URF Fundraiser - The Prostate Net
advertisement

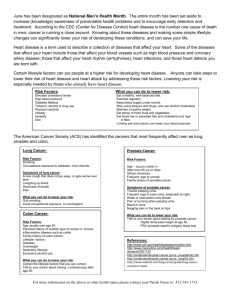
Translational Cancer Research From Laboratory to Practice William J Catalona MD Professor of Urology Director, Clinical Prostate Cancer Program Northwestern University Chicago, Illinois Cancer in Perspective In the US and Globally US Mortality, 2006 Rank Cause of Death No. of % of all deaths deaths • • • 1. Heart Diseases 631,636 26.0 2. Cancer 559,888 23.1 • • • • • • • • • • • 3. Cerebrovascular diseases 137,119 5.7 4. Chronic lower respiratory diseases 124,583 5.1 5. Accidents (unintentional injuries) 121,599 5.0 6. Diabetes mellitus 72,449 3.0 7. Alzheimer disease 72,432 3.0 8. Influenza & pneumonia 56,326 2.3 • 9. Nephritis* 45,344 1.9 • 10. Septicemia 34,234 1.4 *Includes nephrotic syndrome and nephrosis. Source: US Mortality Data 2006, National Center for Health Statistics, Centers for Disease Control and Prevention, 2009. 2009 Estimated US Cancer Cases* Men 766,130 Women 713,220 Prostate 25% 27% Breast Lung & bronchus 15% 14% Lung & bronchus Colon & rectum 10% 10% Colon & rectum Urinary bladder 7% 6% Uterine corpus Melanoma of skin 5% 4% Non-Hodgkin lymphoma 5% Non-Hodgkin lymphoma 4% Melanoma of skin Kidney & renal pelvis 5% 4% Thyroid Leukemia 3% 3% Kidney & renal pelvis Oral cavity 3% 3% Ovary Pancreas 3% 3% Pancreas 19% 22% All Other Sites All Other Sites *Excludes basal and squamous cell skin cancers and in situ carcinomas except urinary bladder. Source: American Cancer Society, 2009. Lifetime Probability of Developing Cancer, Men, 2003-2005* Site Risk All sites† Prostate 1 in 2 1 in 6 Lung and bronchus 1 in 13 Colon and rectum 1 in 18 Urinary bladder‡ 1 in 27 Melanoma§ 1 in 39 Non-Hodgkin lymphoma 1 in 45 Kidney 1 in 57 Leukemia 1 in 67 Oral Cavity 1 in 72 Stomach 1 in 90 * For those free of cancer at beginning of age interval. † All Sites exclude basal and squamous cell skin cancers and in situ cancers except urinary bladder. ‡ Includes invasive and in situ cancer cases § Statistic for white men. Source: DevCan: Probability of Developing or Dying of Cancer Software, Version 6.3.0 Statistical Research and Applications Branch, NCI, 2008. http://srab.cancer.gov/devcan Lifetime Probability of Developing Cancer, Women, US, 2003-2005* Site Risk All sites† Breast 1 in 3 1 in 8 Lung & bronchus 1 in 16 Colon & rectum 1 in 20 Uterine corpus 1 in 40 Non-Hodgkin lymphoma 1 in 53 Urinary bladder‡ 1 in 84 Melanoma§ 1 in 58 Ovary 1 in 72 Pancreas 1 in 75 Uterine cervix 1 in 145 * For those free of cancer at beginning of age interval. † All Sites exclude basal and squamous cell skin cancers and in situ cancers except urinary bladder. ‡ Includes invasive and in situ cancer cases § Statistic for white women. Source: DevCan: Probability of Developing or Dying of Cancer Software, Version 6.3.0 Statistical Research and Applications Branch, NCI, 2008. http://srab.cancer.gov/devcan Cancer Incidence Rates* Among Men, US, 1975-2005 PSA Era Rate Per 100,000 250 Prostate 200 150 Lung & bronchus 100 Colon and rectum 50 Urinary bladder Non-Hodgkin lymphoma Melanoma of the skin 0 1975 1978 1981 1984 1987 1990 1993 1996 1999 2002 2005 Cancer Incidence Rates* Among Women, US, 1975-2005 Rate Per 100,000 250 200 150 Breast 100 Colon and rectum Lung & bronchus 50 Uterine Corpus Ovary 0 1975 Non-Hodgkin lymphoma 1978 1981 1984 1987 1990 1993 1996 1999 2002 *Age-adjusted to the 2000 US standard population and adjusted for delays in reporting. Source: Surveillance, Epidemiology, and End Results Program, Delay-adjusted Incidence database: SEER Incidence Delay-adjusted Rates, 9 Registries, 1975-2005, National Cancer Institute, 2008. 2005 2009 Estimated US Cancer Deaths* Men 292,540 Women 269,800 30% 26% Lung & bronchus Prostate 9% 15% Breast Colon & rectum 9% 9% Colon & rectum Pancreas 6% 6% Pancreas Leukemia 4% 5% Ovary Liver & intrahepatic bile duct 4% 4% Non-Hodgkin lymphoma Esophagus 4% 3% Leukemia Urinary bladder 3% 3% Uterine corpus Non-Hodgkin lymphoma 3% 2% Liver & intrahepatic bile duct Kidney & renal pelvis 3% 2% Brain/ONS 25% 25% Lung & bronchus All other sites ONS=Other nervous system. Source: American Cancer Society, 2009. All other sites Cancer Death Rates* Among Men, US,1930-2005 100 Rate Per 100,000 Lung & bronchus 80 60 PSA Era Stomach Prostate 40 Colon & rectum 20 Pancreas *Age-adjusted to the 2000 US standard population. Source: US Mortality Data 1960-2005, US Mortality Volumes 1930-1959, National Center for Health Statistics, Centers for Disease Control and Prevention, 2008. 2005 2000 1995 1990 1985 1980 1975 1970 1965 1960 1955 Liver 1950 1945 1940 1935 0 1930 Leukemia Cancer Death Rates* Among Women, US,1930-2005 100 Rate Per 100,000 80 60 Lung & bronchus 40 Uterus Breast Colon & rectum Stomach 20 Ovary *Age-adjusted to the 2000 US standard population. Source: US Mortality Data 1960-2005, US Mortality Volumes 1930-1959, National Center for Health Statistics, Centers for Disease Control and Prevention, 2008. 2005 2000 1995 1990 1985 1980 1975 1970 1965 1960 1955 1950 1945 1940 1935 Pancreas 1930 0 Trends in the Number of Cancer Deaths Among Men and Women, US, 1930-2006 300,000 295,000 290,000 Men 285,000 250,000 280,000 Women 275,000 200,000 270,000 Women 265,000 150,000 20 00 20 01 20 02 20 03 20 04 20 05 20 06 Number of Cancer Deaths Men 100,000 50,000 0 1930 1940 1950 1960 1970 1980 1990 2000 Source: US Mortality Data, 1930-2006, National Center for Health Statistics, Centers for Disease Control and Prevention, 2009. Stage of Cancer at the Time of Detection and 5-Year Survival Rates by Stage Stage at Diagnosis 5-Year Survival for Stage Does PSA Screening Save Lives? • • • • Flawed “PLCO study” from the U.S. study: No Better “ERSPC study” from Europe: Yes, by at least 20% Best “Goteborg study” with longer follow-up, by 44% to 56% Recent* Prostate-Specific Antigen (PSA) Test Prevalence (%), by Educational Attainment and Health Insurance Status, Men 50 Years and Older, US, 2001-2006 70 Prevalence (%) 60 58 55 2001 2004 52 50 2002 2006 54 46 42 40 39 40 30 30 28 25 27 20 10 0 Total Less than a high school education No health insurance *A prostate-specific antigen (PSA) test within the past year. Note: Data from participating states and the District of Columbia were aggregated to represent the United States. Source: Behavioral Risk Factor Surveillance System Public Use Data Tape (2001, 2002, 2004, 2006), National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, 2002, 2003, 2005, 2007. What are the latest guidelines for PSA testing? 2009 NCCN Guidelines for PCa Detection • National Comprehensive Cancer Network (NCCN) • “PSA testing is effective and needs to be more rigorously conducted in high-risk men” • “… at age 40, high-risk men be offered a baseline PSA and prostate exam and if their PSA is 1.0 or greater, they should have annual follow-up testing • Consider prostate biopsy for PSA is higher than 2.5 or increasing by more than 0.35 per year 2010 NCCN Guidelines • “Screening in men over 75 years should be considered individually” • “It is neither the intent nor the suggestion of the panel that all men diagnosed with prostate cancer require treatment” 2009 NCCN PCa Management Guidelines • A significant change incorporated into the updated NCCN Guidelines for PCa is the recommendation for active surveillance for many men • “Very low risk” category added using a modified Epstein criteria. Only AS offered and recommended in this category when life expectancy is < 20 years • Men with “low-risk’ prostate cancer who have a life expectancy of less than 10 years should be offered and recommended active surveillance • “Together, you and your doctor can carefully weigh several factors to determine whether active surveillance—that is, not treating the cancer, but instead watching for any indication that the cancer is growing—might be the best course of action” What about active surveillance or watchful waiting? Toronto active surveillance update • UNPROVEN HYPOTHESIS: active surveillance may reduce overtreatment while retaining option for curative treatment if the cancer is progressing • 47% whose cancer was found to be progressing were free of tumor recurrence after 5 yrs • Less than 50% had cancer that was still contained in the prostate at the time of surgery • In Swedish watchful waiting series with 20 years of follow-up, almost 50% died of prostate cancer Johns Hopkins: RRP in Patients Failing Active Surveillance • 48 patients who failed active surveillance and were treated with surgery • 35% had extension of cancer outside the prostate gland, 15% had cancer at the surgical margins, 6% had seminal vesicle/lymph node involvement Does prostate cancer run in families? Prostate Cancer Risk Allele Discovery: Collaboration of William Catalona with deCODE genetics, Inc. Locus SNP OR Chicago OR All Combined 8q24 rs1447295 1.50 1.53 Amundadottir et al. Nature Genetics 2006 Gudmundsson et al. Nature Genetics 2007a 8q24 rs16901979 2.32 1.66 Gudmundsson et al. Nature Genetics 2007a 17q12 rs4430796 1.41 1.22 Gudmundsson et al. Nature Genetics 2007b 17q24 rs1859962 1.25 1.20 Gudmundsson et al. Nature Genetics 2007b 2p15 rs721048 1.22 1.15 Gudmundsson et al. Nature Genetics2008 Xp11.22 rs5945572 1.23 1.23 Gudmundsson et al. Nature Genetics 2008 5p15 rs401681 1.06 1.07 Rafnar et al. Nature Genetics 2008 5p15 rs2736098 1.20 1.13 Rafnar et al. Nature Genetics 2008 3q21 s10934853 1.21 1.12 Gudmundsson et al. Nature Genetics 2009 8q24 rs16902094 1.16 1.21 Gudmundsson et al. Nature Genetics 2009 19q13 rs8102476 1.15 1.12 Gudmundsson et al. Nature Genetics 2009 11q13 refinement SNP rs11228565 1.16 1.23 Gudmundsson et al. Nature Genetics 2009 Reference Might prostate cancer patients carry genetic variants that predispose to other types of cancer? Do genetic factors determine prostate cancer aggressiveness? Identification of factors associated with risk for aggressive PCa is urgently needed Prostate SPOREs Genetics Working Group Specialized Program Of Research Excellence • William Catalona co-chair • Janet Stanford co-chair Northwestern Fred Hutchinson CC • • • • • • • Mayo Clinic Memorial Sloan-Kettering UCSF Harvard Michigan Baylor Johns Hopkins Robert Jenkins Robert Klein John Witte Matt Freedman Kathy Cooney Michael Ittmann William B. Isaacs • Alternates • Ken Offit • Phil Febbo Memorial Sloan-Kettering U Calif San Francisco What else is in the pipeline? A new “nanotechnology” PSA blood test that is 300 times more sensitive than currentlyavailable tests Pro-PSA (p2PSA) Multicenter Pivotal Trial (Beckman-Coulter Incorporated) Pro-PSA is more accurate than PSA for detecting prostate cancer and aggressive forms of the disease William J. Catalona, MD, Lead Investigator. Sites: Baylor, Erasmus, Harvard, Johns Hopkins, Mayo, Michigan, Northwestern, UCLA All subject enrollment and sample testing has been completed. The database is locked and all analyses are complete. All monitoring has been completed. BCI audits at 5 sites are complete. Close-out visits have been completed at 3 sites and all remaining close-out visits have been scheduled for this year. EU approval was received July 2009 and product is available in the EU as of 10/16/09. FDA submission Review of the clinical section of the FDA submission is complete and has been forwarded to the BCI regulatory department for final review. The primary and secondary hypotheses were verified. Results look good. FDA submission for approval in November 2009.