Future Trends in Health Care Electronic Data Interchange Maryland
advertisement

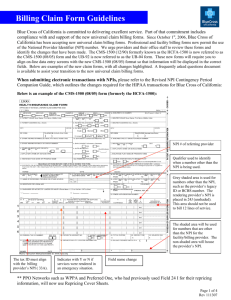
The Privacy Symposium The Sixteenth National HIPAA Summit Cambridge, MA Transactions, Code Sets and Identifiers (NPI) Update Jim Whicker, CPAM Intermountain Healthcare Director of EDI, A/R Management Chair, WEDI AAHAM EDI Liaison NPI – Our Experiences Claims processing ok Unexpected rejections Payer Crosswalks Inability to handle provider who practices in multiple locations 835’s processing mostly without incident Concern for some providers as not all segments fully NPI only Some payers have difficulty with paper and crossover claims Clearinghouse/Payer creating loops and segments not on outbound claim then rejecting claim for non compliance! National Provider ID NPI Additional Issues: Provider required to submit NPI on bill even when referring doc has no NPI/Unable to obtain Medicare Transmittal 235 made recommendations, but has since been rescinded without alternative Provider NPPES and IRS name mismatch Requirement to Update 855 documents with CMS and wait to update NPPES until AFTER CMS updates internal systems. Interaction issue between NPPES and PECOS CMS has processing issues for certain institutional bill types hitting the right area internally for payment. "You really don't need my driver's license officer...I have an NPI, a 10-digit, intelligence-free, numeric identifier." Cartoon by Dave Harbaugh NPRM – 5010, D.0, and ICD-10 Information released for public view Friday, August 15 Publication in Federal Register August 22, 2008 Comments Due October 21, 2008 For 5010 and D.0 Industry internal review for changes – begin September 2008 Internal/External Testing by April 2009 CMS expects to have full compliance by April, 2010 Short process for review of comments and posting of final rule? For ICD-10 Industry begin design and documentation June 2009 Industry build and internally test system changes December 2009 Test with trading partners July 2010 – October 2011 Full compliance October 2011 Still no Attachments final rule, nor plans for a National Payer ID Recommendation to adopt Acknowledgements, Standard ID Card 5010? Why? Current transactions are over 6 years old More than 500 industry requested changes via DSMO Many more industry requested changes via ASC X12 Addresses problems encountered with 4010A1 Improvements to implementation instructions More consistent implementations by trading partners Should reduce Companion Guide TP requirements Upgrade not a HIPAA “Do-over” Change analysis will require a thorough review of all transaction TR3s Analysis is X12 to X12 Less complicated than with round 1 Changes are not a 100% change Some transactions changed very little Other transactions changed moderately Others had significant changes (claims) General changes to all transactions More standardized front matter Addressed industry needs missing from 4010 Clarified intent where previously ambiguous Clarified, Added, or Deleted code values and qualifiers: To address industry requests To reduce confusion from similar or redundant values TR#’s (Implementation Guides) “Free” for 4010, Must be purchased for 5010 837 – Health Care Claims (I, P, D) Fixed significant industry problems: Improved front matter explanation of COB reporting and balancing logic Added COB crosswalk – and examples Section added to explain allowed and approved amounts Subscriber/patient hierarchy modified 837I Provider types were redefined in conjunction with the NUBC code set 837 – Health Care Claims (cont’d) Improved rules and instructions for reporting provider roles and use of NPI Added front matter sections to: Explain Medicaid subrogation Pay-to Plan information Explain reporting of drug claims POA Moved to a specific segment rather than “Kludged” Capability to do ICD-10 837 Professional - Anesthesia minutes Ambulance “Pick-up” information added Dental – easier to coordinate benefits between dental and medical plans Start/Stop dates for crowns/bridges Allows for Tooth numbers with International systems 835 – Claims Payment/Remittance Many improvements are in the Front Matter Tighter business rules to eliminate options and codes Allows compatibility with claims sent under version 4010 for transition Added Health Care Medical Policy – via payer URL Claim status has clearer guidance to report how a claim was adjudicated Better instructions for handling reversals and corrections; interest payments and prompt pay discounts Limits use of denial claim status to specific business case Advanced payments and reconciliation Secondary payment reporting considerations section revised 834 - Enrollment/Disenrollment 820 – Premium Payments 834: Allow usage of ICD-10 for reporting pre-existing condittions Privacy issues addressed Added codes to explain coverage changes Clarifies usage of coverage dates 820: Ability to report additional deductions from payments Method used to deliver remittance Simplifies and clarifies when adjustments to previous payments are needed 270/271 – Eligibility Clarified instructions for sending inquiries: When subscriber is patient When dependent is patient Newly required response information – When a patient has active benefit coverage, the health plan must report: • Beginning effective eligibility date, Plan name, and the Benefit effective dates if different from the overall coverage. • All demographic information needed by the health plan on subsequent transactions must be reported, primary care provider if available, and other payers if known. 270/271 – Eligibility Required alternate search options When payers are unable to find member eligibility information using all the data elements of the primary search, health plans must support inquiries with: Member ID, Last name only, and Date of Birth to help eliminate false negatives. This was a controversial requirement, and was just modified during the June trimester meeting, changes to the TR3 (Implementation Guide) will be forthcoming to reflect this modification. 270/271 – Eligibility (cont’d) Nine categories that must be reported Medical Care Chiropractic Care Dental Care Hospital Emergency Services Pharmacy Professional Visit – Office Vision Mental Health Urgent Care 270/271 – Eligibility (cont’d) Clear requirements for reporting patient responsibility with a monetary amount or percentage Added 38 new service type codes 276/277 – Health Care Claim Status Eliminated sensitive patient information that was unnecessary for business purpose Added Pharmacy related data segments and the use of NCPDP Payment Reject Codes Increased Claim Status segment repeat to > 1 for more detailed status information Added more examples to clarify instructions 278 – Referral Certification and Authorization Little implementation due to constraints under 4010 Added segments for reporting key patient conditions Added/expanded support for various business needs Expanded usage for authorizations Thank You!