Press notice for Vaccines and Alternatives paper
advertisement

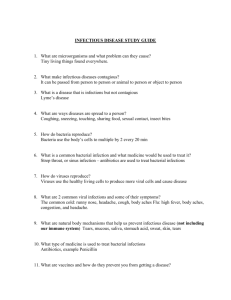
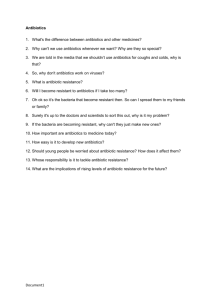
STRICTLY EMBARGOED UNTIL 00:01 GMT, 11 FEBRUARY 2016 PRESS NOTICE 11 February 2016 Jim O’Neill calls for wider use of vaccines and alternative approaches to tackle drug-resistant infections Vaccines and other alternatives can play a vital role in tackling the rise of drug-resistant infections. As existing antibiotics become less effective, because microbes evolve to resist them, we need to use those that we have more responsibly, and ensure that we develop new ones. But even with increased investment, there is no guarantee that we will be able to find enough new antibiotics to tackle this problem in the long-term. Therefore we also need to encourage the development and use of alternative ways to prevent and treat infections. This is the latest in a series of reports by the Review on Antimicrobial Resistance (AMR), before final recommendations are made to the UK Prime Minister in May 2016, setting out a package of actions to tackle drug-resistant infections globally. The report sets out that there are too few vaccines and alternative approaches to antibiotics available for doctors to use to tackle many of our most urgent drug resistance threats. More investment needs to go into developing these products. Vaccines can be useful to combat drug resistance because they reduce the number of infections and avoid antibiotics being used, which is a key driver of drug resistance. But vaccine development takes a long time, often more than 10 years, and is expensive, with the vast majority of potential vaccines failing to reach the market. Of the three “urgent” resistance threats highlighted by the US Centers for Disease Control and Prevention (CDC), we have no vaccines in use for any of them, and too few candidates in clinical trials. These are carbapenemase-producing bacteria (including Klebsiella, E. coli), gonorrhoea and C. difficile. In addition to vaccines and in response to the growing threat of drug-resistant infections, there are many new areas of scientific research emerging that could become alternatives to antibiotics or help reduce our dependence on them by preventing infections. However, for many of the most worrying drug-resistant diseases the current pace of progress and funding offers little to no hope that new products will be available in the next five to ten years. The paper also sets out that we should make more use of products that we already have. There are vaccines available now that could have a massive impact on antibiotic use and resistance, as well as saving many lives if used more widely. For instance, Streptococcus pneumoniae kills over 800,000 children under five years of age worldwide every year. Those deaths would largely be prevented by universal global coverage with a vaccine that is already in use in many parts of the world, the pneumococcal conjugate vaccine. It is estimated that such coverage could also prevent 11.4 million STRICTLY EMBARGOED UNTIL 00:01 GMT, 11 FEBRUARY 2016 days of antibiotic use per year in children younger than five. These children would otherwise be treated for pneumonia and likely given antibiotics. The situation is similar for diarrhoeal disease, also a major cause of child mortality in developing countries and a driver of antibiotic use, both of which could be significantly improved by wider use of the rotavirus vaccine. Vaccines are also a vital way of protecting livestock and fish from infections. The last Review on AMR report showed the extensive use of antibiotics in global agricultural systems and that we need to make better use of vaccines going forward as the pressure increases to optimise antibiotic use. The report suggests three interventions to boost the use of vaccines today and the development of new products. 1. Use existing products more widely in humans and animals. We need to act in the short term to increase the use of existing vaccines and improve the delivery of these in both the community and hospitals for humans, and in agricultural systems for animals. This will involve providing financial support in some cases. For example, in low-income countries where Gavi, UNICEF and others are making great headway towards better vaccine coverage. It is also relevant in some high and middle-income countries, which lack universal coverage for large portions of the population and may be losing out on essential vaccinations. Thinking must also start now to improve the delivery of other alternatives to antibiotics. 2. Renew impetus for early research. We need renewed impetus in the science of vaccines and alternative approaches to make sure researchers in a wide range of fields and countries are funded to look for the solutions that will reduce our dependence on antibiotics and will help tackle drug resistance. To this end, we have previously proposed that a two billion USD five-year global innovation fund should be set up. However, the funding need is large and diverse, and breakthroughs will require long-term, sustained funding from philanthropic organisations, the public sector and companies. 3. Sustain a viable market for needed products. Specific measures must be considered in certain cases where research and development is not at the moment an attractive proposition for prospective vaccine and alternative developers. Depending on the characteristics of the different products, possible interventions include Advance Market Commitments and market entry rewards. These are market interventions that only reward developers for successful products, rather than sharing in the risk of developing a range of products from an earlier stage. Some products are very profitable and may not need much or any public support at all. Others have different market failures, to different degrees, so it is important that the interventions are carefully tailored to each market and product. We have already set out similar proposals that we think can work for the development of new antibiotics and diagnostics, and we will consider the benefits of vaccines for combatting AMR further, alongside the costs of interventions that might be needed, in our final report. To contain the emergence of drug resistance globally, all these interventions will need to be designed to deliver access to the patients who need them, wherever they are and regardless of levels of income. No single country can insulate its citizens from emerging superbugs if they are left to proliferate somewhere else. Another key to global access will lie in more academic teams and companies developing new products where most patients live and at prices they can afford, such as India, China, South Africa, Russia or Brazil. STRICTLY EMBARGOED UNTIL 00:01 GMT, 11 FEBRUARY 2016 Vaccines and alternatives should be a vital part of a broader series of interventions the world needs to make to tackle drug resistance. 2016, will be critical in making this happen. The World Health Assembly, the G7, G20 and UN General Assembly will all be discussing drug resistance. As well as this, industry recently affirmed its commitment with a landmark declaration at Davos, where 85 companies, including vaccine developers, large pharmaceutical companies, diagnostic developers and biotechs, committed to further action to reduce drug resistance, increase research and improve access. This momentum from across the public and private sector landscape means this is a crucial time for the world to make significant progress. The Review will spend the coming months engaging with governments, NGOs and industry globally to discuss and develop these proposals further, with input from an international advisory group, before presenting a final report in the May 2016, covering the whole AMR landscape. Quotes about the report Lord Jim O’Neill, Chairman of the Review on AMR, said: “The problem of drug-resistant infections could be compared to a slow-motion car crash – one that has sadly already begun. 700,000 people are already dying every year from resistant infections, rising to 10 million a year by 2050 without action to hit the brakes now. Antibiotics are important to tackle this threat, but if we can encourage the development and use of vaccines and other alternatives we give the world a better chance of beating drug-resistance.” “Universal coverage with a pneumococcal conjugate vaccine, something that is already used in many parts of the world, could largely prevent the 800,000 yearly deaths of children under five caused by Streptococcus pneumonia. It could also prevent over 11 million days of antibiotic use in these children, reducing the chance of resistance developing.” Dame Sally Davies, Chief Medical Officer for England, said: “Tackling antimicrobial resistance requires a wide range of approaches and developing alternatives to antibiotics, in humans and animals, is critical to the fight. Vaccines have a vital role to play in combatting drug resistance, by preventing infections in the first place. As the latest report from Lord O’Neill makes clear, we need to encourage the development of new products, as well as using existing ones more widely.” Dr Jeremy Farrar, Director of the Wellcome Trust, said: “Drug-resistant infections are a public health emergency that increase the danger of not just one infection, but all infectious diseases for which we have treatments. Our own analysis on how we might use vaccines and other alternatives to tackle this crisis supports the O’Neill team’s report, and suggests they will be an important way we can reduce – but not replace – our need for antibiotics. Vaccines are also critical for controlling epidemics, like Ebola, and endemic diseases such as TB and dengue fever, and how we incentivise developing news ones must take the whole picture into account.” STRICTLY EMBARGOED UNTIL 00:01 GMT, 11 FEBRUARY 2016 Gordon Brown, United Nations Special Envoy for Global Education and former Primer Minister of the United Kingdom, said: “Vaccines have the potential to save millions more lives and tackle the global threat of drug-resistant infections. I have long championed the case for better vaccine access in the emerging world and I am pleased to see this point is at the heart of Jim O’Neill’s carefully researched and very welcome recommendations to combat this problem”. Lelio Marmora, Executive Director, UNITAID, said: “The spread of drug-resistant infections is one of the most alarming developments in global health today. I strongly welcome the AMR Review’s call for the creation of a global innovation fund to stimulate efforts to deal with drug resistance. Vaccines and innovative diagnostics have a fundamental part to play in this effort.” Dr Seth Berkley, CEO of Gavi, the Vaccine Alliance, said: “It is exciting to see such a powerful argument on the important roles vaccines play, not just in preventing diseases and therefore reducing antibiotic usage, but also in directly reducing antimicrobial resistance. New incentives are needed to further accelerate their development.” Florence Séjourné, CEO of Da Volterra and founding member of the BEAM Alliance (Biotech of Europe innovating in Anti-Microbial resistance), said: “We are fully supportive of the recommendations of this new O’Neill Review report, emphasizing the critical need for innovative products that prevent infections as well as limit the rise of antimicrobial resistance: more than one third of products developed by the biotech companies in the BEAM Alliance are alternative approaches which complement antibiotics. This represents a tremendous hope to help shape novel ways to prevent and cure bacterial infections and address the threat of antimicrobial resistance in healthcare. To pursue those brilliant entrepreneurial initiatives, BEAM Alliance especially welcomes much stronger support and recognition by healthcare regulators and payers for such alternative technologies which have clear public health benefits.” Jim Greenwood, President & CEO, Biotechnology Innovation Organization (BIO), said: “To combat AMR, we need a broad infectious disease strategy that leverages not only novel antibiotics and rapid diagnostics, but also vaccines and other innovative biopharmaceutical products. This paper recognizes the value of existing vaccines as well as the tremendous potential of future vaccines and alternative products in preventing and treating infections and, ultimately, stemming the growing tide of resistance. BIO echoes the Review’s conclusion that more must be done to encourage the innovation and uptake of these products. Companies face unique challenges in bringing them to market, requiring tailored interventions rather than a ‘one-size-fits-all’ solution. We applaud the Review’s ongoing work and we look forward to the policy proposals that the Review will put forth in the final report.” STRICTLY EMBARGOED UNTIL 00:01 GMT, 11 FEBRUARY 2016 Notes for Editors 1. AMR or ‘antimicrobial resistance’ is the term used to describe drug-resistant infections, sometimes referred to as ‘superbugs’. Antimicrobials include antibiotics (which act only on bacteria), antivirals, antiparasitics and antifungals. 2. The Report, Vaccines and alternative approaches to reduce our dependence on antimicrobials, will be published on the Review’s website at www.amr-review.org on Thursday 11 February. 3. The UK Prime Minister, David Cameron, commissioned the Review on Antimicrobial Resistance in July of last year to address the growing global problem of drug-resistant infections. It is Chaired by Lord Jim O’Neill and backed by the Wellcome Trust and the UK Government. 4. Lord Jim O’Neill is the current Commercial Secretary to HM Treasury, as well as the Chairman of the Review on AMR. He is an internationally published economist and until 2013 was Chairman of Goldman Sachs Asset Management, having previously been the organisation’s Head of Economic Research. Before chairing the Review on Antimicrobial Resistance, he led the Cities Growth Commission which played a central role in the Government’s decision to devolve significant new powers to large urban centres in the UK starting with Manchester and the Northern Powerhouse project. He is particularly well known for his work in relation to developing and middle-income economies, having coined the BRIC (Brazil, Russia, India, China) acronym – meaning that he is especially well-placed to understand the broad range of international interests raised by antimicrobial resistance. 5. While action to encourage the use and development of vaccines and alternative approaches is crucial to tackling AMR, this represents one part of the solution to the diverse challenges of increasing drug resistance, as outlined in our previous papers and those still to be published in 2016. The Review will be covering health infrastructure in the coming months, before producing its final report in May 2016. 6. The Wellcome Trust is a global charitable foundation that spends more than £700 million a year on advancing human and animal health. It is the second highest-spending charitable foundation in the world, after the Bill & Melinda Gates Foundation, investing principally in biomedical science, the medical humanities and public engagement. The Trust is providing part-funding for the work of the Review, and hosting the team at its London headquarters. 7. The Review will be tweeting about the report via its official account, @ReviewonAMR This press release will also be available on Thursday 11 February at www.amr-review.org. Media enquiries should be addressed to the AMR team on: info@amr-review.org and 020 7611 5722. STRICTLY EMBARGOED UNTIL 00:01 GMT, 11 FEBRUARY 2016 Additional Quotes Jorge Bermudez, Vice-President of Health Production and Innovation, Oswaldo Cruz Foundation, Ministry of Health, Brazil, said: “To address the global problem of drug-resistant infections it is important the we encourage a range of strategies. As Lord O’Neill’s latest report clearly sets out, improving the development of new vaccines, as well as the coverage of existing vaccines, will help to prevent serious infections and reduce antibiotic use. For the world to truly benefit we must make sure that those who need these products most have access to them. Therefore, a clear vision on affordability and ensuring a human rights approach to access and public health are essential”. Bruce Gellin, NVAC Executive Secretary, Deputy Assistant Secretary for Health, US Department of Health and Human Services, said: The turning the tide against antibiotic-resistance requires an all-hand-on-deck approach. One sure way to reduce the inappropriate use of antibiotics is to prevent the diseases that would otherwise be treated by antibiotics. Vaccines have a long history of turning infectious diseases into vaccinepreventable diseases and this report outlines a package of important incentives that can accelerate vaccine development. Dr Manica Balasegaram, Executive Director, MSF Access Campaign, said: "Fully vaccinating children can help contribute to reducing the use of antibiotics, and increasing vaccine coverage in many countries will help improve this. Increasing vaccination coverage will require not only political commitment on the part of countries, but sustainable and affordable vaccine prices. Vaccines need to be affordable if countries are going to vaccinate their children; at the moment, the pneumococcal vaccine, which helps protects against pneumonia and reduce antibiotic use, is too expensive for many countries to adopt, with a middle-income country such as Morocco paying more for the vaccine than France. Research and development that is needs-driven is key, along with policies that ensure the most vulnerable people can access new products affordably; a global R&D fund for medicines, vaccines and diagnostics developed via alternative research incentives will be crucial to achieving this." Timothy Cooke, Chief Executive Officer of NovaDigm Therapeutics and biotechnology industry representative to the US National Vaccine Advisory Committee, said: “This report highlights the critical role that vaccines have played in the fight against antimicrobial resistance by preventing infections and reducing the need for antimicrobial therapy. The current and potential contribution of vaccines to the AMR problem is often underappreciated but this report places vaccines front and center in the discussion. The potential impact of innovative alternative preventative and therapeutic products, mainly being developed by biotechnology companies, is included with an eye toward the future.” Susan Silbermann, President and General Manager, Pfizer Vaccines, said: STRICTLY EMBARGOED UNTIL 00:01 GMT, 11 FEBRUARY 2016 “Pfizer applauds the O’Neill AMR review for raising awareness of the growing problem of antimicrobial resistance. At Pfizer we believe vaccines can play an important role and we are committed to working collaboratively to help ensure broad vaccine access. Market-based incentives to stimulate research and development for all vaccines are a critical part of access to health care.” M. Scott Salka, CEO of AmpliPhi Biosciences, said: “Phage therapy has the potential to not only decrease our dependence on antibiotics but also to spare beneficial bacteria that are crucial to good health. Typical broad-spectrum antibiotics indiscriminately destroy bacteria in a patient, whereas phages specifically target pathogenic bacteria, leaving intact a patient’s healthy microbiome. The opportunity for phage therapy development is now a necessity as the looming threat from antibiotic resistant microbes increases.” Stanley Plotkin, Scientific Advisory Board Member and Emeritus Professor of the University of Pennsylvania, said: “Vaccines have always helped reduce the use of antibiotics and new vaccines directed at troublesome bacteria can do even more”.