PowerPoint_Chapter15 - EMC Paradigm Internet Resource
advertisement

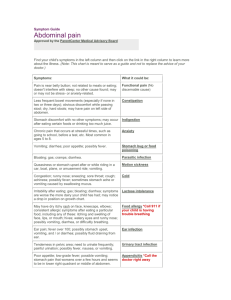
Chapter 15 The Gastrointestinal System and Drug Therapy © Paradigm Publishing, Inc. 2 Chapter 15 Topics • • • • • • • • Anatomy and Physiology of the GI System Diarrhea Constipation Heartburn and Ulcers Nausea and Vomiting Hemorrhoids Other GI Conditions Herbal and Alternative Therapies © Paradigm Publishing, Inc. 3 Anatomy and Physiology of the GI System GI Tract • GI tract has two systems: the upper GI system (the mouth, esophagus, and stomach) and the lower GI system (the intestines, colon, and rectum) • Some organs in the GI system play a major role in the pharmacokinetic process. © Paradigm Publishing, Inc. 4 Anatomy and Physiology of the GI System About the GI System • The GI system processes food and liquids in two ways Digestion: the breakdown of large food molecules to smaller ones Absorption: uptake of essential nutrients into the bloodstream © Paradigm Publishing, Inc. 5 Anatomy and Physiology of the GI System Process of Digestion • Food moves down the esophagus to the stomach • In the stomach Ingested food triggers the release of gastrin (hormone) Stimulates histamine release which increases the number of active proton pumps Stimulates acid production from proton pumps Acid and enzyme secretions digest large particles • Acidic stomach environment (pH: 1 to 2) helps digest food, kills ingested bacteria, and is critical for absorption of certain drugs © Paradigm Publishing, Inc. 6 Anatomy and Physiology of the GI System Process of Absorption • From stomach, food particles enter small intestine, where Most digestion and nutrient absorption takes place due to large surface area Most oral drugs are absorbed systemically • Remaining food particles move to large intestine, where Useful substances such as salt and water are absorbed Nonabsorbable substances (fiber, bacteria) are eliminated as waste (stool) through the rectum and anus © Paradigm Publishing, Inc. 7 Anatomy and Physiology of the GI System Movement of Ingested Food • Peristalsis (process of coordinated muscle contraction) moves food particles through the GI tract In intestines, process called GI motility • Sphincters regulate the speed at which the food particles move through the tract These muscle rings prevent digested substances from moving in the wrong direction • The closing of the lower esophageal sphincter, located between the esophagus and stomach, keeps stomach acid from traveling up the esophagus © Paradigm Publishing, Inc. 8 Anatomy and Physiology of the GI System Other Components of the GI System • Other organs of the GI system include the salivary glands, gallbladder, pancreas, and liver • These organs release secretions that aid in digestion of food and absorption of nutrients The salivary glands produce saliva that helps digest sugars in food and allows for easier swallowing The gallbladder stores bile, a fluid produced by the liver that aids the absorption of fat and cholesterol from the small intestine © Paradigm Publishing, Inc. 9 Anatomy and Physiology of the GI System Pancreas • Pancreatic secretions aid in the digestion of carbohydrates, proteins, and fats and neutralize stomach acid © Paradigm Publishing, Inc. 10 Anatomy and Physiology of the GI System Liver • The liver is the major organ for metabolism of harmful substances and orally administered drugs • Because blood flow from the GI system goes through the liver before entering the body’s circulation, many drugs undergo the first-pass effect First-pass effect: the metabolism of drugs by the liver before they reach their target in the body Result of first-pass effect: full drug dose does not reach the body © Paradigm Publishing, Inc. 11 Anatomy and Physiology of the GI System Liver Function and First-Pass Effect • Alternatives to oral administration are necessary for drugs that will lose their efficacy if they undergo the firstpass effect © Paradigm Publishing, Inc. 12 Diarrhea About Diarrhea • Diarrhea is excessive, soft, or watery stools Excessive can mean large stool volume or more bowel movements than normal (due to increased GI motility) • Two types of diarrhea: acute and chronic Acute diarrhea is common; caused by infections, food poisoning, drugs (see Table 15.1) Infectious causes: bacterial (E. coli, salmonella); protozoal (giardia); viral (Norwalk, rotavirus) Chronic diarrhea is less common; causes are IBS, ulcerative colitis, or Crohn’s disease © Paradigm Publishing, Inc. 13 Diarrhea Drugs for Diarrhea • Antidiarrheal medications treat symptoms; slow transit of food through the GI tract or decrease secretions into it This reduces stool volume and makes stool less watery • Diarrhea is a symptom of a disease, not a disease itself Medications reduce symptoms but do not treat the underlying disease • Antibiotics are used for diarrhea caused by bacterial infection; fluid or electrolyte replacement may be needed © Paradigm Publishing, Inc. 14 Diarrhea Drugs for Diarrhea: Opiate Derivatives • Indication: short-term relief of acute diarrhea • Mechanism of Action: inhibit peristalsis; reduce liquid content of stool • Route: all are oral • Side Effects (common): dizziness, drowsiness • Side Effects (atropine): blurred vision, dry mouth, difficulty urinating • Cautions: diphenoxylate is scheduled (C-V); requires special storage and handling • Caution: seldom used for children under age 2 © Paradigm Publishing, Inc. 15 Diarrhea Drugs for Diarrhea: Bismuth Subsalicylate • • • • • Indications: acute diarrhea, traveler’s diarrhea Indication (other): H. pylori infection Mechanism of Action: makes stools less watery Route: oral; available OTC Side Effects (common): constipation, nausea, vomiting, darkening of tongue and/or stools (temporary, harmless) • Side Effects (severe, rare): tinnitus, confusion, weakness • Cautions: should not be used in patients with aspirin hypersensitivity; typically not given to children/teens • Caution: should not be taken with tetracycline antibiotics © Paradigm Publishing, Inc. 16 Constipation About Constipation • Constipation is characterized by infrequent bowel movements, small stool size, hard stools, or the feeling of incomplete bowel evacuation • Causes of constipation include Diet low in fiber or fluid intake Certain foods or drugs, particularly pain medicines such as opiates and antacids • Dietary and lifestyle changes with drug therapy help Drink plenty of fluids, eat adequate fiber, and exercise regularly © Paradigm Publishing, Inc. 17 Constipation Drugs for Constipation • Indication (laxatives): only as needed short-term Electrolyte abnormalities can occur if taken often • Routes: all are oral; some rectal (suppositories or enemas) • Rectal suppositories or enemas are used for rapid treatment of moderate to severe constipation and in hospitalized patients unable to swallow Rectal suppositories are inserted into rectum; take 15-60 minutes to work Enemas are solutions delivered directly into rectum © Paradigm Publishing, Inc. 18 Constipation Suppository Insertion • Patient should remove the foil wrapping of the suppository and insert the pointed end into the rectum. • Insertion should be far enough into the rectum to avoid release © Paradigm Publishing, Inc. 19 Constipation Drugs for Constipation: Enemas • Enemas are solutions that are delivered into rectum • Indications: rapidly clear out the bowels prior to surgery or diagnostic procedures, such as colonoscopy; remove excessive fecal matter blocking the GI tract • Patient should insert enema tip into the rectum, squeeze the bottle or allow liquid to drain via gravity, hold liquid in rectum 2 to 60 minutes, then defecate © Paradigm Publishing, Inc. 20 Constipation Drugs for Constipation: Bulk-Forming Laxatives • Indications: mild constipation; constipation prevention Use daily for regular bowel movements • Mechanism of Action: draw water and other electrolytes into GI system; facilitate bowel movements; absorb fat and reduce glucose (beneficial for patients with diabetes or high cholesterol) • Side Effects (rare): obstruction of the esophagus or bowels • Caution: avoid in patients with intestinal stenosis • Caution: can affect drug absorption; separate doses from other medications by at least 2 hours © Paradigm Publishing, Inc. 21 Constipation Drugs for Constipation: Stool Softeners • Indication: for patients at risk of becoming constipated • Mechanism of Action: increase water and electrolyte secretions in GI tract; make stools softer, easier to pass • Routes: all are oral; some are also rectal • Side Effects: throat irritation, abdominal pain, diarrhea, intestinal obstruction • Caution: Excessive or long-term use may lead to electrolyte imbalance © Paradigm Publishing, Inc. 22 Constipation Drugs for Constipation: Stimulant Laxatives • Indications: acute constipation, use only as needed shortterm; often used to treat opiate-induced constipation • Mechanism of Action: stimulate parasympathetic neurons that control bowel muscles, enhancing peristalsis and GI motility • Side Effects (common): mild abdominal pain, nausea, vomiting, rectal burning • Caution: do not take with dairy products and antacids • Caution (senna): contraindicated in patients with intestinal obstruction, Crohn’s disease, abdominal pain, pregnancy © Paradigm Publishing, Inc. 23 Constipation Drugs for Constipation: Bowel Prep Laxatives • Indications: evacuation of bowels before surgery or diagnostic procedure; clearing poisons or parasitic worms from GI tract; treatment of bowel impaction • Mechanism of Action: draw water and electrolytes into the GI tract; completely clean out GI tract • Routes: oral and rectal; some available only by prescription • Side Effects (common): abdominal pain, diarrhea, electrolyte loss or imbalance • Cautions: occasional use only; use with caution in patients with kidney problems and children under age 2 © Paradigm Publishing, Inc. 24 Constipation Drugs for Constipation: Miscellaneous Laxatives • Milk of magnesia Indication: mild constipation; common OTC product Route: oral; liquid and chewable tablet forms • Glycerin suppositories Indication: occasional constipation in children • Lactulose Indication: ammonia toxicity and delirium in patients with end-stage liver failure Route: oral; solution form © Paradigm Publishing, Inc. 25 Your Turn Question 1: What are two restrictions for using bismuth subsalicylate? Answer: This medication should not be taken if a patient has aspirin hypersensitivity or is taking tetracycline antibiotics. Question 2: What is the purpose of using enemas? Answer: They are used to rapidly clear out the bowels prior to surgery or diagnostic procedures. © Paradigm Publishing, Inc. 26 Heartburn and Ulcers GERD (Heartburn) • Common complaint; estimated that 10% of people in the United States get heartburn every week • Characterized by a burning or sensation of warmth starting in the gut or chest that may radiate to the neck • In GERD, the lower esophageal sphincter is faulty, allowing acidic stomach contents to move up into the esophagus Acid reflux causes permanent changes in esophageal lining; linked to narrowing and cancer of the esophagus Long-term treatment reduces acidity of the stomach © Paradigm Publishing, Inc. 27 Heartburn and Ulcers Foods and Medications that May Worsen GERD Foods Chocolate Coffee or soda Fatty foods Garlic Onions Orange juice Mint Spicy foods Medications Alcohol Alendronate Anticholinergics Aspirin Barbiturates Caffeine Dopamine © Paradigm Publishing, Inc. Iron Nicotine (from smoking) Nitrates NSAIDs Tetracycline 28 Heartburn and Ulcers Ulcers • Sores or patches of dead tissue along the walls of the GI tract • They occur when the protective lining of the GI tract is worn away and bleeding occurs • The most common cause of ulcers (PUD) is H. pylori, a bacterial parasite that attaches to lining of the stomach Releases toxic chemicals that damage the lining Causes damage to cells in stomach and small intestine • Duodenal ulcers occur in the small intestine just below the stomach; caused by hyperacidity © Paradigm Publishing, Inc. 29 Heartburn and Ulcers Ulcers (continued) • Stress ulcers occur in critically ill patients who are bedridden; mechanism is unknown • Prolonged use of NSAIDs and aspirin can cause ulcers; these acidic drugs irritate and erode GI tissue They also inhibit production of prostaglandins that protect the lining of the stomach from acid secretions When ulceration erodes into a blood vessel, a GI bleed can occur • Long-term NSAID, aspirin, or anticoagulation therapy leads to high risk for ulcers and life-threatening bleeding © Paradigm Publishing, Inc. 30 Heartburn and Ulcers Drugs for GERD and PUD • Most treatments do not directly fix GERD or GI ulcers • Antacids, PPIs, and H2 blockers relieve symptoms of GERD by decreasing acid production in the stomach Drugs for GERD and PUD: Antacids • Indication (short-term): mild to moderate GERD • Mechanism of Action: contain special ions that react with hydrogen ions in the stomach and neutralize acid • Side Effects (common): constipation, diarrhea, stomach pain, nausea, vomiting • Caution: do not take at the same time with antibiotics © Paradigm Publishing, Inc. 31 Heartburn and Ulcers Drugs for GERD and PUD: PPIs • Indications: GERD, PUD, and H. pylori infection • Mechanism of Action: bind to proton pumps in stomach lining, inactivating them; work 24 hours • Routes: all are oral (liquid for infants); some are also IV (for critically ill patients and those at risk for stress ulcers) All prescription; lansoprazole and omeprazole also OTC • Side Effects (rare): headache, nausea, vomiting, diarrhea • Cautions: do not crush or chew delayed-release capsules or tablets ; do not take with digoxin or ketoconazole © Paradigm Publishing, Inc. 32 Heartburn and Ulcers Drugs for GERD and PUD: H2 Blockers • Indications: GERD, PUD • Mechanism of Action: block type 2 histamine receptors in the stomach by decreasing proton pump activity • Routes: all oral; most also IV (critically ill in the hospital) All OTC; work for 8 hours; take as needed • Side Effects (common): headache, diarrhea, and dizziness • Cautions: do not take with digoxin or ketoconazole • Caution (cimetidine): several drug interactions; patient should talk with pharmacist before taking • Caution (ranitidine): avoid in patients with hepatitis © Paradigm Publishing, Inc. 33 Heartburn and Ulcers Drugs for GERD and PUD: Sucralfate • Indications: in products for infants with GERD • Mechanism of Action: coats stomach and small intestine walls, forming a protective barrier against stomach acid • Take on an empty stomach • Cautions: interacts with many drugs Drugs for GERD and PUD: Regimens for H. Pylori • All multidrug regimens consist of a PPI or an H2 blocker to heal the ulcer and antibiotics to kill the bacteria in the GI tract • Combination products also available © Paradigm Publishing, Inc. 34 Nausea and Vomiting About Nausea and Vomiting • Nausea and vomiting are related symptoms caused by various diseases and conditions Morning sickness: occurs in early pregnancy; caused by hormonal changes Motion sickness: follows movement; affects balance • Nausea is the feeling of the need to vomit • Vomiting (also called emesis) is the expulsion of stomach contents out of the mouth; involves reverse peristalsis Defense mechanism to protect the body from harmful substances that have been consumed © Paradigm Publishing, Inc. 35 Nausea and Vomiting About Nausea and Vomiting • All drugs are foreign substances to the body and may trigger nausea and vomiting, including Antibiotics Antiseizure medications Chemotherapy agents Digoxin Opiates Theophylline • Radiation treatments can also cause nausea and vomiting © Paradigm Publishing, Inc. 36 Nausea and Vomiting The CTZ • Blocking receptors for serotonin, dopamine, histamine, and substance P in the CTZ can relieve symptoms of nausea and vomiting © Paradigm Publishing, Inc. 37 Nausea and Vomiting Drugs for Nausea and Vomiting: Anticholinergic Antiemetics • Indication: mild motion sickness • Mechanism of Action: block histamine and acetylcholine (neurotransmitters in the CTZ and vomiting center) • Routes: all are oral; some are also IM; dimenhydrinate is available in an IV form; scopolamine is also transdermal • Side Effects: urinary retention, drowsiness • Cautions: do not take with alcohol or MAOIs; avoid in patients with prostate enlargement or glaucoma; do not give to infants or breast-feeding mothers © Paradigm Publishing, Inc. 38 Nausea and Vomiting Drugs for Nausea and Vomiting: General Antiemetics • • • • Used in inpatient settings; mechanism of action varies Routes: all are oral, IM, and IV; some are also rectal Side Effects (all, common): drowsiness and sedation Side Effects (phenothiazines): EPS side effects (tardive dyskinesia and dystonia) Elderly patients must be closely monitored for EPS • Cautions: sedative effects make driving difficult; do not take with alcohol © Paradigm Publishing, Inc. 39 Nausea and Vomiting Drugs for Nausea and Vomiting: Serotonin Type 3 (5-HT3) Receptor Antagonists • Indication: prevention and treatment of severe nausea and vomiting from chemotherapy, radiation, or anesthesia Potent prescription-only antiemetics • Mechanism of Action: block serotonin type 3 (5-HT3) receptors in the brain and GI tract • Route: all oral and IV; some IM and transdermal patch • Side Effects (common): headache, fatigue, constipation, drowsiness, muscle weakness, dizziness • Caution: sedative effects make driving difficult © Paradigm Publishing, Inc. 40 Nausea and Vomiting Drugs for Nausea and Vomiting: Neurokinin 1 Inhibitor • Indication: Prevention of nausea and vomiting induced by chemotherapy drugs or anesthesia • Mechanism of Action: blocks NK1 receptors, preventing substance P from stimulating nausea • Route: oral; only available by prescription Aprepitant (Emend) is only one on market • Side Effects: fatigue, muscle weakness, constipation • Side Effects (rare, significant): hypotension, kidney and liver dysfunction, slow heart rate, diarrhea, blood changes © Paradigm Publishing, Inc. 41 Your Turn Question 1: How can you tell if a patient is taking medications to treat a peptic ulcer caused by H. pylori? Answer: The patient would be taking a multidrug regimen that consists of a PPI or an H2 blocker to heal the ulcer and antibiotics to destroy the bacteria. The patient may also be taking an antacid. Question 2: A patient has nausea and vomiting during airplane rides. At the pharmacy, he asks if a medicine can stop this from happening. What drug therapy is likely recommended? Answer: OTC anticholinergic agents can be used to treat mild nausea and vomiting for a patient who has motion sickness. © Paradigm Publishing, Inc. 42 Hemorrhoids About Hemorrhoids • Hemorrhoids are blood vessels from the hemorrhoidal cushion (the area surrounding the anal sphincter) that are forced into the anal cavity in response to straining during defecation or passing hard stools Similar to varicose veins, except they occur in the blood vessels near the anus rather than in the legs • Hemorrhoid disease is bleeding and irritation when a blood vessel of the hemorrhoidal cushion ruptures © Paradigm Publishing, Inc. 43 Hemorrhoids Drugs for Hemorrhoids • Medications for hemorrhoids decrease symptoms but do not reduce bleeding or cure the underlying problem • Treatment of mild hemorrhoids Increase water and fiber intake Use topical hemorrhoid agents for itching and pain; witch hazel (an astringent) may help stop bleeding Use pramoxine, a local anesthetic, to treat discomfort • Treatment of moderate to severe hemorrhoids May require topical corticosteroids such as ProctoFoam or surgery © Paradigm Publishing, Inc. 44 Other GI Conditions Irritable Bowel Syndrome (IBS) • Chronic disease with frequent and painful constipation or diarrhea; drug therapy is limited, restricted distribution Ulcerative Colitis and Crohn’s Disease • Both are excessive inflammation of the GI tract, causing chronic diarrhea Drug therapy includes immunosuppressants, salicylates, and anti-inflammatory drugs • Ulcerative colitis can be cured by removing affected portion of colon or large intestine • Crohn’s is an autoimmune disease; cannot be cured © Paradigm Publishing, Inc. 45 Herbal and Alternative Therapies • Ginger is used to reduce nausea associated with surgery, vertigo, and motion sickness • Probiotics are products that contain live cultures of yeast or bacteria Used for diarrhea, constipation, H. pylori infection, antibiotic-induced diarrhea • Lactobacilli are gram-positive bacteria that are normal flora of the human GI tract • S. boulardii is a yeast organism in the human GI tract; used for prevention of diarrhea • Bifidobacteria agents may be effective for diarrhea © Paradigm Publishing, Inc. 46 Summary • • • • • • • • • OTC medicines are used to treat diarrhea Laxatives are used to treat constipation Topical agents are used to treat hemorrhoids PPIs and H2 blockers are used to treat GERD and PUD Antibiotics are also used for PUD caused by H. pylori Antacids are used for GERD to relieve heartburn from food Anticholinergic antiemetics treat mild nausea/vomiting General antiemetics treat nausea in inpatient settings 5-HT3 antagonists (antiemetics) are used for chemotherapy © Paradigm Publishing, Inc. 47