Common Voice Disorders
advertisement

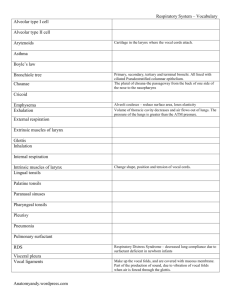
Internal Medicine Grand Rounds: February 28th, 2007 Current Diagnosis and Treatment of Voice Disorders Seth H. Dailey, MD Assistant Professor University of Wisconsin Hospital and Clinics University of Wisconsin School of Medicine Cartilaginous skeleton Intrinsic Musculature • Abductors • Adductors • Tensors Intrinsic Musculature Innervation Abduction Adduction Tension Vocal Fold Anatomy Laryngeal Anatomy • Three surrounding structures- pharynx, trachea and esophagus • Three levels - supraglottis, glottis and subglottis • Three fixed structures - hyoid, thyroid and cricoid • Three mobile structures -epiglottis, false vocal cords and true vocal cords (folds) Laryngeal Anatomy Laryngeal Anatomy Mucosal wave/Phase delay Body-Cover Theory • Changes to mucosal wave – Stiffness – tension Mucosal wave • Velocity increases – Increased airflow – Increased subglottic pressure Laryngeal Physiology • Three main functions - airway, swallowing and voice • Three criteria for voice- generator, vibrator resonator • Three components for high quality glottic voice - closure, pliability and symmetry Indirect mirror examination • Advantages – Quick – Inexpensive – Little equipment • Disadvantages – Gag – Anatomic features – nonphysiologic Flexible laryngoscopy • Advantages – Well tolerated – Complete examination – Video documentation • Disadvantages – More time – Expensive Rigid laryngoscopy • Advantages – Best images – Magnification – Video documentation • Disadvantages – – – – Expensive Nonphysiologic Gag Anatomic features Common disorders affect the “magic three” • Closure - neuromuscular, joint, vocal fold • Pliability - “golden layer” - mass, scar • Symmetry - tension and viscoelasticity • VOICE DISORDERS ARISE FROM A COMBINATION OF THESE ELEMENTS Differential Diagnosis of Hoarseness • Vocal quality- determined by: – distance between vocal cords, – tenseness of the cords – how rapid cords vibrate • Hoarseness is caused by – Differential Diagnosis of Hoarseness Types of voice • Breathy- vocal cords do not approximate so air escapes. • Raspy- harsh voice. Cord thickening due to edema or inflammation. Voice is low in pitch and poor quality Differential Diagnosis of Hoarseness Types of voice • Muffled voice- painful dysphagia and dyspnea • Shaky- high pitch or low soft. – Elderly – debilitated Differential Diagnosis of Hoarseness Acute Hoarseness/Acute Laryngitis • Laryngeal mucous membrane infection, usually viral (adenovirus/ influenza, RSV, coxsackie, rhinovirus) • Also can be due to trauma to throat, vocal abuse, toxic exposure, GI complications, smoking, allergy Differential Diagnosis of Hoarseness Acute Hoarseness/Acute Laryngitis • • • • • • Hoarseness Cough Sore throat Fever Vesicles on soft palate Lymphadenopathy Differential Diagnosis of Hoarseness Acute Hoarseness/Acute Laryngitis • Diagnostics: Laryngoscopy if suspect mass, infection, vocal cord dysfunction • Management: Voice rest, smoking/alcohol cessation, hydration Evaluation of Hoarseness • History is paramount • Projection - tired, breathy and low volume • Quality - ”hoarse”, “gruff”, “raspy” • Range - high, middle and low Evaluation of Hoarseness • • • • • • • • Physical Exam Speaking voice Range profile Fundamental Frequency – F0 Maximum Phonation Time Standard Reading Passages Singing if appropriate – local, regional, bodywide Voice Lab – Acoustics and Aerodynamics Evaluation of Hoarseness • Endoscopic exam – • mirror, flexible endoscope, rigid endoscope • Digital archiving essential for documentation Evaluation of Hoarseness • Studies • CT scan – evaluation of course of RLN • EMG – Is there an nerve to muscle problem? • Double pH probe – What is the severity of Laryngopharyngeal reflux (LPR)? • Microlaryngoscopy – some lesions missed in the office. Evaluation of Hoarseness • Studies – the future…. • Aerodynamics and acoustics – Chaos theory and mathematical modeling • Vocal cord motion – gross arytenoid motion being evaluated endoscopically • Vocal cord pliability – endoscopic rheometers and vocal fold oscillators • Ocular Coherence Tomography/Ultrasound Normal Stroboscopy Neuromuscular Disorders • • • • • Vocal cord paralysis Vocal cord paresis Cricoarytenoid joint dysmobility Presbylaryngis (aging larynx) Muscle Tension Dysphonia (Hyperfunction) Vocal Cord Paralysis • Thoracic, thyroid surgery, “Bell’s” palsy of the larynx • Closure and symmetry • Swallowing and voice • Static Repair - Watch and wait, temporary procedure, permanent procedure (Laryngoplasty). • Dynamic repair Nerve Muscle Transosition Vocal Cord Paresis Vocal Cord Paralysis 2 Videostroboscopy Radiographic studies • MRI • CT Laryngeal EMG • Myopathy – normal frequency of firing but decreased amplitude • Neuropathy – decreased frequency but occasional normal amplitudes • Polyphasic reinnervation potentials indicate some loss of function but reinnervation has begun Laryngeal EMG Differential • • • • • • • • Congenital Inflammatory Neoplastic Traumatic Neurologic Endocrine Iatrogenic Local factors Vocal Cysts Vocal Nodules • Usually bilateral • Voice rest and speech therapy for 6 months • Surgical removal Vocal cord granulomas • LPR • Intubation • Treat medically Glottal Incompetence • • • • • • A “Leaky Valve” pure and simple Loss of total vocal fold volume Loss of pliable layer from use and scar Most often a function of age Temporary Injectables – fat and collagen Permanent – Gore-tex, silastic etc. Cricoarytenoid Joint Dysmobility • • • • • • Intubation, rheumatoid, osteoarthritis Limit range of movement Can’t open or close Voice and airway Medical therapy if appropriate Surgery - move or remove arytenoid Hyperfunction – a.k.a. MTD • • • • • Overactivity of supraglottal musculature Compresses and alters the airstream Often normal glottic function Inciting events can be ANYTHING Voice therapy is used to get the voice “back on track” Epithelial Diseases • Papilloma • Premalignancy (Vocal cord dysplasia) • Malignancy Vocal Cord Papilloma • • • • • • • Most common benign tumor of vcs Pediatric and adult forms Voice and airway Surgery - mechanical or laser debulking Anti-virals in children High risk of permanent dysphonia 585nm Pulsed Dye Laser – Treatment can now be done in the office!!! Vocal Cord Keratosis with Atypia • • • • • • • Smoking and alcohol Repetitive chemical insult to vocal folds Dysplasia into cancer Closure, pliability and symmetry Radiation therapy - not recommended Phonomicrosurgery Pulsed Dye Laser - Treatment can now be done in the office!!! Vocal Cord Cancer • • • • • • • • Smoking and Drinking are synergistic U.S. - 2/3 glottic, Europe 2/3 supraglottic Hoarseness Closure pliability and symmetry Voice and airway Radiation Ultra-narrow margin surgery Endoscopic approach for early cancers – increasing evidence for late cancer also Subepithelial Diseases • • • • • • Vocal cord nodules Vocal cord polyps Vocal cord cysts Reinke’s edema Vocal cord sulcus Vocal cord scar Vocal Cord Nodules • • • • • • Vocal overuse Repetitive microtrauma to mid vocal folds Closure and pliability Reduce demands Voice therapy Surgery – Surgeons much less likely than previously to operate unless firm Vocal Cord Nodules 1 Vocal Cord Nodules 2 Vocal Cord Polyp • • • • • • Vocal overuse Repetitive microtrauma to mid vocal folds Closure and pliability Reduce demands Voice therapy Surgery – Instrumentation and even robotics being applied to improve precision and safety Vocal Fold Cyst • • • • • • Congenital anomaly Uni or bilateral Mucus or keratin Closure, pliability and symmetry Voice only affected Surgery - excise, but not likely to have a normal voice Reinke’s Edema • Benign enlargement and alteration of golden layer • Adult female smokers • Closure, pliability and symmetry • Voice and airway • Surgery - cytoreduction of SLP • Return almost to normal Vocal Fold Scar • Forms at the junction of epithelium and golden layer (SLP) • Decreases the pliability of the membrane • Decreases the closure and therefore the efficiency • Fatigue and projection problems are common • LOSS OF UPPER REGISTER!!! Vocal Cord Sulcus • • • • • • • Developmental loss of SLP Decreased pliability Loss of cycle-to-cycle closure Management with surgery is best hope Slicing technique Fat implantation Medialization Thyroplasty Vocal Cord Inflammatory Diseases • Reflux Laryngopharyngitis (LPR) • Arytenoid Granuloma Arytenoid Granuloma • • • • • • Cartilaginous vocal cord mass Exposed cartilage and acid reflux? Supraglottic modulation of air Voice and airway Surgery - rarely indicated Voice therapy, LPR, inhaled steroids, BOTOX Vocal Cysts Vocal Nodules • Usually bilateral • Voice rest and speech therapy for 6 months • Surgical removal Vocal cord granulomas • LPR • Intubation • Treat medically Vocal Cord Paralysis • Lesion at nuclear level – cadaveric • Lesion above nodose ganglion – abducted • Lesion below nodose ganglion - paramedian Vocal Cord Paralysis • Superior laryngeal nerve – subtle voice changes with decreased pitch range, tilting of the larynx with a rotation of the glottis Vocal Cord Paralysis • Children – Neurologic – Traumatic – Idiopathic • Adults – – – – – Iatrogenic Traumatic Neoplastic Idiopathic neurologic THANK YOU !!! Rule of Thumb • Any patient with hoarseness of two weeks duration or longer must undergo visualization of the vocal cords