Viruses - Dr Magrann
advertisement

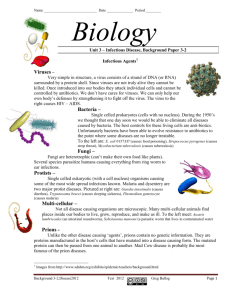
Viruses Viruses • Cause many infections of humans, animals, plants, and bacteria • Cannot carry out any metabolic pathway • Neither grow nor respond to the environment • Cannot reproduce independently • Obligate intracellular parasites Characteristics of Viruses • Cause most diseases that plague industrialized world • Virus – miniscule, acellular, infectious agent having one or several pieces of either DNA or RNA • No cytoplasmic membrane, cytosol, or organelles • Have extracellular and intracellular state Characteristics of Viruses • Extracellular state – – – – – Called virion Protein coat (capsid) surrounding nucleic acid Nucleic acid and capsid also called nucleocapsid Some have phospholipid envelope Outermost layer provides protection and recognition sites for host cells Characteristics of Viruses • Intracellular state – Capsid removed – Virus exists as nucleic acid • • • • • • How Viruses Are Distinguished Type of genetic material they contain Kinds of cells they attack Size of virus Nature of capsid coat Shape of virus Presence or absence of envelope Sizes of Viruses Figure 13.4 Genetic Material of Viruses • Show more variety in nature of their genomes than do cells • May be DNA or RNA; never both • Primary way scientists categorize and classify viruses • Can be dsDNA, ssDNA, dsRNA, ssRNA • May be linear and composed of several segments or single and circular • Much smaller than genomes of cells Hosts of Viruses • Most only infect particular kinds of host’s cells – Due to affinity of viral surface proteins or glycoproteins for complementary proteins or glycoproteins on host cell surface • May only infect particular kind of cell in host • Generalists – infect many kinds of cells in many different hosts Capsid Morphology • Capsids – protein coats that provide protection for viral nucleic acid and means of attachment to host’s cells • Capsid composed of proteinaceous subunits called capsomeres • Come capsids composed of single type of capsomere; other composed of multiple types The Viral Envelope • Acquired from host cell during viral replication or release; envelope is portion of membrane system of host • Composed of phospholipid bilayer and proteins; some proteins are virally-coded glycoproteins (spikes) • Envelope’s proteins and glycoproteins often play role in host recognition Viral Replication • Dependent on host’s organelles and enzymes to produce new virions • Replication cycle may or may not result in death of host cell • Stages of lytic replication cycle – Attachment – Entry – Synthesis – Assembly – Release Attachment of Animal Viruses • Chemical attraction • Animal viruses do not have tails or tail fibers • Have glycoprotein spikes or other attachment molecules that mediate attachment Attachment 14 Entry/Penetration 15 Entry/Penetration Synthesis of Animal Viruses • Each type of animal virus requires different strategy depending on its nucleic acid • Must consider – How mRNA is synthesized? – What serves as template for nucleic acid replication? Genome Replication and Protein Synthesis Figure 13.13 Assembly and Release of Animal Viruses • Most DNA viruses assemble in and are released from nucleus into cytosol • Most RNA viruses develop solely in cytoplasm • Number of viruses produced and released depends on type of virus and size and initial health of host cell • Enveloped viruses cause persistent infections • Naked viruses released by exocytosis or may cause lysis and death of host cell Release Enveloped and Naked • Lysis • Exocytosis 20 Release –Enveloped • Budding Latency of Animal Viruses • When animal viruses remain dormant in host cells • May be prolonged for years with no viral activity, signs, or symptoms • Some latent viruses do not become incorporated into host chromosome • When provirus is incorporated into host DNA, condition is permanent; becomes permanent physical part of host’s chromosome The Role of Viruses in Cancer • Normally, animal’s genes dictate that some cells can no longer divide and those that can divide are prevented from unlimited division • Genes for cell division “turned off” or genes that inhibit division “turned on” • Neoplasia – uncontrolled cell division in multicellular animal; mass of neoplastic cells is tumor • Benign vs. malignant tumors – Metastasis – Cancers How Viruses Cause Cancer • Some carry copies of oncogenes as part of their genomes • Some stimulate oncogenes already present in host • Some interfere with tumor repression when they insert into host’s repressor gene • Several DNA and RNA viruses are known to cause ~15% of human cancers – – – – Burkitt’s lymphoma Hodgkin’s disease Kaposi’s sarcoma Cervical cancer Oncogene Theory Figure 13.15 Culturing Viruses in the Laboratory • In Whole Organisms – Bacteria – Plants and Animals • Embryonated Chicken Eggs • In Cell (Tissue Culture) Culturing Viruses in Embryonated Chicken Eggs Figure 13.17 Culturing Viruses in Cell (Tissue) Culture Figure 13.18 Characteristics of Prions • Proteinaceous infectious agents • Composed of single protein PrP • All mammals contain gene that codes for primary sequence of amino acids in PrP • Two stable tertiary structures of PrP – Normal functional structure with α-helices called cellular PrP – Disease-causing form with β-sheets called prion PrP • Prion PrP converts cellular protein into prion PrP by inducing conformational change Tertiary Structures of PrP Figure 13.21 Prion Diseases • All involve fatal neurological degeneration, deposition of fibrils in brain, and loss of brain matter • Large vacuoles form in brain; characteristic spongy appearance • Spongiform encephalopathies – BSE, CJD, kuru • Only destroyed by incineration; not cooking or sterilization DNA Viruses – Classified based on the type of DNA they contain, the presence or absence of an envelope, size, and the host cells they attack • Contain either double-stranded DNA (dsDNA) or single-stranded DNA (ssDNA) for their genome • Double-stranded DNA viruses – Poxviridae, Herpesviridae, Papillomaviridae, Polyomaviridae, and Adenoviridae Poxviridae • • • • • Double-stranded DNA viruses Have complex capsids and envelopes Largest viruses Infect many mammals Most animal poxviruses are species specific – Unable to infect humans because they cannot attach to human cells • Infection occurs primarily through the inhalation of viruses • Close contact is necessary for infection by poxviruses Poxviridae • Smallpox and molluscum contagiosum are the two main poxvirus diseases of humans • Some diseases of animals can be transmitted to humans • All poxviruses produce lesions that progress through a series of stages Figure 24.2 Smallpox • In the genus Orthopoxvirus • Commonly known as variola • Exists in two forms – Variola major causes sever disease that can result in death – Variola minor causes a less severe disease with a much lower mortality rate • Both forms infect internal organs and then move to the skin where they produce pox • Scars result on the skin, especially on the face Smallpox • There are a number of factors that allowed eradication of smallpox – Inexpensive, stable, and effective vaccine – No animal reservoirs – Obvious symptoms allow for quick diagnosis and quarantine – Lack of asymptomatic cases – Virus is only spread via close contact Smallpox as a Bioweapon • • • • • • can be produced in large quantities stable for storage and transport stable in aerosolized form (up to 2 days) high mortality highly infectious (person-to-person spread) most of the world has little to no immunity Therapy/Prevention of Smallpox • Vaccination – vaccination stopped in 1979 (1972 in U.S.) • last case in U.S. 1949 • 2 million deaths Worldwide in 1967 – Vaccinia virus • leaves scar • Supportive therapy – no effective antiviral once infected Molluscum Contagiosum • Caused by Molluscipoxvirus • Spread by contact among infected children • Sexually active adults can sometimes contract a genital form of the disease • Skin disease characterized by smooth, waxy, tumorlike nodules on the face, trunk, and limbs • Virus produces a weak immune response • Causes neighboring cells to divide rapidly thus acting like a tumor-causing virus Other Poxvirus Infections • Poxvirus infections also occur in animals • Transmission of these poxviruses to humans require close contact with infected animals • Infections of humans are usually mild • Can result in pox and scars but little other damage • Cowpox was used by Edward Jenner to immunize individuals against smallpox Papillomavirus Infections • Causes papillomas, commonly known as warts – Benign growths of the epithelium of the skin or mucous membranes • Papillomas form on many body surfaces • Often painful and unsightly • Genital warts are associated with an increased risk of cancer Epidemiology and Pathogenesis of Papillomavirus Infections • Transmitted via direct contact and via fomites • autoinoculation • Viruses that cause genital warts invade the skin and mucous membranes during sexual intercourse • Genital warts are a common sexually transmitted disease Diagnosis, Treatment, and Prevention • Diagnosis – Usually based on observation of the papillomas – Diagnosis of cancers results from inspection of the genitalia and by a PAP smear in women • Treatment – Some warts can be removed through various methods – Treatment of cancers involves radiation and chemical therapy Diagnosis, Treatment, and Prevention • Prevention – Prevention of most types of warts is difficult – Genital warts can be prevented by abstinence and perhaps safe sex HPV vaccine • 2006 - Advisory committee on immunization practices (ACIP) recommended the HPV vaccine – recommended for girls/women 9-26 yrs old • before sexual contact • recommended at 11-12 years of age – vaccine (Gardasil) protects against 4 HPV strains (HPV 6, 11, 16, and 18) Adenoviridae • One of the causative agents of the common cold • Spread via respiratory droplets • Respiratory infections – Viruses are taken into cells lining the respiratory tract via endocytosis – Symptoms include sneezing, sore throat, cough, headache, and malaise Adenoviridae • Infection of the intestinal tract can produce mild diarrhea • Infection of the conjunctiva can result in pinkeye Adenovirus pathology • diarrhea in children • respiratory infection in children and adults – military recruits • • • • close contact physical activities (deep inhalation of virus into lungs) stress after infection, see immunity Herpesviridae • Viruses attach to a host cell’s receptor and enter the cell through the fusion of its envelope with the cell membrane • Herpesviruses can have latency – They may remain inactive inside infected cells – Viruses may reactivate causing a recurrence of manifestations of the disease Herpesviridae • Herpesviruses include various genera – Simplexvirus, Varicellovirus, Lymphocryptovirus, Cytomegalovirus, Roseolovirus • Herpesviruses are also designated by “HHV” (for “human herpesvirus”) and a number indicating the order in which they were discovered “Newer” nomenclature of the Herpesviridae • • • • • • • • HHV1 = HSV1 HHV2 = HSV2 HHV3 = VZV HHV4 = EBV HHV5 = CMV HHV6 = roseola infantum (major cause) HHV7 = roseola infantum (minor cause) HHV8 = KS 52 Herpes Simplex Infections • Often result in slowly spreading skin lesions • Viruses of this genus are commonly known as herpes simplex virus or HSV • 2 species of herpes simplex – Herpes simplex virus type 1 (HSV-1) – Herpes simplex virus type 2 (HSV-2) Epidemiology and Pathogenesis of HSV Infections • Active lesions are the usual source of infection • Aysmptomatic carriers can shed HSV-2 genitally • Transmission of the viruses occurs through close bodily contact • Viruses enter the body through cracks or cuts in mucous membranes • Skin lesions result from inflammation and cell death at the site of infection • Herpes virions can spread from cell to cell through the formation of syncytia Epidemiology and Pathogenesis of HSV Infections • HSV-1 infections typically occur via casual contact in children • HSV-2 infections are acquired between the ages of 15 and 29 from sexual activity • Herpes infections often result in the recurrence of lesions • Up to two-thirds of patients experience recurrences due to activation of the latent virus Figure 24.5 Diagnosis, Treatment, and Prevention • Diagnosis – Characteristic lesions, especially in the genital region and on the lips, is often diagnostic Diagnosis, Treatment, and Prevention – HSV infections are among the few viral diseases that can be controlled with chemotherapeutic agents – Topical applications of the drugs limit the duration of the lesions and reduce viral shedding – The drugs don’t cure the diseases or free nerve cells of latent viral infections Varicella-Zoster Virus Infections • Commonly referred to as VZV • Causes two diseases – Varicella • Often called chicken pox • Typically occurs in children – Herpes zoster • Also called shingles • Usually occurs in adults Epidemiology and Pathogenesis of VZV Infections • Chickenpox is a highly infectious disease seen most often in children • Viruses enter the skin through the respiratory tract and the eyes • Virus replicate at the site of infection then travel via the blood throughout the body • Chickenpox in adults is typically more severe than the childhood illness Epidemiology and Pathogenesis of VZV Infections • Latent virus can reactivate producing a rash known as shingles • The rash is characteristic for its localization along a dermatome - dorsal roots from the spine Figure 24.10 Epstein-Barr Virus Infections • Also referred to as EBV or HHV-4 • Can cause a number of different diseases Epidemiology and Pathogenesis of EBV Infections • Transmission of EBV usually occurs via saliva • Virions initially infect the epithelial cells of the pharynx and parotid salivary glands • The virus then enters the bloodstream where it invades the B lymphocytes Epidemiology and Pathogenesis of EBV Infections • The viruses become latent in B cells and immortalize them by suppressing apoptosis • Symptoms of infectious mononucleosis arise from the immune response – Cytotoxic T cells kill virus infected B lymphocytes Epidemiology and Pathogenesis of EBV Infections • Cancer development appears to depend in part on various cofactors • Extreme diseases arise in individuals with T cell deficiency – Such individuals are susceptible because infected cells are not removed by cytotoxic T cells allowing the virus to proliferate Cytomegalovirus • Also referred to as CMV • Cells infected with this virus become enlarged • CMV infections is one of the more common infections of humans Cytomegalovirus • Transmission occurs through bodily secretions – Requires close contact and a large exchange of secretion – Usually occurs via sexual intercourse – Also transmitted by in utero exposure, vaginal birth, blood transfusions, and organ transplants • Most CMV infections are asymptomatic Cytomegalovirus • Fetuses, newborns, and immunodeficient patients can develop complications – CMV can cause birth defects and may result in death – AIDS patients or other immunocompromised adults may develop pneumonia, blindness, or cytomegalovirus mononucleosis, which is similar to infectious mononucleosis • CMV causes infectious mononucleosis (second to EBV) Other Herpesvirus Infections • Human herpesvirus 6 (HHV-6) – In the genus Roseolovirus – Causes roseola which is characterized by a pink rash on the face, neck, trunk, and thighs – Linked to multiple sclerosis by some researchers – Can cause mononucleosis-like symptoms – Infection with HHV-6 may make individuals more susceptible to AIDS Other Herpesvirus Infections • Human herpesvirus 8 (HHV-8) – Associated with Kaposi’s sarcoma, a cancer seen in AIDS patients – The virus is not found in cancer-free patients or in normal tissues of victims RNA Viruses • Positive RNA acts like mRNA and can be used by a ribosome to translate protein • Negative RNA must first be transcribed as mRNA to be processed by a ribosome • RNA viruses are categorized by their genomic structure, the presence of an envelope, and the size and shape of their capsid Picornaviridae • Enteroviruses – Polio – Hepatitis A • Rhinovirus 73 Enteroviruses • Found – in respiratory secretions – stool of an infected person – Parents, teachers, and child care center workers may also become infected by contamination of the hands with stool from an infected infant or toddler during diaper changes. Poliomyelitis • First described by Michael Underwood in 1789 • First outbreak described in U.S. in 1843 • 21,000 paralytic cases reported in the U. S. in 1952 • Global eradication in near future Poliovirus • • • • Enterovirus (RNA) Three serotypes: 1, 2, 3 Minimal immunity between serotypes Rapidly inactivated by heat, formaldehyde, chlorine, ultraviolet light • Most poliovirus infections are asymptomatic Poliomyelitis Pathogenesis • Fecal oral entry • Replication in pharynx, GI tract, local lymphatics • Hematologic spread to lymphatics and central nervous system • Viral spread along nerve fibers • Destruction of motor neurons Poliomyelitis—United States, 1950-2007 25000 Inactivated vaccine Cases 20000 15000 10000 Live oral vaccine Last indigenous case 5000 0 1950 1960 1970 1980 1990 2000 Comparison of Polio Vaccines Table 25.2 Polio Vaccination Recommendations • Exclusive use of IPV recommended in 2000 • OPV no longer routinely available in the United States Schedules that Include Both IPV and OPV • Only IPV is available in the United States • Schedule begun with OPV should be completed with IPV • Any combination of 4 doses of IPV and OPV by 5 years constitutes a complete series Polio Vaccine Adverse Reactions • Rare local reactions (IPV) • No serious reactions to IPV have been documented • Paralytic poliomyelitis (OPV) Hepatitis A • • • • Epidemic jaundice described by Hippocrates Differentiated from hepatitis B in 1940s Serologic tests developed in 1970s Vaccines licensed in 1995 and 1996 Hepatitis A Virus • • • • Picornavirus (RNA) Humans are only natural host Stable at low pH Inactivated by high temperature (185°F or higher), formalin, chlorine Hepatitis A Pathogenesis • Fecal oral entry • Viral replication in the liver • Virus present in blood and feces 10-12 days after infection • Virus excretion may continue for up to 3 weeks after onset of symptoms Hepatitis A - United States, 1966-2007 70000 Vaccine Licensed 60000 Cases 50000 40000 30000 20000 10000 0 1966 1970 1975 1980 1985 Year 1990 1995 2000 2005 Hepatitis A Vaccines • Inactivated whole virus vaccines • Pediatric and adult formulations – Pediatric formulations vaccines approved for persons 12 months through 18 years – Adult formulations approved for persons 19 years and older Hepatitis A Postexposure Prophylaxis • For healthy persons 12 months through 40 years of age: – single-antigen hepatitis A vaccine should be administered as soon as possible after exposure • For persons older than 40 years: – immune globulin is preferred – vaccine can be used if IG cannot be obtained MMWR 2007;56(No.41):1080-4 Rhinovirus • Cause most cases of the common cold • Infections are limited to the upper respiratory tract • A single virus is often sufficient to cause a cold • The virus can be spread through aerosols, via fomites, or via hand-to-hand contact Rhinovirus • Direct person-to-person contact is the most common means of transmission • Individuals can acquire some immunity against serotypes that have infected them in the past – As a result, the number of infections tends to decrease with age Diseases of Coronaviruses • Named due to the corona-like halo formed by their envelopes • Transmitted via large droplets from the upper respiratory tract • Second most common cause of colds • Can cause gastroenteritis in children • Diseases are mild • No treatment or vaccine is available 0 Diarrhea Nausea & Vomiting Running nose Sore throat Sputum Dizziness Headache Cough Myalgia Chills & Rigor Fever % of patients Common Symptoms 100 90 80 70 60 50 40 30 20 10 Introduction to the Norwalk Virus Norwalk – genus name for original Norwalk virus and other Norwalk-like viruses. Family Calicivirus. Calicivirae found worldwide, infecting humans, primates, and cattle, among others. Increasingly being recognized as leading cause of food borne illness. History Virus first identified in Norwalk, Ohio, 1973. Noted to commonly be a problem on cruise ships. Associated with contaminated food or water supplies. Infection Noroviruses found in stool and vomit of infected. Very contagious – infection via eating contaminated food, contact with sick individual or contaminated surfaces. Symptoms Acute gastroenteritis. Illness begins suddenly, from 12-48 hours after ingestion. Brief illness period. Very young, elderly, and those with weakened immune systems may experience more severe symptoms. Infectiousness may last up to 2 weeks, no evidence of long-term carriers. Measles • One of five classical childhood diseases • Spread in the air via respiratory droplets • Viral spread requires large, dense populations of people • Viruses infect the respiratory tract and then spread throughout the body Measles • Characteristic lesions called Koplik’s spots appear on the mucous membrane of the mouth • Lesions then appear on the head and spread over the body Measles • Highly contagious viral illness • First described in 7th century • Near universal infection of childhood in prevaccination era • Common and often fatal in developing areas Measles Virus • • • • Paramyxovirus (RNA) Hemagglutinin important surface antigen One antigenic type Rapidly inactivated by heat and light Measles Pathogenesis • Respiratory transmission of virus • Replication in nasopharynx and regional lymph nodes • Primary viremia 2-3 days after exposure • Secondary viremia 5-7 days after exposure with spread to tissues Measles Clinical Features • Incubation period 10-12 days • Prodrome – Stepwise increase in fever to 103°F or higher – Cough, coryza, conjunctivitis – Koplik spots (rash on mucous membranes) Coryza = Head cold Measles Clinical Features • Rash – 2-4 days after prodrome, 14 days after exposure – Maculopapular, becomes confluent – Begins on face and head – Persists 5-6 days – Fades in order of appearance Measles Complications Condition Diarrhea Otitis media Pneumonia Encephalitis Hospitalization Percent reported 8 7 6 0.1 18 0.2 Death Based on 1985-1992 surveillance data Measles Laboratory Diagnosis • Isolation of measles virus from a clinical specimen (e.g., nasopharynx, urine) • Significant rise in measles IgG by any standard serologic assay (e.g., EIA, HA) • Positive serologic test for measles IgM antibody Measles - United States, 1950-2007 Cases (thousands) 900 800 700 Vaccine Licensed 600 500 400 300 200 100 0 1950 1960 1970 1980 1990 2000 Measles Mumps Rubella Vaccine • 12 months is the recommended and minimum age • MMR given before 12 months should not be counted as a valid dose • Revaccinate at 12 months of age or older Adults at Increased Risk of Measles • College students • International travelers • Healthcare personnel – All persons who work in medical facilities should be immune to measles Mumps • Acute viral illness • Parotitis and orchitis described by Hippocrates in 5th century BCE • Viral etiology described by Johnson and Goodpasture in 1934 • Frequent cause of outbreaks among military personnel in prevaccine era Mumps Virus • • • • Paramyxovirus RNA virus One antigenic type Rapidly inactivated by chemical agents, heat, and ultraviolet light Mumps Pathogenesis • Respiratory transmission of virus • Replication in nasopharynx and regional lymph nodes • Viremia 12-25 days after exposure with spread to tissues • Multiple tissues infected during viremia Mumps Complications CNS involvement 15% of clinical cases Orchitis 20%-50% in post- pubertal males Pancreatitis 2%-5% Deafness 1/20,000 Death Average 1 per year (1980 – 1999) Mumps—United States, 1980-2007 14000 12000 Cases 10000 8000 6000 4000 2000 0 1980 1985 1990 Year 1995 2000 2005 Mumps Clinical Case Definition • Acute onset of unilateral or bilateral tender, self-limited swelling of the parotid or other salivary gland lasting more than 2 days without other apparent cause What Is Bronchiolitis? • Bronchiolitis is acute inflammation of the airways, characterised by wheeze • Bronchiolitis can result from a viral infection • Respiratory Syncytial Virus (RSV) may be responsible for up to 90% of bronchiolitis cases in young children Hall CB, McCarthy CA. In: Principles and Practice of Infectious Diseases 2000:1782-1801; Panitch HB et al. Clin Chest Med 1993;14:715-731 115 Diagnosis, Treatment, and Prevention • Diagnosis is based on the signs of respiratory distress verified by immunoassay • Treatment is supportive • Ribavirin is used to treat extreme cases Influenza • Caused by two species of orthomyxovirus, designated types A and B • Infection occurs primarily through inhalation of airborne viruses • Rarely attack cells outside the lungs 118 Influenza • Death of the epithelial cells infected with influenza viruses eliminate the lungs first line of defense against infections, the epithelial lining • Flu patients become more susceptible to secondary bacterial infections TRANSMISSION • AEROSOL – 100,000 TO 1,000,000 VIRIONS PER DROPLET • 18-72 HR INCUBATION • SHEDDING 120 SYMPTOMS • • • • • • FEVER HEADACHE MYALGIA COUGH RHINITIS OCULAR SYMPTOMS 121 CLINICAL FINDINGS • SEVERITY – VERY YOUNG – ELDERLY – IMMUNOCOMPROMISED – HEART OR LUNG DISEASE 122 PULMONARY COMPLICATIONS • CROUP (YOUNG CHILDREN) • PRIMARY INFLUENZA VIRUS PNEUMONIA • SECONDARY BACTERIAL INFECTION – Streptococcus pneumoniae – Staphlyococcus aureus – Hemophilus influenzae 123 Reye’s syndrome • • • • liver - fatty deposits brain - edema vomiting, lethargy, coma risk factors – youth – certain viral infections (influenza, chicken pox) – aspirin 124 NON-PULMONARY COMPLICATIONS • cardiac complications • encephalopathy • liver and CNS – Reye’s syndrome • peripheral nervous system – Guillian-Barré syndrome 125 Guillian-Barré syndrome • 1976/77 swine flu vaccine – 35,000,000 doses • 354 cases of GBS • 28 GBS-associated deaths • recent vaccines much lower risk 126 MORTALITY • MAJOR CAUSES OF INFLUENZA VIRUSASSOCIATED DEATH – BACTERIAL PNEUMONIA – CARDIAC FAILURE • 90% OF DEATHS IN THOSE OVER 65 YEARS OF AGE 127 ANTIGENIC DRIFT • HA and NA accumulate mutations – RNA virus • immune response no longer protects fully • sporadic outbreaks, limited epidemics 128 Figure 25.39 ANTIGENIC SHIFT • “new” HA or NA proteins • pre-existing antibodies do not protect • may get pandemics 130 Figure 25.39 Influenza epidemiology • Influenza A has wide host range – Birds (natural), sea mammals, horses, pigs, humans • Strains are described by antigenicity of HA and NA, which are designated by numbers • Currently 15 HA (1-15) and 9 NA (1-9) described – – – – – 1918 “Spanish flu” pandemic – H1N1 1957 “Asian flu” epidemic – H2N2 1968 “Hong Kong flu” pandemic – H1N2 1977 “swine flu” epidemic – H1N1 1999 – current threat is H5N1, similar to 1918 strain • Epidemiology involves close contact of humans, farm animals, and birds – this especially in Asia • Kills >20,000 per year in the US normally VACCINE • ‘BEST GUESS’ OF MAIN ANTIGENIC TYPES – CURRENTLY • • • • type A - H1N1 type A - H3N2 type B each year choose which variant of each subtype is the best to use for optimal protection 133 VACCINE • inactivated • egg grown • sub-unit vaccine for children • reassortant live vaccine approved 2003 – for healthy persons (those not at risk for complications from influenza infection) ages 5-49 years 134 SUPPORTIVE TREATMENT • REST, LIQUIDS, ANTI-FEBRILE AGENTS (NO ASPIRIN FOR AGES 6MTHS-18YRS) • BE AWARE OF COMPLICATIONS AND TREAT APPROPRIATELY 135 Enveloped, Unsegmented Negative ssRNA Viruses • Includes the Paramyxoviridae, Rhabdoviridae, and Filoviridae families Enveloped, Unsegmented Negative ssRNA Viruses • Rhabdoviridae – Include a variety of plant and animal pathogens – Rabies is the most significant pathogen • Filoviridae – Cause a number of emerging diseases – Include Ebola and Marburg hemorrhagic fevers Rabies • Rabies virus is the causative agent • Classical zoonotic disease of mammals • Primary reservoir of rabies in urban areas is the dog • Bats are the source of most cases of rabies in humans Rabies • Rabies virus is the causative agent • Classical zoonotic disease of mammals • Primary reservoir of rabies in urban areas is the dog Rabies • When the virus infects the central nervous system neurological manifestations specific to rabies develop (such as hydrophobia) • Death results from respiratory paralysis and other neurological complications Diagnosis, Treatment, and Prevention • Diagnosis – Neurological symptoms of rabies are unique and usually sufficient – By the time symptoms and antibodies occur it is too late to intervene • Treatment – Treatment of the site of infection – Injection of human rabies immune globulin – Vaccination with human diploid cell vaccine (HDCV) • Viral replication and movement to the brain is slow enough to allow effective immunity to develop before disease develops Diagnosis, Treatment, and Prevention • Prevention – Vaccination of domestic dogs and cats can help control rabies – Little can be done to eliminate rabies in wild animals Source: Centers for Disease Control and Prevention, November 2010 Hemorrhagic Fevers • Marburg virus and Ebola virus are the causative agents • The natural reservoir and mode of transmission to humans are unknown • Spread from person to person via contaminated bodily fluids, primarily blood, and contaminated syringes • The virions attack many cells of the body, especially macrophages and liver cells • Infections results in uncontrolled bleeding under the skin and from every body opening Hemorrhagic Fevers • The only treatment involves fluid replacement • Up to 90% of human victims die Viral Structure of Ebola • It is a member of the Filoviridae family (the only other member is Marburgvirus). • ss, negative sense RNA • Has a distinct characteristic “6” shape. History • First found in a province in Sudan and its neighboring country, Zaire (1976). The Zaire outbreak 280/318 cases resulted in death. The Sudan strain caused death in 397/602 cases. • 1989: Ebola made its way to the United States. A lab worker was infected by the monkeys he was working with (Maccaca fascicularis). Workers developed antibodies to Ebola, but did not get sick. • 1994: Cote d’ Ivory- only one case here: a scientist conducted an autopsy on a wild chimpanzee. He fell ill, but did not die. Strains Summary In total, there are 4 known, documented strains of Ebola: – – – – Ebola Zaire (EBO-Z): a 90% death rate Ebola Sudan (EBO-Z): lower death rate Ebola Reston Ebola Cote d’ Ivory All strains of Ebola are classified as Biosafety Level 4, meaning Hazmat suits, multiple airlocks, ultraviolet light rooms. Workers must be cleared to handle BSL4. Transmission • One of the easiest methods of transmission in Ebola is through bodily fluids (blood, secretions). • Handling infected animals can also lead to infection with Ebola. • While monkeys were able to transfer Ebola between themselves via airborne particles, this type of aerosol transfer has not been demonstrated setting in a laboratory setting. Symptomology • Incubation periods can be anywhere from 2-21 days. • Common symptoms include: sudden onset of fever, headaches, sore throat, muscle pains, and intense weakness. • More intense symptoms include: maculopapular rash, kidney/liver disfunction. • Possible internal/external bleeding. Coagulpathy • Internal bleeding is caused by Ebola’s coagulpathy ability. This describes a dysfunction in the host blood clotting system. • When infected, host macrophages begin to express Tissue Factor (TF). TF attracts clotting molecules from the blood, leaving the rest of the body susceptible. • Small holes in the capillaries are then cut by Ebola. Without clotting factors, the host bleeds continuously, dying of what some have called “a million cuts.” Reservoirs • Unfortunately, no reservoirs have been identified for Ebola. Several times, scientists have brought in rodents, bats, primates, plants, and arthropods to test for Ebola. • Ebola could not be detected or isolated from any of these reservoirs. Treatment • As there is no known cure for Ebola, treatment options are very limited for patients. • Typically, supportive therapy is used (balancing patient’s fluids, electrolytes, maintaining oxygen status and blood pressure). • While there are no cures yet, that does not mean several groups are not working to create one. Barrier Nursing Techniques • • • • Barrier Nursing Techniques are employed to prevent further infection. Screens are placed around the patient’s bed. Anyone treating the patient must wear gowns, masks, and gloves. Any items used to treat the patient are immediately put into a sterilizing solution afterwards. Changing sheets must also be done with care, to minimize the possibility of launching airborne particles or droplets of contagious material. Cures/Vaccines • 1999: BBC researchers, led by Dr. Maurice Iwu, investigated the garcin kola plant, typically eaten in Western Africa. Medicine men in those areas had long been using it and introduced it to the researchers. In a lab setting, the plant has been shown to inhibit Ebola multiplication. • 2001: Mice injected subcutaneously with Ebola did not become sick, but mounted an immune response. Serum from these mice were used to treat new mice before or after Ebola injection. All of the mice treated with serum survived. Reoviruses • Cause infantile gastroenteritis • Account for approximately 50% of all cases of diarrhea in children requiring hospitalization • Transmitted via the fecal-oral route • usually self-limited • replacement of water and electrolytes • A vaccine is available that provides some protection but has been linked to a rare bowel blockage condition in some children Rotavirus • First identified as cause of diarrhea in 1973 • Most common cause of severe diarrhea in infants and children • Nearly universal infection by 5 years of age • Responsible for up to 500,000 diarrheal deaths each year worldwide Rotavirus Pathogenesis • Entry through mouth • Replication in epithelium of small intestine • Replication outside intestine and viremia uncommon • Infection leads to isotonic diarrhea Rotavirus Immunity • Antibody against VP7 and VP4 probably important for protection • First infection usually does not lead to permanent immunity • Reinfection can occur at any age • Subsequent infections generally less severe Rotavirus Clinical Features • Short incubation period (usually less than 48 hours) • First infection after age 3 months generally most severe • May be asymptomatic or result in severe dehydrating diarrhea with fever and vomiting • Gastrointestinal symptoms generally resolve in 3 to 7 days Rotavirus Complications • • • • • Severe diarrhea Dehydration Electrolyte imbalance Metabolic acidosis Immunodeficient children may have more severe or persistent disease Risk Groups for Rotavirus Diarrhea • Groups with increased exposure to virus – Children in child care centers – Children in hospital wards (nosocomial rotavirus) – Caretakers, parents of these children – Children, adults with immuno- deficiency related diseases (e.g. SCID, HIV, bone marrow transplant) Enveloped, Positive ssRNA Viruses • Includes the Togaviridae, Flaviviridae, and Coronaviridae families • Togaviridae and Flaviviridae – Enveloped, icosahedral, +ssRNA viruses – Designated arboviruses because they are often transmitted by arthropods • Coronaviridae – Enveloped, helical, +ssRNA viruses Rubella • • • • • • • • Togaviridae “German measles’ Rubella virus is the causative agent One of the five childhood diseases that produces skin lesions Infection begins in the respiratory system but spreads throughout the body Characterized by a rash of flat, pink to red spots Infections in children are usually not serious Adults can develop arthritis or encephalitis Rubella • Rubella infections of pregnant women can result in congenital defects or death of the child • Vaccination has been effective at reducing the incidence of rubella Rubella • From Latin meaning "little red" • Discovered in 18th century - thought to be variant of measles • Congenital rubella syndrome (CRS) described by Gregg in 1941 Rubella Pathogenesis • Respiratory transmission of virus • Replication in nasopharynx and regional lymph nodes • Viremia 5-7 days after exposure with spread to tissues • Placenta and fetus infected during viremia Rubella Clinical Features • Incubation period 14 days (range 12-23 days) • Prodrome of low-grade fever • Maculopapular rash 14-17 days after exposure • Lymphadenopathy in second week Epidemic Rubella – United States, 1964-1965 • • • • • 12.5 million rubella cases 2,000 encephalitis cases 11,250 abortions (surgical/spontaneous) 2,100 neonatal deaths 20,000 CRS cases – deaf - 11,600 – blind - 3,580 – mentally retarded - 1,800 Congenital Rubella Syndrome • Infection may affect all organs • May lead to fetal death or premature delivery • Severity of damage to fetus depends on gestational age • Up to 85% of infants affected if infected during first trimester Congenital Rubella Syndrome • • • • • • • Deafness Cataracts Heart defects Microcephaly Mental retardation Bone alterations Liver and spleen damage Rubella Laboratory Diagnosis • Isolation of rubella virus from clinical specimen (e.g., nasopharynx, urine) • Positive serologic test for rubella IgM antibody • Significant rise in rubella IgG by any standard serologic assay (e.g., enzyme immunoassay) Rubella and CRS in the United States • Most reported rubella in the U.S. since the mid-1990s has occurred among foreign-born Hispanic adult • Majority of CRS since 1997 occurred in children of unvaccinated women born to Hispanic women, most born in Latin America Rubella - United States, 1980-2007 4500 4000 3500 3000 2500 2000 1500 1000 500 0 1980 CRS 40 35 30 25 20 15 10 5 0 1985 1990 1995 Year 2000 2005 CRS Cases Rubella Cases Rubella Rubella Case Definition • Acute onset of generalized maculopapular rash, and • Temperature of >99°F (37.2 °C), if measured, and • Arthralgia or arthritis, lymphadenopathy, or conjunctivitis Enveloped, Segmented Negative ssRNA Viruses • Includes the Orthomyxoviridae, Bunyaviridae, and Arenaviridae families • Orthomyxoviridae – Flu viruses • Bunyaviridae, and Arenaviridae – Include hundreds of viruses that normally infect animals but can be transmitted to humans Family Bunyaviridae 5 genera, 250 species Genus Human disease Bunyavirus LaCrosse encephalitis, others Phlebovirus Rift Valley fever, sandfly fever Nairovirus Crimean-Congo hemorrhagic fever Tospovirus Plant virus, no known human disease Hantavirus Hemorrhagic fever with renal syndrome Hantavirus pulmonary syndrome Diseases of Bunyaviruses • Most bunyaviruses are zoonotic pathogens • Usually transmitted to humans by biting arthropods • Infections result with an initial viremia spreading the virus to target organs Diseases of Bunyaviruses • Symptoms are usually mild • Hantviruses are the exception – Transmitted to humans via inhalation of virions in dried deer-mouse urine or feces – American strains can cause a rapid, severe, and often fatal pneumonia called hantavirus pulmonary syndrome Hantavirus Outbreak in the US • HPS was first described in the United States in May 1993 during the investigation of a cluster of cases of acute adult respiratory distress in the Four Corners region. • HPS was found to be caused by a previously unknown hantavirus, Sin Nombre, detected in deer mice. • Sin Nombre caused approximately 200 confirmed cases of HPS during the outbreak, that led to a 50% mortality rate. Hantavirus Genus • Hantavirus Similarities – RNA viruses – Lipid membrane – Tri-segmented genome • Hantavirus Differences – Hantavirus transmitted through aerosolized rodent urine, feces and saliva. – Others genera transmitted through arthropod vectors. Epidemiology and Rodent Hosts • Each strain of hantavirus has a specific rodent host • Hantavirus species appear to have co-evolved with host rodent species • Rodents carrying hantavirus are asymptomatic Transmission of Hantaviruses Chronically infected rodent Horizontal transmission of infection by intraspecific aggressive behavior Virus is present in aerosolized excreta, particularly urine Virus also present in throat swab and feces Secondary aerosols, mucous membrane contact, and skin breaches are also sources of infection Courtesy of CDC Hantavirus Pulmonary Syndrome Countries with reported cases of HPS (no of cases) Canada (36) Countries with no reported cases of HPS United States (335) Panama (31) Bolivia (20) Chile (273) Brazil (168) Paraguay (74) Uruguay (23) Argentina (404) Hantavirus and Host Cells • Virus replication typically halts host macromolecule synthesis • Hantavirus replication does not affect host cell’s natural functions • Hantavirus release does not require host cell lysis • Hantavirus is able to establish a persistent infection in rodent host cells Hantavirus Infection Pathogenesis • Binding of Hantavirus glycoproteins integrin causes disruption of vascular integrity • Capillaries become more permeable • Arteriole vasoconstriction and vasodilation are disrupted • Binding to platelet receptors affects clotting and platelet function Immune Reaction • Immune system activated against Hantavirus epitopes • Virus epitopes expressed on surface of host cells triggers cytotoxic T-cell attack on host tissues • Symptoms are consistent with inflammatory response Laboratory Diagnosis of Hantavirus • Hantavirus is difficult to culture, so morphological identification is difficult • RT-PCR using primers for conserved genome regions allows confirmation of infection • PCR product can be sequenced and compared to known viral sequence database for species identification Clinical Presentation of Hantavirus Infection Three different clinical manifestations of hantavirus infection caused by different viral strains Hemorrhagic fever with renal syndrome (HFRS) • Found in Europe and Asia Nephropathia Epidemica (NE) • Found in Europe Hantavirus pulmonary syndrome (HPS) • Found in north and south America HPS • 1993 four corners outbreak • Cases found in almost all of the Americas • ~50% fatality Stages of Hantavirus Pulmonary Syndrome (HPS) 1) 2) 3) 4) 5) Incubation (4-30 days) Febrile phase Cardiopulmonary phase Diuretic phase Convalescent phase Febrile Phase • 3-5 days • Fever, myalgia, malaise • Other symptoms: headache, dizziness, anorexia, nausea, vomiting, and diarrhea. Cardiopulmonary Phase • 4-24 hours • Presentation and rapid progression of shock and pulmonary edema (4-24h non-productive cough and tachypnea (shortness of breath) • Decreased blood volume fromleakage of high protein fluid from blood to lung • Death within 24-48 hours due to hypoxia (lack of oxygen) and/or myocardial failure Diuretic Phase • • • • • Several days to several weeks Beginning of recovery Rapid clearance of pulmonary edema Resolution of fever and shock Anorexia, fatigue due to dehydration Convalescent Phase • Up to 2 months • Results in chronic decreased small-airway volume and diminished alveolar diffusing capacity Clinical Testing for HPS • Many lab tests and radiographs appear normal • Serological tests more effective • ELISA IgM capture assay, using either SNV, Laguna Negra, or Andes antigens are used in all countries that have previously detected cases • Immunofluorescent test for the presence of antibodies • Blood analysis also may find thrombocytopenia with platelet count less than 150,000 mm in 98% of cases Problems Diagnosing HPS • Symptoms often confused with influenza • Common signs of upper respiratory disease such as sore throat, sinusitis, and ear pain not usually present • Abdominal pain often misinterpreted as appendicitis • Many doctors outside endemic regions fail to recognize or have sufficient testing