Surviving Before Thriving Part II: It Hasn't
advertisement

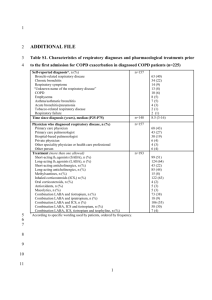
Surviving Before Thriving Part II: Michael J Hewitt, RRT, ACCS, NPS, RCP, FAARC, FCCM Clinical Manager, Respiratory Care Services Rhode Island Hospital & Hasbro Children’s Hospital Principal Teaching Hospital, The Warren Alpert Medical School of Brown University Providence, Rhode Island Chair; Respiratory Section, Society of Critical Care Medicine Secretary, Rhode Island Society for Respiratory Care Conflict of Interest Disclosures I wish to disclose the following potential conflicts of interest: Type of Potential Conflict Details of Potential Conflict Grant/Research Support Consultant Speakers’ Bureaus Financial support Other Monaghan Medical, Hollister, Inc Remember This? The Fork In The Road…. The Road To Extinction? Surviving & Thriving Things Haven’t Gotten Any Better Let’s Review: The Medical Environment Is Still Changing Reimbursement Structures Are Worse Payor Mixes Continue To Be Unfavorable We Are Still Under The Microscope What’s The Big Deal? Our Problems As A Profession Are NOT The Result Of Or The Fault Of The ACA Respiratory Therapy Is Still An Easy Target And It Is Still Our Own Fault It’s Still All About What Value We Bring To The Table: Now More Than Ever How Do We Get There? Reminder: Incentive Spirometry, Albuterol & Mucomyst Ain’t It! Changing Tradition Is The Key To Our Survival It’s That Simple Or Is It? Payor Mixes Are At Critical Mass Some Real Life Examples: Hospital A: 71% Hospital B: 54% Hospital C: 55% Hospital D: 69% Where Does Your Hospital Lie? Changing Tradition Surgical Patients: Aggressive & Proactive (90% Of All Surgical Patients Get Atelectasis) Medicine Patients: Aggressive & More Effective (COPD Is Now On The 30 Day Readmission Penalties List) There’s a Whole New Wave Of Patients On The Way. Who Are They? The Baby Boomers!! (the class of 46-64) aka: The Silver Tsunami 69,500,000 Americans Eligible To Retire In The Next 6 Years Is This COPD Thing Really A Big Deal? My Own Hospital COPD Readmissions <30 Days avg. LOS (June 12-July 14): 8.44 days actual vs. 4.17 expected (UHC) Average Cost Per Readmission: Floor Admission: $35,268.91 ICU Admission: $154,696.00 That = Financial Disaster Where Does Your Hospital Lie? So, Now What? We Develop A Plan/Strategy To Decrease These Readmissions: • • • • Better And More Effective Therapies Education By RT’s (Case Manager Credentialed?) Provide Patients With Better Home Devices Post Discharge Home Visits By RT’s For First 30 Days • Hard Core Data Gathering Opportunities For Success Redefine Oxygen Therapy Transitioning From “The Chase” Go From This: To This: Positive Pressure & Vibratory Therapy High Efficiency Nebulizers Monaghan AeroEclipseTM Aerogen AeroNebTM Aerobika* OPEP in COPD and Bronchiectasis OBJECTIVE – Clinical evaluation of the Aerobika* Oscillatory PEP device in patients with bronchiectasis and COPD • Only COPD patients with chronic bronchitis and/or chronic sputum production were selected METHODOLOGY – n=29; longitudinal 6 week cross-over study – 67 (±10) years old; 13 male, 16 female • COPD (n=15, aged 65±9, 9 male/6 female) • Bronchiectasis (n=14, aged 69±10, 4 male/10 female) – Aerobika* Oscillating PEP (3 weeks)/No device (3 weeks) EVALUATION POINTS – Each Clinic Visit: spirometry, plethysmography, Six Minute Walk Test, St. George’s Respiratory Questionnaire, 4x daily OPEP administration, Symptom diary, 3He MRI Aerobika* Oscillating PEP in COPD and Bronchiectasis COMBINED STUDY RESULTS • Numerous patient outcomes were shown to be statistically improved following use of Aerobika* OPEP – – – – – – • Breathlessness (dyspnea) Quality of Life (SGRQ measures) Cough Frequency Ability to Exercise Ease of Bringing up Sputum Lung Function • Resulting from decreased airway obstruction (improved Slow Vital Capacity%pred) 3He MRI revealed changes in lung ventilation – Increase in air transfer from previously unventilated areas – Decrease in gas trapping (hyperinflation) • No adverse events were recorded Aerobika* OPEP in COPD and Bronchiectasis Additional Opportunities Even More Opportunities • Pre-hospital Rescue CPAP: If You Don’t Have a Tube, You Can’t Get a VAE/VAP. • HFOV In Fluid Resuscitated Trauma Patients • The Role of RT’s in Organ Procurement • What Else? We Are Held Back Only By Ourselves Let’s Check In With The Students: • EMBRACE The Students: • Stop Eating Our Young • The Students Are The Future Back At The Fork In The Road Again…. The Road To Extinction? Surviving & Thriving Are WE (or you) Ready And Willing To Get Past The Fork? So, Are We Really In Trouble? Or Am I Just a Lot Of Hot Gas? Another Real Life Hospital Example: 250 Bed Facility 5-6 RT’s On Days; 4 On Nights 3 Adult ICU’s Trauma ED Typical 12 Hour Shift Workload: • • 35 (525 minutes) to 60 (900 minutes) scheduled RVU’s 7-8 vents, 4-6 BiPAP’s, N.O. administration, infant SiPAP’s, bronch’s, PFT’s yada, yada, yada New Issue: Directed to explore replacing RT’s with “trained” non licensed personnel. Is This Value Based? If You Need Still More Convincing: Kentucky One Health System, Louisville, Ky: Laid Off 500 People; Eliminating Additional 200 Positions Turned Over ED Respiratory Functions To Nursing This Includes Treatments, ABG’s, Vent Management, Etc. Nurses Get a 4 Hour “Refresher Class” In Respiratory Therapy How Did We Get To This? And Finally: Remember These Most Expensive Words In Medicine: “But That’s The Way We’ve Always Done It” Questions? Michael J Hewitt, RRT, ACCS, NPS, RCP, FAARC, FCCM mhewitt@lifespan.org