The Health Care Capital Expenditure Reporting Law: Report to the Minnesota Legislature
advertisement

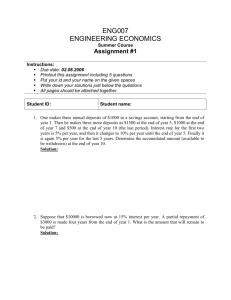
Joint Task Force on Health Care Costs and Quality The Health Care Capital Expenditure Reporting Law: Report to the Minnesota Legislature February, 2003 Joint Task Force on Health Care Costs and Quality The Health Care Capital Expenditure Reporting Law: Report to the Minnesota Legislature February, 2003 As required by Minnesota Statute 3.197: This report cost approximately $12,100 to prepare including staff time, printing and mailing expenses i Dear Interested Party: The 2002 Minnesota Legislature directed the Joint Task Force on Health Care Costs and Quality to study prospective review and approval under Minnesota Statute, section 62J.17, subdivision 6a, for a health care provider making a major spending commitment as defined in Minnesota Statutes, section 62J.17, and to report on whether the law has reduced health care costs or improved health care quality since its enactment in 1992. The attached report fulfills the mandate required by 2002 Minn. Laws, Chapter 384, section 2. This report was assigned to the Joint Task Force on Health Care Cost and Quality, an advisory group, in November, 2001. The task force is composed of ten legislators as well as five members of the Governor’s cabinet. In July, 2002, the task force asked the Minnesota Department of Health (MDH) to produce a first draft of the capital expenditure study for its review. After reviewing several drafts of the report, the Joint Task Force approved a final version in January, 2003. Questions and comments on the report can be directed to Elizabeth Langer of the MDH Health Economics Program at (651)282-5647. Report to the Minnesota Legislature ii The Capital Expenditure Reporting Law iii Table of Contents Introduction 1 Section 1 - Alternative Regulatory Approaches to the Health Care Marketplace 2 Market-Based Approach to Health Care 2 Market Failures - Regulatory Interventions 2 Supplier Induced Demand 3 Physician Self-Referral 3 Section 2 - The Capital Expenditure Reporting Law 5 Specific Statutory Findings on Capital Expenditure Reporting 6 The Capital Expenditure Reporting Law 7 Review of Capital Expenditure Filings 8 Prospective Review Orders 9 Provider Compliance with Capital Expenditure Filings 9 Section 3 - Analysis of the Capital Expenditure Reporting Law 10 Structure of the Law 10 Radiation Therapy Provision in Capital Expenditure Reporting 11 Impact on Cost and Quality 11 Potential Ancillary Effects of Capital Expenditure Reporting Law 12 Section 4 - Discussion and Policy Options 14 1. Repeal Capital Expenditure Reporting Law 14 2. Strengthen Capital Expenditure Reporting Law 15 3. Narrow but Strengthen the Capital Expenditure Reporting Law 15 4. Reinstate Certificate-of-Need Standards 16 5. “Intention to Build” Postings and Challenge Process 16 Report to the Minnesota Legislature iv 6. Strengthen Ban on Physician Self-Referral 17 Recommendations 17 Appendix 1 - Physician Self-Referral Law 19 Appendix 11 - Physician Referral Restrictions 21 Endnotes 23 The Capital Expenditure Reporting Law 1 INTRODUCTION In the early 1990s, the Minnesota Legislature enacted wide-reaching legislation intended to bring about changes to the health care system, including insurance reforms, the creation of the MinnesotaCare subsidized insurance program, global expenditure limits, and retrospective capital expenditure reporting for health care providers. Capital expenditure reporting was created as a temporary measure until all providers were working within capitated Integrated Service Networks (ISNs) or a regulated rate system. The stopgap measure was thought necessary in order to prevent the proliferation of new health care facilities and equipment, which the Legislature had deemed a significant cost driver. Although many of the reforms enacted in 1992 have been repealed, the capital expenditure reporting law remains intact. In 2002, there was considerable debate over the future of the law, and the Legislature directed the Joint Task Force on Health Care Costs and Quality to study the impact of the capital expenditure reporting law contained in Minnesota Statute, section 62J.17, for a health care provider making a major spending commitment. This report will examine whether the law has reduced health care costs or improved health care quality since its enactment in 1992. The Joint Task Force on Health Care Costs and Quality was formed by Governor Ventura along with legislative leaders in November, 2001, to generate immediate and longer-term recommendations to create sustainable and significant improvements for Minnesota’s health care system. The task force is composed of ten legislators as well as five members of the administration. In July, 2002, the task force asked the Minnesota Department of Health (MDH) to produce a first draft of the capital expenditure study for its review. MDH sent out a notice to the health care community inviting interested parties to meet with us to discuss their view of the law. Approximately 20 interviews with a wide-range of stakeholders, including hospitals, physicians groups, and trade associations were conducted. Additionally, legislators active in enacting the original law were interviewed. Second, we reviewed capital expenditure filings from the past 10 years for type and total expenditure of project as well as number of projects by institution. Finally, we reviewed available literature on the law as well as a related federal law. The first section of the report provides a brief overview of alternative regulatory approaches to managing the health care marketplace. The second section of the report gives a history of the law and provides details of the capital expenditure reporting process. The third section contains an analysis of the effectiveness of the capital expenditure reporting law and the fourth section provides policy options for the Joint Task Force and the legislature to consider. Report to the Minnesota Legislature 2 SECTION 1 – Alternative Regulatory Approaches to the Health Care Marketplace There is considerable debate among policymakers regarding the best approach to the delivery and purchasing of health care services. Regulatory approaches can take various forms along a continuum, from minimal oversight of insurance companies to setting allowable charges for certain services and controls on the addition of new technology, to setting global budgets and prioritizing payment for some services over the payment of others. A market-oriented approach involves a greater reliance on competition among providers and private negotiations between buyers and sellers to deliver appropriate amounts of health care services at fair prices to consumers. Market-Based Approach to Health Care Market advocates maintain that a largely unrestrained market would deliver the best possible health care at the lowest possible cost. They feel that “suppliers” of health care (physicians and other health providers) will generate the appropriate supply and type of health services, as demanded by patients (consumers). Additionally, in a field where changes in technology occur rapidly, market advocated argue that consumers, not insurers or government purchasers, should be allowed to decide, through a process of trying out new and alternative options to treatment, what the best choice is.1 Market advocates also believe that efficiencies are gained by eliminating bureaucracy associated with government regulation. Even in our current system, which combines free-market and regulatory features, market advocates would argue that mandates imposed by the government impede consumer choice and drive-up costs, while doing little to improve quality. Most market advocates would argue, however, that regulation can be beneficial in certain circumstances, if those regulations act to create a more competitive marketplace. An example of this would be enforcement of antitrust laws which act to counter situations where free trade is being inhibited. Market Failures – Regulatory Interventions Others believe that health care is fundamentally different from other goods and services and that government should strengthen its current controls on the system. Central to this argument is the belief that health care does not, and perhaps should not, operate under conditions needed for a competitive market. There are four conditions that must be met in order for a market to be considered perfectly competitive. First, consumers must have access to information that allows them to compare price and quality, and information must be equally available to buyers and sellers. Second, the product or service being sold must be uniform, so that if price and quality were the same consumers would be indifferent about which seller they choose to buy from. Third, there must be many buyers and sellers in the market, enough so that no individual buyer or seller has the power to influence prices. Finally, sellers must be able to enter and exit the market easily. The Capital Expenditure Reporting Law 3 Although the model of a perfectly competitive market is useful in theory, in the real world no markets – including the market for health care – meet all of these criteria. First, consumers do not generally have access to meaningful information on quality of providers and services. Information is not shared equally between buyers and sellers as it is, for example, in grocery products. In health care, the seller/producer has a greater level of information than the buyer/patient. Further, the patient relies upon the provider to specify a course of treatment and generally tends to follow the recommendation, regardless of price. There is evidence that in health care, greater supply of available services generates additional demand for services, often without improving health care outcomes.2 Complicating this matter is that unlike other goods, consumers generally do not know the price of the service they are consuming due to our insurance system. While insurance is necessary given the high cost of health care services, it can act to shield consumers from the cost of health care. Additionally, in an era of significant provider and health plan consolidation, there are many fewer sellers and purchasers of services than in previous times. Finally, as there are sizeable barriers for providers to enter the marketplace (schooling and licensure requirements), there is limited freedom of entry into the market. Supplier Induced Demand As mentioned above, suppliers of health services (physicians and other providers) largely control the course of treatment for their patients. This can lead to another problem with an open-market approach to health care, a concept known as supplier induced demand. Supplier induced demand in the health care industry takes place when a provider, motivated by increased profit, encourages a patient to incur more treatment than necessary. Treatment, in this scenario, includes such things as extra diagnostic testing or unnecessary cosmetic work, actions which do not harm a patient, but significantly increases the overall amount of money spent per treatment. Professional “codes of ethics” attached to licensure are intended to strongly discourage physicians and other providers from engaging in this type of practice. Physician Self-Referral A related issue is that of physician self-referral. This takes place when a physician refers a patient for treatment which they don’t directly provide but which occurs in a facility they own. For example, physician self-referral would take place when an orthopedist refers a patient for physical therapy to a facility which the orthopedist owns, but does not practice in or share physical facilities with. Since physician investors are not providing services at these facilities, many believe they constitute legalized kickbacks for the volume of patient referrals the physician generated. Several studies in the late 1980’s and early 1990’s found that physicians involved in the ownership of a clinical laboratory ordered a higher volume of diagnostic tests than physicians who did not own part of a lab.3 Concerns that these business arrangements would lead to higher costs led Congress to enact a series of laws (known as the Stark laws) which prohibit a physician from referring to an entity for various covered Medicare services if the physician or an immediate family member has a financial relationship with the entity (Appendix I, II). Proponents of a regulatory-based system believe that strengthening anti-referral laws would result in significant cost-control. Opponents of anti-referral laws maintain that the laws hamper innovation in health care delivery systems. Report to the Minnesota Legislature 4 Minnesota Statute 62J.23 gives the Commissioner of Health authority to promulgate rules restricting provider self-referral in a manner no less stringent than the federal laws referenced above. In the absence of a new rule, the statute applies the federal anti-kickback laws to all persons in the state. MDH has not proposed new rules in part due to the continual state of revision the federal law was in during the 1990’s. Although there have been recent suggestions that federal law may not be sufficient, MDH has not seen evidence that added state rules would be needed or would have adequate legislative support to withstand the predictable challenge from the provider community. The Capital Expenditure Reporting Law 5 Section 2 – The Capital Expenditure Reporting Law In 1992, Minnesota enacted the first set of a series of far-reaching health reform measures, known as the MinnesotaCare legislation. While the desire to expand access to health services and ensure quality of care were key to the framework of the legislation, the drive to find ways to contain health care costs was also a very visible and critical impetus for the legislation. As noted in the findings section of Minnesota Statute 62J: “The legislature finds that the staggering growth in health care costs is having a devastating effect on the health and cost of living of Minnesota residents…that the number of uninsured and underinsured residents is growing each year and that the cost of health care coverage for our insured residents is increasing annually at a rate that far exceeds the state’s overall rate of inflation. The legislature further finds that it must enact immediate and intensive cost containment measures to limit the growth of health care expenditures, reform insurance practices, and finance a plan that offers access to affordable health care for our permanent residents by capturing dollars now lost to inefficiencies in Minnesota’s health care system. The legislature further finds that controlling costs is essential to the maintenance of the many factors contributing to the quality of life in Minnesota: our environment, education system, safe communities, affordable housing, provision of food, economic vitality, purchasing power, and stable population. It is, therefore, the intent of the legislature to lay a new foundation for the delivery and financing of health care in Minnesota and to call this new foundation the MinnesotaCare Act.”4 While this report addresses Minnesota Statutes section 62J.17, the Capital Expenditure Reporting Law, it is important to remember that 62J.17 was passed in the context of a more global reform of Minnesota’s health care system. As demonstrated below, the legislature envisioned broad reform of the system, with capitated Integrated Service Networks (ISNs) competing on the basis of cost and quality in a regulatory-based, cost-contained environment. Specifically, the MinnesotaCare Acts of 1992 to 1994 contained the following elements: 1992 ! ! ! ! ! ! ! Establishment of Minnesota Health Care Commission Practice parameters for health care providers Retrospective capital expenditure reporting Antitrust exceptions Small employer insurance reforms, including guaranteed issue, guaranteed renewal, and rating restrictions Individual insurance reforms including guaranteed renewal and rating restrictions Creation of MinnesotaCare subsidized insurance program Report to the Minnesota Legislature 6 ! ! Minnesota Employers Insurance Program (MEIP) Rural Health Initiatives 1993 ! ! ! Integrated Service Networks (ISNs) – Integrated care systems or “Super HMOs” which would be paid a capitated rate and had to operate within state-wide expenditure growth limits Regulated All-Payer Option (RAPO) – Statewide physician fee schedule for all care delivered outside of ISN budgets Expenditure growth limits which would cap the amount of money spent on health care services and impose a ten percent per year reduction in the rate of growth for health care expenditures over a five year period 1994 (measures were to be in place by 1997) ! ! ! ! Universal coverage Individual insurance mandate, with guaranteed issue in the individual market Risk adjustment for both private and public sector Universal standard benefit set for insurance products Specific Statutory Findings on Capital Expenditure Reporting Legislative findings for Minnesota Statutes section 62J.17 are particularly instructive, as they give an indication of the legislative intent on passing this piece of legislation. With regard to capital expenditure reporting, the findings state: “…an important factor believed to contribute to escalating costs may be the purchase of costly new medial equipment, major capital expenditures, and the addition of new specialized services. After spending limits are established under 62J.04, providers, patients and communities will have the opportunity to decide for themselves whether they can afford capital expenditures…within the constraints of a spending limit. In this environment, the state’s role in reviewing these spending commitments can be more limited. However, during the interim period until spending targets are established, it is important to prevent unrestrained major spending commitments that will contribute further to the escalation of health care costs and make future cost containment efforts more difficult. In addition, it is essential to protect against the possibility that the legislature’s expression of its attempt to control health care costs may lead a provider to make major spending commitments before targets or other cost containment constraints are fully implemented because the provider recognizes that the spending commitment may not be considered appropriate, needed or affordable within the context of a fixed budget for health care spending. Therefore, the legislature finds that a requirement for reporting health care expenditures is necessary.”5 The Capital Expenditure Reporting Law 7 It appears from this statement that legislators were clearly concerned about a proliferation of building prior to the implementation of global spending limits and wanted the state to be involved in approving major purchases. However, while the overall approach to cost control during this time was regulatory in nature and relied heavily on state government for comprehensive health services planning, it also defined a more limited government role in capital expenditure approvals once global budgets were in place. The state never fully implemented global spending limitations, though, and the legislation does not address whether or not capital expenditure reporting was intended to continue in the absence of larger spending limitations. The “findings” language above seems to indicate that the legislature preferred to rely on the other tools. However, the fact that 62J.17 remains in law, while other pieces of the 62J health reforms have been repealed, seems to indicate a legislative intent to maintain reporting. The Capital Expenditure Reporting Law Effective April 1, 1992, a provider in Minnesota making a major spending commitment (greater than $500,000) is required to submit notification of the expenditure to the commissioner and provide any relevant background information. Major commitments are defined as new medical equipment, capital expenditures for the purpose of providing new health care services (excluding building updates or maintenance, information technology, and replacement of existing equipment), and the offering of new specialized services (such as opening a neonatal care unit). Notification consists of a report, submitted within 60 days of the commitment, that includes the dollar amount and specific purpose of the expenditure. The report is required to contain an impact statement regarding the effect of the expenditure on charges to patients and third party payers. Additionally, statements on clinical effectiveness, equivalent technologies presently available, distance of the new service from currently available services, and any collaborative business arrangements in conjunction with the new service need to be contained in the report filed with the Department. After an application is submitted, the commissioner has the authority to request additional information for the purpose of the review. When an application is considered complete, the commissioner is required to retrospectively review each major spending commitment and determine the appropriateness of the expense. In making the determination, the law directs the commissioner to consider the spending commitment’s impact on cost, access, and quality of health, the clinical and cost-effectiveness of the treatment, and alternatives available to the provider. Although the commissioner is not allowed to prohibit a spending commitment under retrospective review, if a provider fails a review, they may be required, for the following five years, to submit any major spending commitments to the commissioner for prospective approval. A provider that is subject to prospective review must file an application with the commissioner prior to making a major spending commitment. The information required for the application is statutorily identical to that in a retrospective review. Additionally, the commissioner is allowed to solicit information regarding the proposal from sources other than the provider. The commissioner is required, within 60 days of the prospective filing, to determine whether the proposed spending commitment is appropriate in light of alternatives available to the provider and notify the provider of the decision. Report to the Minnesota Legislature 8 There is a unique provision within the law that deals with radiation therapy facilities which was added in 2000. In addition to the criteria listed above for the determination of appropriateness, the commissioner must also consider the following criteria: alternatives available to patients in terms of avoiding unwarranted duplication, based on whether additional capacity is needed in or near an existing facility; and, the best interests of patients, including conflicts of interest, that may be influencing the utilization of the services, facility, or equipment related to the major spending commitment. These additional provisions do not apply, however, to radiation therapy facilities located in hospitals. The capital expenditure reporting law is often compared to a former law in Minnesota aimed at controlling the expansion or addition of hospitals and nursing homes, known as the “Certificate of Need”, or CON, law. When this law was in effect, from 1971to1984, hospitals were required to obtain approval from the Minnesota Department of Health prior to incurring major capital expenditures. The process was lengthy and the review indepth, as the organization under review was required to present evidence that an area was in need of new facilities. The law is no longer in effect, however, a regulation on the number of beds an individual hospital may be licensed for (essentially a moratorium on added capacity), has taken its place. For providers placed under prospective review, the law essentially functions as a CON, as they must receive approval from MDH before proceeding with their capital expenditure. The capital expenditure law differs from CON in the respect that, for providers not under prospective review, the process is retrospective and does not require MDH approval before an expenditure commitment can be made. Review of Capital Expenditure Filings Providers began filing capital expenditure data with the Minnesota Department of Health in 1992 and since that time, over 600 filings have been received. Reported expenses during this time have ranged from $500,000 for an equipment purchase to over $300 million for a clinic expansion project. The majority of the filings, nearly 300, are for upgrades of current equipment or facilities. Purchases of radiation imaging technology, such as MRI, CT, and PET scanners as well as ultrasound machines, are also very common filings. Less frequent are land acquisitions or changes in provider ownership. When a filing is received at MDH, staff typically will check past submissions by the provider to better understand how the current expenditure fits in with other recent filings and may consult with other parts of the Department to ensure compliance with the hospital moratorium and other laws. During the review, staff also examine collaborative relationships between the provider who submitted the filing and any other entity involved in the project as well as the distance of the new project from the nearest equivalent services. As allowed under statute, additional information may be requested from the filing provider. A determination of appropriateness is rendered once all of the above information is collected. During the ten-year span of the law, two providers have been found to have acted inappropriately according to guidelines set out in statute, and thus, placed on prospective review. The Capital Expenditure Reporting Law 9 Prospective Review Orders The first instance of a provider being placed on prospective review involved Minnesota Oncology Hematology Professional Association (MOHPA). MOHPA made a spending commitment in January 1997 to build, in partnership with the Texas-based US Oncology, a comprehensive cancer center in Maplewood, a suburb of St. Paul. When MDH staff learned of the construction of the cancer center, they informed MOHPA of the filing requirements. MOHPA initially claimed they were not subject to review because they didn’t meet the statutory definition of provider. After considerable correspondence with MDH, MOHPA submitted an application for review. However, when MDH asked for additional information regarding the relationship between MOHPA and US Oncology, MOHPA refused to provide the information requested by the Department. Thus, on September 28, 1998, MOHPA was placed on prospective review “due to the tardiness and inadequate detail in reporting their major spending commitment.” MOHPA and US Oncology will remain under prospective review until September 2003. The second instance of a provider being placed on prospective review involved MeritCare Health System, a North Dakota-based health system that owns several clinics in northwestern Minnesota. MeritCare made a spending commitment in September 1999 to add imaging services, radiation therapy, and a same-day surgery center to an existing clinic in Bemidji. North Country Health Services, a hospital located within a hundred yards and connected by a covered walkway to the clinic, had already added a same-day surgery center to their hospital that was not operating near capacity. Through the review process, MDH determined that MeritCare had acted inappropriately in opening a same-day surgery center in such close proximity to an existing facility with excess capacity. MeritCare was placed on prospective review in 2001 and will remain under prospective review until five years from the date of the order. Provider Compliance with Capital Expenditure Filings It is very difficult to measure the extent of provider compliance with the capital expenditure filing requirement because MDH is unable to independently track and monitor all new construction and purchasing. Although MDH has undertaken various measures through the years to increase awareness of the law, it remains likely that there are providers who have not submitted required filings. There have been a number of instances where the department will receive a collection of filings dating back several years from a single provider. There are also situations where fairly large facilities will go for several years without filing expenditure reports, making it likely that expenditures are being incurred but not reported. Report to the Minnesota Legislature 10 Section 3 – Analysis of the Capital Expenditure Reporting Law Structure of the Law While it is quite unambiguous that the capital expenditure reporting law is intended to control health provider capacity, and thus control costs, the law is not clear on criteria for placing a provider on prospective review. The law was constructed in a manner that allows MDH to flexibly apply the law in a variety of circumstances. The review criteria are vague enough that it is difficult to discern how strictly the legislature intended MDH to judge applications. For example, the statute does not contain an explicit definition of “appropriate spending commitments.” The law merely states that the commissioner may consider: “the spending commitment’s impact on cost, access and quality of health care; the clinical and cost-effectiveness of the commitment; and, the alternatives available to the provider” when making a determination.5 Since there is not a reliable mechanism for predetermining a spending commitment’s impact on the cost of health care, even a provider willing to put a great deal of effort into their application would not be able to truly fulfill this particular information requirement. Another issue which frequently arises during MDH review of capital expenditures is that of access to health care. Again, while the statute pertaining to capital expenditures states that access to health care is an important consideration in the determination of appropriateness, it does not define what degree of “access” is considered appropriate. This complicates the review process, because there are many different factors that can be considered when one determines whether a new service is needed to maintain “access” to care. For instance, with regard to highly specialized care, such as organ transplant centers, one might be considered to have access to care because there is a transplant center in the state of Minnesota. When considering less-specialized services, such as annual physicals, the standard is quite different, and if residents must drive more than a certain number of miles to obtain services, they might not be considered to have access to care. The issues becomes significantly more complex when reviewing applications for items such as radiology testing equipment and same-day surgery centers. Access, when expenditure reports are submitted for these types of services, is often defined as what is most convenient for patients. Because there is no standard to say “an area needs XX MRI’s per 100,000 people” nor is there clear legislative guidance as to appropriateness, the factors listed above make it difficult for MDH to determine whether expenditures are appropriate. We speculate that the criteria are vague largely because this law, as originally enacted, was meant to be one temporary aspect of a much larger series of laws aimed at controlling health care costs. Since 1994, most of the cost containment laws have been repealed and the policy debate has largely centered around increasing competition and options for consumers. As a consequence, the department, while vigorous in collecting information regarding expenditures, has approved all applications with the exception of two clear violations of the statute. A final issue in regards to the structure of the law is the ability of an existing group of providers to create a new entity with identical owners. While the existing providers may be creating the new entity for tax purposes it also allows them to escape the reporting requirements of 62J.17. This is due to the definition of “provider” in the The Capital Expenditure Reporting Law 11 statute. The statute defines a “provider” as “any existing provider.” Thus, new providers or providers who are intending to begin practice but have not started yet, are not required to comply with the statute. We were unable to determine the extent to which this issue has occurred. Radiation Therapy Provision in Capital Expenditure Reporting As stated earlier, there is a special provision in 62J.17 dealing with radiation therapy facilities which exist outside of a hospital. In their expenditure filings, stand-alone facilities must examine alternatives available to patients in terms of avoiding unwarranted duplication and the best interests of patients, including conflicts of interest, that may be influencing the utilization of the services, facility, or equipment. Some operators and owners of standalone facilities, stated that they are at an unfair competitive disadvantage due to the special set of regulations. They maintained that hospitals should not be given special considerations in the regulatory field, and that if hospitals cannot compete for services, they shouldn’t be offering them. Additionally, they pointed out that if a hospital decides to build a radiation therapy facility outside of the physical hospital, essentially creating a stand-alone facility, they are still regulated as a hospital, and are exempt from special reporting requirements. In contrast, if a group of physicians built a facility in the identical spot, they would be regulated differently. Hospitals maintain they need the protection the regulation affords them because they are actually at a competitive disadvantage with the stand-alone facilities. They believe that hospitals offer a larger community value in providing services, such as emergency rooms and charity care, which stand-alone facilities need not offer. As such, hospitals argue that their unique status and mission to provide a broad range of services merits different regulatory status than those facilities that offer a single service. The exemption of hospitals from the special reporting and analysis requirements of section 62J.17, subd. 8 raises an interesting public policy issue. While hospitals undoubtedly play an important role in ensuring a broad range of services for patients and providing expensive, but not particularly profitable, services such as 24 hour emergency rooms, it can be questioned whether entities providing essentially the same services should be regulated in a differential manner, particularly if both can build stand-alone facilities and have different regulations apply. There is a public policy argument for ensuring preservation of hospital-based services; the question is, whether differential regulation is the correct means to meet this public policy goal. Impact on Cost and Quality During the course of our investigation for this study, we found little evidence that the capital expenditure reporting law has had an impact on institutional planning. With one exception, out of approximately twenty interviews conducted, interviewees uniformly saw the capital expenditure reporting process as an administrative hurdle that had very little influence on their ultimate decisions to acquire new technology or add additional services. Many administrators commented that the case they had to present to their board of directors or senior management prior to committing to a capital expenditure was as, if not more, stringent than capital expenditure reporting requirements. Report to the Minnesota Legislature 12 Administrators interviewed for this study felt the law’s impact on health care costs has been minimal. Many cited the fact that, as only two providers have been placed on prospective review during the past ten years, it is fair to conclude that controls placed on an institution’s ability to incur new capital expenditures have been very limited. Given the proliferation in recent years of facilities providing care in such profitable areas of health care as imaging, radiation therapy, and heart treatment, it is clear that this law, as currently written and applied, has placed few capacity constraints on the system. It is again important to remember that the capital expenditure reporting law was passed in the context of a global health reform initiative, most pieces of which have been repealed. In the narrow area of radiation therapy, some of the administrators we met with argued that the law has had a significant impact on controlling capacity. As stated earlier in the report, one of the two organizations that have been placed on prospective review is MOHPA, an oncology group. MOHPA was placed on prospective review following the construction of a comprehensive cancer center in Maplewood for their failure to comply with MDH requests for information related to the facility. A primary competitor to MOHPA maintains that if MOHPA had not been placed on prospective review four years ago, they would have built several cancer treatment facilities and monopolized the market in this area. This competitor told us that they feel the law has prevented this from happening and thus, held costs down in the area of cancer treatment. It is possible that, absent the law, groups placed under prospective review for failure to comply with the statute would have continued to build excess capacity. In this way, the law potentially did curb capacity. However, we have no way of knowing what would have occurred absent the law. With regard to quality, the majority of administrators agreed that the law has not had an impact on quality. This is due, in part, to the lack of guidance within the original legislation on which to judge whether or not new equipment or services would have a discernable impact on quality of health care. As it currently stands, so long as the capital expenditure in question is safe and effective, MDH does not engage in the much larger question of whether or not the expenditure will ultimately improve health care quality in the broader community. As MDH hasn’t used quality criteria to stop facilities from being built or equipment from being purchased, the law has also likely had little to no impact on health care quality. The current state of quality of care is partially a reflection of the investments in equipment and services that providers have chosen to make. We think it is unlikely that providers have considered the law when planning construction of new facilities or equipment purchases; that is, while they may have invested in equipment that they believe improve quality of care, these investments were likely made without regard to the law. Potential Ancillary Effects of Capital Expenditure Reporting Law Several people interviewed for this study expressed concern that not only do they believe the capital expenditure reporting law has failed to control costs, but they think the law has the potential to encourage institutions to over-build. Over-building would take place when an institution has made a capital spending commitment and decides to build a larger facility than needed in order to prevent competitors from building a similar facility. By constructing a facility, institutions can claim they have extra capacity and therefore make the argument that a similar facility within the area results in an inappropriate expenditure. The Capital Expenditure Reporting Law 13 The Department witnessed an issue similar to over-building when a hospital notified us that they were adding radiation therapy services to the hospital. When MDH approved the expenditure, the hospital presented their approval letter to a multi-specialty group clinic who also wanted to build a radiation therapy center. Hospital officials told clinic administrators they could not proceed with their plans to add radiation therapy to the clinic or they would be found, by MDH, to have incurred inappropriate expenditures. Ultimately, the hospital dropped its plans to build the center and the clinic moved forward in constructing its facility. This issue reinforces the above concerns regarding a lack of guidance contained within the law. The law is silent on the issue of two providers filing nearly simultaneously for essentially identical projects. While two projects in the same geographic area are certain to result in over-capacity and increased spending, MDH does not have implicit authority or guidance on how to deal with the situation. While MDH can request that two parties work together, if they ultimately decide to move forward with their projects, the statute contains no guidance on how to deal with this situation. Similar to over-investing is the strategy of tactically adding services to a facility so that an institution’s competitor will be prevented from offering the identical service. For instance, a provider may choose to purchase imaging equipment in a marketplace they expect their competitor to enter. By entering the market first, they can potentially prevent their competitor from building a similar facility or adding similar equipment. Report to the Minnesota Legislature 14 Section 4 – Discussion and Policy Options During the course of conducting this study, we found little evidence that the Capital Expenditure Reporting Law has had an impact on health care costs or quality. Similarly, we think it is unlikely that providers have taken the law into significant consideration when planning the construction of new facilities or equipment purchases. There is currently little or no discussion, and certainly very little consensus, around what we, as a state, want to get from our health care system. Costs within the system are rising rapidly and growing faster than overall wages or the rate of the economy. A rapid rate of health care cost growth and the allocation of more of the overall economy to health care is, per se, neither good nor bad. It does mean that fewer resources are available to allot to non-health care activities. The “correct” level of health care spending and whether we are getting value out of the health system are issues about which there is limited agreement. Cost growth could be “good” if it means that more Minnesotans are getting higher quality care and/or that our growing need for care is simply being met as the population ages. If, on the other hand, health care costs reflect inefficiencies, unnecessary or poor quality care, private and public payers might reasonably look for more rigorous cost controls. At present, there is little consensus on government’s role in the health care system. There are particular gaps in agreement on the extent to which government should assure or directly measure quality, or should make value judgments about expenditures. In order for any policy initiative to succeed from this process, it is vital that lawmakers discuss the direction they believe the state should go with regard to regulating the health care system. Does the state want to encourage competition by moderating current regulations and allow for providers and facilities to compete more vigorously against one another? If so, issues such as the hospital moratorium, the prohibition on for-profit health plans, and scope of practice laws, may need to be examined. Conversely, do policymakers feel that attempts to encourage competition won’t succeed due to the unique characteristics of the health care industry? If so, policymakers may think the state needs to be more involved with structuring the market. Or does the answer lie somewhere in between? For instance, should the state repeal or modify certain regulations and simultaneously examine areas that may require greater regulatory scrutiny? Six policy options for lawmakers to consider with regard to capital expenditure reporting follow. 1. Repeal Capital Expenditure Reporting Law This review concludes that it is unlikely that the capital expenditure reporting law has had a measurable impact on health care costs or quality in Minnesota. Providers reported that the law served more as a bureaucratic hoop to jump through than as a meaningful part of their decision process regarding facility or treatment expansion. Finally, the proliferation of health facilities and specialty services lend further evidence that the law has been largely ineffective in controlling costs or having an impact on quality. The capital expenditure reporting law was intended to be partnered with several other reform-oriented measures aimed at controlling health care costs. These other measures, such as global budget limits and state-wide health planning, were repealed prior to having been implemented, placing more burden on a law never intended to be a major ongoing tool in limiting cost growth, at least as currently written and applied. Given these factors, it is reasonable to examine repealing statute 62J.17. The Capital Expenditure Reporting Law 15 2. Strengthen Capital Expenditure Reporting Law Alternatively, legislators may conclude that although the law in its current form has not been effective, the correct policy solution is not to dismantle the regulation, but to strengthen weak areas of the law. For instance, policymakers could choose to statutorily define “appropriate spending commitment” and thus provide MDH with clear standards to judge expenditure filings. Legislators could also set parameters regarding access to health care. This would involve making decisions on acceptable waiting times for receiving certain services. Additionally, decisions would need to be made concerning acceptable driving distances for services. Finally, and perhaps most controversially, legislators would need to determine what level of utilization would be considered to put a facility at “full” capacity. For instance, if a CT scanner at a non-hospital location is only in use 80 percent of the time between 8:00am to 4:00pm, Monday through Friday, is the machine considered to be near capacity, or should operators be required to extend their hours of business before purchasing a new machine? A strengthened law should also provide guidance on such issues as what MDH should do if two similar facilities are being constructed simultaneously in the same geographic area or if MDH has knowledge of providers overbuilding in order to prevent their potential competitors from adding services. Additionally, the law should amend the definition of “provider” to include new providers or providers intending to begin practice. While a law such as this would certainly ensure that providers meet a stronger standard for purchasing new equipment or constructing a new facility, it is unclear if the law would have a measurable impact on health care costs or quality. The law would need to be constructed in such a manner that MDH is empowered to stringently review filings and meaningfully penalize those who do not comply with the regulation. Additionally, it would be important to set up an evaluation mechanism associated with the law to measure its impact on costs and quality. 3. Narrow but Strengthen the Capital Expenditure Reporting Law If legislators have concerns with entirely dismantling the regulation or, conversely, enacting a new, all-encompassing regulation, an alternative may be to amend aspects of the current law. Upon further examination, lawmakers could determine that particular types of expenditures are responsible for a large amount of overall capital expenditure growth and specifically regulate that category of expenses. A variation of this approach is currently in place in 62J.17, with radiation therapy facilities having an additional set of reporting and evaluation requirements. Under this option, the legislature may choose to repeal the broad reporting requirements while leaving in place and perhaps strengthening requirements for a more narrow group of providers. In addition to narrowing the type of expense reviewed, lawmakers would be advised to update the amount of expense which triggers a review (currently anything over $500,000) so that it maintains pace with inflation. Another consideration would include whether or not reviews should take place prospectively or retrospectively. Finally, lawmakers would need to consider creating more specific standards by which the regulating body would judge pending applications. Report to the Minnesota Legislature 16 It is unclear whether a law structured such as this would have a more significant impact than current statute. Additionally, discerning which category of expenses have the greatest impact on overall health spending in the state would require considerably more detailed data collection and analysis than the legislature has previously supported. 4. Reinstate Certificate-of-Need Standards Given strong evidence regarding rising health care costs, lawmakers might come to the conclusion that market forces have failed to positively impact the health care system and a greater level of regulation is needed in order to control costs. Lawmakers could explore the possibility of requiring all providers to undergo a prospective review prior to committing funds to a new facility or service expansion above a certain dollar amount. Instating a prospective review process for capital expenses over a set amount would involve many decisions on the part of lawmakers. A dollar amount which triggers a prospective review would need to be agreed upon, as would expenses (such as remodeling, new building and service expansions) covered by the new law. Additionally, clear standards for approval or denial of the proposed expense would need to be stated in statute. Another consideration would be regarding resource allocation to the regulatory body overseeing the process. Implementing the regulation would be a labor intensive process and require several dedicated staff to ensure that reviews take place in a timely manner. Finally, lawmakers would need to consider appropriate sanctions for those found to be violating the law. If lawmakers choose to go this route, they should explore the effectiveness of the former certificate-of-need standard. During the interviews conducted for this study, we inquired about administrators’ thoughts toward the former law. They reported finding the process lengthy and cumbersome. Additionally, interviewees uniformly stated they believed that most proposals eventually wound up being approved, it just took longer because of the process. Finally, many expressed their belief that the law cost providers a significant amount of money, due to the substantial legal fees associated with gaining approval for a new hospital. A study conducted in 1984 by MDH concurs with these opinions and states that, “between 1978 and 1983, only two percent of certificate of need applications were denied.”6 5. “Intention to Build” Postings and Challenge Process Providers planning a project which cost over a certain dollar amount would be required to file a notice with MDH prior to beginning the building phase of the project. MDH would not review the project; rather, they would publicly post the project for a period of time (30-60 days). During this time period, other providers would have the ability to challenge the proposal and, if need be, MDH would hold a hearing on the matter and make a determination of appropriateness. The Capital Expenditure Reporting Law 17 6. Strengthen Ban on Physician Self-Referral In our interview process, many people suggested that the incursion of capital expenditures, per se, is not a major cost driver in the current system. Rather, they feel that exemptions to the federal ban on physician selfreferral, and the capital expenditures this encourages physicians to incur, is a larger issue. As such, the legislature could consider strengthening Minnesota Statute 62J.23, which governs provider conflicts of interest. Minnesota Statute requires that restrictions on provider conflicts of interest be no less stringent than the Medicare anti-kickback statutes in place. The statue also gives the Commissioner of Health the authority to adopt more rigorous rules. Because rulemaking is a lengthy and cumbersome process that can simply be overturned by statute if there is not legislative support for the policy, a more direct approach would be for the legislature to pass a law to tighten any perceived loopholes in the anti-kickback laws. As noted earlier, there are two principal exemptions within the federal law that apply to both ownership interests and compensation arrangements. The physician services exemption permits referrals for health services that are furnished by a member or physician in the same group practice as the referring physician, or under the supervision of the referring physician. The in-office ancillary services exception permits referral for provision of health services in the same building in which the referring physician, or their group, routinely provides the full range of the group’s or physician’s medical services. The group practice exemption is more problematic than the ancillary services exemption and could be tightened to only include large, multi-specialty group practices. This would potentially disallow situations where a singlespecialty group includes one physician of a different specialty and obtains an exemption from the law. Recommendations In reviewing the above options, the Task Force members considered making a recommendation to repeal or amend the existing statute. However, when it became clear they would not be able to reach a consensus opinion, they decided to submit the report without making any specific recommendations for statutory change. Report to the Minnesota Legislature 18 The Capital Expenditure Reporting Law 19 Appendix I – Physician Self-Referral Law Physician self-referral takes place when a physician refers a patient for treatment at a facility which they own, but do not necessarily provide services in. For example, physician self-referral would take place when an orthopedist refers a patient for physical therapy to a specific facility which they own. When physician investors are not providing services at facilities they own, many believe they constitute legalized kickbacks for the volume of patient referrals the physician generated. Several studies generated during the late 1980s and early 1990s fueled the concern of policymakers. For instance, Hillman and others found that self-referring physicians were 4 times more likely to order imaging services for patients versus radiologist-referring physicians.7 Additionally, similar concerns were pointed out by Scott and Mitchell with regards to clinical laboratories. They found that physicians involved in the ownership of a clinical laboratory ordered a higher volume of diagnostic tests than physicians who did not own part of a lab.8 Studies such as those listed above lead Congress to enact a law that has become known as “Stark I,” a prohibition on physician referrals to clinical laboratories which they or a family member had an ownership stake in. In 1998, new rules were proposed to update and expand the regulation to include a majority of health services and the law is now referred to as “Stark II.” Generally, the law prohibits a physician to refer to an entity for various covered Medicare/Medicaid services if the physician or an immediate family member has a financial relationship with the entity. Services covered under the law are: clinical laboratory services; inpatient and outpatient hospital services; radiology and other imaging services; physical and occupational therapy services; durable medical equipment; parenteral and enteral nutrients; radiation therapy services and supplies; outpatient prescription drugs; home health services; and prosthetics, orthotics, and related supplies. Radiology services which are considered preventive, such as mammograms, are not subject to regulation.9 There are two principal exemptions within the law which apply to both ownership interests and compensation arrangements. The physician services exemption permits referrals for health services that are furnished by a member or physician in the same group practice as the referring physician, or under the supervision of the referring physician. Some of the main requirements which must be met to be considered a group practice include: the expenses and income of the practice must be distributed according to methods determined before expenses were incurred or revenue produced; physicians may not be compensated based on the volume or monetary value of their referrals; and, the group practice must have centralized decision-making, consolidated billing, accounting and financial reporting, and centralized utilization review.10 The in-office ancillary services exception permits referral for provision of health services in the same building in which the referring physician, or their group, routinely provides the full range of the group’s or physician’s medical services. Indirect financial arrangements, in which the is relationship formed through an intervening third party, are also included. This would apply when a physician has an ownership interest in, or compensation arrangement with, an entity that has an agreement with a hospital to which the physician refers.11 Report to the Minnesota Legislature 20 In the eyes of many critics, the exemptions to the federal law render it fairly ineffective. During the interviews conducted for this study, one detractor stated that the group practice exemption is often exploited by single-specialty groups who hire a physician outside of their specialty in order to obtain multi-specialty status. The interviewee claimed this is particularly true for single-specialty groups that are dependent on other physicians for referrals. A physician-oriented publication backs up the claim that the regulation is not as restrictive as intended in its authorizing legislation, “The Final Rule is intended to provide more flexibility to providers by interpreting the prohibitions narrowly and the exemptions broadly. In fact, it appears that providers may find that the Final Rule permits them to establish relationships once thought prohibited or the restructure existing arrangements to make them more productive.”12 Supporters of the current structure of the federal regulation would say it allows for physicians to collaborate with their colleagues and design more innovative mechanisms to deliver health care. They balk strongly at the idea a physician would order unnecessary treatment for a patient, but concede that evidence is less clear on diagnostic testing. Evidence on this topic is quite murky. It certainly appeared, during the early 1990’s, that physician ownership of facilities was a cause for concern. However, new research on the topic is virtually non-existent. The only recent study completed on the topic found that, when physicians owed ambulatory surgery or diagnostic imaging centers, they were more likely to refer patients to their centers than to hospitals.13 One must be cautioned in interpreting these results due to the very small sample size employed by the researchers. Another issue to note is that the bulk of the literature on this topic was completed prior the implementation of the latest version of the Stark regulation. Thus, it is not yet possible to measure if the regulation has had an impact on referrals and costs. State policymakers may wish to consider pressing for more federal action on this topic. For instance, Congress could be petitioned to direct the Agency for Health Quality and Research (AHRQ) to update the research on the impacts of self referral (or on broader questions of capacity and links to cost and quality). Or, the legislature may wish to debate adding more state level regulations in this area, in which case concerns about Minnesota’s attractiveness as a practice climate for providers should be anticipated. The Capital Expenditure Reporting Law 21 Appendix II Physician Referral Restrictions Physician Self-Referral Physician self-referral takes place when a physician refers a patient for treatment at a facility which they own. This is a very common practice which can involve services such as mammograms, blood work, or ultrasounds. Some believe that physician self-referral becomes a concern when a physician refers a patient to a facility which they own, but do not provide services in. Since physician investors are not providing services at these facilities, many have raised concerns that these referrals constitute legalized kickbacks for the volume of patient referrals the physician generated. History of Stark I and II By 1989, lawmakers at the federal level became concerned because a number of studies had shown that physician referrals to facilities which they had a financial relationship with, but did not practice at, encouraged excessive use of those services. This led Congress to enact a limited ban on physician self-referral for Medicare patients. This became known as “Stark I.” The original ban was narrow in its scope, only prohibiting physician ownership of clinical laboratories. After Stark I was enacted, a number of states enacted prohibitions on an additional number of health services (see list on following page) In 1998, new rules were proposed to update and expand the regulation to include a greater number of health services. The law is now referred to as “Stark II.” Stark II Specifics Stark II prohibits a physician from referring a Medicare or Medicaid patient to a facility which they, or an immediate family member, have a financial relationship with, but do not practice at. The services, facilities, or equipment included in this ban are: ! ! ! ! ! ! ! ! clinical laboratories; physical therapy services; occupational therapy services; radiology services and supplies; radiation therapy services and supplies; durable medical equipment and supplies; parenteral and enteral nutrients, equipment, and supplies; prosthetics, orthotics, and prosthetic devices and supplies; Report to the Minnesota Legislature 22 ! ! ! home health services; outpatient prescription drugs; and, inpatient and outpatient hospital services. There are two specific exemptions in Stark II. The Physician Services Exemption permits referrals for all services that are furnished by a member or physician in the same group practice as the referring physician, or under the supervision of the referring physician. The In-Office Ancillary Services Exemption permits referral for services in the same building the referring physician, or their group, routinely provides the full range of the group’s or physician’s medical services. States with Self-Referral Restrictions Following is a list of states that have enacted additional self-referral restrictions (33 total). Many of the states listed, including Minnesota, have adopted the Stark restrictions for their entire insured population, not just Medicare and Medicaid enrollees. ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! Alaska, Arizona, Arkansas California, Colorado, Connecticut Florida Georgia Illinois Kansas, Kentucky Maine, Maryland, Massachusetts, Michigan, Minnesota, Missouri Nevada, New Jersey, New York, North Dakota Ohio, Oklahoma Pennsylvania Rhode Island South Carolina, South Dakota Tennessee Utah Virginia Washington The Capital Expenditure Reporting Law 23 Endnotes 1 Green, Martin. The Economics of Health Care. Office of Health Economics, London, UK. 2 Wennberg, John. The Dartmouth Atlas of Medical Care. Scott E, Mitchell JM. Ownership of Clinical Laboratories by Referring Physicians: Effects on Utilization, Charges, and Profitability. Medical Care 1994; vol. 32, no. 2, pp 164-174. 3 4 Minnesota Statutes 62J 5 Minnesota Statutes section 62J.17 Minnesota Department of Health. “Certificate of Need Review in Minnesota: Past Effectiveness and Issues for the Future.” March, 1984. 6 Hillman BJ, et. al. Frequency and Costs of Diagnostic Imaging In Office Practice – A Comparison of SelfReferring and Radiologist-Referring Physicians. New England Journal of Medicine, December 6, 1990. 7 Scott E, Mitchell JM. Ownership of Clinical Laboratories by Referring Physicians: Effects on Utilization, Charges, and Profitability. Medical Care 1994; vol. 32, no. 2, pp 164-174. 8 9 www.hcfa.gov/medlearnfaqs/faqphys.html 10 CMS guidance Lebowitz, PH. Self-Referral Rule Holds Risk and Opportunity. Radiology Management, September/October 2001. 11 Lebowitz, PH. Self-Referral Rule Holds Risk and Opportunity. Radiology Management, September/October 2001. 12 Lynk WJ, Longley CS. The Effects of Physician-Owned Surgicenters on Hospital Outpatient Surgery. Health Affairs 2002; vol. 21, no. 4. 13 Report to the Minnesota Legislature 24 The Capital Expenditure Reporting Law To obtain additional copies of this report, please contact: Minnesota Department of Health Minnesota Health Information Clearinghouse P.O. Box 64975 St. Paul, Minnesota 55164-0975 (651) 282-6314; (800) 657-3793 TDD (651) 215-8980 If you require this document in another format, such as large print, Braille or cassette tape, call (651) 282-6314 Printed with a minimum of 10% post-consumer materials. Please recycle.