The Dying Person
advertisement

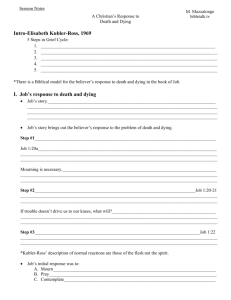
CHAPTER 41 THE DYING PERSON INTRODUCTION † Some deaths are sudden, others expected † Accepting one’s own mortality is a developmental stage of life † Your feelings about death affect the care you give † Must understand the dying process to meet dying person’s physical, psychological, social, & spiritual needs TERMINAL ILLNESS † Illness or injury for which no reasonable expectation of recovery exists † Doctors can’t predict time of death † Hope and the will to live strongly influence living and dying ATTITUDES ABOUT DEATH † Experiences, culture, religion, and age influence attitudes † Attitudes change as age & circumstances change † Dying people often need hospital, nursing center, hospice, or home care † Family often involved in process ATTITUDES ABOUT DEATH † When death occurs funeral director called to take body † Many adults & children have never had contact with dying person or at time of death † Practices & attitudes differ among cultures † Attitudes influenced greatly by religion RELIGION’S AFFECT ON DYING † Beliefs about life after death influence attitude toward death (ex: reincarnation is belief that spirit or soul is reborn into another human body or into another form of life) † Rites & rituals during dying process or at death influenced by religion † Religion offers comfort to some people as they or loved one are dying AGE’S AFFECT ON DYING † Adults: † Fear pain & suffering, dying alone, invasion of privacy, loneliness, and separation from loved ones † Worry about loved ones left behind † Resent death ability to keep from dreams † Age 3-5 think death is temporary † Blame themselves † See death as punishment for being bad AGE’S AFFECT ON DYING † Age 5-7 † Know death is final † Think death only happens to others † Relate death to punishment & body mutilation (ideas from TV, cartoons, video games, movies, fairy tales) † Older persons † Fewer fears than younger persons, but may fear dying alone † Know it will come, may welcome it (free of pain & suffering) or think of as reunion with loved one STAGES OF DEATH & DYING DESCRIBED BY ELISABETH KUBLER-ROSS Denial: “No, not me!” Anger: “Why me?” May be outraged & jealous of healthy Bargaining: make promises to bargain for more time – may be on spiritual level Depression: mourn things lost & that will be lost Acceptance: calm & at peace NOTE: may not go through stages in order, may go back & forth, may never get to last stage PSYCHOLOGICAL, SOCIAL, AND SPIRITUAL NEEDS Dying person may want: Family & friend’s present To talk about fears & anxieties To be alone Listen and let them express feeling in own way Use touch to show caring (along with silence) May want to see spiritual leader Provide privacy Be courteous to leader Handle spiritual objects with respect PHYSICAL NEEDS Dying may take minutes, hours, weeks: Body processes slow Person is weak LOC change Keep comfortable and maintain dignity Vision blurs: Explain what doing May turn toward light, avoid bright lights Dark room may frighten Eyes may be ½ open with secretions in corners – good eye care essential PHYSICAL NEEDS Hearing one of last functions lost Assume they can hear you – provide reassurance & explanations Speak in normal voice Speech become difficult Anticipate needs Don’t ask questions that require long answers Continue to talk to person PHYSICAL NEEDS Mouth Oral hygiene promotes comfort As death nears & unable to take frequent oral fluids, frequent oral care important (esp. if can’t swallow) Carefully clean nose (crusting) & apply lubricant prn Circulation fails & body temp rises as death nears: Skin cool & mottled Diaphoretic – have increased need for skin care & changing gown/ linens, use light covers PHYSICAL NEEDS • Appetite slowly decreases to point of no intake – Meat, first to avoid, followed by breads/fruits/vegetables; then sweets only then liquids onto sips water only – Assist family to accept this loss of appetite PHYSICAL NEEDS Elimination Incontinence may occur – pericare needed Constipation & urinary retention may necessitate enemas & catheters Comfort and positioning Good alignment & changing positions Analgesics prn May need Semi-Fowlers position to make breathing easier PHYSICAL NEEDS Person’s room should be comfortable & pleasant: Well lit & ventilated Remove unnecessary equipment Keep upsetting equipment out of site Arrange mementos, religious items, flowers, or significant items in view Family members may be present all the time Room may be near nurses’ station FAMILY † Hard time for family – show feelings by being available & courteous † Stay as long as they wish - respect the right to privacy, but don’t ignore care of patient † Family members need support, understanding, courtesy, and respect – go thru same stages as patient † Family may desire spiritual leader also HOSPICE CARE † Focuses on the physical, emotional, social, and spiritual needs of dying † May be part of hospital or nursing center or separate agency – many offer home care † Not concerned with cure or life-saving measures, but comfort & preserving quality of life † Provides follow-up care and support groups for survivors LEGAL ISSUES † Much attention given to right to die † Consent is needed for any treatment. † The Patient Self-Determination Act and OBRA (right to accept or refuse medical treatments) – Advance Directives: † Living wills: document with wishes † Durable power of attorney † “Do not resuscitate” orders written by MD after consulting with patient & family QUALITY OF LIFE † Person has right to die in peace & with dignity † Dying person’s bill of rights (see p. 810) † Right to privacy before & after death – drape & screen † Right to visit with others in privacy – family able to come & go freely, private room if possible † Right to confidentiality (diagnosis & condition) † Free from mistreatment or restraints † Right to safe & home-like setting – protect property, keep odor-free, neat & clean † Right to personal choice – advance directives – staff must respect choices SIGNS OF DEATH † Signs may occur rapidly or slowly: † Movement, muscle tone, sensation lost – mouth may stay open † Peristalsis slows – distention, fecal incontinence or impaction common † Body temperature rises – feels cold, looks pale, & perspires heavily † Circulation fails – pulse fast, weak, irregular & BP falls † Respiratory system fails – Cheyne-Stokes or slow respirations & mucous collects (death rattle) † Pain decreases as loses consciousness † At time of death: no pulse, respirations, or blood pressure & pupils are fixed and dilated † Doctor must pronounce dead (coroner or medical examiner may pronounce or be notified) CARE OF THE BODY AFTER DEATH – POSTMORTEM CARE The right to privacy and the right to be treated with dignity and respect apply after death (close drapes, curtains, doors) Care begins after pronounced dead Goal is to maintain good appearance of body - discoloration & skin damage prevented, handle gently Valuables gathered to give to family Other patients may need support CARE OF THE BODY AFTER DEATH – POSTMORTEM CARE Rigor mortis (rigidity of skeletal muscles) develops 2-4 hours after death Body positioned in normal body alignment before rigor mortis sets in Body should appear in comfortable position for viewing by family Moving body may cause expulsion of air from lungs or intestines, normal sounds produced Standard Precautions CARE OF THE BODY AFTER DEATH – POSTMORTEM CARE Raise bed to comfortable level Place pillow under head & shoulders Close eyelids gently by pulling lashes down Close mouth using rolled washcloth under chin to support closed position prn Follow facility policy for dentures (in mouth or in cup to be sent to mortuary) Remove tubes, replace dressings, inventory valuables CARE OF THE BODY AFTER DEATH – POSTMORTEM CARE Bathe soiled areas & comb hair If family coming to view: Apply clean gown & bed linen Cover body to shoulders Arrange room neatly Provide for privacy Identify & assemble belongings - place in labeled bags for family – document After body is removed, strip unit Follow instructions per charge nurse CARE OF THE BODY AFTER DEATH – POSTMORTEM CARE Observe & report: What was done with belongings Unusual occurrences related to care Unusual responses of family or residents Any other significant observations Remove & discard gloves, wash hands