Chronic pain - The practical Nurse Practitioner
advertisement

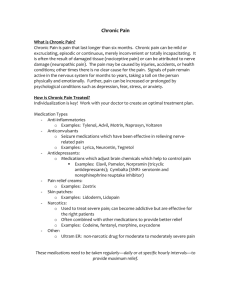
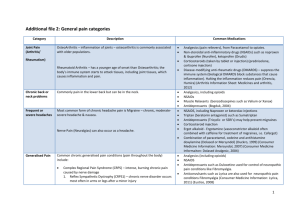
T “What do you mean my MRI is negative? My back still hurts! “My whole body aches.” Annemarie M. Kallenbach RN CNP No Disclosures docakilah.wordpress.com Fibromyalgia and chronic back pain are two time consuming and frustrating diagnoses seen frequently in clinical practice Choosing to treat or transferring care to a consultant or specialist has benefits and drawbacks. Understanding the use of pain contracts /partner agreements and frequent intervals of visits will improve outcomes. Chronic low back pain and fibromyalgia share two clinical features. The visits are not quick The visits are not easy. Implementing a consistent algorithm that incorporates current recommendations in today’s busy clinic will yield improved results in patient care. Chronic pain must to be addressed in a multi directive model. A clear, practical chart checklist will keep treatment plan on course. Pain response Labor Stubbing toe on chair leg Burning shoulder pain from too much time on computer Jot down 5 honest reactions to seeing back painrecurrent, fibromyalgia follow up on your schedule. Time consuming Frustrated Angry Nervous Agitated Scared Skeptical Excited for the challenge. Ready to try a multiple facet approach to treatment. Armed with excellent resources. Frustrated Angry Nervous Agitated Scared Skeptical Excited for the challenge Ready to try a multiple approach to treatment Armed with excellent resources Does you patient have chronic pain? Has a complete workup been done in the past? Labs, diagnostics Has your patient been screened for mental health problems? Does your patient have a diagnosis of mental health problems? Is it the correct diagnosis? Is the patient adequately treated for mental health (pharmacologic agents, talk therapy, support groups, behavior modification) Do you believe you can have an honest patient provider relationship? Does your patient have the ability to go to a chiropractor, PT, massage therapist, acupuncturist, etc? Is your patient already on routine opiods? Is your patient willing to partner to reduce/eliminate ineffective opiods? Do you have time and interest in treating? Do you have knowledge to treat? Can you prescribe narcotics? What classes of narcotics? Long acting narcotics, including Methodone? Do you have knowledge regarding medical marijuana? Do you understand parameters for prescribing opioids? Do you have relationships with local pharmacists? Do you have the ability to drug screen your patient? Does your state have medical marijuana? Does your state have a narcotic prescription reporting mechanism? Taking a Pain History • Location • Radiation • Onset: sudden or insidious • Duration • Frequency: continuous or intermittent • Description • Intensity • Alleviating factors • Exacerbating factors Neck Shoulder Total body Lumbar Knee Anti inflamatory Elavil/Pamelor Neurontin Lyrica Antidepressent SSRI SNRI Mood stabilizer Anxiolytic Opiod Tramadol Sleep agent SUBOXONE, METHADONE Was it complete? Exam findings X-ray MRI Consult notes Orthopedic Pain management Neurosurgeon Injection therapy Psychologist Dates Goals Patient’s adherence to sessions and to home exercises Trial of TENS Tobacco smoker Drug dependence Alcoholic Partner agreement Pain contract signed Treatment Options: A Guide for People Living with Pain Dedicated to eliminating the under treatment of pain in America. www.painknowledge.org/opioidtoolkit/docs/Tr eatment%20Options.pdf The following organizations are represented by those who helped create this publication: American Academy of Pain Management American Academy of Pain Medicine American Alliance of Cancer Pain Initiatives American Board of Hospice and Palliative Medicine American Holistic Nursing Association American Pain Society American Society for Pain Management Nursing American Society of Regional Anesthesiologists Association of Oncology Social Work Healing Touch International Intercultural Cancer Council International Association for the Study of Pain Midwest Nursing Research Society National Association of Social Workers Oncology Nursing Society HELPFUL HINTS ON YOUR ROAD TO PAIN RELIEF Keep the following tips in mind as you seek treatment for your pain: • Chronic pain can result in physical and psychological challenges. It is important to accept support from loved ones—you need and deserve all the help you can get. • Be sure to seek treatment as early as possible to avoid further problems. • Do not allow your physical illness or pain to take over your life. Pain is a part of you, but it should not define who you are. • Try not to let past frustrations of failed treatments stand in your way; there are a wide range of treatments available as detailed in this guide. While your pain might not go away completely, there are ways to reduce it so that it is bearable and you can reclaim parts of your life. HELPFUL HINTS ON YOUR ROAD TO PAIN RELIEF Keep the following tips in mind as you seek treatment for your pain: • Chronic pain can result in physical and psychological challenges. It is important to accept support from loved ones— you need and deserve all the help you can get. • Be sure to seek treatment as early as possible to avoid further problems. • Do not allow your physical illness or pain to take over your life. Pain is a part of you, but it should not define who you are. • Try not to let past frustrations of failed treatments stand in your way; there are a wide range of treatments available as detailed in this guide. While your pain might not go away completely, there are ways to reduce it so that it is bearable and you can reclaim parts of your life. COMMON FEATURES OF AN OPIOID AGREEMENT •Sign an opioid agreement to be kept in your medical file (ask for your own copy) •Obtain prescriptions from only one doctor •Have your prescriptions filled at one pharmacy •Come in for regular office visits (every 2-4 weeks or so) •Agree to have periodic urine drug screening •Bring your pills in to be counted during visits • Follow any additional rules not listed above http://www.painknowledge.org/opioidtoolkit/docs/Treatment%20Options.pdf Tobacco smoker Drug dependence Alcoholic In process Resolved Concern for metal illness Past history of mental illness Family history of mental illness Bipolar depression Yes/No Treated satisfactorily Yes/No Depression Yes/No Treated satisfactorily Yes/No In process Resolved Mental health Addictive disorder Chronic pain NOT! Depression screen Becks inventory PHQ-9 Bipolar screen – Mood disorder questionnaire (MDQ) http://www.fehb.org/CSE/CCSEConference201 2/BeckDepressionInventory.pdf http://www.nhlbi.nih.gov/meetings/workshops/ depression/instruments.htm http://www.ncbi.nlm.nih.gov/pmc/articles/PMC 1495268/ www.ncbi.nlm.nih.gov/pubmed/12505821 The rate of lumbar spine magnetic resonance imaging in the USis growing at an alarming rate. Evidence that it is not accompanied by improved patient outcomes. Overutilization correlates with, and likely contributes to, a 2- to 3-fold increase in surgical rates over the last 10 years. Knowledge of imaging abnormalities can actually decrease self-perception of health and may lead to fearavoidance and catastrophizing behaviors that may predispose people to chronicity. LEVEL OF EVIDENCE: Diagnosis/prognosis/therapy, level 5. Flynn TW, Smith B, Chou R. Appropriate use of diagnostic imaging in low back pain: a reminder that unnecessary imaging may do as much harm as good. J Orthop Sports Phys Ther. 2011 Nov;41(11):838-46. Epub 2011 Jun 3. Suspect cauda equina Longer pain than 6-12 weeks Patient is amenable to injection therapy Directed care to PT Pain management 4 legs of treatment w/ psychologist Borrie, RA. (2001). Thinking About Pain Psychologically based pain management can provide relief for pain patients. http://www.practicalpainmanagement.com/treatmen ts/psychological/thinking-about-pain NSAIDs, acetaminophen, skeletal muscle relaxants (for acute low back pain), and tricyclic antidepressants (for chronic low back pain) are effective for pain relief. Opioids, tramadol, benzodiazepines, and gabapentin (for radiculopathy) are effective for pain relief. Systemic corticosteroids are ineffective . Adverse events, such as sedation, varied by medication, although reliable data on serious and long-term harms are sparse. Most trials were short term (< or =4 weeks). Few data address efficacy of dual-medication therapy compared with monotherapy, or beneficial effects on functional outcomes. Chou R, Huffman LH; American Pain Society; American College of Physicians. (2007). Medications for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007 Oct 2;147(7):505-14. Osteoarthritis (AC R 2000) • Self-management programs • Weight loss • Aerobic exercise • Range-of-motion exercises • Muscle-strengthening exercises • Assistive devices • Occupational/physical therapy • Joint protection/energy conservation Low Back Pain (Chou 2007) Acupressure/acupuncture • Functional restoration • Interdisciplinary rehabilitation • Interferential therapy • Massage • Transcutaneous/percutaneous electrical nerve stimulation • Spinal manipulation Chemonucleolysis is moderately superior to placebo injection but inferior to surgery. (good) Epidural steroid injection is moderately effective for short-term (but not long-term) symptom relief. (fair) Spinal cord stimulation is moderately effective for failed back surgery syndrome with persistent radiculopathy, though devicerelated complications are common. (fair) Prolotherapy, facet joint injection, intradiscal steroid injection, and percutaneous intradiscal radiofrequency thermocoagulation are not effective. (good) Insufficient evidence exists to reliably evaluate other interventional therapies. Chou R, Atlas SJ, Stanos SP, Rosenquist RW.Nonsurgical interventional therapies for low back pain: a review of the evidence for an American Pain Society clinical practice guideline. Spine (Phila Pa 1976). 2009 May 1;34(10):1078-93 Case studies used to treat chronic pain, including salicylates, acetaminophen, nonsteroidal anti-inflammatory drugs, tricyclic antidepressants, anticonvulsants, N-Methyl-D-Aspartate receptor antagonists, lidocaine, skeletal muscle relaxants, and topical analgesics. http://www.ncbi.nlm.nih.gov/pubmed/14567202 Gordon, DB, (2003). Nonopioid and adjuvant analgesics in chronic pain management: strategies for effective use. HYPERLINK North Am. 2003 Sep;38(3):447-64,vi. http://www.ncbi.nlm.nih.gov/pubmed/21176430 Mease, PJ. (2009). Further strategies for treating fibromyalgia: the role of serotonin and norepinephrine reuptake inhibitors. Am J Med. Dec;122(12 Suppl):S44-55 11/18 painful tender points Multimodal pharmacological treatment also combined with nonpharmacological therapy. Only three drugs (duloxetine, milnacipram, pregabalin) are approved by the American Food and Drug Administration (FDA) and none by the European Medicines Agency (EMEA Most of the drugs improve only one or two symptoms; no drug capable of overall symptom control is yet available. Tricyclic antidepressants (TCAs), selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), opioids, non-steroidal anti-inflammatory drugs (NSAIDs), growth hormone, corticosteroids and sedative hypnotics. As no single drug fully manages FM symptoms, multicomponent therapy should be used from the beginning. Gradually increasing low doses is suggested in order to maximize efficacy. The best treatment should be individualized and combined with patient education and non-pharmacological therapy. http://www.omniaeducation.com/emails/2012i mages/echo_pain/ECHO_Pain_web.pdf?utm _source=Omnia+Education&utm_campaign= 43b013690cPain_Echo1_4_2012&utm_medium=email CME Borrie, RA. (2001). Thinking About Pain Psychologically based pain management can provide relief for pain patients. http://www.practicalpainmanagement.com/treatments/psychological/thinkingabout-pain Chou R, Qaseem A, Snow V, et al; for the Clinical Efficacy Assessment Subcommittee of the American College of Physicians and the American College of Physicians/American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491. Chou R, Fanciullo GJ, Fine PG, et al; for the American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113-130. Chou R, Atlas SJ, Stanos SP, Rosenquist RW.Nonsurgical interventional therapies for low back pain: a review of the evidence for an American Pain Society clinical practice guideline. Spine (Phila Pa 1976). 2009 May 1;34(10):1078-93 Flynn TW, Smith B, Chou R. Appropriate use of diagnostic imaging in low back pain: a reminder that unnecessary imaging may do as much harm as good. J Orthop Sports Phys Ther. 2011 Nov;41(11):838-46. Epub 2011 Jun 3. Franco M, Iannuccelli C, Atzeni F, Cazzola M, Salaffi F, Valesini G, Sarzi-Puttini P. Pharmacological treatment of fibromyalgia. Clin Exp Rheumatol. 2010 Nov-Dec;28(6 Suppl 63):S110-6. Epub 2010. Each king in a deck of playing cards represents a great king from history. Hearts - Charlemagne Diamonds - Julius Caesar. Clubs - Alexander the Great Spades= King David