transplant patients are surrounded by a dedicated team that provides them with the compass to guide them through their health crises and to support them long after they leave the hospital. THE CLINICAL FRONTIER 46 HOW A NURSERY RHYME SAVES LIVES 46 FIGHTING CANCER WHILE PRESERVING FERTILITY 47 SOLVING THE SCID PUZZLE TO HELP SICK BABIES 48 LIVING WITHOUT PAIN 50 2012 ANNUAL REVIEW 51 HIGHLIGHTS OF THE YEAR 52 FINANCIAL STATEMENT 62 GIFT REPORT 65 Articles from Southwestern Medicine and other news and information from UT Southwestern are available online at www.utsouthwestern.edu. N umbered among those 10,000 graduates are some of the world’s foremost scientists, distinguished physicians, and honored educators – men and women who have far outpaced even the bold aspirations of the community leaders who initially envisioned a medical school that Dallas could call its own. “It is a remarkable achievement for an institution that granted its first degree in 1944. The sheer number underscores the importance of UT Southwestern in preparing physicians and physician-scientists who care for the people of Texas and beyond,” said Dr. Daniel K. Podolsky, President of UT Southwestern. Today, more than 300 current UT Southwestern faculty members are the product of their own medical school, including more than 50 professors, three department chairs, seven former chairmen, and one former dean and president. The alumni range from Nobel Prize winners to astronauts, from politicians to biotech pioneers. Their discoveries have changed the way medicine is practiced. Their decisions have been etched into the history books. Their curiosity has charted unknown territories from the microbial to the celestial. “It is humbling to be part of a community comprised of so many who are making a difference in the state of Texas and around the world,” Dr. Podolsky said. “It’s an exciting milestone that conveys the true magnitude of our educational mission and, through it, impacts the lives of untold numbers of patients cared for by our more than 10,000 physician alumni.” Inventory of accomplishments The inventory of alumni accomplishments covers a broad swath of medical and cultural achievements. The Medical School has educated physicians desperately needed for World War II and researchers who defined Gulf War syndrome. It produced the doctors who cared for John F. Kennedy in his final moments and the physicians who rode aboard the space flights of which he dreamed. It trained the minds behind the invention of Gatorade and the Nobel-winning scientific discoveries that led to lifesaving statins. UT Southwestern alumni have written many of the foundational textbooks that educate the latest generations of doctors, along with the latest papers on the cutting edge of stem cell and DNA research. They peer into the invisible realms of molecular structures to battle heart disease and cancer and track the progression of infectious diseases across entire populations. Yet, they still hold dear the skills needed to coax a smile from a sickly child facing the toughest of futures. “Among our graduates are those who make scientific advances that improve the treatment and prevention of disease, as well as the teachers of the future generations of physicians and physician-scientists serving as members of our faculty and the faculty of many other medical schools across the country,” Dr. Podolsky said. For the purposes of primary care education, UT Southwestern is the highestranked medical school in Texas and No. 21 in the country (out of more than 140 medical schools) according to the most recent data by U.S. News & World Report. In the same rankings, UT Southwestern also is listed among the top 25 medical schools in the nation in research, one of only 10 medical schools in the country in the top 25 for both the primary care and research categories. UT Southwestern faculty, residents, and students annually provide direct care to nearly 100,000 hospitalized patients and oversee approximately 2 million outpatient visits. The broad range of patient care is backed by extraordinary science – more than 200 labs spread across the Medical Center campus provide the building blocks for future care. Funding from federal agencies, foundations, companies, and private donors provides more than $400 million per year for more than 3,500 research projects that engage, inspire, and attract the next generation of students. CLASS OF 1983 Dr. Francisco G. Cigarroa In 2009, Dr. Cigarroa became the 10th Chancellor of The University of Texas System, one of the largest public systems of higher education in the nation. President George W. Bush appointed him to serve as a member of the President’s Committee on the National Medal of Science, and President Barack Obama appointed him to serve as a commissioner on the White House Initiative on Educational Excellence of Hispanic Americans. Dr. Cigarroa is the first Hispanic to head a major public university system in the country. Today, the magnitude of achievement embodied in the UT Southwestern faculty is stunning. It includes: E Five Nobel laureates, more than any other medical center in the world. E 19 members of the National Academy of Sciences, the most prestigious scientific society in America. E 18 members of the Institute of Medicine, the medical component of the NAS. E 12 Howard Hughes Medical Institute investigators. E 15 members of the American Academy of Arts and Sciences. SOUTHWESTERN MEDICINE 5 Team Patients at UT Southwestern’s multiple sclerosis center receive more than just cutting-edge medical care. They receive help in living TLC better lives while they battle their debilitating disease. To t a l L i f e C a r e B Y D E B O R A H WO R M S E R Susan Sides adored helping patients as a nurse at Children’s Medical Center Dallas. She held increasingly responsible positions there for more than 15 years after her first episode of multiple sclerosis and even after a 2002 stroke, all that time presenting a brave facade. “I hid the MS from some of my co-workers and tried to hide it from my daughter, who was 9 when I had the stroke. I tried to act normal, but I wasn’t OK. I was under a lot of stress,” recalled the 46-yearold Frisco, Texas, wife, mother, and health care professional. Mrs. Sides and many MS patients like her have benefited greatly over the years from Dr. Elliot Frohman’s decision to move Dallas in 1995 as Director of the new Multiple Sclerosis Program and Clinical Center at UT Southwestern Medical Center. Dr. Frohman, Professor of Neurology and Neurotherapeutics and of Ophthalmology, said colleagues across the country wondered why the former chief resident of neurology at Johns Hopkins Hospital would put his promising research career on hold to concentrate on patient care, which consumed his time for the first four years of the clinic’s existence. “It was very clear that this was a place that was very serious about establishing a major center for clinical care, for research, and for education,” he said, explaining his conviction that UT Southwestern would help turn his dream of a comprehensive-care, clinical-research center into reality. SOUTHWESTERN MEDICINE 13 “MS is a progressive condition, and life is progressive.” — Registered Nurse Diana Logan with MS patient Susan Sides “For patients who are on crutches or are wheelchair bound, it is difficult to get to multiple doctor appointments. Even when the area is wheelchair accessible, it can be too exhausting for patients with low energy. We help them cut through those barriers by having as much care as possible in one place,” Mrs. Logan said. A health passport When patients arrive at the TLC clinic, they receive a slip of paper that becomes their global health passport. In addition to the MS center’s social worker, nurse practitioner, and physician assistants, the TLC clinic also offers a physical therapist for gait assessments and a registered dietitian for nutritional counseling. Like everything about MS, even its nutritional aspects are complex: Some MS patients deal with obesity, while MS makes others dangerously underweight, Mrs. Logan explained. It’s Monday, 7:30 a.m., and the first thing Mrs. Logan does for her TLC client is to listen. Intensely. She begins by asking: “What does this disease keep you from doing? What bugs you the most?” She then carefully follows a checklist that asks about mobility, mood, memory problems, energy level, etc., in order to get a comprehensive view of the patient’s condition, problems, and possible goals. “It really doesn’t matter how smart I think I am or how smart any of us think we are or what we want the patient to do,” Mrs. Logan said, echoing one of Dr. Frohman’s oft-quoted treatment pearls. Often by the time she’s finished her detailed assessment, she’s changed her mind about what the goals should be. “What is most important is that the TLC goals are set by the patient,” she added. Together, Mrs. Logan and her patients brainstorm strategies to achieve those goals. Next, the patient takes the global health passport to another member of the team and the process repeats. At the end of the day, the patient has a fully signed passport, a printout of goals and strategies, and an appointment in three to four months. “They are very compassionate, and they treat me like I’m the only person they have to worry about,” Mrs. Sides said. “TLC is totally brilliant because it incorporates the four things that are very important in your life when you have MS: treating your symptoms, your emotions, your diet, and your physical activity.” SOUTHWESTERN MEDICINE 15 1 UT Southwestern forges ahead with new clinical and research technologies designed to improve the quality of patient care. The reach of UT Southwestern Medical Center’s technological advances in patient care can be seen in the lives of patients who have been touched by them – in the operating rooms across the Medical Center or in clinics beyond Dallas. Decatur, a small town of about 6,000 people located 60 miles northwest of Dallas, is where patients like Dana Clinesmith have virtual access to UT Southwestern doctors. “To have this technology available in Decatur near my home is huge,” Mrs. Clinesmith said, staring at a large flat-screen monitor displaying UT Southwestern genetics counselor Sara Pirzadeh-Miller in Fort Worth. The Decatur city councilwoman and breast cancer patient recently had her risk for cancers that could be passed down to her two sons assessed through a state-of-the art communication system now deployed by UT Southwestern. It enables medical partners in four counties to conduct cancer screenings and make referrals. “It will be a big relief for me to know that we could catch any hereditary cancer risk early,” Mrs. Clinesmith said. Cancer genetics counselors at the Harold C. Simmons Comprehensive Cancer Center in Dallas and at UT Southwestern’s Moncrief Cancer Institute in Fort Worth are now literally linked with disparate parts of North Texas in a project spearheaded by Dr. David Euhus, Director of the Mary L. Brown Breast Cancer Genetics and Risk Assessment Program. By Alex Lyda SOUTHWESTERN MEDICINE 29 Whether it’s telemedicine, phone texting to communicate with patients, state-of-the-art medical records, or robotic surgery, UT Southwestern continues to stay ahead of the curve when it comes to improving the quality of care provided to patients. The telemedicine video suites in Parker, Wise, Hood, and Johnson counties offer secure, high-speed computer technology connecting genetics counselors with patients who might otherwise never be seen. While the set-up may look familiar, it should not be confused with Skype, FaceTime, or other popular ways to communicate via the Internet – owing to the protection of private medical information. On one end, either in Dallas or Fort Worth, is a Simmons Cancer Center genetics counselor. On the other, at one of the dozens of rural partners (usually a community hospital), are a nurse and the patient. “I’m pretty familiar with technology, but the patient suite is very comfortable, even for those who aren’t used to computers,” Mrs. Clinesmith said. “The large monitors make it feel in many ways like the doctor is in the room with you.” Mrs. Clinesmith’s concern about the risk of passing cancer to her sons isn’t unreasonable. By current estimates, at least 5 percent of all cancers are caused by a specific inherited syndrome, and approximately 10 percent of cancers run in families. In many families, a pattern of Dana Clinesmith, breast cancer patient 30 Dr. David Euhus, Professor of Surgery cancer is obvious. In others, a pattern may not be so easily identified because the families are small or their health history is incomplete. On the day Mrs. Clinesmith talked with Mrs. Pirzadh-Miller, the UT Southwestern genetics counselor, she learned how cancer can be inherited and was given a cancer-risk analysis with a saliva sample. Despite the prospect of additional radiation treatments, she plans to open a bed and breakfast near Fort Worth with the help of her sons. “I am about to start a new business that will involve my sons, so they need to be healthy!” Mrs. Clinesmith said. Most of the telemedicine architecture is housed in the new $22 million Fort Worth facility that the Moncrief Cancer Institute unveiled in November 2012. The Moncrief Cancer Institute, under the direction of Dr. Keith Argenbright, and the Simmons Cancer Center have partnered with other medical facilities and cancer organizations to provide breast cancer screenings and diagnostics to reach underserved women in 15 outlying counties. Included in their arsenal is a high-tech mobile mammography unit that already has been used to screen thousands of women. “We’re using the latest in communications technology and our mobile resources to reach out to diverse, rural communities – especially those that have limited access to health care and are most in need of services,” Dr. Argenbright said. G oing mobile improves c linical outcomes The ability to connect with long-distance patients also is taking place on a mobile and wireless level, with devices that are as ubiquitous as the iPhone. Dr. Sumeet Teotia, Assistant Professor of Plastic Surgery, and Dr. Roshni Rao, Associate Professor of Surgery, for example, have shown that text follow-ups after breast cancer surgery can improve clinical outcomes and can help doctors intervene more quickly in the event of post-operative complications. A study led by Dr. Teotia and Dr. Rao involved more than 100 women who underwent breast reconstruction after mastectomy. They found that text messaging – as a medium of post-operative communication between doctors and patients – led to greater adherence to medical advice and improved recovery times. “Patients said that being able to communicate with their surgeon via text helped them feel empowered as an advocate for their own care,” Dr. Rao said. “And women who exchanged texts with their surgeon made significantly fewer clinic visits and phone calls.” National studies have shown that if patients are empowered with all the tools necessary for them to make informed medical decisions, they feel in charge of their health. Patients also feel more in charge of their care if given the opportunity to see and manage their medical information online. P roviding instant access to patient medical records From the patients’ perspective, the most visible use of technology at UT Southwestern is when they visit their physicians. Doctors have electronic access to their patients’ medical records – including radiology images, laboratory reports, clinic notes, medications, discharge papers, and summaries of previous visits in the UT Southwestern Health System. UT Southwestern University Hospitals and Clinics all use electronic medical records, an effort that began in 2002. This commitment was driven by an anonymous donor, who challenged the university to develop an information technology infrastructure to improve the quality of care. Additional donations, including a $10 million endowment from Dallas philanthropists, helped UT Southwestern become the first major medical center in the Dallas-Fort Worth area to implement electronic medical records across all of its clinical practice groups, making patient care safer and more efficient. Electronic health records (EHRs) are able to pull together all of a patient’s information – from the results of the last cholesterol check with a primary care doctor to CT scans done by an orthopaedic specialist – in one place that is remotely accessible by physicians. Such an amalgamation of health care information from institutions that may be separated by geography or from doctors who are affiliated with different hospitals is priceless for both the doctor and patient, said Dr. DuWayne Willett, Professor of Internal Medicine and Chief Medical Informatics Officer for UT Southwestern. He is in charge of designing the implementation of EHRs across campus. An accurate patient – Dr. Roshni Rao history, preserved digitally, allows doctors to avoid ordering repetitive and unneeded tests, if the results of previous ones can be summoned in an instant, Dr. Willett said. For instance, trends in a heart patient’s blood pressure and cholesterol level, identified with the help of an electronic record that moves with the patient, can allow the cardiologist or primary care physician to prescribe preventive medications and lifestyle changes to reduce the patient’s chance of developing a heart attack. “Patients said that being able to communicate with their surgeon via text helped them feel empowered.” SOUTHWESTERN MEDICINE 31 Dr. DuWayne Willett, Professor of Internal Medicine and Chief Medical Informatics Officer In 2009, as part of the American Recovery and Reinvestment Act, the White House authorized nearly $1.2 billion in grants to help health care providers begin using electronic health records. In 2010, Congress approved new financial incentives for hospitals that use electronic health records and imposed penalties that will mean decreased Medicare reimbursements for health care institutions that fail to use electronic health records by 2015. The comply-or-perish pressure to overhaul the traditional paper health records system is being met head-on by UT Southwestern in the adoption of an EHR system called “Epic” that is quickly becoming the industry leader. Far from being a static platform, the EHR system deployed by UT Southwestern can work behind the scenes, when a person’s medical history may seem inactive or may have undergone slight, subtle changes that can still have a big impact on one’s health. Epic has the capability, because of its innovative “rules logic,” to analyze developments and new information about a person’s symptoms, condition, or treatment along the continuum of care and offer recommendations that support clinical decisions, Dr. Willett said. The EHR software also can be configured to recommend treatment plans for patients with a specific condition, based on evidence that such measures have proved effective for a majority of similar patients. And because Epic is the market leader in EHR software, UT Southwestern can query other institutions in the network for key information in the patient’s file in real time, Dr. Willett said, eliminating the need for phoning from afar and waiting on lab results to be faxed or mailed to the receiving doctor. 32 Within UT Southwestern, the EHR’s secure messaging system allows instantaneous routing of results and other messages among all of a patient’s caregivers, promoting the “team” care of a patient that is so crucial in today’s complex medical environment. Clinicians receiving a secure message have instant access to the breadth of a patient’s electronic health record so they can locate pertinent information crucial to a medical decision – even if the patient was seen across campus earlier the same day. Radiology images also are viewable by the physician online shortly after they are performed. Dr. Willett is helping extend the reach of UT Southwestern’s EHR by working with Dr. Ronald Peshock, Assistant Dean for Informatics, to enable it to be the basis of research protocols, showing that the EHR not only is useful in the clinic, but in identifying disease trends across patient populations in a research setting. Using Epic data drawn from more than 400 patients at Parkland and UT Southwestern-affiliated hospitals, Dr. David Gerber, an oncologist and Assistant Professor of Internal Medicine, is looking at trends involving the use of CT scanning for the early detection of lung cancer. Additionally, more than 50,000 patients have used the Medical Center’s MyChart system to schedule appointments, refill prescriptions, or ask questions of their health care providers over an encrypted, secure Internet connection. “We’ve surrounded all aspects of patient care with information technology,” said Suresh Gunasekaran, Associate Vice President for Health System Information Resources. “And we’re consistently investing in all aspects of information technology, from patient Internet access to supply-chain automation to how doctors take care of patients. Any way in which we can use new technology to support our fight against disease allows us to tailor our therapies and keep track of our patients’ progress in real time.” T ouching patients' lives with robotic hardware Surgery on the high-tech da Vinci robot housed within UT Southwestern’s robotics teaching lab can seem like child’s play – like building a Lego castle on a video screen. While moving tiny blocks, it is difficult to imagine these are the same pincers that slice through tissue, hold artery ends together so they can be stitched, or trim cancer from healthy tissue with granular precision in an operating room. Future robotic surgeons receive their training at the state-of-the-art SCMIS (Southwestern Center for Minimally Invasive Surgery) teaching lab, led by Dr. Daniel Scott, Professor of Surgery, and Dr. Robert Rege, Chairman of Surgery at UT Southwestern. Across the Medical Center campus, four similar da Vinci robots loom above patients every day. For patients like Beth Nail, whose life literally was touched by a da Vinci, the curative power of superior surgical acumen aided by the best technology available is unforgettable. The 53-year-old Allen, Texas, resident and retired nurse suffers from diverticulitis, a chronic condition where the bulging sacs of the intestine’s inner lining become inflamed or infected. One evening in late July, a particularly nasty flare-up forced her to go the hospital. Mrs. Nail had a routine chest X-ray, required to rule out tuberculosis before an overnight stay. The X-ray revealed a suspicious golf ball-size mass in her lung, possibly cancer. Doctors said it needed to be removed as soon as possible. “After my initial shock, I looked into my options and realized that a thoracotomy, or a traditional open surgery on the lungs, can be very involved and hard to recover from,” said Mrs. Nail, who decided to look into the advantages of robotic surgery. Mrs. Nail and patients like her, ultimately were convinced to come to UT Southwestern for their treatment because of its renowned surgeons and the technological marvel that robotic surgical machines represent. “When I hurried to find the best place for robotic surgery, I kept coming back to UT Southwestern,” she said. “And the best man for the job was Dr. Kemp Kernstine because he had access to the latest robots.” Dr. Kernstine is Chief of Thoracic Surgery at UT Southwestern. “The advantages of robotic surgery are precision, smaller incisions, less pain, and quicker healing times,” he said. The surgeons’ ability to access hidden crevices is amplified by the robot while the overall “surgical insult” to the patient is reduced. UT Southwestern's da Vinci surgical robot SOUTHWESTERN MEDICINE 33 Instead of eight weeks of recovery, Mrs. Nail was up in five weeks. She fully was able to return to her new job as a massage therapist shortly thereafter. (Some patients, depending on the complexity of the surgery, can be out in as few as two days.) After following up with Dr. Randall Hughes, Associate Professor of Internal Medicine, Mrs. Nail was declared cancer-free. “The robotics team got it all, and for that they deserve their reputation as tops in their field. But they took a very personal approach with me, taking the time to literally draw out what the robot was going to do and explaining in nontechnical terms how the procedure would work,” she said. T he newest radiation technologies In further defining the line between healthy and diseased tissue, surgery is not the only area in which improving technologies are tracing the borders as precisely as possible. Thanks to an unprecedented technological investment that UTSW is leading in North Texas, certain hand-in-glove approaches that blend surgery with radiation are increasingly offering patients a more comprehensive way of treating their diseases. UT Southwestern is building a mecca for the latest in disease-fighting technologies, designed to take the fight against cancer to the subatomic level. The VERO – a highly advanced stereotactic body radiation therapy (SBRT) device and the only one of its kind in the Western Hemisphere – started whirring and treating patients with its ultraprecise radiation beam in 2012. SBRT involves multiple beams focused on a targeted area in a three-dimensional space, similar to the “surround sound” of a home entertainment system, where the viewer is centrally seated. Dr. Robert Timmerman, Professor of Radiation Oncology and Neurological Surgery, is using SBRT to study and treat lung cancer, 34 while building on data that show a certain tumor-inhibiting compound developed at UT Southwestern has a heightened effect when combined with SBRT, but not with conventional radiation treatment. Researchers at UT Southwestern already have shown that the compound bavituximab not only will inhibit the development of blood vessels supplying a tumor, but will attack the tumor more aggressively following treatment with the more potent form of SBRT radiation offered via the VERO. In broadening its arsenal of radiation oncology treatments, UT Southwestern is considering the possibility of opening a stateof-the-art proton therapy center for North Texas. Subject to future approval by the UT System Board of Regents, the $220 million, 108,000-square-foot center would be funded and owned by San Diego-based Advanced Particle Therapy, and would be operated by UT Southwestern physicians and staff. It would feature five treatment vaults, as well as laboratory space for researchers. The heart of the new proton facility would be a particle accelerator capable of speeding up protons to a super-fast velocity – roughly 112,000 miles per second or 60 percent of the speed of light. As one of the most advanced radiation treatment technologies available, proton therapy offers a more precise and aggressive approach to destroying cancerous tumors than conventional X-ray radiation. Proton therapy’s controlled beam of protons can be deposited, because of its heavier mass, on a specific target with less collateral damage. “A proton center here would offer patients in the region access to the best possible treatment options while providing us with an unparalleled opportunity to study and apply this technology,” said Dr. Hak Choy, Chairman of Radiation Oncology. “The precision of the proton beam allows for unprecedented focus and intensity, especially in kids where access can be anatomically much tighter.” Claire Mendenhall, Director of Radiation Oncology Services; Dr. Timothy Solberg, Professor of Radiation Oncology P and Radiology; and Dr. Hak Choy, Chairman of Radiation rotecting future generations, near and far Whether the healing touch is 100 miles away or a mere 10 feet, UT Southwestern’s footprint in technology applied to research and patient care is growing with an intensity that points to an even brighter future ahead. But for patients facing an uncertain one, caretakers can take heart in the simple wisdom of patients themselves. “I don’t let any preoccupations about the future get in the way of doing the most I can in a given day,” said Mrs. Clinesmith, who was delighted to find she had not passed a genetic risk for cancer to her sons. As for Mrs. Nail, her new line of work has proved physically demanding, but well within her capability after her surgery. “Being a massage therapist, sometimes you have to put your whole weight into the massage, to get deep into the tissue,” Mrs. Nail said. “It turns out that I was able to do that fairly quickly after robotic surgery. Oncology, hold plans for the proposed proton center. “That heavy machinery with a delicate touch – and the people behind it – made a big difference.” Dr. Choy holds the Nancy B. and Jake L. Hamon Distinguished Chair in Therapeutic Oncology Research. Dr. Kernstine holds the Robert Tucker Hayes Foundation Distinguished Chair in Cardiothoracic Surgery. Dr. Timmerman holds the Effie Marie Cain Distinguished Chair in Cancer Therapy Research. Dr. Euhus holds the Marilyn R. Corrigan Distinguished Chair in Breast Cancer Surgery. Dr. Scott holds the Frank H. Kidd Jr., M.D., Distinguished Professorship in Surgery. Dr. Rege holds the Hall and Mary Lucile Shannon Distinguished Chair in Surgery. SOUTHWESTERN MEDICINE 35 By Jan Jarvis and Lisa Warshaw Carolyn Swann “Our multidisciplinary team approach creates a close relationship with patients, providing both cutting-edge and patient-centered care to an increasing number of transplant patients.” - Carolyn Swann, Associate Vice President for Heart, Lung, and Vascular, and Solid Organ Transplant Services 38 It was Dec. 26, and Randy Gideon was waking up from his bilateral lung transplant. Laid up and heavily sedated in the intensive care unit, the well-known Fort Worth architect was surrounded by machines with tubes spilling from his torso. “When I came to, I had this ‘ah-ha’ conscious moment. I could breathe. I still remember how unbelievable it felt to take a deep breath,” Mr. Gideon said. Just a few feet away, on the other side of the glass window, the transplant team was huddled. Transplant coordinator, pharmacist, social worker, dietitian, physical therapist, nurse, surgeon, and transplant physician were all there discussing Mr. Gideon’s case – just as they do for every transplant patient at UT Southwestern Medical Center. It takes a robust multidisciplinary team of medical experts to save lives. In all, some 50 people envelop transplant recipients, providing the compass to guide them through their health crises and to support them long after they leave the hospital. “As an academic medical center, we bring advanced research to the bedside, benefiting patients who come to our institution with few remaining alternatives,” said Carolyn Swann, Associate Vice President for Heart, Lung, and Vascular, and Solid Organ Transplant Services. “Our multidisciplinary team approach creates a close relationship with patients, providing both cutting-edge and patient-centered care to an increasing number of transplant patients.” UT Southwestern is nationally recognized and repeatedly honored for its transplant program, which is among the most comprehensive in the nation. Its lung transplant program ranks among the highest in one-year and three-year survival rates after transplantation, according to the Scientific Registry of Transplant Patients. UT Southwestern, which began its lung transplantation program in 1990, has an 84 percent survival rate one year after surgery and a 70 percent survival rate three years after surgery. And now, with established programs for heart, lung, kidney, and liver, UT Southwestern is pushing the limits of medicine with the recent approval for hand transplants. Since its organ transplant program began, hundreds of patients in end-stage organ failure have received a second lease on life. During their transplant journey, they are put at the center of a world-class transplant team. Financial coordinators help them wade through the mountains of insurance-related paperwork. Speech pathologists assist lungtransplant patients with re-learning to swallow after surgery. And then there are the team members who work on the front lines with patients to help ease the burden of undergoing a lifechanging surgery. The Transplant Coordinator The transplant coordinator is the person who makes the call at 2 a.m. and says, “We have an organ for you!” Mr. Gideon nearly missed his call. His wife, Beth, had mistakenly turned the phones on vibrate. It was only when he heard the continuous hum of the vibration that he persuaded his wife to check her phone. His Christmas gift had arrived a day late. A familiar voice was on the other end. Although 20 minutes had passed, there was still time for him to make it, Senior Transplant Coordinator Melanie Alford assured him. The couple would have to pack extra oxygen tanks in their car just to make the drive from Fort Worth to Dallas, but they would get there. And Ms. Alford would be waiting to greet them upon arrival. Long before a transplant coordinator makes the call announcing an organ has been located, she already has established a special bond with the recipient. “From the moment we meet, we begin a lifetime relationship,” Ms. Alford said. “We spend long hours and long days with these patients. It’s a labor of love.” The transplant coordinator is the direct point of contact, helping patients survive until they get their organ. “Sadly, people on the waiting list can die, so we want to do everything we can to keep that from happening,” said Laura Restall, Senior Transplant Coordinator. The bond strengthens when patients go home. “We teach them how to live post-transplant,” Ms. Alford said. “Our goal is to help patients recover as much health and vitality as possible.” Each patient leaves a lasting impression on the transplant team. “Before his transplant, there was one young man who could barely walk across the room without needing oxygen,” said Marcie Buford, Senior Lung Transplant Coordinator. “Then one day I saw him running down the hallway. That’s when you know you’re making a difference,” she said. The Pharmacist Transplant patients fight organ rejection right from the start. Helping prevent infection and resist rejection is a balancing act that falls in part to the pharmacists, who walk a tightrope as patients deal with an onslaught of medications. It takes a medicine cabinet full of drugs to keep a person thriving following a transplant. “The first cup they take has 12 to 15 pills in it,” said Dr. Sarah Wright, Transplant Pharmacist. Lung transplant patient Randy Gideon spends 30 minutes each week organizing his pills into daily doses. Patients meet with the pharmacists prior to hospital discharge to learn what the pills look like, their purpose, dosage, and when to take them. “Teaching patients about their new meds is one of my favorite things about my job,” Dr. Wright said. “You see the panic on their face when they’re confronted with all these pills, but I’m able to help them become well-educated and comfortable with their new medications.” “We are a bridge over troubled waters. And when the waters are the roughest, we pull out our bag of tricks. Pick the day, we work miracles.” - April Morgan, Transplant Social Worker April Morgan SOUTHWESTERN MEDICINE 39 It can get complex quickly. Pharmacists must be aware of how all the medications interact, including over-the-counter and prescription drugs that patients also may be taking. If a drug is not covered by insurance, Dr. Wright will work in conjunction with the physicians, coordinators, and social workers to search for a less-expensive, but equally effective alternative. Pharmacists helped Mr. Gideon fine-tune the dosage of the anti-rejection medication cyclosporine, which came in liquid form and must be taken at specific times during the day. Taking the liquid form limited his ability to go out in public, but when he was switched to capsules, his post-transplant life got easier. “I still have to go out with a backpack full of medicine, but I now can go out and watch my son play baseball,” Mr. Gideon said. The Social Worker From conducting psychological assessments to helping family members file medical-leave paperwork, social workers are at the forefront of patient advocacy. Need a place to stay close “I had one patient who didn’t believe she would ever walk again. But she did; little by little, she got stronger.” - Rebecca Parnell, Physical Therapist to the hospital? Ask a social worker. Need help with exorbitant medication costs? A social worker can help with that, too. “We are a bridge over troubled waters,” said April Morgan, Transplant Social Worker. “And when the waters are the roughest, we pull out our bag of tricks. Pick the day, we work miracles.” Consider the potential liver transplant patient who was turned down by other institutions because he was aggressive and combative. In his most desperate moment, he turned to UT Southwestern, where social workers proved he deserved a second chance. He got it. “Surgeons and physicians on the team carry the weight of the responsibility,” Mrs. Morgan said. “But to a family with no place to stay, no food to eat, and a general lack of concrete resources, the care social workers provide means just as much.” “Surgeons and physicians carry the weight of the responsibility on the team,” Mrs. Morgan said. “But to a family with no place to stay, no food to eat, and a general lack of concrete resources, the care social workers provide means just as much.” 40 The Dietitian What is the one food transplant patients can’t eat? Grapefruit. It interferes with the essential anti-rejection medication. For a transplant patient, a baked potato is a healthy food choice. “It has half the potassium a kidney patient needs for the day,” said Lynn Henderson, Registered Dietitian. Without a dietitian teaching patients how to eat after a transplant, organ recipients can easily make some dangerous choices. Long before a transplant occurs, dietitians are busy individualizing a nutrition plan and helping recipients learn to make healthy choices. When someone needs to lose or gain weight, dieticians are there to help. If a person’s body mass index (BMI) is too high, a nutritionist can work with them to lower it to an acceptable level in order to get on the organ list. “A lot of fat in the mid-section makes surgery more difficult,” said Francis Dang, Registered Dietitian. An acceptable BMI for a lung transplant patient is less than 30. For a heart and kidney patient, it is less than 35. But it goes up to 40 for a liver patient. A normal BMI is between 18.5 and 24.9. Post-transplant patients need to take dietary precautions to counterbalance the side effects of their medications. Increased blood pressure, high cholesterol, and weight gain are among the issues addressed by nutritionists. “We help patients make better dietary decisions,” Ms. Dang said. Pulmonary fibrosis had ravaged Mr. Gideon’s lungs, leaving him inactive and 40 pounds underweight. Dietitians counseled him on weight gain measures he could take at home, in conjunction with the exercise regimen prescribed by physical therapists. The Physical Therapist “When I left the hospital, I was so weak that stepping up a curb was almost unimaginable,” Mr. Gideon said. Like many lung transplant recipients, Mr. Gideon had lost every shred of strength and stamina. Not surprisingly, lung transplant patients often are apprehensive when they start pulmonary rehabilitation. Sometimes they come in using a wheelchair, said Rebecca Parnell, a Physical Therapist who works with lung transplant recipients. “They have that scared, deer-in-the-headlights look,” she said, “But when they leave, they are already walking a mile.” Mrs. Parnell is firm but gentle as she teaches patients exercises to restore their range of motion, to increase their strength, and to improve their balance. Their bodies are not used to any activity after months of bed rest. “The beautiful thing about the body is that it adapts to stress,” Mrs. Parnell said. “My job is to stress them at a safe level.” Patients face a lot of peaks and valleys during their journey toward recovery, but if they don’t give up, they will be able to accomplish their goals. “I had one patient who didn’t believe she would ever walk again,” Mrs. Parnell said. “But she did; little by little, she got stronger.” Mr. Gideon hopes that with time and hard work, he, too, will regain his strength. “Transplant changes you physically and emotionally and in lots of ways you don’t realize until you’re into it,” he said. “I was really into fly fishing, and I hope to do it again. I’ve just got to get my stamina back and feel like I have the strength to stand in a river or ocean.” Rebecca Parnell, Physical Therapist SOUTHWESTERN MEDICINE 41 UTSW transplant programs offer hope and the chance of a new life Multidisciplinary transplant teams have made the difference in hundreds of patients’ lives. Whether monitoring the condition of a donor heart that offers the last chance for a dying patient or offering an amputee the opportunity to once again caress his child’s cheek, UT Southwestern's teams continue to provide the best in patient care so transplant recipients can lead healthier and more productive lives. Heart transplant patient Stephen Lund with Dr. Joseph Mishkin HEART TRANSPLANT Fighting to save a life Stephen Lund arrived at UT Southwestern wearing a birthday hat and holding a party horn. The celebratory occasion was the first birthday of his new heart. The 62-year-old Tyler resident first came to UT Southwestern when doctors in his area could no longer help him. His case was too severe. He urgently needed a heart transplant, but his organs were failing one by one. Doctors couldn’t put him on the waiting list for a new heart until his vitals showed improvement. “Everything was shutting down,” Mr. Lund said. “People were counseling my wife and our three children. They were essentially planning my funeral.” But his UT Southwestern doctors wouldn’t give up. They placed a temporary left ventricular assist device (LVAD) in Mr. Lund’s chest to ease his ailing heart and to give his other organs a chance to recover. 42 Dr. Joseph Mishkin, Assistant Professor of Internal Medicine, stayed up 40 hours straight to monitor Mr. Lund’s progress, hoping the LVAD would turn the state of his organs around. It did. Mr. Lund was put on the waiting list. Three days later, the call came. There was a heart that matched Mr. Lund’s specifications. The problem was the donor organ appeared overstressed and not viable. But Dr. Mishkin persisted. He chose to monitor the organ, and his patience was rewarded. Its statistics improved, making it a viable option for his patient. “They are all an amazing group of people,” Mr. Lund said of his UT Southwestern caregivers. “Their knowledge and their medical ability is unrivaled. But their personal care is just as important as, or more important than, the other.” Said Dr. Mishkin: “This was a group effort. The entire transplant team was fighting to save this man’s life.” Lisa Warshaw KIDNEY TRANSPLANT A stroke of luck In 2001, an accident turned into a stroke of luck for Billy Mark Munkres. “When I went to the doctor, he did an X-ray of my ribs and told me I didn’t have any broken bones,” said Mr. Munkres, then 35. “But he saw something on the kidney – I had cancer.” Mr. Munkres, who lives in Omaha, Texas, was referred to UT Southwestern Medical Center, where his misfortune led to a lifesaving surgery to remove his kidney. If the accident had not occurred, his cancer might have progressed. The odds of discovering that he had von Hippel-Lindau syndrome, a genetic disorder that causes the abnormal growth of tumors, were even more remote. Although he recovered quickly, Mr. Munkres was warned that the disorder likely would lead to more tumors. After a decade of monitoring, that prediction became reality. Only this time, Mr. Munkres would need a transplant after the removal of his remain- ing kidney. In October 2012, he became one of a growing number of patients at UT Southwestern to undergo a kidney transplant from a living donor. In Mr. Munkres' case, it was someone he had known for years. “It was such a blessing,” he said. “Most people wait five or six years for a kidney, but I was really fortunate to have such a good friend.” In some ways, Mr. Munkres’ luck goes beyond friendship. At UT Southwestern, he found a dynamic, nationally recognized kidney transplant program. Since 2007, there have been more than 200 kidney transplants performed at UT Southwestern. Physicians from UT Southwestern performed the first kidney transplant in Texas in 1964. “We set the bar very high,” said Dr. Jason Schwartz, Associate Professor of Surgery. “Our goal is to be the premier program in the region.” Jan Jarvis “It was such a blessing. Most people wait five or six years for a kidney, but I was really fortunate to have such a good friend.” - Billy Mark Munkres, kidney transplant patient SOUTHWESTERN MEDICINE 43 Dr. Juan Arenas (second from left) with a group of medical students LIVER TRANSPLANT Increasing the donor pool While she waited for a liver transplant, Kelli Lee Yonker was admitted to St. Paul University Hospital at least a dozen times in 10 months. “I would black out,” she said. “Toxins would build up in my body, and I just wouldn’t wake up.” Twice, she got the call that a liver transplant was available, only to learn that the organ was not a match. As her weight plunged, the school librarian held onto her belief that she eventually would get a transplant. On Sept. 4, 2011, she did. “I’ve been perfectly fine ever since, but I know I would not be here if not for the wonderful nurses and doctors at UT Southwestern,” she said. “They were so warm and welcoming.” 44 Since 2007, the UT Southwestern transplant team has performed more than 80 liver transplants. One of the immediate priorities is improving organ donations so more lives can be saved, said Dr. Juan Arenas, Chief of Surgical Transplantation. “Nationally, the donor pool has become very stagnant in the last 10 years,” he said. “It remains fixed, which leads to high mortality.” Still, the outlook is positive, Dr. Arenas said. “With the careful selection of candidates, improvements in immunosuppressants, and new treatments, liver transplantation is now probably the best it has ever been,” he said. The focus will continue to be on saving lives and giving patients such as Mrs. Yonker a second chance. “People who see me now cannot believe the difference,” she said. “I am very, very lucky to have found the right liver transplant surgeons to do such a good job.” Jan Jarvis HAND TRANSPLANT A life-changing option Hands grasp a steering wheel, fix dinner, screw in a light bulb, and perform hundreds of tasks each day. But when someone loses a hand to an accident or illness, that’s not what they miss most. It’s the sense of touch, said Dr. Tae Chong, Assistant Professor of Plastic Surgery and director of the reconstructive transplant program at UT Southwestern. “They want to feel their baby’s face or their spouse’s hand,” he said. Through the UT Southwestern Reconstructive Hand Transplant Program, amputees have the opportunity to do exactly that. The program is the first in the region to offer transplantation to those who have lost one or both hands below the elbow. Worldwide, more than 70 hands have been transplanted on 50 patients. UT Southwestern has set the groundwork and is ready to join the elite group of medical centers in this country that are dedicated to providing amputees with a life-changing option. Having already been successful with solid organ transplants, UT Southwestern is poised to expand with this state-of-the-art hand program, said Dr. Rod Rohrich, Chairman of Plastic Surgery. “Hand transplantation is in the forefront of modern medicine due to breakthroughs in technology and immunology,” he said. The program also meets a growing need because of injuries that occurred during the wars in Iraq and Afghanistan. “We have vets returning with no arms or legs due to body armor, which saves lives but not limbs,” Dr. Rohrich said. Dr. Rohrich holds the Betty and Warren Woodward Chair in Plastic and Reconstructive Surgery and the Crystal Charity Ball Distinguished Chair in Plastic Surgery. Jan Jarvis When someone loses a hand to an accident or illness, that’s not what they miss most. It’s the sense of touch. “They want to feel their baby’s face or their spouse’s hand.” - Dr. Tae Chong, Assistant Professor of Plastic Surgery and director of the reconstructive transplant program at UT Southwestern Dr. Tae Chong demonstrates a color wheel to match skin tones. SOUTHWESTERN MEDICINE 45 THE CLINICAL FRONTIER (special section) How a nursery rhyme saves lives By Lisa Warshaw When the school bell rang, Derrick Ephraim’s heart stopped beating. The 41-year-old middle school gym teacher suffered a heart attack in 2011. “You never know when it is coming,” Mr. Ephraim said. “It just snuck up on me. I’m young and active; cardiac arrest was far from my thoughts.” Co-workers called 911 and performed cardiopulminary resuscitation (CPR) as they waited for emergency personnel. Paramedics eventually resuscitated Mr. Ephraim, thanks in part to techniques pioneered at UT Southwestern Medical Center. In fact, dramatically improved survival rates for cardiac arrest victims throughout North Texas can be credited in part for the research led by UT Southwestern’s Dallas-Fort Worth Center for Resuscitation Research – part of the Resuscitation Outcomes Consortium (ROC). Beginning in 2008, DFW-based emergency responders have been trained to perform a minimally interrupted chest compression method of CPR. This method, which performs compressions at a specific, constant rate, significantly improves the chances of returning a pulse to victims following cardiac arrest. 46 Dr. Ahamed Idris, Professor of Surgery (specializing in Emergency Medicine) and Internal Medicine at UT Southwestern, set out to discover whether the rate of chest compressions used by first responders affected the outcome of resuscitation. He found out it does. The study’s findings pinpoint a sweet spot for the number of chest compressions performed each minute on cardiac-arrest victims. “Performing chest compressions too slow or too fast yields a substantially lower chance of restoring a heartbeat,” Dr. Idris said. “Research indicates that a rate of 100 to 120 chest compressions per minute is exactly where you need to be in order to increase survival.” Today, Mr. Ephraim is among the many whose lives have been saved thanks in part to this research. By training its first responders to maintain the proper rate of chest compressions, the city of Mesquite has seen a fourfold increase in the survival rate over a five-year period – from 3 percent in 2006 to 12 percent in 2011. The city of Carrollton saw a 340 percent increase in survival rates – from 4 percent in 2006 to 14 percent in 2011. Dallas went from 3.9 percent in 2006 to 9.4 percent in 2011 – a 141 percent increase. Area first responders were trained on the chest compression method, and trained again. “We kept training them until we saw the results we wanted,” Dr. Idris said. “Today, the results are outstanding. I’m thrilled.” Some paramedics use a metronome to keep the beat. Repeatedly singing the popular children’s nursery rhyme, “Row, Row, Row Your Boat,” also helps keep the rate of chest compression in the recommended sweet spot, Dr. Idris said. The study tracked CPR efforts by rescue units in DFW and nine other metropolitan areas: Seattle, Portland, Ore., San Diego, Dallas, Milwaukee, and Pittsburgh, in addition to three Canadian cities: Vancouver, Toronto, and Ottawa. Since data collection began more than six years ago, ROC's database has compiled information from 175,000 patients, including 20,000 from the DFW region, which includes eight cities, 31 hospitals, six trauma centers, and more than 5,000 first responders. “Our research outcomes may guide the future training of first responders. The implications of this study are destined to have global repercussions,” Dr. Idris said. Fighting cancer while preserving fertility By Jan Jarvis Camerine Day dreamed of having two children with her husband, Matt, a high school biology teacher. But in a single October afternoon, those dreams evaporated when a Pap test showed something suspicious. A cone biopsy in December followed, and the results turned out to be far worse than the personal trainer ever imagined. She had cervical cancer. “I was 24 years old and had just gotten married,” Mrs. Day said. “It was so depressing to be told I’d never be able to have kids.” After her physician insisted that a hysterectomy was her only option, she turned to her grandparents for advice. They suggested she contact UT Southwestern Medical Center with the hope that gynecological oncologists there could offer an alternative to a radical hysterectomy that would end all chances of her ever having a child. “All I really wanted was someone to try,” Mrs. Day said. She found that someone in Dr. Siobhan Kehoe, Assistant Professor of Obstetrics and Gynecology. Dr. Kehoe is among a small but growing number of physicians in the U.S. who are blazing new frontiers in fertility preservation. Advances in fertility-sparing procedures are allowing physicians such as Dr. Kehoe to treat cancer while enhancing the patient’s quality of life. UT Southwestern is among a handful of medical institutions in the country offering fertility-sparing techniques for gynecological cancer patients such as Mrs. Day. Each year, about 12,200 women in the U.S. are diagnosed with cervical cancer, 42 percent of them under the age of 45. Endometrial cancer, which typically strikes older women, also is being diagnosed in a growing number of younger patients, who might benefit from fertility-sparing procedures. Among the 47,000 women in the U.S. with endometrial cancer, about 10 percent are of child-bearing age. A month after her diagnosis with adenocarcinoma, Mrs. Day became the first patient at UT Southwestern to undergo a radical trachelectomy, a delicate procedure that involves the removal of the cervix while preserving the uterus. Before a trachelectomy is performed, the lymph nodes in the pelvic area are removed to determine if the cancer has spread. If cancer is found, a hysterectomy must be performed. Otherwise, the surgeon removes the cervix and part of the vagina. The uterus is then attached to what remains of the vagina. The cervix is replaced with a cerclage, a type of suture placed in the lower uterus to hold any future pregnancies in place. “It’s a challenging procedure, but these women are so young, and this procedure allows them to have the cancer treated appropriately while preserving their fertility,” Dr. Kehoe said. Being diagnosed with cancer is a shock at any age. For young women who want to have a family, the loss may be compounded by the feeling that their purpose in life is gone, said Dr. Jeff Kendall, Associate Professor of Psychiatry at the Harold C. Simmons Comprehensive Cancer Center. “It’s a challenging procedure, but these women are so young, and they want to preserve their fertility.” —Dr. Siobhan Kehoe SOUTHWESTERN MEDICINE 47 THE CLINICAL FRONTIER (special section) “We originally wanted two kids, but after all this, if we get just one I’ll be so happy.” —Camerine Day “Cancer changes their life goals and dreams,” he said. “It forces them to go in a different direction.” With fertility-preserving procedures, at least one of the challenges they face as cancer survivors is removed, Dr. Kendall said. That doesn’t mean they don’t grapple with the same fears that other cancer patients do, he said. “Their life is still changed by the diagnosis,” Dr. Kendall said. “The difference is they don’t have to realign their goal of having a family.” Still, other fears arise, most commonly the concern that the more fertility-sparing treatment will put them at a greater risk for cancer later in life. “Most young patients want to preserve their fertility,” Dr. Kehoe said. “But they also want to know they’re cured.” It doesn’t have to be an either-or decision. Radical trachelectomy has been shown to be just as effective as a radical hysterectomy for women with early-stage cancer. That should help put some women’s minds at ease when weighing the pros and cons of the treatment. Mrs. Day, who has been given the green light to try getting pregnant, said she’s just grateful for the chance. “We originally wanted two kids, but after all this, if we get just one I’ll be so happy,” she said. Solving the SCID puzzle to help sick babies By Jan Jarvis Photos of beautiful babies with chubby cheeks and bright eyes fill the office of Dr. Maite de la Morena, Associate Professor of Pediatrics and Internal Medicine at UT Southwestern Medical Center. But their robust appearance sometimes defies reality. In some cases, these are children who appear healthy at birth, but then at around three months, get an infection. “They get sicker and sicker and never recover,” said Dr. de la Morena, Director of the Jeffrey Modell Primary Immunodeficiency Center at Children’s Medical Center Dallas. For decades, parents have buried these babies without ever knowing the reason why. But that sad scenario is changing. Today at UT Southwestern, a multidisciplinary team of physicians and researchers not only has the answer to why these babies get so sick, but it has the expertise to save their lives. With the addition of a new statewide screening program, 48 these babies can be diagnosed and treated before they ever get sick. The complex puzzle known as severe combined immunodeficiency, or SCID, is no longer the mystery it was 40 years ago. Then the only way to dodge death was to live in a sterile container as the so-called “bubble boy” did until his death at age 12. UT Southwestern experts now are able to offer hope to families facing this difficult diagnosis. Children born with SCID have little or no immune system to fight off illness. The most common type of SCID is caused by a gene found on the X chromosome and affects only males. The first sign that something is wrong occurs when the baby develops a common childhood illness. Such was case with Carter Smith, who was the picture of health until he got diarrhea when he was 3 months old. Severe dehydration and fever followed. After receiving intravenous fluids for several days at a regional medical center, Carter did not bounce back. By the time he was referred to Children’s Medical Center, Carter had pneumonia and was a very sick little boy. “We were afraid he was going to die,” said Pete Smith, Carter’s father. Within a day of Dr. de la Morena seeing Carter, a blood test confirmed the diagnosis of SCID. Mr. Smith said they were lucky to find Dr. de la Morena when they did. Since SCID is rare, experts able to diagnose it quickly are uncommon. “We feel like it was the grace of God that we ended up here,” he said. To help the Smiths make the journey from diagnosis to treatment and ultimate recovery took a team from various disciplines that guided the family at every step. “When we found out what Carter had, I thought it was imminent death,” Mr. Smith said. “I had no idea what to do next.” What came next was a stem cell transplant, in which cells were taken from the bone marrow of Carter’s mother and introduced into the baby. The expectation is that the new cells will rebuild the immune system, said Dr. Andrew Koh, Assistant Professor of Pediatrics and Microbiology in the Harold C. Simmons Comprehensive Cancer Center. “This is the only true remedy for SCID,” he said. The disease affects only 1 in 125,000 children. By the time a child is diagnosed, he’s often too sick for a transplant, Dr. de la Morena said. “If a child can get a transplant when they’re still healthy, the chances of survival and leading a normal life are very good,” she said. The outlook for babies with SCID is getting brighter. In 2012, Texas added SCID to the list of 28 diseases that all newborns in the state are screened for at birth. A baby with an abnormal screening test is referred to a pediatric immunologist, which in the North Texas region would most likely be Dr. de la Morena. By screening babies at birth, SCID can be diagnosed before 3 months of age, when a bone marrow transplant promises the best chance for survival, said Dr. Franklin Fuda, Assistant Professor of Pathology. “After three months, you have missed that window of opportunity,” he said. “But if you catch it at birth, you can treat these kids in a timely fashion, and they do very well.” Carter was fortunate. He’s now a healthy little boy who celebrated his fifth birthday in October 2012. “He’s a real success story, and a lot of it has to do with the doctors who treated him,” Mr. Smith said. “It was a team effort to find the solution. I can’t say enough about this group.” SOUTHWESTERN MEDICINE 49 THE CLINICAL FRONTIER (special section) Living without pain By Russell Rian “Pain management has multiple goals, but I think it really depends on the patient’s goal.” —Dr. Carl Noe 50 The true toll of chronic pain isn’t revealed in the numbers alone – 100 million adults in the U.S. suffer from it at an estimated cost of $635 billion. The real impact comes individually, revealed perhaps in a gasp and a grimace. So while the pain management field continually evolves with new treatments, therapies, and medicines, any strategy must be centered on the patient, said Dr. Carl Noe, Director of UT Southwestern’s Eugene McDermott Center for Pain Management. “Pain management has multiple goals, but I think it really depends on the patient’s goal,” said Dr. Noe, Professor of Anesthesiology and Pain Management. “How the pain affects the individual, and his or her life and livelihood, is critical. If your small finger on a nondominant hand hurts, that’s not the same as if you’re a violinist, and that pain is disabling. So we tailor treatments to the individual’s goals.” The McDermott Center uses the latest scientific advances and procedures to diagnose, locate, and treat everything from back pain to abdominal pain, foot pain to headaches. The Center covers adult and pediatric pain management, cancer pain management, and interventional therapies such as minimally invasive procedures for back pain and other pain syndromes. While the list of chronic and acute pains is formidable, so is the Center’s arsenal to quell them. Minimally invasive options can involve painspecific nerve-block agents applied to joints and nerves, or fully implantable, programmable drug pumps for chronic pain that help reduce site infections and promote independence. Minimally invasive surgeries are done routinely in order to remove scar tissue – a process called lysis of adhesion – and to alleviate pain in people with back or neck problems. Other procedures include pulse radiofrequency, which heats and destroys nerve endings to interrupt pain messaging signals to the brain, and vertebroplasty, a surgical cement injected into injured or fractured spines. Interdisciplinary programs for back pain, chronic pain, and medication reduction have been developed over the past two years. They include medical pain management, behavioral medicine, and physical therapy. The majority of treatments at the Center are for back pain, arthritis, headaches, and cancerrelated pain. But what sets the McDermott Center for Pain Management apart is the forceful combination of therapy and unique research that provides access to the latest techniques and technologies. “There’s nothing like our Center,” said Dr. Noe, who has been the author or co-author of numerous publications in the field. For some, pain management was often a temporary fix to a chronic problem. But Texas Instruments co-founder Eugene McDermott and his family envisioned something better. Mr. McDermott showed appreciation of the pain management field early on with contributions to sponsor visiting professorships, student scholarships and lectures, and underwriting anesthesia research and the development of monitoring equipment in the field of anesthesiology. “The critical contributions of the McDermotts cannot be understated. The research and care they have underwritten have had a substantial and tangible effect in alleviating the pain and suffering of thousands who have found relief at the Center over the years,” said Dr. Charles Whitten, Chairman of Anesthesiology and Pain Management. The McDermott Center for Pain Management was among the first facilities of its kind to launch a coordinated attack on chronic pain by joining multiple disciplines from the Departments of Anesthesiology and Pain Management, Physical Medicine and Rehabilitation, and Psychiatry. It has evolved into the longest running interdisciplinary program in the DallasFort Worth area, as well as the region’s only endowed pain management center. Dr. Whitten holds the Margaret Milam McDermott Distinguished Chair in Anesthesiology and Pain Management. Finish 2 A R N E N V 0 1 2 U A L I E W 52 HIGHLIGHTS OF THE YEAR 42 62 FINANCIAL STATEMENT 44 65 GIFT REPORT 53 55 SOUTHWESTERN MEDICINE 51 H I G H L I G H T S of the year FA L L 2011 QUICK USE OF DEFIBRILLATOR MAKES DIFFERENCE Paramedics who deliver defibrillator shocks within three minutes of arriving at the scene of a cardiac arrest can boost survival rates in some cases, a clinical study involving UT Southwestern emergency physicians revealed. More people with a potentially fatal abnormal heart rhythm called ventricular fibrillation survive when paramedics perform cardiopulmonary resuscitation while setting up defibrillator machines, then deliver electrical shocks within three minutes of arrival. The real-world findings involved Dr. Ahamed Idris, Professor of Emergency Medicine and Internal Medicine, and were reported in The New England Journal of Medicine. Dr. Idris heads the Dallas-Fort Worth arm of the Resuscitation Outcomes Consortium, funded by the National Institutes of THE WORK OF DRS. AHAMED IDRIS AND LYNN ROPPOLO, ASSOCIATE PROFESSOR OF SURGERY, IS ELEVATING FIRST-RESPONSE CARE FOR CARDIAC ARRESTS. 52 Health. The consortium is a $120 million joint U.S. - Canadian series of clinical trials aimed at identifying the best on-scene practices for traumas and cardiac-arrest cases. The Dallas-Fort Worth arm has the highest participation in the U.S., with about 4,500 people enrolled annually. Dr. Idris, a pioneer in resuscitation research, has helped revolutionize the list of critical steps that paramedics should take within a few minutes. RESEARCHERS SHOW NUMEROUS MUTATIONS led to a key step in cancer development called anchorage-independent growth, meaning cells piled up on top of each DR. JERRY SHAY other rather than aligning neatly. The groundbreaking investigation was selected by the Faculty of 1000 – an international group of leading scientists and researchers – to be recognized in the top 2 percent of published articles in biology and medicine. LEAD TO COLON CANCER UT Southwestern scientists reported there are at least 70 genetic mutations involved in the formation of colon cancer, far more than previously thought. The researchers, led by Dr. Jerry Shay, Professor of Cell Biology, suggest a new approach to colon cancer treatments – targeting multiple genes and pathways simultaneously. Current cancer treatments target just one or two known cancerdriver genes. While patients may get transient tumor burden reduction, tumor growth almost always returns. UTSW’s research contradicts previous thinking that only a few mutated genes are important in the development of cancerous tumors. Under the old model, scientists believed there were 151 candidate genes and that mutations in just eight to 15 of them would lead to cancer. According to the investigation at UT Southwestern, mutations to these candidate genes play significant roles in cancer development. Inactivating the function of any of these tumor-suppressing genes COMPOUND KILLS DANGEROUS INFLUENZA STRAIN A compound tested by scientists at UT Southwestern destroys several viruses, including the deadly Spanish flu that killed an estimated 30 million people in the worldwide pandemic of 1918. This compound – which acts by increasing the levels of a human anti-viral protein – potentially could be developed into a new drug to combat the flu, a virus that tends to mutate into strains resistant to antiinfluenza drugs. Dr. Beatriz Fontoura, Professor of Cell Biology, said that while current drugs act on the virus, investigators at UTSW were working to uplift a DR. BEATRIZ host/human FONTOURA anti-viral response at the cellular level. In cell testing done in New York, the compound successfully H I G H L I G H T S HIGH HOPES POUR INTO CLEMENTS UNIVERSITY HOSPITAL I n a special onsite ceremony, the CONSTRUCTION OF THE WILLIAM P. CLEMENTS JR. UNIVERSITY HOSPITAL IS CHANGING THE NORTH CAMPUS SKYLINE. knocked out three types of influenza as well as a smallpoxrelated virus and an animal virus. The compound is among others that the research team is testing that induce an infectionfighting human protein called REDD1. The scientists discovered the protein is a key human barrier for infection. In all, the UT Southwestern-led research team tested 200,000 compounds for those that would inhibit flu virus infection. A total of 71 were identified. According to the National Institutes of Health, influenza hospitalizes more than 200,000 people in the U.S. each year, with about 36,000 fatalities related to the illness. Worldwide, flu kills about 500,000 people annually. hopes and aspirations of 1,000 UT Southwestern employees, donors, and community supporters were poured into the foundation of the new University Hospital, an $800 million stateof-the-art facility slated to open in late 2014. October’s foundation-laying event commemorated a key milestone for the construction of the new facility, which began in March 2011 with site preparation. The 12-floor, 460-bed hospital is an essential step in UT Southwestern’s strategy to become one of the nation’s top 10 comprehensive academic medical centers. By late winter, UT Southwestern leaders had announced that the new building on a 32-acre site on the southwest side of Harry Hines Boulevard between Mockingbird Lane and Inwood Road will be named the William P. Clements Jr. University Hospital. The name honors legendary Texas Gov. William P. Clements Jr., who died in May 2011, in recognition of his 2009 gift of $100 million to the Southwestern Medical Foundation, the largest single gift for the benefit of UT Southwestern in the institution’s history. UTSW President Dr. Daniel K. Podolsky said the Medical Center was deeply honored by Mr. Clements’ confidence, shown through the unrestricted gift, and “proud to name the new hospital in commemoration of a true Texas giant, certain that it will have the transformational effect he envisioned.” SOUTHWESTERN MEDICINE 53 H WINTER 2011-2012 ZALE LIPSHY’S PATIENT CARE GETS NATIONAL PRAISE UT Southwestern was the nation’s only academic medical center to win two major patient satisfaction awards – the Patient Voice Award and the Summit Award for inpatient services – from Press Ganey, a national consulting firm specializing in health care performance. Both awards recognized outstanding care provided to patients at Zale Lipshy University Hospital. Executive Vice President for Health System Affairs Dr. Bruce Meyer said that the findings – through patient feedback – reflect the consistent excellence UTSW strives to deliver to patients through its team-care approach. Press Ganey selected Patient Voice Award winners based on federal data that measures patient satisfaction in areas such as communication with doctors and nurses, responsiveness of hospital staff, pain management, cleanliness, and I G H L I G H T S quietness. Winning hospitals had to score an overall rating in the 90th percentile or higher. For the Summit Award, UT Southwestern won for its inpatient services by ranking in at least the 95th percentile every three months for three consecutive years. The consulting firm evaluated data from August 2008 through July 2011. Only 37 Summit Awards were presented out of more than 1,000 eligible hospitals. CAMPUS CROWD CELEBRATES 5TH NOBEL LAUREATE The UT Southwestern community enthusiastically shared in a mid-December celebration of Dr. Bruce A. Beutler’s triumphant return home with the 2011 Nobel Prize in Physiology or Medicine for his 1990s research that identified the mammalian receptor for innate immunity, the body’s first response to invasion by bacteria and other pathogens. Dr. Beutler is the fifth UTSW faculty member so honored. “We welcome Bruce back not UT SOUTHWESTERN MEDICAL SCHOOL DEAN DR. GREG FITZ (LEFT) AND UTSW PRESIDENT DR. DANIEL K. PODOLSKY (RIGHT) HELPED WELCOME NOBEL LAUREATE DR. BRUCE BEUTLER BACK TO CAMPUS AFTER HIS 2011 RECOGNITION IN SWEDEN. 54 for the work he has done in the past, as proud as we are of that, but for the work we know he’s going to do in the future,” UT Southwestern President Dr. Daniel K. Podolsky said to the crowd of campus leaders, faculty members, staff, and community supporters gathered in the Tom and Lula Gooch Auditorium. The honor, Dr. Podolsky said, “is especially satisfying because it recognizes groundbreaking work which was done right here at UT Southwestern as a member of our faculty.” Dr. Beutler completed his internship and residency in neurology at UTSW and served on the Internal Medicine faculty and was a Howard Hughes Medical Institute Investigator from 1986 to 2000. He returned to campus in September 2011 as Director of the Center for the Genetics of Host Defense. Dr. Beutler said his trip to Sweden to accept the honor was humbling at times. “I went to the Nobel museum, and there I saw my name juxtaposed with all the scientific greats of the last century … It was a little hard for me to believe.” Dr. Michael Brown and Dr. Joseph Goldstein, who won UT Southwestern’s first Nobel Prize in 1985 for their discovery of the basic mechanisms of cholesterol metabolism, were among those who spoke at the event. Dr. Brown ruefully recalled the many times he tried to talk Dr. Beutler out of the work because of its immense difficulty. “And even after he made his enormous discovery, I didn’t realize the importance of it … A true discovery comes as a surprise, and it does take a while to appreciate the broad significance of it. And there’s no question that his discovery has that impact.” H SPRING 2012 DIAGNOSTIC TEST COULD REVOLUTIONIZE BRAIN-TUMOR CARE Researchers at UT Southwestern led by Dr. Elizabeth Maher, Associate Professor of Internal Medicine and Neurology and DR. ELIZABETH NeurotheraMAHER peutics, developed the first clinical application of a new imaging technique to diagnose brain tumors. The test could preclude the need for surgery in patients whose tumors are located in areas of the brain too dangerous to biopsy. This new magnetic resonance spectroscopy technique provides a definitive diagnosis of cancer based on imaging of a protein associated with a mutated gene found in 80 percent of low- and intermediate-grade gliomas. Presence of the mutation also means a better prognosis. Dr. Maher said the finding, reported in Nature Medicine, “is a major breakthrough for brain tumor patients” and is the only direct metabolic consequence of a genetic mutation in a cancer cell that can be identified through noninvasive imaging. MANGELSDORF’S WORK GARNERS PRESTIGIOUS I G H L I G H T S worldwide for outstanding contributions in endocrinology and diabetes research. In announcing the award, Karolinska Institutet officials said the UTSW Chairman of Pharmacology’s “work on nuclear receptors led to landmark discoveries of how regulatory pathways govern cholesterol, lipid, and bile acid homeostasis. He defined crucial signal-transduction networks in their entirety.” Nuclear receptors are proteins that turn genes on and off, serving as sensors that protect human cells against elevated levels DR. DAVID of lipids. Dr. MANGELSDORF Mangelsdorf and his laboratory team have identified several new molecules, or ligands, that activate so-called orphan nuclear receptors whose biological functions previously had remained unknown. Dr. Daniel K. Podolsky, President of UT Southwestern, said the international honor “recognizes excellence in scientific discovery and the fruits of Dr. Mangelsdorf’s determination to unlock mysteries surrounding human metabolism. This research holds important implications for the treatment of several diseases.” INTERNATIONAL HONOR Director of the Eugene McDermott Center for Human Growth and Development, Dr. Hobbs leads investigations DR. HELEN that focus on HOBBS identifying genetic factors that contribute to variations in the levels of cholesterol in the blood, especially low-density lipoprotein (LDL) cholesterol. Elevated levels of LDL increase the risk of a heart attack. Since 1999 Dr. Hobbs has led the Dallas Heart Study, a longitudinal, multiethnic, population-based study of risk factors underlying cardiovascular disease. The study, funded by the Donald W. Reynolds Foundation, involves thousands of participants. Collaborating with Dr. Jonathan Cohen, Professor of Internal Medicine, Dr. Hobbs identified people with a genetic mutation that kept them from making normal amounts of the PCSK9 protein. Those with the mutation have a 28 percent reduction in LDL cholesterol levels and an 88 percent reduction in risk of coronary heart disease over a 15-year period compared to those without the mutation. OLSON WINS PASSANO AWARD FOR SEMINAL HEART RESEARCH Dr. David Mangelsdorf received CHOLESTEROL METABOLISM the 2012 Rolf Luft Award for research that has advanced understanding of nuclear receptor pathways. The annual recognition from the Karolinska Institutet, the prestigious medical university in Sweden that is also home to the Nobel Assembly, honors one scientist HOBBS 1ST GOTTO PRIZE INVESTIGATIONS EARN Dr. Helen Hobbs, who studies the genetics of cholesterol metabolism, won the inaugural Antonio M. Gotto Jr. Prize in Atherosclerosis Research from the International Atherosclerosis Society. Chairman of Molecular Biology Dr. Eric Olson won the 2012 Passano Award for identifying major genetic pathways that control the development of the heart and other muscles. Passano Foundation officials noted that Dr. Olson’s discoveries at the interface of developmental biology and medicine SOUTHWESTERN MEDICINE 55 H “have profoundly influenced our understanding of the mechanisms responsible for development and dysfunction of DR. ERIC OLSON the heart.” The recognition honors U.S.-based research that leads to real-world applications in clinical medicine. Discoveries in Dr. Olson’s laboratory have “unveiled the molecular underpinnings of congenital and acquired diseases of the heart and established a foundation for the advancement of new cardiovascular therapeutics,” said Dr. Joseph Goldstein, Chairman of Molecular Genetics and co-winner of the 1985 Nobel Prize in Physiology or Medicine. Twenty-three Passano Award recipients have gone on to win the Nobel Prize, including three who have regental professorships at UTSW: Dr. Goldstein; his co-winner, Dr. Michael Brown, Director of the Erik Jonsson Center for Research in Molecular Genetics and Human Disease; and Dr. Alfred Gilman, Regental Professor Emeritus of Pharmacology who shared the 1994 Nobel Prize in Physiology or Medicine. NAS RECOGNIZES MOLECULAR BIOLOGY CONTRIBUTIONS OF CHEN Dr. Zhijian “James” Chen, Professor of Molecular Biology, was recognized with the National Academy of Sciences Award in Molecular Biology. 56 DR. Zhijian “James” Chen I G H L I G H T S NAS officials noted that Dr. Chen was “honored for two contributions important for cancer and immunity: discovering an unsuspected component in a central signaling pathway and identifying an unprecedented role for a subcellular organelle in fighting viral infection.” Dr. Daniel K. Podolsky, President of UTSW, said Dr. Chen “has applied powerful techniques of molecular biology to understand the fundamental mechanisms of cell response to viral infections.” The Howard Hughes Institute Investigator’s research focuses on cellular signaling in the immune system, particularly the protein ubiquitin, so named because it is ubiquitously, or universally, found in all cells. Dr. Chen’s discoveries noted by the NAS are important for understanding the fundamental mechanisms of cancer and immunity, and they identify potential new targets for the development of drugs to fight infection by common viruses such as hepatitis C, West Nile, and influenza. TAMEST SELECTS SCHERER FOR O’DONNELL AWARD Dr. Philipp Scherer, Director of the Touchstone Center for Diabetes Treatment, received The Academy of Medicine, Engineering and Science of Texas’ 2012 Edith and Peter O’Donnell Award in medicine. Dr. Scherer received the award based in part on his research into fat-derived hormones that control sensitivity to insulin. The blood levels of adiponectin – a protein he discovered in 1994 – decline as a person gains weight, which offers potential as a good predictor of diabetes, heart disease, and cancer risk. The selection committee cited Dr. Scherer’s research on fat cells called adipocytes. The DR. Philipp group also Scherer noted Dr. Scherer’s discovery of how fat cells communicate with other tissues and regulate the release of their hormones. Adiponectin, for instance, is secreted almost reciprocally with another fatderived hormone, leptin. Dr. Scherer in 2007 demonstrated that excess adiponectin in mice can prompt fat tissue to expand in a healthy, non-inflamed way, thereby generating the “world’s fattest healthy mice” resistant to development of diabetes. INVESTIGATORS MOVE TO UNLOCK CLOCK COMPLEX UT Southwestern researchers continue to take major steps toward understanding the cellular clock, mapping for the first time the atomic-level architecture of a key component of the timekeeper that governs the body’s daily rhythms. The daily, or circadian, cycles guided by the body’s clocks affect our ability to get a good night’s sleep, how fast we DR. JOSEPH recover from TAKAHASHI jet lag, and even the best time to give cancer treatments, said Dr. Joseph Takahashi, Chairman of Neuroscience and a pioneer in the study of circadian rhythms. Understanding the structure of the cellular clock could lead H to better treatments for insomnia, diabetes, and cancer. Mapping the 3-D structure of the key component in the cellular clock – called the CLOCK: BMAL1 transcriptional activator complex – will have a great impact on the study of circadian rhythms and in other areas like toxicology and the growth of nerve cells, in which proteins in the same family play central roles, Dr. Takahashi said. SUMMER 2012 SCIENTISTS RECEIVE PRC DISTINGUISHED AWARDS The President’s Research Council presented its 2012 Distinguished Young Researcher Awards to a pair of outstanding UT Southwestern investigators. The recipients – Dr. Arun Radhakrishnan, Assistant Professor of Molecular Genetics, and Dr. Puneeth Iyengar, Assistant Professor of Radiation Oncology – each received a $65,000 award. Dr. Radhakrishnan is studying how cholesterolsensing membrane proteins measure the concentration of cholesterol in endoplasmic reticulum (ER) membranes. Using purified ER membranes, he and his research team have shown that these sensors respond in a switch-like fashion to small changes in membrane cholesterol to regulate cholesterol levels in cells. Dr. Radhakrishnan, who joined the faculty in 2011, was previously a faculty member at Weill Cornell Medical College and a postdoctoral Fellow at UTSW. He earned his doctorate degree from Stanford University after graduating from the University of California, Berkeley. Dr. Iyengar, a faculty member since 2010, is studying cachexia – the massive loss of fat and muscle – that is found in many I G H L I G H T S who are interested in learning about and advancing medical research at UT Southwestern. THREE SCHOOLS CONFER 452 DEGREES Diplomas were received by DR. ARUN DR. PUNEETH RADHAKRISHNAN IYENGAR disease states, including cancer, infectious disease, liver disease, and heart failure. He said understanding of the condition may add to the knowledge of the mechanisms leading to obesity, the opposite condition to cachexia. Dr. Iyengar earned his doctorate and medical degrees from Albert Einstein College of Medicine and a Bachelor of Science from Massachusetts Institute of Technology. The Distinguished Young Researcher Award is presented annually by the PRC, which is made up of community leaders 227 UT Southwestern Medical School students and 122 UT Southwestern Graduate School of Biomedical Sciences students in June commencement ceremonies. In mid-December 2011, 103 students graduated from the UT Southwestern School of Health Professions. The graduates included students from physical therapy, physician assistant studies, clinical nutrition, medical laboratory sciences, prosthetics-orthotics, and radiation therapy. U.S. Sen. Kay Bailey Hutchison delivered the keynote address to the Medical School graduates and guests. The school’s 68th commencement ceremony included the confer- UT SOUTHWESTERN MEDICAL SCHOOL’S SUMMER COMMENCEMENT IN JUNE INCLUDED A NOTED MILESTONE – CONFERENCE OF THE SCHOOL’S 10,000TH DEGREE. SOUTHWESTERN MEDICINE 57 H I G H L I G H T S A TEAM OF MORE THAN 50 PHYSICIANS, NURSES, AND OTHER CLINICAL SPECIALISTS COLLABORATED IN THE FLAWLESS DELIVERY AND CARE OF THE JONES QUINTUPLETS, BORN AT ST. PAUL UNIVERSITY HOSPITAL. ence of the school’s 10,000th degree. Since its establishment in 1943, UTSW has now conferred 10,164 medical degrees. Southwestern Medical Foundation’s Ho Din Award, the top honor for a graduating medical student, was presented to Dr. Thomas Heyne. The Graduate School’s address was delivered by Nobel Laureate Dr. Bruce A. Beutler, Director of the Center for the Genetics of Host Defense. Dr. Tina Han received the Nominata Award, given to the outstanding Graduate School student. [See story ….. Page 2] BIRTH OF QUINTS DEMONSTRATES DEDICATED CARE One of the nation’s first set of 2012 quintuplets – three boys and two girls – were born August 9 at UT Southwestern’s St. Paul University Hospital to missionaries Carrie and Gavin Jones. A specially trained multidisciplinary delivery team of more than 50 UTSW specialists, nurses, technicians, and thera- 58 pists – including dedicated units for each infant – managed the successful births, delivered in less than five minutes. The five infants – Will Edward, David Stephen, Marcie Jane, Seth Jared, and Grace Elise – were cared for in St. Paul’s Neonatal Intensive Care Unit for months before they reached weight, post-birth age, and health markers. Dr. Patricia Santiago-Munoz, Associate Professor of Obstetrics and Gynecology, delivered the infants. She said the births went as expected, thanks to Mrs. Jones’ strong spirit and months of coordination on the part of the medical team, which included a specially designated “CODE 5” alert when the time came. The babies’ 27-week weight at birth ranged from 1 pound, 12 ounces to 2 pounds, 11 ounces, said Dr. Gary Burgess, Medical Director of the NICU, who oversaw care for the five children. Mr. and Mr. Jones, along with their 8-year-old son, Isaac, serve as missionaries in the South Pacific nation of Papua New Guinea, north of Australia. APPOINTMENTS FOR 2011-2012 The following individuals were appointed to endowed positions or to major leadership positions at UT Southwestern during the past fiscal year. ■ Dr. Hunt Batjer, Chairman of Neurological Surgery, and to the Lois C.A. and Darwin E. Smith Distinguished Chair in Neurological Surgery. ■ Dr. Perry Bickel, Chief of Endocrinology, and to the J.D. and Maggie E. Wilson Distinguished Chair in Biomedical Research. ■ Dr. Preston Blomquist, to the Dr. W. Maxwell Thomas Chair in Ophthalmology ■ Dr. Stephen Cannon, to the Patricia A. Smith Distinguished Chair in Neuromuscular Disease Research, in Honor of Gil Wolfe, M.D. ■ Dr. Diego Castrillon, to the John H. Childers, M.D. Professorship in Pathology. ■ Dr. David Chason, to the M.R. & E. Hudson Foundation Professorship in Radiology, in Honor of Edward E. Christensen, M.D. H ■ Arnim Dontes, Executive Vice President for Business Affairs. ■ Dr. David Farrar, to the J. Wayne Streilein, M.D., Professorship in Immunology. ■ Dr. Andrew Feranchak, to the Willis C. Maddrey, M.D., Professorship in Liver Disease. ■ Dr. Kevin Gill, to the Aaron A. Hofmann, M.D., and Suzanne Hofmann Distinguished Chair in Orthopaedic Surgery in Honor of Richard E. Jones, M.D. ■ Dr. Frederick Grinnell, to the Robert McLemore Professorship in Medical Science. ■ Dr. Donald Hilgemann, to the Floyd C. Rector Jr., M.D, Professorship in Acid-Base Regulation. ■ Randy Jones, Associate Vice President and Chief Administrative Officer for Ambulatory Care. ■ Dr. David Karp, to the Fredye Factor Chair in Rheumatoid Arthritis Research. ■ Dr. Kemp Kernstine, Chief of Thoracic Surgery. ■ Dr. Makoto Kuro-o, to the Frederic C. Bartter Professorship in Vitamin D Research. ■ Dr. Jayanthi Lea, to the Patricia Duniven Fletcher Distinguished Professorship in Gynecological Oncology. ■ Dr. Robert Lenkinski, to the Charles A. and Elizabeth Ann Sanders Chair in Translational Research, and the Jan and Bob Pickens Distinguished Professorship in Medical Science, in Memory of Jerry Knight Rymer and Annette Brannon Rymer and Mr. and Mrs. W.L. Pickens ■ Dr. Beth Levine, to the Charles Cameron Sprague Distinguished Chair in Biomedical Science. I G H L I G H T S ■ Dr. Chris Madden, Associate Vice President for Parkland Health & Hospital System Affairs. ■ Dr. James Malter, Chairman of Pathology. ■ Dr. Darren McGuire, to the Dallas Heart Ball Chair for Research on Heart Disease in Women. ■ Dr. David Scott Miller, to the Amy and Vernon E. Faulconer Distinguished Chair in Medical Science. ■ Dr. R. Tyler Miller, to the John S. Fordtran, M.D., Professorship in Calcium Research ■ Dr. Chandra Mohan, to the McGee Foundation Chair in Arthritis Research. ■ Dr. Ivan Pedrosa, to the Jack Reynolds, M.D., Chair in Radiology. ■ Dr. Margaret Phillips, to the Beatrice and Miguel Elias Distinguished Chair in Biomedical Science. ■ Dr. Vanessa Rogers, to the Norman F. Gant, Jr., M.D. Chair in Obstetrics and Gynecology. ■ Dr. Michael Rosen, Chairman of the Department of Biophysics. ■ Dr. Theodora Ross, to the H. Ben and Isabelle T. Decherd Chair in Internal Medicine, in Honor of Henry M. Winans Sr., M.D., and the Jeanne Ann Plitt Professorship in Breast Cancer Research. ■ Dr. Anne Satterthwaite, to the Peggy Chavellier Professorship for Arthritis Research and Treatment. ■ Dr. Sandra Schmid, Chairman of Cell Biology, and to the Cecil H. Green Distinguished Chair in Cellular and Molecular Biology. ■ Dr. Amer Shakil, to the Perry E. Gross, M.D., Distinguished Chair in Family Medicine, the Stanley Gilbert, M.D., Professorship in Family Practice, and the Dr. Bill Ross Professorship in Family Practice. ■ Dr. Jeanne Sheffield, to the Alvin “Bud” Brekken Professorship in Obstetrics and Gynecology. ■ Dr. Xiankai Sun, to the Dr. Jack Krohmer Professorship in Radiation Physics. ■ Carolyn Swann, Associate Vice President for Heart, Lung, and Vascular, and Solid Organ Transplant Services at University Hospitals & Clinics. ■ Dr. Stan Taylor, Associate Vice President and Chief Medical Officer for Ambulatory Care at the University Clinics. ■ Dr. Carlos Timaran, to the G. Patrick Clagett Professorship in Vascular Surgery. ■ Dr. Jose Torrealba, to the Drs. George and Anne Race Distinguished Professorship of Pathology. ■ Dr. Steven Vernino, to the Dr. Bob and Jean Smith Foundation Distinguished Chair in Neuromuscular Disease Research. ■ Dr. John Warner, Chief Executive Officer for University Hospitals. ■ Dr. Steven Wolf, to the Golden Charity Guild Charles R. Baxter, M.D. Chair. ■ Dr. Jeffrey Zigman, to the Mr. and Mrs. Bruce G. Brookshire Professorship in Medicine, and the Diana and Richard C. Strauss Professorship in Biomedical Research. SOUTHWESTERN MEDICINE 59 H MAJOR GIFTS IN 2011-2012 Philanthropists continued to demonstrate their commitment to UT Southwestern in 20112012, providing support for a variety of research, clinical, and educational programs. Major new pledges and gifts received in the fiscal year 20112012 included: ■ $8,400,000 from an anonymous donor to support research programs at UT Southwestern. ■ $6,000,000 from Lyda Hill to establish the Lyda Hill Endowment for Systems Biology. ■ $3,000,000 from Mr. and Mrs. Howard M. Meyers to Southwestern Medical Foundation to support the construction of UT Southwestern’s new William P. Clements Jr. University Hospital. ■ $1,525,000 from Jimmie C. LaFollette, through a bequest to Southwestern Medical Foundation, in support of research into intracranial hemorrhagic stroke, macular degeneration, glaucoma, and non-Hodgkin lymphoma at UT Southwestern. ■ $1,390,000 from proceeds of the 2011 Sweetheart Ball to Southwestern Medical Foundation in support of heart research at UT Southwestern. ■ $1,000,000 from The Dedman Foundation to Southwestern Medical Foundation to support the construction of UT Southwestern’s new William P. Clements Jr. University Hospital. ■ $1,000,000 from the Roger Horchow family to Southwestern Medical Foundation to support the construction of UTSW’s new William P. Clements Jr. University Hospital. 60 I G H L I G H T S ■ $1,000,000 from the Lowe Foundation to Southwestern Medical Foundation to establish the Erma Lowe Center for Alzheimer's Disease Research. ■ $1,000,000 from the estate of Shirley Pollock, through a bequest to Southwestern Medical Foundation, to support the Lawrence S. Pollock Jr. Center for Intestinal Cancer Research. ■ $1,000,000 from the estate of Patricia A. Smith to establish the Patricia A. Smith Distinguished Chair in Neuromuscular Disease Research, in Honor of Gil Wolfe, M.D. ■ $407,352 from the estate of Patricia Alford Box, through a bequest to Southwestern Medical Foundation, to support UT Southwestern research of chronic lymphocytic leukemia. ■ $400,000 from the Hartwell Foundation to provide individual and collaborative biomedical research fellowships for promising early-career investigators at UTSW. ■ $400,000 from the Lupe Murchison Foundation to Southwestern Medical Foundation to support Alzheimer's disease research under the direction of Dr. Joachim Herz. ■ $350,000 from Yukie Niwa, M.D., Ph.D., to support research of rheumatic diseases under the direction of Dr. Joel D. Taurog. ■ $332,195 from the Howard Hughes Medical Institute to support flow cytometry technology. ■ $300,000 from the National Multiple Sclerosis Society to support continuing education and clinical programs for multiple sclerosis. ■ $250,000 from the International Mental Health Research Organization to support the 2011 IMHRO Rising Star. Generous contributions and pledges of $100,000 to $249,999 were received from a number of additional donors, including the following new commitments from: ■ An anonymous donor to support research on microRNAbased anti-cancer therapeutics under the direction of Dr. Joshua Mendell. ■ An anonymous donor to support lung cancer programs in honor of Drs. Hak Choy, J. Michael DiMaio, Jonathan E. Dowell, and David A. Pistenmaa. ■ An anonymous donor to Southwestern Medical Foundation to provide unrestricted support for UT Southwestern. ■ The Cain Foundation to support a fellowship in urology. ■ The Canary Foundation to support lung cancer research. ■ The David M. Crowley Foundation to support peripheral nerve and pain management research and activities in the David M. Crowley Research and Rehabilitation Laboratory. ■ Dr. and Mrs. Adi F. Gazdar to Southwestern Medical Foundation to establish the Adi Gazdar, M.D., Annual Lectureship in Translational Medicine, and the Adi and Celia Gazdar Fund in Translational Cancer Research. ■ Mr. and Mrs. Mark Gibson, through The Melchizedek Fund of Communities Foundation of Texas, to Southwestern Medical Foundation to support research, education, and clinical care programs at UT Southwestern. ■ David C. Haley to support diabetes research. ■ Mr. and Mrs. G. Houston Hall to Southwestern Medical Foundation to support the construction of UT Southwestern’s new William P. Clements Jr. University Hospital. H ■ Mr. and Mrs. J. Davis Hamlin to Southwestern Medical Foundation to support education, research, and clinical care programs at UT Southwestern, in honor of Dr. and Mrs. Kern Wildenthal and Dr. Amy Phelan. ■ The Hoblitzelle Foundation to Southwestern Medical Foundation to endow the Ron Anderson, M.D., Professorship in Clinical Care and Education at Parkland Memorial Hospital. ■ Mr. and Mrs. Peter M. Holt to support corneal research. ■ The Dixie S. Jones Foundation Testamentary Trust to support the care and/or treatment of children under the age of 18. ■ The Mary Kay Foundation to support breast cancer research. ■ Once Upon a Time… to endow the Nadine and Tom Craddick Professorship in Medical Education and to Southwestern Medical Foundation to support education, research, and clinical care programs at UT Southwestern. ■ The Charles Y.C. Pak Foundation to support metabolic kidney disease research and to establish the John S. Fordtran, M.D., Professorship in Calcium Research. ■ The Perkins-Prothro Foundation to Southwestern Medical Foundation to support the construction of UT Southwestern’s new William P. Clements Jr. University Hospital. ■ Pfizer Inc. to support the 2012 Pfizer Fellows in the Medical Scientist Training Program at UT Southwestern. I G H L I G H T S ■ The Vin and Caren Prothro Foundation to Southwestern Medical Foundation to support the construction of UT Southwestern’s new William P. Clements Jr. University Hospital. ■ Bette Claire Schuttler, through a bequest to Southwestern Medical Foundation, for research into cancer and Alzheimer’s disease. ■ James Cleo Thompson Jr., through a bequest to Southwestern Medical Foundation, to establish a fund for bladder cancer research under the direction of Dr. Ganesh Raj. ■ Mr. and Mrs. Gifford O. Touchstone to support diabetes research under the direction of Dr. Roger Unger. ■ The Ivor and Mildred Wold Charitable Fund to Southwestern Medical Foundation to support the Mildred Wyatt and Ivor P. Wold Center for Geriatric Care. SOUTHWESTERN MEDICINE 61