Group A (NI) - The Canadian Neonatal Network
advertisement

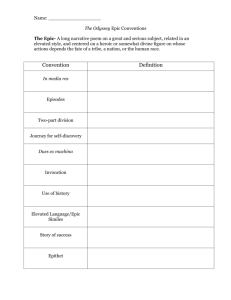
EPIC Evidence-based Practice Identification and Change Past, Present, and Future Shoo K. Lee, MBBS, FRCPC, PhD Director, Canadian Neonatal Network™ Scientific Director, iCARE Professor of Pediatrics, University of Alberta EPIC/PHSI Training Workshop November 9 & 10, 2006 Toronto ON Presentation Objectives • Overview how EPIC evolved • Describe the science behind EPIC • Describe future EPIC plans Background • Continuous Quality Improvement (CQI) methods have been investigated for reducing bronchopulmonary dysplasia (BPD) and nosocomial infection (NI) in the NICU • Limitation - existing CQI techniques employ a subjective, uncritical approach to practice change that may not be evidence based How did EPIC Evolve? Problems with traditional continuous quality improvement (CQI) approaches Subjective Not always evidence-based Seldom use data from institutions in question Mostly intra-institutional in nature Results are not always generalizeable We developed EPIC to improve upon traditional CQI approaches EPIC Objectives • To develop a new scientific method for QI – EPIC that is: (a) Evidence-based – uses published evidence (b) Objective – uses data from individual hospitals to identify practices for targeted intervention (c) Collaborative – uses a national network to share expertise and experience • To test whether EPIC reduces BPD and NI in a cluster randomized controlled trial of Canadian NICUs The Thee Pillars of EPIC 1. Objective Systematic reviews of evidence 2. Quantitative analysis Multi-centre outcomes and practices Identifies practices associated with outcome variation that can be targeted for intervention 3. Utilizes collective multi-disciplinary expertise Infection control, quality improvement, etc Method • • • • • • • • Prospective cluster randomized controlled trial 12 NICUs Randomization – 6 BPD, 6 NI Each group Control for other Additional controls - 5 other NICUs in CNN that were not participating in the study All infants < 32 weeks gestation were enrolled Definition: (a) BPD – O2 need at 36 weeks GA (b) NI – Positive Blood, CSF or Urine culture 2 phases (a) Baseline period (1 year) (b) Intervention period (2 years) Funded by Canadian Institutes of Health Research EPIC - Baseline Period (Year 1) • • • • • • • Baseline data collection on outcomes and practices Train multi-disciplinary hospital teams Review of published literature Meeting to share findings Identify Critical Care Pathways Qualitative research – identify barriers to change Data analysis – identify practice differences associated with outcome variation for targeted intervention Data Analysis to Identify Practices for Targeted Intervention • Grouped Data Analysis - compare outcome variations among NICUs - identify non-therapy and therapy related risk factors - estimate the attributable risk of risk factors • Individual Hospital Data Analysis - calculate hospital specific incidence rates - identify hospital specific risk factors for targeted intervention - conduct trend analysis using control charts • Generalized linear mixed effects model - to adjust results for the cluster randomized design • Monte Carlo Bootstrap Simulation - to estimate the 95% confidence limits for control charts Therapy Related Risk Factor for NI - PICC • Therapy related risks - central lines, - mechanical ventilation, - parenteral nutrition, - lack of enteral feeding • 40% of nosocomial infection associated with central lines • PICC lines carried highest risk Adjusted probability for developing nosocomial infection for PICC lines Line type Risk-Ratio for NI Umbilical catheters 2.0 Broviac cathethers 3.1 PICC catheters 3.5 EPIC – Intervention Period (2 Years) • • • • • • • Develop practice change strategies Prepare supporting materials NICU staff communication and training Implement practice change strategies Quarterly change cycles Control Chart feedback Revise strategies, reinforce change Results Group C EPIC Non-EPIC 5 NICU 12 NICU Excluded 1 NICU Group A Group B NI BPD NI BPD 5 NICU 6 NICU N = 2666 N = 3275 Control 5 NICU N = 1129 Selected Patient Characteristics Characteristics Number NI 2336 BPD 2316 Control 1129 Mean Gestation (wk) Mean Birthweight (kg) Mean SNAP-II Male sex (%) 28.5 1246 11.2 57.2 28.9 1315 9.8 55.5 28.9 1150 12.6 56.3 Outborn (%) Cesarean section (%) Apgar <7 at 5 min (%) 37.5 54.1 20.3 18.0 55.5 19.1 14.9 58.8 44.0 Antenatal steroids (%) 71.1 70.7 90.5 Group A (NI) – Incidence of NI Theoretical Infection Rate of Infant in NIT Group, NI Study (Monte Carlo Bootstrap, n=1000) 27.0% 25.0% 24.1% Percentage of infected baby 23.0% 21.0% 19.5% 19.0% 18.3% 17.1% 17.0% 16.1% 15.9% 16.0% 16.5% 15.0% 13.0% 12.6% 11.0% 9.0% Baseline Oct Dec.2003 JanM ar.2004 AprJun.2004 JulSept .2004 Study period Oct Dec.2004 JanM ar.2005 AprJun.2005 JulSept .2005 Group A (NI) – Incidence of BPD Observed Incidence Rate of CLD Baby at Week 36 in NIT Group, CLD Study 48.0% 44.0% 40.0% Percentage of CLD baby 38.9% 36.0% 32.0% 31.7% 29.3% 28.0% 28.2% 27.3% 25.4% 24.0% 23.8% 24.2% 23.1% 20.0% 16.0% Baseline Oct-Dec.2003 Jan-Mar.2004 Apr-Jun.2004 Jul-Sept.2004 Study period Oct-Dec.2004 Jan-Mar.2005 Apr-Jun.2005 Jul-Sept.2005 Group A (NI) – Duration of Oxygen Need Observed Length of Oxygen Support for CLD Baby in NIT Group, CLD Study 12 Mean length of oxygen support (day) 11 10 9.2 9 8.91 8.62 8.39 8 7.46 7.34 7 6.35 6.13 6 6.25 5 4 Baseline Oct-Dec.2003 Jan-Mar.2004 Apr-Jun.2004 Jul-Sept.2004 Study period Oct-Dec.2004 Jan-Mar.2005 Apr-Jun.2005 Jul-Sept.2005 Group B (BPD) – Incidence of BPD Group B (BPD) – Duration of Oxygen Need Group B (BPD) – Incidence of NI Theoretical Infection Rate of Infant in CLD Group, NI Study (Monte Carlo Bootstrap, n=1000) 23.0% 21.0% Percentage of infected baby 19.9% 19.0% 17.3% 17.0% 16.5% 15.0% 13.8% 13.7% 13.0% 12.7% 12.6% 11.2% 11.0% 10.4% 9.0% 7.0% Baseline Oct Dec.2003 JanM ar.2004 AprJun.2004 JulSept .2004 Study period Oct Dec.2004 JanM ar.2005 AprJun.2005 JulSept .2005 Group C (Controls) – Incidence of BPD Observed Incidence Rate of CLD Baby at Week 36 in Control Group, CLD Study 36.0% Percentage of CLD baby 31.0% 26.0% 24.7% 22.3% 22.6% 23.2% 22.5% 21.0% 18.6% 18.5% 16.0% 14.9% 14.7% 11.0% 6.0% Baseline Oct-Dec.2003 Jan-Mar.2004 Apr-Jun.2004 Jul-Sept.2004 Study period Oct-Dec.2004 Jan-Mar.2005 Apr-Jun.2005 Jul-Sept.2005 Group C (Controls) – Duration of Oxygen Need Observed Length of Oxygen Support for CLD Baby in Control Group, CLD Study 22 Mean length of oxygen support 9day) 20 18 16 14.64 14 13.73 13.33 12.76 12.58 12 11.88 11.48 10.43 10 8.62 8 6 4 Baseline Oct-Dec.2003 Jan-Mar.2004 Apr-Jun.2004 Jul-Sept.2004 Study period Oct-Dec.2004 Jan-Mar.2005 Apr-Jun.2005 Jul-Sept.2005 Group C (Controls) – Incidence of NI Percentage of NI(ever infected) control group (Non-EPIC group) 25.0% 20.0% 15.0% 14.5% 12.3% 16.0% 14.0% 13.7% 11.8% 10.0% 5.0% 10.3% 7.2% 6.0% 0.0% baseline Oct03- Jan04Dec03 Mar04 Apr04- Jul04- Oct04- Jan05- Apr05- Jul05Jun04 Sept04 Dec04 Mar05 Jun05 Sept05 Quarter Mortality, ROP, IVH Group A (NI) Group B (BPD) Group C (Control) Baseline 8th quarter P value Baseline 8th quarter P value Baseline 8th quarter P value 5.7 5.4 NS 5.0 4.2 NS 6.0 3.3 NS ROP >stage 3 9.5 8.5 NS 4.8 5.4 NS 5.1 7.9 NS IVH >grade 3 10.3 9.9 NS 7.8 9.6 NS 8.5 14.6 NS Mortality Conclusions • EPIC is effective at reducing NI and BPD in the NICU • Interventions targeting one outcome may affect other outcomes • EPIC may be more effective and less costly at improving quality of care than traditional CQI methods EPIC Research Program EPIC Process EPIC-I 2002-2005 EPIC/PHSI 2006-2009 EPIC-II 2007-2010 NIT reduced by 60% CLD reduced by 40% Target multiple outcomes Target two outcomes Test generalizeability Improve upon EPIC-I Target multiple outcomes Test generalizeability Improve upon EPIC/PHSI Improvements in EPIC/PHSI Eliminate feedback delays one button reports short term feedback & unverified data Decrease onus of data collection Use only relevant CNN data Facilitate communication Knowledge Broker Divide NICUs into 4 groups for quarterly teleconferences, site visits, mentorship Ease implementation 4 groups will have mix of experienced EPIC sites EPIC/PHSI Plan Make what we learned in EPIC-I available to all Canadian NICUs in EPIC/PHSI Training of Infection Teams – MD, RN, QI Introduce the EPIC interventions-best practice template Review EPIC-I literature reviews Review qualitative findings from EPIC-I Barriers and facilitators to change Develop change strategies for each NICU Implementation of EPIC interventions Acknowledgements to CIHR, Micheal Smith Foundation, & Canadian Neonatal NetworkTM EPIC Investigators • • • • • • • • • • • • • • Khalid Aziz, Memorial U Ross Baker, U of Toronto Keith Barrington, McGill U Catherine Cronin, U Manitoba Jill Hoube, UBC Andrew James, U Toronto Joanne Langley, Dalhousie David SC Lee, UWO Shoo K Lee, U Alberta Robert Liston, UBC Ying MacNab, UBC Claudio Martin, UWO Derek Matthew, Victoria Gen H Jochen Moehr, U Victoria • • • • • • • • • • • • Arne Ohlsson, U Toronto Abraham Peliowski, U Alberta Robert Platt, McGill U K. Sankaran, U Saskatchewan Mary Seshia, U Manitoba Nalini Singhal, U Calgary Bonnie Stevens, U Toronto Anne Synnes, UBC Paul Thiesen, BC Children’s H Peter Von Dadelszen, UBC Robin Walker, U Ottawa Elizabeth Whynot, BC Women’s • Robin Whyte, Dalhousie U • John Zupancic, Harvard U