Bakersfield College Associate Degree Nursing NURS B28 - Medical Surgical Nursing 4
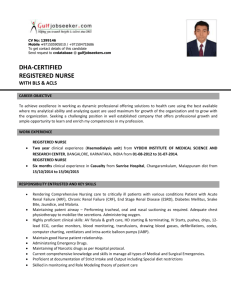
advertisement

1 Bakersfield College Associate Degree Nursing NURS B28 - Medical Surgical Nursing 4 Unit 1 - COURSE INTRODUCTION INTRODUCTION This unit will present the instructional syllabus and define the Student Learning Outcomes (SLO) for Nursing B28, a level 4 course. The instructional syllabus is an essential part of the learning process. It serves as a learning contract that clearly states the responsibilities of both the student and the instructor. It outlines information such as the course objectives and policies, teaching and learning activities, lecture topics, the evaluation process, and dates of examinations and assignments. Additionally, the syllabus helps promote independent student learning and accountability in the educational process. The syllabus also defines Level 4 objectives and course expectations. It is expected that the Level 4 student will integrate all previously acquired knowledge, provide care to patients who have critical and complex disease states utilizing the nursing process, and assume the leadership role. In meeting the Program Student Learning Outcomes, the graduate will be prepared to competently transition from student to entry level Registered Nurse. OBJECTIVES Upon completion of this unit, the student will: Theory 1. Relate Level 4 SLO’s to the Program Student Learning Outcomes. 2. Compare the attributes of Provider of Care, Manager of Care and Member of the Profession for the Level 4 Associate Degree Student Nurse to those attributes in Levels 1 through 3. 3. Differentiate the SLO in the Medical Surgical Nursing Courses Levels 1 through 3, from those in this Level 4 course. 4. Explain course policies, expectations and requirements as outlined in the syllabus for both the theory and clinical components of Nursing B28. 5. Verbalize the attendance policy, and criteria for student evaluation in the theory component of Nursing B28. Clinical 1. Recognize the roles of the Provider of Care, Manager of Care, and Member of the Profession for a Level 4 nursing student, and model the specific behavior. 2. Relate course policies, expectations, requirements, and evaluation criteria as outlined in the Clinical Manual to the theory component of Nursing B28. 3. Verbalize the attendance policy, and criteria for student evaluation in the laboratory component of NURS B28. 4. Interpret the student laboratory rotation matrix. 5. Discuss the advanced application of the nursing process when caring for patients who have critical and complex medical conditions. 2 Unit 2 – PROFESSIONAL ISSUES AND NURSING PRACTICE INTRODUCTION Nursing practice takes place in many settings. The nursing roles in the critical care areas will be presented, along with associated professional issues. Common stressors which affect the critically ill client and the critical care nurse will be examined along with appropriate stress reduction measures. Teaching learning principles as related to critical care will be presented. Community based care and leadership will be discussed. The concepts of critical thinking, caring and comfort, and elements of diversity are also explored. Principles of assessment with multiple traumas and a community disaster are presented. The legal and ethical conflicts relevant to the client and nurse in the critical care settings will be examined. Discontinuation of life support systems in critical care will be discussed, including legal and ethical issues related to organ donation. The roles of the Provider of Care, Manager of Care, and Member of the Profession are integrated to promote successful transition from graduate nurse to entry level Registered Nurse (RN). OBJECTIVES Upon completion of this unit, the student will: Theory 1. Recall the roles of the medical surgical-nurse and define how they relate to the Level 4 nursing student. 2. Define Critical Care Nursing and describe the role of the critical care nurse 3. Discuss the purposes and functions of the professional organizations that support critical care practice. 4. Identify and describe professional certifications. 5. Identify current trends and issues. 6. Evaluate the effects of the critical care environment on the nurse, patient, and family. 7. Describe the decision making process, including goal setting, prioritization and delegation. Discuss employment issues that affect the new graduate nurse. 8. Discuss employment issues that affect the new graduate nurse. 9. Describe advanced patient assessment and triage. 10. Explain the pathophysiology and apply the nursing process to traumatic injury 11. Analyze disaster planning, and response to include bioterrorism. 12. Analyze environmental emergencies and collaborative management of hypothermia, heat-related emergencies, and near drowning. 13. Recall ethical principles and discuss how they relate to critical care patients. 14. Identify legal and professional obligations of critical care nurses. 15. Identify and discuss selected ethical and legal issues in critical care nursing practice. 16. Identify the purposes and needs for nurse licensure, the significance of nurse practice acts and implications of regulatory agencies. 17. Describe ethical and legal concerns related to end-of-life care. 18. Discuss cultural considerations in end-of-life care. 3 19. Describe nursing interventions to support the patient and family during the end-of-life stage. 20. Explain accepted guidelines for discontinuation of life support systems. 21. Describe the indications for organ transplantation. 22. Discuss the collaborative management necessary for care of the organ transplant patient. 23. Discuss policies that apply to organ donation and transplantation Discuss rejection as the major obstacle organ transplantation. 24. Explain clinical manifestations of rejection. 25. Discuss the purpose, action and possible adverse effects of immunosuppressant Clinical 1. Incorporate the roles of Provider of Care, Manager of Care, and Member of Profession in the medical surgical, critical care, and specialized environments. 2. Differentiate the role and scope of the critical care nurse from the medical surgical nurse 3. Discuss the concerns expressed by critically ill patients. 4. Discuss ways to identify and meet the needs of families of critically ill patients. 5. Describe strategies a nurse might utilize to communicate with the critically ill client. 6. Relate critical thinking to the nursing process, and evidenced based practice. 7. Explore the relationship between critical thinking and problem solving. 8. Analyze data to establish priorities, and anticipate the care for increasingly complex clients / families. 9. Consistently demonstrate reflective reasoning, analytic skill, sensitivity, and knowledge of resources and possible solutions in order to effectively make decisions, problem solve, organize, and prioritize, and delegate care for individuals and/or groups of clients. 10. Demonstrate Fiscal responsibility in the clinical setting. 11. Analyze specific examples of role transitions as a leader, manager, and follower. 12. Compare the strategies used during a previous transition: strengthening internal resources, negotiating a role, growing with mentors or learning necessary skills. 13. Identify the role of the emergency department (ED) nurse. 14. Differentiate between emergency department triage versus mass casualty triage 15. Discuss Hospital Emergency Incident Command System (HEICS). 16. Identify the correct sequence of priorities utilizing the A thru I trauma assessment in treatment of the client who has the multi system trauma. 17. Discuss predisposing factors and interventions for environmental emergencies: heat exhaustion, heatstroke, frostbite, hypothermia, and near-drowning. 18. Discuss the nurse’s responsibility for bioterrorism preparedness. 19. Describe ethical dilemmas encountered in your own experience. 20. Analyze different approaches to ethical dilemmas and the implication of each approach. 21. Discuss the purpose of obtaining licensure to practice as a registered nurse in the state of California. 22. Describe the Nurse Practice Act, how it can be obtained and its purpose 23. Discuss the composition, purpose of the BRN, its relationship with the public, with nursing programs and registered nurses in California 24. Describe the importance of belonging to a professional nursing organization for nursing practice and lifelong career development. 4 25. Discuss concepts of end-of-life care, including palliative care; communication and conflict resolution; withholding or withdrawing therapy; and psychological support of the patient, family members, and health care providers. 26. Discuss components of communicating with families regarding organ donation and endof-life issues. 27. Describe the components of communicating with potential organ recipients. 28. Summarize the procedure followed for organ donation. 29. Specify ethical dilemmas related to discontinuation of life support systems. 5 Unit 3– BIOPSYCHOSOCIAL CONCEPTS RELATED TO HEALTH CARE INTRODUCTION Communication between members of the healthcare team, as well as with patients and families, is of utmost importance in facilitating an amicable work environment and appropriate patient care. Additionally, patient care must include effective pain management to ensure patient comfort, as well as to promote positive patient outcomes. Concepts of caring, critical thinking, professionalism, collaboration, and diversity are integrated throughout this unit. The roles of the Provider of Care, Manager of Care, and Member of the Profession are integrated to promote successful transition from graduate nurse to entry level Registered Nurse (RN) when addressing communication and pain management. OBJECTIVES Upon completion of this, the student will: Theory 1. 2. 3. 4. 5. Differentiate various communication pathways: organizational, persuasion, negotiation Demonstrate an understanding of the process of conflict resolution in the leadership role. Analyze how assertiveness and responsiveness may be helpful to effective leadership. Discuss methods/tools for assessing pain and anxiety in the critically ill client. Analyze nursing interventions for sedation and pain control and continuous IV infusions for sedation, pain, anxiety. Clinical 1. 2. 3. 4. 5. \ Evaluate leadership and management implications of communication. Critique techniques for becoming more assertive. Demonstrate problem solving techniques to provide relief of acute pain. Complete a thorough and complete pain assessment. Identify appropriate pain management strategies that are nonpharmacological. 6 Unit 4 – PROBLEMS OF OXYGENATION INTRODUCTION Maintaining a patent airway and ensuring adequate ventilation are essential for all patients. Therefore, it is critical for the student to possess a solid understanding of respiratory anatomy and physiology in order to care for patients who have critical and complex medical conditions. A brief review of respiratory anatomy and physiology, oxygen delivery devices, single use suctioning techniques, and arterial blood gas (ABG) interpretation will be presented. Care and management of patients with artificial airways, including tracheostomies and endotracheal tubes (ETT), and inline and subglottal suctioning will be introduced. Additionally, in depth information regarding chest trauma, acute respiratory failure, mechanical ventilation, ventilator acquired pneumonia (VAP), primary pulmonary hypertension (PPH), pulmonary embolism (PE), acute respiratory distress syndrome (ARDS), and thoracic surgery will be presented. The role of the nurse as the Provider of Care, Manager of Care, and Member of the Profession are integrated to promote successful transition from graduate nurse to entry level Registered Nurse when caring for a patient who has problems in oxygenation. OBJECTIVES Upon completion of this unit, the student will: Theory 1. Recall normal respiratory anatomy and physiology, and previously acquired knowledge of single use suctioning techniques, chest drainage systems, oxygen delivery systems and basic ABG interpretation. 2. Explain the components of an advanced respiratory assessment as they relate to caring for clients who have selected critical and complex medical conditions, including mechanical ventilation and thoracic surgeries. 3. Discuss the etiologies, pathophysiologies, clinical manifestations, and complications for clients who have selected critical and complex medical conditions related to the respiratory system, including: Chest trauma Acute respiratory failure PPH PE ARDS Thoracic surgeries 4. Explain the collaborative management, as appropriate, including: diagnostic and laboratory data, nutrition, nursing diagnosis and interventions, pharmacology, surgical and nonsurgical treatments, safety, teaching and learning needs, and health promotion for clients who have selected critical and complex medical conditions related to the respiratory system, and who require selected oxygen delivery systems. 5. Explain respiratory changes associated with aging, and summarize age appropriate care, for clients who have selected critical and complex medical conditions. 7 6. Differentiate ABG results in terms of full and partial compensation, and mixed disturbances. 7. Classify acid-base imbalances according to their underlying causes, and relate their clinical significance. 8. Differentiate selected types, modes, and associated settings of mechanical ventilation, and relate them to various pathophysiological processes and ABG results. Clinical 1. Demonstrate accountability for the provision and evaluation of nursing care that conforms to professional standards and incorporates legal and ethical responsibilities of the nurse, especially the rights of the clients. 2. Function as a client advocate by identifying and utilizing appropriate resources. 3. Differentiate the elements of an advanced pulmonary assessment. 4. Critique and organize data to establish priorities when caring for patients who have selected critical and complex medical conditions related to the respiratory system. 5. Create individualized nursing care plans for patients who have selected critical and complex medical conditions related to the respiratory system, and revise the plan of care as needed to optimize patient outcomes. 6. Incorporate syndrome diagnoses and collaborative problems, per NANDA, into care plans, as appropriate. 7. Anticipate and minimize complications when caring for patients who have critical and complex medical conditions related to the respiratory system. 8. Support all aspects of care with evidence based practice to clients who have critical and complex medical conditions related to the respiratory system. 9. Evaluate learning needs of the patient and / or their family, and design an appropriate teaching plan for disease prevention, health promotion, and self care for clients who have selected critical and complex medical conditions related to the respiratory system. 10. Demonstrate care and respect for the patient’s uniqueness, developmental level, sociocultural background, spiritual beliefs, perceptions and values for patients who have critical and complex medical conditions related to the respiratory system. 11. Interpret ABG results and relate them to the underlying physiologic processes when caring for patients who have critical and complex medical conditions, and anticipate the appropriate medical and nursing interventions. 12. Verify the mechanical ventilator settings, and correlate them to the patient’s condition and ABG results. 13. Recognize potential complications associated with mechanical ventilation. 14. Explain the weaning criteria associated with mechanical ventilation. 15. Correlate hemodynamics responses to effects of mechanical ventilation. 8 UNIT 5 – PROBLEMS OF CARDIAC OUTPUT AND TISSUE PERFUSION INTRODUCTION It is imperative for the student to possess a solid understanding of cardiac anatomy and physiology, in order to care for patients who have critical and complex medical conditions. A brief review of cardiac anatomy and physiology and Basic Life Support (BLS) will be presented. In depth information regarding hypertensive crisis, coronary artery disease (CAD), angina, myocardial infarction (MI), acute coronary syndrome (ACS), valvular heart disease, pericardial effusion, cardiac tamponade, aortic aneurysms, and cardiogenic and distributive shock will also be presented. Additionally, basic rhythm interpretation, dysrhythmias, advanced cardiac life support (ACLS), and hemodynamic monitoring will be introduced. The role of the nurse as the Provider of Care, Manager of Care, and Member of the Profession are integrated to promote successful transition from graduate nurse to entry level Registered Nurse when caring for a patient who has problems with cardiac output and tissue perfusion. OBJECTIVES Upon completion of this unit, the student will: Theory 1. Recall normal cardiac anatomy and physiology, and previously acquired knowledge of the key elements of BLS, hypertension, and shock. 2. Explain the components of an advanced cardiac assessment as they relate to caring for clients who have selected critical and complex medical conditions, selected dysrhythmias, and invasive hemodynamic monitoring. 3. Discuss the etiologies, pathophysiology, clinical manifestations, and complications for clients who have selected critical and complex medical conditions related to the cardiovascular system, including: a. Hypertensive crisis b. CAD c. Angina d. MI e. ACS f. Valvular heart disease g. Aortic aneurysms h. Pericardial effusion i. Cardiac tamponade j. Shock k. Dysrhythmias l. Cardiac emergencies 9 4. Explain the collaborative management, as appropriate, including: diagnostic and laboratory data, nutrition, nursing diagnosis and interventions, pharmacology, surgical and nonsurgical treatments, safety, teaching and learning needs, and health promotion for clients who have selected critical and complex medical conditions related to the cardiovascular system. 5. Explain cardiovascular changes associated with aging, and summarize age appropriate care, for clients who have selected critical and complex medical conditions. 6. Correlate the components of the electrocardiogram (ECG) with the cardiac conduction system. 7. Identify key features of normal sinus rhythm and selected dysrhythmias. 8. Demonstrate a systematic approach in interpreting selected rhythm strips. 9. Differentiate the pathophysiologic mechanisms for selected dysrhythmias and organize them in terms of lethality, emergency management (BLS and ACLS), and pharmacological interventions. 10. Outline the hemodynamic consequences and signs and symptoms of selected dysrhythmias. 11. Summarize the nursing and medical responsibilities of selected dysrhythmias. 12. Describe the components of a hemodynamic monitoring system. 13. Describe the indications, normal parameters, complications, and nursing implications associated with invasive monitoring of right atrial, pulmonary artery, and intra-arterial pressures. 14. Discuss common medications used in the critical care area, and explain their effects on hemodynamic readings. 15. Explain the clinical relevance of altered hemodynamic values. Clinical 1. Integrate all previously learned knowledge while caring for critical and complex clients. 2. Incorporate the roles of a Level 4 Provider of Care, Manager of Care, and Member of the Profession when caring for patients who have critical and complex medical conditions related to the cardiovascular system. 3. Differentiate the elements of an advanced cardiac assessment. 4. Critique and organize data to establish priorities when caring for patients who have selected critical and complex medical conditions related to the cardiovascular system. 5. Anticipate and minimize complications when caring for patients who have critical and complex medical conditions related to the cardiovascular system. 6. Create individualized nursing care plans for patients who have selected critical and complex medical conditions related to the cardiovascular system, and revise the plan of care as needed to optimize patient outcomes. 7. Incorporate collaborative problems into care plans, as appropriate. 8. Evaluate learning needs of the patient and / or their family, and design an appropriate teaching plan for disease prevention, health promotion, and self care for clients who have selected critical and complex medical conditions related to the cardiovascular system. 9. Classify selected cardiac medications used in critical care environments, anticipate their desired and adverse effects, and correlate them with selected cardiovascular conditions. 10 10. Verify drug and intravenous solution delivery rates for patients who have selected critical and complex medical conditions related to the cardiovascular system. 11. Describe how cultural perspectives affect the critically and terminally ill client, and how these are addressed in the critical care setting. 12. Function as a client advocate when caring for patients with who have selected critical and complex medical conditions related to the cardiovascular system. 13. Demonstrate proper ECG lead placement for leads I, II, III, and MCL 1. 14. Measure the atrial and ventricular rates by utilizing two methods. 15. Interpret selected cardiac rhythms, and incorporate into the plan of care. 16. Attribute physiologic responses to observed dysrhythmias. 17. Implement BLS and ACLS algorithms, as appropriate, under the guidance of the clinical instructor and / or RN preceptor. 18. Identify the components of pressurized system. 19. Differentiate elements of an advanced cardiac assessment, related hemodynamic monitoring. 20. Create a nursing care plan which integrates and correlates advanced cardiac data for a patient with altered cardiovascular function. 21. Critique and organize data to establish priorities when caring for patients with right atrial pulmonary artery, and intra- arterial pressure. 22. Relate physiologic conditions and treatment modalities for a client with invasive hemodynamic monitoring. 11 Unit 6 – PROBLEMS OF HEMATOLOGICAL SYSTEM INTRODUCTION Hematological functions are vital in maintaining homeostasis as they promote tissue perfusion and oxygenation. These intricate responses can be easily disrupted in patients who have critical and complex medical conditions. Because of this, it is imperative the Level 4 student review and understand the anatomy and physiology of the hematological system, and relate the associated assessment findings to develop effective nursing strategies when caring for patients who have critical and complex medical conditions. Care and management of patients with alterations in red blood cells (RBC’s), thrombocytopenia and disseminated intravascular coagulation (DIC) will be discussed. The role of the nurse as the Provider of Care, Manager of Care, and Member of the Profession are integrated to promote successful transition from graduate nurse to entry level Registered Nurse when caring for a patient who has problems in the hematological system. OBJECTIVES Upon completion of unit, the student will: Theory 1. Recall normal hematologic anatomy and physiology, and previously acquired knowledge of blood formation, blood and blood products, hematopoietic cells, coagulation factors, anemia and hematologic disorders. 2. Explain the components of an advanced hematologic assessment as they relate to caring for clients who have selected critical and complex medical conditions. 3. Explain the coagulation mechanism and the role it plays in maintaining homeostasis. 4. Discuss etiologies, pathophysiologies, clinical manifestations, and complications for clients who have selected critical and complex medical conditions related to the hematologic system, including: Anemia DIC Thrombocytopenia 5. Explain the collaborative management, as appropriate, including: diagnostic and laboratory data, nutrition, nursing diagnosis and interventions, pharmacology, surgical /nonsurgical treatments, safety, teaching /learning needs, and health promotion for clients who have selected critical and complex medical conditions related to the hematologic system. 6. Relate hematologic changes associated with aging, and summarize age appropriate care, for clients who have selected critical and complex medical conditions. Clinical 1. Differentiate the elements of an advanced hematologic assessment, including: patient history, genetic risks, petechiae, and laboratory data. 12 2. Identify laboratory tests used in evaluating patients with anemia, DIC, and thrombocytopenia. 3. Relate the clinical presentation and laboratory findings in the patient with anemia, DIC and thrombocytopenia. 4. Explain the relationship of anemia to oxygen saturation (SpO2), cardiac output, and oxygen transport. 5. Develop and evaluate a care plan for a client with anemia, DIC, and thrombocytopenia. 13 Unit 7 – PROBLEMS OF MOBILITY, SENSATION, AND COGNITION INTRODUCTION The need for analgesics and sedatives to maintain patient safety and comfort is important. The goal is to find a balance between providing a balance between compassionate patient care and avoiding oversedation. Because of this, it is imperative the Level 4 student understand the differences among levels of sedation and relate the associated assessment findings to develop effective nursing strategies when caring for patients who have critical and complex medical conditions requiring sedation/analgesia. Care and management of patients receiving neuromuscular blockade and conscious sedation will be discussed. The role of the nurse as the Provider of Care, Manager of Care, and Member of the Profession are integrated to promote successful transition from graduate nurse to entry level Registered Nurse when caring for a patient who has problems of mobility, sensation, and cognition system. OBJECTIVES Upon completion of unit, the student will: Theory 1. Analyze nursing interventions for sedation and pain control for neuromuscular blockades and continuous intravenous infusions for sedation. 2. Differentiate between medically induced coma and therapeutic paralysis. 3. Analyze pharmacological agents used to provide conscious sedation and neuromuscular blockade Clinical 1. Discuss levels of sedation. 2. Identify appropriate anxiety and pain management strategies for the client receiving neuromuscular blockade 3. Describe evaluation of the client receiving neuromuscular blockade. 14 UNIT 8 – PROBLEMS OF NEUROLOGICAL FUNCTION INTRODUCTION Neurological injury and illness can produce devastating results. In order to care for patients who have critical and complex neurological conditions, it is imperative for the student to possess a solid understanding of neurological anatomy and physiology and of the disease processes affecting the neurological along with potential outcomes. A brief review of neurological anatomy and physiology will be presented. In depth information regarding traumatic brain injury (TBI), spinal cord trauma, Guillian Barre’, cerebral aneurysms, increased intracranial pressure (ICP), and neurogenic shock will be introduced. The role of the nurse as the Provider of Care, Manager of Care, and Member of the Profession are integrated to promote successful transition from graduate nurse to entry level Registered Nurse when caring for a patient who has problems with neurological function. OBJECTIVES Upon completion of this unit, the student will: Theory 9. Recall normal neurological anatomy and physiology and previously acquired knowledge regarding problems of neurological function. 10. Explain the components of an advanced neurological assessment as they relate to caring for clients who have selected critical and complex neurological conditions and intracranial pressure monitoring. 11. Discuss the etiologies, pathophysiology, clinical manifestations, and complications for clients who have selected critical and complex medical conditions related to the neurological system, including: • Traumatic brain injury (TBI) • Spinal cord trauma • Guillian Barre’ • Cerebral aneurysms • Increased intracranial pressure (ICP) • Neurogenic shock 12. Explain the collaborative management, as appropriate, including: diagnostic and laboratory data, nutrition, nursing diagnosis and interventions, pharmacology, surgical and nonsurgical treatments, safety, teaching and learning needs, and health promotion for clients who have selected critical and complex medical conditions related to the neurological system. 13. Explain neurological changes associated with aging, and summarize age appropriate care, for clients who have selected critical and complex medical conditions. 14. Describe the indications, normal parameters, complications, and nursing implications associated with intracranial pressure monitoring. 15. Discuss common pharmacological agents used for patients who have selected critical and complex medical and surgical conditions related to the neurological system. 15 Clinical 1. Integrate all previously learned knowledge while caring for critical and complex clients. 2. Incorporate the roles of a Level 4 Provider of Care, Manager of Care, and Member of the Profession when caring for patients who have critical and complex medical conditions related to the neurological system. 3. Differentiate the elements of an advanced neurological assessment. 4. Critique and organize data to establish priorities when caring for patients who have selected critical and complex medical conditions related to the neurological system. 5. Anticipate and minimize complications when caring for patients who have critical and complex medical conditions related to the neurological system. 6. Create individualized nursing care plans for patients who have selected critical and complex medical conditions related to the neurological system, and revise the plan of care as needed to optimize patient outcomes. 7. Incorporate collaborative problems into care plans, as appropriate. 8. Evaluate learning needs of the patient and / or their family, and design an appropriate teaching plan for disease prevention, health promotion, and self care for clients who have selected critical and complex medical conditions related to the neurological system. 9. Classify selected medications used in critical care environments, anticipate their desired and adverse effects, and correlate them with selected neurological conditions. 10. Verify drug and intravenous solution delivery rates for patients who have selected critical and complex medical conditions related to the neurological system. 11. Describe how cultural perspectives affect the critically and terminally ill client, and how these are addressed in the critical care setting. 12. Function as a client advocate when caring for patients with who have selected critical and complex medical conditions related to the neurological system. 13. Differentiate elements of an advanced neurological assessment, related intracranial pressure monitoring. 14. Create a nursing care plan which integrates and correlates advanced neurological data for a patient with altered neurological function. 15. Critique and organize data to establish priorities when caring for patients with increased intracranial pressure monitoring. 16. Relate physiologic conditions and treatment modalities for a client with intracranial pressure monitoring. 16 UNIT 9 – PROBLEMS OF REGULATION AND METABOLISM INTRODUCTION The goal of this unit is to provide the learner with the key information needed to care for clients with alterations in metabolic function. An in depth review of clients with diabetes insipidus (DI) and syndrome of inappropriate antidiuretic syndrome (SIADH) is provided. The unit contains information on nursing care of the client with diabetes insipidus and syndrome of inappropriate antidiuretic syndrome. Each disorder is discussed in terms of etiology, pathophysiology, clinical manifestations, complications, and collaborative management. Nursing diagnoses and client outcomes are identified. A nursing process approach is used for nursing management with a focus on health promotion and self care. The roles of provider of care, manager of care, and member of the profession are integrated to promote success in transitioning student from level 3 to level 4 meeting outcome criteria. OBJECTIVES Upon completion of Unit, the student will be able to: Theory 1. Recall anatomy and physiology of the endocrine system including regulation of electrolytes and osmolality. 2. Discuss the etiologies, pathophysiology, clinical manifestations, and complications for clients who have selected critical and complex medical conditions related to the neurological system, including: • Diabetes insipidus • Syndrome of inappropriate anti-diuretic hormone 3. Explain the collaborative management including: diagnostic and laboratory data, nutrition, nursing diagnosis and interventions, pharmacology, surgical and nonsurgical treatments, safety, teaching and learning needs, and health promotion for clients with DI and SIADH. 4. Explain endocrine changes associated with aging and summarize age appropriate care for clients with DI and SIADH. Clinical 1. Analyze clinical changes and laboratory data to determine the effectiveness of interventions for critically ill clients with diabetes insipidus and syndrome of inappropriate antidiuretic syndrome. 2. Utilize critical thinking skills to develop, evaluate, and revise a plan of care for a critically ill client with diabetes insipidus and syndrome of inappropriate antidiuretic syndrome. 3. Priortize and implement health teachings for the client with diabetes insipidus and syndrome of inappropriate antidiuretic syndrome. 4. Demonstrate patient advocacy when caring for a client with diabetes insipidus and syndrome of inappropriate antidiuretic syndrome. 17 UNIT 10 – PROBLEMS OF DISGESTION, NUTRITION, AND ELIMINATION INTRODUCTION The goal of this unit is to provide the learner with the key information needed to care for critically ill clients with alterations of the gastrointestinal function. An in depth review of clients with digestion, nutrition, and elimination problems are provided. The unit contains information on nursing care of the critically ill client with hepatic failure, hepatorenal failure, and gastrointestinal bleeding. Each disorder is discussed in terms of etiology, pathophysiology, clinical manifestations, complications, and collaborative management. Nursing diagnoses and client outcomes are identified. A nursing process approach is used for nursing management with a focus on health promotion and self care. The roles of provider of care, manager of care, and member of the profession are integrated to promote success in transitioning student from level 3 to level 4 meeting outcome criteria. OBJECTIVES Upon completion of the Unit, the student will be able to: Theory 1. Recall normal gastrointestinal anatomy and physiology and previously acquired knowledge regarding problems of digestion, nutrition, and elimination. 2. Explain the components of an advanced gastrointestinal assessment as they relate to caring for clients who have selected critical and complex problems of digestion, nutrition, and elimination. 3. Discuss the etiologies, pathophysiology, clinical manifestations, and complications for clients who have selected critical and complex medical conditions related to the gastrointestinal system, including: • hepatic failure • hepatorenal failure • acute gastrointestinal bleeding 4. Explain the collaborative management, as appropriate, including: diagnostic and laboratory data, nutrition, nursing diagnosis and interventions, pharmacology, surgical and nonsurgical treatments, safety, teaching and learning needs, and health promotion for clients who have selected critical and complex medical conditions related to digestion, nutrition, and elimination. 5. Explain digestion, nutrition, and elimination changes associated with aging, and summarize age appropriate care, for clients who have selected critical and complex medical conditions. 6. Discuss common pharmacological agents used for patients who have selected critical and complex medical and surgical conditions related to digestion, nutrition, and elimination. 18 Clinical 1. Integrate all previously learned knowledge while caring for critical and complex clients. 2. Incorporate the roles of a Level 4 Provider of Care, Manager of Care, and Member of the Profession when caring for patients who have critical and complex medical conditions related to problems of digestion, nutrition, and elimination. 3. Differentiate the elements of an advanced gastrointestinal assessment. 4. Critique and organize data to establish priorities when caring for patients who have selected critical and complex medical conditions related to the gastrointestinal system. 5. Anticipate and minimize complications when caring for patients who have critical and complex medical conditions related to problems of digestion, nutrition, and elimination. 6. Create individualized nursing care plans for patients who have selected critical and complex medical conditions related to the gastrointestinal system, and revise the plan of care as needed to optimize patient outcomes. 7. Incorporate collaborative problems into care plans, as appropriate. 8. Evaluate learning needs of the patient and / or their family, and design an appropriate teaching plan for disease prevention, health promotion, and self care for clients who have selected critical and complex medical conditions related to problems of digestion, nutrition, and elimination. 9. Classify selected medications used in critical care environments, anticipate their desired and adverse effects, and correlate them with selected gastrointestinal conditions. 10. Verify drug and intravenous solution delivery rates for patients who have selected critical and complex medical conditions related to the gastrointestinal system. 11. Describe how cultural perspectives affect the critically and terminally ill client, and how these are addressed in the critical care setting. 12. Function as a client advocate when caring for patients with who have selected critical and complex medical conditions related to the gastrointestinal system. 13. Critique and organize data to establish priorities when caring for patients with problems of digestion, nutrition, and elimination. 14. Relate physiologic conditions and treatment modalities for a client with problems of digestion, nutrition, and elimination. 19 Unit 11 – PROBLEMS OF EXCRETION INTRODUCTION The renal system plays an integral role in maintaining homeostasis through regulation of fluid and electrolyte balance, filtration of waste products, acid base balance, and blood pressure control. Thus, it is imperative for the student to possess a solid understanding of renal anatomy and physiology, in order to care for patients who have critical and complex medical conditions. A brief review of renal anatomy and physiology will be presented. In depth information regarding acute renal failure (ARF) and renal transplant will be presented. Additionally, care of patients requiring peritoneal and hemodialysis with will be introduced. The roles of the Provider of Care, Manager of Care, and Member of the Profession are integrated to promote successful transition from graduate nurse to entry level Registered Nurse (RN) when caring for a patient who has problems of excretion. OBJECTIVES Upon completion of this unit, the student will: Theory 1. Recall normal renal anatomy and physiology and previously acquired knowledge regarding problems of renal function. 2. Explain the components of an advanced renal assessment as they relate to caring for clients who have selected critical and complex renal conditions and dialysis. 3. Discuss the etiologies, pathophysiology, clinical manifestations, and complications for clients who have selected critical and complex medical conditions related to the renal system, including: • Acute renal failure • Renal transplant 4. Explain the collaborative management, as appropriate, including: diagnostic and laboratory data, nutrition, nursing diagnosis and interventions, pharmacology, surgical and nonsurgical treatments, safety, teaching and learning needs, and health promotion for clients who have selected critical and complex medical conditions related to the renal system. 5. Explain renal changes associated with aging, and summarize age appropriate care, for clients who have selected critical and complex medical conditions. 6. Describe the indications, complications, and nursing implications associated with dialysis. 7. Discuss common pharmacological agents used for patients who have selected critical and complex medical and surgical conditions related to the renal system. 20 Clinical 1. Integrate all previously learned knowledge while caring for critical and complex clients. 2. Incorporate the roles of a Level 4 Provider of Care, Manager of Care, and Member of the Profession when caring for patients who have critical and complex medical conditions related to the renal system. 3. Differentiate the elements of an advanced renal assessment. 4. Critique and organize data to establish priorities when caring for patients who have selected critical and complex medical conditions related to the renal system. 5. Anticipate and minimize complications when caring for patients who have critical and complex medical conditions related to the renal system. 6. Create individualized nursing care plans for patients who have selected critical and complex medical conditions related to the renal system, and revise the plan of care as needed to optimize patient outcomes. 7. Incorporate collaborative problems into care plans, as appropriate. 8. Evaluate learning needs of the patient and / or their family, and design an appropriate teaching plan for disease prevention, health promotion, and self care for clients who have selected critical and complex medical conditions related to the renal system. 9. Classify selected medications used in critical care environments, anticipate their desired and adverse effects, and correlate them with selected renal conditions. 10. Verify drug and intravenous solution delivery rates for patients who have selected critical and complex medical conditions related to the renal system. 11. Describe how cultural perspectives affect the critically and terminally ill client, and how these are addressed in the critical care setting. 12. Function as a client advocate when caring for patients with who have selected critical and complex medical conditions related to the renal system. 13. Differentiate elements of an advanced renal assessment related to dialysis. 14. Create a nursing care plan which integrates and correlates advanced renal data for a patient with altered renal function. 15. Critique and organize data to establish priorities when caring for patients with dialysis. 16. Relate physiologic conditions and treatment modalities for a client with dialysis. 21 Unit 12 – PROBLEMS OF PROTECTION INTRODUCTION Introduction This unit uses a nursing process approach to discuss alterations of the integument caused by burns. Burn injuries are in many respects the worst tragedies an individual can experience. Because of the systemic effects of the burn injury this unit will provide and overview of psychological implications, prolonged hospitalization, and comprehensive nursing care that is required during the emergent, acute phase, and rehabilitative phase. Other problems of protection include Multisystem Organ Dysfunction Syndrome (MODS). In depth information regarding MODS will be presented. The usual assessment findings, plan of care, nursing interventions, and evaluation of the interventions according to outcome criteria will be presented. OBJECTIVES Upon completion of this unit, the student will: Theory 1. Recall normal anatomy and physiology of the skin (structure and function).and previously acquired knowledge regarding problems of the skin. 2. Explain the components of an advanced skin assessment as they relate to caring for the burn client. 3. Discuss the etiologies, pathophysiology, clinical manifestations, and complications for clients who have selected critical and complex medical conditions related to the renal system, including: • Burns • MODS 4. Discuss types, causative agents and burn classification by depth and extent of injury. 5. Calculate the total body surface area involved in a burn injury using the rule of nines. 6. Explain the collaborative management, as appropriate, including: diagnostic and laboratory data, nutrition, nursing diagnosis and interventions, pharmacology, surgical and nonsurgical treatments, safety, teaching and learning needs, and health promotion for clients with burns and clients with MODS. 7. Explain integumentary changes associated with aging, and summarize age appropriate care, for clients who have selected critical and complex medical conditions. 8. Describe the indications, complications, and nursing implications associated with fluid resuscitation of the burn client 9. Use the Parkland formula to establish the correct rate and timing of fluid replacement. 10. Discuss common pharmacological agents used for the burn client and the patient with MODS. 22 Clinical 1. Integrate all previously learned knowledge while caring for critical and complex clients. 2. Incorporate the roles of a Level 4 Provider of Care, Manager of Care, and Member of the Profession when caring for patients who have critical and complex medical conditions related to burns and MODS. 3. Differentiate the elements of an advanced integumentary assessment. 4. Critique and organize data to establish priorities when caring for the client with burns and MODS. 5. Anticipate and minimize complications when caring for patients who have critical and complex medical conditions related to burns and MODS. 6. Create individualized nursing care plans for patients who have selected critical and complex medical conditions related to burns and MODS, and revise the plan of care as needed to optimize patient outcomes. 7. Incorporate collaborative problems into care plans, as appropriate. 8. Evaluate learning needs of the patient and / or their family, and design an appropriate teaching plan for disease prevention, health promotion, and self care for clients who have selected critical and complex medical conditions related to burns and MODS. 9. Classify selected medications used in critical care environments, anticipate their desired and adverse effects, and correlate them with burn and MODS clients. 10. Verify drug and intravenous solution delivery rates for patients who have selected critical and complex medical conditions related to burns and MODS 11. Describe how cultural perspectives affect the critically and terminally ill client, and how these are addressed in the critical care setting. 12. Function as a client advocate when caring for patients with who have selected critical and complex medical conditions related to burns and MODS. 13. Differentiate elements of an advanced integumentary assessment 14. Create a nursing care plan which integrates and correlates advanced renal data for a patient with burns or MODS. 15. Critique and organize data to establish priorities when caring for clients with burns or MODS. 16. Relate physiologic conditions and treatment modalities for a client with burns or MODS.