Marfan's Syndrome
advertisement

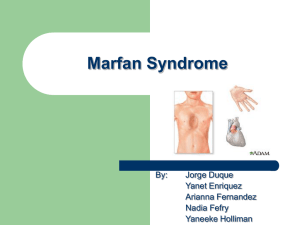
Welcome, Applicants! Marfan Syndrome and related disorders SARA FABER, MP3 MORNING REPORT 1/8/10 Overview Epidemiology Genetics/Pathophysiology Diagnosis/Clinical Features Management Differential Diagnosis Epidemiology First described in 1896; named in 1902. Common inherited connective tissue disorder Incidence: 1 in 3000-5000; approximately 200,000 Americans affected M = F; men with shorter life expectancy Races affected equally Genetics Autosomal dominant; variable expression ~25% spontaneous mutations Genes involved in Marfan Syndrome phenotype: Fibrillin-1 (MFS) Microfibril glycoprotein in both elastic and non elastic tissues > 97 different mutations TGFBR (MFS type II or Loeys-Dietz) Works through apoptosis and cell cycle regulation; prevents proper incorporation of fibrillin into tissue Also with triad: hypertelorism, bifid uvula or cleft palate, generalized arterial tortuosity Other gene mutations may lead to similar phenotypes Abraham Lincoln Diagnosis Clinical diagnosis: the Ghent criteria physical exam: 6 organ systems involved family history genetic testing If (+) family history, additionally you need: Involvement of 2 organ systems including 1 major criterion If (–) family history, additionally you need: Major criterion from 2 systems and involvement of a 3rd system Clinical Features HEENT: Eye: superior lens dislocation (ectopia lentis) Oropharynx: high palate and crowded dentition Cardiac: Mitral valve prolapse Aortic root dilation Pulmonary: Spontaneous pneumothorax Neurologic: Dural ectasia Skin: Stretch marks Clinical Features Musculoskeletal: Tall stature (dolichostenomelia) Long digits (arachnodactyly) Thumb sign (distal phalanx protrudes beyond border of clenched fist) Wrist sign (thumb and fifth digit overlap when around the wrist) Sternal deformity (prominent pectus) Scoliosis > 20 degrees Joint hypermobility Arm span exceeding height (ratio >1.05) Reduced elbow extension (<170 degrees) Medial displacement of medial malleolus Jonathan Larson, playwright/composer Cardiovascular Complications Most common cause of M&M (~80%) Aortic root disease aneurysms, AR, dissection In 50% children In up to 80% of adults May lead to neurovascular complications AR murmur: decrescendo, diastolic Mitral valve prolapse (minor criterion) In 60-80% patients; most common valve disorder Worsens with time, complicated by rupture MVP murmur: ejection click, holosystolic Arrhythmias MKSAP Question A 22-year-old man is evaluated as part of a routine examination...He is 171.5 cm (78 in) tall and weighs 72.8 kg (185 lb) with pectus excavatum. Blood pressure is 134/65 mm Hg bilaterally, and pulse rate is 76/min and regular. He has a high arched palate. There is a 2/6 decrescendo diastolic murmur at the right upper sternal border while in the upright posture. There is moderate scoliosis, joint hypermobility, and the patient's thumb and fifth digit overlap when circling the opposite wrist (“wrist sign”). What’s the most appropriate next step in management? A Chest radiograph B Transthoracic echocardiogram C Aortic magnetic resonance angiogram D Transesophageal echocardiogram Management: screening/counseling Annual echocardiogram Annual ophtho exam and orthopedic involvement as needed Counseling regarding physical activities Genetic counseling Management: medications Beta blockade Standard of care for adult patients (no data on children) Based on studies of propranolol versus placebo Slower rate of aortic dilatation with beta blockade Survival at 10 yrs not significantly improved Calcium channel blockers? ARBs Recent animal study models of FBN1 mutants demonstrated decreased rate of aortic dilatation Mechanism is via TGFBR One randomized trial of 17 patients is complete: larger study is now ongoing Management: surgical intervention • Better survival with elective repair • Variable recommendations for aortic root diameter at which intervention warranted – – – ACC/AHA: diameter > 5.0 cm ESC: diameter > 4.5 cm Rate of increase > 0.5 cm/year • Earlier intervention indicated in women desiring pregnancy • Annual imaging post-op still necessary Similar phenotypes Congenital contractual arachnodactyly: FBN2 MASS (Mitral valve prolapse, aortic dilation, skin and skeletal abnormalities): FBN1 Joint hypermobility syndrome Ehlers-Danlos: mutation of type V collagen Stickler syndrome: mutation of type II and XI collagen Take home points Marfan Syndrome is relatively common If you have a patient < 40 with evidence of aortic root changes, think MFS No cure, so cardiovascular management is key Annual echo Beta blockade Counseling on physical activity References Lacina, S. What’s new in outpatient cardiology. Curr Opin in Ped. 2009; 21:605-610. Midla, G. Diagnosis and management of patients with Marfan syndrome. JAAPA 2008; 21(2): 21-25. Attias, D, et al. Comparison of Clinical Presentations and Outcomes Between Patients with TGFBR2 and FBN1 Mutations in Marfan Syndrome and Related Disorders. Circulation 2009; 120: 2541-2549. Loeys, B, et al. Aneurysm Syndromes Caused by Mutations in the TGF-B Receptor. NEJM 2006;355:788-798.