Cholera Definition

Poliomyelitis
Dept. Of Infectious Disease
2nd Affiliated Hospital
CMU
Definition
Poliomyelitis is acute infectious disease caused by poliovirus.
Infantile paralysis.
Pathologic lesions: motor neurons in the gray matter in the anterior horn of the spinal cord..
Clinical feature:
Definition
Clinical feature: fever sore throat muscle pain paralysis
Etiology
Causative agent: poliovirus
family Picornaviridae, genus Enterovirus
single strain RNA
Resistance: Sensitive to heat, oxidant ultraviolet rays
Etiology
Serotype: on the basis of neutralization tests.
Type I
Type II
Type III
no cross immunity
Epidemiology
Source of infection patients and carriers: inapparent inf. & non-paralytic inf.
Route of transmission air-borne, respiratory tract: fecal-oral route:
Epidemiology
Susceptibility: universal susceptible to polio
covert infection >90%
paralytic patients<1%
lifelong immunity to same type virus
Epidemiologic features
children under 5yrs, 6m~5yrs
summer & fall
Pathogenesis
poliovirus air oral epithelial cells (in pharynx, intestine) regional lymphatics
Ab covert infection blood stream first viremia Ab abortive infection second viremia blood-brain barrier
CNS paralytic type non-paralytic type
Pathology
Place of lesion:
all of CNS
spinal cord, brain stem
motor neurons in anterior horns of cervical & lumbar enlargement of spinal cord.
Pathology
Pathologic features
neuron necrosis
inflammatory infiltrate of leukocyte,lymphocyte.
Clinical manifestation
Incubation period: 5~14 days
Clinical types
Covert infection: >90%
Abortive poliomyelitis: 4~8%
Non-paralytic poliomyelitis:
Paralytic poliomyelitis: 1%~2%
Clinical manifestation
Paralytic poliomyelitis
Prodromal period
preparalytic period
paralytic period
convalescent period
sequela period
Clinical manifestation
Prodromal period:(1~4d)
upper respiratory tact infection: fever, fatigue, sore throat, headache
intestinal tract infection: vomiting, diarrhea, constipation abortive poliomyelitis
Clinical manifestation
Preparalytic period
progressing this phase without prodromal phase
1~6days after symptoms of prodromal phase
without prodromal phase
Clinical manifestation
Preparalytic period
fever: two-hump fever(10~30%)
symptoms & signs of CNS
severe headache & vomiting
dysphoria or lethargy
muscle pain
Clinical manifestation
Preparalytic period
symptoms & signs of CNS
cutaneous hyperesthesia
hyperhidrosis
meningeal irritations (neck stiffness Kernigs & Brudzinskis signs positive) 3~6d , nonparalytic poliomyelitis
Clinical manifestation
Paralytic period
paralysis types
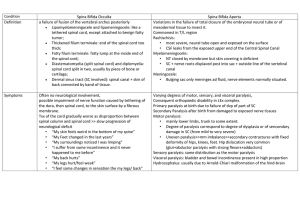
spinal type
brain stem type
mixed type
brain type
Clinical manifestation
Paralytic period
Spinal type: most common
paralysis features :
flaccid (hypomyotonia ,tendon reflexes are weak or absent)
asymmetric distribution:
without sensory loss
Clinical manifestation
Paralytic period
Spinal type: most common
paralysis muscles
paralysis of extremities: leg >arm; proximal
> distal
paralysis of diaphragmatic & intercostal muscles affects respiratory movement
paralysis of abdominal muscle -- stubborn constipation
Clinical manifestation
Paralytic period
Brain stem type
cranial nerve paralysis: 7&10, then 9&12, facial paresis
dysphagia, high-pitched voice
respiratory center paralysis:
central respiratory failure:
cacorhythmic breathing ect.
vasomotor center paralysis:
Clinical manifestation
Paralytic period
brain type - polio-encephalitis high fever, convulsion, disturbance of consciousness, tonic paralysis
mixed type spinal type + brain stem type
Clinical manifestation
Convalescent period
paralytic muscles begin to recover distal > proximal,
at first 3~4 month quick recovery,
6 month later recovery slowly,the recovery process reaches its limit around 18 months
Clinical manifestation
Sequela period
persistent paralysis
muscular atrophies
deformities of limbs
Laboratory Findings
Cerebrospinal fluid
aseptic menigitis
pleocytosis: 50~500
×
10 9 /L
protein: normal or slightly increase
albuminocytologic dissociation
glucose and chloride; normal
virus isolation: pharynx, feces, blood or CSF,brain.
Laboratory Findings
Serological test:
Specific IgM Ab (blood & CSF)
Neutralized Ab
Complement combining Ab four fold rise
Diagnosis
Epidemiological data:
Clinical manifestation:
Laboratory findings:
Abortive or non-paralytic polio
isolation of virus or serological test
paralytic polio - clinical diagnosis
Differential Diagnosis
Guillain-Barre Syndrome
symmetric, ascending paralysis with loss of sensation
CSF: protein elevate with absent or minimal pleocytosis, albuminocytologic dissociation
rapid and complete recovery
Differential Diagnosis
Paralysis caused by other enterovirus
Coxsackie or ECHO viruses: no epidemic no sequelae
Treatment
Prodromal & preparalytic P
isolation & rest in bed:
not accept muscular injection & operation
hot moist pack to muscles
50%GS&VitC 1~2g iv, IFN
hydrocortison
Treatment
Paralytic period:
limb paralysis
nursing for paralytic limbs
Put the limbs on function position
Vit C ATP ivdrop
Galanthamin or Prostipmin iM
Treatment
treatment for respiratory obstacle
bulbar paralysis
dysphgia
keep air way clear (sputum aspiration postural drainage )
tracheal intubation
tracheotomy tank respirator
Treatment
treatment for respiratory obstacle
respiratory center paralysis
respiratory stimulant
tracheotomy tank respirator
respiratory muscle paralysis
mild observation
tank respirator
Treatment
Convalescent & sequela period
acupuncture
massage
Prevention
control of source of infection:
isolation: 40 days after the onset of illness
protection of susceptible population :
attenuated live vaccine by oral killed virus vaccine